Abstract
Romania faces significant disparities in access to emergency healthcare. This study employs a national geospatial analysis and network-based GIS modelling to assess current spatial accessibility to emergency care services and to develop a scenario-based spatial model for Romania, aiming to improve access to these services. This study is the first to design such a scenario and to do so at a national level. To improve access to the emergency network, this study proposes establishing additional emergency units at designated hospitals. Integrating national-scale data into the Network Analyst tools, we identify critical gaps in emergency service coverage, with current estimates indicating that approximately 65% of the rural population lives in areas with limited or no access to emergency care. Travel time to the nearest emergency care unit exceeds 120 min in remote rural regions, highlighting a severe spatial inequity in healthcare provision. The results show that in our scenario, the total proportion of the population that has to travel for more than 30 min to the nearest emergency care unit has dropped from almost 60.28% to 35.63% when travelling in a private car, and from 72.58% to 46.08% when travelling in an ambulance. In fact, the total number of inhabitants reaching an emergency facility within 30 min increases by more than 4.7 million when travelling by private car and by more than 5 million when travelling by ambulance. These findings underscore the importance of spatial planning in the development of healthcare infrastructure and provide quantitative, spatially explicit evidence to support infrastructure planning and policy decisions aimed at reducing the urban–rural healthcare divide. This study contributes to the broader discourse on spatial justice and health equity, offering local or national authorities a basis for developing improved healthcare policies to improve coverage and reduce the urban–rural healthcare divide.
1. Introduction
Healthcare accessibility has been an intensely debated topic over recent decades. Studies have addressed not only the spatial accessibility to medical services but also the various factors influencing an individual’s capacity to access healthcare [1,2]. While some authors define accessibility as the degree “of fit between the consumer and the system”, with a better fit, reflecting better access, more often studies characterise accessibility to health services as the ability of the population to request and obtain medical care [3]. According to McEntee [4], the core of accessibility is “the use of services”, but recent studies stipulate that the discussion should be oriented more towards the capacity to reach different services, with accessibility being influenced based on the hierarchy, importance, number and territorial display of facilities [5,6,7]. Over the past few decades, many researchers have recognised the four dimensions of accessibility: acceptability, affordability, availability, and physical location [8,9].
In discussing healthcare, Peters [8] defines accessibility as the ability of each individual to reach and meet their needs for medical services. The difficulties associated with identifying specific types of healthcare inequity stem from varying definitions and their underlying objective of ensuring geographical accessibility [10]. In line with this, Mooney defines six distinct types of inequities, one of them being equality of access for equal need [11,12]. Accessibility studies usually fall into two distinct sets. The first adopt methodologies based on datasets, yielding hypothetical results. These are often reported at the population level and discuss “potential accessibility”. The other set of studies relies on direct observation and addresses “observed accessibility”. They differ in their findings: while the first produce objective results, relevant on a general, macro scale, the latter provide subjective outcomes, which are often reported at the individual level [13]. With an increased concern in recent decades regarding the dysfunctions of medical systems when serving the general population, Mayaud discussed the need for equal accessibility to be considered a crucial dimension of the modern medical system [14]. One relevant concept in this discussion is that of spatial justice. It has its theoretical origins in the work of Durand and Lefebvre, who first argued that territorial social inequalities are transformed into territorial inequalities [15]. Over time, the concept was taken up by Harvey, who explored how unequally distributed economic resources are reflected at the level of a territory [16]. However, after 2010, it was clearly defined as the equitable distribution of services, social resources, and opportunities to every individual in a community [17]. More recently, the concept has extended to reducing social discrepancies at the territorial level, and it is widely applied in planning, social geographies, studies on smart cities, and transportation and mobility [18]. This is where this study responds to the current needs of the specialised literature as well as the decision-making process that authorities must undergo when improving healthcare accessibility, especially accessibility to a highly sought-after service: emergency care.
Emergencies are often viewed in the specialised literature as the most readily available healthcare services that respond to critical situations [19]. Access to emergency care quantifies levels of accessibility, aiming to demonstrate a lack of planning in facility distribution and/or identify existing geographical barriers to access, a common concern in modern studies [20]. More detailed analyses identify inequities and vulnerabilities in a healthcare network, studying access by emergency typologies, quantifying access by age, or by health needs, as seen in Brenner [21] and Turner [22].
Apart from mathematical methods, such as Cartesian methods applied at different geographical scales, and the Euclidean and Manhattan distances, which measure the shortest path in a straight line or the distance between two points on a rectangular grid [23], the recent literature has increasingly been dominated by GIS methods ranging from kernel density to network analysis [24]. GIS methodologies have become more and more popular due to their strong alignment with geographical realities [25,26]. These methods are effective in highlighting territorial disparities in health service provision and identifying areas that need improved access [27]. Most common methods, like the gravity-based model [28,29], the provider-to-population ratio [30], and the two-step floating catchment area (2FCSA), quantify the relationship between space and population by either specifying a certain number of health providers or accounting for access and costs [31,32]. 2FSCA, for example, was adapted, developed, and re-adapted by different authors [33,34], and has contributed to a better understanding of the costs associated with accessibility to various healthcare services over time [32]. Recent studies using 2FSCA proved that more remote areas will always have higher costs and poorer access [35,36,37]. By relating distances to the resident population and medical infrastructure, GIS methods have been used to highlight territorial deficiencies and dysfunctions [38,39] and pressing needs of health systems worldwide [7], analysing populations on a large scale [40], with a focus on the accessibility of target groups in society, such as studies of elderly access [25,41] or access to specific types of health services [42,43,44]. They are useful for identifying neonatal care resources [45], disparities in cardiovascular infrastructure and needs [42], inequities in population–provider relations [43], and even showing a lack of medical personnel in developed countries, such as Japan’s rural areas [44]. Moreover, GIS studies on accessibility have come to treat multivalent accessibility with different means of transport [7], showing differences in access between public transport, private car, or even in the case of walking [46], showing an increase in interest in the field of transportation mode and routes [47]. Our study builds upon the international discourse on spatial justice, contributing an empirical and methodological perspective from an under-researched European context. While comparable GIS-based studies have been conducted in Finland [6], Japan [36], and Brazil [14], a comprehensive national-scale analysis for Romania has not yet been undertaken. By applying network-based GIS modelling, this research extends the global evidence base on healthcare accessibility to include Eastern Europe and provides a transferable analytical framework for other regions facing similar infrastructural constraints.
In Romania, studies on healthcare accessibility have predominantly focused on public hospitals [48] and, to a lesser extent, in cardiovascular hospitals [42]. Alternatively, newer approaches addressed the lack of accessibility to vaccine centres during the COVID-19 pandemic [49]. These analyses have brought attention to the uneven distribution of medical infrastructure, particularly highlighting disparities between urban and rural areas, or the existence of medical deserts. While research [48] has revealed shortcomings in the Romanian healthcare system—such as workforce shortages and insufficient planning—there remains a notable lack of comprehensive studies of emergency healthcare provision, emergency care service accessibility, and the spatial inequalities that persist across the different regions of the country.
The Romanian healthcare system and infrastructure developed, after the Second World War, based on the Semanko model, in which most healthcare units, and specifically hospitals—as the most important ones—were placed and developed in urban areas, leaving the rural parts of the country depending on small health centres. The same highly centralised Semanko model has been implemented in other countries from Central and Eastern Europe and the former USSR [50]. Although Romania has undergone a series of reforms to its medical system since the 1989 fall of the communist regime, the distribution of the main resources still reflects the Semanko pattern. Additionally, the country has a complex topography, which makes it a particularly pertinent case for GIS-based accessibility analysis. Consequently, accessibility studies conducted in Romania are relevant to several other territories, as they respond to an international need for replicability.
The Romanian emergency healthcare system is organised around a network of public hospital-based emergency departments and coordinated ambulance services. The delivery of emergency care is primarily facilitated by Emergency Receiving Units (ERU) and Emergency Receiving Compartments (ERC). These facilities are complemented by a network of ambulance stations and substations operated by County Ambulance Services (CAS) [51]. Significant obstacles persist regarding comprehensive coverage and reducing response times, particularly in remote rural communities due to infrastructure limitations and shortages of medical personnel. These characteristics make Romania an ideal case for evaluating how spatial configuration affects access to emergency services.
This study represents the first attempt in Romania to address the issue of accessibility to emergency healthcare services at 1 km2 grids. The objectives of this study are to evaluate the existing accessibility to emergency care and propose an improved configuration of the emergency network through a scenario-based spatial analysis. This research offers the first national-level GIS assessment of emergency healthcare accessibility in Romania and introduces an improved model, according to specific criteria, to support health policy and spatial planning decisions. These proposals build on the existing health infrastructure and could significantly improve access to healthcare services for the population, such as reducing response times for critical emergencies and ensuring equitable healthcare delivery in underserved areas.
2. Materials and Methods
2.1. Data
2.1.1. The Emergency Healthcare Network
In Romania, the emergency healthcare network is structured on three levels of emergency care units [52,53], depending on the rank of the hospital they are attached to:
Specialised Emergency Receiving Compartments (ERC-S) are the fewest; they are found only in very specialised hospitals, classified as rank I, which offer highly specialised treatment. These hospitals are located in the largest cities of the country.
Emergency Receiving Units (ERU) are usually located in County Hospitals, Regional Hospitals or University Hospitals, classified either as rank I but most often as rank II units, that have emergency medicine specialists/doctors, residents, nurses with specific training, advanced equipment (Computed Tomography, permanent laboratory, resuscitation rooms, mobile intensive care) and function by priority code flows (red, yellow, green, blue, white).
Emergency Receiving Compartments (ERC) are found in rank III hospitals. These units are smaller and depend administratively and professionally on a county/regional ERU, as they can only treat emergencies of minor or moderate severity. For serious cases (major trauma, heart attack, vascular accidents, complex surgical emergencies), the ERC stabilises the patients and then transfers them to a hospital with ERU.
The Romanian public hospital network also includes rank IV and V units, but these have limited capacity or operate within a single medical speciality and cannot provide emergency care; they can only cover consultancies in their guard rooms. Apart from these, nine units have not been assigned to any rank [54].
Data on emergency units were collected from the website of each public hospital, aiming to track operational emergency units.
2.1.2. New Proposed Emergency Healthcare Units (PEU)
To improve access, we considered potential new locations for ERC and identified 65 facilities in total. Based on the latest available list of public hospitals on the Health Ministry’s Website (https://www.ms.ro/ro/; accessed on 12 May 2025), the selected 65 public hospitals are ranked as III units that do not currently have an ERC. The reasoning behind this choice was that rank III hospitals can offer basic healthcare services and equipping them with an ERC would be less of a financial burden than setting up such an emergency unit in a rank IV or V hospital.
The 65 PEU locations were identified through a selection process based on three spatial variables: population size, population density, and proximity to existing emergency care facilities. These criteria were integrated using spatial overlay and network distance analysis in ArcGIS Pro 3.0, aiming to identify locations that would most effectively enhance service coverage in underserved regions. Although this approach does not include an explicit objective function or algorithmic decision variables, it represents a scenario designed to simulate potential improvements to the national emergency care network.
As the first criterion, only hospitals located in towns with populations greater than 5000 inhabitants were considered. This threshold ensures that the selected locations serve a sufficiently large community to justify the establishment of an emergency healthcare facility both administratively and financially.
In addition to the population size, population density was a second criterion. Only areas with a density exceeding 100 inhabitants per square kilometre were included, as higher density indicates a greater need for accessible emergency services.
Finally, proximity to existing emergency care facilities was considered. Specifically, we only included towns situated more than 20 km from the nearest hospital equipped with emergency healthcare units. This criterion was designed to target areas currently underserved by the emergency healthcare network, thereby reducing response times and improving overall accessibility for the population.
2.1.3. Ambulance Station and Sub-Station Network
Transport to emergency healthcare services in Romania is typically provided by ambulances. They depart from locations near hospitals in stations and substations, organised at the county level, to facilitate intervention times and transportation to hospitals. To obtain ambulance data, we utilised the actual network of stations and substations available on the Ministry of Health’s website (https://www.ms.ro/ro/; accessed on 15 April 2025) and identified a total of 353 ambulance stations and substations that are relatively uniformly localised across the country. These were considered as departure points in calculating the travel time by ambulance.
2.1.4. Population Data
Population data were collected online from the website of the European Environment Agency (https://www.eea.europa.eu/en; accessed on 12 April 2025). We utilised the latest available open-source population grids, available at a 1 square kilometre resolution, in .shp format. We extracted data sets for Romania containing population data from the last census (2021). We chose only the grids containing population. Additionally, we utilised .shp public data from ANCPI (https://www.ancpi.ro/; accessed on 20 March 2025), which includes all Local Administrative Units (LAU2), to calculate densities and to extract population statistics by urban/rural localities.
2.1.5. Road Data Collecting and Mapping
Romania had at the end of 2024 a total of 86,847 km of public roads, from which only 51.5% are modernised, being covered with heavy-medium asphalt surfaces. 23.7% are covered with thin-surfaced asphalt and over 24.8% are covered with cobblestone or dirt/mud. Approximately 25.7% of the modernised roads and 37.7% of thin-surfaced asphalt roads have exceeded their service life [55]. The general poor quality of the road system affects travel time across the country. The road system used in this study was established through the Analyst function, which is a component of the Network Analyst programme. When representing main roads on the exported maps, we used open-source data available on OpenStreetMap, selecting only highways, express roads, European, national, and county roads.
2.2. Methods
2.2.1. Geocoding Points
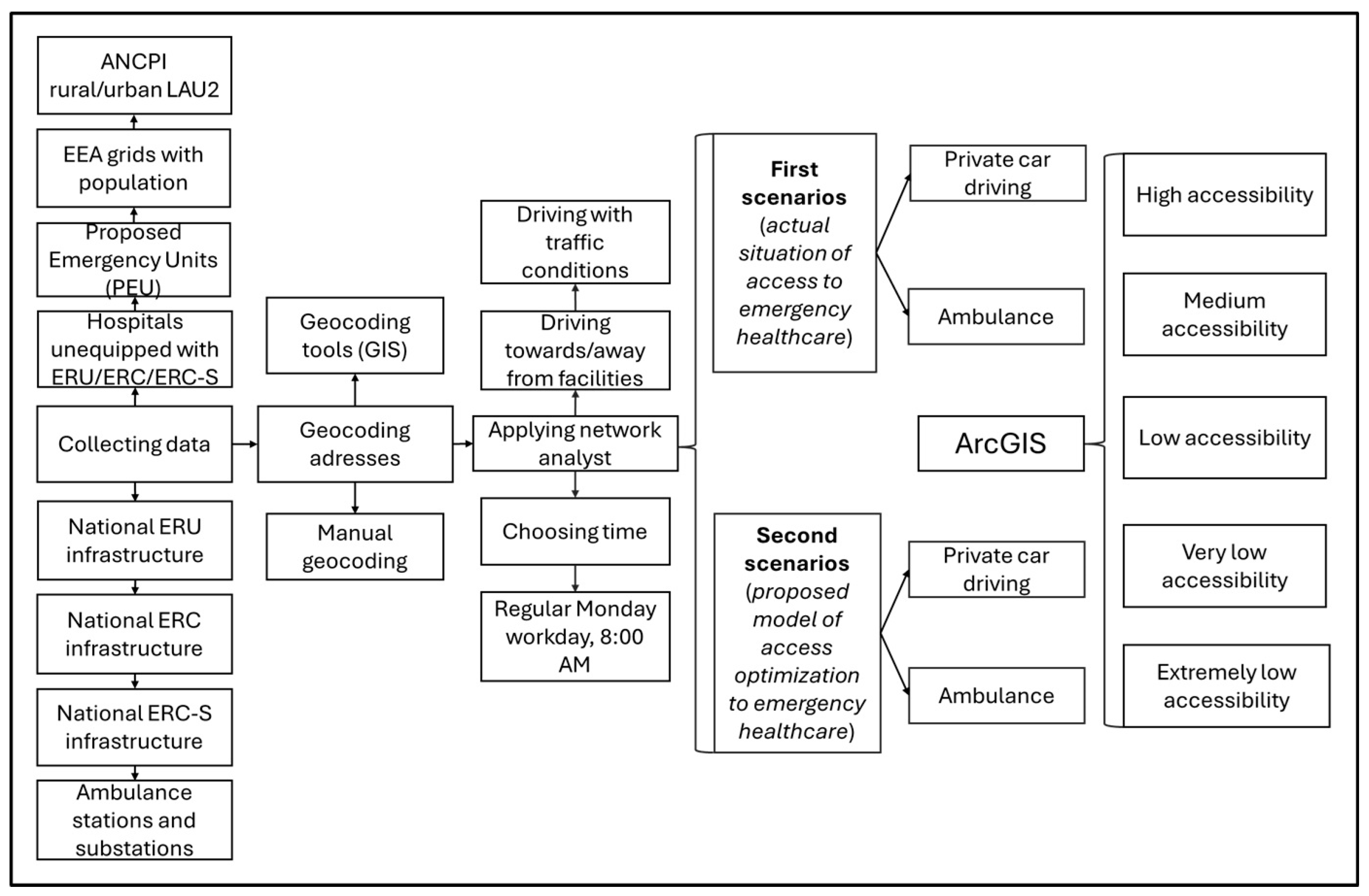
The current emergency care infrastructure was transformed into vectorial datasets using geocoding tools, following the precise addresses of Emergency Receiving Units (ERU), Emergency Receiving Compartments (ERC), Specialised Emergency Receiving Compartments, as well as the location for Proposed Emergency Units (PEU). Additionally, the locations of ambulance stations and substations were also geocoded for analysis. This process enabled accurate spatial analysis of the distribution and accessibility of emergency services within the study area (Figure 1).
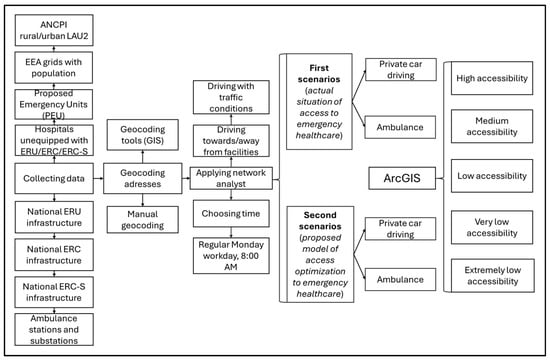
Figure 1.
Methodological framework.
2.2.2. Calculating Accessibility
While distance remains a significant factor, numerous studies highlight that travel time is of greater importance [56,57]. For this reason, this analysis prioritised travel time over distance. Starting from the Hansen-type potential/gravity accessibility formula [58], redeveloped by many authors [59,60,61,62] and used in travel time calculation by [63,64], we considered:
where accessibility to a facility (αf), calculated for a certain time of travel (t0), to be equal with Σi∈D, defined as the sum of contribution points (i), seen as a mathematical set of all contribution points (D) (considered in this case the centroid of each population grid), depending on travel time from the contribution point to facility (cif), at a certain time (t0). We adapted the formula, considering a certain time of travel (t0), in this case 8:00 a.m., a regular working day, Monday, and used the ArcGIS Network Analyst tool to calculate travel time and distance towards facilities when considering driving with a private car, as well as towards and from facilities when considering driving with an ambulance.
When applying the Network Analyst, several parameters, such as traffic conditions by hour and street type, were automatically taken into account. All accessibility analyses were conducted using traffic data from a typical Monday working day at 8:00 a.m. to ensure consistency. This represents a baseline scenario commonly used in spatial accessibility studies to approximate normal operational conditions of the emergency transport network. Because the model uses static travel speeds, it does not capture short-term temporal variations (e.g., rush-hour congestion or nighttime free-flow conditions). However, given that the analysis operates at a national scale and focuses on structural spatial inequalities rather than momentary performance, this assumption provides a stable and representative basis for comparative assessment across regions. We calculated the distance and accessibility from the point of origin to the destination facility for private cars. In the case of ambulances, the analysis included both the journey to the facility and the return trip.
Two types of accessibility were considered: first, accessibility was assessed based on the existing emergency health infrastructure, with results reflecting the population’s current accessibility. Then, we considered a scenario of accessibility based on existing emergency healthcare infrastructure and the proposed emergency units (PEU), reflecting a situation that aims to improve access.
For each of the two types of accessibility calculated we considered two modes of transportation: by private car, applying the function of an effective operational speed of 30 km/h within localities and 70 km/h outside localities, and by ambulance, applying the function of an effective operational speed of 50 km/h within localities and 90 km/h outside localities. We chose an average +20 km/h speed of an ambulance compared with a private car, as proved by Lupa [65], than in case of emergencies, ambulances are going faster with +20 km/h, than when driving as a regular car, respecting speed limits. According to the Romanian Government Emergency Ordinance No. 195/2002, ambulances are exempt from speed limits, and all drivers are required to yield immediately to emergency vehicles [66]. As such, despite the legal speed limit in Romania being 50 km/h in localities and 90/100/120/130 km/h outside localities, depending on the road hierarchy, we considered a lower effective operational speed for the two transportation modes, because of the road conditions that determine a smaller effective operational speed [67].
These speeds are network model parameters for travel time only; they do not include dispatch, on-scene, loading, or handover intervals. In the case of ambulance access, the intervention time was determined by summing two key components: the time required for the ambulance to reach the location and the subsequent transportation time from that location to the designated emergency facility. This process created a final aggregated data layer in the analysis.
When evaluating accessibility to emergency healthcare services, many international studies adopt a 20 min threshold as the critical time window for reaching emergency care facilities, reflecting standards primarily derived from high-income countries with well-developed road and transport infrastructure [7]. However, previous Romanian and Eastern European studies have demonstrated that this benchmark does not accurately reflect local conditions due to terrain complexity, dispersed settlement patterns, and suboptimal road infrastructure, which significantly increase travel times [42,48]. In the Romanian context, empirical analyses of hospital accessibility (e.g., Cioclu et al., 2024) have therefore adopted a 30 min threshold as a more realistic critical travel time for emergency access [68]. Following these national-scale precedents and in order to maintain methodological consistency, this study also applied a 30 min cut-off for critical accessibility. It is important to note that this adjustment does not imply equivalent survival outcomes to those observed at the 20 min benchmark; rather, it reflects a contextual adaptation that accounts for Romania’s specific infrastructural and geographical constraints.
To provide a clearer understanding of spatial accessibility to emergency healthcare facilities, the results of the travel time analyses were classified into five distinct accessibility categories based on the duration required to reach these services: high accessibility (which translates into a relatively short travel time 0–30 min): medium accessibility (with travel times between 30 and 60 min), low accessibility (with travel times of 60 to 90 min), very low accessibility (where travel times are either 90 to 120 min and extremely low accessibility (where travel times exceed 120 min). Extended travel durations represent substantial barriers to timely emergency care and highlight areas with the most critical access challenges.
It is important to note that the travel speeds used in this analysis represent average, uniform values, applied consistently nationwide to ensure comparability between regions. These values do not account for local variations in traffic congestion, road quality, weather conditions, or delays caused by specific urban settings such as parking, building access, or the time it takes ambulance teams to reach the patient. While these simplifications inevitably reduce the granularity of real-world dynamics, they allow for the identification of large-scale spatial patterns and disparities in accessibility to emergency care across the country. The created model provides a generalised representation of travel time rather than a precise simulation of every local condition.
2.3. Limitations
This study is subject to several methodological limitations stemming from the assumptions underlying the modelling of travel times. Although the road network was modelled in detail, uniform average speeds were applied to both private cars and ambulances, without differentiation by local traffic conditions or road surface type. The publicly available data on the quality of the road network in ArcGIS Pro for Romania is considerably lower than that available for the United States, for example. Consequently, variations caused by traffic congestion, weather, or road maintenance are not reflected in the results. In addition, the analysis did not account for the time needed for patients or ambulance staff to reach the vehicle (e.g., from high-rise buildings) or for waiting times at hospitals, which can be significant in large urban centres. These simplifications may lead to an overestimation of disparities between urban and rural accessibility levels. Nonetheless, they enable consistent national-level comparisons and the identification of areas most affected by limited access. Future studies could integrate dynamic traffic data and time-dependent network analyses to refine these estimates.
A further limitation concerns the use of static travel-time estimates for typical weekday conditions (Monday, 8:00 a.m.). The model does not reflect temporal fluctuations in traffic or emergency response conditions that can occur throughout the day or week. Nevertheless, since our objective was to assess spatial accessibility patterns rather than temporal variability in real-time performance, we consider the results robust enough to identify structural inequities.
The accessibility model focuses on spatial travel times rather than clinical appropriateness or patient condition. The assumption that all individuals can use a private car oversimplifies real-world emergencies. In reality, many patients—particularly those in critical condition—can not travel without medical assistance, and ambulance transport remains indispensable even when travel times are longer. This study also does not consider ambulance type, year of manufacture, or engine capacity, which can significantly overinfluence intervention and transport times.
Additionally, the study begins with the most precise open-source population data currently available, at a granularity of 1 km2, reference year 2021. However, this data may differ considerably from reality, as each km2 is assigned a value based on the time distance from its centre to the most significant facility. Additionally, the study does not account for the potential for additional queues upon arrival at emergency units, as the public health system in Romania is notorious for hour-long waiting times for medical interventions, despite being free of charge [69]. Moreover, in certain cases, urgent situations may take priority over others due to the severity of the injury or emergency, meaning that reaching an emergency unit does not guarantee receiving medical care.
Spatially disaggregated (grid-level) data on the age structure of the population is not available at a 1 km2 scale; as such, this study considered the total population residing in each grid and reported it as a percentage of the total population of Romania, which, according to the 2021 national census, is 19,104,220. Consequently, potential age-related differences in the need for emergency medical transport, particularly among infants and the elderly, could not be explicitly assessed. This represents a limitation of the study, as age composition is an important factor influencing healthcare demand and emergency service utilisation.
3. Results
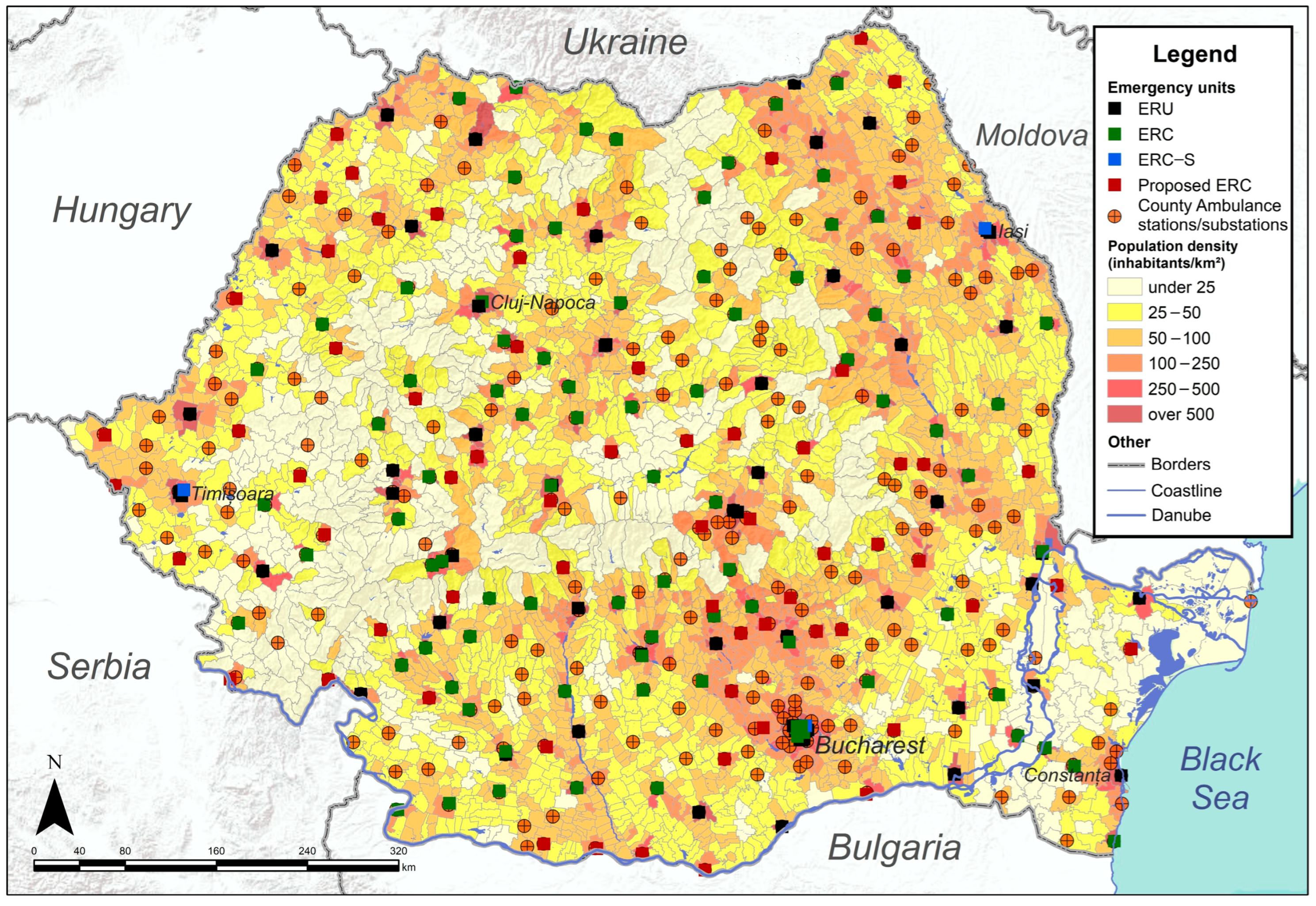
3.1. Distribution of Emergency Healthcare Facilities
Figure 2 maps the distribution of emergency healthcare units across the country. It identifies 159 facilities, relatively uniformly distributed throughout the country. These include 61 hospitals equipped with ERUs, with most of them (42) situated in cities that are county residences. ERCs are located in 91 hospitals across municipalities and large cities. These present an uneven distribution, marked by gaps in northwestern, western, southeastern and even southern parts of the country. Additionally, seven hospitals located only in the country’s largest cities have ERC-S (Figure 2).
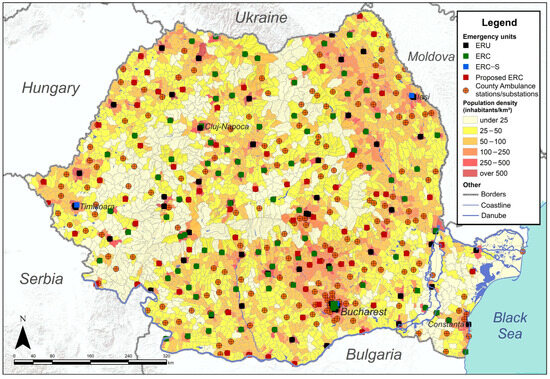
Figure 2.
Distribution of Emergency healthcare units.
Figure 2 also details the 65 emergency units proposed in this study. These units are strategically distributed to address areas currently lacking ERU, ERC, or ERC-S facilities, like the northwestern, southeastern, and western parts of the country. The results suggest that PEUs close the gap in areas where existing emergency units are underrepresented, thereby creating a more comprehensive nationwide network.
The 353 ambulance stations and sub-stations are well-distributed, but small gaps exist in areas of low population density, such as the southwest, north, and extreme east, as well as the centre of the country. Most importantly, the southern part of the country represents a hotspot for ambulance stations and substations, largely due to its high population density and proximity to the capital city, Bucharest (Figure 2).
3.2. Accessibility to the Current Network of Emergency Units
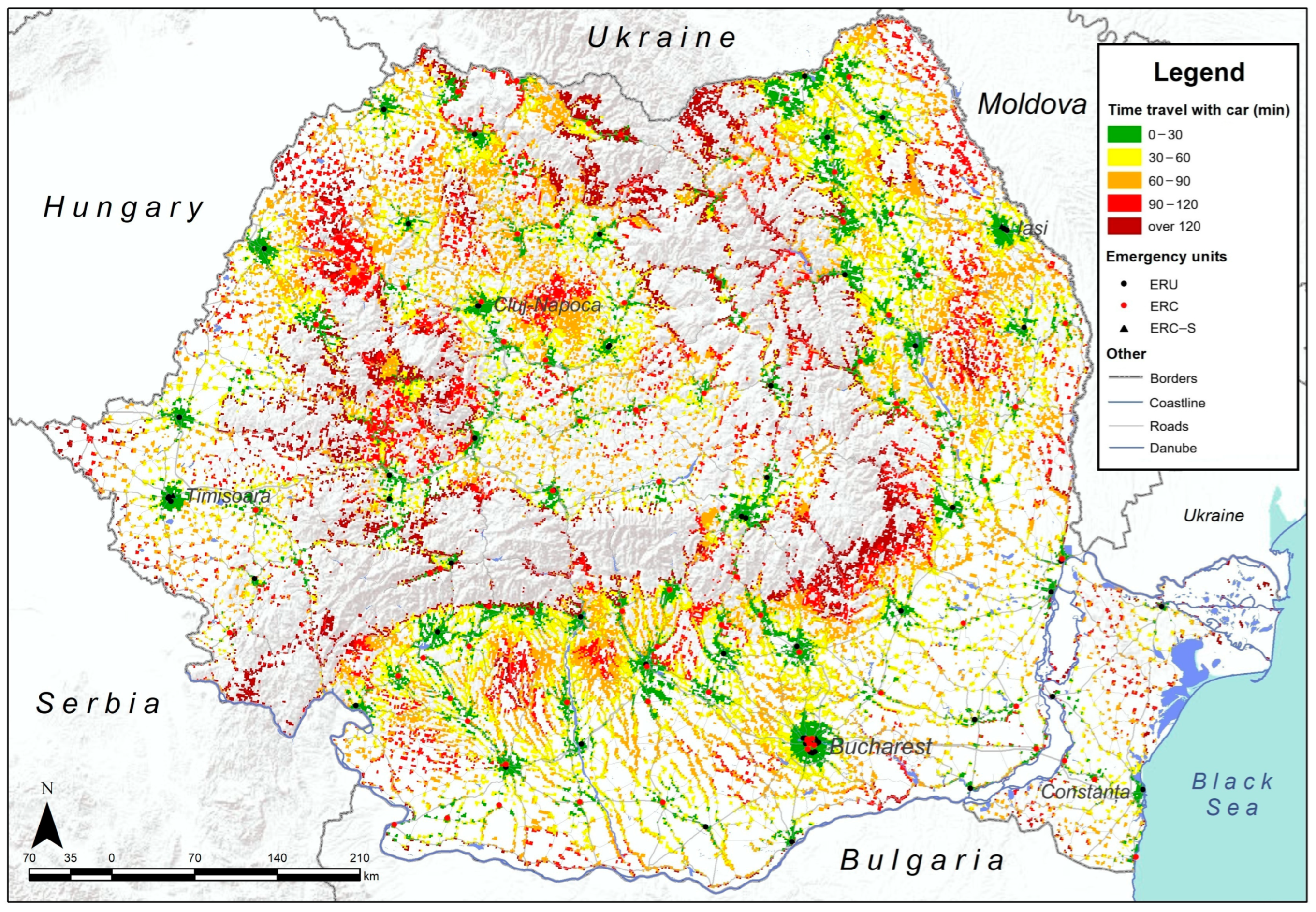
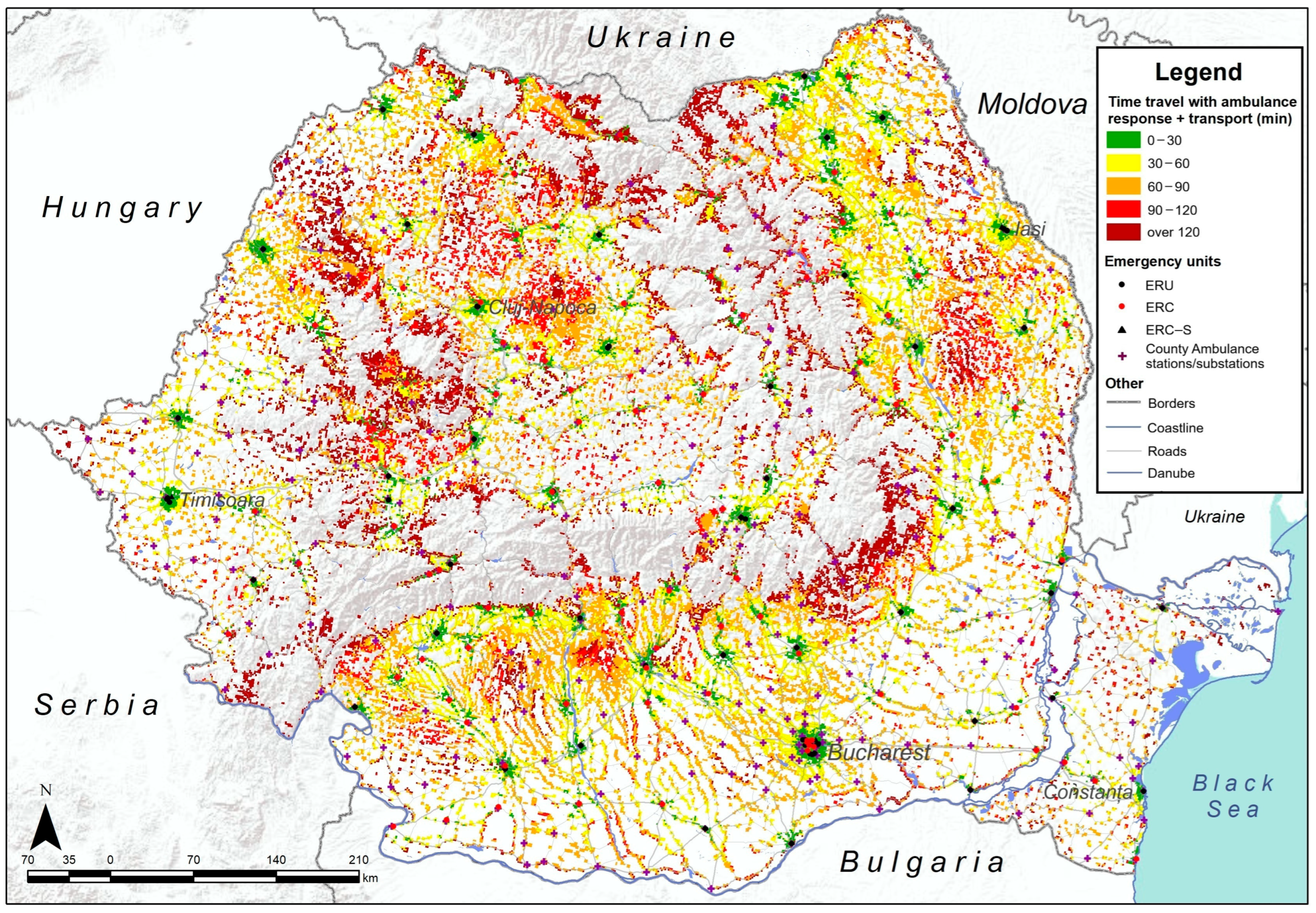
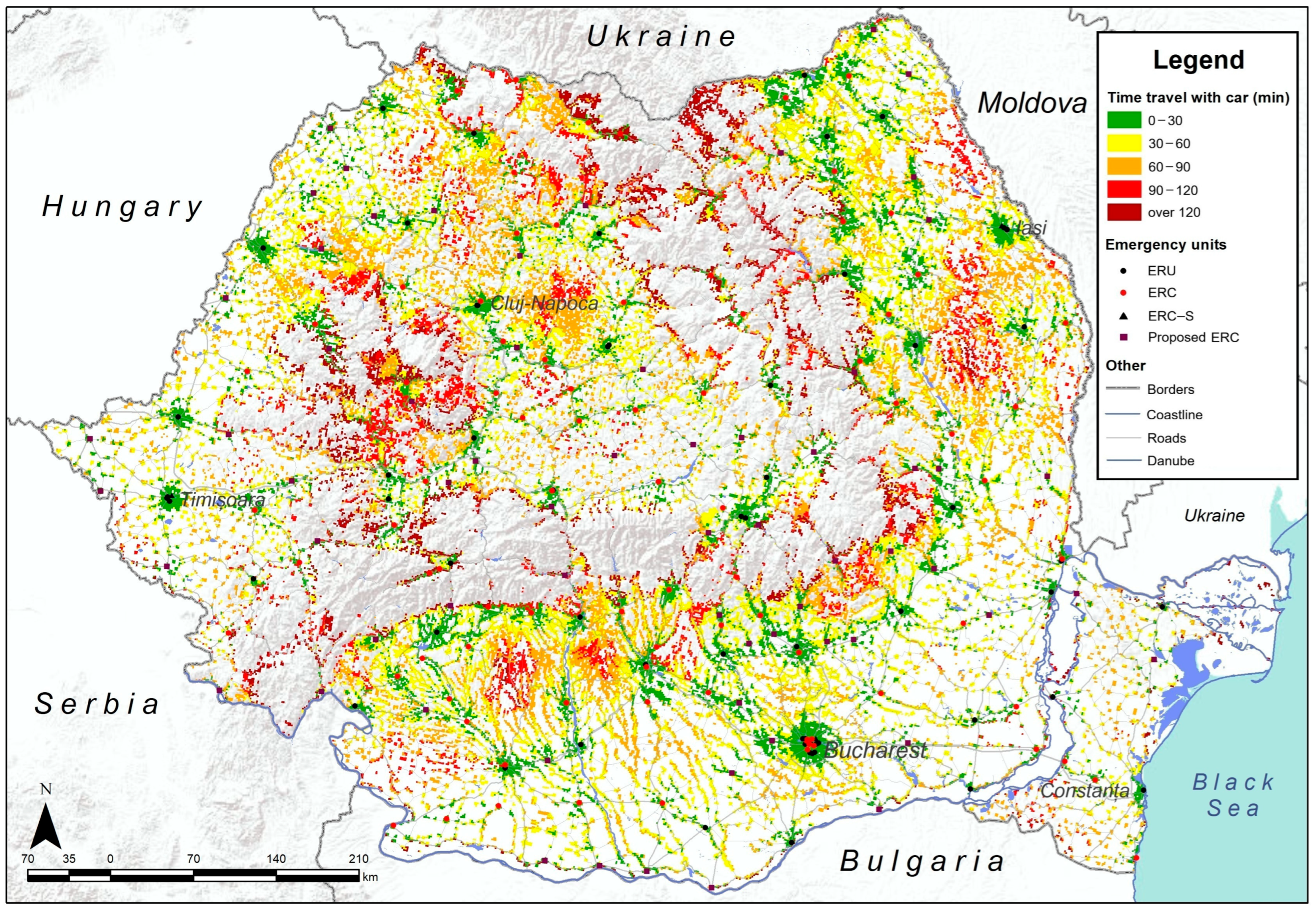
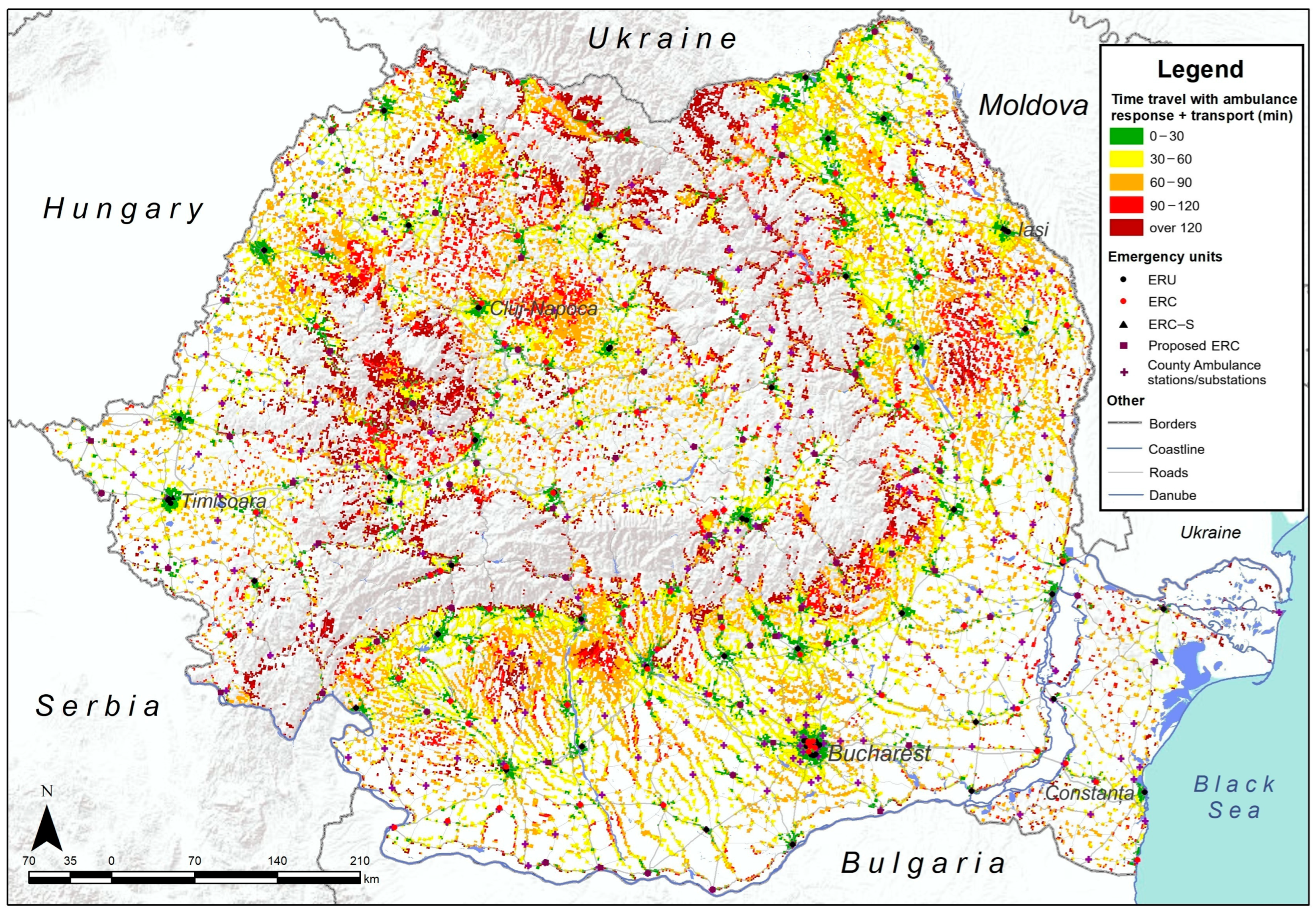
Urban–rural disparities in accessibility were assessed using the official national classification of localities, which distinguishes between urban (municipalities) and rural (communes) administrative units. In the accessibility maps (Figure 3, Figure 4, Figure 5 and Figure 6), major cities and urban boundaries are overlaid to help readers unfamiliar with Romania visualise these contrasts. Urban centres generally display dense coverage and shorter travel times, whereas peripheral rural regions, particularly in mountainous and eastern areas, remain underserved.
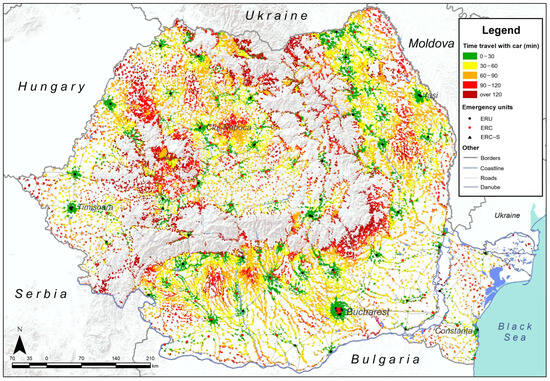
Figure 3.
Travel time by private car to current emergency healthcare units.
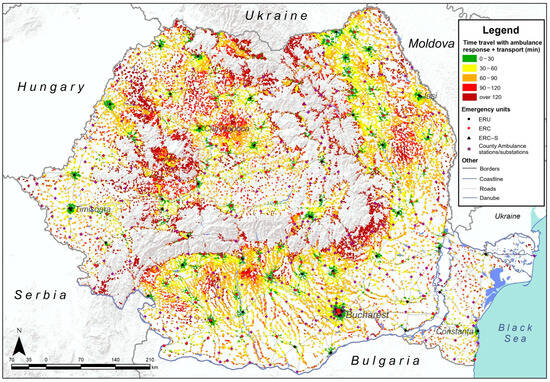
Figure 4.
Travel time by ambulance to current emergency healthcare units.
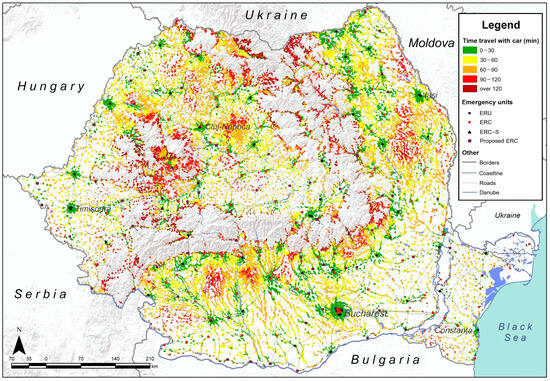
Figure 5.
Improved travel times when travelling by private car.
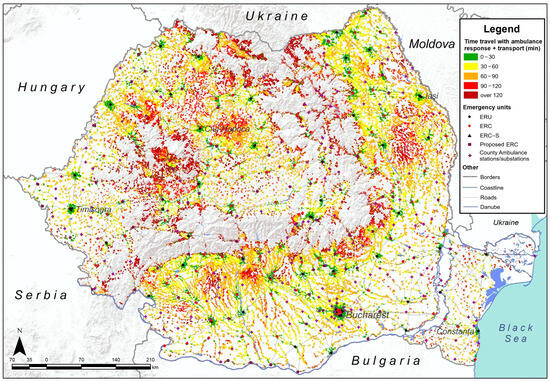
Figure 6.
Improved travel times when travelling by ambulance.
Accessibility to emergency healthcare, starting from the current network of 159 emergency units located in public hospitals, was considered first. We calculated the time required for travel to the nearest emergency healthcare units by private car and ambulance, revealing gaps in accessibility for both modes of transportation (Figure 3 and Figure 4).
Findings reveal that areas with high accessibility are very fragmented and tend to cluster around major urban centres and their immediate surroundings. In contrast, the majority of rural areas fall into medium or low accessibility categories, indicating a less favourable situation for rapid emergency healthcare access outside of large cities.
Greater accessibility can be achieved with a private car, because travelling with an ambulance creates more pronounced gaps in accessibility, as shown in Figure 4.
3.2.1. Accessibility When the Travel Means Is a Private Car
When travelling by private car, results show that accessibility deteriorates rapidly from urban centres to rural areas (Figure 3). However, the results show that over 61% of Romanians could not reach an emergency unit within 30 min (Table 1). Only 7.5 million Romanians, approximately 39% of the population, benefit from high accessibility, while over 7 million are living in areas registering medium accessibility (Table 1). Additionally, findings show that 2.7 million people register as having low accessibility, and for 1.6 million, the situation is even worse. Moreover, in some cases, travel time to an emergency unit can exceed 120 min, mainly due to remoteness and long distances. According to Figure 3, most underserved areas are situated in the centre-west, northwest and centre-southeast of the country. They are populated areas, even though they are in rural environments. As this study shows, nowadays, high accessibility to emergency units in Romania is limited primarily to major cities and is scarce in the surrounding rural areas.

Table 1.
Population accessibility to emergency healthcare units by travel time categories.
3.2.2. Accessibility When the Travel Means Is an Ambulance
When calculating travel time for ambulances, considering interventions at public stations and ambulance sub-stations nationwide, the results show that the situation is even more concerning than travel by private car. According to Table 1, only 5.2 million people (27.42%) can reach an emergency unit within a critical timeframe, while over 8.4 million fall into the medium accessibility category, 3.5 million experience low accessibility, and over 1.8 million have very low accessibility, meaning they need to travel for longer than 120 min. According to Figure 4 and Table 1, most parts of the counties outside urban centres fall below the threshold of having to travel under 30 min, but 72.58% of the population could not reach an emergency unit in a critical time (Table 1). Deprived areas in terms of accessibility to emergency units when travelling by ambulance are distributed throughout the country, with the lowest accessibility levels recorded in the centre-west, the northwest, and in areas overlapping the Carpathian Mountains (Figure 4). Despite a general image of low accessibility, the southern parts of the country tend to offer better ambulance travel times than the northern regions.
3.3. Accessibility Improvement
In order to optimise accessibility, we developed a scenario to evaluate how adding Proposed Emergency Units (PEUs) would impact emergency healthcare access. In this scenario, we calculated the time required to travel to the nearest healthcare emergency unit after adding the Proposed Emergency Units (PEUs) to the existing network. The PEUs are situated in currently ranked III hospitals [51] that could be equipped with emergency units. Thus, 65 such hospitals were identified (Figure 1). They are situated in localities with over 5000 inhabitants, usually 20 km from the nearest already existing hospital with an emergency unit. Ultimately, accessibility was calculated for a total number of 224 emergency units. Accessibility improvements were assessed using the same two modes of transportation: by private car (Figure 5) and by ambulance (Figure 6). Findings show that both travel modes result in higher accessibility categories compared to the initial situation, where the current accessibility was calculated. Entire areas in southern, north-western and north-eastern Romania register higher accessibility levels in this scenario. Although access has improved nationwide and gaps have narrowed in intensity, a significant lack of accessibility still exists in remote areas, particularly in the north and central-west. Meanwhile, disparities between the south and north have been alleviated, and travel by private car remains a more suitable option.
3.3.1. Improved Accessibility When the Travel Means Is a Private Car
When using a private car (Figure 5), statistical data shows a growth of over 25% in terms of high accessibility, now available to 64.37% of the population. However, 4.2 million Romanians are still living in areas with medium accessibility, while 1.6 million register low accessibility. The very low accessibility category includes a few with over 800,000 people in the proposed scenario, dropping from 1.6 million; however, the uneven distribution persists, as shown in Figure 5. Approximately 35.63% of the population, mainly concentrated in areas of medium and low accessibility, which result in long travel times, can be found all across the country. In the north, centre-western areas, and even southern areas, consistently longer travel times still seem to prevail. The northwest, centre-south and north-east of the country register the most visible changes.
3.3.2. Improved Accessibility When the Travel Means Is an Ambulance
When the considered transportation mode is an ambulance, travel times improve considerably, and the proportion of the population served within the high accessibility category—defined as being able to reach an emergency unit within 30 min—increases from approximately 26.5% in the current accessibility typology to 53.92% in our scenario. Even though high accessibility reached over 10.3 million in the proposed scenario, 5.2 million people still live in areas of medium accessibility, while 2.1 million and 1.3 million people live in areas of low and very low accessibility, respectively. Figure 6 shows that, compared with the current accessibility typology, the urban–rural gap is more pronounced when travelling with an ambulance, with better accessibility typically found in urban cores, while rural areas still experience medium or low accessibility.
In terms of accessibility to the current emergency healthcare network, for example, when travelling by private car from a rural environment, only 14.8% of the rural population reached an emergency care unit in less than 30 min (Table 2), and most rural citizens live in medium accessibility areas (47.8%), low accessibility areas (22.8%) and even very low accessibility areas. Urban areas show a higher accessibility rate of over 62.4% of inhabitants, indicating a significant discrepancy. However, 37.5% of the urban population still reported medium or low accessibility, due to many small towns lacking emergency units or even functioning hospitals, and therefore depend on other urban localities.

Table 2.
Population (%) accessibility to emergency healthcare units in rural and urban areas.
The accessibility issue seems more acute when travelling with an ambulance, as only over 8.3% of the rural population live in areas with high accessibility. The most notable aspect is that a significant proportion (44.4%) enjoys medium accessibility, and another share (21.2%) has low accessibility to emergency units (Table 2).
4. Discussion
Romania’s current healthcare network still bears the imprint of communist spatial arrangement, characterised by strong centralisation and a hospital-centric model concentrated in urban areas. Many communal and small city hospitals, which existed before the 1989 Revolution, are in an acute state of degradation, resulting from a lack of funds for health infrastructure despite numerous reforms [70]. This process has created significant inequalities in healthcare provision [48], and this legacy persists in today’s emergency infrastructure, where ERUs and ERCs are located within I, II and III-ranked hospitals—the only facilities equipped with complex medical technology and sufficient medical personnel to treat such cases [51]. Nowadays, lower-level hospitals often operate with only a guard room, where, in most cases, patients are redirected based on the severity of their emergency and sent by ambulance to the nearest emergency unit. Romania closed more hospitals than it opened in the past decades.
A first phase involved the closure of 67 units, as a result of the 2011 reform, of which 36 have been reopened and 20 reconverted into nursing homes [71]. Severe medical emergencies are usually directed to the closest ERUs within the rank I and II hospitals, while less severe cases are handled by ERCs in rank III hospitals. This means that large urban centres remain overrepresented in emergency service provision, while peripheral and rural territories have been structurally underserved for decades, creating spatial injustice. This historical path dependency contributes to the pronounced spatial inequalities identified in our analysis, confirming that accessibility gaps are not merely infrastructural but institutional in nature.
In Romania, access to emergency healthcare units is usually granted to ambulances, but it can also be accepted if a patient travels by private car or public transport to the hospital [51]. However, road congestion, particularly during rush hours in urban areas, further delays emergency response times. Out of the total ambulance fleet, 1516 vehicles (57.7%) have accumulated over 300,000 km, with 1011 exceeding 500,000 km. By the end of 2017, 1568 ambulances out of 2090 (75%) had already surpassed the maximum operational lifespan established by Government Decision No. 2139/2004, which regulates the classification and standard service durations of fixed assets. These vehicles operate continuously, 24 h a day, under increasingly demanding conditions. The public ambulance fleet is now largely obsolete, with over 80% of the vehicles meeting the criteria for decommissioning [72].
Many hospitals are equipped with specially designed parking to ensure access by private car, but this is not always the case. When it comes to ambulances, they typically begin their journeys from a specific hospital or strategically located stations and substations. These are located both across cities and in rural areas to reduce intervention times. Although the current networks of hospitals with emergency facilities, as well as of ambulance stations and substations, cover most of Romania (Figure 2), the accessibility analysis reveals visible inequalities across the country.
The current spatial accessibility indicates that over 60.2% of the population (11.5 million people) are deprived of timely access (within 30 min) to hospitals equipped with emergency facilities when travelling by private car, and over 72.5% (13.8 million people) when travelling by ambulance. More than half of the population is affected by a lack of accessibility within the critical 30 min time frame, creating a significant discrepancy between urban and rural areas, as shown in Table 2. Only 7.5 million people, when travelling with a private car or 5.2 million people, when travelling with an ambulance, live in areas with high accessibility brackets, with the most common categories remaining the moderate accessibility and low accessibility categories (Figure 3, Figure 4, Figure 5 and Figure 6), both of which translate into a travel time longer than the critical one (Table 1). Urban areas have the advantage of concentrating most emergency care facilities, with rural residents also having to rely on the same facilities. This situation contributes to long waiting times and overcrowded emergency facilities. Our proposed scenario, which entails the establishment of 65 additional ERCs, would contribute to the decongestion of existing facilities and significantly reduce travel times, thereby improving overall accessibility to emergency care services.
Across eastern and south-eastern Europe, quantified travel time and distance indicators show similar large urban–rural disparities, with several national networks still missing common 30–60 min targets for definitive emergency care. In Slovenia, analysis of the current general-hospital network found 84.3% of the population can reach a hospital by car within 30 min, rising to 95.3% within 45 min; new proposed scenarios showed similar coverage at 30 min and that as few as two strategically located hospitals could still place 81.4% of residents within 60 min [73]. In Bulgaria, the Health System Review reports that approximately 15% of settlements experience access times of >30 min for emergency medical services, with many rural areas being underserved [74]. EU monitoring indicates that in about two-thirds of European NUTS-3 regions, the average travel time by car to the nearest hospital is <15 min. However, they identify lagging regions—many in the east and south-east with mountainous or island geographies—that exceed that threshold, underscoring persistent geographic inequities in rapid hospital access. Although the proposed scenario with 65 new ERCs increases access for more than 12.2 million people when travelling in a private car and 10.3 million when travelling by ambulance, its implementation is conditioned by doctor shortages. In Romania, a total of 48.332 doctors are practising, according to 2024 NIS data. Many existing personnel are concentrated in large cities, making it crucial to retain doctors in small urban and rural areas [75]. However, the results of this study are optimistic, as its scenario shows a 25% increase in access to emergency healthcare, indicating that improvements can be made. Moreover, it appears that areas with medium, low, and very low accessibility diminished in size, with very low accessibility values persisting only sporadically (Figure 3, Figure 4, Figure 5 and Figure 6).
These findings demonstrate pronounced spatial inequalities in access to emergency healthcare in Romania, with accessibility rapidly decreasing outside major urban centres. Approximately two-thirds of the rural population live beyond a 30 min travel time to the nearest emergency unit. Figure 3 illustrates that accessibility deteriorates as one moves farther from large and medium-sized cities. This decline is primarily attributed to distance, but is also exacerbated by morning traffic conditions.
Ambulance accessibility in urban areas is improved in the proposed scenario, where over 44.8% of the population registers high accessibility (Table 2). Nevertheless, fewer than half of urban inhabitants still do not benefit from access within a 30 min timeframe, mostly because many cities, as shown in Figure 3, lack hospitals equipped with these facilities. Table 2 confirms that a private car remains a better travel mode, both in rural and urban areas, due to its practical one-way route, although this is contingent upon the actual state of the patient and the severity of the emergency. The good accessibility to emergency care services in urban areas could also be explained by the fact that Romania’s development landscape exhibits a persistent core–periphery and urban–rural divide: the capital Bucharest, Ilfov region, and a handful of western growth poles concentrate socio-economic advantages, while many eastern and southern counties remain structurally disadvantaged [76]. These disparities are visible in small areas too: spatial-statistics research drawing on a Social Disadvantage Index shows that the highest concentrations of disadvantage occur in the north–east, south–east, south and south–west, with only intermittent relief around metropolitan nodes [77].
Urban high accessibility when travelling with a private car (Table 2) increased by 20%, demonstrating improved accessibility, with better travel times reaching 85% of urban inhabitants in the proposed scenario. Approximately 15% of urban inhabitants who do not benefit from high accessibility are situated in the periphery of big cities or in remote, small towns across the country. It is essential to note that morning traffic creates access gaps, even in large cities, especially in cases when a low number of roads link neighbourhoods, thus serving as the sole access routes and becoming overcrowded. When travelling by ambulance in the proposed scenario, over 80.7% of the urban population registered high accessibility. However, 19.2% of measured medium or low accessibility categories are situated at the peripheries of large cities or in small urban localities across the country, which usually still do not benefit from an emergency unit (Figure 6).
While the private car remains the fastest travel mode in terms of theoretical accessibility, this finding must be interpreted cautiously. In real emergency situations, private car transport is often not medically appropriate or feasible, especially when patients require on-site first aid or continuous medical supervision during transfer services that only trained emergency personnel can provide. The modelled car-based accessibility represents potential access, as defined by Wang et al. [13], rather than observed or effective access. In practice, vehicle availability and severity of medical urgency determine the actual mode of transport. In some cases, paid semi-private alternatives, such as taxi services or private medical transport, may play an intermediate role when ambulances are delayed or unavailable, though these modes were beyond the scope of this study.
In the proposed scenario, rural accessibility by private car increased significantly to 41% due to the proposed emergency units, which are situated in small urban areas with less traffic congestion, making access from surrounding rural environments easier; however, approximately 36.3% fall into the medium accessibility category. From a transport perspective, EU benchmarking and investment analyses consistently highlight Romania’s limited coverage with high-capacity roads beyond the main corridors, as well as the below-EU-average quality of the existing network, factors that continue to hinder spatial inequalities and mobility [78]. Although recent expansions have led to notable improvements, significant disparities persist. As in 2024, Romania’s road network comprised approximately 1155 km of motorways and 121 km of expressways. Nevertheless, most counties remain dependent on lower-class roads, with the total public road network extending to 86,847 km, of which 20.7% are national roads, 40.4% are county roads, and 38.9% are communal roads [55]. Although the nominal network speeds used for ambulances in the model are 50 km/h within localities and 90 km/h outside localities, the effective end-to-end time for ambulance transport is typically longer than that for a private car because it includes two travel segments (to the patient and then to the facility). This explains why ambulance-based accessibility may appear less favourable than private-car accessibility. Still, rural areas registered an increase in terms of low accessibility (Table 2).
Despite results showing an increase in accessibility in both rural and urban areas, the concentration of emergency infrastructure in areas with good access, particularly in densely populated urban settlements, can cause travel times to increase significantly outside urban environments. This occurs due to traffic conditions, poor road infrastructure, narrow roads, and historical planning issues in many localities. Also, spatial accessibility can vary due to meteorological conditions, poor road infrastructure, and repair procedures that require traffic participants to reduce their speed below the normal limit, resulting in even longer travel times.
The proposed emergency network has a total of 224 emergency units, that contains 159 existing emergency units and new 65 PEUs (Table 3). This could alleviate the waiting times and reduce patient pressure within the hospital network. This study demonstrates that introducing new emergency facilities could lead to a significant increase in access for nearly 24.65% of the population when travelling by private car and for nearly 26.49% when travelling by ambulance. There is also a reduction in total share of population accounting medium, low, very low and extremely low travel times, from 60.28% to 35.63% when travel by private car and from 72.58% to 46.07% when travel by ambulance. This study also highlights the need for efficiency in planning and better organisation of the current emergency care network in order to improve population accessibility.

Table 3.
Percentage change in population accessibility to emergency units (Current vs. Improved).
5. Conclusions
This study could serve as a starting point for planning emergency units and provide recommendations for future administrative measures and researchers. For example, it could serve to improve the current emergency network and facilitate easy duplication for various medical research and health services, both public and private. Starting from national data for population and accessibility calculation functions, this study, utilising modern technology, demonstrates the need for planning and macro-scaling the view of real accessibility needs, as reported in geographical and demographic reality data sets.
The originality of this research lies in its integration of network-based GIS modelling at a national scale with a scenario optimisation approach tailored to Romania’s specific emergency care infrastructure. While earlier studies have highlighted uneven healthcare distribution, none have systematically modelled the spatial effects of potential infrastructure reforms. The framework developed in this study extends the methodological frontier of accessibility studies and can be readily applied to other Central and Eastern European countries with similar territorial and infrastructural challenges.
Access to emergency healthcare is a significant issue in Romania, with discrepancies between urban and rural areas persisting nationwide. This deprives a large share of the population of a quick yet critical healthcare need. While Romania’s health infrastructure is uniformly distributed, in reality, it lacks emergency units, resulting in uneven access during serious situations and depriving more than 60% of its inhabitants. Key improvements can be achieved by equipping hospitals with emergency units, which could significantly optimise healthcare for many Romanian patients, especially in small urban centres, and also result in substantial improvements in rural areas. Small towns and adjacent rural localities, which contain the most rural population in Romania, could achieve good accessibility if the right decisions are taken. This study demonstrates that starting from the current network of hospitals and equipping some with emergency infrastructure can increase accessibility for more than 25% of the population. This approach reduces gap areas and improves the time it takes to travel to the nearest emergency unit for over 5 million inhabitants.
Given the current healthcare infrastructure, there is significant potential to enhance access to emergency services. With the implementation of appropriate reforms, it is estimated that over 64.37% of the population could benefit from emergency healthcare within a 30 min timeframe. This improvement would represent a substantial increase in timely access for many communities, particularly in rural and underserved areas.
Future research directions should also concentrate on gap areas and new infrastructure needs, correlated with demographic data sets, to address the actual lack of accessibility. There is also a need to focus on studies that examine the access of vulnerable population groups to these types of healthcare services, highlight the territorial dysfunctions of healthcare systems, and identify realistic strategies to reduce disparities and improve population access to healthcare.
Author Contributions
Conceptualization, C.C. and L.D.; methodology, C.C. and L.D.; software, C.C.; validation, L.D. and A.M.; formal analysis, C.C., A.C. and A.-A.P.; investigation, C.C. and L.D.; resources, A.C. and A.-A.P.; data curation, A.M., A.C. and A.-A.P.; writing—original draft preparation, C.C. and L.D.; writing—review and editing, A.M. and L.D.; visualisation, C.C.; supervision, L.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data presented in this study are available on request from the corresponding authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Liu, S.; Qin, Y.; Xu, Y. Inequality and Influencing Factors of Spatial Accessibility of Medical Facilities in Rural Areas of China: A Case Study of Henan Province. Int. J. Environ. Res. Public Health 2019, 16, 1833. [Google Scholar] [CrossRef]
- Penchansky, R.; Thomas, J.W. The Concept of Access: Definition and Relationship to Consumer Satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Cu, A.; Meister, S.; Lefebvre, B.; Ridde, V. Assessing Healthcare Access Using the Levesque’s Conceptual Framework—A Scoping Review. Int. J. Equity Health 2021, 20, 116. [Google Scholar] [CrossRef]
- McEntee, M.K. Accessibility of Mental Health Services and Crisis Intervention to the Deaf. Am. Ann. Deaf. 1993, 138, 26–30. [Google Scholar] [CrossRef]
- Cuervo, L.G.; Martínez-Herrera, E.; Cuervo, D.; Jaramillo, C. Improving equity using dynamic geographic accessibility data for urban health services planning. Gac. Sanit. 2022, 36, 497–499. [Google Scholar] [CrossRef]
- Ishikawa, T.; Mizuguchi, H.; Murayama, H.; Fujiwara, K.; Tanikawa, T.; Kobayashi, E.; Ogasawara, K. Relationship between Accessibility and Resources to Treat Acute Ischemic Stroke. Hokkaido, Japan: Analysis of Inequality and Coverage Using Geographic Information Systems. Health Policy Technol. 2019, 8, 337–342. [Google Scholar] [CrossRef]
- Kotavaara, O.; Nivala, A.; Lankila, T.; Huotari, T.; Delmelle, E.; Antikainen, H. Geographical Accessibility to Primary Health Care in Finland—Grid-Based Multimodal Assessment. Appl. Geogr. 2021, 136, 102583. [Google Scholar] [CrossRef]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Hafizur Rahman, M. Poverty and Access to Health Care in Developing Countries. Ann. N. Y. Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, O. Access to Health Care in Developing Countries: Breaking down Demand Side Barriers. Cad. Saúde Pública 2007, 23, 2820–2834. [Google Scholar] [CrossRef]
- Albuquerque, P.C.; Felipe, L.L.; Lopes, J.F.; Tassinari, W.D.S.; Zicker, F.; Fonseca, B.D.P. Geographic Accessibility to Hospital Childbirths in Brazil (2010–2011 and 2018–2019): A Cross-Sectional Study. Lancet Reg. Health-Am. 2025, 42, 100976. [Google Scholar] [CrossRef] [PubMed]
- Mooney, G.H. Equity in Health Care: Confronting the Confusion. Eff. Health Care 1983, 1, 179–185. [Google Scholar]
- Paul, E.; Deville, C.; Bodson, O.; Sambiéni, N.E.; Thiam, I.; Bourgeois, M.; Ridde, V.; Fecher, F. How Is Equity Approached in Universal Health Coverage? An Analysis of Global and Country Policy Documents in Benin and Senegal. Int. J. Equity Health 2019, 18, 195. [Google Scholar] [CrossRef]
- Wang, J.; Du, F.; Huang, J.; Liu, Y. Access to Hospitals: Potential vs. Observed. Cities 2020, 100, 102671. [Google Scholar] [CrossRef]
- Mayaud, J.R.; Tran, M.; Nuttall, R. An Urban Data Framework for Assessing Equity in Cities: Comparing Accessibility to Healthcare Facilities in Cascadia. Comput. Environ. Urban. Syst. 2019, 78, 101401. [Google Scholar] [CrossRef]
- Durand, C.; Lefebvre, H. Le Droit à La Ville. In L’Homme et la Société; Au Dossier de la Révolte Étudiante; Éditions Anthropos: Paris, France, 1968; pp. 250–251. [Google Scholar]
- Harvey, D. Spaces of Hope; Edinburgh University Press: Edinburgh, UK, 2022; ISBN 978-0-7486-1268-0. [Google Scholar]
- Soja, E.W. Seeking Spatial Justice; Globalization and Community Series; University of Minnesota Press: Minneapolis, MN, USA, 2010; ISBN 978-0-8166-6667-6. [Google Scholar]
- Özcelik, Z.; Hamamcioglu, C. From District to Street: A Multi-Scale Analysis of Spatial Justice through the 15-Minute City Framework in Beyoğlu, Istanbul. J. Urban. Mobil. 2025, 8, 100163. [Google Scholar] [CrossRef]
- D’Arcy, J.; Doherty, S.; Fletcher, L.; Neto, A.S.; Jones, D. Intensive Care Unit Admission from the Emergency Department in the Setting of National Emergency Access Targets. Crit. Care Resusc. 2023, 25, 84–89. [Google Scholar] [CrossRef]
- Isaacson, J.E.; Joiner, A.P.; Kozhumam, A.S.; Caruzzo, N.M.; De Andrade, L.; Iora, P.H.; Costa, D.B.; Vissoci, B.M.; Sartori, M.L.L.; Rocha, T.A.H.; et al. Emergency Care Sensitive Conditions in Brazil: A Geographic Information System Approach to Timely Hospital Access. Lancet Reg. Health-Am. 2021, 4, 100063. [Google Scholar] [CrossRef]
- Brenner, J.M.; Blutinger, E.; Ricke, B.; Vearrier, L.; Kluesner, N.H.; Moskop, J.C. Ethical Issues in the Access to Emergency Care for Undocumented Immigrants. J. Am. Coll. Emerg. Physicians Open 2021, 2, e12461. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.J.; Francetic, I.; Watkinson, R.; Gillibrand, S.; Sutton, M. Socioeconomic Inequality in Access to Timely and Appropriate Care in Emergency Departments. J. Health Econ. 2022, 85, 102668. [Google Scholar] [CrossRef]
- Apparicio, P.; Abdelmajid, M.; Riva, M.; Shearmur, R. Comparing Alternative Approaches to Measuring the Geographical Accessibility of Urban Health Services: Distance Types and Aggregation-Error Issues. Int. J. Health Geogr. 2008, 7, 7. [Google Scholar] [CrossRef]
- Spencer, J.; Angeles, G. Kernel Density Estimation as a Technique for Assessing Availability of Health Services in Nicaragua. Health Serv. Outcomes Res. Methodol. 2007, 7, 145–157. [Google Scholar] [CrossRef]
- Cheng, L.; Yang, M.; De Vos, J.; Witlox, F. Examining Geographical Accessibility to Multi-Tier Hospital Care Services for the Elderly: A Focus on Spatial Equity. J. Transp. Health 2020, 19, 100926. [Google Scholar] [CrossRef]
- Doi, S.; Inoue, T.; Ide, H.; Nakamura, T.; Fujita, S.; Takabayashi, K. Using GIS to Simulate Inpatient’s Behavior and Visualize Healthcare Demand. Procedia Comput. Sci. 2013, 22, 1361–1368. [Google Scholar] [CrossRef][Green Version]
- Huang, Z.; Kawamura, K.; Kitayama, T.; Li, Q.; Yang, S.; Miyake, T. GIS-Based Study of Dental Accessibility and Caries in 3-Year-Old Japanese Children. Int. Dent. J. 2023, 73, 550–557. [Google Scholar] [CrossRef]
- Zhu, M.; Zuo, Y.; Liang, X.; Cui, H. Urban–Rural Public Transport Accessibility Evaluation Based on Improved Gravity Model with Actual Time. Proc. Inst. Civ. Eng.-Munic. Eng. 2025, 178, 55–67. [Google Scholar] [CrossRef]
- Luo, W. Using a GIS-Based Floating Catchment Method to Assess Areas with Shortage of Physicians. Health Place 2004, 10, 1–11. [Google Scholar] [CrossRef]
- Wong, J.J.; Wang, D.; Hogg-Johnson, S.; Mior, S.A.; Côté, P. Prevalence and Characteristics of Healthcare Utilization with Different Providers among Canadians with Chronic Back Problems: A Population-Based Study. Brain Spine 2024, 4, 102812. [Google Scholar] [CrossRef]
- Tao, Z.; Zhang, R.; Liu, C.; Zhong, Q. On the Modifiable Areal Unit Problem (MAUP) in Healthcare Accessibility Measurement via the Two-Step Floating Catchment Area (2SFCA) Method. Health Place 2025, 93, 103468. [Google Scholar] [CrossRef]
- Radke, J.; Mu, L. Spatial Decompositions, Modeling and Mapping Service Regions to Predict Access to Social Programs. Ann. GIS 2000, 6, 105–112. [Google Scholar] [CrossRef]
- Wang, Y.; Han, Y. Measuring Maritime Search and Rescue (SAR) Accessibility Using an Improved Spatiotemporal Two-Step Floating Catchment Area Method: A Case Study in the South China Sea. J. Transp. Geogr. 2025, 124, 104155. [Google Scholar] [CrossRef]
- Delamater, P.L. Spatial Accessibility in Suboptimally Configured Health Care Systems: A Modified Two-Step Floating Catchment Area (M2SFCA) Metric. Health Place 2013, 24, 30–43. [Google Scholar] [CrossRef]
- Schoo, J.; Schüssler, F. The Future of General Practitioner Care in Lower Saxony, Germany: An Analysis of Actual vs. Target States Using a GIS-Based Floating Catchment Area Method. Geospat. Health 2025, 20, 56–68. [Google Scholar] [CrossRef]
- Kanuganti, S.; Sarkar, A.K.; Singh, A.P. Quantifying Accessibility to Health Care Using Two-Step Floating Catchment Area Method (2SFCA): A Case Study in Rajasthan. Transp. Res. Procedia 2016, 17, 391–399. [Google Scholar] [CrossRef]
- Raeesi, A.; Hashtarkhani, S.; Tara, M.; Sargolzaei, N.; Kiani, B. Empowering Access: Unveiling an Overall Composite Spatial Accessibility Index to Healthcare Services in Southeastern Iran. Int. J. Equity Health 2025, 24, 35. [Google Scholar] [CrossRef] [PubMed]
- McLafferty, S.L. GIS and Health Care. Annu. Rev. Public Health 2003, 24, 25–42. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measures of Spatial Accessibility to Health Care in a GIS Environment: Synthesis and a Case Study in the Chicago Region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Zhou, Y.; Xu, Q.; He, J. Socioeconomic Status, Health, Subjective Well-Being and Worries about Healthcare Accessibility among Chinese Citizens—Based on an Age-Gender-Region Stratified Model. Int. Rev. Econ. Financ. 2025, 102, 104390. [Google Scholar] [CrossRef]
- Zhang, Y.; Cao, M.; Cheng, L.; Gao, X.; De Vos, J. Exploring the Temporal Variations in Accessibility to Health Services for Older Adults: A Case Study in Greater London. J. Transp. Health 2022, 24, 101334. [Google Scholar] [CrossRef]
- Cioclu, A.; Dumitrache, L.; Nae, M.; Mareci, A. Potential Spatial Accessibility to Cardiovascular Hospitals in Romania. Systems 2024, 12, 160. [Google Scholar] [CrossRef]
- Cheng, G.; Zeng, X.; Duan, L.; Lu, X.; Sun, H.; Jiang, T.; Li, Y. Spatial Difference Analysis for Accessibility to High Level Hospitals Based on Travel Time in Shenzhen, China. Habitat. Int. 2016, 53, 485–494. [Google Scholar] [CrossRef]
- Yoshida, S.; Matsumoto, M.; Kashima, S.; Koike, S.; Tazuma, S.; Maeda, T. Geographical Distribution of Family Physicians in Japan: A Nationwide Cross-Sectional Study. BMC Fam. Pract. 2019, 20, 147. [Google Scholar] [CrossRef]
- Li, Q.; Li, X.; Zhang, Q.; Zhang, Y.; Liu, L.; Cheng, X.; Yi, B.; Mao, J.; Chen, C.; He, S.; et al. A Cross-Sectional Nationwide Study on Accessibility and Availability of Neonatal Care Resources in Hospitals of China: Current Situation, Mortality and Regional Differences. Lancet Reg. Health-West. Pac. 2021, 14, 100212. [Google Scholar] [CrossRef]
- Jenkins, H.E.; Ayuk, S.; Puma, D.; Brooks, M.B.; Millones, A.K.; Jimenez, J.; Lecca, L.; Galea, J.T.; Becerra, M.; Keshavjee, S.; et al. Geographic Accessibility to Health Facilities Predicts Uptake of Community-Based Tuberculosis Screening in an Urban Setting. Int. J. Infect. Dis. 2022, 120, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Mavoa, S.; Witten, K.; McCreanor, T.; O’Sullivan, D. GIS Based Destination Accessibility via Public Transit and Walking in Auckland, New Zealand. J. Transp. Geogr. 2012, 20, 15–22. [Google Scholar] [CrossRef]
- Dumitrache, L.; Nae, M.; Dumbrăveanu, D.; Simion, G.; Suditu, B. Contrasting Clustering in Health Care Provision in Romania: Spatial and Aspatial Limitations. Procedia Environ. Sci. 2016, 32, 290–299. [Google Scholar] [CrossRef]
- Petrovici, N.; Belbe, S.; Mare, C.; Cotoi, C. Hybrid Health Regimes: Access to Primary Care Physicians and COVID-19 Vaccine Uptake across Municipalities in Romania. Soc. Sci. Med. 2023, 337, 116305. [Google Scholar] [CrossRef]
- Joseph, A.E.; Phillips, D.R. Accessibility and Utilization: Geographical Perspectives on Health Care Delivery; Harper & Row: New York, NY, USA, 1984; ISBN 978-0-06-318276-9. [Google Scholar]
- Romanian Parliament. Law 95/2006 on Healthcare Reform (Republished); Monitorul Oficial al României no. 652/2015; Monitorul Oficial Publishing House: Bucharest, Romania, 2015. [Google Scholar]
- Romanian Parliament. Law 310/2022 on Approving Government Ordinance No. 18/2021 Amending and Supplementing Law No. 95/2006 on Health Reform and Amending Certain Legislative Acts in the Field of Health, as Well as Repealing Article 4 of Law No. 584/2002 on Measures to Prevent the Spread of AIDS in Romania and to Protect Persons Infected with HIV or Suffering from AIDS; Monitorul Oficial al României no. 1117/2022; Monitorul Oficial Publishing House: Bucharest, Romania, 2022. [Google Scholar]
- Ministry of Public Health. Order 1706/2007 on the Management and Organization of Emergency Reception Units and Departments; Monitorul Oficial al României no. 724/2007; Monitorul Oficial Publishing House: Bucharest, Romania, 2007. [Google Scholar]
- Ministry of Public Health. Order 323/2011 on the Approval of the Methodology and Minimum Mandatory Criteria for the Classification of Hospitals According to Competence; Monitorul Oficial al României no. 274/2011; Monitorul Oficial Publishing House: Bucharest, Romania, 2011. [Google Scholar]
- National Institute of Statistics (NIS). 2024 Lungimea Căilor de Transport, la Sfârșitul Anului 2024. Available online: https://insse.ro/cms/ro/content/lungimea-c%C4%83ilor-de-transport-la-sf%C3%A2r%C5%9Fitul-anului-2024-0 (accessed on 8 November 2025).
- Gao, F.; Jaffrelot, M.; Deguen, S. Measuring Hospital Spatial Accessibility Using the Enhanced Two-Step Floating Catchment Area Method to Assess the Impact of Spatial Accessibility to Hospital and Non-Hospital Care on the Length of Hospital Stay. BMC Health Serv. Res. 2021, 21, 1078. [Google Scholar] [CrossRef]
- Zhao, P.; Li, S.; Liu, D. Unequable Spatial Accessibility to Hospitals in Developing Megacities: New Evidence from Beijing. Health Place 2020, 65, 102406. [Google Scholar] [CrossRef]
- Hansen, W.G. How Accessibility Shapes Land Use. J. Am. Inst. Plan. 1959, 25, 73–76. [Google Scholar] [CrossRef]
- Albacete, X.; Olaru, D.; Paül, V.; Biermann, S. Measuring the Accessibility of Public Transport: A Critical Comparison Between Methods in Helsinki. Appl. Spat. Anal. 2017, 10, 161–188. [Google Scholar] [CrossRef]
- Geurs, K.T.; Van Wee, B. Accessibility Evaluation of Land-Use and Transport Strategies: Review and Research Directions. J. Transp. Geogr. 2004, 12, 127–140. [Google Scholar] [CrossRef]
- Miller, E. Measuring Accessibility: Methods and Issues; International Transport Forum Discussion Papers; OECD Publishing: Paris, France, 2020. [Google Scholar]
- Soukhov, A.; Páez, A.; Higgins, C.D.; Mohamed, M. Introducing Spatial Availability, a Singly-Constrained Measure of Competitive Accessibility. PLoS ONE 2023, 18, e0278468. [Google Scholar] [CrossRef]
- Büttner, B.; Kinigadner, J.; Ji, C.; Wright, B.; Wulfhorst, G. The TUM Accessibility Atlas: Visualizing Spatial and Socioeconomic Disparities in Accessibility to Support Regional Land-Use and Transport Planning. Netw. Spat. Econ. 2018, 18, 385–414. [Google Scholar] [CrossRef]
- Park, J.; Goldberg, D.W. A Review of Recent Spatial Accessibility Studies That Benefitted from Advanced Geospatial Information: Multimodal Transportation and Spatiotemporal Disaggregation. ISPRS Int. J. Geo-Inf. 2021, 10, 532. [Google Scholar] [CrossRef]
- Lupa, M.; Chuchro, M.; Sarlej, W.; Adamek, K. Emergency Ambulance Speed Characteristics: A Case Study of Lesser Poland Voivodeship, Southern Poland. Geoinformatica 2021, 25, 775–798. [Google Scholar] [CrossRef]
- Romanian Government. Government Emergency Ordinance No. 195/2002 (Republished) on Circulation on Public Roads; Monitorul Oficial al României no. 670/2006; Monitorul Oficial Publishing House: Bucharest, Romania, 2006. [Google Scholar]
- Romanian Government. Decision No. 85/2003 Approving the Regulations for the Implementation of Government Emergency Ordinance No. 195/2002 on Traffic on Public Roads; Monitorul Oficial al României no. 58/2003; Monitorul Oficial Publishing House: Bucharest, Romania, 2003. [Google Scholar]
- Cioclu, A.; Dumitrache, L.; Mareci, A.; Nae, M. Tackling Cardiovascular Care Deserts in Romania: Expanding Population Access in Underserved Areas. Healthcare 2024, 12, 2577. [Google Scholar] [CrossRef]
- Dumitrache, L.; Nae, M. The Changing Landscapes of Hospitals in the Urban Areas: Evidence from Romania. In Urban Dynamics, Environment and Health; Sinha, B.R.K., Ed.; Springer Nature Singapore: Singapore, 2023; pp. 415–436. ISBN 978-981-9957-43-9. [Google Scholar]
- Guțoiu, G. Development Inequalities of Romanian Physical Public Healthcare Infrastructure: The Case of Hospital Beds. J. Stud. Res. Hum. Geogr. 2021, 15, 37–52. [Google Scholar] [CrossRef]
- Scîntee, S.G.; Vlădescu, C.; Sagan, A.; Hernández-Quevedo, C. The Unexpected Outcomes of the Closure of 67 Inpatient Care Facilities in 2011 in Romania. Health Policy 2018, 122, 1161–1164. [Google Scholar] [CrossRef]
- Grasu, R.A.; Armean, P. Evaluation of the Activity of the Public Ambulance Services in Romania from the Perspective of Human Resources. Acta Medica Transilv. 2023, 28, 7–11. [Google Scholar]
- Blatnik, P.; Bojnec, Š. Optimal Network of General Hospitals in Slovenia. Int. J. Environ. Res. Public Health 2023, 20, 4235. [Google Scholar] [CrossRef]
- Georgieva, L.; Salchev, P.; Dimitrova, R.; Dimova, A.; Avdeeva, O. Bulgaria Health System Review; World Health Organization 2007, on behalf of the European Observatory on Health Systems and Policies: Geneva, Switzerland, 2007. [Google Scholar]
- Apostu, S.A.; Vasile, V.; Marin, E.; Bunduchi, E. Factors Influencing Physicians Migration—A Case Study from Romania. Mathematics 2022, 10, 505. [Google Scholar] [CrossRef]
- Eurostat. Eurostat Regional Yearbook, 2024 ed.; European Commission: Ispra, Italy, 2024; Available online: https://ec.europa.eu/eurostat/web/products-flagship-publications/w/ks-ha-24-001 (accessed on 10 November 2025).
- Ursu, C.-D.; Benedek, J. Exploring Local Income Inequalities by Using Spatial Statistics. Emphasis on Romanian Metropolitan Areas. East. J. Eur. Stud. 2024, 15, 298–323. [Google Scholar] [CrossRef]
- Opriş-Sîrca, P.-T. Transport Axes and Corridors in Romania—Policy Issues and Opportunity for Territorial Development. J. Settl. Spat. Plan. 2024, 15, 133–144. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).