Non-Optimal Wet-Bulb Temperature and Short-Term Black Carbon Exposure Largely Impact Emergency Department Visits for Cause-Stable Ischemic Heart Disease
Abstract
1. Introduction
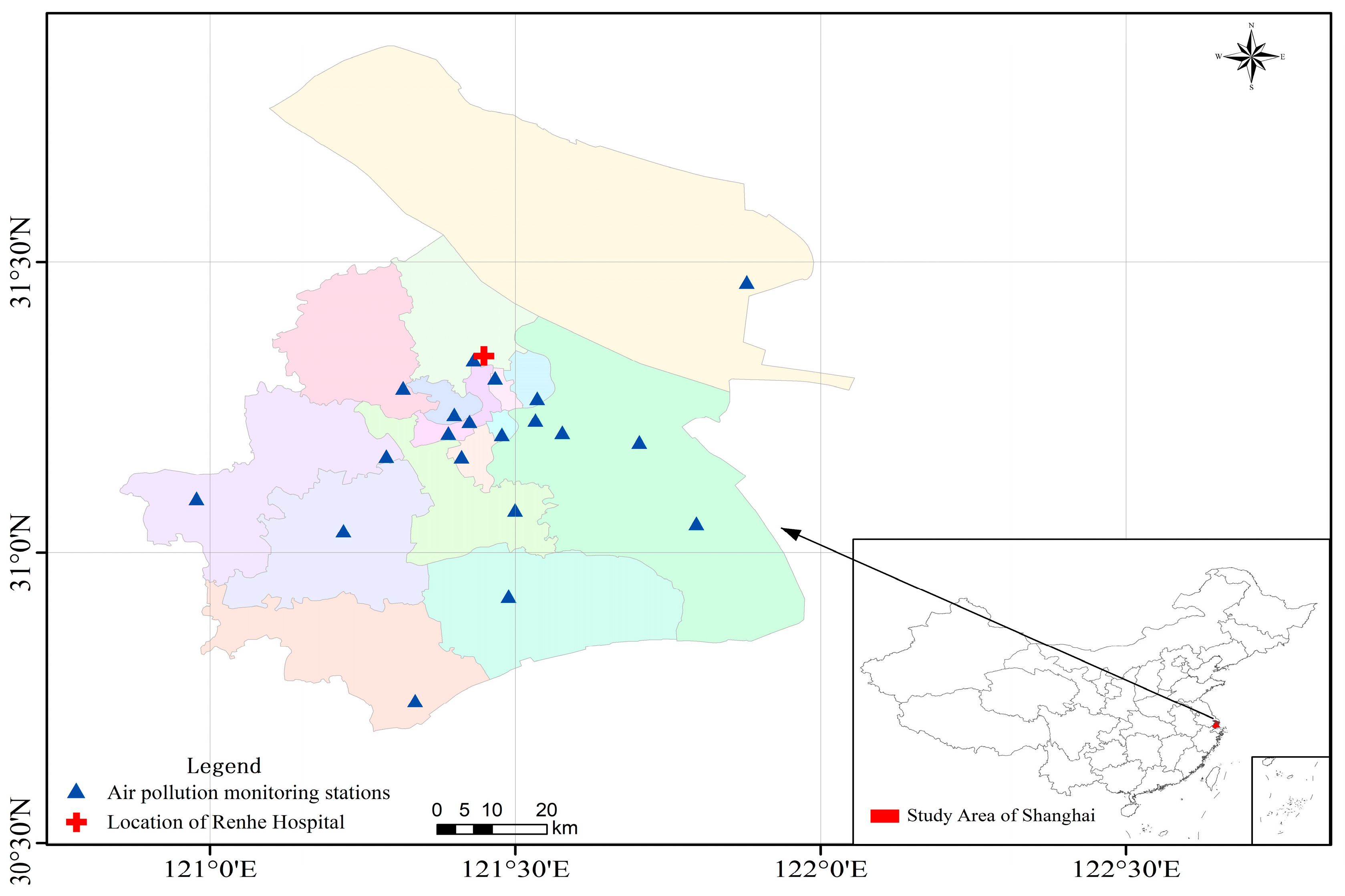
2. Materials and Methods
2.1. Wet-Bulb Temperature (WBT)
2.2. Black Carbon (BC)
2.3. Other Air Pollutant Data
2.4. Emergency Department Visits of Cause-Stable Ischemic Heart Disease (CSIHD)
2.5. Methods
2.5.1. Distributed Lag Nonlinear Model (DLNM)
2.5.2. Interaction Effect of DLNM on Wet-Bulb Temperature and Black Carbon
2.5.3. The Fraction and Number of Emergency Department Visits for CSIHD Attributed to Various Ranges of WBT/BC Exposure
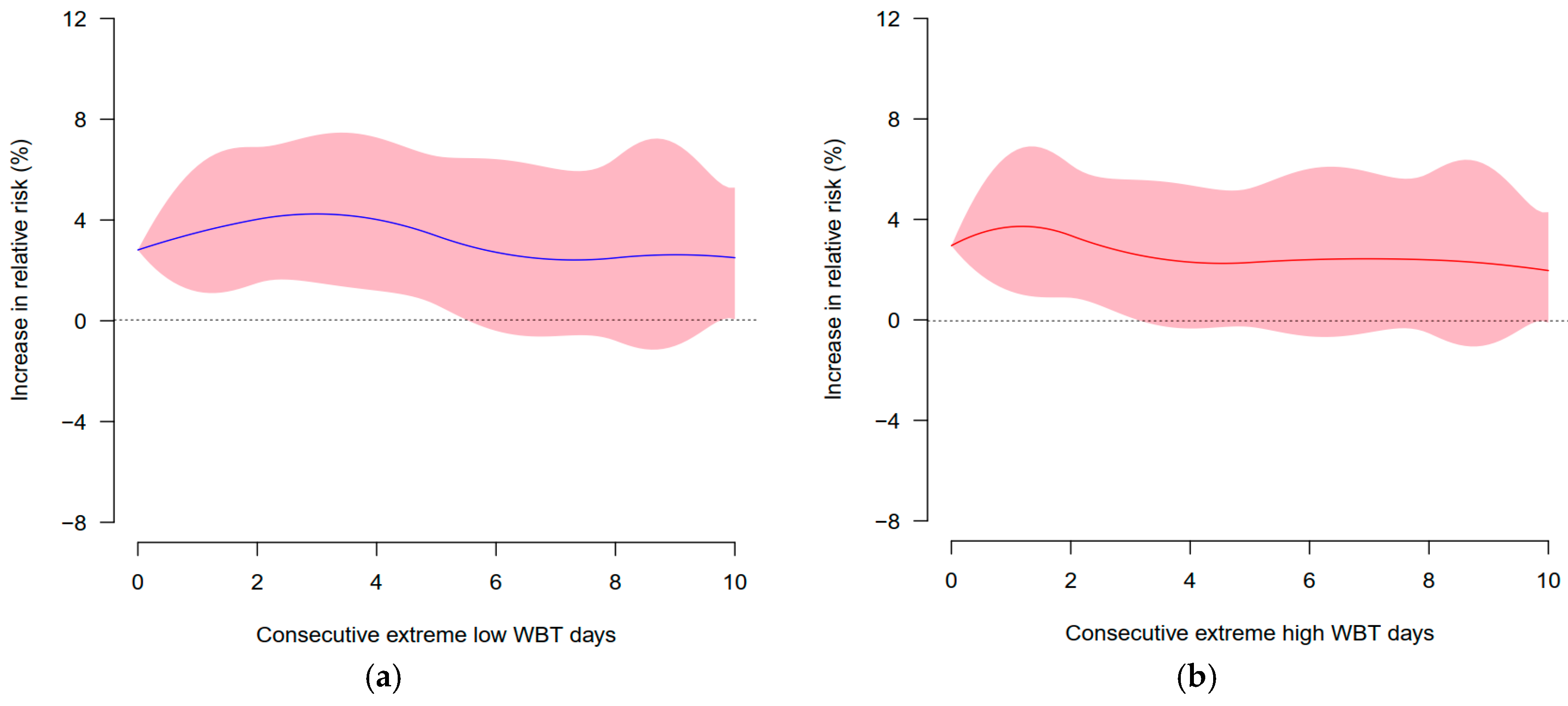
2.5.4. Effects of Short-Term Consecutive Extreme Exposure to WBT/BC
2.5.5. Sensitivity Analysis
3. Results
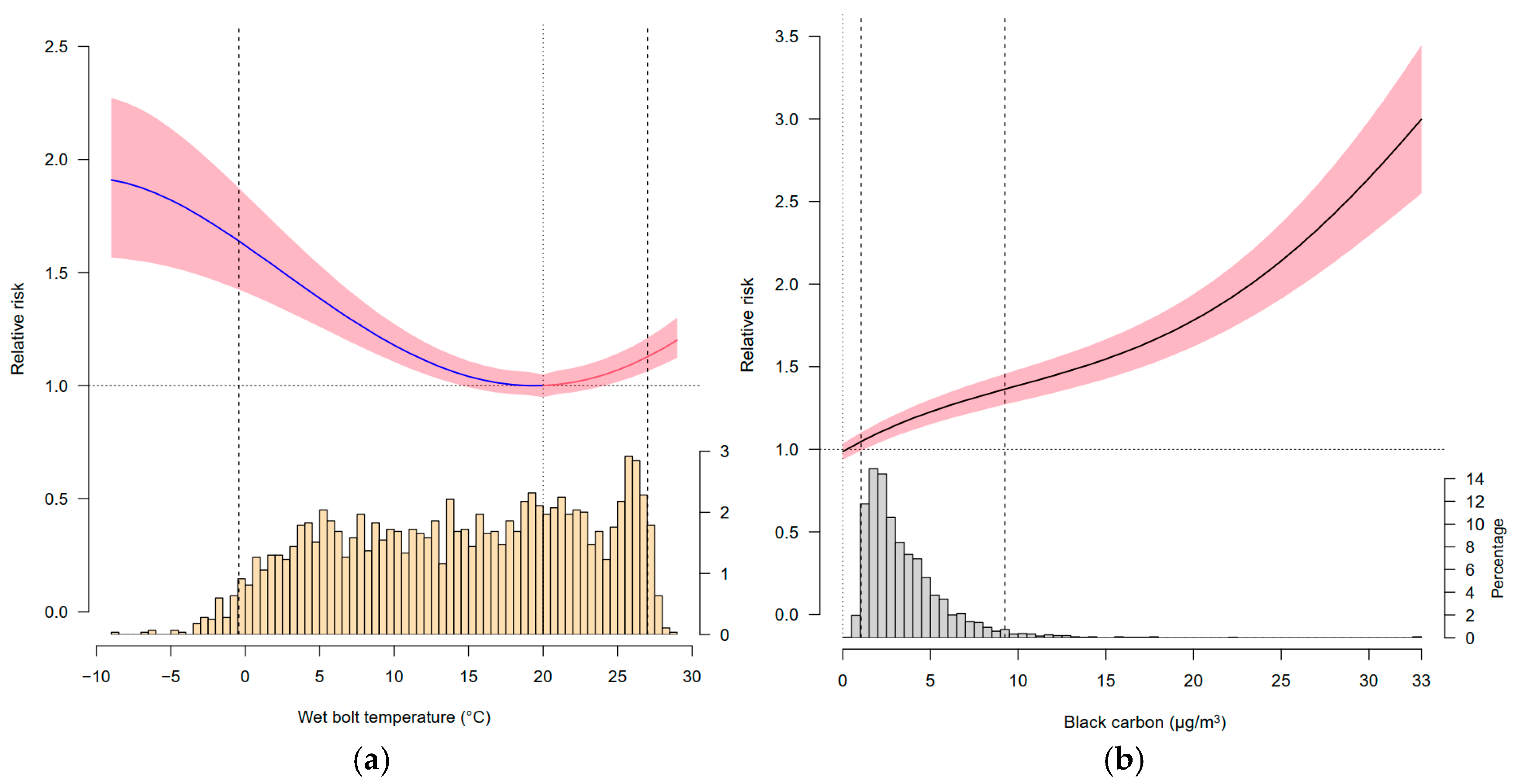
3.1. Association of WBT or BC Exposure with the Risk of Emergency Department Visits for CSIHD
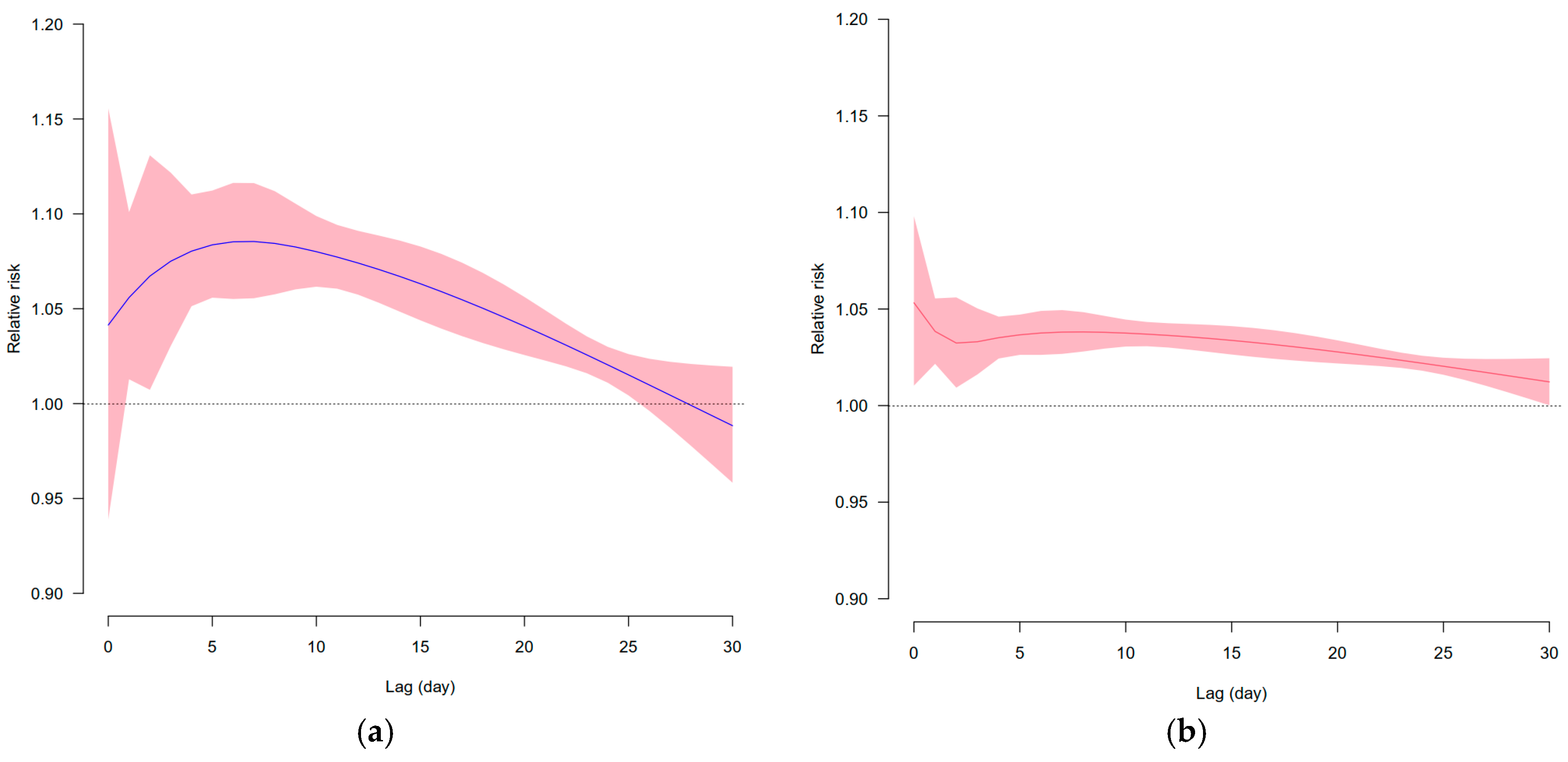
3.2. Lagged Effects of WBT or BC Exposure
3.3. Emergency Department Visits for CSIHD Attributed to Various Ranges of WBT or BC
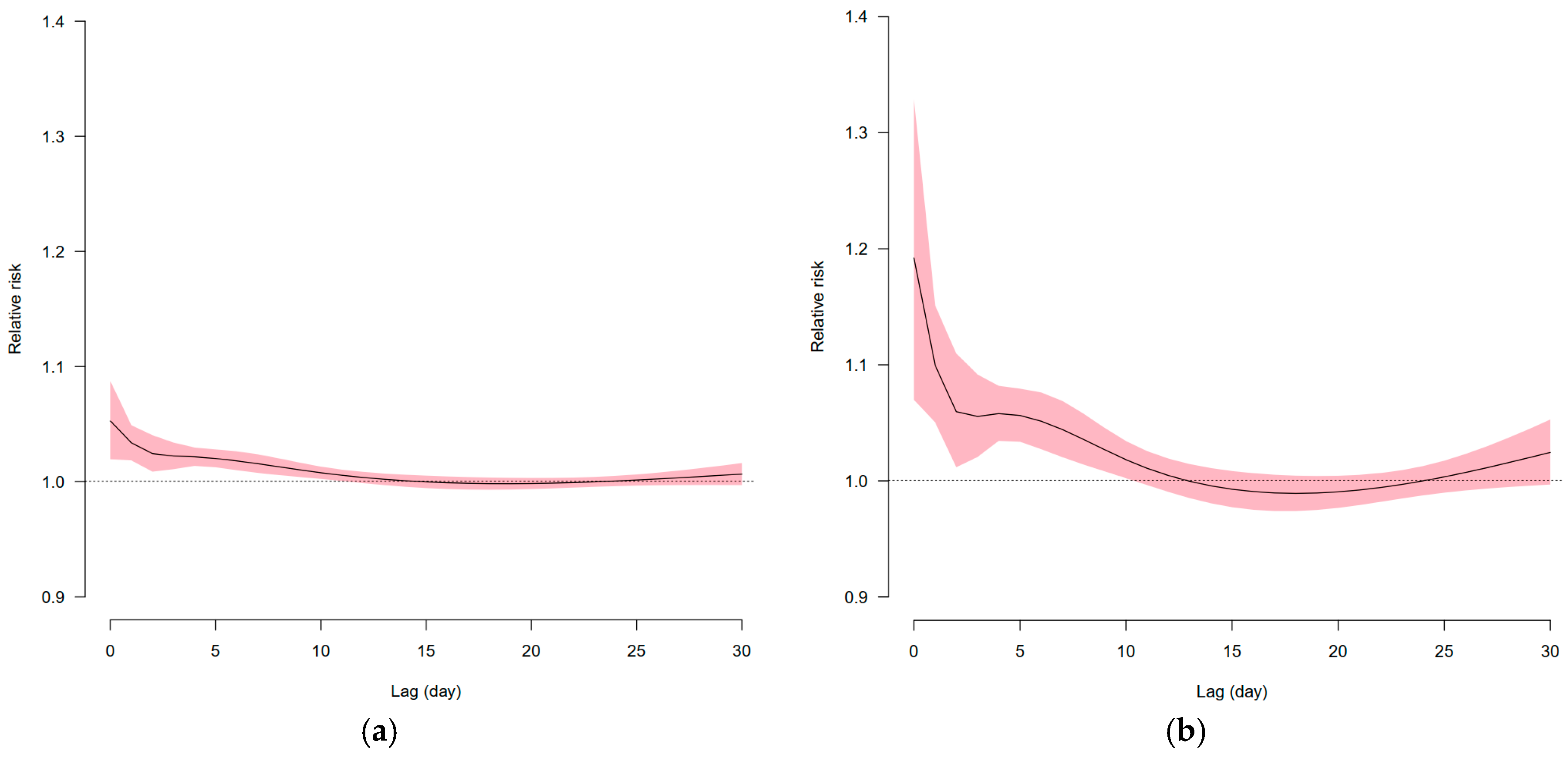
3.4. Effects of Short-Term Consecutive Extreme High and Low Exposure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cramer, W.; Guiot, J.; Fader, M.; Garrabou, J.; Gattuso, J.; Iglesias, A.; Lange, M.A.; Lionello, P.; Llasat, M.C.; Paz, S.; et al. Climate change and interconnected risks to sustainable development in the Mediterranean. Nat. Clim. Change 2018, 8, 972–980. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B. The Impact of Heat Waves on Mortality. Epidemiology 2011, 22, 68–73. [Google Scholar] [CrossRef]
- Wing, O.E.J.; Lehman, W.; Bates, P.D.; Sampson, C.C.; Quinn, N.; Smith, A.M.; Neal, J.C.; Porter, J.R.; Kousky, C. Inequitable patterns of US flood risk in the Anthropocene. Nat. Clim. Change 2022, 12, 156–162. [Google Scholar] [CrossRef]
- Ban, J.; Lu, K.; Wang, Q.; Li, T. Climate change will amplify the inequitable exposure to compound heatwave and ozone pollution. One Earth 2022, 5, 677–686. [Google Scholar] [CrossRef]
- Xu, F.; Qu, Y.; Bento, V.A.; Song, H.; Qiu, J.; Qi, J.; Wan, L.; Zhang, R.; Miao, L.; Zhang, X.; et al. Understanding climate change impacts on drought in China over the 21st century: A multi-model assessment from CMIP6. Npj Clim. Atmos. Sci. 2024, 7, 32. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, W.; Hou, K.; Lin, J.; Zhou, C.; Tong, X.; Wang, Z.; Wang, Y.; Jiang, Y.; Wang, Z.; et al. Air pollution-induced missed abortion risk for pregnancies. Nat. Sustain. 2019, 2, 1011–1017. [Google Scholar] [CrossRef]
- Burke, M.; González, F.; Baylis, P.; Heft-Neal, S.; Baysan, C.; Basu, S.; Hsiang, S. Higher temperatures increase suicide rates in the United States and Mexico. Nat. Clim. Change 2018, 8, 723–729. [Google Scholar] [CrossRef]
- Tran, H.M.; Tsai, F.; Lee, Y.; Chang, J.; Chang, L.; Chang, T.; Chung, K.F.; Kuo, H.; Lee, K.; Chuang, K.; et al. The impact of air pollution on respiratory diseases in an era of climate change: A review of the current evidence. Sci. Total Environ. 2023, 898, 166340. [Google Scholar] [CrossRef]
- Weinberger, K.R.; Haykin, L.; Eliot, M.N.; Schwartz, J.D.; Gasparrini, A.; Wellenius, G.A. Projected temperature-related deaths in ten large U.S. metropolitan areas under different climate change scenarios. Environ. Int. 2017, 107, 196–204. [Google Scholar] [CrossRef]
- Yoo, E.; Eum, Y.; Roberts, J.E.; Gao, Q.; Chen, K. Association between extreme temperatures and emergency room visits related to mental disorders: A multi-region time-series study in New York, USA. Sci. Total Environ. 2021, 792, 148246. [Google Scholar] [CrossRef]
- Zhao, Q.; Zhang, Y.; Zhang, W.; Li, S.; Chen, G.; Wu, Y.; Qiu, C.; Ying, K.; Tang, H.; Huang, J.; et al. Ambient temperature and emergency department visits: Time-series analysis in 12 Chinese cities. Environ. Pollut. 2017, 224, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Woodward, A.; Chen, B.; Liu, Q. Temperature, hospital admissions and emergency room visits in Lhasa, Tibet: A time-series analysis. Sci. Total Environ. 2014, 490, 838–848. [Google Scholar] [CrossRef]
- Zhang, Y.; Ebelt, S.T.; Shi, L.; Scovronick, N.C.; D’Souza, R.R.; Steenland, K.; Chang, H.H. Short-term associations between warm-season ambient temperature and emergency department visits for Alzheimer’s disease and related dementia in five US states. Environ. Res. 2023, 220, 115176. [Google Scholar] [CrossRef]
- Dong, J.; Brönnimann, S.; Hu, T.; Liu, Y.; Peng, J. GSDM-WBT: Global station-based daily maximum wet-bulb temperature data for 1981–2020. Earth Syst. Sci. Data 2022, 14, 5651–5664. [Google Scholar] [CrossRef]
- Yan, Y.; Xu, Y.; Yue, S. A high-spatial-resolution dataset of human thermal stress indices over South and East Asia. Sci. Data 2021, 8, 229. [Google Scholar] [CrossRef] [PubMed]
- Bucci, A.; Sanmarchi, F.; Santi, L.; Golinelli, D. Evaluating the nonlinear association between PM10 and emergency department visits. Socio-Econ. Plan. Sci. 2024, 93, 101887. [Google Scholar] [CrossRef]
- Muhsin, H.A.; Steingrimsson, S.; Oudin, A.; Åström, D.O.; Carlsen, H.K. Air pollution and increased number of psychiatric emergency room visits: A case-crossover study for identifying susceptible groups. Environ. Res. 2022, 204, 112001. [Google Scholar] [CrossRef]
- Trentalange, A.; Renzi, M.; Michelozzi, P.; Guizzi, M.; Solimini, A.G. Association between air pollution and emergency room admission for eye diseases in Rome, Italy: A time-series analysis. Environ. Pollut. 2024, 343, 123279. [Google Scholar] [CrossRef]
- Guo, P.; Feng, W.; Zheng, M.; Lv, J.; Wang, L.; Liu, J.; Zhang, Y.; Luo, G.; Zhang, Y.; Deng, C.; et al. Short-term associations of ambient air pollution and cause-specific emergency department visits in Guangzhou, China. Sci. Total Environ. 2018, 613–614, 306–313. [Google Scholar] [CrossRef]
- Ugalde-Resano, R.; Riojas-Rodríguez, H.; Texcalac-Sangrador, J.L.; Cruz, J.C.; Hurtado-Díaz, M. Short term exposure to ambient air pollutants and cardiovascular emergency department visits in Mexico city. Environ. Res. 2022, 207, 112600. [Google Scholar] [CrossRef]
- Wei, J.; Wang, J.; Li, Z.; Kondragunta, S.; Anenberg, S.; Wang, Y.; Zhang, H.; Diner, D.; Hand, J.; Lyapustin, A.; et al. Long-term mortality burden trends attributed to black carbon and PM2·5 from wildfire emissions across the continental USA from 2000 to 2020: A deep learning modelling study. Lancet Planet. Health 2023, 7, e963–e975. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.; Pozzer, A.; Haines, A.; Klingmüller, K.; Münzel, T.; Paasonen, P.; Sharma, A.; Venkataraman, C.; Lelieveld, J. Global health burden of ambient PM2.5 and the contribution of anthropogenic black carbon and organic aerosols. Environ. Int. 2022, 159, 107020. [Google Scholar] [CrossRef]
- Cao, S.; Zhang, S.; Gao, C.; Yan, Y.; Bao, J.; Su, L.; Liu, M.; Peng, N.; Liu, M. A long-term analysis of atmospheric black carbon MERRA-2 concentration over China during 1980–2019. Atmos. Environ. 2021, 264, 118662. [Google Scholar] [CrossRef]
- Xu, X.; Yang, X.; Zhu, B.; Tang, Z.; Wu, H.; Xie, L. Characteristics of MERRA-2 black carbon variation in east China during 2000–2016. Atmos. Environ. 2020, 222, 117140. [Google Scholar] [CrossRef]
- Zhou, Y.; Jin, Y.; Zhang, Z. Short-term exposure to various ambient air pollutants and emergency department visits for cause-stable ischemic heart disease: A time-series study in Shanghai, China. Sci. Rep. 2023, 13, 16989. [Google Scholar] [CrossRef] [PubMed]
- Niu, Y.; Gao, Y.; Yang, J.; Qi, L.; Xue, T.; Guo, M.; Zheng, J.; Lu, F.; Wang, J.; Liu, Q. Short-term effect of apparent temperature on daily emergency visits for mental and behavioral disorders in Beijing, China: A time-series study. Sci. Total Environ. 2020, 733, 139040. [Google Scholar] [CrossRef]
- Yang, R.; Wang, Y.; Dong, J.; Wang, J.; Zhang, H.; Bao, H. Association between ambient temperature and cause-specific respiratory outpatient visits: A case-crossover design with a distributed lag nonlinear model in Lanzhou, China. Urban. Clim. 2022, 46, 101303. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsberg, B.; et al. Mortality risk attributable to high and low ambient temperature: A multicountry observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Hou, K.; Zhang, L.; Xu, X.; Yang, F.; Chen, B.; Hu, W.; Shu, R. High ambient temperatures are associated with urban crime risk in Chicago. Sci. Total Environ. 2023, 856, 158846. [Google Scholar] [CrossRef]
- Renjie, C.; Peng, Y.; Lijun, W.; Cong, L.; Yue, N.; Weidong, W.; Yixuan, J.; Yunning, L.; Jiangmei, L.; Jinlei, Q.; et al. Association between ambient temperature and mortality risk and burden: Time series study in 272 main Chinese cities. BMJ-Brit Med. J. 2018, 363, k4306. [Google Scholar]
- Lin, L.; Huang, P.; Weng, L. Selecting Path Models in SEM: A Comparison of Model Selection Criteria. Struct. Equ. Model. A Multidiscip. J. 2017, 24, 855–869. [Google Scholar] [CrossRef]
- Zhang, L.; Liu, W.; Hou, K.; Lin, J.; Song, C.; Zhou, C.; Huang, B.; Tong, X.; Wang, J.; Rhine, W.; et al. Air pollution exposure associates with increased risk of neonatal jaundice. Nat. Commun. 2019, 10, 3741. [Google Scholar] [CrossRef]
- Peng, W.; Fan, Z.; Duan, J.; Gao, W.; Wang, R.; Liu, N.; Li, Y.; Hua, S. Assessment of interactions between influencing factors on city shrinkage based on geographical detector: A case study in Kitakyushu, Japan. Cities 2022, 131, 103958. [Google Scholar] [CrossRef]
- Zhang, H.; Dong, G.; Wang, J.; Zhang, T.; Meng, X.; Yang, D.; Liu, Y.; Lu, B. Understanding and extending the geographical detector model under a linear regression framework. Int. J. Geogr. Inf. Sci. 2023, 37, 2437–2453. [Google Scholar] [CrossRef]
- Gasparrini, A.; Leone, M. Attributable risk from distributed lag models. BMC Med. Res. Methodol. 2014, 14, 55. [Google Scholar] [CrossRef]
- Hou, K.; Zhang, L.; Xu, X.; Yang, F.; Chen, B.; Hu, W. Ambient temperatures associated with increased risk of motor vehicle crashes in New York and Chicago. Sci. Total Environ. 2022, 830, 154731. [Google Scholar] [CrossRef] [PubMed]
- Goel, H.; Shah, K.; Kumar, A.; Hippen, J.T.; Nadar, S.K. Temperature, cardiovascular mortality, and the role of hypertension and renin–angiotensin–aldosterone axis in seasonal adversity: A narrative review. J. Hum. Hypertens. 2022, 36, 1035–1047. [Google Scholar] [CrossRef]
- Hystad, P.; Larkin, A.; Rangarajan, S.; Al Habib, K.F.; Avezum, Á.; Calik, K.B.T.; Chifamba, J.; Dans, A.; Diaz, R.; du Plessis, J.L.; et al. Associations of outdoor fine particulate air pollution and cardiovascular disease in 157,436 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet Planet. Health 2020, 4, e235–e245. [Google Scholar] [CrossRef]
- Li, T.; Yu, Z.; Xu, L.; Wu, Y.; Yu, L.; Yang, Z.; Shen, P.; Lin, H.; Shui, L.; Tang, M.; et al. Residential greenness, air pollution, and incident ischemic heart disease: A prospective cohort study in China. Sci. Total Environ. 2022, 838, 155881. [Google Scholar] [CrossRef]
- Cheng, B.; Pan, C.; Cai, Q.; Liu, L.; Cheng, S.; Yang, X.; Meng, P.; Wei, W.; He, D.; Liu, H.; et al. Long-term ambient air pollution and the risk of musculoskeletal diseases: A prospective cohort study. J. Hazard. Mater. 2024, 466, 133658. [Google Scholar] [CrossRef]
- Nemmar, A.; Hoet, P.H.M.; Vanquickenborne, B.; Dinsdale, D.; Thomeer, M.; Hoylaerts, M.F.; Vanbilloen, H.; Mortelmans, L.; Nemery, B. Passage of Inhaled Particles into the Blood Circulation in Humans. Circulation 2002, 105, 411–414. [Google Scholar] [CrossRef] [PubMed]
- Lippmann, S.J.; Fuhrmann, C.M.; Waller, A.E.; Richardson, D.B. Ambient temperature and emergency department visits for heat-related illness in North Carolina, 2007–2008. Environ. Res. 2013, 124, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zheng, M.; Lv, J.; Shi, T.; Liu, P.; Wu, Y.; Feng, W.; He, W.; Guo, P. Interactions between ambient air pollutants and temperature on emergency department visits: Analysis of varying-coefficient model in Guangzhou, China. Sci. Total Environ. 2019, 668, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Wadhera, R.K.; Shen, C.; Gondi, S.; Chen, S.; Kazi, D.S.; Yeh, R.W. Cardiovascular Deaths During the COVID-19 Pandemic in the United States. J. Am. Coll. Cardiol. 2021, 77, 159–169. [Google Scholar] [CrossRef]
- Roth, G.A.; Vaduganathan, M.; Mensah, G.A. Impact of the COVID-19 Pandemic on Cardiovascular Health in 2020: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2022, 80, 631–640. [Google Scholar] [CrossRef]
- Venter, Z.S.; Aunan, K.; Chowdhury, S.; Lelieveld, J. Air pollution declines during COVID-19 lockdowns mitigate the global health burden. Environ. Res. 2021, 192, 110403. [Google Scholar] [CrossRef]
- Hu, M.; Chen, Z.; Cui, H.; Wang, T.; Zhang, C.; Yun, K. Air pollution and critical air pollutant assessment during and after COVID-19 lockdowns: Evidence from pandemic hotspots in China, the Republic of Korea, Japan, and India. Atmos. Pollut. Res. 2021, 12, 316–329. [Google Scholar] [CrossRef]


| Variables | Time Span | Mean Value | Minimum Value | 25th Percentile | 50th Percentile | 75th Percentile | Maximum Value |
|---|---|---|---|---|---|---|---|
| Emergency department visits for CSIHD | 2013–2020 | 6.32 | 1 | 4 | 6 | 8 | 23 |
| WBT (°C) | 2013–2020 | 14.39 | −8.92 | 7.43 | 14.87 | 21.49 | 28.74 |
| BC (μg/m3) | 2013–2020 | 3.47 | 0.4 | 1.87 | 2.82 | 4.4 | 32.69 |
| O3 (μg/m3) | 2013–2020 | 93.11 | 6.18 | 62.3 | 88.03 | 117.13 | 280 |
| NO2 (μg/m3) | 2013–2020 | 41.44 | 5.24 | 27.86 | 37.71 | 51.84 | 140.08 |
| SO2 (μg/m3) | 2013–2020 | 13.14 | 4 | 7.4 | 10.54 | 14.92 | 106.9 |
| CO (μg/m3) | 2013–2020 | 0.78 | 0.31 | 0.56 | 0.67 | 0.86 | 19.92 |
| Variables | Lag Days | Relative Risk and 95% Confidence Interval (CI) | ||
|---|---|---|---|---|
| Estimated Value | Lower Bound of 95% CI | Upper Bound of 95% CI | ||
| 2.5th percentile WBT | 0 | 1.042 | 0.938 | 1.157 |
| 15 | 1.068 | 1.043 | 1.076 | |
| 28 | 0.987 | 0.935 | 1.022 | |
| 97.5th percentile WBT | 0 | 1.057 | 1.016 | 1.093 |
| 15 | 1.032 | 1.026 | 1.041 | |
| 28 | 1.018 | 1.012 | 1.023 | |
| 2.5th percentile BC | 0 | 1.061 | 1.021 | 1.085 |
| 15 | 1.002 | 0.923 | 1.097 | |
| 28 | 1.001 | 0.964 | 1.192 | |
| 97.5th percentile BC | 0 | 1.326 | 1.072 | 1.187 |
| 15 | 0.986 | 0.974 | 1.013 | |
| 28 | 1.022 | 0.994 | 1.043 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Q.; Hou, K.; Xu, X.; Wang, Z. Non-Optimal Wet-Bulb Temperature and Short-Term Black Carbon Exposure Largely Impact Emergency Department Visits for Cause-Stable Ischemic Heart Disease. Atmosphere 2025, 16, 542. https://doi.org/10.3390/atmos16050542
Chen Q, Hou K, Xu X, Wang Z. Non-Optimal Wet-Bulb Temperature and Short-Term Black Carbon Exposure Largely Impact Emergency Department Visits for Cause-Stable Ischemic Heart Disease. Atmosphere. 2025; 16(5):542. https://doi.org/10.3390/atmos16050542
Chicago/Turabian StyleChen, Qianrong, Kun Hou, Xia Xu, and Zhen Wang. 2025. "Non-Optimal Wet-Bulb Temperature and Short-Term Black Carbon Exposure Largely Impact Emergency Department Visits for Cause-Stable Ischemic Heart Disease" Atmosphere 16, no. 5: 542. https://doi.org/10.3390/atmos16050542
APA StyleChen, Q., Hou, K., Xu, X., & Wang, Z. (2025). Non-Optimal Wet-Bulb Temperature and Short-Term Black Carbon Exposure Largely Impact Emergency Department Visits for Cause-Stable Ischemic Heart Disease. Atmosphere, 16(5), 542. https://doi.org/10.3390/atmos16050542






