Ventilation Methods against Indoor Aerosol Infection of COVID-19 in Japan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ventilation Measures against COVID-19 in Japan
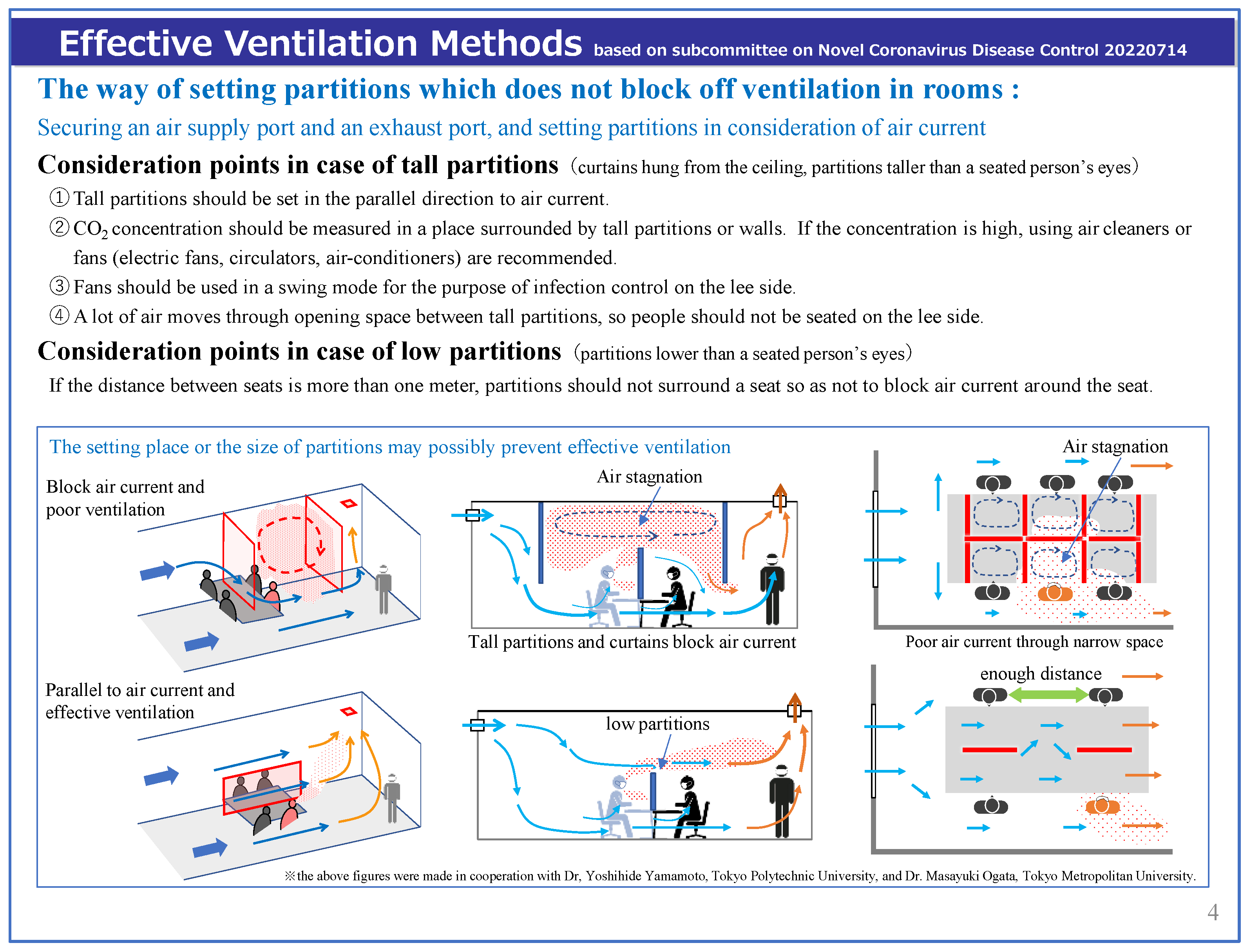
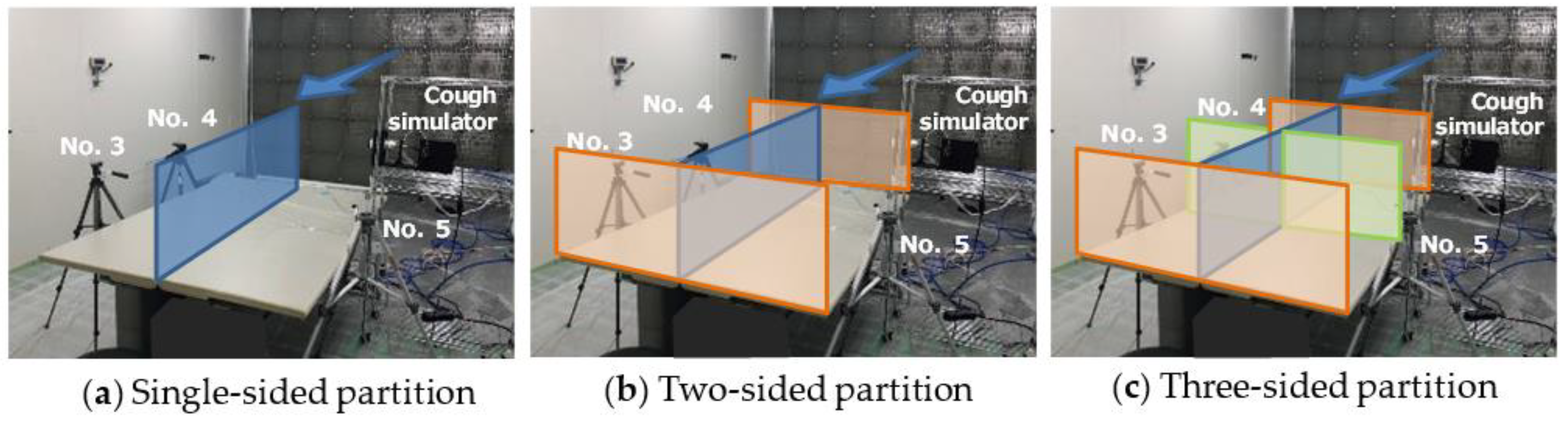
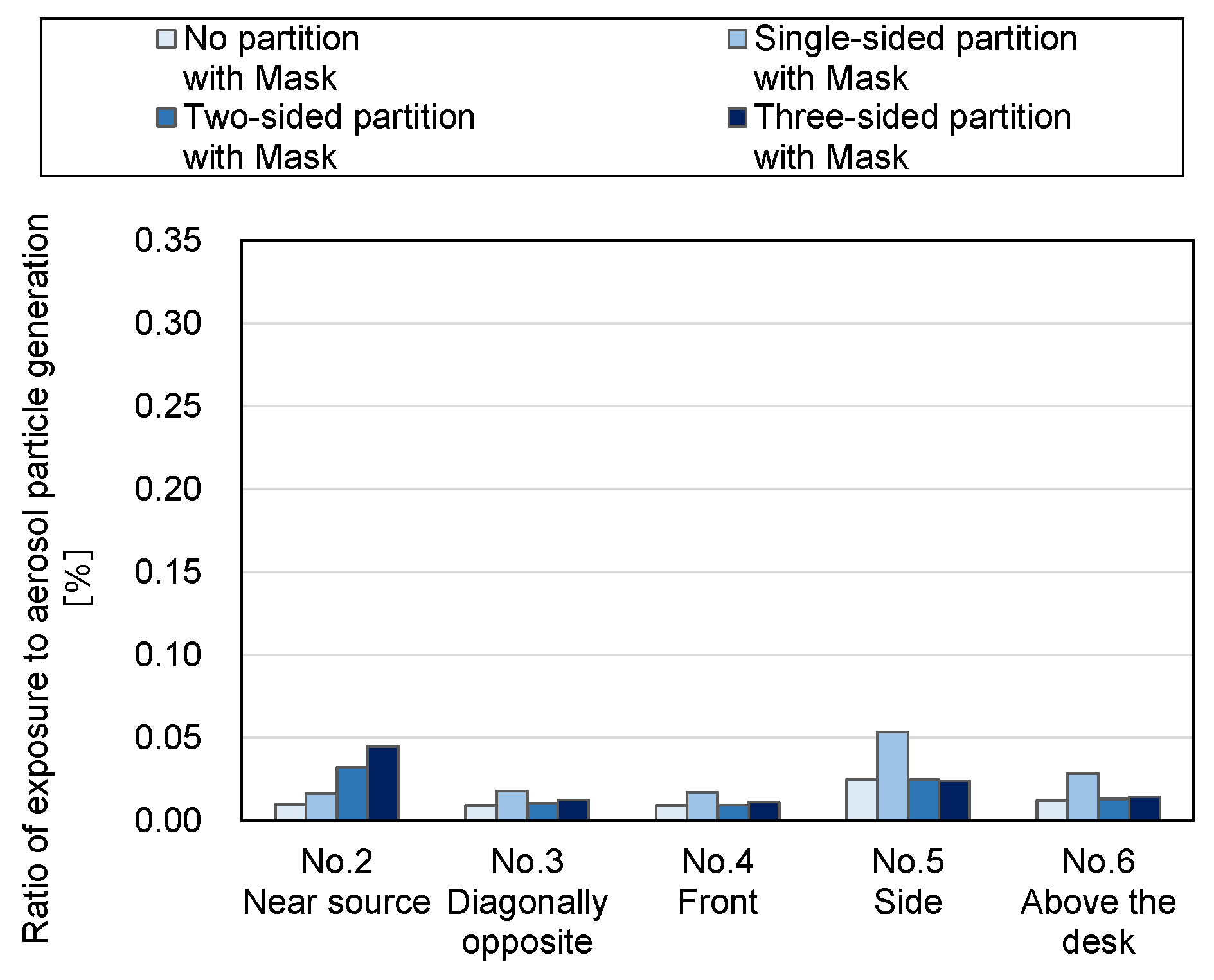
2.2. Way of Setting Partitions Considering Ventilation Effectiveness
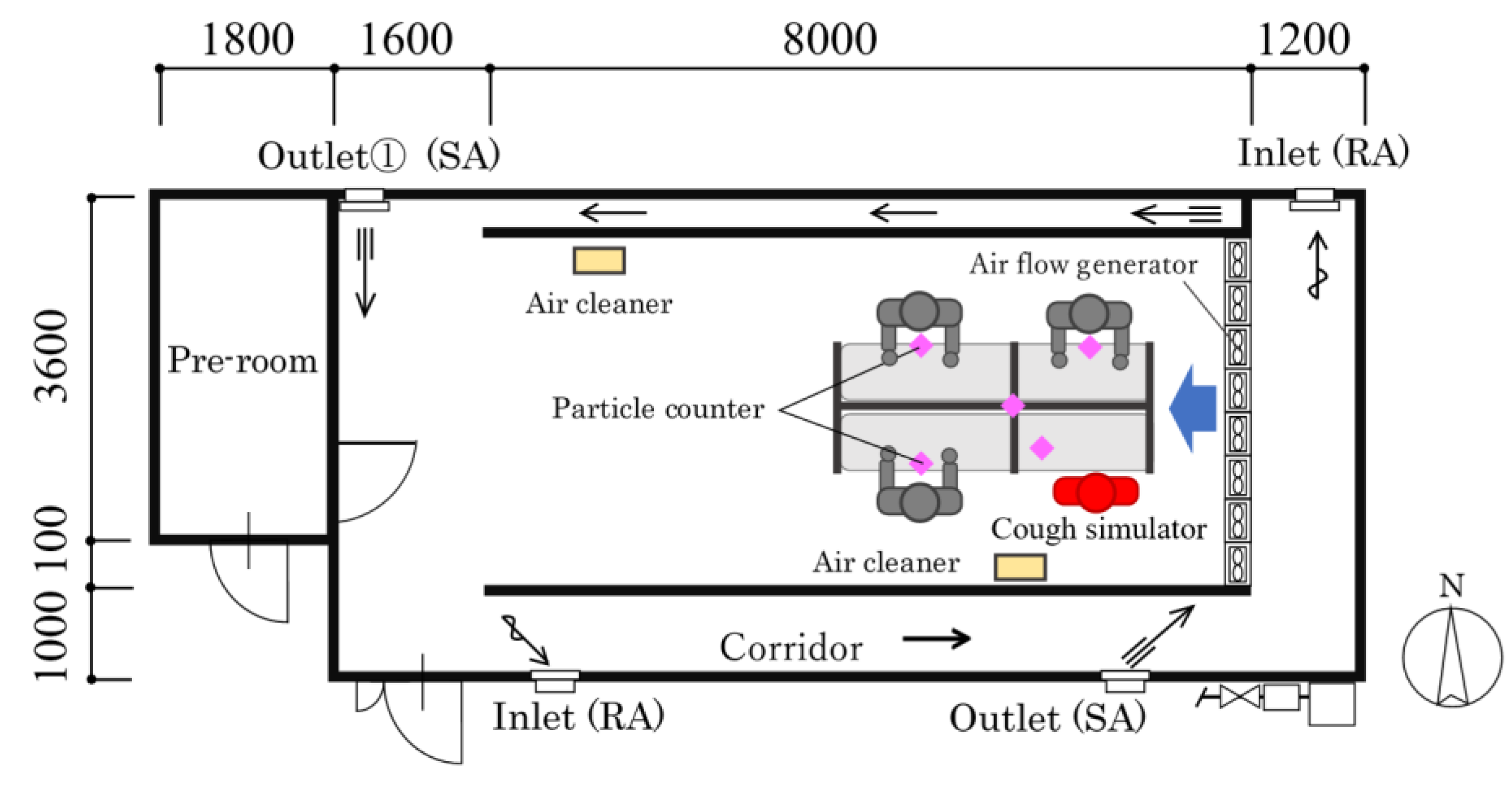
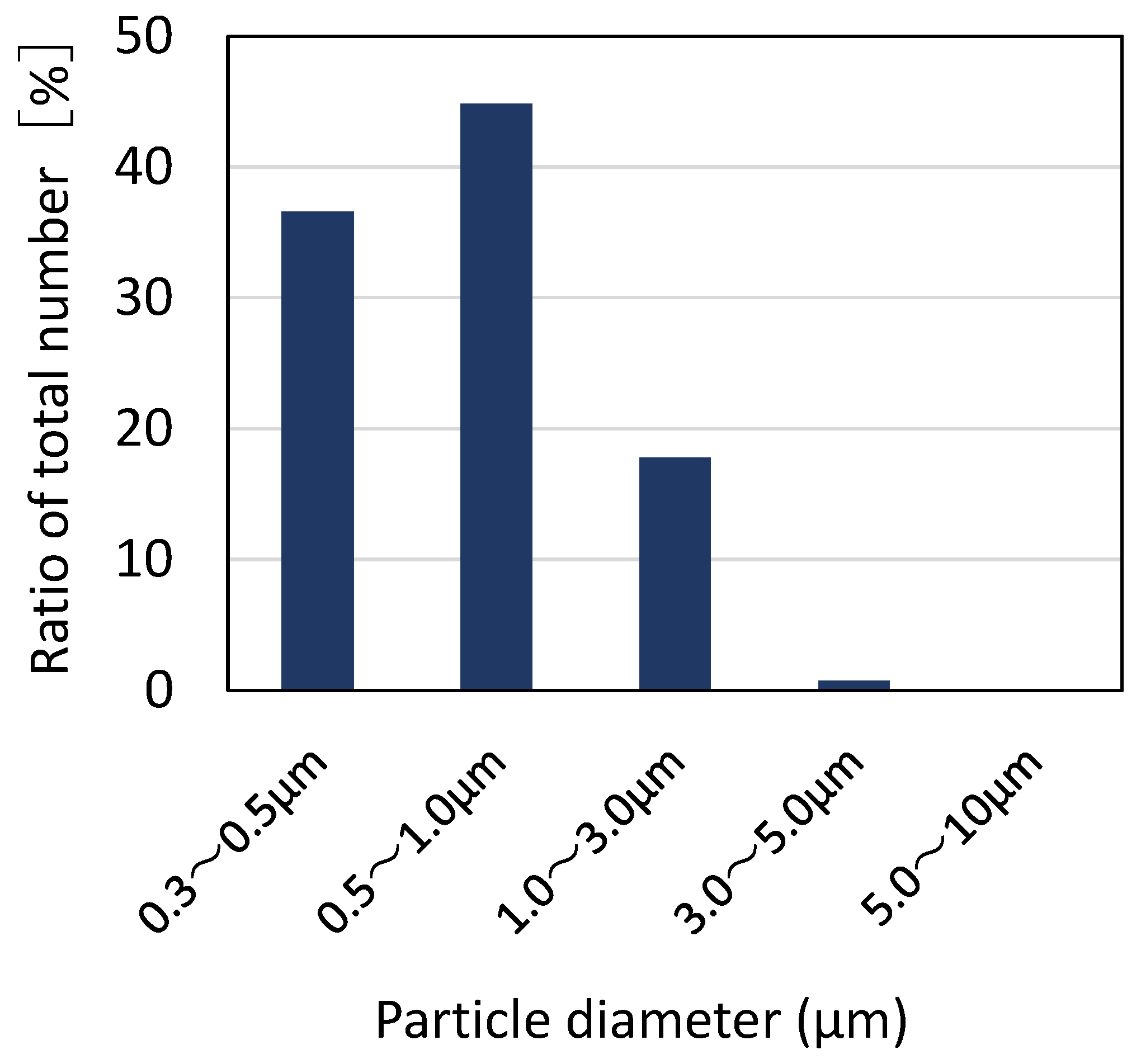
2.2.1. Experimental Setup
2.2.2. Evaluation Method of Experimental Results
2.3. Effective Ventilation Methods in an Emergent Proposal by Subcommittee on Novel Coronavirus Disease Control (14 July 2022)
3. Results
3.1. Ventilation Measures against COVID-19 in Japan
3.1.1. Effective Ventilation Methods in “Closed and Poorly-Ventilated Indoor Spaces” in Commercial Facilities, etc. (30 March 2020) [4]
3.1.2. Advisory Board on COVID-19 Control of the Ministry of Health, Labour and Welfare (30 July 2020)
3.1.3. Measures against COVID-19 Concerning Summer Indoor Environment in Japan (May 2020) [9]
- [In every indoor space]
- Enough ventilation is necessary to prevent the infection of COVID-19.
- Opening windows is an effective ventilation method, and it is desirable to open them wider and for a longer time.
- In summer, air-conditioning is essential for good health, such as heat stroke prevention. (In winter, heating is essential for good health, such as heat shock.)
- General air-conditioners do not function as ventilators, so mechanical ventilation or opening windows is necessary.
- When windows are open, it is necessary to prevent animals or insect pests from coming in.
- [In case an air-conditioner and a ventilation system are equipped]
- 6.
- It is necessary to ensure the operation of designed ventilation rates by maintaining and inspecting the equipment.
- 7.
- It is recommended to control the number of people in a room, to ensure the ventilation rate for a person and shorten people’s stay in a room.
- 8.
- Measures such as the improvement of ventilation effects through the development of air-conditioners and ventilation systems, and the use of air cleaners and humidifiers in winter, have to be discussed considering the characteristics of each building, that is, what it is used for, how often it is used, or what kind of air-conditioner or ventilation system it has.
3.1.4. Effective Ventilation Methods in “Closed and Poorly-Ventilated Indoor Spaces” in Winter (27 November 2020) [10]
- (1)
- In commercial facilities, etc., where mechanical ventilation systems are installed, the required ventilation rates (30 m3 per hour per person) should be kept, and room temperature and relative humidity should be kept at 18 °C or higher and 40% or higher, with the adjustment of the rates of fresh air supply by the mechanical ventilation system.
- (2)
- In commercial facilities, etc., without mechanical ventilation facilities or in commercial facilities, etc. in which ventilation rates are not enough with their mechanical ventilation facilities, on condition that room temperature and humidity should be kept at 18 °C or higher and 40% or higher, a window should be open all the time while heating systems are on. The use of humidifiers is also effective.
- (3)
- In case the indoor temperature and relative humidity are under 18 °C and 40% while windows are open, the use of portable air cleaners is effective in compensating for the lack of ventilation. In such cases, portable air cleaners of which the filtration type is HEPA (High Efficiency Particulate Air) and of which airflow rates are about 5 m3 per minute or more should be used, and air cleaners should be settled within 10 m2 around people in the room, and the wind direction of the air cleaner should correspond to the direction of fresh air supply to make an air current.
- (4)
- To confirm the ventilation of a room, CO2 concentration should always be measured, and the value should be under 1000 ppm. However, when an air cleaner is used while a window is open, the measurement of CO2 concentration does not reflect the effect of the air cleaner, so it cannot be an appropriate evaluation.
3.1.5. The Infection Routes of SARS-CoV-2 by the National Institute of Infectious Diseases (Published on 28 March 2022) [11]
- (1)
- breathing in an aerosol containing virus floating in the air (aerosol infection)
- (2)
- the attachment of droplets containing the virus on bare mucous membranes such as mouths, noses, or eyes (droplet infection)
- (3)
- fingers touching bare mucous membranes after touching droplets containing the virus or the surface of things with a virus (contact infection)
3.2. Way of Setting Partitions Considering Ventilation Effectiveness
3.3. Effective Ventilation Methods in an Emergent Proposal by Subcommittee on Novel Coronavirus Disease Control (14 July 2022)
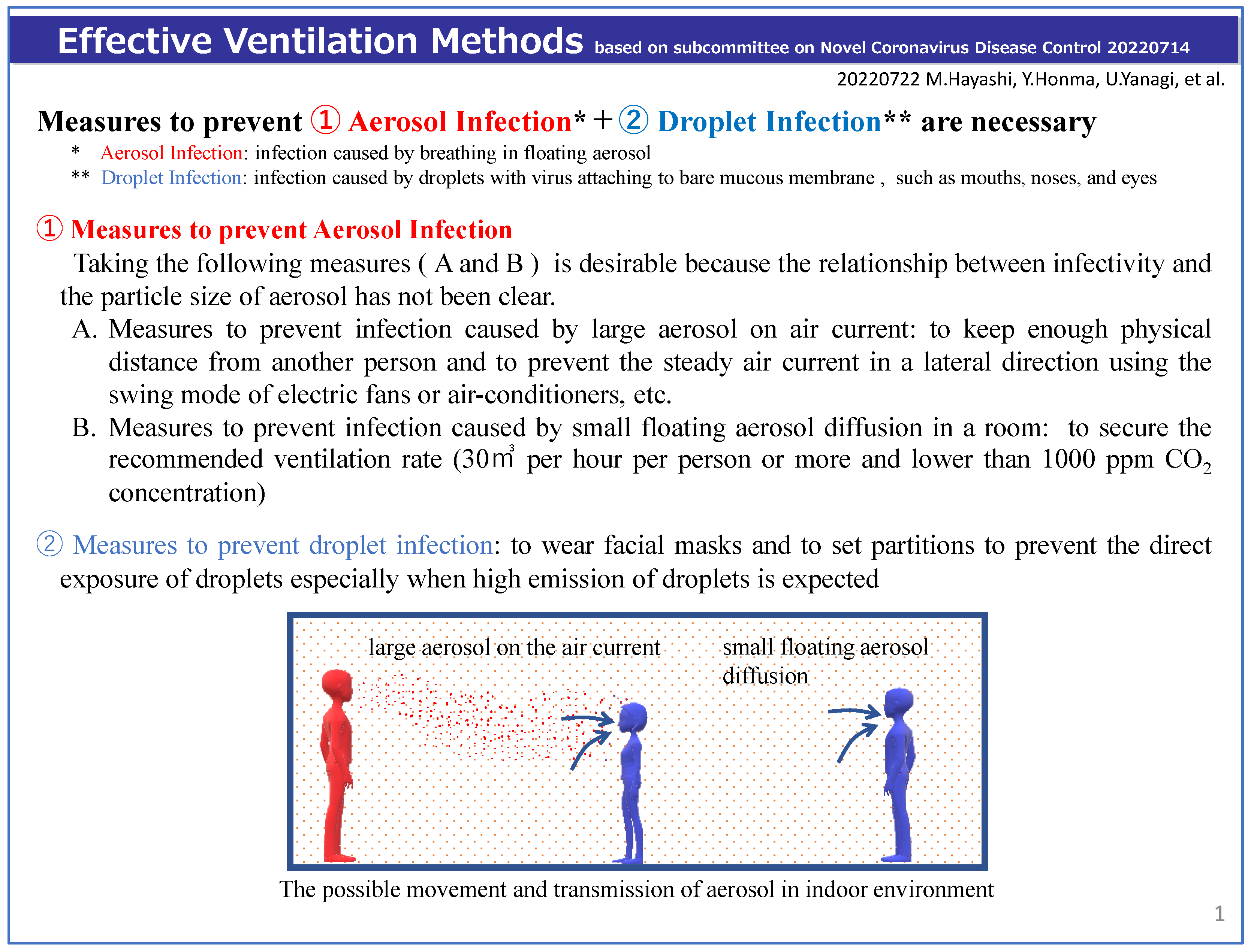
3.3.1. Measures against the Two Types of Aerosol Infection (Figure 8)
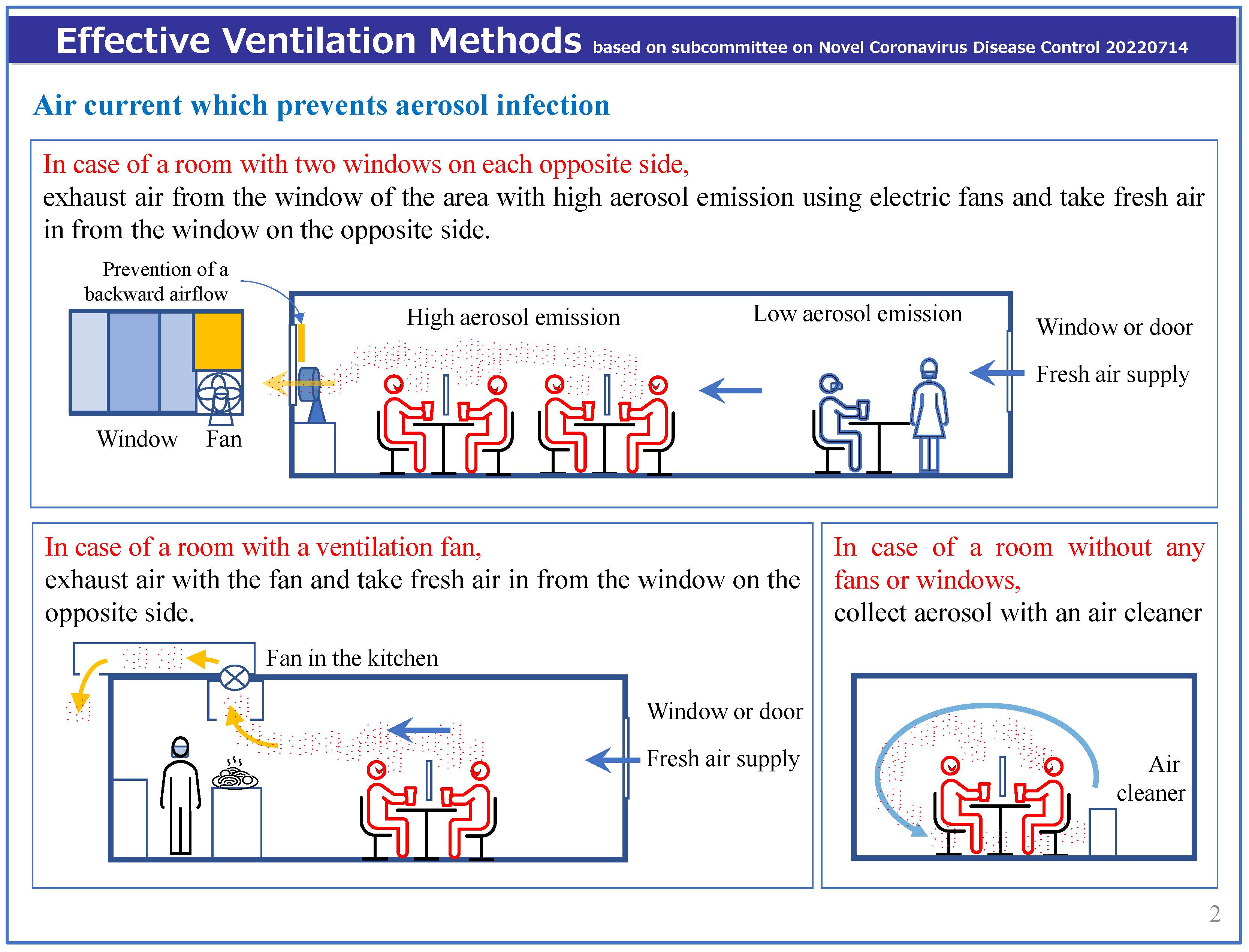
3.3.2. Effective Ventilation Measures against Aerosol Infection (Figure 9 and Figure 10)

3.3.3. Measures against Droplet Infection without Any Disturbance of Air Current (Figure 11)
3.3.4. The Matters That Require Attention Considering the Characteristics of Facilities
- (1)
- Desirable air current is “a patient ⇒ a fan (circulator or mechanical fan) ⇒ a vent (exhaust fan or window + fan)”. A fan should be set on the lee side of a patient’s breath, and no one should be away from the space between a patient and a fan. In the case of a patient’s care, a nursing person (wearing a facial mask) ⇒ a patient ⇒ a fan ⇒ a vent (exhaust fan or window) (Figure 3)
- (2)
- When nursing a patient who is not wearing a facial mask, for example, giving a patient a meal, bathing a patient, or cleaning a patient’s mouth, etc., a nursing person should wear both a face shield and a facial mask to prevent droplet infection and the space should be well ventilated in case of much aerosol emission.
- (3)
- In order to get enough air current, the mechanical power and location of fans should be adjusted (The direction of the air current should be confirmed using a smoke tester, smoke from an incense stick, a piece of tissue paper, or thread).
- (4)
- CO2 concentration monitors should be used in locker rooms, dressing rooms, staff rooms, etc. to know the state of ventilation in each room and to limit the number of people in the room if necessary.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Novel Coronavirus Infectious Disease Control Experts Meeting. View on Novel Coronavirus, Infectious Disease Control. 9 March 2020. Available online: https://www.mhlw.go.jp/content/10900000/000606000.pdf (accessed on 23 November 2022). (In Japanese)
- Prime Minister’s Office. Let’s Avoid These Three Conditions When We Go Out! Flyer. Available online: https://www.kantei.go.jp/jp/content/000061234.pdf (accessed on 23 November 2022). (In Japanese)
- The Society of Heating. Air-Conditioning and Sanitary Engineers of Japan (SHASE) and Architectural Institute of Japan (AIJ), Role of Ventilation in the Control of the COVID-19 Infection: Emergency Presidential Discourse. Available online: https://www.aij.or.jp/jpn/databox/2020/20200323_Eng_final.pdf (accessed on 23 November 2022). (In Japanese).
- The Ministry of Health, Labour and Welfare. Reference Data Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ in Commercial Facilities, etc. 30 March 2020. Available online: https://www.mhlw.go.jp/content/10900000/000616069.pdf (accessed on 1 October 2022). (In Japanese)
- The Ministry of Health, Labour and Welfare. Toward the Managers of Commercial Facilities, Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’. 3 April 2020. Available online: https://www.mhlw.go.jp/content/10900000/000618969.pdf (accessed on 1 October 2022). (In Japanese)
- The Ministry of Health, Labour and Welfare. Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ while Avoiding Heatstroke. 17 June 2020. Available online: https://www.mhlw.go.jp/content/10900000/000640913.pdf (accessed on 1 October 2022). (In Japanese)
- The Ministry of Health, Labour and Welfare. Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ in Winter. 27 November 2020. Available online: https://www.mhlw.go.jp/content/000698868.pdf (accessed on 1 October 2022). (In Japanese)
- Ogata, M.; Ichikawa, M.; Tsutsumi, H.; Ariga, T.; Hori, S.; Tanabe, S.-I. Measurement of cough droplet deposition using the cough machine. J. Environ. Eng. (Transactions AIJ) 2018, 83, 57–64. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, M.; Yanagi, U.; Azuma, K.; Kagi, N.; Ogata, M.; Morimoto, S.; Hayama, H.; Mori, T.; Kikuta, K.; Tanabe, S.; et al. Measures against COVID-19 concerning Summer Indoor Environment in Japan. Jpn. Arch. Rev. 2020, 3, 423–434. [Google Scholar] [CrossRef]
- The Ministry of Health, Labour and Welfare. Reference Data Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ in Winter. 27 November 2020. Available online: https://www.mhlw.go.jp/content/10906000/000698849.pdf (accessed on 1 October 2022). (In Japanese)
- National Institute of Infectious Diseases. Infection Routes of SARS-CoV-2. 28 March 2022. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/2484-idsc/11053-covid19-78.html (accessed on 1 October 2022). (In Japanese).
- World Health Organization (WHO). Coronavirus Disease (COVID-19) How Is It Transmitted? 2021. Available online: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted (accessed on 5 November 2022).
- Centers for Disease Control and Prevention (CDC). Scientific Brief: SARS-CoV-2 Transmission. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html (accessed on 25 October 2022).
- Jang, S.; Han, S.H.; Rhee, J.-Y. Cluster of Coronavirus Disease Associated with Fitness Dance Classes, South Korea. Emerg. Infect. Dis. 2020, 26, 1917–1920. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Sun, W.; Huang, J.; Gamber, M.; Wu, J.; He, G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1343–1345. [Google Scholar] [CrossRef] [PubMed]
- Katelaris, A.L.; Wells, J.; Clark, P.; Norton, S.; Rockett, R.; Arnott, A.; Sintchenko, V.; Corbett, S.; Bag, S.K. Epidemiologic Evidence for Airborne Transmission of SARS-CoV-2during Church Singing, Australia, 2020. Emerg Infect Dis. 2021, 27, 1677–1680. [Google Scholar] [CrossRef] [PubMed]
- Toyokawa, T.; Shimada, T.; Hayamizu, T.; Sekizuka, T.; Zukeyama, Y.; Yasuda, M.; Nakasone, T.; Nakamura, Y.; Okano, S.; Kudaka, J.; et al. Transmission of SARS-CoV-2 during a 2-h domestic flight to Okinawa, Japan, March 2020. Influenza Other Respir. Viruses. 2022, 16, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Chong, A.; Lasternas, B.; Peck, T.G.; Tham, K.W. Quantifying the effectiveness of desk dividers in reducing droplet and airborne virus transmission. Indoor Air 2021, 32, e129520. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Xi, C.; Wang, J.; Feng, Z.; Nasiri, F.; Cao, S.-J.; Haghighat, F. Mitigating COVID-19 infection disease transmission in indoor environment using physical barriers. Sustain. Cities Soc. 2021, 74, 103175. [Google Scholar] [CrossRef] [PubMed]
- Lessler, J.; Grabowski, M.K.; Grantz, K.H.; Badillo-Goicoechea, E.; Metcalf, C.J.E.; Lupton-Smith, C.; Azman, A.S.; Stuart, E.A. Household COVID-19 risk and in-person schooling. Science 2021, 372, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Ogata, M.; Tanabe, S.; Hayashi, M.; Kagi, N. Aerosol Shielding Effect by Partitions, HP of the Architectural Institute of Japan. Available online: http://www.collaborate.wind.t-kougei.ac.jp/document/JURC_211028.pdf (accessed on 1 October 2022). (In Japanese).
- Available online: https://www.mhlw.go.jp/content/000851077.pdf (accessed on 1 October 2022). (In Japanese).
- Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (accessed on 1 October 2022).
- Bourouiba, L. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential implications for reducing transmission of COVID-19. JAMA 2020, 323, 1837–1838. [Google Scholar] [CrossRef] [PubMed]
- Rosti, M.E.; Olivieri, S.; Cavaiola, M.; Seminara, A.; Mazzino, A. Fluid dynamics of COVID-19 airborne infection suggests urgent data for a scientific design of social distancing. Sci. Rep. 2020, 10, 22426. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, J. Dose-response Relation Deduced for Coronaviruses From Coronavirus Disease 2019, Severe Acute Respiratory Syndrome, and Middle East Respiratory Syndrome: Meta-analysis Results and its Application for Infection Risk Assessment of Aerosol Transmission. Clin. Infect. Dis. 2020, 73, e241–e245. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.G.; Ibrahim, A.M. Indoor Air Changes and Potential Implications for SARS-CoV-2 Transmission. JAMA 2021, 325, 2112–2113. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Kobayashi, K.; Kim, H.; Kaihara, N. The state of the indoor air environment in buildings and related tasks in Japan. J. Natl. Public Health 2020, 69, 63–71. Available online: https://www.niph.go.jp/journal/data/69-1/202069010008.pdf (accessed on 1 October 2022). (In Japanese).
- WHO. Roadmap to Improve and Ensure Good Indoor Ventilation in the Context of COVID-19. Available online: https://www.who.int/publications/i/item/9789240021280 (accessed on 1 October 2022).



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hayashi, M.; Yanagi, U.; Honma, Y.; Yamamoto, Y.; Ogata, M.; Kikuta, K.; Kagi, N.; Tanabe, S.-i. Ventilation Methods against Indoor Aerosol Infection of COVID-19 in Japan. Atmosphere 2023, 14, 150. https://doi.org/10.3390/atmos14010150
Hayashi M, Yanagi U, Honma Y, Yamamoto Y, Ogata M, Kikuta K, Kagi N, Tanabe S-i. Ventilation Methods against Indoor Aerosol Infection of COVID-19 in Japan. Atmosphere. 2023; 14(1):150. https://doi.org/10.3390/atmos14010150
Chicago/Turabian StyleHayashi, Motoya, U Yanagi, Yoshinori Honma, Yoshihide Yamamoto, Masayuki Ogata, Koki Kikuta, Naoki Kagi, and Shin-ichi Tanabe. 2023. "Ventilation Methods against Indoor Aerosol Infection of COVID-19 in Japan" Atmosphere 14, no. 1: 150. https://doi.org/10.3390/atmos14010150
APA StyleHayashi, M., Yanagi, U., Honma, Y., Yamamoto, Y., Ogata, M., Kikuta, K., Kagi, N., & Tanabe, S.-i. (2023). Ventilation Methods against Indoor Aerosol Infection of COVID-19 in Japan. Atmosphere, 14(1), 150. https://doi.org/10.3390/atmos14010150





