Abstract
The importance of effective ventilation as one of the measures against COVID-19 is widely recognized worldwide. In Japan, at the early stage of the pandemic, in March 2020, an official announcement was made about basic ventilation measures against COVID-19. WHO also used the term “long-range aerosol or long-range airborne transmission” for the first time in December 2021. Based on the aerosol infection control measures before 2021 by the Japanese government, we conducted experiments on methods related to partition placement as an element of effective ventilation methods. In July 2022, the governmental subcommittee on Novel Coronavirus Disease Control provided an emergent proposal about effective ventilation methods to prevent two types of aerosol infection; infection by large aerosol on the air current and infection by small floating aerosol diffusion in a room. They also showed the way of setting droplet prevention partitions, which do not block off ventilation based on this investigation’s results.
1. Introduction
The importance of effective ventilation as one of the measures against COVID-19 is widely recognized in the world now. In Japan, at the early stage of the pandemic, in March 2020, an official announcement was made about basic ventilation measures against COVID-19. However, its infection system in poorly-ventilated indoor spaces has not yet been made clear, and it is quite difficult to show the required ventilation rates or air flow rates to prevent infection. In July 2022, the governmental subcommittee on Novel Coronavirus Disease Control provided an emergent proposal about effective ventilation methods to prevent aerosol infection. This report shows the content of this proposal and the investigation’s results used as a basis for the proposal.
2. Materials and Methods
2.1. Ventilation Measures against COVID-19 in Japan
Since January 2020, COVID-19 outbreaks have occurred in Japan, and pandemic waves have been repeated. At the first stage of the pandemic, a person was assumed to be infected with COVID-19 through contact with the virus (from fingers to mouth, nose, or eyes, etc.) or breathing in droplets containing the virus, and its infection risk was not thought to be high in daily life. However, after the detailed investigation of early outbreak cases, an aerosol containing virus in the air is supposed to be a possible infection source. At the Ministry of Health, Labour and Welfare’s Expert Meeting on Novel Coronavirus Infectious Disease Control on 9 March 2020, “A View on Novel Coronavirus Infectious Disease Control” was announced [1]. Subsequently, on 18 March, the Prime Minister’s Office, together with the Ministry of Health, Labour and Welfare (MHLW), published a leaflet titled “Let’s Avoid These Three Conditions When We Go Out!” [2], according to which closed spaces with poor ventilation, crowded places, and close contact are to be avoided. They already announced the importance of ventilation at this stage. This is the well-known “3Cs”. The Society of Heating, Air-Conditioning and Sanitary Engineers of Japan (SHASE) and Architectural Institute of Japan (AIJ) posted “Role of ventilation in the control of the COVID-19 infection: Emergency presidential discourse on 23 March 2020 [3]. On 30 March 2020, MHLW first posed the required ventilation rate in commercial facilities [4]. The Japanese government concluded that a closed and poorly-ventilated indoor space is one of the outbreak factors and that enough ventilation is necessary [5,6,7]. The outlines of the detailed investigation papers on ventilation measures are summarized.
2.2. Way of Setting Partitions Considering Ventilation Effectiveness
2.2.1. Experimental Setup
We experimented to confirm the aerosol shielding effect of the desk-top partitions. The experiment was conducted by arranging island-shaped desks for four people in an artificial climate chamber (Figure 1) and measuring how the aerosol concentration at each point changed at various partition shapes. Here, a multi-fan generated an indoor airflow of 0.13 m/s. By generating such an airflow, we thought it would be possible to evaluate a situation where the indoor airflow was below the quiescent airflow (0.15 m/s) and reproduce the situation on the downwind side, where the risk of diffusion is high. Figure 2 shows the experimental view of the tabletop partition experiment. The aerosol concentrations were measured in the respiratory area (No. 2 to 5) and near the ceiling (No. 6) under the following conditions: no partition, single-sided partition, two-sided partition, and three-sided partition. Figure 3 shows three types of partition used in this experiment: a “single-sided partition” installed parallel to the wind direction, a “two-sided partition” that surrounds every person in two directions, and a “three-sided partition” that surrounds every person in three directions. For the aerosol source, we used a cough simulator [8]. A simulated cough was ejected in the form of compressed air, and an aqueous solution of water, sodium chloride, and glycerol were used as artificial saliva. The average droplet mass and exhaled air volume were 11.3 mg and 0.97 L, respectively. The cough air temperature was heated to 32 °C using a heater. Also, an experiment was conducted under the condition that a nonwoven fabric mask was attached to the cough simulator. Indoor temperature and humidity in the climate chamber were 26 °C and 50%RH, respectively. Measurements were taken for 10 min after 5 coughs were generated at 10-s intervals by a cough simulator. Measurements were performed once in each case.
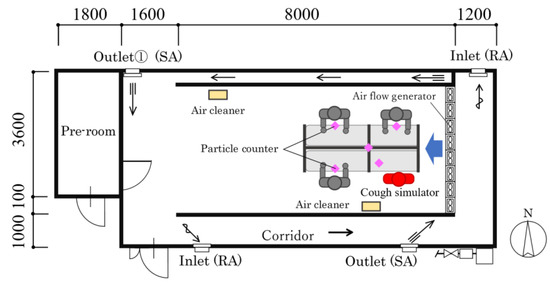
Figure 1.
Plan of the artificial climate chamber with an airflow generator.
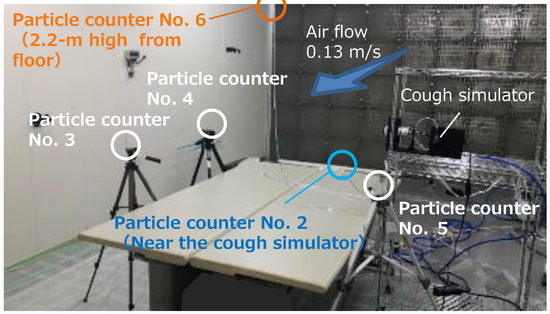
Figure 2.
Experimental view of the tabletop partition experiment.
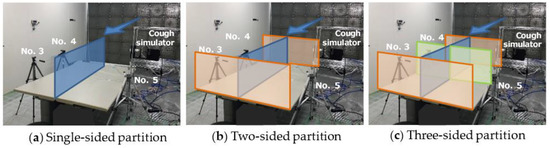
Figure 3.
Partition installation conditions.
Figure 4 shows the particle size distribution of a single cough generated from a cough simulator. In order to identify the particle size distribution, aerosol concentrations within the chamber with an air volume of 12 m3 were measured by a particle counter and particle size distribution was expressed as a ratio of the total number of particles 5 min after it was generated from the cough simulator.
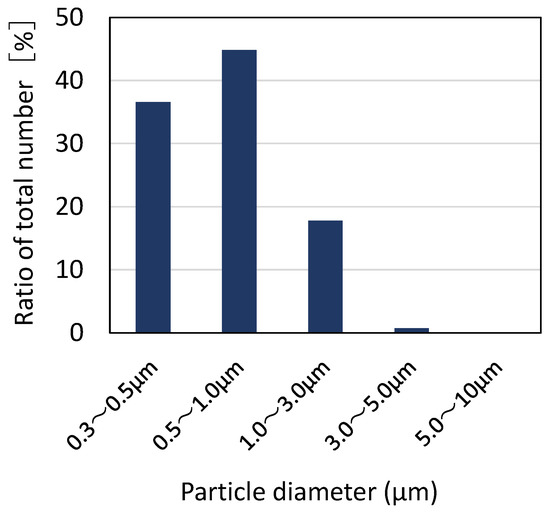
Figure 4.
Particle size distribution generated from cough simulator.
2.2.2. Evaluation Method of Experimental Results
To evaluate the aerosol shielding effect of the desk-top partitions, we calculated the ratio of the aerosol inhalation amount for 10 min to generated aerosol at each measurement point (No. 2–6). The inhalation quantity was based on the assumption that the volumetric human breathing rate is 0.5 L × 15 times/min. The amount of aerosol inhaled for 10 min was evaluated using the particle counter after five coughs with a cough simulator. To confirm the amount of aerosol generated during the experiment, we measured the aerosol concentration (particle size of 0.3–3.0 μm) when coughing five times in a vinyl chamber of a specific volume. As a result, the amount of aerosol generated was predicted to be 3.0 × 109 counts.
2.3. Effective Ventilation Methods in an Emergent Proposal by Subcommittee on Novel Coronavirus Disease Control (14 July 2022)
The effective ventilation methods to prevent aerosol infection were investigated using these study results. The ventilation methods were used for the emergent proposal by the governmental subcommittee on Novel Coronavirus Disease Control in about July 2022.
3. Results
3.1. Ventilation Measures against COVID-19 in Japan
3.1.1. Effective Ventilation Methods in “Closed and Poorly-Ventilated Indoor Spaces” in Commercial Facilities, etc. (30 March 2020) [4]
In “the view on the measures against COVID-19” (published on 9 and 19 March 2020) of the expert meeting against COVID-19, they showed three conditions common in the spaces where outbreaks occurred. Based on this view, the emergency headquarters of the Ministry of Health, Labour and Welfare showed recommended ventilation methods to improve the ventilation in “closed and poorly-ventilated spaces” in commercial facilities many people use.
As for mechanical ventilation systems, the required ventilation rates in the Act on Maintenance of Sanitation in Buildings (30 m3 per hour per person) should be assured in every room. If the ventilation rates of a space are lower, the number of persons in the space should be reduced, and the required ventilation rates per person should be assured.
As for opening windows, ventilation times should be twice or more per hour (opening a window wide for several minutes once or more per half an hour). If two or more windows are in a space, windows facing each other should be open to make an air current. If there is only one window, both the window and the door should be open.
3.1.2. Advisory Board on COVID-19 Control of the Ministry of Health, Labour and Welfare (30 July 2020)
At the first stage of the COVID-19 pandemic, its infection route was assumed to be through “droplets containing virus” and “contact with virus”. However, in Japan, around the time when the basic policies toward COVID-19 were adopted in February, other infection routes were pointed out and measures were taken. Recently “micro-droplet infection” has been recognized in the world. On the other hand, while walking outside, shopping or dining at a shop or a restaurant where infection control measures are taken, or commuting on well-ventilated trains, the possibility of “micro-droplet infection” is assumed to be weak.
3.1.3. Measures against COVID-19 Concerning Summer Indoor Environment in Japan (May 2020) [9]
This report summarizes ventilation measures for summer air-conditioning based on the latest evidence collected concerning COVID-19. Some recommendations concerning air-conditioning and ventilation are shown for various situations because it is difficult to specify standard values of ventilation rates etc. from the evidence presently available. Furthermore, the following measures are recommended.
- [In every indoor space]
- Enough ventilation is necessary to prevent the infection of COVID-19.
- Opening windows is an effective ventilation method, and it is desirable to open them wider and for a longer time.
- In summer, air-conditioning is essential for good health, such as heat stroke prevention. (In winter, heating is essential for good health, such as heat shock.)
- General air-conditioners do not function as ventilators, so mechanical ventilation or opening windows is necessary.
- When windows are open, it is necessary to prevent animals or insect pests from coming in.
- [In case an air-conditioner and a ventilation system are equipped]
- 6.
- It is necessary to ensure the operation of designed ventilation rates by maintaining and inspecting the equipment.
- 7.
- It is recommended to control the number of people in a room, to ensure the ventilation rate for a person and shorten people’s stay in a room.
- 8.
- Measures such as the improvement of ventilation effects through the development of air-conditioners and ventilation systems, and the use of air cleaners and humidifiers in winter, have to be discussed considering the characteristics of each building, that is, what it is used for, how often it is used, or what kind of air-conditioner or ventilation system it has.
3.1.4. Effective Ventilation Methods in “Closed and Poorly-Ventilated Indoor Spaces” in Winter (27 November 2020) [10]
The headquarters of the Ministry of Health, Labour and Welfare suggested the recommended methods to achieve both effective ventilation in “closed and poorly-ventilated indoor spaces” and the prevention of the negative influence of lower indoor temperature on health.
- (1)
- In commercial facilities, etc., where mechanical ventilation systems are installed, the required ventilation rates (30 m3 per hour per person) should be kept, and room temperature and relative humidity should be kept at 18 °C or higher and 40% or higher, with the adjustment of the rates of fresh air supply by the mechanical ventilation system.
- (2)
- In commercial facilities, etc., without mechanical ventilation facilities or in commercial facilities, etc. in which ventilation rates are not enough with their mechanical ventilation facilities, on condition that room temperature and humidity should be kept at 18 °C or higher and 40% or higher, a window should be open all the time while heating systems are on. The use of humidifiers is also effective.
- (3)
- In case the indoor temperature and relative humidity are under 18 °C and 40% while windows are open, the use of portable air cleaners is effective in compensating for the lack of ventilation. In such cases, portable air cleaners of which the filtration type is HEPA (High Efficiency Particulate Air) and of which airflow rates are about 5 m3 per minute or more should be used, and air cleaners should be settled within 10 m2 around people in the room, and the wind direction of the air cleaner should correspond to the direction of fresh air supply to make an air current.
- (4)
- To confirm the ventilation of a room, CO2 concentration should always be measured, and the value should be under 1000 ppm. However, when an air cleaner is used while a window is open, the measurement of CO2 concentration does not reflect the effect of the air cleaner, so it cannot be an appropriate evaluation.
3.1.5. The Infection Routes of SARS-CoV-2 by the National Institute of Infectious Diseases (Published on 28 March 2022) [11]
SARS-CoV-2 infects a person through the exposure of an aerosol containing infectious virus emitted from the nose or mouth of an infected person. The main three infection routes are:
- (1)
- breathing in an aerosol containing virus floating in the air (aerosol infection)
- (2)
- the attachment of droplets containing the virus on bare mucous membranes such as mouths, noses, or eyes (droplet infection)
- (3)
- fingers touching bare mucous membranes after touching droplets containing the virus or the surface of things with a virus (contact infection)
The shorter the distance between a person and an infected person (within about 1–2 m), the higher the infection risk becomes and the longer the distance (more than about 1–2 m), the lower the risk becomes [12,13]. Especially in poorly-ventilated or closed spaces, the time and the distance in which particles containing the virus are emitted by an infected person become long. The infection cases in such environments have been reported nationally and globally, even when a person stays away from an infected person [14,15,16,17].
3.2. Way of Setting Partitions Considering Ventilation Effectiveness
Physical barriers are thought to shield the relatively large respiratory droplets infected persons produce and prevent droplet transmission. Therefore, they have been actively installed since the beginning of the outbreak, especially in restaurants and elderly care facilities where it is challenging to install masks. Even now, partitions are recommended for elderly facilities where it is challenging to wear masks at all times, and it is difficult to avoid the three Cs—closed spaces, crowded places, and close-contact settings of the facility. However, there have been cases where excessive installation of partitions has resulted in the obstruction of ventilation in the room. There is also a concern that partitions may act as soundproofing, resulting in louder conversations, which may increase the generation of respiratory aerosol particles.
Li et al. [18] evaluated the impact of desk partitions on transmission by coughing in an experiment and reported that the risk of exposure to an infected person sitting opposite an infected person who is the source of the outbreak is reduced. In contrast, the aerosol reflection by the partition increases the risk of exposure to those sitting next to the infected person. Ren et al. [19] investigated the effect of desk partition height on the dispersion of aerosol particles in open offices by numerical simulation. They found that a height of at least 40 cm from the desk surface is recommended to prevent aerosol propagation, and within 4 m of an exhaust vent, at 60 cm. However, the physical barrier is ineffective at distances greater than 4 m from the exhaust vent. In addition, extensive online survey data in the US reported that the installation of desk shields is associated with an increased risk in face-to-face schooling settings [20]. However, these reports are the results of experiments and analyses under limited conditions or statistical analyses in which causal relationships are unclear. Universal conclusions need to be drawn about the impact of desk partitions on aerosol transmission in indoor environments after examining their impact on exposure risk.
Therefore, it can be said that it is necessary to sort out the critical points of installing partitions from the perspective of preventing aerosol infection. In particular, the effectiveness of partitions in buildings with adequate basic infection control measures, such as masks and ventilation, must be re-examined. Therefore, the author’s research group experimented on the relationship between partitions and aerosol exposure at the Wind Engineering Research Center of Tokyo Polytechnic University [21]. The results of the experiment will be presented in the next section.
Figure 5 shows the results of an aerosol visualization experiment when a cough simulator against a partition generated a cough. The partition is 60 cm above the tabletop, but after the aerosol hit the partition, a portion of the aerosol rose and overcame the partition.
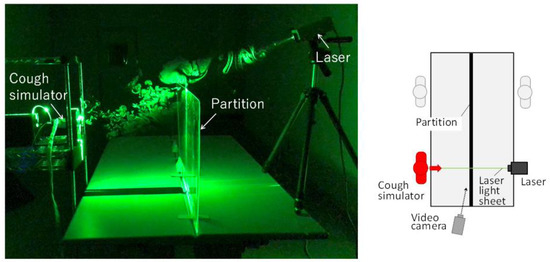
Figure 5.
Aerosol overcoming partitions.
A summary of the experimental results regarding the presence or absence of masks on the cough simulator and the shape of the partition is shown in Figure 6 and Figure 7. Comparing the results with and without masks, it can be seen that masks significantly reduce exposure to aerosol particles. In addition, in the case of the three-sided partition, the partition itself blocked the airflow in the room so that highly concentrated aerosols tended to stagnate around the source and took time to diffuse. Incidentally, the comparison of measurement results between cases shown in these figures uses a single measurement result.
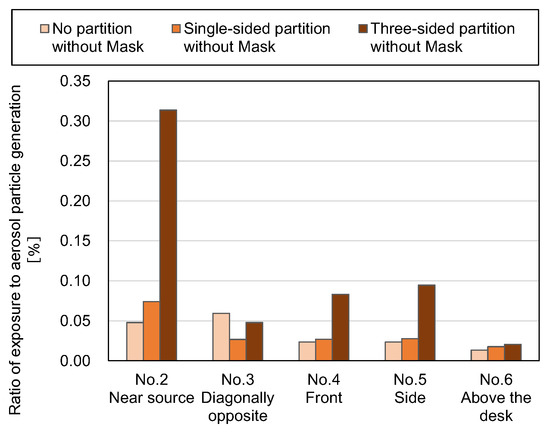
Figure 6.
Effect of partition shape (without mask) [21].
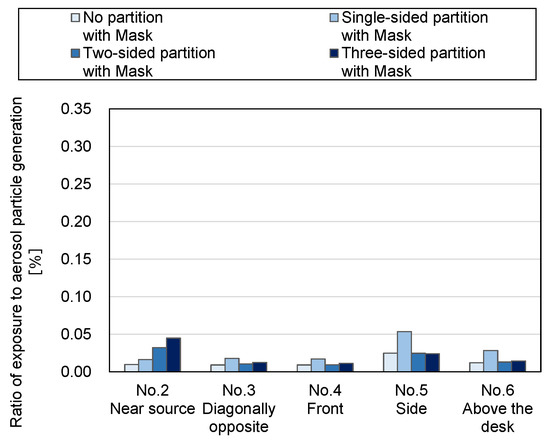
Figure 7.
Effect of partition shape (with mask) [21].
These experiments suggest that it may be difficult to block the infection route by aerosols only by installing partitions since aerosols flow with indoor air. It is known that aerosols with a particle size of 0.3 to 3.0 μm evaluated in the experiments have a smaller reduction effect due to deposition than droplets with a larger particle size, but even with regard to deposition, aerosols directly impact the partition surface because they follow the airflow generated on the partition surface and move with it. It is expected that aerosols would be small and that the number of aerosols reduced by deposition on the partition surface would not be expected. As a result, the generated aerosols will continue to drift around the partition even after impact. Therefore, it can be said that the aerosol must eventually be quickly expelled by ventilation. In offices where proper masking and social distance are required for all employees, the emphasis should be placed on improving the ventilation efficiency of the entire room and avoiding obstruction or stagnation of the room airflow due to excessive partitions.
3.3. Effective Ventilation Methods in an Emergent Proposal by Subcommittee on Novel Coronavirus Disease Control (14 July 2022)
In July 2022, the governmental subcommittee on Novel Coronavirus Disease Control provided an emergent proposal about effective ventilation methods to prevent two types of aerosol infection; infection by large aerosol on the air current and infection by small floating aerosol diffusion in a room. They also showed the way of setting droplet prevention partitions, which do not block off ventilation based on this investigation results.
3.3.1. Measures against the Two Types of Aerosol Infection (Figure 8)
In ventilation measures before this proposal, assuring enough ventilation rates is required to exhaust aerosol from indoor spaces. In this proposal, further effective ventilation methods were recommended, considering the following characteristics of aerosol infection.
The size of aerosol containing viruses emitted from an infected person ranges from less than 1 μm to more than 100 μm. Large aerosols fall by gravity, but small aerosols float in the air. Water in the aerosol evaporates in a few seconds and the aerosol becomes smaller and lighter. Aerosol emitted with a cough or a sneeze goes fast in front. However, when conversing in a low voice or when a speaker wears a facial mask, aerosol floats along with the indoor current. Especially in the weak indoor air current, it floats upward with the ascending current from a person’s heat. However, in most cases, the aerosol moves along with the air current from air-conditioners or ventilation facilities.
Therefore, when a person is close to an infected person’s expiration, not only small aerosols but also large aerosols are transmitted to another person. On the other hand, when the distance between persons is far, large aerosols fall to the floor and small aerosol concentration becomes weakened while it is diffusing. However, in poorly-ventilated indoor spaces, diffused aerosols accumulate and aerosol concentration becomes high regardless of the distance. Considering this movement of aerosols, it is necessary to take measures against both A: infection close to an infected person’s expiration and B: infection by aerosol diffusion filled in poorly-ventilated indoor spaces.
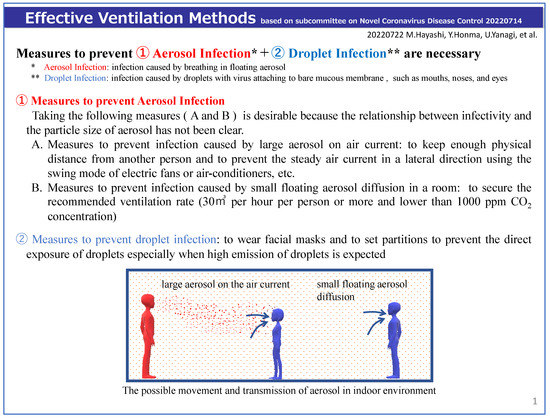
Figure 8.
Measures to prevent two types of aerosol movement.
3.3.2. Effective Ventilation Measures against Aerosol Infection (Figure 9 and Figure 10)
As an effective method to prevent aerosol infection A, air current in a room should be taken into consideration. As an effective method concerning B, it is necessary to ensure enough ventilation rates. Effective control of indoor aerosol concentration as well as infection risk control close to an infected person’s expiration is possible by exhausting air from the area where much aerosol is emitted and taking fresh air in from the opposite side of the room. To make this air current, indoor air should be exhausted with a fan in the kitchen or a mechanical fan, and windows or doors on the opposite side should be open. If it is impossible to make the air current, air cleaners should be used to collect aerosols.
It is necessary to pay attention to the change of the indoor environment for the worse when outdoor air flows into a room in summer and winter, which has been repeatedly pointed out so far. It is necessary to adjust heating or air-conditioning while monitoring indoor temperature, humidity, and CO2 concentration.
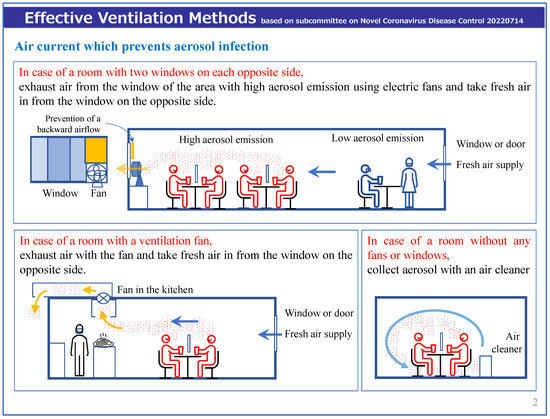
Figure 9.
Effective ventilation methods against two aerosol infection types.
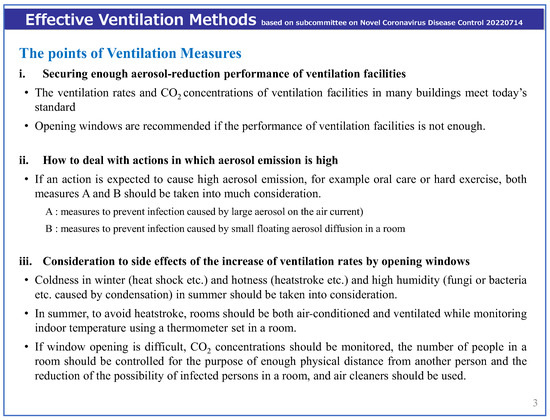
Figure 10.
The points of effective ventilation measures.
3.3.3. Measures against Droplet Infection without Any Disturbance of Air Current (Figure 11)
To prevent droplets, a kind of barrier between persons (partitions or curtains, etc.) is necessary, especially when facial masks are not available. However, since tall partitions or curtains from the ceiling block air current, aerosol concentration may become high. To avoid air stagnation, lower partitions should be set in a parallel direction to the air current.
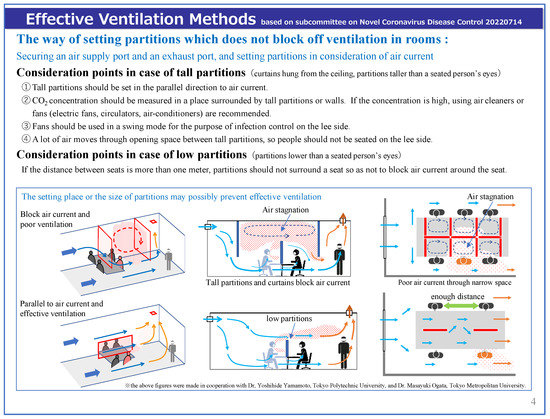
Figure 11.
The way of setting partitions which does not block off ventilation.
3.3.4. The Matters That Require Attention Considering the Characteristics of Facilities
Recommended air current in facilities for the elderly was suggested as follows.
- (1)
- Desirable air current is “a patient ⇒ a fan (circulator or mechanical fan) ⇒ a vent (exhaust fan or window + fan)”. A fan should be set on the lee side of a patient’s breath, and no one should be away from the space between a patient and a fan. In the case of a patient’s care, a nursing person (wearing a facial mask) ⇒ a patient ⇒ a fan ⇒ a vent (exhaust fan or window) (Figure 3)
- (2)
- When nursing a patient who is not wearing a facial mask, for example, giving a patient a meal, bathing a patient, or cleaning a patient’s mouth, etc., a nursing person should wear both a face shield and a facial mask to prevent droplet infection and the space should be well ventilated in case of much aerosol emission.
- (3)
- In order to get enough air current, the mechanical power and location of fans should be adjusted (The direction of the air current should be confirmed using a smoke tester, smoke from an incense stick, a piece of tissue paper, or thread).
- (4)
- CO2 concentration monitors should be used in locker rooms, dressing rooms, staff rooms, etc. to know the state of ventilation in each room and to limit the number of people in the room if necessary.
4. Discussion
Infections occur when the following three elements of infection are aligned: infected person, susceptible host, infection route, and exposure to a certain load of pathogens. Therefore, the basis for infectious disease measures is to remove any one of these elements. An engineering strategy is a measure of the infection route.
Over the past two years, official views on the transmission route of COVID-19 have changed. At the beginning of the COVID-19 pandemic, the Japanese Ministry of Health, Labour and Welfare (MHLW) and WHO clearly stated that COVID-19 was transmitted through contact and droplet transmission. About two years later, the MHLW indicated that aerosol transmission is one of the major transmission routes in its “COVID-19 Medical Treatment Guide, Version 6.0” published on 2 November 2021 [22]. WHO also used the term long-range aerosol or long-range airborne transmission for the first time on 23 December 2021 [23]. There is now a consensus that aerosol transmission is one of the major transmission routes for COVID-19.
Many cases have demonstrated that COVID-19 is transmitted by close contact or exposure to droplets and aerosol containing pathogens because droplets released from coughing, sneezing, etc. evaporate in the air to form various particle sizes and are diffused in the room by indoor airflow. There is a large quantity of viable SARS-CoV-2 around infected individuals, thus increasing the risk of infection. Furthermore, as viable SARS-CoV-2 spreads in indoor spaces, its concentration decreases as it becomes diluted through ventilation or filtration, and its infection risk becomes relatively low. However, the concentration of viable SARS-CoV-2 released from other individuals can become high because of cloud formation owing to indoor airflow properties [24,25]. In these cases, the risk of infection becomes high even when infected individuals are far away from other individuals. Therefore, the risk of infection owing to droplets near the infected individual is generally high when no measures have been implemented; however, there is a risk of infection in some cases, even when individuals are far away from infected individuals. This can be explained by the dose-response relationship. Zhang et al. investigated the human dose-response relationship based on infection risk data obtained from animal experiments and meta-analysis using mice and virus shedding in human exhalation. They showed that the median infection risk via aerosol transmission with 1-h exposure (10−6 to 10−4) was significantly lower than the risk caused by close contact (10−1) in a room with an area of 10–400 m2 with one infected individual in it and with a typical ventilation rate of 1 air change per hour [26]. Allen et al. recommended 4–6 ACH (Air changes per hour) for the equivalent ventilation rate by the ventilation and/or filtration method [27]. The concentration of indoor pathogens will be low if a sufficient equivalent ventilation rate is provided through ventilation and/or filtration, and the infection risk will decrease as a result.
There are risks of infection due to aerosol inhalation in the following two situations: (1) momentary direct exposure to high-concentration aerosols due to cough or vocalization, and (2) the increase of respiratory air concentration due to poor ventilation efficiency. In addition, the longer a person stays in the room, the greater the amount of inhalation becomes. Regarding (1), masks and partitions have been useful as the main countermeasures. Moreover, regarding (2), it is necessary to confirm that they are also effective countermeasures. Experimental results in this study show that wearing a mask significantly reduced the amount of aerosol generation in the room. However, small aerosol particles leak through the space between the mask and the face and drift around the generation source. In addition, in the experimental case of the box partition, the aerosol concentration around the source increased because the partition blocked the indoor airflow, and the aerosol tended to take time to dilute. These results mean that since aerosols move along the path of indoor airflow, it is impossible to completely block the infection route of aerosol particles by installing partitions alone. Therefore, adequate ventilation is necessary in addition to partitions to reduce the risk of aerosol infection by aerosols. Furthermore, for high ventilation efficiency, partitions should be installed in a way that does not cause air stagnation in the room.
In Japan, the countermeasures against COVID-19 have been carried out since the early stage of the pandemic. The first countermeasures about “avoidance of three conditions” were decided using the survey results on cluster cases in buildings and ships with these three conditions: a closed and poorly-ventilated space, a crowded place with many people, and a scenario where people stay close while talking or vocalization. However, it was difficult to show the specific figures for infection control. In order to avoid poorly-ventilated spaces, the Japanese government investigated the past standards and the state of ventilation performance in Japan. Health centers have inspected buildings according to the law for environmental health in buildings (LEHB) since 1970. The standard value of indoor carbon dioxide concentrations is 1000 ppm, but the nonconformity rate has increased since 1999 and reached 28 % in 2019 [28]. Therefore, it is difficult to keep a high ventilation rate in all buildings. The Japanese government requires every building owner to keep 30 m3 per hour per person as the minimum ventilation rate. They recommend that if the ventilation rates are lower than the value, the number of people should be reduced in a room and carbon dioxide meters to monitor ventilation should also be set. However, these countermeasures were immediately decided to control the pandemic. The reexamination of the evidence data is always necessary.
In July 2022, Subcommittee on Novel Coronavirus Disease Control Effective showed ventilation methods based on the latest findings. It was still difficult to evaluate the infection risk by large aerosols and small aerosols. Therefore, they required consideration of both indoor air currents and keeping ventilation rates. These ventilation strategies are thought to be essentially the same as those in the roadmap on ventilation by WHO [29].
Japanese researchers have been investigating the transmission routes for COVID-19 considering the survey results of cluster cases and the latest domestic and overseas findings on infections since the early stage of the pandemic. In the latest proposal, the Japanese government indicated “aerosol infection”, as an infection route in which infectivity is lower than airborne infection. However, it cannot be ignored that there were multiple transmission routes at the same time in many cluster cases. Because it is the most difficult to identify an infection route by floating viruses among the multiple routes, this route may have been neglected. Therefore, it is still very important to study the infectivity under an indoor air environment.
5. Conclusions
This paper shows ventilation measures against COVID-19 before 2022 in Japan and the investigation results on aerosol transmission and the ventilation characteristics in rooms using droplet prevention partitions. In the last part of this paper, the contents of “effective ventilation methods in an emergent proposal by Subcommittee on Novel Coronavirus Disease Control on 14 July 2022” is introduced. This proposal is based on the latest findings on aerosol transmission with SARS-CoV-2 and the investigation results on setting partitions considering ventilation effectiveness.
In the early stage of the pandemic, the required ventilation rate was assumed to be 30 m3 per hour per person, based on the outbreak cases of COVID-19 in Japan. However, it has been difficult to clarify the required ventilation rate for infection control. Therefore, opening windows or using air cleaners was also recommended, along with mechanical ventilation. In 2021, many research institutes, including WHO, showed the importance of ventilation strategies to control aerosol infection of COVID-19. Since the early stage of the pandemic, partitions have been used in most restaurants, offices, and so on, to prevent droplet infection in Japan. However, in some cases, the partitions block airflow and the aerosol concentrations become high in the space surrounded by partitions, where the infection risk is higher.
In July 2022, the Japanese government showed that it is necessary to prevent two types of aerosol infection. The airflow must be controlled to prevent infection by large aerosols in the air. The ventilation rate must be kept enough to prevent infection by small floating aerosol diffusion in rooms. They also showed the way of setting partitions for droplet prevention which does not block off ventilation based on the latest investigation results.
Effective ventilation methods to control aerosol infection will contribute to infection control in the building. It will be more important to make standards on indoor airflow and ventilation to control indoor aerosol infection according to the infectivity and toxicity of viruses.
Author Contributions
Conceptualization, M.H.; methodology, U.Y.; validation, Y.H.; investigation, Y.Y., M.O., N.K. and K.K.; writing, M.H., U.Y., Y.Y. and M.O.; original draft preparation, M.H., U.Y., Y.Y, M.O. and K.K.; writing-review and editing, N.K., S.-i.T. and K.K.; visualization, M.H., U.Y., Y.Y. and M.O.; supervision, M.H., U.Y. and S.-i.T.; funding acquisition, M.H. and U.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by MHLW “Research on Emerging and Re-emerging Infectious Diseases and Immunization” Program Grant Number JPMH19HA1003.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author and the first author.
Acknowledgments
Many thanks to S the committee members of the Subcommittee on Novel Coronavirus Disease Control for their guidance on ventilation strategies for infections. Many thanks to Suguru Mori, Shuang Yan, Kenichi Kobayashi, Michiko Bando, Kentaro Yamaguchi, Tomoaki Okuda, Takeshi Muto, and Consultant Haruo Hashimoto for their comments and suggestions. We are grateful for the comments and suggestions from the reviewers.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Novel Coronavirus Infectious Disease Control Experts Meeting. View on Novel Coronavirus, Infectious Disease Control. 9 March 2020. Available online: https://www.mhlw.go.jp/content/10900000/000606000.pdf (accessed on 23 November 2022). (In Japanese)
- Prime Minister’s Office. Let’s Avoid These Three Conditions When We Go Out! Flyer. Available online: https://www.kantei.go.jp/jp/content/000061234.pdf (accessed on 23 November 2022). (In Japanese)
- The Society of Heating. Air-Conditioning and Sanitary Engineers of Japan (SHASE) and Architectural Institute of Japan (AIJ), Role of Ventilation in the Control of the COVID-19 Infection: Emergency Presidential Discourse. Available online: https://www.aij.or.jp/jpn/databox/2020/20200323_Eng_final.pdf (accessed on 23 November 2022). (In Japanese).
- The Ministry of Health, Labour and Welfare. Reference Data Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ in Commercial Facilities, etc. 30 March 2020. Available online: https://www.mhlw.go.jp/content/10900000/000616069.pdf (accessed on 1 October 2022). (In Japanese)
- The Ministry of Health, Labour and Welfare. Toward the Managers of Commercial Facilities, Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’. 3 April 2020. Available online: https://www.mhlw.go.jp/content/10900000/000618969.pdf (accessed on 1 October 2022). (In Japanese)
- The Ministry of Health, Labour and Welfare. Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ while Avoiding Heatstroke. 17 June 2020. Available online: https://www.mhlw.go.jp/content/10900000/000640913.pdf (accessed on 1 October 2022). (In Japanese)
- The Ministry of Health, Labour and Welfare. Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ in Winter. 27 November 2020. Available online: https://www.mhlw.go.jp/content/000698868.pdf (accessed on 1 October 2022). (In Japanese)
- Ogata, M.; Ichikawa, M.; Tsutsumi, H.; Ariga, T.; Hori, S.; Tanabe, S.-I. Measurement of cough droplet deposition using the cough machine. J. Environ. Eng. (Transactions AIJ) 2018, 83, 57–64. [Google Scholar] [CrossRef]
- Hayashi, M.; Yanagi, U.; Azuma, K.; Kagi, N.; Ogata, M.; Morimoto, S.; Hayama, H.; Mori, T.; Kikuta, K.; Tanabe, S.; et al. Measures against COVID-19 concerning Summer Indoor Environment in Japan. Jpn. Arch. Rev. 2020, 3, 423–434. [Google Scholar] [CrossRef]
- The Ministry of Health, Labour and Welfare. Reference Data Ventilation Methods to Improve ‘Closed and Poorly-Ventilated Indoor Spaces’ in Winter. 27 November 2020. Available online: https://www.mhlw.go.jp/content/10906000/000698849.pdf (accessed on 1 October 2022). (In Japanese)
- National Institute of Infectious Diseases. Infection Routes of SARS-CoV-2. 28 March 2022. Available online: https://www.niid.go.jp/niid/ja/2019-ncov/2484-idsc/11053-covid19-78.html (accessed on 1 October 2022). (In Japanese).
- World Health Organization (WHO). Coronavirus Disease (COVID-19) How Is It Transmitted? 2021. Available online: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted (accessed on 5 November 2022).
- Centers for Disease Control and Prevention (CDC). Scientific Brief: SARS-CoV-2 Transmission. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/sars-cov-2-transmission.html (accessed on 25 October 2022).
- Jang, S.; Han, S.H.; Rhee, J.-Y. Cluster of Coronavirus Disease Associated with Fitness Dance Classes, South Korea. Emerg. Infect. Dis. 2020, 26, 1917–1920. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Sun, W.; Huang, J.; Gamber, M.; Wu, J.; He, G. Indirect Virus Transmission in Cluster of COVID-19 Cases, Wenzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1343–1345. [Google Scholar] [CrossRef] [PubMed]
- Katelaris, A.L.; Wells, J.; Clark, P.; Norton, S.; Rockett, R.; Arnott, A.; Sintchenko, V.; Corbett, S.; Bag, S.K. Epidemiologic Evidence for Airborne Transmission of SARS-CoV-2during Church Singing, Australia, 2020. Emerg Infect Dis. 2021, 27, 1677–1680. [Google Scholar] [CrossRef] [PubMed]
- Toyokawa, T.; Shimada, T.; Hayamizu, T.; Sekizuka, T.; Zukeyama, Y.; Yasuda, M.; Nakasone, T.; Nakamura, Y.; Okano, S.; Kudaka, J.; et al. Transmission of SARS-CoV-2 during a 2-h domestic flight to Okinawa, Japan, March 2020. Influenza Other Respir. Viruses. 2022, 16, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Chong, A.; Lasternas, B.; Peck, T.G.; Tham, K.W. Quantifying the effectiveness of desk dividers in reducing droplet and airborne virus transmission. Indoor Air 2021, 32, e129520. [Google Scholar] [CrossRef] [PubMed]
- Ren, C.; Xi, C.; Wang, J.; Feng, Z.; Nasiri, F.; Cao, S.-J.; Haghighat, F. Mitigating COVID-19 infection disease transmission in indoor environment using physical barriers. Sustain. Cities Soc. 2021, 74, 103175. [Google Scholar] [CrossRef] [PubMed]
- Lessler, J.; Grabowski, M.K.; Grantz, K.H.; Badillo-Goicoechea, E.; Metcalf, C.J.E.; Lupton-Smith, C.; Azman, A.S.; Stuart, E.A. Household COVID-19 risk and in-person schooling. Science 2021, 372, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Ogata, M.; Tanabe, S.; Hayashi, M.; Kagi, N. Aerosol Shielding Effect by Partitions, HP of the Architectural Institute of Japan. Available online: http://www.collaborate.wind.t-kougei.ac.jp/document/JURC_211028.pdf (accessed on 1 October 2022). (In Japanese).
- Available online: https://www.mhlw.go.jp/content/000851077.pdf (accessed on 1 October 2022). (In Japanese).
- Available online: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (accessed on 1 October 2022).
- Bourouiba, L. Turbulent Gas Clouds and Respiratory Pathogen Emissions: Potential implications for reducing transmission of COVID-19. JAMA 2020, 323, 1837–1838. [Google Scholar] [CrossRef] [PubMed]
- Rosti, M.E.; Olivieri, S.; Cavaiola, M.; Seminara, A.; Mazzino, A. Fluid dynamics of COVID-19 airborne infection suggests urgent data for a scientific design of social distancing. Sci. Rep. 2020, 10, 22426. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, J. Dose-response Relation Deduced for Coronaviruses From Coronavirus Disease 2019, Severe Acute Respiratory Syndrome, and Middle East Respiratory Syndrome: Meta-analysis Results and its Application for Infection Risk Assessment of Aerosol Transmission. Clin. Infect. Dis. 2020, 73, e241–e245. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.G.; Ibrahim, A.M. Indoor Air Changes and Potential Implications for SARS-CoV-2 Transmission. JAMA 2021, 325, 2112–2113. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Kobayashi, K.; Kim, H.; Kaihara, N. The state of the indoor air environment in buildings and related tasks in Japan. J. Natl. Public Health 2020, 69, 63–71. Available online: https://www.niph.go.jp/journal/data/69-1/202069010008.pdf (accessed on 1 October 2022). (In Japanese).
- WHO. Roadmap to Improve and Ensure Good Indoor Ventilation in the Context of COVID-19. Available online: https://www.who.int/publications/i/item/9789240021280 (accessed on 1 October 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).