MRSA Colonization in Workers from Different Occupational Environments—A One Health Approach Perspective
Abstract
:1. Introduction
2. Materials and Methods
2.1. Workplaces and Workers Assessed
2.2. Samples Collection
2.3. Staphylococcus Aureus Identification
3. Results
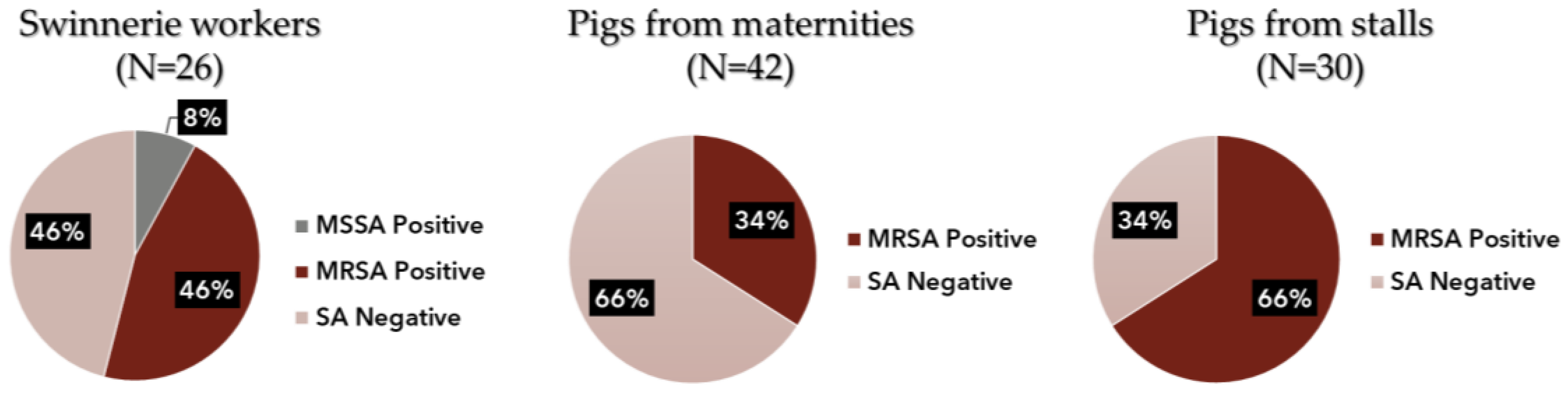
3.1. Swineries
3.2. Veterinary Clinic
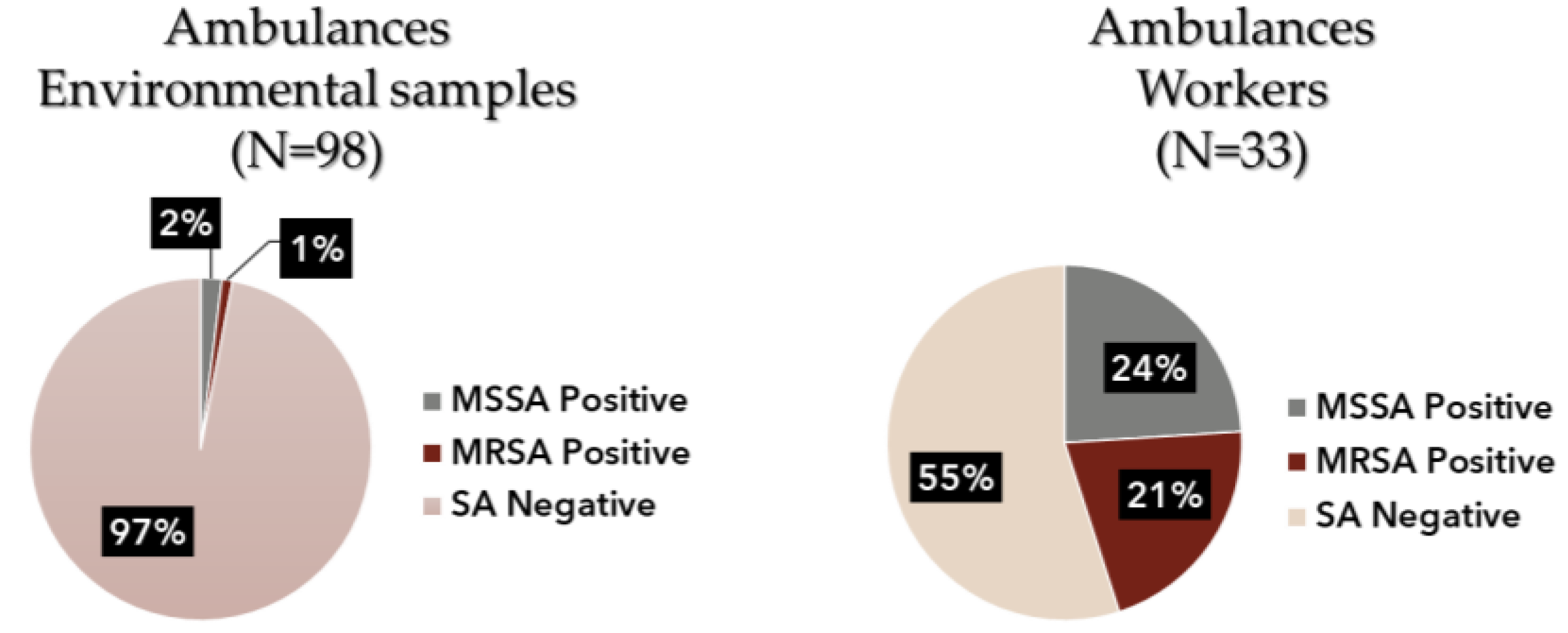
3.3. Ambulances
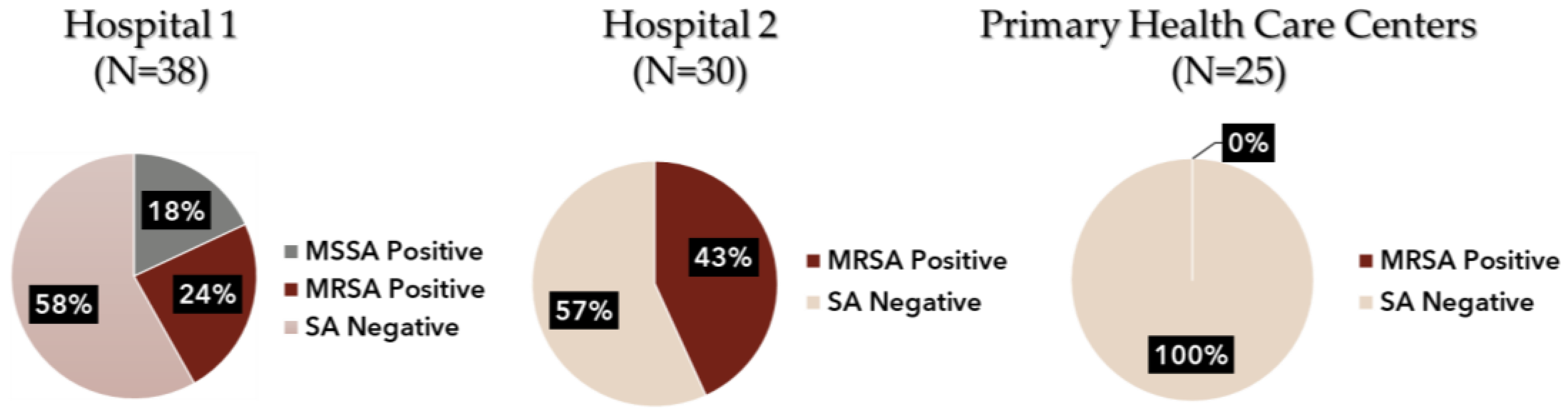
3.4. Healthcare Environment
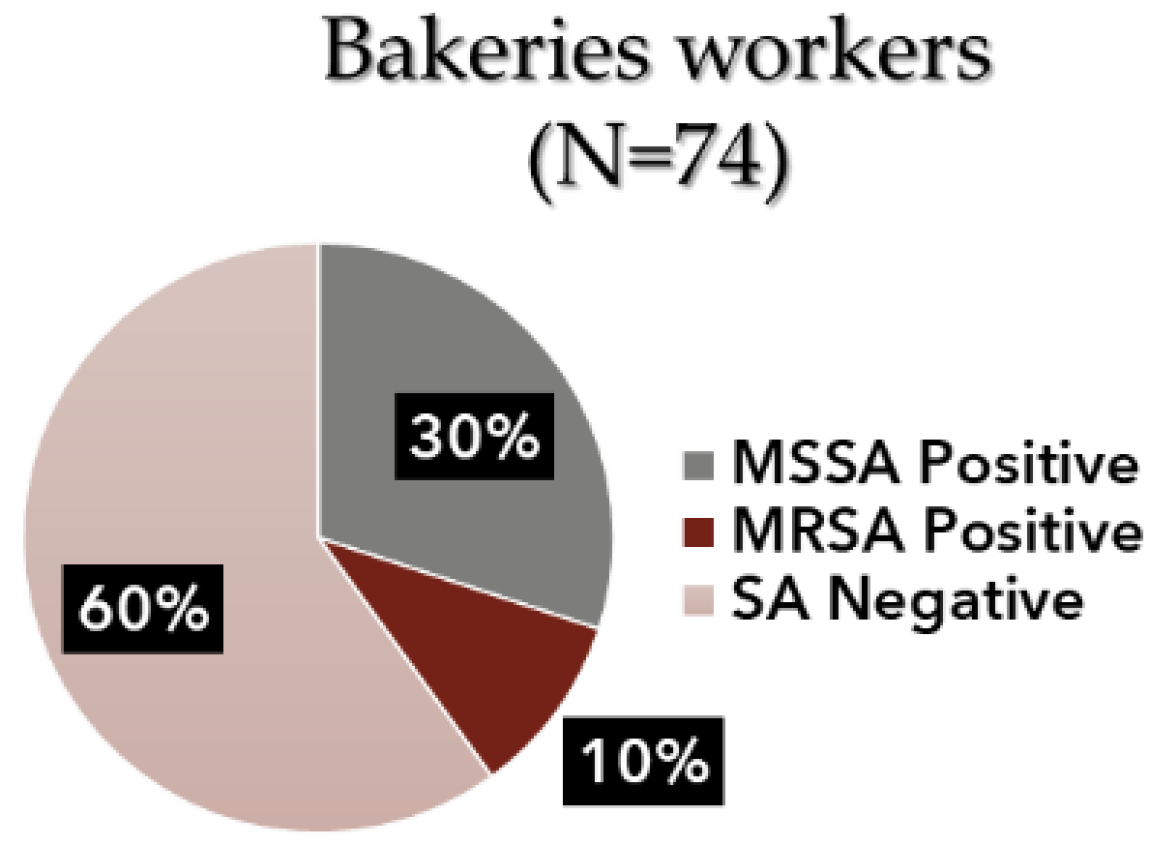
3.5. Bakeries
3.6. Control Group
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lakhundi, S.; Zhang, K. Methicillin-Resistant Staphylococcus aureus: Molecular Characterization, Evolution, and Epidemiology. Clin. Microbiol. Rev. 2018, 31, e00020-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tong, S.Y.C.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G., Jr. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, N.A.; Sharma-Kuinkel, B.K.; Maskarinec, S.A.; Eichenberger, E.M.; Shah, P.P.; Carugati, M.; Holland, T.L.; Fowler, V.G., Jr. Methicillin-resistant Staphylococcus aureus: An overview of basic and clinical research. Nat. Rev. Microbiol. 2019, 17, 203–218. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control Surveillance of Antimicrobial Resistance in Europe—Annual Report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2017; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2018; ISBN 978-2-85653-642-1.
- World Health Organisation WHO. What Is Antibiotic Resistance? Available online: https://sites.wpro.who.int/antibiotic_awareness/?page_id=96 (accessed on 22 January 2019).
- Programa de Prevenção e Controlo de Infeções e de Resistência Aos Antimicrobianos. Direção Geral Saúde 2017, 8, 24.
- Norma No 018/2014, atualizada a 27/04/2015; Prevenção e Controlo de Colonização e Infeção Por Staphylococcus aureus Resistente à Meticilina (MRSA) Nos Hospitais e Unidades de Internamento de Cuidados Continuados Integrados 2015; Direção Geral de Saúde: Lisbon, Portugal, 2015.
- Kinross, P.; Petersen, A.; Skov, R.; Van Hauwermeiren, E.; Pantosti, A.; Laurent, F.; Voss, A.; Kluytmans, J.; Struelens, M.J.; Heuer, O.; et al. Livestock-associated meticillin-resistant Staphylococcus aureus (MRSA) among human MRSA isolates, European Union/European Economic Area countries, 2013. Eurosurveillance 2017, 22, 16-00696. [Google Scholar] [CrossRef] [Green Version]
- European Food Safety Authority (EFSA); European Centre for Disease Prevention and Control (ECDC). The European Union summary report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2017. EFSA J. 2019, 17, e05598. [Google Scholar] [CrossRef]
- Nair, R.; Perencevich, E.N.; Blevins, A.E.; Goto, M.; Nelson, R.E.; Schweizer, M.L. Clinical Effectiveness of Mupirocin for Preventing Staphylococcus aureus Infections in Nonsurgical Settings: A Meta-analysis. Clin. Infect. Dis. 2016, 62, 618–630. [Google Scholar] [CrossRef] [Green Version]
- Ribeiro, E.; Pereira, A.; Vieira, C.; Paulos, I.; Marques, M.; Swart, T.; Monteiro, A. Bacteria Bioburden Assessment and MRSA Colonization of Workers and Animals from a Portuguese Swine Production: A Case Report. In Occupational Safety and Hygiene VI; CRC Press: London, UK, 2018; pp. 351–354. [Google Scholar] [CrossRef]
- Ribeiro, E.; Monteiro, A. Bacterial Contamination Assessment and MRSA Colonization in the Context of Occupational Exposure in Portuguese Swine Productions. Int. Symp. Occup. Saf. Hyg. Proc. B. SHO 2020, 2020, 257–261. [Google Scholar]
- Viegas, C.; Monteiro, A.; Ribeiro, E.; Caetano, L.A.; Carolino, E.; Assunção, R.; Viegas, S. Organic dust exposure in veterinary clinics: A case study of a small-animal practice in Portugal. Arch. Ind. Hyg. Toxicol. 2018, 69, 309–316. [Google Scholar] [CrossRef] [Green Version]
- Viegas, C.; Sousa, P.; Dias, M.; Caetano, L.A.; Ribeiro, E.; Carolino, E.; Twarużek, M.; Kosicki, R.; Viegas, S. Bioburden contamination and Staphylococcus aureus colonization associated with firefighter’s ambulances. Environ. Res. 2021, 197, 111125. [Google Scholar] [CrossRef]
- Negrinho, A.; Serrano, D.; Shone, S.; Ribeiro, E.; Ferreira, B. Prevalência Da Colonização Nasal Por MRSA Nos Técnicos de ACSP Num Hospital Do Distrito de Lisboa: Estudo-Caso. In Proceedings of the III Congresso Nacional de Ciências Biomédicas Laboratoriais, Lisbon, Portugal, 25–27 October 2019. [Google Scholar]
- Dahms, C.; Hübner, N.-O.; Cuny, C.; Kramer, A. Occurrence of methicillin-resistant Staphylococcus aureus in farm workers and the livestock environment in Mecklenburg-Western Pomerania, Germany. Acta Vet. Scand. 2014, 56, 53. [Google Scholar] [CrossRef] [PubMed]
- Van Cleef, B.A.G.L.; Van Benthem, B.H.B.; Verkade, E.J.M.; Van Rijen, M.M.L.; Kluytmans-van den Bergh, M.F.Q.; Graveland, H.; Bosch, T.; Verstappen, K.M.H.W.; Wagenaar, J.A.; Bos, M.E.H.; et al. Livestock-Associated MRSA in Household Members of Pig Farmers: Transmission and Dynamics of Carriage, A Prospective Cohort Study. PLoS ONE 2015, 10, e0127190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bos, M.E.H.; Verstappen, K.M.; van Cleef, B.A.G.L.; Dohmen, W.; Dorado-García, A.; Graveland, H.; Duim, B.; Wagenaar, J.A.; Kluytmans, J.A.J.W.; Heederik, D.J.J. Transmission through air as a possible route of exposure for MRSA. J. Expo. Sci. Environ. Epidemiol. 2016, 26, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Viegas, C.; Faria, T.; Monteiro, A.; Caetano, L.A.; Carolino, E.; Gomes, A.Q.; Viegas, S. A Novel Multi-Approach Protocol for the Characterization of Occupational Exposure to Organic Dust—Swine Production Case Study. Toxics 2017, 6, 5. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Aarnink, A.J.A.; de Jong, M.C.M.; Groot Koerkamp, P.W.G. Airborne Microorganisms from Livestock Production Systems and Their Relation to Dust. Crit. Rev. Environ. Sci. Technol. 2014, 44, 1071–1128. [Google Scholar] [CrossRef]
- Feld, L.; Bay, H.; Angen, Ø.; Larsen, A.R.; Madsen, A.M. Survival of LA-MRSA in Dust from Swine Farms. Ann. Work Expo. Health 2018, 62, 147–156. [Google Scholar] [CrossRef] [Green Version]
- van Rijen, M.M.L.; Bosch, T.; Verkade, E.J.M.; Schouls, L.; Kluytmans, J.A.J.W.; on behalf of the CAM Study Group. Livestock-Associated MRSA Carriage in Patients without Direct Contact with Livestock. PLoS ONE 2014, 9, e100294. [Google Scholar] [CrossRef] [Green Version]
- Larsen, J.; Petersen, A.; Sørum, M.; Stegger, M.; Van Alphen, L.; Valentiner-Branth, P.; Knudsen, L.K.; Larsen, L.S.; Feingold, B.; Price, L.B.; et al. Meticillin-resistant Staphylococcus aureus CC398 is an increasing cause of disease in people with no livestock contact in Denmark, 1999 to 2011. Eurosurveillance 2015, 20, 30021. [Google Scholar] [CrossRef] [Green Version]
- Deiters, C.; Günnewig, V.; Friedrich, A.W.; Mellmann, A.; Köck, R. Are cases of Methicillin-resistant Staphylococcus aureus clonal complex (CC) 398 among humans still livestock-associated? Int. J. Med. Microbiol. 2015, 305, 110–113. [Google Scholar] [CrossRef]
- Nielsen, R.T.; Kemp, M.; Holm, A.; Skov, M.N.; Detlefsen, M.; Hasman, H.; Aarestrup, F.M.; Kaas, R.S.; Nielsen, J.B.; Westh, H.; et al. Fatal Septicemia Linked to Transmission of MRSA Clonal Complex 398 in Hospital and Nursing Home, Denmark. Emerg. Infect. Dis. 2016, 22, 900–902. [Google Scholar] [CrossRef] [Green Version]
- Viegas, C.; Faria, T.; Caetano, L.A.; Carolino, E.; Quintal-Gomes, A.; Twarużek, M.; Kosicki, R.; Viegas, S. Characterization of Occupational Exposure To Fungal Burden in Portuguese Bakeries. Microorganisms 2019, 7, 234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viegas, C.; Fleming, G.T.A.; Kadir, A.; Almeida, B.; Caetano, L.A.; Gomes, A.Q.; Twarużek, M.; Kosicki, R.; Viegas, S.; Coggins, A.M.; et al. Occupational Exposures to Organic Dust in Irish Bakeries and a Pizzeria Restaurant. Microorganisms 2020, 8, 118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mondal, H.; Gupta, I.; Nandi, P.; Ghosh, P.; Chattopadhyay, S.; Mitra, G.D. Nasal Screening of Healthcare Workers for Nasal Carriage of Methicillin Resistance Staphylococcus aureus, Vancomycin Resistance Staphylococcus aureus and Prevalence of Nasal Colonization with Staphylococcus aureus in Burdwan Medical College and Hospital. Int. J. Contemp. Med. Res. 2016, 3, 3342–3346. [Google Scholar]
- Dulon, M.; Peters, C.; Schablon, A.; Nienhaus, A. MRSA carriage among healthcare workers in non-outbreak settings in Europe and the United States: A systematic review. BMC Infect. Dis. 2014, 14, 363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mainous, A.G.; Hueston, W.J.; Everett, C.J.; Diaz, V.A. Nasal Carriage of Staphylococcus aureus and Methicillin-Resistant S aureus in the United States, 2001–2002. Ann. Fam. Med. 2006, 4, 132–137. [Google Scholar] [CrossRef] [Green Version]
- Touimi, G.B.; Bennani, L.; Berrada, S.; Moussa, B.; Bennani, B. Prevalence and antibiotic resistance profiles of Staphylococcus sp. isolated from food, food contact surfaces and food handlers in a Moroccan hospital kitchen. Lett. Appl. Microbiol. 2020, 70, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, O.B. Prevalence of Methicillin-Resistant Staphylococcus aureus and Classical Enterotoxin Genes among Sudanese Food Handlers. Cureus 2020, 12, e12289. [Google Scholar] [CrossRef]
- Ribeiro, E.; Clérigo, A. Assessment of Staphylococcus aureus Colonization in Bakery Workers: A Case Study. In Vertentes e Desafios da Segurança 2017;. Leiria, Portugal, 2017. In Vertentes e Desafios da Segurança 2017; Simões & Linhares: Leiria, Portugal.
- Ghasemzadeh-Moghaddam, H.; Neela, V.; van Wamel, W.; Hamat, R.A.; Shamsudin, M.N.; Hussin, N.S.C.; Aziz, M.N.; Haspani, M.S.M.; Johar, A.; Thevarajah, S.; et al. Nasal carriers are more likely to acquire exogenous Staphylococcus aureus strains than non-carriers. Clin. Microbiol. Infect. 2015, 21, 998.e1–998.e7. [Google Scholar] [CrossRef] [Green Version]
- Pittet, D.; Hugonnet, S.; Harbarth, S.; Mourouga, P.; Sauvan, V.; Touveneau, S.; Perneger, T.V. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet 2000, 356, 1307–1312. [Google Scholar] [CrossRef]
- Safdar, N.; Abad, C. Educational interventions for prevention of healthcare-associated infection: A systematic review. Crit. Care Med. 2008, 36, 933–940. [Google Scholar] [CrossRef]
- Rohde, R.E.; Ross-Gordon, J. MRSA model of learning and adaptation: A qualitative study among the general public. BMC Health Serv. Res. 2012, 12, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haag, A.F.; Fitzgerald, J.R.; Penadés, J.R. Staphylococcus aureus in Animals. Microbiol. Spectr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Walser, S.M.; Gerstner, D.G.; Brenner, B.; Bünger, J.; Eikmann, T.; Janssen, B.; Kolb, S.; Kolk, A.; Nowak, D.; Raulf, M.; et al. Evaluation of exposure–response relationships for health effects of microbial bioaerosols–A systematic review. Int. J. Hyg. Environ. Health 2015, 218, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Clements, M.O.; Foster, S.J. Stress resistance in Staphylococcus aureus. Trends Microbiol. 1999, 7, 458–462. [Google Scholar] [CrossRef]
- Kramer, A.; Schwebke, I.; Kampf, G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 2006, 6, 130. [Google Scholar] [CrossRef] [Green Version]
- Schulz, J.; Friese, A.; Klees, S.; Tenhagen, B.A.; Fetsch, A.; Rösler, U.; Hartung, J. Longitudinal Study of the Contamination of Air and of Soil Surfaces in the Vicinity of Pig Barns by Livestock-Associated Methicillin-Resistant Staphylococcus aureus. Appl. Environ. Microbiol. 2012, 78, 5666–5671. [Google Scholar] [CrossRef] [Green Version]
- Agersø, Y.; Vigre, H.; Cavaco, L.M.; Josefsen, M.H. Comparison of air samples, nasal swabs, ear-skin swabs and environmental dust samples for detection of methicillin-resistant Staphylococcus aureus (MRSA) in pig herds. Epidemiol. Infect. 2014, 142, 1727–1736. [Google Scholar] [CrossRef]


| Occupational Environment/Control Group | Biological Samples | Environmental Samples | References |
|---|---|---|---|
| Swineries (N = 5) | Nasopharyngeal swabs (N = 68; 26 humans and 42 animals) | Not performed | [11,12] |
| Veterinary clinic (N = 1) | Nasopharyngeal swabs (N = 14) | Not performed | [13] |
| Ambulance crew (N = 12) | Nasopharyngeal swabs (N = 33) | Surface swabs (N = 98) performed on floor, gurney handle, chairs, entrance and ceiling handle, washstand, shelves, driver’s cabin (wheel) and air exit of the medical cabin | [14] |
| Healthcare Environment (N = 3) | Nasopharyngeal swabs (N = 93; 38 from Hospital 1, 30 from Hospital 2, 25 from PHCC) | Not performed | [15] |
| Bakeries (N = 13) | Nasopharyngeal swabs (N = 74) | Not performed | Data not published |
| Control group (N = 2) | Nasopharyngeal swabs (N = 55; 25 from Study 1, 30 from Study 2) | Not performed | Data not published |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, K.; Viegas, C.; Ribeiro, E. MRSA Colonization in Workers from Different Occupational Environments—A One Health Approach Perspective. Atmosphere 2022, 13, 658. https://doi.org/10.3390/atmos13050658
Oliveira K, Viegas C, Ribeiro E. MRSA Colonization in Workers from Different Occupational Environments—A One Health Approach Perspective. Atmosphere. 2022; 13(5):658. https://doi.org/10.3390/atmos13050658
Chicago/Turabian StyleOliveira, Ketlyn, Carla Viegas, and Edna Ribeiro. 2022. "MRSA Colonization in Workers from Different Occupational Environments—A One Health Approach Perspective" Atmosphere 13, no. 5: 658. https://doi.org/10.3390/atmos13050658
APA StyleOliveira, K., Viegas, C., & Ribeiro, E. (2022). MRSA Colonization in Workers from Different Occupational Environments—A One Health Approach Perspective. Atmosphere, 13(5), 658. https://doi.org/10.3390/atmos13050658







