Heat is a specific issue in terms of climate change due to the negative effects on morbidity/mortality and on human health in general. Measures and recommendations against heat and its effects should reach affected people, helpers and decision makers and should, therefore, be communicated in an appropriate and easily understandable way.
The aim of this editorial is to provide very specific communication aspects in terms of the short- and long-term communication of heat and heat effects.
The health risks to be expected from anthropogenically influenced climate change are not locally limited, but of a global scale. Regarding its characteristics and possible manifestations, the health consequences of climate change can occur in both direct and indirect ways, which is why they are also considered separately. Direct consequences are primarily and directly caused, for example, by temperature extremes, such as periods of cold and heat. During such periods, there can be effects related to deterioration in the health status of patients with diseases of the cardiovascular system and the respiratory tract, possibly resulting in death. The health consequences of climate change are not only of a physical nature; they can also be indirect psychological and social burdens. These include stress, anxiety and depression, so-called secondary health effects.
The complex and multi-causal interrelationships have so far made it difficult to make concrete statements and forecasts about the health consequences of climate change. However, according to the current knowledge, it is expected that climate change will lead to an increase in extreme meteorological events in the future, which will also increase the health risks for the population [1].
Heat waves hold the biggest risks, and they are associated with periods of unusually high temperatures and a lack of night-time cooling that can last for several days. The level of these extreme conditions, which is mostly determined on the basis of heat conditions and duration, differs depending on the area of application and region of investigation [2]. A uniform definition of heat waves does not exist and is almost impossible due to the complexity and the different requirements for a definition, including in the approach towards different geographic/climatic contexts. Often, a threshold is set for temperature and minimum duration, using absolute or relative thresholds. Relative thresholds are more suited for comparison between different countries, as humans are adapted to the regional and local climate [3].
Since the heat waves of summer 2003, countries and cities in Europe have started to develop emergency plans, including early warning systems [4]. With accurate and early weather forecasts, thorough knowledge of the effects of heat, and education and advice for citizens and targeted measures for vulnerable populations, as well as appropriate landscape and urban planning measures, the number of avoidable deaths should be reduced in future heat waves [5,6].
The negative health consequences of heat waves have been both demonstrated and documented within mortality data for numerous countries, and have thus far been well studied by the international scientific community. During the well-known heat wave in the summer of 2003, which hit large parts of Western and Central Europe in early August, around 7600 additional deaths were recorded in Germany [3] and over 70,000 for Europe [7,8,9]. Not only in the mortality data, but also in other data linked to health systems (i.e., hospital admissions and emergency room visits), the negative influence of heat waves is unambiguously palpable.
The following facts are known:
- -
- Causes of death were heart stroke, cardiovascular disease, renal disease, and respiratory and metabolic disorders due to heat stress.
- -
- The age group over 70 was most affected, especially in the case of women.
- -
- People with chronic diseases were more at risk than others as a result of exacerbating inherent symptoms and vulnerabilities.
- -
- Vulnerable, low-income populations (and their inherently associated living standards/conditions) were the most affected by the additional mortality rates.
The extreme heat was higher in cities than elsewhere. Although it is noted that increases in temperatures in peri-urban and rural areas were also witnessed, thus raising the need to apply caution in Urban Heat Island (UHI) comparative calculation methodologies as well.
The effects of heat on people’s health depend on three influencing factors: the duration, frequency and intensity to which people are exposed. For healthy people, slightly increased demands on thermoregulation, which are met by appropriate activity, behaviour, and sufficient fluid intake, reduce the threat and/or challenge presented to the biometeorological system. Heat puts strain on the cardiovascular system, and the body is exposed to higher stress in order to keep the core body temperature constant. For people with pre-existing health implications and problems, this additional stress can exacerbate numerous existing susceptibilities, which is why heat has also been shown to have a significant influence on other diseases, including respiratory diseases. If thermoregulation is restricted, disturbances of the water and electrolyte balance can occur, which can lead to life-threatening impairments of the cardiovascular system. In addition to medical factors, socioeconomic and environmental issues are among the risk factors of heat-related mortality, including, but not limited to, increased ozone and particulate matter levels.
People with health problems are generally limited in their ability to adapt to heat, and, therefore, suffer more from heat stress than healthy people. In addition, an adjustment of medication may be necessary during hot weather. For example, given the influences of heat upon blood vessel dilation and/or widening, those that rely on medication to regulate their blood pressure should consult with their doctor or pharmacist at the beginning of the summer to account for such heat wave events. Invariably, such recommendations are again related to other urban socioeconomic dynamics, which reiterates the important recognition that such preventative measures (in the daily lives of urban inhabitants) may not be as easy for some. However, the objective causality of not undertaking such measures, when needed, will emphatically present the same risk for those with similar cardiovascular afflictions, irrespective of their socioeconomic standing. In addition to the aforementioned groups of people, small children and infants, as well as people with limited mobility, also have an increased risk of suffering from heat.
Early warning systems, such as Heat Health Warnings Systems (HHWS), are required not only for information, but for the protection of the population as well. One example, which combines meteorological and epidemiological factors, is the HHWS in Germany. From May to the beginning of September, the German Meteorological Service (DWD) issues warnings for the current day and the following day if the perceived temperature (a temperature, which combines the effect of air temperature, humidity, wind, and radiation fluxes) exceeds the warning thresholds at 14:00 time. Based on the numerical weather forecast, it is calculated if (and up to which amount) the heat warning threshold “severe heat stress” is exceeded in the respective district. At the same time, it is also checked whether the indoor temperature at night falls below a certain threshold, as a recovery phase is ensured if there is a corresponding night-time cooling. At a perceived temperature of 38 °C and higher, a warning is automatically issued without taking the night-time situation into account [4].
It is well known that cities are warmer overall in comparison to their surrounding peri-urban and rural areas. Following the same logic, and in light of the growing climate change agendas since the turn of the century, such settings are becoming continually more contingent on long-term adaptation measures. The urban climate is the climate modified by the interaction with built-up areas and their cause-and-effect relationship with one another (including excess heat generation and the emission of air pollutants). The urban climate is a climate that is modified by anthropogenically changed land use. In the discussion on climate change, the urban climate has a special status due to the large local population density, and the locally high levels of energy consumption [10,11].
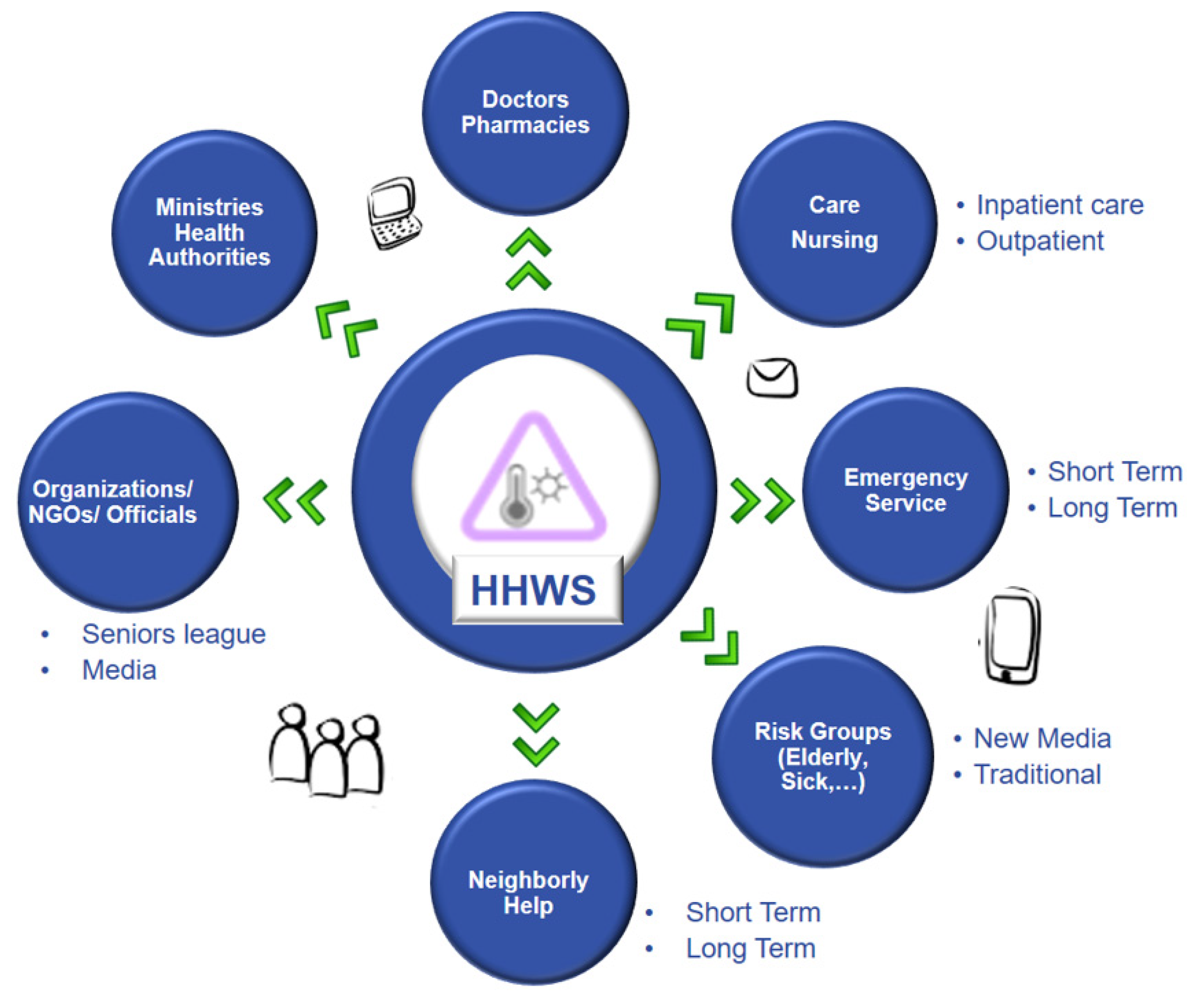
The HHWS in Germany is aimed, in particular, at old people’s homes and nursing homes, but also at the general population (Figure 1). In Germany, current heat warnings are disseminated via a newsletter system, the internet or a smart phone app. Once a heat warning has been issued, the competent health authorities of the federal states compile a list of intervention measures and monitor the implementation of these measures. In addition, they have the option of further disseminating the warning to the population via radio and television. Overall, the information of the heat warning system is available via the DWD website (www.dwd.de, accessed on 10 January 2022), the warning smartphone app, or the newsletter and can alert not only the general population, but also, in particular, care facilities and hospitals to take preparatory measures (Figure 1). Cities and the elderly are also given special consideration during heat warnings [4]. Behavioural measures for heat cramps, heat exhaustion or heat stroke can be taken from [9].
Figure 1.
Communication paths for heat health warnings.
The different existing communication channels are shown in Figure 1. These are not only bodies that have an official character, but also neighborhood help and non-official bodies (NGOs). The communication of heat should address and include dissemination from modern communication channels (apps, newsletters and social networks); the media (TV and press releases); specific groups of affected people (including the elderly), as well as prevention and care groups (doctors, pharmacies and hospital staff); rescue and Caritas associations; volunteers (neighborhood help) and official helpers (care people); and supporting associations. Another consideration is the traditional methods of communication (television and teletext), as well as information material (flyers and leaflets) and prevention training and care staff.
In general, heat warnings should include the area of the warning, elevation affects, if cities are affected more than rural areas, specific information for vulnerable and risk groups (with a focus on the most affected groups, such as elderly people), duration of heat (amount of days with warning) and measure/s to be taken against the heat.
It can be argued that people living in cities are now already experiencing anthropogenic, i.e., human-made, climate change [10,11]. A key feature of the urban climate is the UHI, which can average around 2–3 °C in annual mean, and in some cases, can reach up to 10 °C for short periods at night. The main cause of overheating in cities is due to the presence of more surfaces (especially vertical surfaces), with a large amount of solar radiation reflection and absorption and the low possibility of releasing heat into the air (i.e., as a result of lower sky view factors). The second major cause of heat generation and intensity is heat storage due to building materials. The input to create the heat island happens during the day, but the resultant effects manifest both during the day and night. Measures to reduce heat in cities, whether they are energy-related or health-related, should always aim to address the main causes and effects. Common mitigation and adaptation measures in the field of the microclimate are mostly linked to “Green and Blue” factors. Such measures to reduce the UHI and summer heat stress for people include green roofs and façade greening, as well as artificial shading measures for buildings, open spaces and green areas. Here, not only the reduction in air temperature and humidity should be targeted, but more the solar radiation and wind, which can be significantly modified and influenced by urban planning, and architectural and landscape measures [12,13,14,15]. Heat waves are more stressful for urban residents than for rural residents due to the UHI effect. Urbanization, in addition to demographic change, is also increasing the proportion of at-risk groups for this reason
In the German Strategy for Adaptation to Climate Change, adaptation measures to heat waves are highlighted by the Federal Government as urgent fields of action. In 2008, the World Health Organization (WHO) issued recommendations on “heat action plans” to prevent heat-related health damage through comprehensive activities at different levels. Heat warning systems are mentioned as one instrument to prevent negative health impacts [16].
Heat action plans, which aim at comprehensive intervention measures for health protection, serve as prevention for health consequences against climate change. They follow an integrative approach that combines short-, medium- and long-term health protection measures in a common framework and comprise eight fields of action. The recommendations are intended to assist in the preparation of such adapted heat action plans [16,17]. The recommendations for action include activities that can be implemented in the short term (e.g., establishing communication channels) and in the longer term (e.g., urban planning measures). While in some cases, implementation is already well advanced (e.g., establishment of the heat warning system), other activities still leave a large amount of room for development and represent, above all, a challenge for the future (e.g., establishment of mortality rates, harvesting effect control and the monitoring of measures).
The aim of these recommendations is to encourage each competent authority, even with limited human and financial resources, to move forward with the development of a heat action plan with the available “on-board resources” in order to be better prepared for heat waves. Many of the measures can be implemented at low cost, as it is essentially a matter of raising awareness of the issue in order to bring about changes in behavior patterns among those affected. Structural measures can also sometimes be implemented at a relatively low cost, e.g., in changes to existing buildings that are already necessary, in urban planning or in building projects. In addition to this recognition, one must also embrace that efforts against urban heat vulnerability can take place at different scales, whereby in situ adaptation does not need to be the first step to reducing vulnerability [15]. It is more often the case that action must take place in the form of identification and warning in the shorter term; while not always directly physical, it continues to be a form of adaptation, one which can also embrace the existing socioeconomic and environmental factors/vulnerabilities in the shorter term, and later, further inform physical adaptive measures in cities as well.
A consensus of all stakeholders is important for this: the goal is to protect the health of the population from the negative consequences of extreme heat, which must be approached by acknowledging its three key factors: duration, frequency and intensity. Heat action plans are to be drawn up individually by states or municipalities, as the local conditions, and in particular, the climatic conditions, form the basis of the development and implementation of suitable measures [16].
Adaptation measures should consider acute and long-term aspects. Heat warning systems for different spatial and temporal resolutions to protect the different vulnerable risk groups with corresponding measures in the framework of heat action plans are indispensable tools of adaptation measures. Furthermore, the development of climate-adapted urban planning for cities to combat heat predominantly at the microscale must also be a part of the aforementioned heat action plans.
As exemplified by the case of Germany, the disclosed examples pertaining to heat warnings and adaptation efforts in cities are focused upon moderate climates. Resultantly, it should be noted that the aforementioned lessons and/or approaches discussed cannot be directly applied within other climatic contexts or regions. Here, the linkage with locality (both in terms of the relationship with the climate itself, but also with the urban fabric) is paramount, where specific thresholds for heat warnings should be adjusted for other specific regions based upon basic biometeorological and epidemiological understanding.
Unequivocally, if the possibility for tailored training exists, then this should be exploited as much as possible. Adjacently, and more so if such training is not feasible, effective audience-sensitive interdisciplinary communication becomes all the more important.
In the long term, it also has to be stated that adaptation possibilities at the microscale not only include different facets of the climate, but also edaphic and management issues, which have to be considered. In addition, when specifically approaching cases of heat stress, it is equally significant to appreciate that many options exist nowadays. Following this consideration is the symbiotically growing (i) number of classification, framework and organization approaches of different measure typologies (e.g., of blue and green solutions), along with their subsequent potential benefits, and (ii) in-progress or completed international examples (both in the form of adaptation strategies and measures), which mark an important invigorative departure from previous levels of applicative apprehension and uncertainty.
Two last factors to be addressed are associated with the comprehension that heat is not only an issue for human health. In addition, it covers many other aspects, such as animal health; general health systems; and urban systems that sustain life, including nutrition systems, circadian rhythms, walkability habits, and inner/outer urban transportation infrastructure. For this reason, heat-related issues target more than one sector, and heat health warnings can be useful for other applications and sectors during heat waves, and in general extreme conditions.
Finally, heat can be seen as a hazard, which has a social dimension that affects not only human health in terms of mortality and hospital admission rates, but within the general emergency and health systems themselves. Perpetually, such a hazard is not limited to either outdoor or indoor contexts, and it must be met with general urban infrastructure factors, including the double-edged sword of reliance on energy to mitigate excess levels of heat stress from our daily occupational health indoors and outdoors [18].
Funding
This research received no external funding.
Conflicts of Interest
The author declares no conflict of interest.
References
- Matzarakis, A. Das Hitzewarnsystem des Deutschen Wetterdienstes (DWD) und seine Relevanz für die menschliche Gesundheit. Gefahrst. Reinhalt. Der Luft Bd 2016, 76, 457–460. [Google Scholar]
- Graw, K.; Muthers, S.; Matzarakis, A. Hitzewellen und Hitzewarnungen in Städten. In Warnsignal Klima: Die Städte; GEO Magazin-Hamburg: Hamburg, Germany, 2019. [Google Scholar] [CrossRef]
- An der Heiden, M.; Muthers, S.; Niemann, H.; Buchholz, U.; Grabenhenrich, L.; Matzarakis, A. Schatzung hitzebedingter Todesfalle in Deutschland zwischen 2001 und 2015. Bundesgesundheitsblatt Gesundh. Gesundh. 2019, 62, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Matzarakis, A.; Laschewski, G.; Muthers, S. The Heat Health Warning System in Germany—Application and Warnings for 2005 to 2019. Atmosphere 2020, 11, 170. [Google Scholar] [CrossRef] [Green Version]
- Matzarakis, A. Hitzeereignisse: Charakteristika, Gesundheitsrelevanz und Anpassungsmöglichkeiten. Geographische Rundschau 2021, 2021, 8–13. [Google Scholar]
- Mücke, H.; Matzarakis, A. Klimawandel und Gesundheit. In Handbuch für Umweltmedizin. Ecomed, LandsbergamLech; Wichmann, E., Fromme, H., Eds.; Ecomed: Landsberg, Germany, 2017; pp. 1–38. [Google Scholar]
- Robine, J.-M.; Cheung, S.L.; Le Roy, S.; Van Oyen, H.; Herrmann, F.R. Report on Excess Mortality in Europe during Summer 2003; EU Community Action Programme for Public Health, Grant Agreement: Brussels, Belgium, 2007; p. 28. [Google Scholar]
- Robine, J.M.; Cheung, S.L.; Le Roy, S.; Van Oyen, H.; Griffiths, C.; Michel, J.-P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Mücke, H.-G.; Matzarakis, A. Klimawandel und Gesundheit: Tipps für Sommerliche Hitze und Hitzewellen; Deutscher Wetterdienst: Offenbach, Germany, 2019; Available online: https://www.umweltbundesamt.de/publikationen/klimawandel-gesundheit-tipps-fuer-sommerliche-hitze (accessed on 10 January 2022).
- Matzarakis, A.; Paramita, B. Equity, Equality and Justice in Urban Housing Development; UPI Press: Bandung, Germany, 2018; pp. 1–327. [Google Scholar]
- Oke, T.R.; Mills, G.; Christen, A.; Voogt, J.A. Urban Climates; Cambridge University Press: Cambridge, UK, 2017. [Google Scholar]
- Matzarakis, A. Stadtklima vor dem Hintergrund des Klimawandels. Gefahrst.–Reinhalt. Der Luft 2013, 73, 115–118. [Google Scholar]
- Matzarakis, A. Das Stadtklima–Herausforderung heute und für die Zukunft. Der Archit. 2018, 5, 36–39. [Google Scholar]
- Santos Nouri, A.; Matzarakis, A. The Maturing Interdisciplinary Relationship between Human Biometeorological Aspects and Local Adaptation Processes: An Encompassing Overview. Climate 2019, 7, 134. [Google Scholar] [CrossRef] [Green Version]
- Santos Nouri, A.; Costa, J.; Santamouris, M.; Matzarakis, A. Approaches to Outdoor Thermal Comfort Thresholds through Public Space Design: A Review. Atmosphere 2018, 9, 108. [Google Scholar] [CrossRef] [Green Version]
- Straff, W.; Mücke, H.-G.; Baeker, R.; Baldermann, C.; Braubach, A.; Litvinovitch, J.; Matzarakis, A.; Petzold, G.; Rexroth, U.; Schroth, S. Handlungsempfehlungen für die Erstellung von Hitzeaktionsplänen zum Schutz der menschlichen Gesundheit. Bundesgesundheitsblatt-Gesundh.–Gesundh. 2017, 60, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Zielo, B.; Matzarakis, A. Bedeutung von Hitzeaktionspläne für den präventiven Gesundheitsschutz in Deutschland. Gesundheitswesen 2017, 79. [Google Scholar] [CrossRef] [PubMed]
- Klinenberg, E. Heat Wave: A Social Autopsy of Disaster in Chicago; University of Chicago Press: Chicago, IL, USA, 2015. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).