The Effects of Air Quality on Hospital Admissions for Chronic Respiratory Diseases in Petaling Jaya, Malaysia, 2013–2015
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Site
2.2. University of Malaysia Medical Centre (UMMC) Data
2.3. Pollution Data
2.4. Weather Data
2.5. Time Series Analysis
3. Results
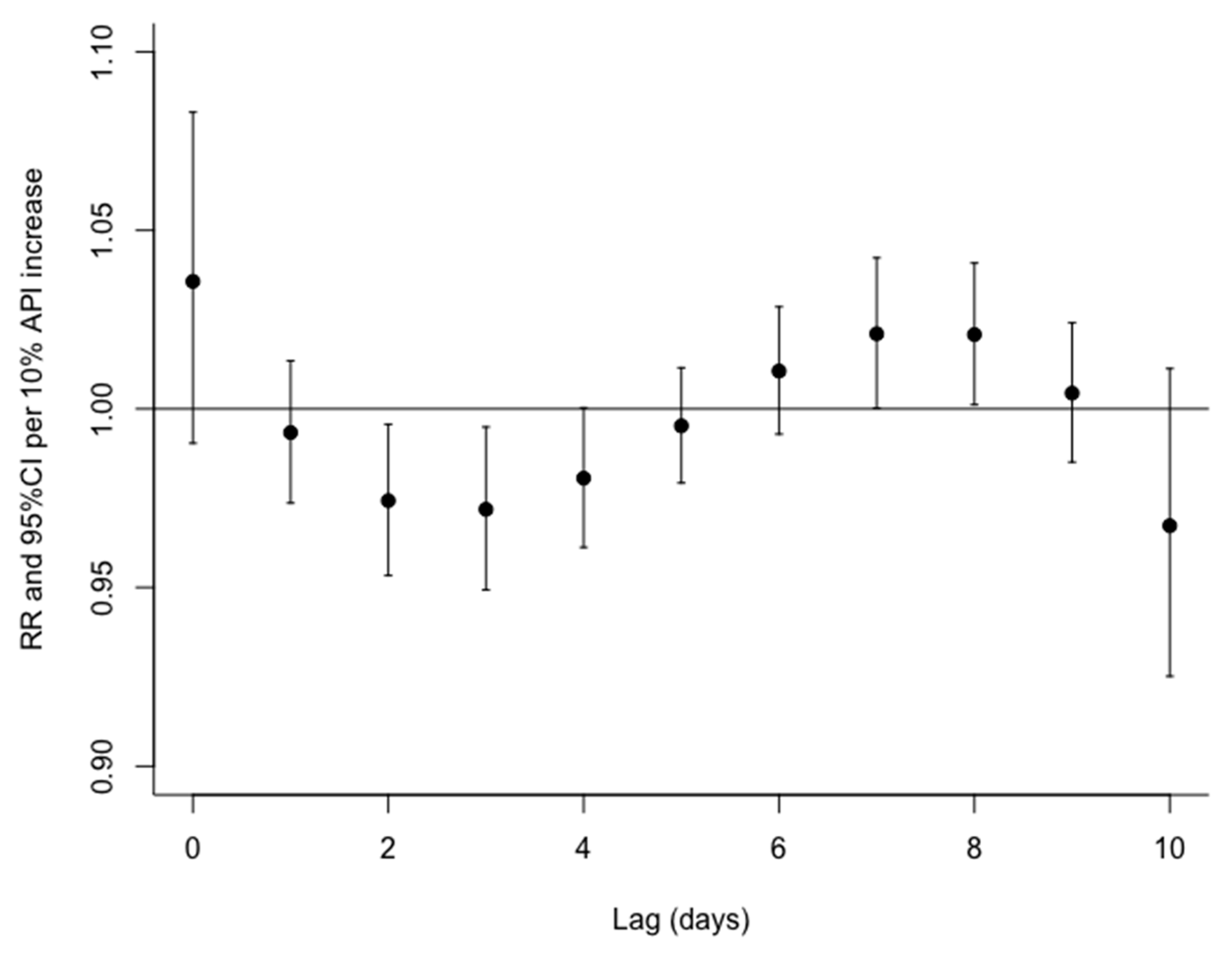
3.1. Single Day Lagged Models
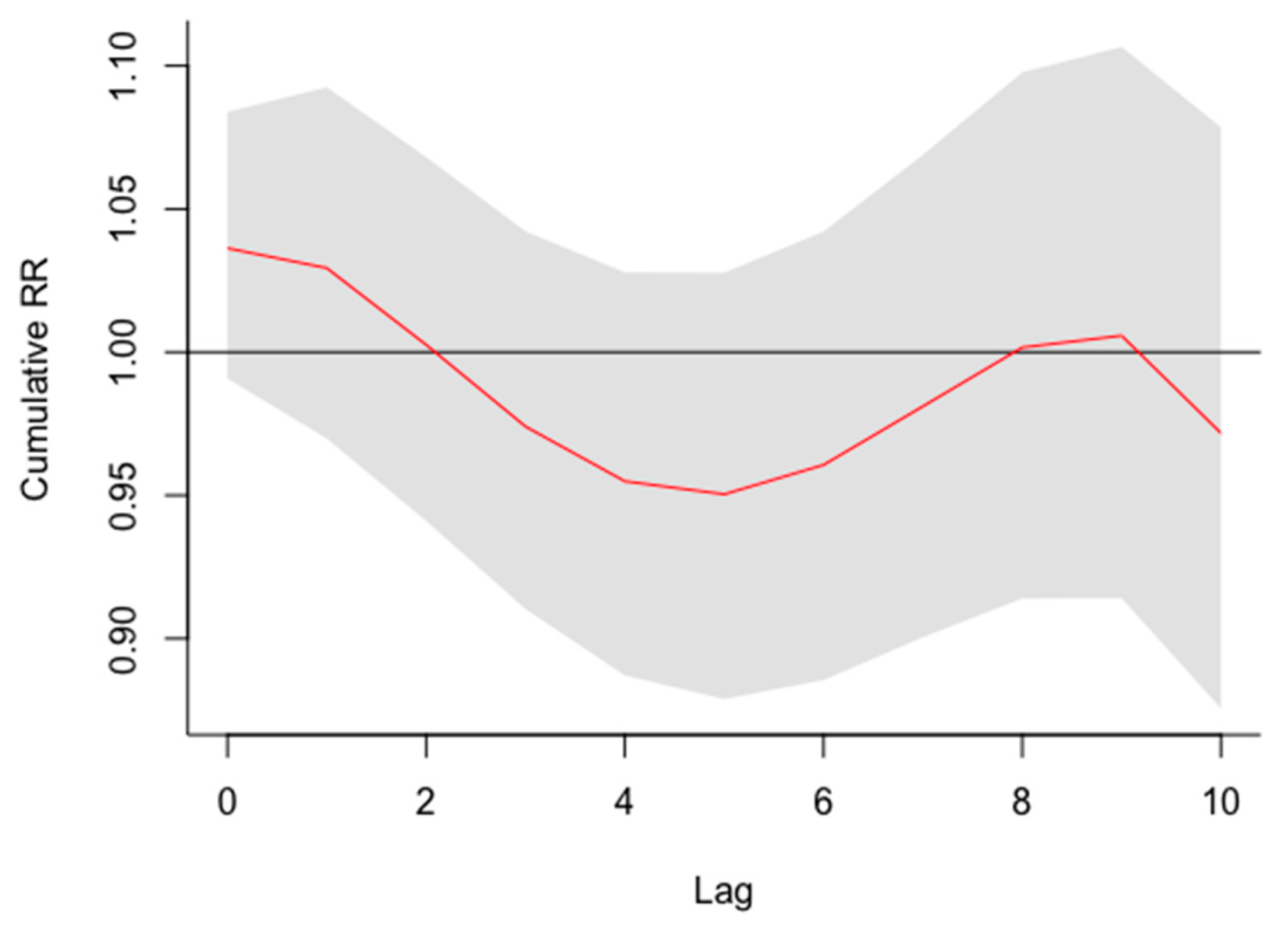
3.2. Cumulative Effect
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- HEI International Scientific Oversight Committee. Outdoor Air Pollution and Health in the Developing Countries of Asia: A Comprehensive Review; Special Report 18; Health Effects Institute: Boston, MA, USA, 2010. [Google Scholar]
- Tajudin, M.A.; Khan, M.F.; Mahiyuddin, W.R.; Hod, R.; Latif, M.T.; Hamid, A.H.; Abd Rahman, S.; Sahani, M. Risk of concentrations of major air pollutants on the prevalence of cardiovascular and respiratory diseases in urbanized area of Kuala Lumpur, Malaysia. Ecotoxicol. Environ. Saf. 2019, 171, 290–300. [Google Scholar] [CrossRef]
- WHO. WHO. WHO releases country estimates on air pollution exposure and health impact. In New Interactive Maps Highlight Areas within Countries that Exceed WHO Air Quality Limits; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Rafaj, P.; Kiesewetter, G.; Gül, T.; Schöpp, W.; Cofali, J.; Klimont, Z.; Purohit, P.; Heyes, C.; Amann, M.; Borken-Kleefeld, J.; et al. Outlook for clean air in the context of sustainable development goals. Glob. Environ. Chang. 2018, 53, 1. [Google Scholar] [CrossRef]
- Usmani, R.S.; Saeed, A.; Abdullahi, A.M.; Pillai, T.R.; Jhanjhi, N.Z.; Hashem, I.A. Air pollution and its health impacts in Malaysia: A review. Air Qual. Atmos. Health 2020, 13, 1093–1118. [Google Scholar] [CrossRef]
- Afroz, R.; Hassan, M.N.; Ibrahin, N.A. Review of air pollution and health impacts in Malaysia. Environ. Res. 2003, 92, 71–77. [Google Scholar] [CrossRef]
- Department of Environment (DOE). Malaysia Environmental Quality Report; MoNRE: Kuala Lumpur, Malaysia, 2015.
- Qureshi, M.I.; Rasli, A.M.; Awan, U.; Ma, J.; Ali, G.; Alam, A.; Sajjad, F.; Zaman, K. Environment and air pollution: Health services bequeath to grotesque menace. Environ. Sci. Pollut. Res. 2015, 22, 3467–3476. [Google Scholar] [CrossRef]
- Awang, M.F.; Jalaludin, J.; Latif, M.T.; Fandi, N.F. Exposure to PM2.5 in urban area and respiratory health symptoms among urban workers in Klang Valley. IOP Conf. Ser. Earth Environ. Sci. 2019, 228, 012015. [Google Scholar] [CrossRef]
- Abidin, E.Z.; Semple, S.; Rasdi, I.; Ismail, S.N.; Ayres, J.G. The relationship between air pollution and asthma in Malaysian schoolchildren. Air Quality. Atmos. Health 2014, 7, 421–432. [Google Scholar] [CrossRef]
- Mabahwi, N.A.; Leh, O.L.H.; Musthafa, S.N.; Aiyub, K. Air quality-related human health in an urban region. Case study: State of Selangor, Malaysia. Environ. Asia 2018, 11, 194–216. [Google Scholar]
- Latif, M.T.; Othman, M.; Idris, N.; Juneng, L.; Abdullah, A.M.; Hamzah, W.P.; Khan, M.F.; Sulaiman, N.M.; Jewaratnam, J.; Aghamohammadi, N.; et al. Impact of regional haze towards air quality in Malaysia: A review. Atmos. Environ. 2018, 177, 28–44. [Google Scholar] [CrossRef]
- Wong, L.P.; Alis, H.; Aghamohammadi, N.; Ghadimi, A.; Sulaiman, N.M. Control measures and health effects of air pollution: A survey among public transportation commuters in Malaysia. Sustainability 2017, 9, 1616. [Google Scholar] [CrossRef] [Green Version]
- Sulong, N.A.; Latif, M.T.; Khan, M.F.; Amil, N.; Ashfold, M.J.; Wahab, M.I.; Chan, K.M.; Sahani, M. Source apportionment and health risk assessment among specific age groups during haze and non haze episodes in Kuala Lumpur, Malaysia. Sci. Total Environ. 2017, 1, 556–570. [Google Scholar] [CrossRef]
- Jie, Y. Air Pollution Associated with Sumatran Forest Fires and Mortality on the Malay Peninsula. Pol. J. Environ. Stud. 2017, 26, 163–171. [Google Scholar] [CrossRef]
- Makar, M.; Antonelli, J.; Di, Q.; Cutler, D.; Schwartz, J.; Dominici, F. Estimating the Causal Effect of Fine Particulate Matter Levels on Death and Hospitalization: Are Levels Below the Safety Standards Harmful? Epidemiology 2017, 28, 627. [Google Scholar] [CrossRef]
- Schwartz, J.; Bind, M.A.; Koutrakis, P. Estimating causal effects of local air pollution on daily deaths: Effect of low levels. Environ. Health Perspect. 2017, 125, 23–29. [Google Scholar] [CrossRef] [Green Version]
- Alari, A.; Schwarz, L.; Zabrocki, L.; Le Nir, G.; Chaix, B.; Benmarhni1, T. The effects of an air quality alert program on premature mortality: A difference-in-differences evaluation in the region of Paris. Environ. Int. 2021, 156, 106583. [Google Scholar] [CrossRef]
- Costa, A.F.; Hoek, G.; Brunekreef, B.; Ponce de Leon, A.C. Air pollution and deaths among elderly residents of Sao Paulo, Brazil: An analysis of mortality displacement. Environ. Health Perspect. 2017, 25, 349–354. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, J. Is there harvesting in the association of airborne particles with daily deaths and hospital admissions? Epidemiology 2001, 1, 55–61. [Google Scholar] [CrossRef]
- Hajat, S.; Armstrong, B.G.; Gouveia, N.; Wilkinson, P. Mortality displacement of heat-related deaths: A comparison of Delhi, Sao Paulo, and London. Epidemiology 2005, 1, 614–620. [Google Scholar] [CrossRef]
- Qi, H.; Pu, V.C.; Tia, L. Short-term effects of fine and coarse particles on deaths in Hong Kong elderly population: An analysis of mortality displacement. Environ. Pollut. 2018, 241, 148–154. [Google Scholar] [CrossRef]
- Sherina, M.S.; Rampal, L.; Hejar, A.R.; Rozali, A.; Mohd Yunus, A. Prevalence of urban poor and its health related factors in the state of Selangor, Malaysia. Malays. J. Med. Health Sci. 2011, 7, 17–25. [Google Scholar]
- Usmani, R.S.; Pillai, T.R.; Hashel, I.A.; Marjani, M.; Shaharudil, R.; Latif, M.T. Air pollution and cardiorespiratory hospitalization, predictive modeling, and analysis using artificial intelligence techniques. Environ. Sci. Pollut. Res. 2021, 1, 1–13. [Google Scholar]
- Zizi, N.M.; Noor, N.M.; Hashim, N.I.; Yusuf, S.Y. Spatial and Temporal Characteristics of Air Pollutants Concentrations in Industrial Area in Malaysia. In IOP Conference Series: Materials Science and Engineering; IOP Publishing: Bristol, UK, 2018. [Google Scholar]
- Quek, D. The Malaysian healthcare system: A review. In Proceedings of the Intensive Workshop on Health Systems in Transition, Kuala Lumper, Malaysia, 29–30 April 2009; pp. 29–30. [Google Scholar]
- Mead, M.I.; Castruccio, S.; Latif, M.T.; Nadzir, M.S.; Dominick, D.; Thota, A.; Crippa, P. Impact of the 2015 wildfires on Malaysian air quality and exposure: A comparative study of observed and modeled data. Environ. Res. Lett. 2018, 13, 044023. [Google Scholar] [CrossRef]
- Rani, N.L.; Azid, A.; Khali1, S.I.; Juahit, H.; Samsudir, M.S. Air Pollution Index Trend Analysis in Malaysia, 2010–2015. Polish J. Environ. Stud. 2018, 27, 801–807. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Gasparrini, A.; Hajat, S.; Smeeth, L.; Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 2013, 42, 1187–1195. [Google Scholar] [CrossRef]
- Pope, C.A.; Schwartz, J. Time series for the analysis of pulmonary health data. Am. J. Respir. Crit. Care Med. 1996, 154, S229–S233. [Google Scholar] [CrossRef]
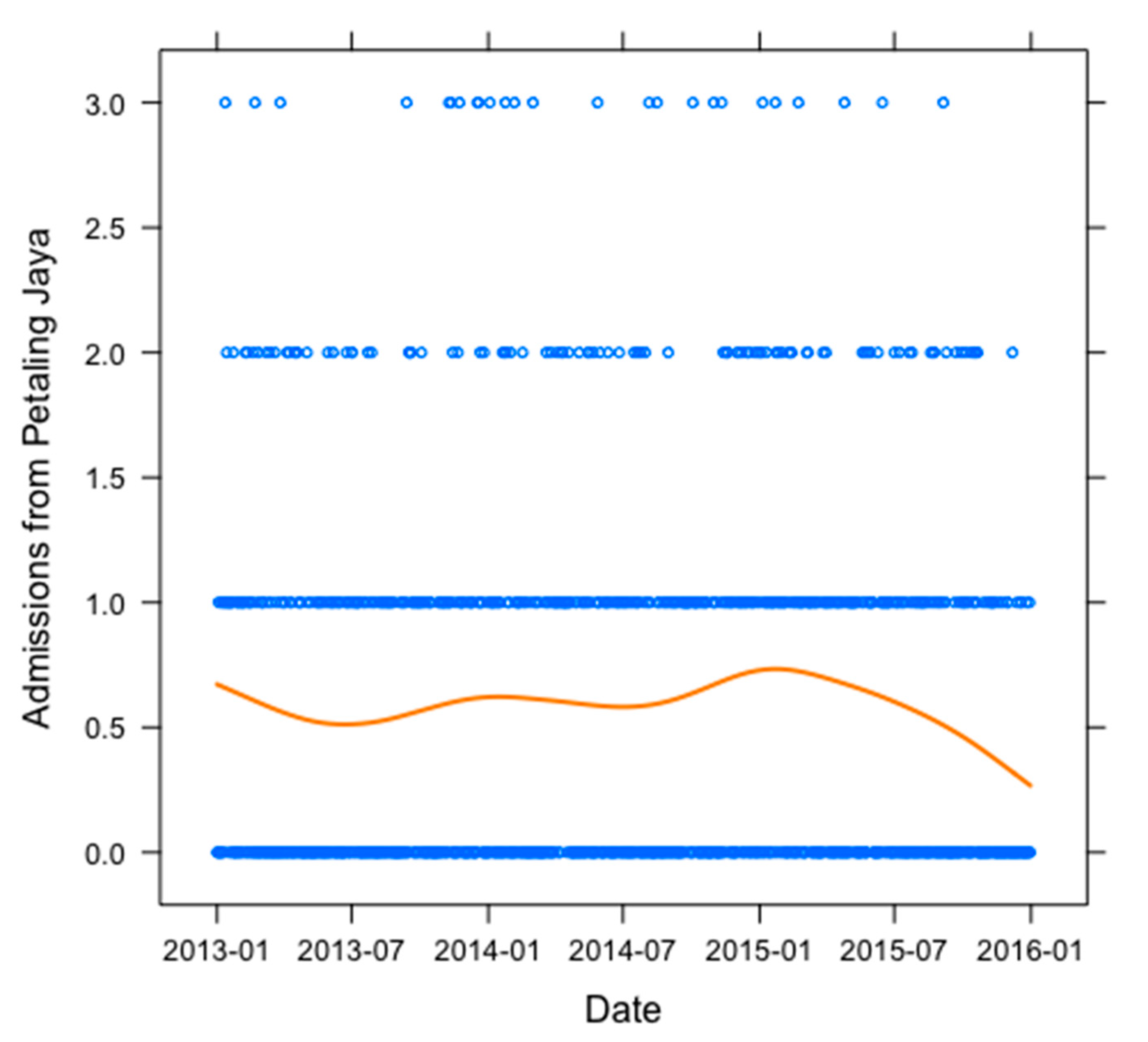
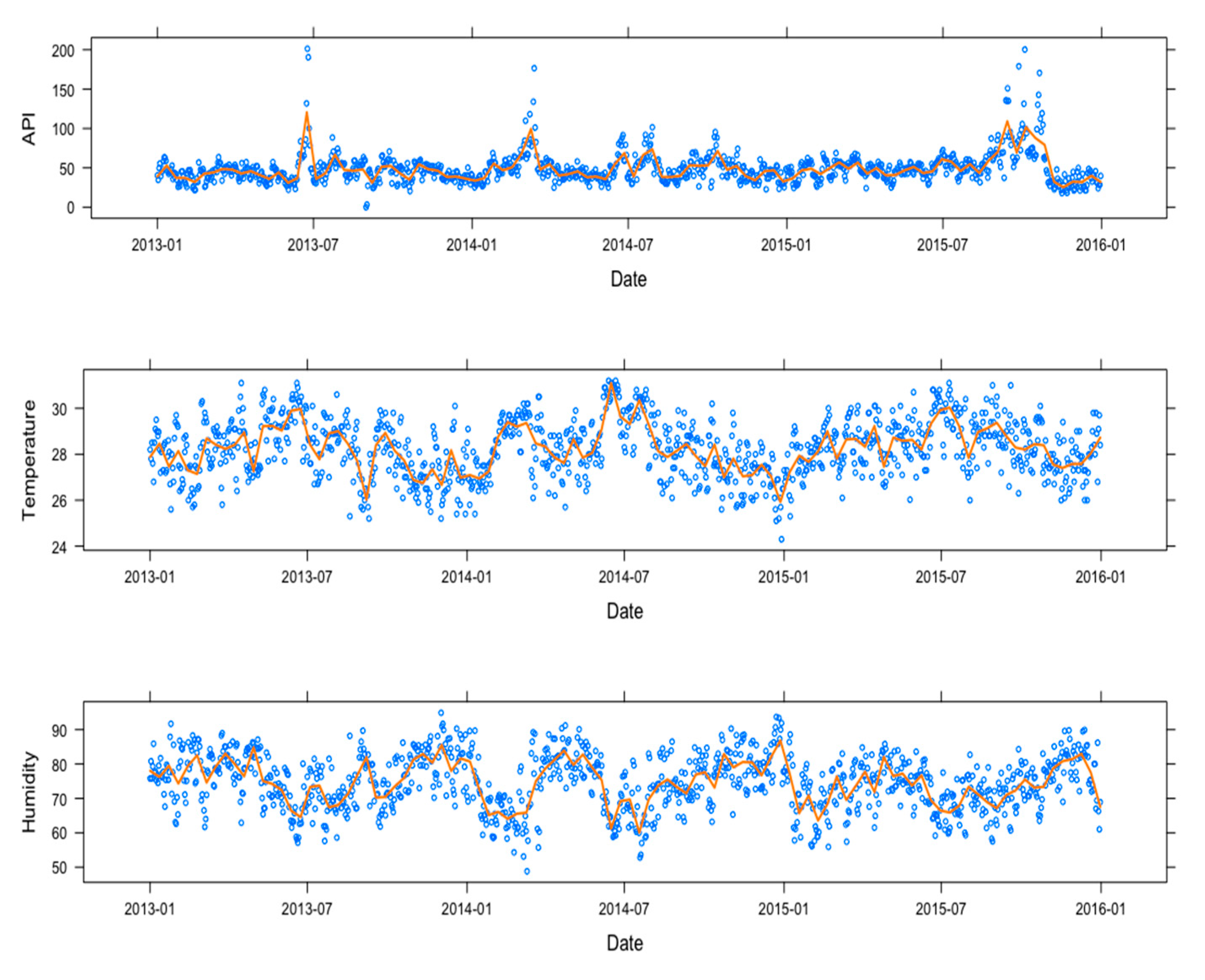
| Total Admissions | Daily Mean | Standard Deviation | Min | Max | Days API > 100 | |
|---|---|---|---|---|---|---|
| Total Admissions to UMMC | 1222 | 1.15 | 0 | 5 | ||
| Daily Admissions for Petaling Jaya residents | 494 | 0.58 | 0.75 | 0 | 3 | |
| Air pollution Index (API) | 49.24 | 19.9 | 0 | 201.3 | 24/1095 | |
| Temperature | 28.27 | 1.26 | 24.3 | 31.2 | ||
| Humidity | 74.66 | 7.99 | 48.8 | 94.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morrissey, K.; Chung, I.; Morse, A.; Parthasarath, S.; Roebuck, M.M.; Tan, M.P.; Wood, A.; Wong, P.-F.; Frostick, S.P. The Effects of Air Quality on Hospital Admissions for Chronic Respiratory Diseases in Petaling Jaya, Malaysia, 2013–2015. Atmosphere 2021, 12, 1060. https://doi.org/10.3390/atmos12081060
Morrissey K, Chung I, Morse A, Parthasarath S, Roebuck MM, Tan MP, Wood A, Wong P-F, Frostick SP. The Effects of Air Quality on Hospital Admissions for Chronic Respiratory Diseases in Petaling Jaya, Malaysia, 2013–2015. Atmosphere. 2021; 12(8):1060. https://doi.org/10.3390/atmos12081060
Chicago/Turabian StyleMorrissey, Karyn, Ivy Chung, Andrew Morse, Suhanya Parthasarath, Margaret M. Roebuck, Maw Pin Tan, Amanda Wood, Pooi-Fong Wong, and Simon P. Frostick. 2021. "The Effects of Air Quality on Hospital Admissions for Chronic Respiratory Diseases in Petaling Jaya, Malaysia, 2013–2015" Atmosphere 12, no. 8: 1060. https://doi.org/10.3390/atmos12081060
APA StyleMorrissey, K., Chung, I., Morse, A., Parthasarath, S., Roebuck, M. M., Tan, M. P., Wood, A., Wong, P.-F., & Frostick, S. P. (2021). The Effects of Air Quality on Hospital Admissions for Chronic Respiratory Diseases in Petaling Jaya, Malaysia, 2013–2015. Atmosphere, 12(8), 1060. https://doi.org/10.3390/atmos12081060







