Abstract
The effects of charged solar particles hitting the Earth’s magnetosphere are often harmful and can be dangerous to the human organism. The aim of this study was to analyze the associations of geomagnetic storms (GSs) and other space weather events (solar proton events (SPEs), solar flares (SFs), high-speed solar wind (HSSW), interplanetary coronal mass ejections (ICMEs) and stream interaction regions (SIRs)) with morbidity from acute myocardial infarction (AMI) and mortality from ischemic heart diseases (IHDs) during the period 2000–2015 in Kaunas (Lithuania). In 2000–2015, 12,330 AMI events (men/women n = 6942/5388) and 3742 deaths from IHD (men/women n = 2480/1262) were registered. The results showed that a higher risk of AMI and deaths from IHD were related to the period of 3 days before GS—a day after GS, and a stronger effect was observed during the spring–autumn period. The strongest effect of HSSW was observed on the day of the event. We found significant associations between the risk of AMI and death from IHD and the occurrence of SFs during GSs. We also found a statistically significant increase in rate ratios (RRs) for all AMIs and deaths from IHD between the second and fourth days of the period of ICMEs.
1. Introduction
Intense solar activity results in solar flares, coronal mass ejections (CMEs), and high-speed solar wind (HSSW) streams. These events can generate geomagnetic storms (GSs). A number of studies have shown that solar and geomagnetic activities (GMAs) affect a wide range of human behavioral and health outcomes, with the nervous and cardiovascular systems being the most clearly impacted. However, the specifics of the biological mechanisms in animals and humans are not yet completely understood [1,2,3].
The effects of charged solar particles hitting the Earth’s magnetosphere are often harmful and can be dangerous to the human organism. Electromagnetic radiation has an effect on the specific acute conditions of the patients’ brain, nerves, or heart. Most studies linked to the space weather–human health associations focused on the effects of GSs on the cardiovascular system [4,5,6]. On days when GSs occur, changes in blood clotting, sedimentation rates, and the human pulse have been observed [7,8]. Studies have shown that GS increased the risk of acute myocardial infarction (AMI) and stroke [9,10,11,12]. Apart from this, the effects on human cardiovascular system were detected 2–3 days before GS and during the recovery GS phase [13,14,15,16,17,18]. Some weather pattern or stratospheric conditions such as quasi-biennial oscillation (QBO) may be influenced by GSs. The risk of AMI was positively associated with the GS due to stream interaction regions with a lag of 0–2 days during the east QBO phase and was negatively associated with them during the west QBO phase [19]. The correlations of blood pressure and heart rate with GMAs in young and healthy populations were stronger during special weather conditions [20].
Statistically significant associations were found between other space weather events such as the solar proton events (SPEs), HSSW, solar flares (SFs), and the solar wind interaction area (stream interaction regions (SIRs)) and human health. According to J. Venclovienė et al., SPEs increase the risk of emergency admission for AMIs, and the effect of GSs on the risk of AMI is stronger if a GS occurs in conjunction with SPEs [21]. The risk of ventricular fibrillation during hospital admission due to acute coronary syndrome was associated with stream interaction regions (SIRs) and a lag of 0–3 days [22]. The days of the arrivals of high-speed plasma streams during stronger SIRs and 1–2 days before–after were associated with a higher rate of AMI [19]. Statistically significant correlations between the daily number of C-class SFs, ≥M-class SF, and CMEs and arrhythmias were found [23].
During GSs, blood clotting increases because of the activated platelet function, and this results in the increased number of patients with ischemic heart disease (IHD). AMI events occurring during magnetic storms and greater solar activity are characterized by a more severe course of IHD, complications, and more frequent cases of death [19]. There are no studies about the effect of HSSWs and SIRs on the risk of IHD.
There have been few comparisons of the results of studies on the possible effects of the main constituents of space weather related to changes in geomagnetic activity and the occurrence of geomagnetic storms (interplanetary coronal mass ejections (ICMEs), SPEs, SFs, HSSW, and SIRs) on humans (especially by sex). Knowledge about the relationship between the aforementioned factors and human health would allow for better preparedness for any future space weather events and their impacts. The success of these measures depends on the understanding of the basic processes of space weather impacts on the Earth and humans.
The easiest approach for studying correlations between GMAs and some other process requires access to parameter measurements recorded over long time periods (for instance, statistical data from medical institutions, long-term sociological data, dynamics of stock market indices, etc.). To establish correlations, these series of observations can be juxtaposed with indices of GMAs, which can be found from open access sources. The relative simplicity of such studies has led to the production of a vast number of publications.
The aim of this study was to analyze the associations of GSs and other space weather events that cause GSs (interplanetary coronal mass ejections (ICMEs) and SIRs) or are associated with the strength of GSs (SPEs, SFs, and HSSW) with morbidity from AMIs and mortality from IHD during the period 2000–2015.
2. Material and Methods
This study was conducted in Kaunas city, which has a population of about 286,000 and is located in Central Lithuania (geographic coordinates: 54°53′ N; 23°58′ E). In the present study, we focused on the period 2000–2015. This study was carried out based on the data of the IHD register (from 1983) in Kaunas city, which were gathered in compliance with the recommendations of the project MONICA (Monitoring of Trends and Determinants in Cardiovascular Disease) [24]. The IHD register is run by a group of scientists at the Laboratory of Population Studies, Institute of Cardiology, the Lithuanian University of Health Sciences. The IHD register included Kaunas inhabitants aged 25–64 years, whose data were verified based on the MONICA project protocol recommendations, and those aged ≥65 years, whose data were not verified. The main data sources were as follows: hospital statistical forms of discharged patients, hospital records, outpatient records, medical death certificates, and protocols of path anatomical and forensic investigation [24]. The study population comprised all Kaunas populations aged 25 years and more, who were diagnosed with AMI or who died due to IHD (patients who did not survive up to 28 days with a diagnosis of AMI) (ICD-10 codes I20–I25). The term “AMI” covers all non-fatal initial and repeated AMI events. While performing data analysis, AMI and deaths from IHD (fatal AMI) were evaluated in subject groups by sex and age. The study population was stratified into two age categories: 25–64 and ≥65 years. During the period 2000–2015, 12,330 AMI events (excluding deaths events) (male/female n = 6942/5388) and 3742 deaths events from IHD (male/female n = 2480/1262) were registered. Total indicates mean AMI and deaths from IHD together. Table 1 depicts the distribution of events of AMI and deaths from IHD by sex and age.

Table 1.
Distribution of events of acute myocardial infarction (AMI) and deaths from ischemic heart disease (IHD) by sex and age.
The Solar Cycle and Space Weather Events
One of the main solar activity cycles lasts about 11 years. During this cycle, the number of sunspots, related GMA, and the quantity of high-energy protons are changing. The most common and the longest available index of solar activity is the sunspot number, which is a synthetic index and is useful for the quantitative representation of the overall solar activity outside the grand minimum. During the grand Maunder minimum, however, it may give only a clue about solar activity whose level may drop below the sunspot formation threshold. [25].
In the present study, we focused on the period that coincided with solar cycle No. 23 and a part of No. 24. The figure below shows the monthly variation in the daily mean sunspot number, solar wind speed, and the Ap index (Ap-index provides a daily average level for geomagnetic activity) (Figure 1A), and the annual rate of the days of ICMEs, SPEs, X-class SFs, and high-speed plasma streams (HSPSs) (Figure 1B).
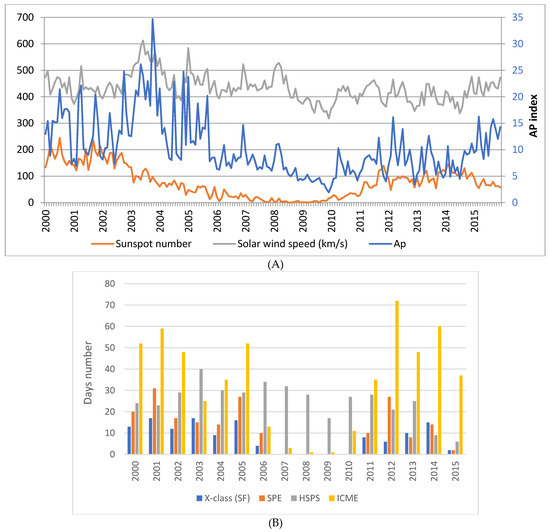
Figure 1.
(A) The monthly variation in the daily mean sunspot number, solar wind speed, and the Ap index; (B) the annual rate of the days of interplanetary coronal mass ejections (ICMEs), solar proton events (SPEs), X-class solar flares (SFs), and high-speed plasma streams (HSPSs).
In this study, the X-class SFs, SPEs, GSs, HSSW, and the arrivals of high-speed plasma streams (HSPSs) during SIRs with maximal solar wind speed (SWS) >500 km/s were employed as space weather events. In our study, SPEs were defined as the daily flux of solar proton >10 MeV energy over 10 proton flux units (pfu). GSs were defined as the Ap index (the daily mean value of 3 h Ap indices) ≥30 nT [26]; this definition is used by the National Oceanic and Atmospheric Administration Space Weather Prediction Center. The Ap index characterizes how intense the planetary magnetic activity is, especially at sub-auroral mid-latitudes [27,28]. The Ap index is defined by using the 3 h standardized K indices from 13 observatories at corrected geomagnetic latitudes between 44° and 60°. The standardization of the K indices is performed to account for the time-of-year and UT response; the Niemengk station (52.04° N) is chosen as the reference station (as its latitude is close to that of Kaunas city (52.38° N). In this study, HSSW was defined as the daily mean SWS over 530 km/s. The cut-off 530 km/s was detected by using the classification tree method. The space weather data were downloaded from websites (Table 2).

Table 2.
Description of space weather data.
In our previous work [19], the daily AMI rate was negatively associated with air temperature and the QBO phase, and was positively associated with a high atmospheric pressure, a higher wind speed, a higher North Atlantic Oscillation (NAO) index, SW dynamic pressure with a lag of 4 days, and the mean SWS with a lag of 3–7 days. These environmental variables were included in the multivariate models. The values of daily NAO indices were obtained from the National Oceanic and Atmospheric Administration database [35]. Monthly QBO indices were downloaded from the database of the Climate Data Center [36].
3. Statistical Analysis
Statistical data analysis was carried out by using SPSS 20 software (IBM Corp. Armonk, NY, USA). Correlations between continuous predictors were assessed by using Spearman’s correlation coefficient. As the daily numbers of medical records Yt are a non-negative count variable, we suppose that Yt followed the Poisson distribution with mean λt, depending on predictor variables. The associations between the daily space weather conditions and the risk of AMI morbidity and mortality from IHD were evaluated by using the multivariate Poisson regression model, which was specified as [19]
where X(1), X(2),…, X(k) are predictors, and β1, β2, …, βk are regression coefficients. In Poisson regression, the exp(βi) is defined as the adjusted (for the remaining predictors) rate ratio (RR), i = 1, 2,…,k.
We analyzed the impact of X-class SFs, ICMEs, GSs, SPEs, HSSW, and HSPSs by including them as binary variables (1—the day of the event, and 0—the day without of the event) in the multivariate model with covariates: the quadratic trend of the long-term time, the month and the day of the week (categorical predictors with the categories Monday, …, Sunday, and holidays not coinciding with weekends), air temperature, both low and high atmospheric pressure (respectively, >1021 hPa and <1007 hPa), high wind speed (>5.85 m/s), the NAO index over the 75th percentile, the QBO phase, solar wind dynamic pressure with a lag of 4 days, and the mean solar wind speed with a lag of 3–7 days (in the models without HSSW). These variables of solar wind and the aforementioned weather variables were statistically significant in the model for all AMIs conceived during the period 2000–2012. The effects of meteorological variables were presented in an earlier publication [19].
We also analyzed how the rate ratios (RRs) of AMI and death from IHD varied 1–3 days after the event (lag 1–3 days). For this purpose, the variable reflecting the lag (from 0 to 3) of the event was included in the model for total AMI and death from IHD as a categorical variable; other days were used as the reference category. If the time period between two successive ICMEs was less than 3 days, then we analyzed these ICMEs and days between them as a single event. Additionally, we analyzed the effect of 1–3 days before (lags −3; −2; and −1) high-speed plasma streams, SPEs, the period of ICMEs, and the effect of 1–3 days before the stormy period, defined as the duration of GS and the period between two successive GS if this period lasted 1–3 days. Based on the regression coefficients and their p-values for each lag, we created new binary variables as the presence of a space weather event during the period of the selected lags without gaps. The optimal delay was selected using the Akaike information criterion.
As the effect of geomagnetic activity on some weather variables was stronger in winter, and the number of days of GS had a stronger seasonal variation, to assess the effect of GS, we performed the analysis during different seasons. Apart from this, we evaluated the combined effects (the combination of two factors) of the space weather variables. The effects of the selected space weather variables were analyzed separately for males and females as well as for younger and elderly subjects.
To confirm the statistical associations between space weather and acute health events, we performed a set of superposed epoch analyses for the response of the daily rates and RRs of AMI and death from IHD on the key days defined by the categories of the selected space weather variables. The superposed epoch analysis was performed for GS, ICME, HSPS, and SPE events.
For testing statistical hypotheses, the significance level 0.05 was used. If p-value (the probability that we would observe a more extreme test statistic in the direction of the alternative hypothesis, if the null hypothesis is true) was <0.05, we rejected a null hypothesis. For testing multiple hypotheses, the results of Simes (1986) [37] can be used. Suppose there are n hypotheses (H1, H2, …, Hn), and the overall rate of type I error is α. We can reject all Hi, when pi ≤ iα/n for i = 1, 2, …, n, where pi is the p-value of the test statistics of Hi, i = 1, 2, …, n, and pi is the ith smallest of the p-values.
To assess the impact of environmental variables, we used adjusted rate ratios (RRs), their 95% confidence intervals (CI), and p-value of coefficients in the multivariate Poisson regression model. We did not present p if p >0.5 and did not present the RRs for those outcomes (all AMI, non-fatal AMI, or deaths from IHD) for which p-values in all groups were >0.5.
4. Results
During the period 2000–2015, GSs occurred on 310 (5.3%) days. Most commonly, GSs were observed in autumn and least commonly in winter (2.9%) (Table 3). SPEs were observed on 195 (3.3%) days. SPEs were also most commonly observed in autumn, and least commonly, in winter (Table 3). The rate of ICME days was lower in winter. During the studied period, one or more X-class SFs were observed on 129 days. The days when the most powerful X-class SF (>X10 intensities) were registered were 3 April, 2001, 15 April 2001, 28–29 October 2003, 4 November 2003, and 7 September 2005. HSSWs were observed on 1003 days (Table 3).

Table 3.
Number and percentage of the days with space weather events by different seasons.
During the studied period, low positive correlations of the Ap index and SWS and air temperature and the NAO index were observed. Higher correlations between these variables were observed during winter (Table 4).

Table 4.
Correlations between weather and space weather variables during all the study period and in winter.
A higher daily rate of AMIs and deaths from IHD (but non-significantly) was observed three days before the period of successive GSs and on days of GS and 1 day after the period of GSs. This period was statistically significantly associated with an increase in RR for all AMI (RR = 1.06, 95% CI 1.01–1.11), p = 0.01 and non-fatal AMI (RR = 1.06, 95% CI 1.01–1.12), p = 0.014, all AMI in females (RR = 1.08, 95% CI 1.01–1.15), p = 0.024, and for deaths from IHD in females aged ≥65 years (RR = 1.23, 95% CI 1.03–1.47), p = 0.02.The analysis of the RRs of AMI performed during different seasons showed a stronger effect of GSs with a lag of 0–1 day during summer. The analysis also showed the effect of GSs with a lag of −3–1 day on non-fatal AMI, especially during summer and spring. An increase in the risk of AMI was not related to the time of 3 days before GS, days of GS, and the day after GS during winter (Figure 2).
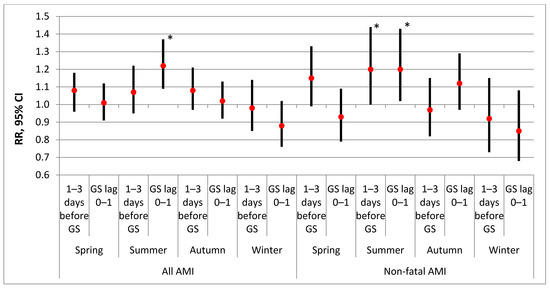
Figure 2.
The effect of geomagnetic storm (the period of 3 days before GS, days of GS, and 1 day after GS) on the risk of AMI by different seasons. * p < 0.05.
During spring–autumn, the periods of 3 days before GS, days of GS, and 1 day after GS were associated with an increase in RR for all AMI and non-fatal AMI in the total subgroup, for all AMI in females aged ≥65 years, for non-fatal AMI in males and males aged 25–64 years, and for deaths from IHD in females aged ≥65 years (Table 5). Apart from this, during spring–autumn, the effects of both “3 days before GS” and “the days of GS and 1 day after GS” on the risk of AMI were found (RRs were, respectively, 1.09 (95% CI 1.02–1.16, p = 0.012) and 1.07 (95% CI 1.00–1.14, p = 0.037). We analyzed the interaction between the winter period and the variable reflecting the effect of GS. For total AMI, AMI in males, and non-fatal AMI in males, the RRs for the interaction term was lower than 0.90, and the p-values fluctuated between 0.065 and 0.070. No statistical significance was found in females for AMI or for death from IHD. Only in males aged ≥65 years, the RR was statistically significant (RR = 0.72, p = 0.014)

Table 5.
The effect of geomagnetic storm (the periods of 3 days before GS, days of GS, and 1 day after GS) on the risk of AMI and death from IHD during spring–autumn by sex and age group.
We found significant associations between the risk of AMI and death from IHD and the occurrence of SFs during GSs. The evaluation of the impact of the days of SFs with a lag of 0–1 day occurring during GSs and SFs occurring 1 day after the period of Ap ≥ 30 on the risk of all and non-fatal AMIs showed an increase in RR for all AMI in males aged 25–64 years. On days of SF with a lag of 0–2 coincident with days of GS with a lag of 1 day, RR increased for deaths from IHD in all patients and in males (Table 6). In case of GS lasting several days, a stronger effect of SF occurring during GS (especially in its initial phase, before the peak) was found.

Table 6.
The effect of X-class solar flares (days of SFs with a lag of 0–1 day during GSs or SFs 1 day after the period of GSs) on the risk of AMI and the effect of SFs with a lag of 0–2 coincident with days of GSs with a lag of 1 day on deaths from IHD during the whole studied period by sex and age group.
We found a statistically significant increase in RRs for all AMI and deaths from IHD between the second and fourth days of the period of ICMEs (successive ICMEs and 1–2 days between them). The effect was stronger for females, especially for those aged ≥65 years (Table 7).

Table 7.
The effect of ICMEs (the period of days 2–4 of ICMEs) on the risk of AMIs and deaths from IHD by sex and age group.
The strongest effect of HSSW was found on the day of the event. The effect of HSSW was associated with an increase in RR for all AMI. AMI in all males and males aged ≥65 years, for non-fatal AMI in all males and males aged ≥65 years, and in females aged 25–64 years (Table 8).

Table 8.
The effect of HSSW (daily solar wind speed >530 km/s) on the risk of AMIs and deaths from IHD by sex and age group.
After the quadratic trend was included in the model, no significant effect of HSPS on an increase in RR for AMI was found (for all subgroups, p > 0.5). The effect of HSPS with a lag of −3 to 3 days was associated with an increase in RR for all IHD and IHD in all males and males aged 25–64 years (Table 9).

Table 9.
The effects of HSPSs (lag −3 to 3 days) and SPEs (lag 1–3 days) on the risk of death from IHD during the whole period by sex and age group.
No significant effect of SPEs on the RRs for AMIs was found (all p > 0.5). The effect of SPEs was associated with an increase in RR for death from IHD in all patients, in females, and in females aged ≥65 years (Table 8). The effect of SPEs with a lag of 1–3 days confirmed the results of the superposed epoch analyses (Figure 3B).
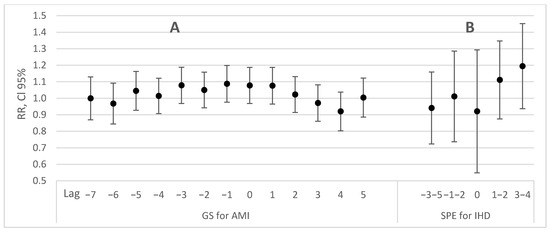
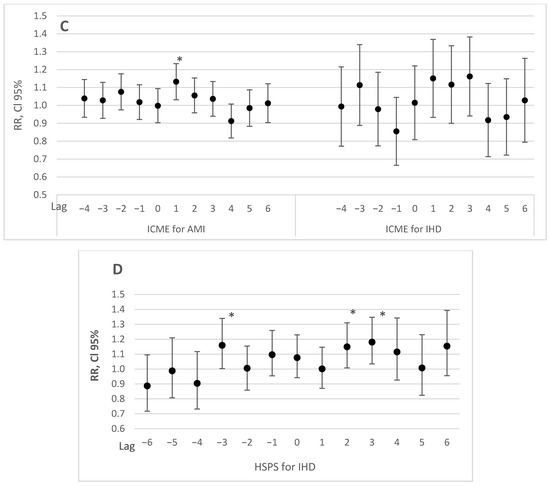
Figure 3.
The superposed epoch analyses of the rate ratios for AMI and death from IHD with the key days being the GSs (A), SPEs (B), ICMEs (C), and HSPSs (D) (RRs with 95% CI in the multivariate model). Zero corresponds to the day of the onset of the stormy period, the period of ICME, HSPS, and SPE. * p < 0.05.
The results of the superposed epoch analyses (Figure 3) confirmed the observed effects of the period of three days before GS—the onset of GS and the effect of days 2–4 of ICMEs on the risk of AMI and deaths from IHD. An increase in RRs for death from IHD was found on days 1–4 after the onset of SPEs (Figure 3B) and on the third day before HSPS (Figure 3D). There is another peak (increase) on the third day before the onset of the ICMEs period (Figure 3C). This is the time of the onset of CMEs, and it is associated with a small peak on day ‘−3’ in Figure 3A, presenting the effect of GS. Consequently, the result that “the risk was increased” from day −3 to day 1 of GS suggests a relation between this time period and the time of the start of the solar events and the time of their propagation from the Sun to the Earth. We note that, in most cases, these strong CMEs and ICMEs were accompanied by simultaneous flare emissions. Thus, radiations (e.g., X-rays, UV), energetic particles (e.g., electrons) and electromagnetic waves (e.g., radio) arrive on Earth very quickly. It is probable that these emissions had some influence on the risk of death from IHD, albeit no significant effect was found.
The multivariate models created with several significant weather variables showed a statistically significant effect of HSSW on AMIs and non-fatal AMIs in men, a significant effect of GS on non-fatal AMIs, and a significant effect of ICME on the risk of AMI and death from IHD in females aged ≥65. The results of the combined effect of space weather variables are presented in Table 10. Both GSs with a lag of (−3–1) days and the period between the second and fourth days of the period of ICMEs were associated with the risk of total AMI (according to Simes’ theorem [37] with n = 2 and cut-off for p-values 0.05 and 0.025). Both ICMEs, SPEs, and HSPS were associated with the risk of death from IHD (according to Simes’ theorem [37] with n = 3 and cut-off for p-values 0.05, 0.0333, and 0.01667). The risk of death from IHD was associated with both SF occurring during GS and HSPS in males, and with both ICMEs and SPEs in females (Table 10).

Table 10.
Multivariate associations between the occurrence of AMI and death from IHD and space weather variables.
5. Discussion
The results obtained in our research suggest that a higher risk of AMI morbidity and mortality from IHD often coincided with the most expressed space weather variations. Depending on the different models used, many statistically significant relationships were found in different subgroups between some space weather events such as GS, ICMEs, X-class SF occurring during GS, SPE, HSSW, and the arrivals of high-speed plasma streams during SIRs, and AMI morbidity and mortality from IHD in Kaunas region during the period 2000–2015. In each case, the statistically significant relationship was different, and is described in more detail in the Results and Discussion parts. The current study revealed that the risk of AMI morbidity and mortality from IHD was significantly increased on the days around the days of impact over the threshold of space weather, but the effects depended on age and sex.
Our results showed that the periods of 3 days before the stormy period, days of GS, and 1 day after GS were associated with an increase in RRs. The effects on humans before GS could be explained by solar heliospheric disturbances before the onset of GS. During the studied period, the three days before the stormy period, a higher mean value of solar wind density and a higher rate of X-class SF, SPEs, and ICMEs was observed. The cause of the pre-stormy effect was more widely discussed in [21].
Comparing our current results with those of our previous study [18] with a similar methodology but a different period, we found that trends in many cases remained similar. In both studies, the highest GS-related risk of non-fatal AMI was observed in younger males, while females ≥65 years of age had the highest risk of death from IHD.
Meanwhile, in a similar study, J. Venclovienė et al. (2020) determined that a higher risk of AMI was positively associated with active-stormy local GMA. The risk of AMI positively associated with the GS due to stream interaction regions with a lag of 0–2 days during the east QBO phase (RR = 1.10, p = 0.046) and was negatively associated with them during the west QBO phase (RR = 0.82, p = 0.024) [19].
We found a stronger effect during the period spring–autumn. The results of the associations between humans’ physiological variables and GMAs in young and healthy population showed that if the air temperature was below 6 °C, there were significant correlations of Kp indices with diastolic blood pressure (negative) and with heart rate (positive); for the whole studied period, the correlations were non-significant [20]. According to previous authors’ results, we can presume, that during the cold period, the human cardiovascular system is more responsive to higher GMA, and this is one of the reasons why patients seek early contacts with medical professionals. Therefore, AMI and deaths from IHD during GS occurred less frequently in winter. However, the results obtained by Kleimenova et al. (2008) showed that more than 95% of the winter storms were associated with an increase in hospital admissions due to AMI, but only about 3% of the summer magnetic storms showed the same association. The results of Kleimenova et al. (2008) are not in line with our results. However, they were obtained during the period 1979–1981, during the maximum of the 21st solar cycle [38]. During the 20th and the 21st solar cycles, the rates of days of GSs were similar in winter and non-winter periods, and only during both the 23rd and the 24th solar cycles, was the rate of days of GSs statistical significantly lower in winter as compared to the non-winter period. It is probable that a lower rate of days of GS during winter resulted in a weaker effect of GSs during winter.
We found that there was an effect of GS on the risk of deaths from IHD only in females aged ≥65 years. In a study performed in 263 USA cities, a significant association was found between daily geomagnetic disturbances (GMD) assessed by Kp indices and total mortality from cardiovascular diseases (CVDs) and deaths from myocardial infarction (MI) [39]. In winter, the effects were even stronger when the authors adjusted the models for 24 h particulate matter (PM2.5). We had no data of PM2.5 for the whole studied period, but the inclusion of the daily NO2 concentration which strongly correlated with PM2.5 did not show any changes in the effects of GS [39]. However, adjusting for the effect of ICME, the effect of GS on the risk of deaths from IHD was observed only in females aged ≥65 years.
When acute vascular events were excluded, the main cause of death in most patients was related to electrical heart instability and heart rhythm disturbances (ventricular tachycardia, fibrillation, complete atrioventricular block, and electromechanical dissociation) [4]. Some of the mechanisms whereby GMA influences human health are associated with a decrease in heart rate variability [12,40], an increase in blood pressure [41,42], and a decrease in melatonin levels [43,44]. According to Dimitrova et al., GMA levels and sex did not reveal a statistically significant difference in the reaction of arterial blood pressure (BP) of men and women to local and global GMA changes. Nevertheless, the post hoc analysis indicated that women possibly had a higher sensitivity. The arterial BP of men did not differ significantly, even within the combinations of separate global GMA levels, whereas the arterial BP of women for GMA levels 4 and 5 differed significantly from that observed for levels 1–3. For the SBP, there was also a significant difference for levels 4 and 5 [42]. These factors increased the risk of myocardial ischemia and other CVDs [45]. Among the mechanisms whereby GMA influences human health, the one mentioned most frequently is that involving melatonin and the Schumann resonance [5,46]. In addition, GS sharply disturbs the rhythm of the external synchronizer of biological rhythms [47] and is therefore accompanied by an adaptation stress reaction of the organism [48]. Melatonin plays a central role in the regulation of diurnal variation of many human systems. Many cardiovascular variables associated with prognosis after acute coronary syndromes (ACS)—such as heart rate, blood pressure, and platelet endothelial function—exhibit diurnal variation; a circadian clock also exists in cardiomyocytes [49,50]. Specific links between melatonin and CVD have been indicated [50]. Human melatonin production decreases in the presence of coronary artery disease [51] and during AMI [50]. Melatonin acts as a potent antioxidant agent, reducing myocardial damage induced by ischemia reperfusion [50]. It has been found that greater reductions in melatonin production are observed in patients with a higher risk of AMI or sudden death [52].
Meanwhile, we should not forget that the differences that can be observed between different studies could be explained by the fact that GSs have different origins. It is quite probable that physiological reactions are not directly related to GMAs and, respectively, to the intensity of the storms, but also depend on the sources of solar events [15].
We detected significant effects of SF occurring during GS on all AMI and on deaths from IHD, especially among males. For deaths from IHD in males, this effect was statistically significant, adjusting for other space weather variables. The effect of SF can be explained by their effect on the first modes of the Schumann resonance (SR). During high-energy solar proton events, the solar X-ray burst preceding proton precipitation was accompanied by an increase in first-mode frequency [53]. X-class SF affect the ionosphere. The change in ionospheric parameters is related to changes in the parameters of the Schumann resonance and the changes in the atmospheric electricity, and thus may explain a greater part of the variability in the number of deaths from AMI [54].
In our study, the strongest effect of HSSW was found on the day of the event. This effect of HSSW was associated with an increase in RRs for all AMIs and AMIs in males aged ≥65 years, and for non-fatal AMI in males aged ≥65 years and in females aged 25–64 years. In the previous studies performed during the period of maximum solar or GMA during the 23rd solar cycle, the days of HSSW defined as SWS > 600 km/s were associated with a deterioration in cardiovascular health. During days of HSSW, the risk of ACS in patients with diabetes was increased by 1.95 times (p < 0.001), and in patients with the metabolic syndrome—by 1.86 (p = 0.001) times, as compared to days without either of these events or 2 days prior to or after them [55]. The risk of ACS in patients with chronic atrial fibrillation was associated with HSSW (lag 0–3 days, OR = 1.39, p = 0.03). In our study, some effects of the days of SWS > 600 km/s were non-significant, and only on the days of SWS > 530 km/s was there a statistically significant increase in RR. However, our study covered the period of 16 years and included a long period of low GMA.
The effect of SPEs was associated with an increase in RRs for death from IHD in all patients and in females, and was significant, adjusting for other space weather variables. The effect of HSPS with a lag of −3 to 3 days was associated with an increase in RR for death from IHD in all patients and in males, and was significant, adjusting for other space weather variables. A higher hazard ratio (HR) for cardiovascular death in females with ACS on days of SPE and on the second day after SPE was found [45].
High-speed solar wind, ICMEs, SPEs, SIRs, and GS are the main sources of energetic particles—protons, electrons, and heavier ions precipitating into the atmosphere [56,57]. Thus, these space weather events are related to the modulation of both the conductivity of the atmospheric column and the ionospheric potential and affect global electric circuit (GEC) and atmospheric electricity [58]. The effects of SPE, SWS, and HSPS on the risk of AMI and deaths from IHD may be explained by their effect on the flow of the downward current density (Jz) in GEC, affecting meteorology via changes in cloud microphysics [58] because these predictors were positively associated with the energetic particle flux. More discussions about the effect of SWS and SIR on weather and on the risk of AMI are presented in [19]. The direct impact of environmental electric and magnetic fields produced during GMD or other space weather events [59] on the human autonomic nervous system (ANS) may explain their effects on the total CVD and AMI deaths found in our study.
Interactions between GMD with ANS are likely to induce some reactions in the body’s electrophysiology that leads to damage to organ functions and death. Studies have described the mechanisms by which GMD may regulate ANS and body systems via a magneto-reception system [60].
A close alignment between the GMA rhythms and the electrophysiology of the human body has been observed in ultrasound waves from heart structures by echocardiogram, in brain waves by electroencephalogram, and peripheral nerve activity that is controlled by the ANS [45,61].
Resistance of a body to space weather events depends on their effect and intensity. It is especially important at an initial stage of the disease; later, the influence decreases gradually [62] as the human body is capable of adapting to the environmental impact. The impact of the aforementioned factors on human health also depends on sex, age, and general health status [63].
The results obtained in our study showed that the risk of AMI was associated with HSSW in males, especially in those aged ≥65 years, and with ICMEs in females, especially in those aged ≥65 years. The results of the multivariate model showed that the risk of death from IHD was associated with more space weather events: HSPS and SF occurring during GS had an impact in males, and ICME and SPE affected females.
Our results may help in the understanding of the population’s sensitivity under different space weather conditions. The prognostic monitoring of geomagnetic and other space weather variations in hospitals may help to detect the period of a higher risk in patients with cardiovascular problems.
6. Limitations and Strengths
One limitation of this study was that the cases were identified in retrospect, and it is possible that some cases of AMI occurring in Kaunas during the period 2000–2015 were overlooked. However, given the extensive data collection protocol, this number is likely not significant, and should not influence our results.
It is possible that some cases identified and recorded as AMI represented in fact some other pathology rather than an acute myocardial syndrome. This is more likely in the elderly group aged 65 or more, in which both survivors and non-survivors were recorded according to clinical diagnosis, without subsequent verification.
This is less likely in the younger age group (25 to 64 years) because both incident and mortality data were assessed by a combination of symptoms, ECG changes, serum enzyme activity, and autopsy findings.
In our study, we did not adjust for other confounding factors, including physical daily activity, smoking and other behavioral factors, and the effects of other pre-existing diseases (hypertension, diabetes, or previous AMI), air pollution, or medication use. The method of the registration of deaths from IHD strictly followed the protocol and quality control procedures according to the WHO MONICA project criteria.
7. Conclusions
The present study showed that a higher risk of AMI and death from IHD in females aged ≥65 years was related to the period of three days before GS—a day after GS, and a stronger effect was observed during the period spring–autumn. An increase in the risk of all AMIs and deaths from IHD was associated with days of X-class SFs and 1 day after occurring during GS, and a stronger effect was found in men. A higher risk of AMIs was found on days of HSSW (daily solar wind speed >530 km/s). A statistically significant increase in RRs for all AMI and deaths from IHD was found between the second and fourth days of the period of ICMEs (successive ICMEs and 1–2 days between them). The effect was stronger for females, especially for those aged ≥65 years. An increase in the risk of death from IHD was associated with SPEs with a lag of 1–3 days and with the period of 3 days before HSPS—3 days after them.
The effects of GSs, ICMEs, and SPEs was stronger in females, and the effect of H-class SF, HSSW, and HSPS was stronger in males. According to the results of the complex effect of space weather variables, we found that both GS had a lag of −3–1 days and the period between the second and fourth days of ICMEs were associated with the risk of total AMI. The risk of death from IHD was associated with both SFs occurring during GS (X-class SF on or two days after GS) and HSPS (with a lag of −3 to 3 days) in males and with both ICMEs (between the second and fourth days of the period of ICMEs) and SPEs (with a lag of 1–3 days) in females.
Author Contributions
Conceptualization, V.V., J.V. and R.R.; methodology, J.V. and V.V.; data curation, D.L., D.K.-B., R.R. and A.T.; formal analysis, J.V., D.K. and V.V.; investigation, D.L., D.K.-B., R.R. and A.T.; writing—original draft preparation, V.V. and J.V.; writing—review and editing, V.V., J.V., A.T., D.K., D.L., D.K.-B., R.R. All authors have read and agreed to the published version of the manuscript.
Funding
This project has received funding from the European Social Fund (Title: ‘’The Impact of Climate Change on Public Health”, Project no. 09.3.3-LMT-K-712-19-0002) under grant agreement with the Research Council of Lithuania (LMT).
Institutional Review Board Statement
Institutional Review Board Statement: The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Lithuanian Bioethics Committee (No. 14-27, 3 December 2001).
Informed Consent Statement
Not applicable.
Data Availability Statement
Space weather parameters data supporting reported results can be found in National Center for Environmental Information database (https://www.ngdc.noaa.gov/stp/space-weather/solar-data/solar-features/solar-flares/x-rays/goes/xrs/?fbclid=IwAR0yMkbQw-aVuwtCpUtQzeh1LaYD77XmrHJk3AfTqXxpJrSNOHWtODqQWZA, (accessed on 10 December 2020)) also in the National Geophysical Data Center OMNIWEB database (https://omniweb.gsfc.nasa.gov/, (accessed on 10 December 2020)) and Space Radiation Lab at California Institute of Technology (http://www.srl.caltech.edu/ACE/ASC/DATA/level3/icmetable2.htm, (accessed on 10 December 2020)). Acute myocardial infarction database is not publicly available.
Acknowledgments
We thank the Research Council of Lithuania for the grant and for the opportunity to develop this kind of research.
Conflicts of Interest
No conflicts of interest.
References
- Khorseva, N.I. Using psychophysiological indices to estimate the effect of cosmophysical factors (Review). Izv. Atmos. Ocean. Phys. 2013, 49, 839–852. [Google Scholar] [CrossRef]
- Freund, F.; Stolc, V. Nature of pre-earthquake phenomena and their effects on living organisms. Animals (Basel) 2013, 3, 513–531. [Google Scholar] [CrossRef] [PubMed]
- McCraty, R.; Atkinson, M.; Stolc, V.; Alabdulgader, A.A.; Vainoras, A.; Ragulskis, M. Synchronization of human autonomic nervous system rhythms with geomagnetic activity in human subjects. Int. J. Environ. Res. Public Health 2017, 14, 770. [Google Scholar] [CrossRef] [PubMed]
- Stoupel, E. Effect of geomagnetic activity on cardiovascular parameters. J. Clin. Basic Cardiol. 1999, 2, 34–40. [Google Scholar] [CrossRef]
- Palmer, S.J.; Rycroft, M.J.; Cermack, M. Solar and geomagnetic activity, extremely low frequency magnetic and electric fields and human health at the Earth’s surface. Surv. Geophys. 2006, 27, 557–595. [Google Scholar] [CrossRef]
- Díaz-Sandoval, R.; Erdélyi, R.; Maheswaran, R. Could periodic patterns in human mortality be sensitive to solar activity? Ann. Geophys. 2011, 29, 1113–1120. [Google Scholar] [CrossRef]
- Otsuka, K.; Cornélissen, G.; Weydahl, A.; Holmeslet, B.; Hansen, T.L.; Shinagawa, M.; Kubo, Y.; Nishimura, Y.; Omori, K.; Yano, S.; et al. Geomagnetic disturbance associated with decrease in heart rate variability in a subarctic area. Biomed. Pharmacother. 2000, 55, 51–56. [Google Scholar] [CrossRef]
- Azcárate, T.; Mendoza, B.; Levi, J.R. Influence of geomagnetic activity and atmospheric pressure on human arterial pressure during the solar cycle 24. Adv. Space Res. 2016, 58, 2116–2125. [Google Scholar] [CrossRef]
- Villoresi, G.; Breus, T.K.; Dorman, L.I.; Iuchi, N. Effect of interplanetary and geomagnetic disturbances on the increase in number of clinically serious medical pathologies (myocardial infarct and stroke). Biofizika 1995, 40, 983–993. [Google Scholar] [PubMed]
- Gurfinkel, V.S.; Levik, Y.S.; Kazennikov, O.V.; Selionov, V.A. Locomotor-Like movements evoked by leg musclevibration in humans. Eur. J. Neurosci. 1998, 10, 1608–1612. [Google Scholar] [CrossRef] [PubMed]
- Stoupel, E.; Domarkiene, S.; Radisauskas, R.; Abramson, E. Sudden cardiac death and geomagnetic activity: Links to age, gender and agony time. J. Basic Clin. Physiol. Pharmacol. 2002, 13, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Cornelissen, G.; Halberg, F.; Breus, T.; Syutkina, E.; Baevsky, R.; Weydahl, A.; Watanabe, Y.; Otsuka, K.; Siegelova, J.; Fiser, B.; et al. Non-Photic solar associations of heart rate variability and myocardial infarction. J. Atmos. Sol. Terr. Phys. 2002, 64, 707–720. [Google Scholar] [CrossRef]
- Ramón, E.R.; Figueredo, P.S.; Figueredo, S.S. Geomagnetic activity related to acute myocardial infarctions: Relationship in a reduced population and time interval. Geofís. Int. 2004, 43, 265–269. [Google Scholar]
- Kleimenova, N.G.; Kozyreva, O.V.; Breus, T.K.; Rapoport, S.I. Pc1 geomagnetic pulsations as a potential hazard of the myocardial infarction. J. Atmos. Sol. Terr. Phys. 2007, 69, 1759–1764. [Google Scholar] [CrossRef]
- Dimitrova, S.; Mustafa, F.R.; Stoilova, I.; Babayev, E.S.; Kazimov, E.A. Possible influence of solar extreme events and related geomagnetic disturbances on human cardio-vascular state: Results of collaborative Bulgarian–Azerbaijani studies. Adv. Space Res. 2009, 43, 641–648. [Google Scholar] [CrossRef]
- Papailiou, M.; Mavromichalaki, H.; Kudela, K.; Stetiarova, J.; Dimitrova, S. Effect of geomagnetic disturbances on physiological parameters: An investigation on aviators. Adv. Space Res. 2011, 48, 1545–1550. [Google Scholar] [CrossRef]
- Mavromichalaki, H.; Papailiou, M.; Dimitrova, S.; Babayev, E.S.; Loucas, P. Space weather hazards and their impact on human cardio-health state parameters on Earth. Nat. Hazards 2012, 64, 1447–1459. [Google Scholar] [CrossRef]
- Vaičiulis, V.; Radišauskas, R.; Ustinavičienė, R.; Kalinienė, G.; Tamošiūnas, A. Associations of morbidity and mortality from coronary heart disease with heliogeophysical factors. Environ. Sci. Pollut. Res. 2016, 23, 18630–18638. [Google Scholar] [CrossRef] [PubMed]
- Vencloviene, J.; Radisauskas, R.; Vaiciulis, V.; Kiznys, D.; Bernotiene, G.; Kranciukaite-Butylkiniene, D.; Tamosiunas, A. Associations between quasi-biennial oscillation phase, solar wind, geomagnetic activity, and the incidence of acute myocardial infarction. Int. J. Biometeorol. 2020, 64, 1207–1220. [Google Scholar] [CrossRef]
- Ozheredov, V.A.; Chibisov, S.M.; Blagonravov, M.L.; Khodorovich, N.A.; Demurov, E.A.; Goryachev, V.A.; Kharlitskaya, E.V.; Eremina, I.S.; Meladze, Z.A. Influence of geomagnetic activity and earth weather changes on heart rate and blood pressure in young and healthy population. Int. J. Biometeorol. 2017, 61, 921–929. [Google Scholar] [CrossRef]
- Vencloviene, J.; Babarskiene, R.; Slapikas, R. The association between solar particle events, geomagnetic storms, and hospital admissions for myocardial infarction. Nat. Hazards 2013, 65, 1–12. [Google Scholar] [CrossRef]
- Kiznys, D.; Vencloviene, J.; Milvidaitė, I. The associations of geomagnetic storms, fast solar wind, and stream interaction regions with cardiovascular characteristic in patients with acute coronary syndrome. Life Sci. Space Res. 2020, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mavromichalaki, H.; Preka-Papadema, P.; Theodoropoulou, A.; Paouris, E.; Apostolou, T. A study of the possible relation of the cardiac arrhythmias occurrence to the polarity reversal of the solar magnetic field. Adv. Space Res. 2017, 59, 366–378. [Google Scholar] [CrossRef]
- The WHO MONICA Project. Available online: https://www.thl.fi/monica/index.html (accessed on 10 December 2020).
- Usoskin, I.G. A history of solar activity over millennia. Living Rev. Sol. Phys. 2017, 14, 3. [Google Scholar] [CrossRef]
- Palacios, J.; Guerrero, A.; Consuelo, C.; Saiz, E.; Cerrato, Y. Defining scale thresholds for geomagnetic storms through statistics. Nat. Hazards Earth Syst. Sci. Discuss. 2018, 1–17. [Google Scholar] [CrossRef]
- Adebesin, B.O.; Ikubanni, S.O.; Ojediran, J.O.; Kayode, J.S. An investigation into the geomagnetic and ionospheric response during a magnetic activity at high and mid-latitute. Res. J. Appl. Sci. 2011, 6, 512–519. [Google Scholar] [CrossRef][Green Version]
- Lockwood, M.; Bentley, S.N.; Owens, M.J.; Barnard, L.A.; Scott, C.J.; Watt, C.E.; Allanson, O.; Freeman, M.P. The development of a space climatology: 2. The distribution of power input into the magnetosphere on a 3-hourly timescale. Space Weather 2019, 17, 157–179. [Google Scholar] [CrossRef]
- National Center for Environmental Information Database. Available online: https://www.ngdc.noaa.gov/stp/space-weather/solar-data/solar-features/solar-flares/x-rays/goes/xrs/?fbclid=IwAR0yMkbQwNaVuwtCpUtQzeh1LaYD77XmrHJk3AfTqXxpJrSNOHWtODqQWZA (accessed on 10 December 2020).
- The National Geophysical Data Center OMNIWEB database. Available online: http://omniweb.gsfc.nasa.gov/ (accessed on 10 December 2020).
- Space Radiation Lab at California Institute of Technology. Available online: http://www.srl.caltech.edu/ACE/ASC/DATA/level3/icmetable2.htm (accessed on 10 December 2020).
- British Geological Survey. Available online: http://www.geomag.bgs.ac.uk/data_service/data/magnetic_indices/apindex.html?fbclid=IwAR3Rdsot9Sgub6KO6BozpgZY7gIlvOjiTYL6GBGqWqu-6bci3K1_VTTVD3c (accessed on 10 December 2020).
- Institute of Geophysics and Planetary Physics. Available online: http://www.ssc.igpp.ucla.edu/~jlan/ACE/Level3/SIR_List_from_Lan_Jian.pdf (accessed on 10 December 2020).
- Solar-Terrestrial Relations Observatory. Available online: https://stereo-ssc.nascom.nasa.gov/pub/ins_data/impact/level3/LanJian_STEREO_SIR_List.txt (accessed on 10 December 2020).
- National Oceanic and Atmospheric Administration. Available online: https://ftp.cpc.ncep.noaa.gov/cwlinks/ (accessed on 10 December 2020).
- Climate Data Center. Available online: http://www.daculaweather.com/4_qbo_index.php (accessed on 10 December 2020).
- Simes, R.J. An improved bonferroni procedure for multiple tests of significance. Biometrika 1986, 73, 751–754. [Google Scholar] [CrossRef]
- Kleimenova, N.G.; Kozyreva, O.V.; Michnowski, S.; Kubicki, M. Effect of magnetic storms in variations in the atmospheric electric field at midlatitudes. Geomagn. Aeron. 2008, 48, 622–630. [Google Scholar] [CrossRef]
- Zilli Vieira, C.L.; Alvares, D.; Blomberg, A.; Schwartz, J.; Coull, B.; Huang, S.; Koutrakis, P. Geomagnetic disturbances driven by solar activity enhance total and cardiovascular mortality risk in 263 U.S. cities. Environ Health 2019, 18, 83. [Google Scholar] [CrossRef]
- Watanabe, Y.; Cornélissen, G.; Halberg, F.; Otsuka, K.; Ohkawa, S.I. Associations by signatures and coherences between the human circulation and helio- and geomagnetic activity. Biomed. Pharmacother. 2000, 55, 76–83. [Google Scholar] [CrossRef]
- Ghione, S.; Mezzasalma, L.; Seppia, C.; Papi, F. Do geomagnetic disturbances of solar origin affect arterial blood pressure? J. Hum. Hypertens. 1998, 12, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, S.; Stoilova, I.; Yanev, T.; Cholakov, I. Effect of local and global geomagnetic activity on human cardiovascular homeostasis. Arch. Environ. Health 2004, 59, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Weydahl, A.; Sothern, R.B.; Cornélissen, G.; Wetterberg, L. Geomagnetic activity influences the melatonin secretion at latitude 70 degrees. N Biomed. Pharmacother. 2001, 55. [Google Scholar] [CrossRef]
- Burch, J.B.; Reif, J.S.; Yost, M.G. Geomagnetic disturbances are associated with reduced nocturnal excretion of a melatonin metabolite in humans. Neurosci. Lett. 1999, 266, 209–212. [Google Scholar] [CrossRef]
- Vencloviene, J.; Babarskiene, R.; Milvidaite, I.; Kubilius, R.; Stasionyte, J. The effect of solar-geomagnetic activity during and after admission on survival in patients with acute coronary syndromes. Int. J. Biometeorol. 2014, 58, 1295–1303. [Google Scholar] [CrossRef] [PubMed]
- Cherry, N. Schumann resonance and sunspot relations to human health effects in Thailand. Nat. Hazards 2003, 29, 1–11. [Google Scholar] [CrossRef]
- Oraevskiĭ, V.N.; Breus, T.K.; Baevskiĭ, R.M.; Rapoport, S.I.; Petrov, V.M.; Barsukova, Z.V.; Gurfinkel’, I.; Rogoza, A.T. Effect of geomagnetic activity on the functional status of the body. Biofizika 1998, 43, 819–826. [Google Scholar]
- Breus, T.; Baevskii, R.; Chernikova, A. Effects of geomagnetic disturbances on humans functional state in space flight. J. Biomed. Sci. Eng. 2012, 5, 341–355. [Google Scholar] [CrossRef]
- Durgan, D.J.; Hotze, M.A.; Tomlin, T.M.; Egbejimi, O.; Graveleau, C.; Abel, E.D.; Shaw, C.A.; Bray, M.S.; Hardin, P.E.; Young, M.E. The intrinsic circadian clock within the cardiomyocyte. Am. J. Physiol. Heart Circ. Physiol. 2005, 289, 1530–1541. [Google Scholar] [CrossRef]
- Dominguez-Rodriguez, A.; Abreu-Gonzalez, P.; Sanchez-Sanchez, J.J.; Kaski, J.C.; Reiter, R.J. Melatonin and circadian biology in human cardiovascular disease. J. Pineal Res. 2010, 49, 14–22. [Google Scholar] [CrossRef]
- Yaprak, M.; Altun, A.; Vardar, A.; Aktoz, M.; Ciftci, S.; Ozbay, G. Decreased nocturnal synthesis of melatonin in patients with coronary artery disease. Int. J. Cardiol. 2003, 89, 103–107. [Google Scholar] [CrossRef]
- Tengattini, S.; Reiter, R.J.; Tan, D.X.; Terron, M.P.; Rodella, L.F.; Rezzani, R. Cardiovascular diseases: Protective effects of melatonin. J. Pineal Res. 2008, 44, 16–25. [Google Scholar] [CrossRef]
- Roldugin, V.C.; Maltsev, Y.P.; Vasiljev, A.N.; Schokotov, A.Y.; Belyajev, G.G. Schumann resonance frequency increase during solar X-ray bursts. J. Geophys. Res. 2004, 109. [Google Scholar] [CrossRef]
- Podolská, K. The impact of ionospheric and geomagnetic changes on mortality from diseases of the circulatory system. J. Stroke Cerebrovasc. Dis. 2018, 27, 2. [Google Scholar] [CrossRef] [PubMed]
- Vencloviene, J.; Babarskiene, R.M.; Kiznys, D. A possible association between space weather conditions and the risk of acute coronary syndrome in patients with diabetes and the metabolic syndrome. Int. J. Biometeorol. 2017, 61, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Richardson, I.G.; Cane, H.V. Near-Earth interplanetary coronal mass ejections during solar cycle 23 (1996–2009): Catalog and summary of properties. Sol. Phys. 2010, 264, 189–237. [Google Scholar] [CrossRef]
- Sinnhuber, M.; Nieder, H.; Wieters, N. Energetic particle precipitation and the chemistry of the mesosphere/lower thermosphere. Surv. Geophys. 2012, 33, 1281–1334. [Google Scholar] [CrossRef]
- Tinsley, B.A. The global atmospheric electric circuit and its effects on cloud microphysics. Rep. Prog. Phys. 2008, 71. [Google Scholar] [CrossRef]
- Schrijver, C.J.; Mitchell, S.D. Disturbances in the US electric grid associated with geomagnetic activity. J. Space Weather Space Clim. 2013, 3, A19. [Google Scholar] [CrossRef]
- Kirschvink, J.L.; Jones, D.S.; MacFadden, B.J. Magnetite Biomineralization and Magnetoreception in Organisms: A New Biomagnetism; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Caswell, J.M.; Carniello, T.N.; Murugan, N.J. Annual incidence of mortality related to hypertensive disease in Canada and associations with heliophysical parameters. Int. J. Biometeorol. 2016, 60, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Styra, D.; Ušovaitė, A.; Damauskaitė, J.; Juozulynas, A. Leaps in cardiovascular diseases after a decrease of hard cosmic ray flux and atmospheric pressure in Vilnius city in 2004–2007. Int. J. Biometeorol. 2009, 53, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.; Zanobetti, A.; Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S cities. Environ. Health Perspect. 2002, 110, 859–863. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).