Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009
Abstract
:1. Introduction
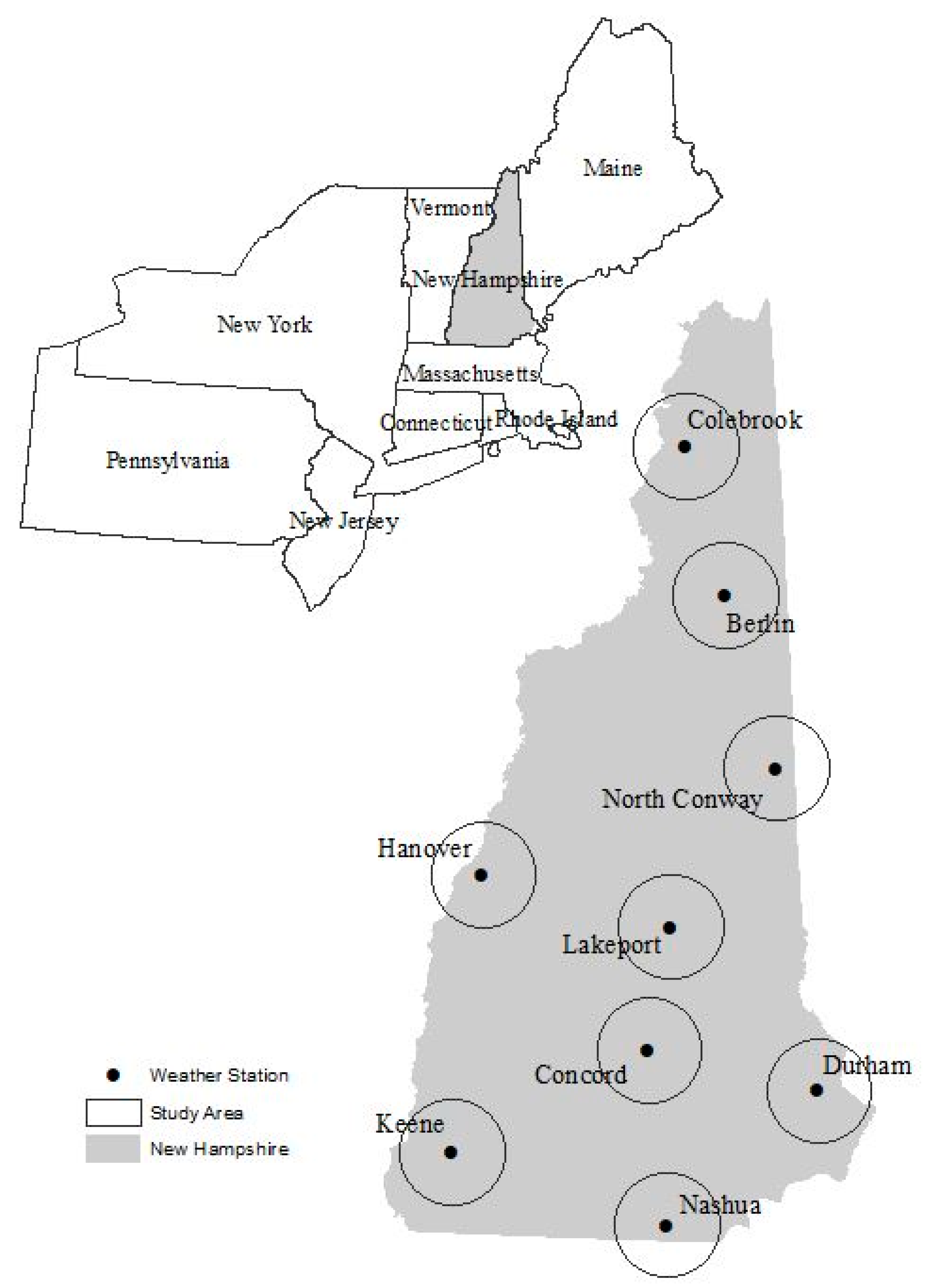
2. Methods
3. Results
3.1. Injury Rates–Primary Health Outcomes
3.2. Injury Rates–Secondary (Environmental) Health Outcomes
3.3. Statistical Relationship between Climate and Health
3.4. Regression Analyses
3.4.1. All-Cause Injury ~ Tmax
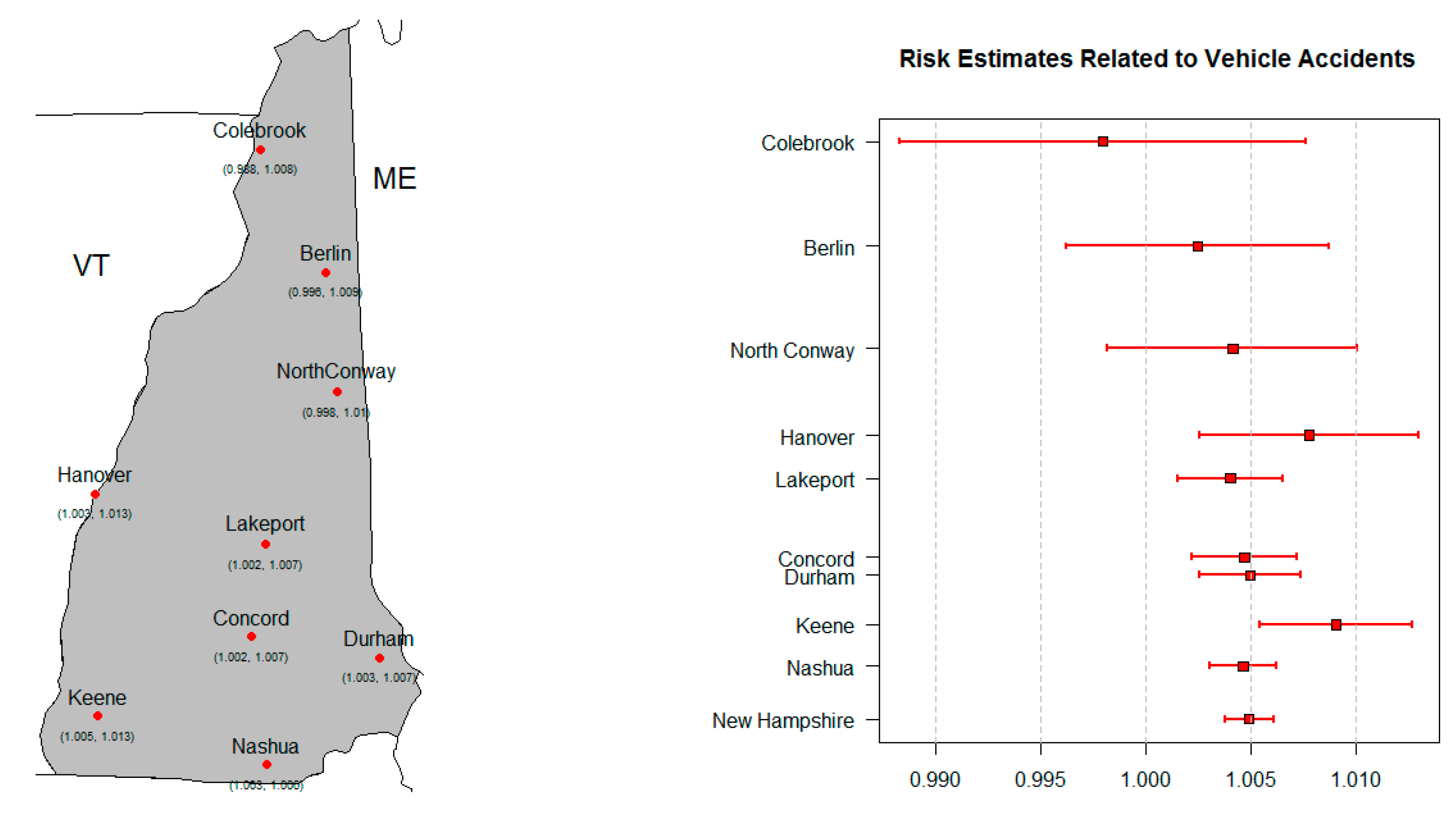
3.4.2. Vehicle Accidents ~ Tmax
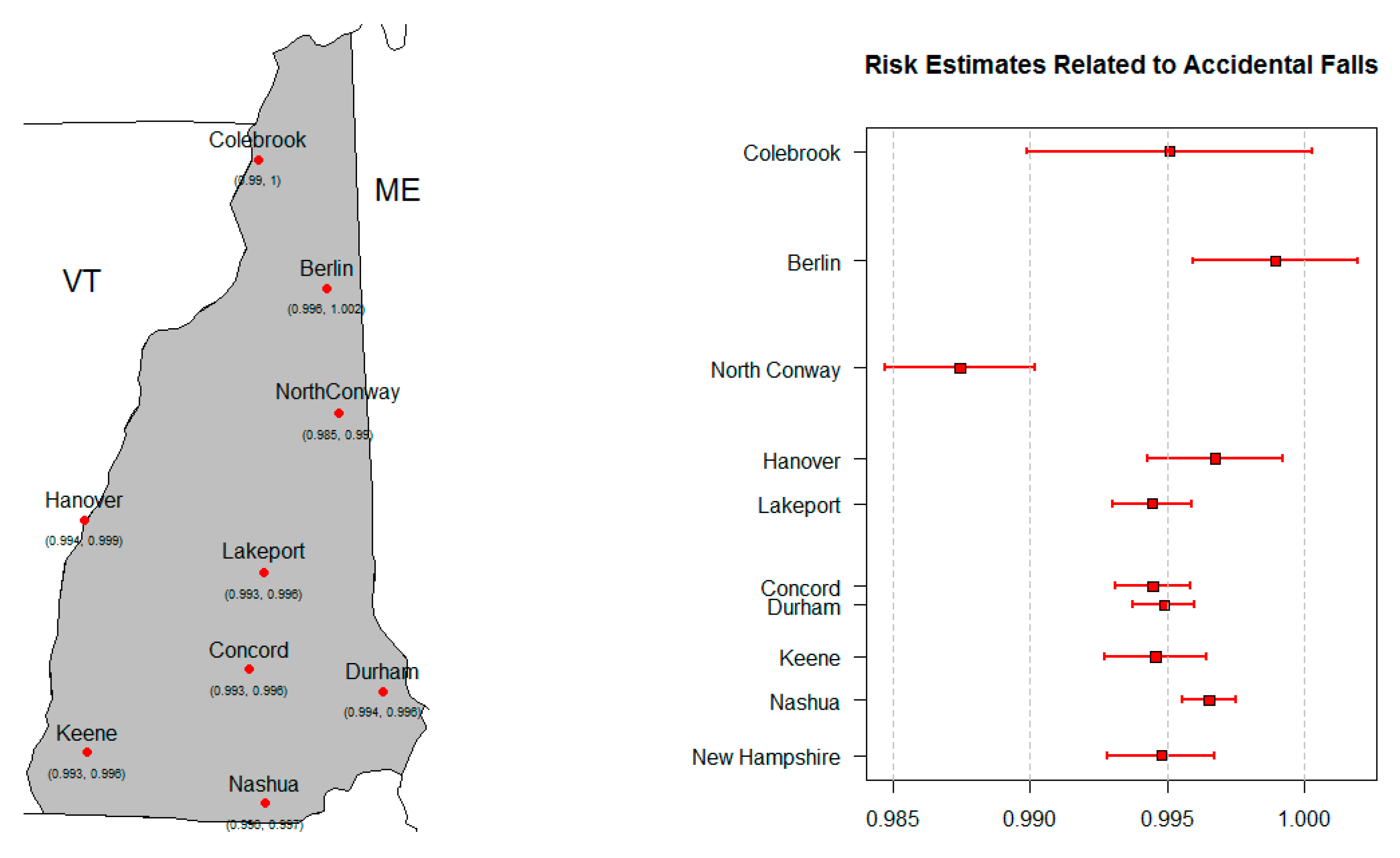
3.4.3. Accidental Falls ~ Tmax
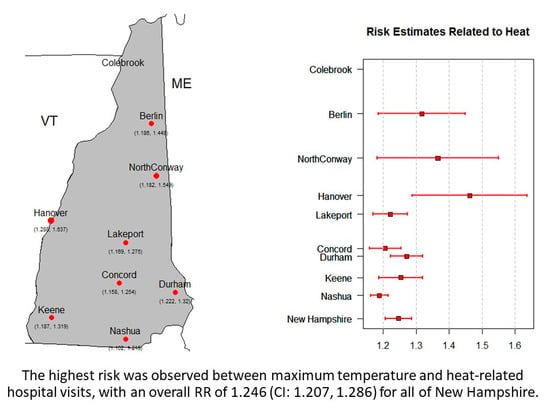
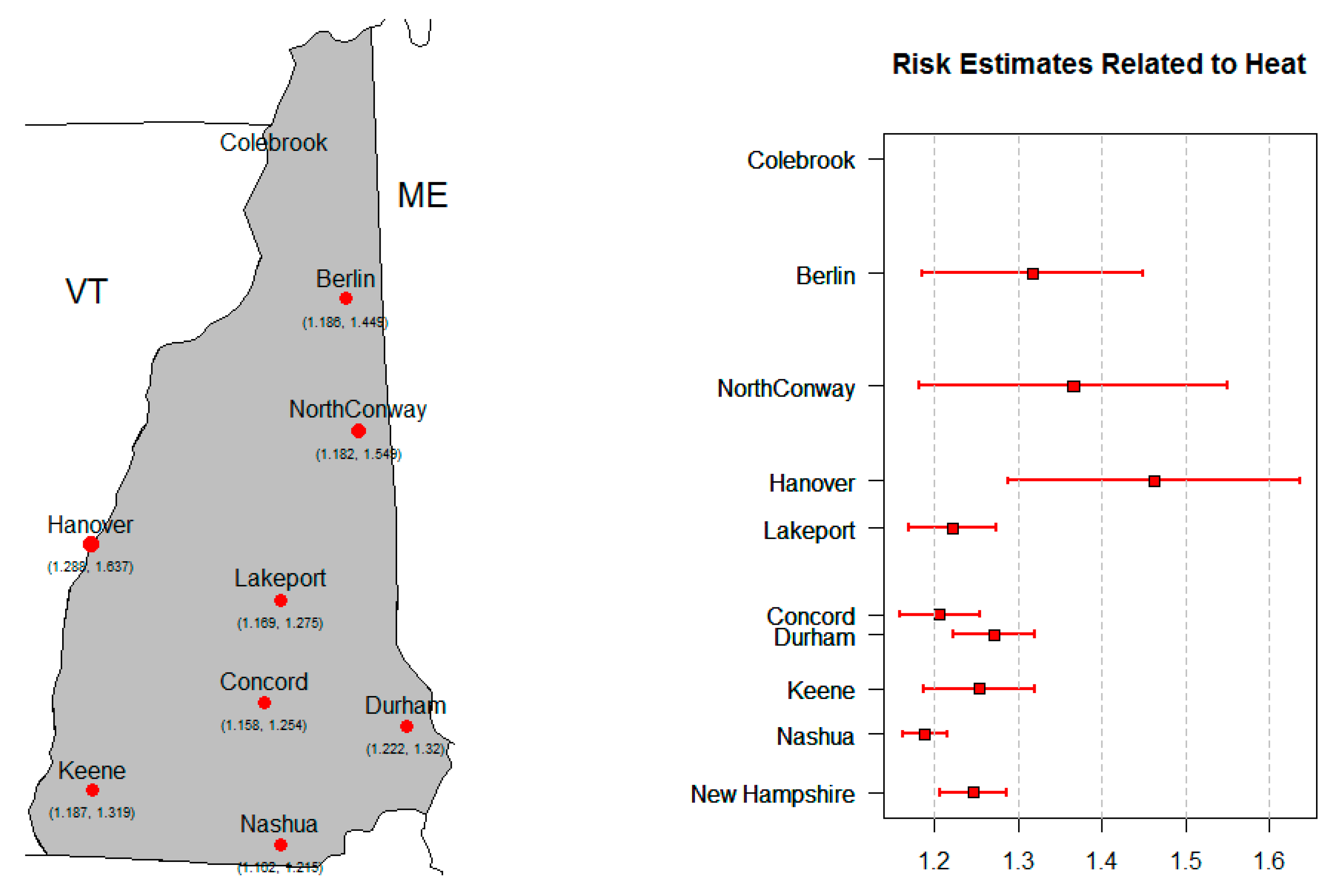
3.4.4. Heat-Related Injury ~ Tmax
4. Discussion
4.1. Injury Rates
4.2. Exposure Metrics
4.3. Relative Risks
4.4. Comparative Studies
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- NCDC. Climate of New Hampshire; NCDC Climate Services Branch Report 7; NCDC: Asheville, NC, USA, 2017.
- Meehl, G.A.; Tebaldi, C.; Walton, G.; Easterling, D.; McDaniel, L. Relative increase of record high maximum temperatures compared to record low minimum temperatures in the U.S. Geophys. Res. Lett. 2009, 36. [Google Scholar] [CrossRef] [Green Version]
- Balbus, J.; Crimmins, A.; Gamble, J.L.; Easterling, D.R.; Kunkel, K.E.; Saha, S.; Sarofim, M.C.C. 1: Introduction: Climate Change and Human Health. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 25–42. [Google Scholar]
- U.S. Global Change Research Program. 2014 National Climate Assessment; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014. Available online: http://nca2014.globalchange.gov/report/our-changing-climate/precipitation-change (accessed on 31 August 2016).
- IPCC. Summary for Policy Makers. In Climate Change The Physical Science Basis; Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Stocker, T.F., Qin, D., Plattner, G.-K., Tignor, M., Allen, S.K., Boschung, J., Nauels, A., Xia, Y., Bex, V., Midgley, P.M., Eds.; IPCC: Geneva, Switzerland, 2013. [Google Scholar]
- Knowlton, K.; Rotkin-Ellman, M.; King, G.; Margolis, H.G.; Smith, D.; Solomon, G.; Trent, R.; English, P. The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environ. Health Perspect. 2009, 117, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Pearson, D.; Malig, B.; Broadwin, R.; Green, R. The effect of high ambient temperature on emergency room visits. Epidemiology 2012, 23, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Kent, S.T.; McClure, L.A.; Zaitchik, B.F.; Smith, T.T.; Gohlke, J.M. Heat waves and health outcomes in Alabama (USA): The importance of heat wave definition. Environ. Health Perspect. 2014, 122, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, E.; Gasparrini, A.; Wang, X.; Chen, H.; Yagouti, A.; Fleury, M.D.; Cakmak, S. Extreme ambient temperatures and cardiorespiratory emergency room visits: Assessing risk by comorbid health conditions in a time series study. Environ. Health 2014, 13, 5. [Google Scholar] [CrossRef] [Green Version]
- Michelozzi, P.; Accetta, G.; de Sario, M.; D’Ippoliti, D.; Marino, C.; Baccini, M.; Biggeri, A.; Anderson, H.R.; Katsouyanni, K.; Ballester, F.; et al. High temperature and hospitalizations for cardiovascular and respiratory cases in 12 European cities. Am. J. Respir. Crit. Care Med. 2009, 179, 383–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dawson, J.; Weir, C.; Wright, F.; Bryden, C.; Aslanyan, S.; Lees, K.; Bird, W.; Walters, M. Associations between meteorological variables and acute stroke hospital admissions in the west of Scotland. Acta Neurol. Scand. 2008, 117, 85–89. [Google Scholar] [CrossRef]
- Garssen, J.; Harmsen, C.; de Beer, J. The effect of the summer 2003 heat wave on mortality in the Netherlands. Eurosurveillance 2005, 10, 165–168. [Google Scholar] [CrossRef]
- Kovats, R.S.; Johnson, H.; Griffith, C. Mortality in southern England during the 2003 heat wave by place of death. Health Stat Q. 2006, 29, 6–8. [Google Scholar]
- Le Tertre, A.; Lefranc, A.; Eilstein, D.; Declercq, C.; Medina, S.; Blanchard, M.; Chardon, B.; Fabre, P.; Filleul, L.; Jusot, J.F.; et al. Impact of the 2003 Heatwave on All-Cause Mortality in 9 French Cities. Epidemiology 2006, 17, 15. [Google Scholar] [CrossRef]
- Parks, R.M.; Bennet, J.E.; Tamura-Wicks, H.; Kontis, V.; Toumi, R.; Danaei, G.; Essati, M. Anamalously warm temperatures are associated with increased injury deaths. Nat. Med. 2020, 26, 65–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. Environmental Protection Agency. Understanding the Link between Climate Change and Extreme Weather. 2016. Available online: https://www.epa.gov/climate-change-science/understanding-link-between-climate-change-and-extreme-weather (accessed on 10 October 2016).
- Menne, M.J.; Durre, I.; Korzeniewski, B.; McNeal, S.; Thomas, K.; Yin, X.; Anthony, S.; Ray, R.; Vose, R.S.; Gleason, B.E.; et al. Global Historical Climatology Network—Daily (GHCN-Daily), Version 3.12; NOAA National Climate Data Center: Asheville, NC, USA; p. 2012.
- NOAA National Climatic Data Center. Available online: http://doi.org/10.7289/V5D21VHZ (accessed on 10 October 2016).
- Thacker, M.T.F.; Lee, R.; Sabogal, R.I.; Henderson, A. Overview of deaths associated with natural events, United States, 1979-2004. Disasters. 2008, 32, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.E.; Johnson, R.L. Injuries in the State of New Hampshire 2001–2009; New Hampshire Department of Health and Human Services, Division of Public Health Services, Injury Surveillance Program: Concord, NH, USA, 2012; p. 96. [Google Scholar]
- Kovats, R.S.; Hajat, S.; Wilkinson, P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in greater London, UK. Occup. Environ. Med. 2004, 61, 893–898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, J.; Samet, J.M.; Patz, J.A. Hospital admissions for heart disease: The effects of temperature and humidity. Epidemiology 2004, 15, 755–761. [Google Scholar] [CrossRef]
- Armstrong, B. Models for the relationship between ambient temperature and daily mortality. Epidemiology 2006, 17, 624–631. [Google Scholar] [CrossRef]
- Muggeo, V.M.; Hajat, S. Modelling the non-linear multiple-lag effects of ambient temperature on mortality in Santiago and Palermo: A constrained segmented distributed lag approach. Occup. Environ. Med. 2009, 66, 584–591. [Google Scholar] [CrossRef]
- Hastie, T.; Tibshirani, R. Generalized additive models. Stat. Sci. 1986, 1, 297–310. [Google Scholar] [CrossRef]
- Schwartz, J. Nonparametric smoothing in the analysis of air pollution and respiratory illness. Can. J. Stat. 1994, 22, 471–488. [Google Scholar] [CrossRef]
- Kelsall, J.E.; Samet, J.M.; Zeger, S.L.; Xu, J. Air pollution and mortality in Philadelphia, 1974–1988. Am. J. Epidemiol. 1997, 146, 750–762. [Google Scholar] [CrossRef]
- Dominici, F.; Samet, J.M.; Zeger, S.L. Combining evidence on air pollution and daily mortality from the twenty largest U.S. cities: A hierarchical modeling strategy (with discussion). J. R. Stat. Soc. Ser. A 2000, 163, 263–302. [Google Scholar] [CrossRef]
- Schwartz, J. Air pollution and hospital admissions for heart disease in eight U.S. counties. Epidemiology 1999, 10, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.M.; Dominici, F.; Curriero, F.C.; Coursac, I.; Zeger, S.L. Fine particulate air pollution and mortality in 20 U.S. cities: 1987–1994. N. Emgl. J. Med. 2000, 343, 1742–1757. [Google Scholar] [CrossRef] [PubMed]
- Katsouyanni, K.; Touloumi, G.; Samoli, E.; Gryparis, A.; Le Tertre, A.; Monopolis, Y.; Rossi, G.; Zmirou, D.; Ballester, F.; Boumghar, A.; et al. Confounding and effect modification in the short-term effects of ambient particles on total mortality: Results from 29 European cities within the APHEA2 project. Epidemiology 2001, 12, 521–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dominici, F.; McDermott, A.; Zeger, S.L.; Samet, J.M. On the use of generalized additive models in time-series studies of air pollution and health. Am. J. Epidemiol. 2002, 156, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. Information theory as an extension of the maximum likelihood principle. In Second International Symposium on Information Theory; Petrov, B.N., Csaki, F., Eds.; Akademiai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- Sakamoto, Y.; Ishiguro, M.; Kitagawa, G. Akaike Information Criterion Statistics; KTK Scientific Publisher: Tokyo, Japan, 1988. [Google Scholar]
- Guisan, A.; Edwards, T.C., Jr.; Hastie, T. Generalized linear and generalized additive models in studies of species distributions: Setting the scene. Ecol. Model. 2002, 157, 89–100. [Google Scholar] [CrossRef] [Green Version]
- Barry, S.C.; Walsh, A. Generalized additive modelling and zero inflated count data. Ecol. Model. 2002, 157, 179–188. [Google Scholar] [CrossRef]
- Constantin de, M.G.; Murtugudde, R.; Sapiano, M.R.; Nizam, A.; Brown, C.W.; Busalacchi, A.J.; Yunus, M.; Nair, G.B.; Gil, A.I.; Lanata, C.F.; et al. Environmental signatures associated with cholera epidemics. Proc. Natl. Acad. Sci. USA 2008, 105, 17676–17681. [Google Scholar] [CrossRef] [Green Version]
- Almeida, S.P.; Casimiro, E.; Calheiros, J. Effects of apparent temperature on daily mortality in Lisbon and Oporto, Portugal. Environ. Health 2010, 9. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Barnett, A.G.; Pan, X.; Yu, W.; Tong, S. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag non-linear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef] [Green Version]
- Gronlund, C.J.; Zanobetti, A.; Schwartz, J.D.; Wellenius, G.A.; O’Neill, M.S. Heat, heat Waves, and Hospital Admissions among the Elderly in the United States. Environ. Health Perspect. 2014, 122, 1187–1192. [Google Scholar] [CrossRef] [Green Version]
- Leonard, K.J.; Rauner, M.S.; Schaffhauser-Linzatti, M.M.; Yap, R. The effect of funding policy on day of week admissions and discharges in hospitals: The cases of Austria and Canada. Health Policy 2003, 63, 239–257. [Google Scholar] [CrossRef]
- Lin, S.; Luo, M.; Walker, R.J.; Liu, X.; Hwang, S.A.; Chinery, R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 2009, 20, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Wei-ping, M.; Gu, S.; Wang, Y.; Zhang, X.; Wang, A.; Zhao, N.; Song, Y. The use of mixed generalized additive modeling to assess the effect of temperature on the usage of emergency electrocardiography examination among the elderly in Shanghai. PLoS ONE 2014, 9, e100284. [Google Scholar]
- Samoli, E.; Schwartz, J.; Wojtyniak, B.; Touloumi, G.; Spix, C.; Balducci, F.; Medina, S.; Rossi, G.; Sunyer, J.; Bacharova, L.; et al. Investigating regional differences in short-term effects of air pollution on daily mortality in the APHEA project: A sensitivity analysis for controlling long-term trends and seasonality. Environ. Health Perspect. 2001, 109, 349–353. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Normand, S.L. Meta-Analysis: Formulating, Evaluating, Combining, and Reporting. Stat. Med. 1999, 18, 321–359. [Google Scholar] [CrossRef]
- Alessandrini, E.; Sajani, S.Z.; Scotto, F.; Miglio, R.; Marchesi, S.; Lauriola, P. Emergency ambulance dispatches and apparent temperature: A time series analysis in Emilia–Romagna, Italy. Environ. Res. 2011, 111, 1192–1200. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 2012, 31, 3821–3839. [Google Scholar] [CrossRef] [Green Version]
- Ueda, K.; Nitta, H.; Ono, M.; Takeuchi, A. Estimating mortality effects of fine particulate matter in Japan: A comparison of time-series and case crossover analyses. J. Air Waste Manag. Assoc. 2012, 59, 1212–1218. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2015; ISBN 3-900051-07-0. Available online: http://www.R-project.org/ (accessed on 1 August 2016).
- Ostro, B.; Rauch, S.; Green, R.; Malig, B.; Basu, R. The effects of temperature and use of air conditioning on hospitalizations. Am. J. Epidemiol. 2010, 172, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Nelson, N.G.; Collins, C.L.; Comstock, R.D.; McKenzie, L.B. Exertional heat-related injuries treated in emergency departments in the U.S.; 1997–2006. Am. J. Prev. Med. 2011, 40, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.R.; Barnett, A.G.; Connell, D.; Tong, S. Ambient temperature and cardiorespiratory morbidity: A systematic review and meta-analysis. Epidemiology 2012, 23, 594–606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bai, L.; Ding, G.; Gu, S.; Bi, P.; Su, B.; Qin, D.; Xu, G.; Liu, Q. The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011-2013. Environ. Res. 2014, 132, 212–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gasparrini, A.; Armstrong, B. The impact of heat waves on mortality. Epidemiology 2011, 22, 68–73. [Google Scholar] [CrossRef] [Green Version]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Biggeri, A.; Bisanti, L.; Cadum, E.; Caranci, N.; de’Donato, F.; De Lisio, S.; De Maria, M.; et al. Vulnerability to Heat-Related Mortality: A Multicity, Population-Based, Case-Crossover Analysis. Epidemiology 2006, 17, 315–323. [Google Scholar] [CrossRef]
- Wake, C.P.; Burakowski, E.A.; Wilkinson, P.; Hayhoe, K.; Stoner, A.; Keeley, C.; LaBranche, J. Climate Change in Southern New Hampshire: Past, Present and Future; The Sustainability Institute, 2014; Volume 2, Available online: https://scholars.unh.edu/sustainability/2 (accessed on 25 September 2016).
- Moolgavkar, S. Air pollution and hospital admissions for diseases of the circulatory system in three U.S. metropolitan areas. J. Air Waste Manag. Assoc. 2000, 50, 1199–1206. [Google Scholar] [CrossRef] [Green Version]
- Levy, A.R.; Bensimon, D.R.; Mayo, N.E.; Leighton, H.G. Inclement weather and the risk of hip fracture. Epidemiology 1998, 9, 172–177. [Google Scholar] [CrossRef]
- Carder, M.; McNamee, R.; Beverland, I.; Elton, R.; Cohen, G.R.; Boyd, J.; Agius, R.M. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup. Environ. Med. 2005, 62, 702–710. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Ha, J.S.; Park, J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch. Environ. Occup. Health 2006, 61, 265–270. [Google Scholar] [CrossRef]
- Yip, F.Y.; Flanders, W.D.; Wolkin, A.; Engelthaler, D.; Humble, W.; Neri, A.; Lewis, L.; Backer, L.; Rubin, C. The impact of excess heat events in Maricopa County, Arizona: 2000-2005. Int. J. Biometeorol. 2008, 52, 765–772. [Google Scholar] [CrossRef]

| Event | ICD-9 Code or Ecode |
|---|---|
| All-Cause | 800-999 |
| Motor Vehicle Accidents | E810-E829; E846-E849 |
| Accidental Falls | E880-E888 |
| Natural and Environmental | E900; E901; E904.3; E907; E908; 991-992 |
| Accidental Drowning | E910 |
| Carbon Monoxide Poisoning | E868 |
| Natural Event | ICD-9 Code or Ecode |
|---|---|
| Cold | E900; 991 |
| Heat | E900; 992 |
| Exposure | E904.3 |
| Lightning | E907 |
| Storms and floods | E908 |
| Exposures | Outcomes |
|---|---|
| Daily Maximum Temperature ≥90 °F (≥32 °C) (Heat Metric 1; HM1) | All-Cause Injury (All) |
| Daily Maximum Temperature ≥95 °F (≥35 °C) (Heat Metric 2; HM2) | Motor Vehicle Accidents (Veh) |
| Daily Maximum Temperature ≤32 °F (≤0 °C) (Cold Metric 1; CM1) | Accidental Falls (Falls) |
| Daily Precipitation ≥1″ (Precipitation Metric 1; PM1) | Accidents due to Natural or Environmental Causes (Environmental) |
| Daily Precipitation ≥2″ (Precipitation Metric 2; PM2) | Accidental Drowning |
| Maximum Temperature (Tmax) | CO Poisoning |
| Daily Precipitation (Precip) | Cold Visits |
| Heat Visits | |
| Lightning | |
| Exposure | |
| Storms and Floods |
| Study Area | Population | All-Cause Injuries | Vehicle Accidents | Accidental Falls | Environ. | Accidental Drowning | CO Poisoning |
|---|---|---|---|---|---|---|---|
| Berlin | 15,230 | 15,976.5 | 1873.5 | 5366.6 | 35.0 | 5.1 | 16.8 |
| Colebrook | 5981 | 16,671.3 | 2142.0 | 5342.8 | 46.4 | 0 | 18.6 |
| Concord | 137,419 | 9999.7 | 1398.2 | 3063.4 | 23.8 | 3.1 | 5.3 |
| Durham | 186,340 | 11,420.8 | 1323.9 | 3486.5 | 28.2 | 2.6 | 5.7 |
| Hanover | 36,982 | 8565.7 | 1124.3 | 2804.4 | 18.9 | 2.1 | 7.5 |
| Keene | 64,661 | 9325.6 | 1462.2 | 2906.8 | 28.7 | 3.1 | 7.2 |
| Lakeport | 89,170 | 15,126.4 | 2332.1 | 4590.7 | 38.1 | 6.6 | 11.3 |
| Nashua | 405,785 | 10,987.2 | 1656.1 | 3269.5 | 22.8 | 3.3 | 7.3 |
| North Conway | 20,706 | 12,937.7 | 1589.4 | 4642.2 | 31.1 | 3.8 | 8.0 |
| Study Area | Population | Cold | Heat | Weather Not Specified | Lightning | Storms and Floods |
|---|---|---|---|---|---|---|
| Berlin | 15,230 | 19.7 | 13.9 | 0.7 | 0.7 | 0 |
| Colebrook | 5981 | 33.4 | 9.3 | 0 | 1.9 | 1.9 |
| Concord | 137,419 | 11.3 | 9.4 | 1.5 | 1.2 | 0.3 |
| Durham | 186,340 | 10.9 | 14.3 | 1.4 | 1.6 | 0.1 |
| Hanover | 36,982 | 9.6 | 7.8 | 0.3 | 1.2 | 0 |
| Keene | 64,661 | 11 | 14.6 | 1.5 | 1.4 | 0.2 |
| Lakeport | 89,170 | 19.1 | 13.8 | 2.9 | 2.4 | 0 |
| Nashua | 405,785 | 10.6 | 12.3 | 2.1 | 1 | 0.1 |
| North Conway | 20,706 | 17.2 | 9.7 | 2.1 | 2.1 | 0 |
| Study Area | Strongest | 2nd Strongest | 3rd Strongest |
|---|---|---|---|
| Berlin | All/Tmax (0.193) | Veh/Tmax (0.135) | Heat/HM1 (0.134) |
| Colebrook | Heat/HM1 (0.109) | All/Tmax (0.108) | Falls/ Tmax (−0.072) |
| Concord | All/Tmax (0.407) | Heat/HM1 (0.340) | Heat/Tmax (0.233) |
| Durham | Heat/HM1 (0.507) | All/Tmax (0.497) | Environmental/HM1 (0.335) |
| Hanover | All/Tmax (0.290) | Heat/HM1 (0.181) | Heat/HM2 (0.165) |
| Keene | All/Tmax (0.292) | Heat/HM1 (0.249) | Veh/Tmax (0.210) |
| Lakeport | All/Tmax (0.440) | Heat/HM1 (0.368) | Heat/Tmax (0.226) |
| Nashua | All/Tmax (0.554) | Heat/HM1 (0.353) | Heat/Tmax (0.348) |
| North Conway | Falls/ Tmax (−0.216) | Falls/ CM1 (0.187) | Veh/Tmax (0.155) |
| Strongest | 2nd Strongest | |
|---|---|---|
| Berlin | All/Tmax /Warm (0.132) | Heat/HM1/Warm (0.131) |
| Colebrook | Heat/HM1/Warm (0.119) | Cold/Tmax /Cool(−0.097) |
| Concord | Heat/ HM1/Warm (0.309) | Heat/Tmax /Warm (0.279) |
| Durham | Heat/HM1/Warm (0.504) | Heat/Tmax /Warm (0.400) |
| Hanover | All/ Tmax /Warm (0.207) | Heat/HM1/Warm (0.197) |
| Keene | Heat/ HM1/Warm (0.225) | Heat/Tmax /Warm (0.212) |
| Lakeport | Heat / HM1/Warm (0.368) | Heat/Tmax /Warm (0.286) |
| Nashua | Heat / Tmax /Warm (0.366) | Heat/HM1/Warm (0.341) |
| North Conway | Heat / HM1/Warm (0.140) | Heat/HM2/Warm (0.129) |
| Exposure–Outcome | Model |
|---|---|
| All-cause Injury ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 Summer + εt |
| Vehicle Accidents ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 Summer + εt |
| Accidental Falls ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 EWMcold + εt |
| Heat-related Visits ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 EWMhot + εt |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neugent, K.; Bush, K.F.; Kelsey, E.; Cahillane, M.; Laflamme, E. Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009. Atmosphere 2020, 11, 281. https://doi.org/10.3390/atmos11030281
Neugent K, Bush KF, Kelsey E, Cahillane M, Laflamme E. Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009. Atmosphere. 2020; 11(3):281. https://doi.org/10.3390/atmos11030281
Chicago/Turabian StyleNeugent, Kelly, Kathleen F. Bush, Eric Kelsey, Matthew Cahillane, and Eric Laflamme. 2020. "Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009" Atmosphere 11, no. 3: 281. https://doi.org/10.3390/atmos11030281
APA StyleNeugent, K., Bush, K. F., Kelsey, E., Cahillane, M., & Laflamme, E. (2020). Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009. Atmosphere, 11(3), 281. https://doi.org/10.3390/atmos11030281