Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009
Abstract
1. Introduction
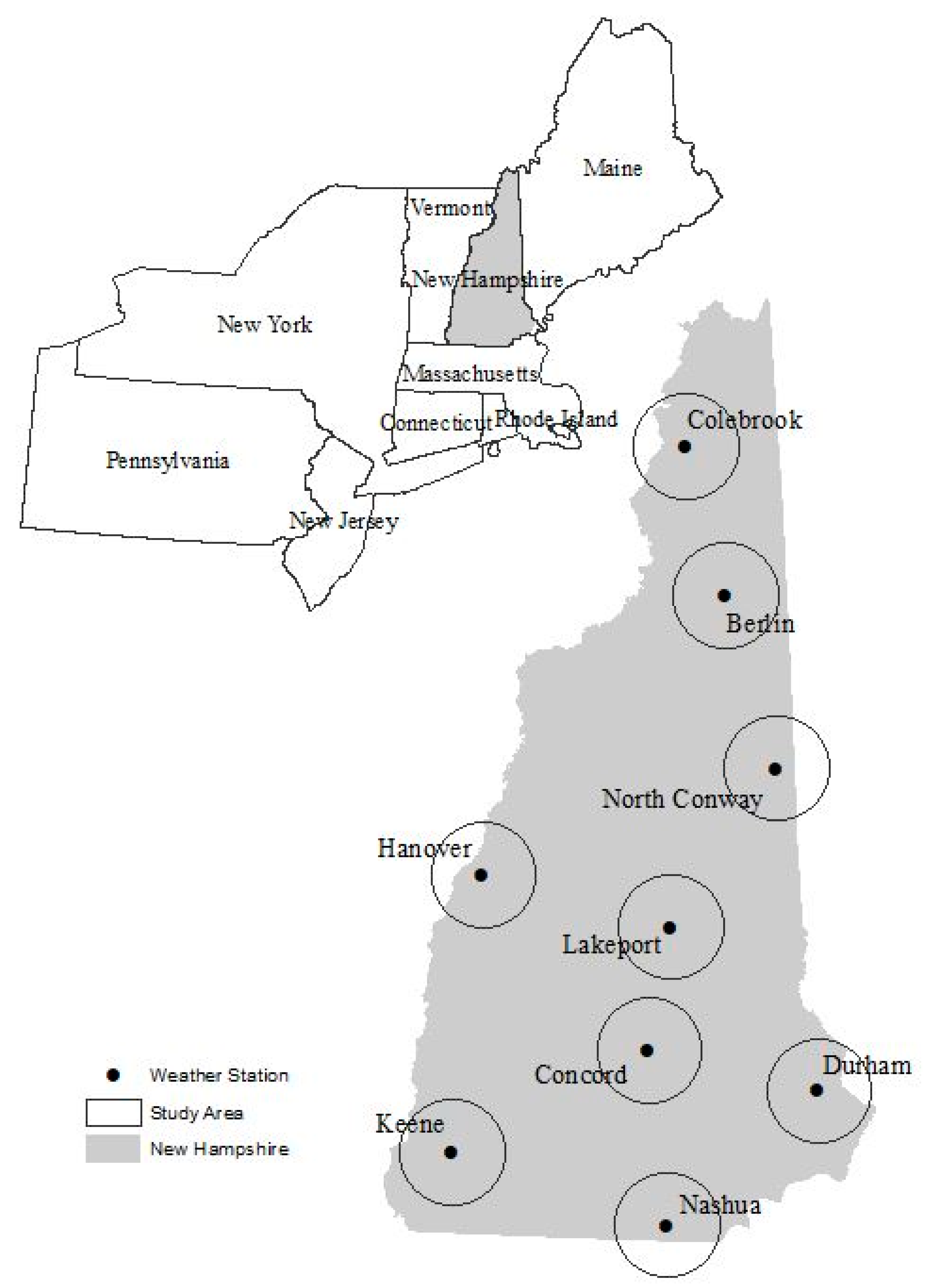
2. Methods
3. Results
3.1. Injury Rates–Primary Health Outcomes
3.2. Injury Rates–Secondary (Environmental) Health Outcomes
3.3. Statistical Relationship between Climate and Health
3.4. Regression Analyses
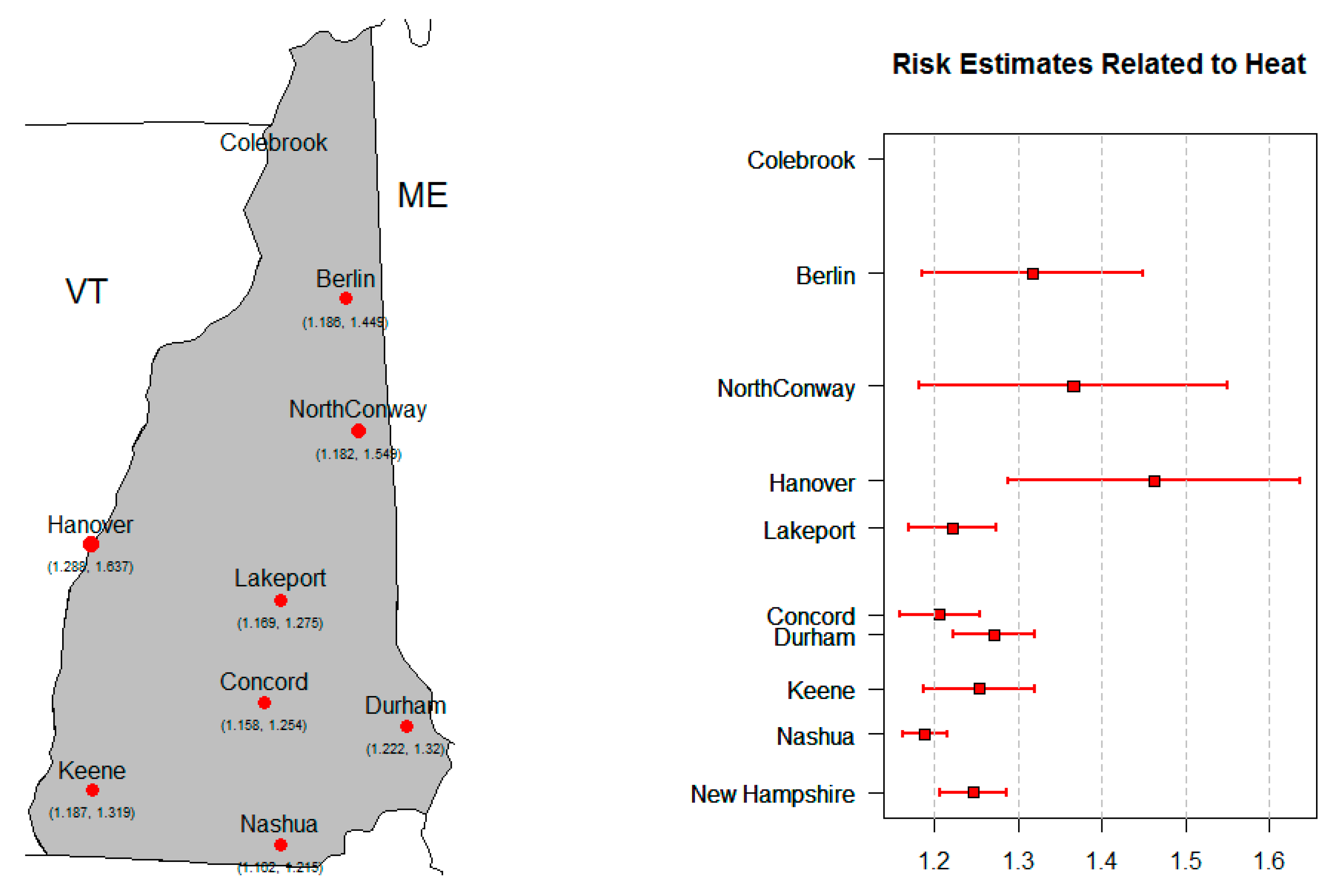
3.4.1. All-Cause Injury ~ Tmax
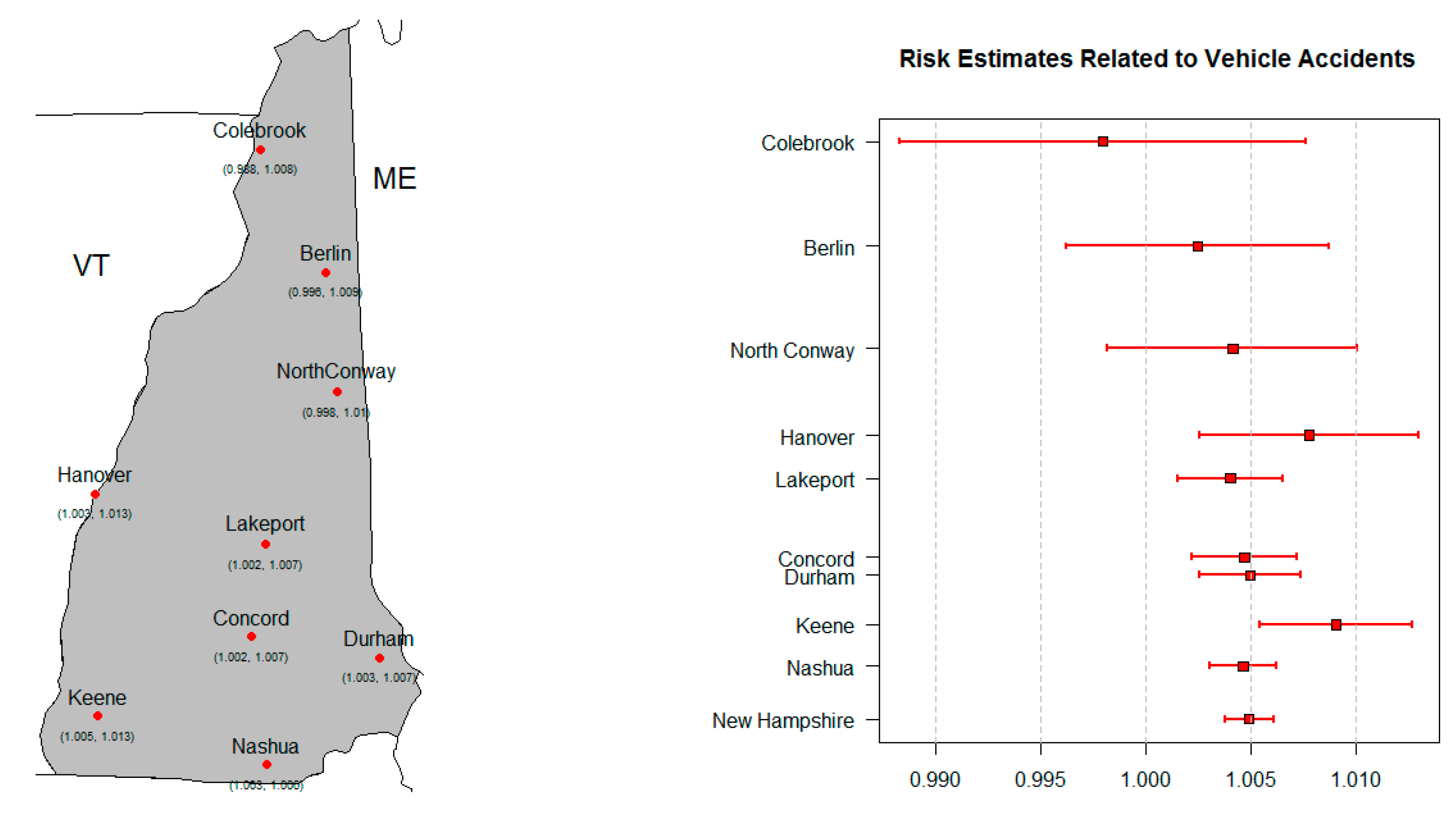
3.4.2. Vehicle Accidents ~ Tmax
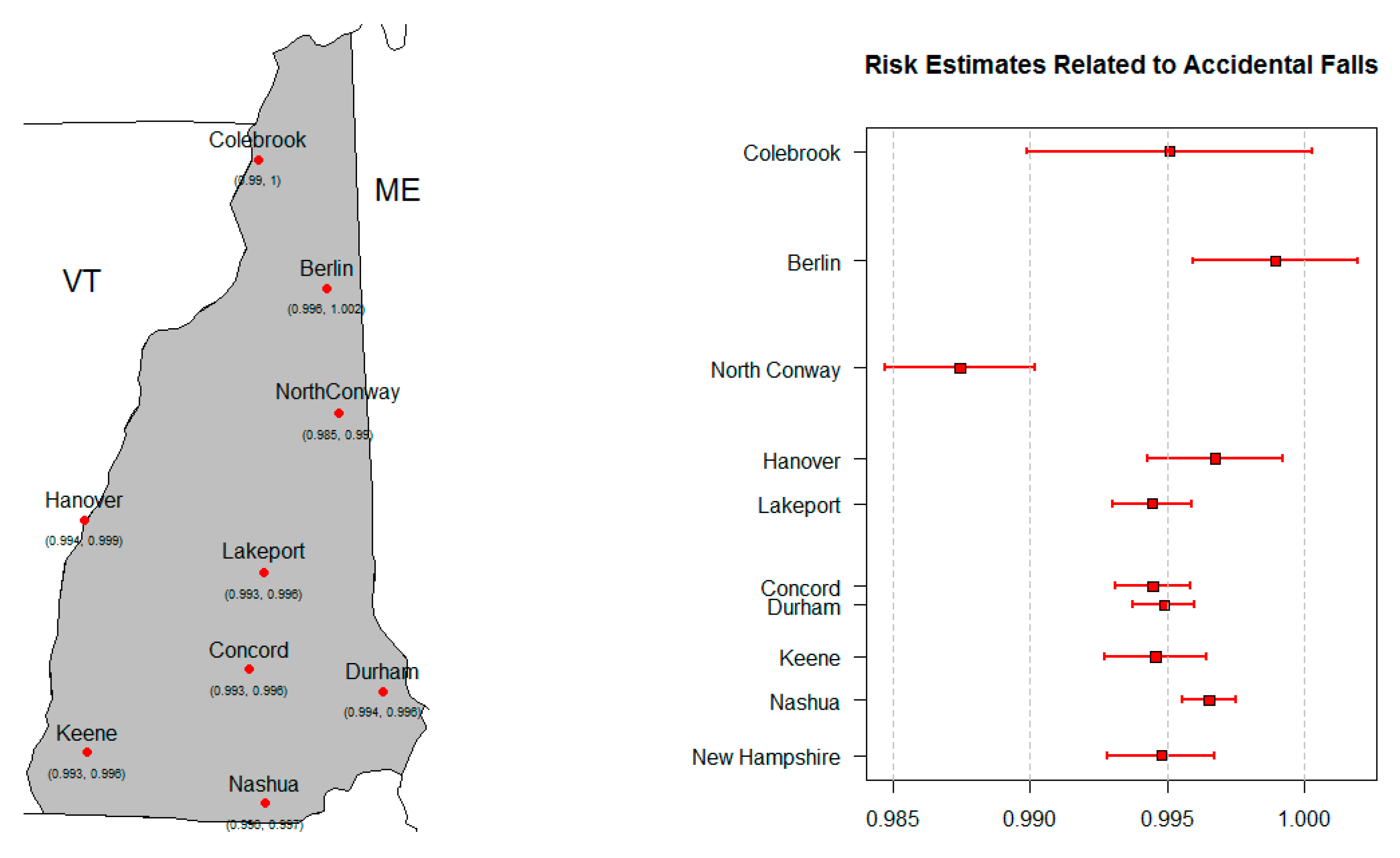
3.4.3. Accidental Falls ~ Tmax
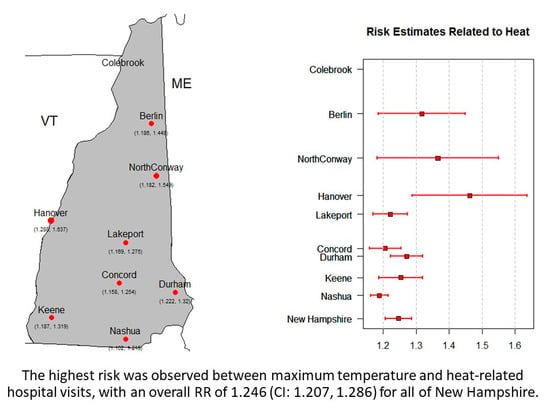
3.4.4. Heat-Related Injury ~ Tmax
4. Discussion
4.1. Injury Rates
4.2. Exposure Metrics
4.3. Relative Risks
4.4. Comparative Studies
4.5. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- NCDC. Climate of New Hampshire; NCDC Climate Services Branch Report 7; NCDC: Asheville, NC, USA, 2017.
- Meehl, G.A.; Tebaldi, C.; Walton, G.; Easterling, D.; McDaniel, L. Relative increase of record high maximum temperatures compared to record low minimum temperatures in the U.S. Geophys. Res. Lett. 2009, 36. [Google Scholar] [CrossRef]
- Balbus, J.; Crimmins, A.; Gamble, J.L.; Easterling, D.R.; Kunkel, K.E.; Saha, S.; Sarofim, M.C.C. 1: Introduction: Climate Change and Human Health. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 25–42. [Google Scholar]
- U.S. Global Change Research Program. 2014 National Climate Assessment; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2014. Available online: http://nca2014.globalchange.gov/report/our-changing-climate/precipitation-change (accessed on 31 August 2016).
- IPCC. Summary for Policy Makers. In Climate Change The Physical Science Basis; Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Stocker, T.F., Qin, D., Plattner, G.-K., Tignor, M., Allen, S.K., Boschung, J., Nauels, A., Xia, Y., Bex, V., Midgley, P.M., Eds.; IPCC: Geneva, Switzerland, 2013. [Google Scholar]
- Knowlton, K.; Rotkin-Ellman, M.; King, G.; Margolis, H.G.; Smith, D.; Solomon, G.; Trent, R.; English, P. The 2006 California heat wave: Impacts on hospitalizations and emergency department visits. Environ. Health Perspect. 2009, 117, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Basu, R.; Pearson, D.; Malig, B.; Broadwin, R.; Green, R. The effect of high ambient temperature on emergency room visits. Epidemiology 2012, 23, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Kent, S.T.; McClure, L.A.; Zaitchik, B.F.; Smith, T.T.; Gohlke, J.M. Heat waves and health outcomes in Alabama (USA): The importance of heat wave definition. Environ. Health Perspect. 2014, 122, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, E.; Gasparrini, A.; Wang, X.; Chen, H.; Yagouti, A.; Fleury, M.D.; Cakmak, S. Extreme ambient temperatures and cardiorespiratory emergency room visits: Assessing risk by comorbid health conditions in a time series study. Environ. Health 2014, 13, 5. [Google Scholar] [CrossRef]
- Michelozzi, P.; Accetta, G.; de Sario, M.; D’Ippoliti, D.; Marino, C.; Baccini, M.; Biggeri, A.; Anderson, H.R.; Katsouyanni, K.; Ballester, F.; et al. High temperature and hospitalizations for cardiovascular and respiratory cases in 12 European cities. Am. J. Respir. Crit. Care Med. 2009, 179, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.; Weir, C.; Wright, F.; Bryden, C.; Aslanyan, S.; Lees, K.; Bird, W.; Walters, M. Associations between meteorological variables and acute stroke hospital admissions in the west of Scotland. Acta Neurol. Scand. 2008, 117, 85–89. [Google Scholar] [CrossRef]
- Garssen, J.; Harmsen, C.; de Beer, J. The effect of the summer 2003 heat wave on mortality in the Netherlands. Eurosurveillance 2005, 10, 165–168. [Google Scholar] [CrossRef]
- Kovats, R.S.; Johnson, H.; Griffith, C. Mortality in southern England during the 2003 heat wave by place of death. Health Stat Q. 2006, 29, 6–8. [Google Scholar]
- Le Tertre, A.; Lefranc, A.; Eilstein, D.; Declercq, C.; Medina, S.; Blanchard, M.; Chardon, B.; Fabre, P.; Filleul, L.; Jusot, J.F.; et al. Impact of the 2003 Heatwave on All-Cause Mortality in 9 French Cities. Epidemiology 2006, 17, 15. [Google Scholar] [CrossRef]
- Parks, R.M.; Bennet, J.E.; Tamura-Wicks, H.; Kontis, V.; Toumi, R.; Danaei, G.; Essati, M. Anamalously warm temperatures are associated with increased injury deaths. Nat. Med. 2020, 26, 65–70. [Google Scholar] [CrossRef] [PubMed]
- U.S. Environmental Protection Agency. Understanding the Link between Climate Change and Extreme Weather. 2016. Available online: https://www.epa.gov/climate-change-science/understanding-link-between-climate-change-and-extreme-weather (accessed on 10 October 2016).
- Menne, M.J.; Durre, I.; Korzeniewski, B.; McNeal, S.; Thomas, K.; Yin, X.; Anthony, S.; Ray, R.; Vose, R.S.; Gleason, B.E.; et al. Global Historical Climatology Network—Daily (GHCN-Daily), Version 3.12; NOAA National Climate Data Center: Asheville, NC, USA; p. 2012.
- NOAA National Climatic Data Center. Available online: http://doi.org/10.7289/V5D21VHZ (accessed on 10 October 2016).
- Thacker, M.T.F.; Lee, R.; Sabogal, R.I.; Henderson, A. Overview of deaths associated with natural events, United States, 1979-2004. Disasters. 2008, 32, 303–315. [Google Scholar] [CrossRef] [PubMed]
- Thomas, K.E.; Johnson, R.L. Injuries in the State of New Hampshire 2001–2009; New Hampshire Department of Health and Human Services, Division of Public Health Services, Injury Surveillance Program: Concord, NH, USA, 2012; p. 96. [Google Scholar]
- Kovats, R.S.; Hajat, S.; Wilkinson, P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in greater London, UK. Occup. Environ. Med. 2004, 61, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Samet, J.M.; Patz, J.A. Hospital admissions for heart disease: The effects of temperature and humidity. Epidemiology 2004, 15, 755–761. [Google Scholar] [CrossRef]
- Armstrong, B. Models for the relationship between ambient temperature and daily mortality. Epidemiology 2006, 17, 624–631. [Google Scholar] [CrossRef]
- Muggeo, V.M.; Hajat, S. Modelling the non-linear multiple-lag effects of ambient temperature on mortality in Santiago and Palermo: A constrained segmented distributed lag approach. Occup. Environ. Med. 2009, 66, 584–591. [Google Scholar] [CrossRef]
- Hastie, T.; Tibshirani, R. Generalized additive models. Stat. Sci. 1986, 1, 297–310. [Google Scholar] [CrossRef]
- Schwartz, J. Nonparametric smoothing in the analysis of air pollution and respiratory illness. Can. J. Stat. 1994, 22, 471–488. [Google Scholar] [CrossRef]
- Kelsall, J.E.; Samet, J.M.; Zeger, S.L.; Xu, J. Air pollution and mortality in Philadelphia, 1974–1988. Am. J. Epidemiol. 1997, 146, 750–762. [Google Scholar] [CrossRef]
- Dominici, F.; Samet, J.M.; Zeger, S.L. Combining evidence on air pollution and daily mortality from the twenty largest U.S. cities: A hierarchical modeling strategy (with discussion). J. R. Stat. Soc. Ser. A 2000, 163, 263–302. [Google Scholar] [CrossRef]
- Schwartz, J. Air pollution and hospital admissions for heart disease in eight U.S. counties. Epidemiology 1999, 10, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Samet, J.M.; Dominici, F.; Curriero, F.C.; Coursac, I.; Zeger, S.L. Fine particulate air pollution and mortality in 20 U.S. cities: 1987–1994. N. Emgl. J. Med. 2000, 343, 1742–1757. [Google Scholar] [CrossRef] [PubMed]
- Katsouyanni, K.; Touloumi, G.; Samoli, E.; Gryparis, A.; Le Tertre, A.; Monopolis, Y.; Rossi, G.; Zmirou, D.; Ballester, F.; Boumghar, A.; et al. Confounding and effect modification in the short-term effects of ambient particles on total mortality: Results from 29 European cities within the APHEA2 project. Epidemiology 2001, 12, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; McDermott, A.; Zeger, S.L.; Samet, J.M. On the use of generalized additive models in time-series studies of air pollution and health. Am. J. Epidemiol. 2002, 156, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. Information theory as an extension of the maximum likelihood principle. In Second International Symposium on Information Theory; Petrov, B.N., Csaki, F., Eds.; Akademiai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- Sakamoto, Y.; Ishiguro, M.; Kitagawa, G. Akaike Information Criterion Statistics; KTK Scientific Publisher: Tokyo, Japan, 1988. [Google Scholar]
- Guisan, A.; Edwards, T.C., Jr.; Hastie, T. Generalized linear and generalized additive models in studies of species distributions: Setting the scene. Ecol. Model. 2002, 157, 89–100. [Google Scholar] [CrossRef]
- Barry, S.C.; Walsh, A. Generalized additive modelling and zero inflated count data. Ecol. Model. 2002, 157, 179–188. [Google Scholar] [CrossRef]
- Constantin de, M.G.; Murtugudde, R.; Sapiano, M.R.; Nizam, A.; Brown, C.W.; Busalacchi, A.J.; Yunus, M.; Nair, G.B.; Gil, A.I.; Lanata, C.F.; et al. Environmental signatures associated with cholera epidemics. Proc. Natl. Acad. Sci. USA 2008, 105, 17676–17681. [Google Scholar] [CrossRef]
- Almeida, S.P.; Casimiro, E.; Calheiros, J. Effects of apparent temperature on daily mortality in Lisbon and Oporto, Portugal. Environ. Health 2010, 9. [Google Scholar] [CrossRef]
- Guo, Y.; Barnett, A.G.; Pan, X.; Yu, W.; Tong, S. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag non-linear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef]
- Gronlund, C.J.; Zanobetti, A.; Schwartz, J.D.; Wellenius, G.A.; O’Neill, M.S. Heat, heat Waves, and Hospital Admissions among the Elderly in the United States. Environ. Health Perspect. 2014, 122, 1187–1192. [Google Scholar] [CrossRef]
- Leonard, K.J.; Rauner, M.S.; Schaffhauser-Linzatti, M.M.; Yap, R. The effect of funding policy on day of week admissions and discharges in hospitals: The cases of Austria and Canada. Health Policy 2003, 63, 239–257. [Google Scholar] [CrossRef]
- Lin, S.; Luo, M.; Walker, R.J.; Liu, X.; Hwang, S.A.; Chinery, R. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 2009, 20, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Wei-ping, M.; Gu, S.; Wang, Y.; Zhang, X.; Wang, A.; Zhao, N.; Song, Y. The use of mixed generalized additive modeling to assess the effect of temperature on the usage of emergency electrocardiography examination among the elderly in Shanghai. PLoS ONE 2014, 9, e100284. [Google Scholar]
- Samoli, E.; Schwartz, J.; Wojtyniak, B.; Touloumi, G.; Spix, C.; Balducci, F.; Medina, S.; Rossi, G.; Sunyer, J.; Bacharova, L.; et al. Investigating regional differences in short-term effects of air pollution on daily mortality in the APHEA project: A sensitivity analysis for controlling long-term trends and seasonality. Environ. Health Perspect. 2001, 109, 349–353. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Normand, S.L. Meta-Analysis: Formulating, Evaluating, Combining, and Reporting. Stat. Med. 1999, 18, 321–359. [Google Scholar] [CrossRef]
- Alessandrini, E.; Sajani, S.Z.; Scotto, F.; Miglio, R.; Marchesi, S.; Lauriola, P. Emergency ambulance dispatches and apparent temperature: A time series analysis in Emilia–Romagna, Italy. Environ. Res. 2011, 111, 1192–1200. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat. Med. 2012, 31, 3821–3839. [Google Scholar] [CrossRef]
- Ueda, K.; Nitta, H.; Ono, M.; Takeuchi, A. Estimating mortality effects of fine particulate matter in Japan: A comparison of time-series and case crossover analyses. J. Air Waste Manag. Assoc. 2012, 59, 1212–1218. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2015; ISBN 3-900051-07-0. Available online: http://www.R-project.org/ (accessed on 1 August 2016).
- Ostro, B.; Rauch, S.; Green, R.; Malig, B.; Basu, R. The effects of temperature and use of air conditioning on hospitalizations. Am. J. Epidemiol. 2010, 172, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Nelson, N.G.; Collins, C.L.; Comstock, R.D.; McKenzie, L.B. Exertional heat-related injuries treated in emergency departments in the U.S.; 1997–2006. Am. J. Prev. Med. 2011, 40, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Turner, L.R.; Barnett, A.G.; Connell, D.; Tong, S. Ambient temperature and cardiorespiratory morbidity: A systematic review and meta-analysis. Epidemiology 2012, 23, 594–606. [Google Scholar] [CrossRef] [PubMed]
- Bai, L.; Ding, G.; Gu, S.; Bi, P.; Su, B.; Qin, D.; Xu, G.; Liu, Q. The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011-2013. Environ. Res. 2014, 132, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B. The impact of heat waves on mortality. Epidemiology 2011, 22, 68–73. [Google Scholar] [CrossRef]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Biggeri, A.; Bisanti, L.; Cadum, E.; Caranci, N.; de’Donato, F.; De Lisio, S.; De Maria, M.; et al. Vulnerability to Heat-Related Mortality: A Multicity, Population-Based, Case-Crossover Analysis. Epidemiology 2006, 17, 315–323. [Google Scholar] [CrossRef]
- Wake, C.P.; Burakowski, E.A.; Wilkinson, P.; Hayhoe, K.; Stoner, A.; Keeley, C.; LaBranche, J. Climate Change in Southern New Hampshire: Past, Present and Future; The Sustainability Institute, 2014; Volume 2, Available online: https://scholars.unh.edu/sustainability/2 (accessed on 25 September 2016).
- Moolgavkar, S. Air pollution and hospital admissions for diseases of the circulatory system in three U.S. metropolitan areas. J. Air Waste Manag. Assoc. 2000, 50, 1199–1206. [Google Scholar] [CrossRef]
- Levy, A.R.; Bensimon, D.R.; Mayo, N.E.; Leighton, H.G. Inclement weather and the risk of hip fracture. Epidemiology 1998, 9, 172–177. [Google Scholar] [CrossRef]
- Carder, M.; McNamee, R.; Beverland, I.; Elton, R.; Cohen, G.R.; Boyd, J.; Agius, R.M. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup. Environ. Med. 2005, 62, 702–710. [Google Scholar] [CrossRef]
- Kim, H.; Ha, J.S.; Park, J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch. Environ. Occup. Health 2006, 61, 265–270. [Google Scholar] [CrossRef]
- Yip, F.Y.; Flanders, W.D.; Wolkin, A.; Engelthaler, D.; Humble, W.; Neri, A.; Lewis, L.; Backer, L.; Rubin, C. The impact of excess heat events in Maricopa County, Arizona: 2000-2005. Int. J. Biometeorol. 2008, 52, 765–772. [Google Scholar] [CrossRef]

| Event | ICD-9 Code or Ecode |
|---|---|
| All-Cause | 800-999 |
| Motor Vehicle Accidents | E810-E829; E846-E849 |
| Accidental Falls | E880-E888 |
| Natural and Environmental | E900; E901; E904.3; E907; E908; 991-992 |
| Accidental Drowning | E910 |
| Carbon Monoxide Poisoning | E868 |
| Natural Event | ICD-9 Code or Ecode |
|---|---|
| Cold | E900; 991 |
| Heat | E900; 992 |
| Exposure | E904.3 |
| Lightning | E907 |
| Storms and floods | E908 |
| Exposures | Outcomes |
|---|---|
| Daily Maximum Temperature ≥90 °F (≥32 °C) (Heat Metric 1; HM1) | All-Cause Injury (All) |
| Daily Maximum Temperature ≥95 °F (≥35 °C) (Heat Metric 2; HM2) | Motor Vehicle Accidents (Veh) |
| Daily Maximum Temperature ≤32 °F (≤0 °C) (Cold Metric 1; CM1) | Accidental Falls (Falls) |
| Daily Precipitation ≥1″ (Precipitation Metric 1; PM1) | Accidents due to Natural or Environmental Causes (Environmental) |
| Daily Precipitation ≥2″ (Precipitation Metric 2; PM2) | Accidental Drowning |
| Maximum Temperature (Tmax) | CO Poisoning |
| Daily Precipitation (Precip) | Cold Visits |
| Heat Visits | |
| Lightning | |
| Exposure | |
| Storms and Floods |
| Study Area | Population | All-Cause Injuries | Vehicle Accidents | Accidental Falls | Environ. | Accidental Drowning | CO Poisoning |
|---|---|---|---|---|---|---|---|
| Berlin | 15,230 | 15,976.5 | 1873.5 | 5366.6 | 35.0 | 5.1 | 16.8 |
| Colebrook | 5981 | 16,671.3 | 2142.0 | 5342.8 | 46.4 | 0 | 18.6 |
| Concord | 137,419 | 9999.7 | 1398.2 | 3063.4 | 23.8 | 3.1 | 5.3 |
| Durham | 186,340 | 11,420.8 | 1323.9 | 3486.5 | 28.2 | 2.6 | 5.7 |
| Hanover | 36,982 | 8565.7 | 1124.3 | 2804.4 | 18.9 | 2.1 | 7.5 |
| Keene | 64,661 | 9325.6 | 1462.2 | 2906.8 | 28.7 | 3.1 | 7.2 |
| Lakeport | 89,170 | 15,126.4 | 2332.1 | 4590.7 | 38.1 | 6.6 | 11.3 |
| Nashua | 405,785 | 10,987.2 | 1656.1 | 3269.5 | 22.8 | 3.3 | 7.3 |
| North Conway | 20,706 | 12,937.7 | 1589.4 | 4642.2 | 31.1 | 3.8 | 8.0 |
| Study Area | Population | Cold | Heat | Weather Not Specified | Lightning | Storms and Floods |
|---|---|---|---|---|---|---|
| Berlin | 15,230 | 19.7 | 13.9 | 0.7 | 0.7 | 0 |
| Colebrook | 5981 | 33.4 | 9.3 | 0 | 1.9 | 1.9 |
| Concord | 137,419 | 11.3 | 9.4 | 1.5 | 1.2 | 0.3 |
| Durham | 186,340 | 10.9 | 14.3 | 1.4 | 1.6 | 0.1 |
| Hanover | 36,982 | 9.6 | 7.8 | 0.3 | 1.2 | 0 |
| Keene | 64,661 | 11 | 14.6 | 1.5 | 1.4 | 0.2 |
| Lakeport | 89,170 | 19.1 | 13.8 | 2.9 | 2.4 | 0 |
| Nashua | 405,785 | 10.6 | 12.3 | 2.1 | 1 | 0.1 |
| North Conway | 20,706 | 17.2 | 9.7 | 2.1 | 2.1 | 0 |
| Study Area | Strongest | 2nd Strongest | 3rd Strongest |
|---|---|---|---|
| Berlin | All/Tmax (0.193) | Veh/Tmax (0.135) | Heat/HM1 (0.134) |
| Colebrook | Heat/HM1 (0.109) | All/Tmax (0.108) | Falls/ Tmax (−0.072) |
| Concord | All/Tmax (0.407) | Heat/HM1 (0.340) | Heat/Tmax (0.233) |
| Durham | Heat/HM1 (0.507) | All/Tmax (0.497) | Environmental/HM1 (0.335) |
| Hanover | All/Tmax (0.290) | Heat/HM1 (0.181) | Heat/HM2 (0.165) |
| Keene | All/Tmax (0.292) | Heat/HM1 (0.249) | Veh/Tmax (0.210) |
| Lakeport | All/Tmax (0.440) | Heat/HM1 (0.368) | Heat/Tmax (0.226) |
| Nashua | All/Tmax (0.554) | Heat/HM1 (0.353) | Heat/Tmax (0.348) |
| North Conway | Falls/ Tmax (−0.216) | Falls/ CM1 (0.187) | Veh/Tmax (0.155) |
| Strongest | 2nd Strongest | |
|---|---|---|
| Berlin | All/Tmax /Warm (0.132) | Heat/HM1/Warm (0.131) |
| Colebrook | Heat/HM1/Warm (0.119) | Cold/Tmax /Cool(−0.097) |
| Concord | Heat/ HM1/Warm (0.309) | Heat/Tmax /Warm (0.279) |
| Durham | Heat/HM1/Warm (0.504) | Heat/Tmax /Warm (0.400) |
| Hanover | All/ Tmax /Warm (0.207) | Heat/HM1/Warm (0.197) |
| Keene | Heat/ HM1/Warm (0.225) | Heat/Tmax /Warm (0.212) |
| Lakeport | Heat / HM1/Warm (0.368) | Heat/Tmax /Warm (0.286) |
| Nashua | Heat / Tmax /Warm (0.366) | Heat/HM1/Warm (0.341) |
| North Conway | Heat / HM1/Warm (0.140) | Heat/HM2/Warm (0.129) |
| Exposure–Outcome | Model |
|---|---|
| All-cause Injury ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 Summer + εt |
| Vehicle Accidents ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 Summer + εt |
| Accidental Falls ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 EWMcold + εt |
| Heat-related Visits ~ Tmax | log(Yt) = β0 + β1 Tmax + s(time) + β2 DOW + β3 EWMhot + εt |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neugent, K.; Bush, K.F.; Kelsey, E.; Cahillane, M.; Laflamme, E. Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009. Atmosphere 2020, 11, 281. https://doi.org/10.3390/atmos11030281
Neugent K, Bush KF, Kelsey E, Cahillane M, Laflamme E. Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009. Atmosphere. 2020; 11(3):281. https://doi.org/10.3390/atmos11030281
Chicago/Turabian StyleNeugent, Kelly, Kathleen F. Bush, Eric Kelsey, Matthew Cahillane, and Eric Laflamme. 2020. "Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009" Atmosphere 11, no. 3: 281. https://doi.org/10.3390/atmos11030281
APA StyleNeugent, K., Bush, K. F., Kelsey, E., Cahillane, M., & Laflamme, E. (2020). Overview of Injuries Associated with Extreme Weather Events in New Hampshire, U.S., 2001–2009. Atmosphere, 11(3), 281. https://doi.org/10.3390/atmos11030281