1. Introduction
Exposure to air pollution causes serious health damage and affects many organ systems, including the respiratory system. Although this issue is usually associated with large cities, it is now a global problem. According to the World Health Organization (WHO) [
1], it is the cause of premature death in more than 3 million people per year worldwide and may get worse, becoming the leading cause of deaths from environmental issues in the near future.
Exposure to air pollution is an issue in Brazil. Emissions of pollutants from the burning of fossil fuels by motor vehicles is the main cause of pollution in a large number of Brazilian cities and towns, as even small towns have a large vehicle fleet contributing to the poor air quality [
2,
3,
4].
Campaigns have promoted reducing the number of vehicles in circulation as well as encouraging the use of bicycles and walking as means of transportation, with the aim of reducing the pollution as well as to promote improved health. However, the results are still incipient [
5,
6].
When sports or physical exercises are practiced in outdoor environments in regions of high pollutants concentration, especially near roads with a heavy vehicle circulation, an additional question comes up: can physical exercise inhibit or augment pollutants deposition in the respiratory system? [
7]. It is very reasonable to hypothesize that they can, since the practice of sports or physical exercises often causes hyperventilation, enabling larger amounts of pollutants to enter the respiratory system. Besides, mouth instead of nasal breathing is more often used while conducting physical exercise, thereby skipping the normal mechanisms of air filtration [
8,
9].
Despite the large number of publications demonstrating the health benefits of physical exercises [
10,
11], their practice in polluted environments raises the question of whether increased inhalation of pollutants could have harmful effects or not [
12]. Consequently, this raises the questions about the health gains and health losses when practicing physical exercise outdoor in areas with pollutant concentrations above those recommended as being safe by the WHO [
13].
Concerning the evaluation of the impact to health of air pollutants exposure, fractional exhaled nitric oxide is a useful tool used to evaluate pulmonary inflammation in several airway diseases [
14]. According to the American Thoracic Society (ATS) [
15], FeNO levels above 25 parts per billion (ppb) can be used as a cut off rate for asthma diagnosis and to follow airway diseases, since this remarkable parameter is closely associated with lung inflammation [
15]. Furthermore, to amplify the analysis of the inflammatory effect of pollutant exposure in the airways, evaluations of proinflammatory cytokines, such as tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), IL-17A, and the anti-inflammatory IL-10 are widely accepted in the literature [
16,
17,
18].
Regarding the compounds composing the polluted air, particulate matter (PM) has received special attention, since increased levels of PM are associated with premature deaths worldwide [
13,
14]. Particulate matter, a complex mixture of all solid and liquid particles of organic and inorganic substances suspended in the air [
13], has a wide diameter range from 10 μm to submicron particles that are < 0.1 μm. It is widely accepted that the smallest particles are the most dangerous to human health due to their ability to penetrate the body in large quantities through the respiratory system and thereby promote cellular damage [
15,
16]. According to the review of Morawska et al. [
16], the selection of the PM diameter evaluated in the studies is not a trivial aspect and can provide essential data regarding its impact on human health.
In Sao Paulo, winter is the season with the greatest pollution due to a sum of climatic factors in which the cold air prevents the dispersion of PM. This is accentuated by the fact that this season frequently presents very low rainfall rates and high concentrations of PM [
17], with levels above that recommended by the WHO [
1,
18]. Therefore, there is a combination of highly unhealthy pollutants at this time of the year, and PM concentrations are not the same during the beginning and the end of this season [
17].
This study took advantage of these climate characteristics in two distinct moments that present different concentrations of pollutants, particularly PM, by observing the responses of two groups of individuals: one composed by sedentary people and the other by street runners. However, it is noteworthy that both groups lived, worked, and the group of runners performed outdoor physical training, in the same area during the same period, leading to expected similar exposure to environmental levels of air pollutants.
Regarding the effects of physical exercise in polluted environments, the literature is still conflicted [
12], as there are still doubts about the positive and negative results proceeding from the activities in these environments on the point of view of the inflammatory response of the airway. Faced with this scope, pro- and anti-inflammatory cytokines were evaluated as well as the exhaled fraction of nitric oxide (FeNO) in the airway.
2. Materials and Methods
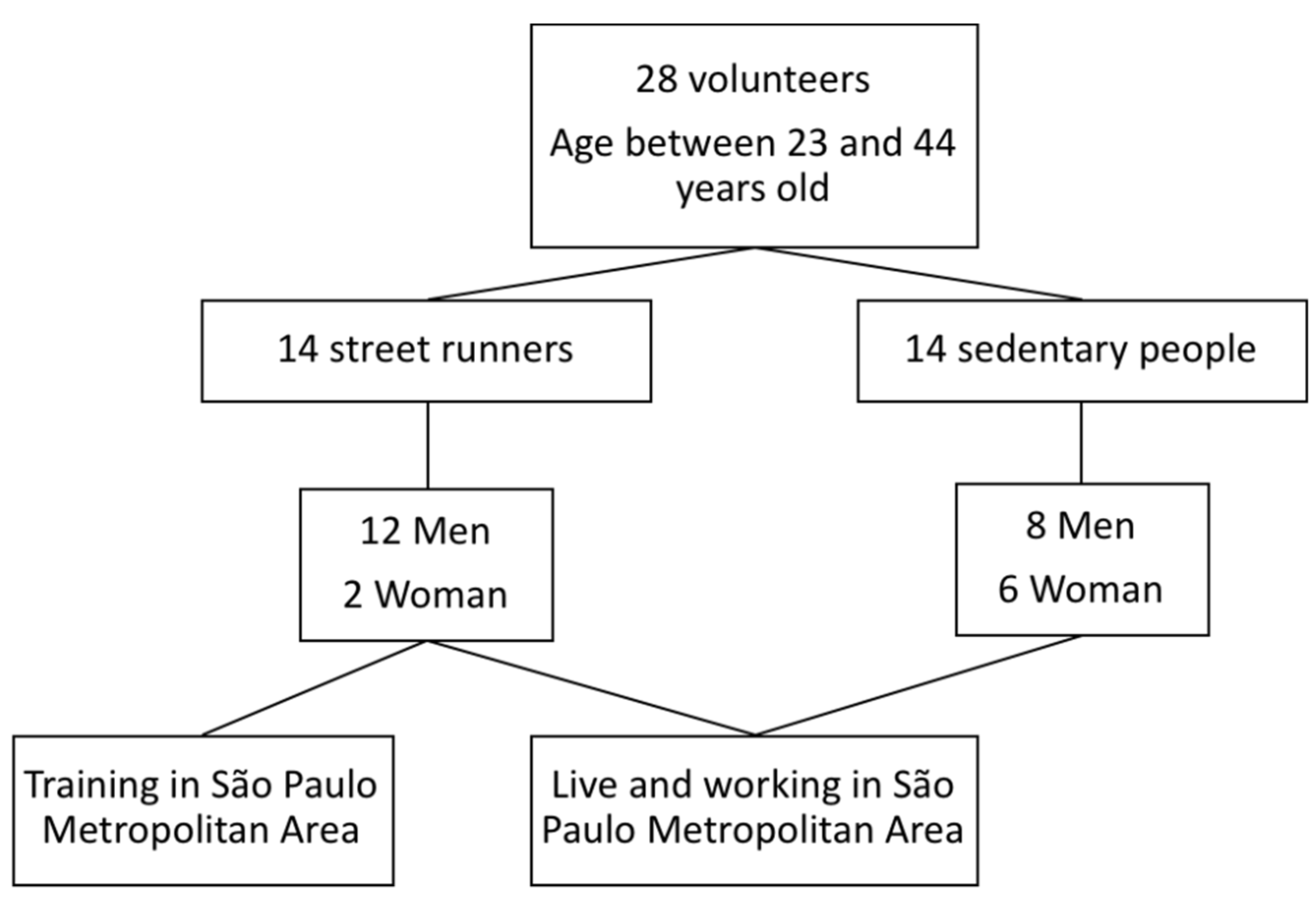
As shown in the flow diagram (
Figure 1), 28 male and female volunteers, ranging in age between 23 and 44 years old, were recruited for this study. The volunteers were divided into two groups: street runners (
n = 14, aged 37.4 ± 6.6) and sedentary people (
n = 14, aged 32.2 ± 6.9). Both volunteer groups were composed by individuals who lived and worked in the metropolitan area of Sao Paulo. Subjects in the running group trained at least three times per week for six months prior to the study in the same area. In addition, among the inclusion criteria, these volunteers should have to completed at least a 10 km race in the six months prior to the study within 1 h 10 min (at a minimum average speed of 8.5 km/h). In relation to the subjects enrolled in the sedentary group, they should not have practiced regular physical activity during the last 12 months.
The exclusion criteria were a diagnosis of cardiovascular disease, respiratory disease, or chronic inflammatory disease, as well as smoking, fertile women who had not been using hormonal contraceptives, and volunteers using corticosteroids. In addition, individuals that lived or worked in areas where pollutants were not monitored by the Environmental Company of Sao Paulo State (CETESB) monitoring system were excluded.
All volunteers were informed of the objectives and risks of the study and were included by signing the Informed Consent Form of the Research Ethics Committee of the Federal University of Sao Paulo under No. 0570/2017. All experiments were performed in accordance with the Declaration of Helsinki [
19].
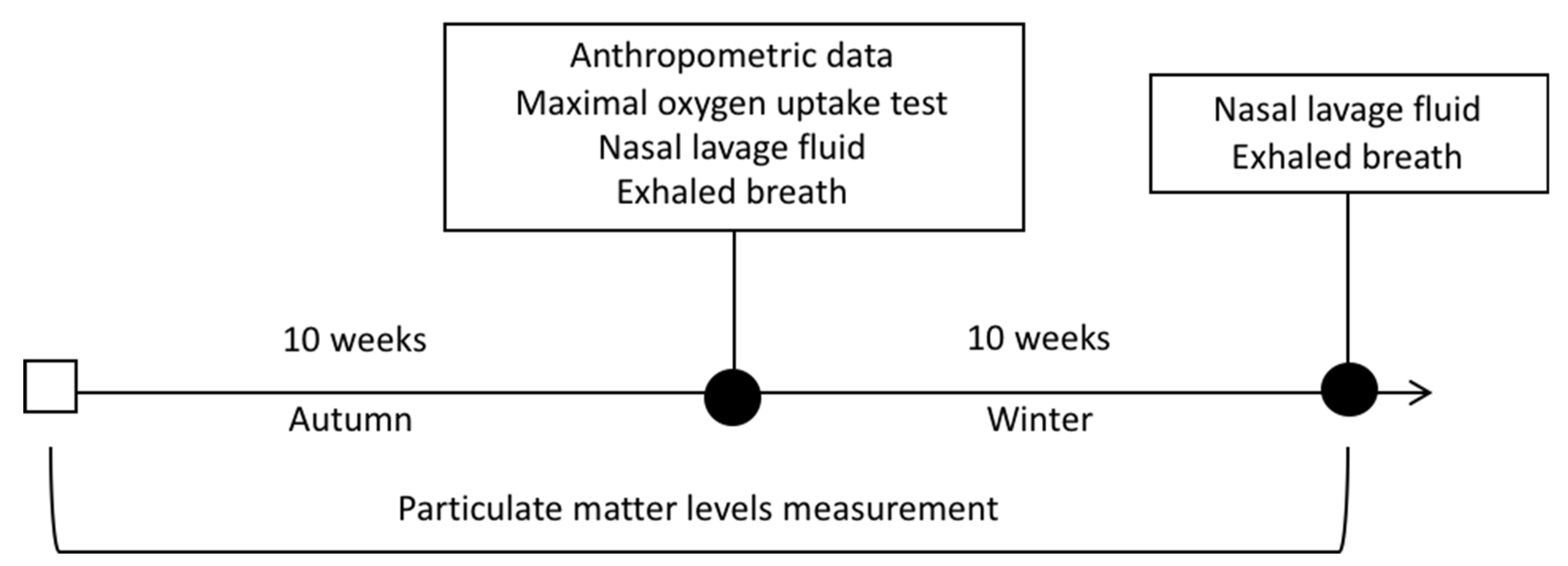
The experimental design (
Figure 2) is detailed below: the first sampling occurred before winter with anthropometric measurements, aerobic capacity assessment, nasal lavage fluid collection, and exhaled air assessment. After 10 weeks, the second collection was performed, with the assessment of exhaled air and a nasal lavage fluid collection. Pollutants levels were monitored for 10 weeks preceding the first sampling (before winter) and were maintained until the last collection.
2.1. Mounting the Pollutant Levels Database
The data for the pollutants came from the database of the CETESB. According to Gonçalves et al. [
20], PM levels are recognized as the main pollutants found in winter due to the lower incidence of rainfall in the state of São Paulo during this period. Therefore, hourly data of PM
2.5 and PM
10 were obtained from 20 monitoring stations located in the São Paulo Metropolitan Region (
https://servicos.cetesb.sp.gov.br/qa/), based on the volunteers’ place of residence, work and training of all volunteers for 20 consecutive weeks (
Figure 2). To obtain the PM
10 data, a large volume sampler was used coupled with an inertial particulate separator for the determination of the inhalable particulate concentration (PM
10), which was suspended in the atmosphere by using gravimetric and β-radiation methods. For PM
2.5, we used a sampler for determination of the fine inhalable particle concentration with gravimetric/impaction-cyclone and β-radiation methods (
https://cetesb.sp.gov.br/ar/redes-de-monitoramento/). All monitoring systems strictly followed the quality assurance/quality control (QA/QC) procedure established by CETESB, as approved by the State Council of the Environment (CONSEMA) of the State of São Paulo.
2.2. Aerobic Capacity Assessment
Aerobic capacity was obtained by applying and analyzing the results of the maximum oxygen consumption (VO
2max), by using the Ellestad protocol, which consists of a three-minute staged test and an increase in both speed and inclination, as described by Ellestad et al. [
21] The tests performed provided maximum measurements, which were interrupted by limiting symptoms/intense physical tiredness.
2.3. Nasal Lavage Collection and Determination of Cytokine Concentration
Nasal lavage fluid is a mildly invasive technique used to determine various airway molecules. For this collection, the volunteers remained seated and performed a cervical extension. Then, 10 mL of saline (0.9% NaCl) were instilled with a syringe, with 5 mL in each nostril. After 10 s, the volunteers bent their heads and expelled the resulting fluid into a disposable vial. Samples of the nasal lavage obtained were frozen at −80 °C (−176 °F) for determination of cytokine concentrations in the upper respiratory tract.
Concentrations of the following cytokines: interleukin (IL) -6, IL-10, IL-17 A, and tumor necrosis factor (TNF)-α were determined in the supernatant of the nasal lavage by using the U-PLEX MSD multiplex kit (Meso Scale, Discovery, Rockville, MD, USA), and by following all of the manufacturer’s instructions correctly.
The protein concentration in the nasal lavage was used to normalize the cytokine concentration values. To determine the total protein concentration in the supernatant of the nasal lavage, the kit BCA developed by Pierce ™ (Pierce Biotechnology, Rockford, IL, USA) was used. For this evaluation, the study followed the instructions provided by the manufacturer of the kit.
Subsequently, all of the values obtained were individually corrected for total protein concentration to normalize concentrations by using the formula: [cytokines/μg] = [cytokines pg/mL]/[total protein μg/mL].
2.4. Exhaled Air Collection and Determination of the Fraction of Exhaled Nitric Oxide (FeNO)
In agreement with ATS, all volunteers were instructed not to consume coffee or any other food or drink with caffeine in its composition within 12 h before collection [
22]. In addition, to obtain exhaled air, the volunteers were instructed to breathe normally in the mouthpiece for approximately four seconds at the time of collection. Afterwards, they performed a maximum inspiration. Following this, the volunteers were asked to exhale steadily for approximately four seconds and the speed of the air release was monitored by an air volume display with a 12 cm H
2O pressure setting, ensuring a stable flow of 200 mL/s. For all the procedure previously described, we used a kit from Sievers (Sievers Instruments Inc., Boulder, CO, USA), composed by a “pipe” with an air passage valve that can be opened and closed manually and a numbered air volume display showing the air in balloons (Mylar bags). After collecting these balloons, they were sealed and stored in a completely dark place. It worth mentioning that the samples were obtained in a single test. The concentration of NO (recorded in parts per billion) was determined within four hours after chemiluminescent collection in a Sievers apparatus (model Sievers NOA 280, Boulder, CO, USA) [
22]. The NO analyzer was calibrated daily using a device that filters the NO present in ambient air and a reference gas with a known concentration of NO (standard mixture for NO calibration at 45 ppb NO
2) (White Martins industrial gases AS, São Paulo, SP, Brazil).
2.5. Statistical Analysis
Statistical analysis was achieved by using a computer software called GraphPad Prism 7 version 7.0a. All data obtained in this study were previously compared with the Gaussian curve and in order to evaluate the normal distribution, we used the Shapiro-Wilk test followed by the Levene test to evaluate the variance homogeneity. Anthropometric and maximal oxygen uptake data were analyzed by Student’s t-test and the data were presented as a mean and standard deviation. Data regarding cytokines and FeNO levels were compared for intragroup and intergroups (runners and sedentary groups) by using the Wilcoxon test and were presented as a median and interquartile range. In the analysis of air pollutants ten weeks before and after the baseline, we used the Mann-Whitney test. Statistical significance was established with p values < 0.05.
3. Results
As shown in
Table 1, during 10 weeks of winter, the PM levels were higher than in the 10 weeks prior to the onset of winter.
Table 2 shows that, as expected, the runners’ group presented a higher VO
2max than the sedentary group. In addition, the runners’ group also demonstrated a lower total fat mass compared to the sedentary group. No differences were found in the other anthropometric parameters.
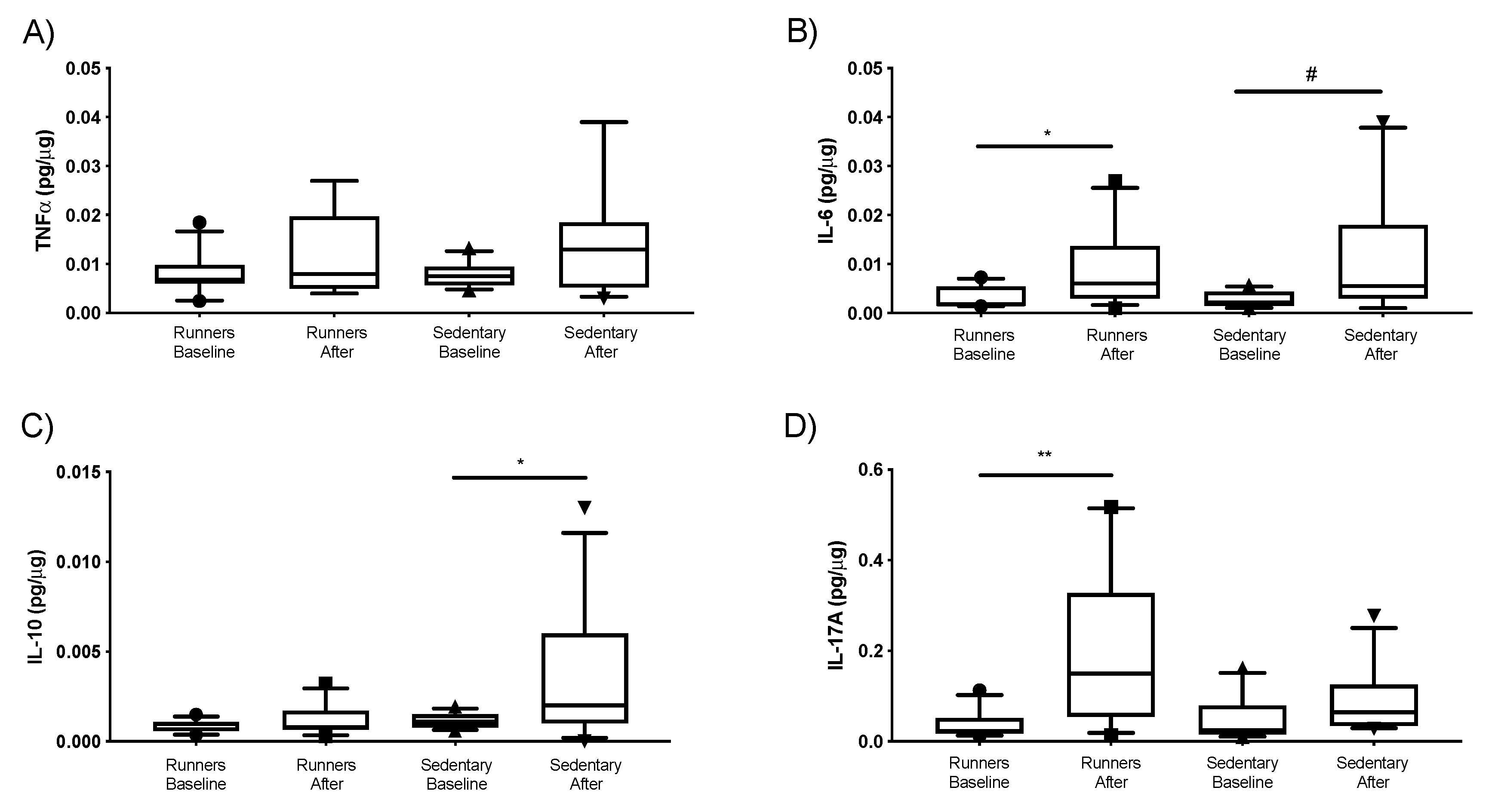
As shown in
Figure 3, no differences in cytokine concentrations were observed between the runners and sedentary groups. Nevertheless, in the comparison between time points, we observed an increase of IL-6 levels (
Figure 3B) in both groups. IL-10 levels were increased in the sedentary group after 10 weeks of PM exposure compared to the baseline (
Figure 3C), and the runners’ group presented an increase of IL-17A levels after 10 weeks of high PM exposure compared to the baseline (
Figure 3D).
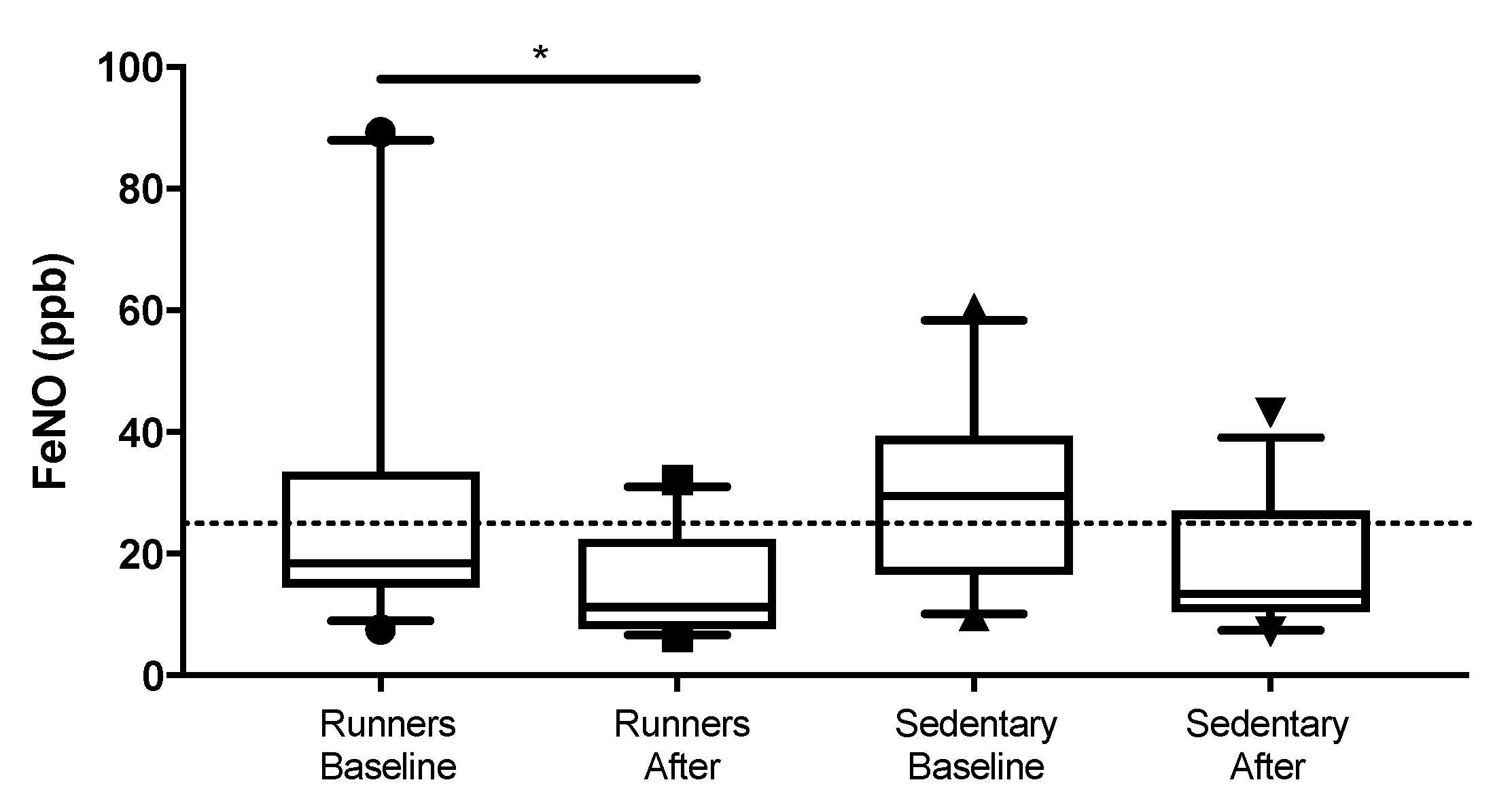
As shown in
Figure 4, there was a significant decrease in FeNO levels of the runners’ group after 10 weeks of high levels of PM exposure compared to the baseline (
p = 0.025). It is important to highlight that this reduction observed in the runners’ group led the FeNO levels below the cut-off (25 ppb), which is associated with the presence of lung inflammation according to ATS/ERS [
22]. In relation to the sedentary group, no differences were found between the time points and the runner’s group (
p > 0.05).
4. Discussion
In this study, we demonstrated that a higher exposure to PM for ten weeks elicited different responses in runners and sedentary people in terms of cytokine concentrations in upper airway and FeNO levels. No differences were found in TNF-α levels for both groups. The sedentary group presented an increase in IL-6 and IL-10 cytokines levels, whereas the runners’ group showed increased levels of IL-6 and IL-17A, as well as decreased FeNO levels.
It is widely accepted that increased air pollutant exposition, especially involving PM exposure, can induce lung inflammation and that FeNO is a well-established biomarker of pulmonary inflammation. Based on this information, it would be reasonable to infer that the higher PM exposure is able to induce an increase of FeNO levels, which already was reported in the literature [
23]. Interestingly, in this study, we verified that the increased average of PM levels (around 25% higher for both PM
2.5 and PM
10) found after 10 weeks of baseline was not able to induce lung inflammation in both groups, since the FeNO levels did not increase in the samples obtained after this period. Although we cannot affirm that the volunteers purposefully avoided air pollutant exposure in order to preserve their health, we can suggest that the lack of elevation in FeNO levels can be attributed to the fact that, in accordance with the literature, lung inflammation induced by PM exposure generally occurs in acute situations [
23]. So, even though the averaged of PM levels were higher during this period, variations in its level should have occurred and, consequently, should have contributed to minimizing the lung inflammation, which was observed in the FeNO levels analysis for both groups.
It has been reported that elevations in the concentration and deposition of air pollutant particles in the airways are closely associated with lung inflammation [
24]. As previously mentioned, an increase in ventilation has been observed during endurance training, which can putatively lead to an elevation of air pollutant deposition, including particulate matter, in the airways [
25]. Taken together, it was expected that the constant hyperventilation imposed by regular endurance training could lead to higher PM deposition in the airways and consequently could induce lung inflammation. However, unexpectedly, our results showed that the runners’ FeNO levels found before the winter and after ten weeks with the elevation of the PM levels were not significantly different to the values observed in the sedentary group. In addition, significant reductions of FeNO levels were found after the increased PM exposure in the runners’ group comparing to the baseline levels. It is also worth highlighting that the values of FeNO levels observed in the majority of runners after ten weeks of baseline data were below the cut-off (25 ppb). Therefore, these results allow us to suggest that a regular practice of endurance training can decrease lung inflammation [
25,
26], even in runners in whom an increased PM deposition in the airways could have occurred. In addition, our results reinforce the widely accepted ability of exercise training to promote an anti-inflammatory status, including in lung tissue, which can putatively mitigate the harmful effect of a higher PM deposition in the airways. Corroborating with the results we obtained in humans, Vieira et al. [
23] demonstrated that mice exposed to diesel particles when trained had less lung inflammation than untrained animals exposed to the same environment.
It is widely accepted that among several control mechanisms used to avoid or at least to ameliorate the impact of PM exposure in the airways, mucus secretion is considered to be the first-line defense against air pollutant particles [
27]. In a general way, mucins are the major molecule that compounds the mucus and is essential for airway defense due to the capacity of binding pathogenic agents and pollutant particles [
28]. It has been demonstrated that cytokines, such as IL-6, IL-10, and IL-17A are associated with mucus secretion in different situations [
29,
30].
In this study, runners presented an increase of IL-17A and IL-6 levels after ten weeks of elevated PM exposure compared to the baseline values. Both cytokines are involved in the Th17 immune response and, according to the literature, IL-17A is able to induce expression of the mucins gene in primary bronchial cells from health donors mediated by IL-6, showing paracrine mediation between these cytokines [
29,
30,
31]. Based on these outcomes, elevations of IL-6 and IL-17A levels in airways can drive the increase of mucus secretion, which may improve the mucosal protection against the PM deposition and consequently decrease lung inflammation. Although the mucus concentration was not evaluated in this study, we can presume that the increased levels of IL-6 and IL-17A found in the airways of the runners’ group can be involved in the activation of a regulatory mechanism of mucosal protection against the harmful effect of PM exposure.
Regarding our results for the sedentary group, we found increased IL-6 and IL-10 levels after 10 weeks of elevated PM exposure. It has been reported that IL-10 expression in the airways is constitutive and it is increased in patients with chronic obstructive pulmonary disease, asthma, and bronchial hyperresponsiveness, as well as in response to challenges that impose an inflammatory response in airways, such as smoking, and also after prolonged exposition to allergens or other external substances, such as PM, though the induction of T regulatory cells [
32,
33,
34]. Although we did not evaluate the presence of T regulatory cells in the airways of volunteer groups, we can suggest that the higher IL-6 levels in the sedentary group, which clearly indicates that an inflammatory response was induced, could consequently elicit the up-regulation of IL-10 expression in the airways.
Despite both Th17 and Th2 immune responses presenting an increase in mucus production, the induction of the Th2 immune response is associated with lung inflammation, even though FeNO levels did not differ between the values found before and after higher PM exposure in the sedentary group.
Taken together, our results demonstrate that the practice of outdoor endurance training modulates the mucosal airway response against PM exposure in a different way to the manner observed for a sedentary lifestyle. Even though the sedentary volunteers did not present inflammatory airway disease, which would be in accordance with the Th2 immune response found here, the maintenance of a Th2 immune response can putatively be deleterious to the respiratory tract [
35]. In this study, the increase of IL-17A, found in runners, can avoid the effect of PM exposure driving to a Th2 immune response, as observed in sedentary people, leading to the improvement of lung protection in runners [
36].
Limitations of the Study
While this study presents variables that should be interpreted with caution, such as the small number of volunteers that could directly impact on the power of statistical tests used to calculate the statistical significances, leading to false-negative results (or type-II error), the relevant differences found here in the FeNO and cytokine levels in samples obtained from two populations presenting well-defined lifestyles (runners and sedentary people) before and after ten weeks of increased PM exposure can jointly mitigate the limitations of this study.
Another limiting point worth mentioning is that, according to the literature and as previously described, the particle diameter represents a fundamental aspect that should be considered. As previously cited, PM has a wide diameter ranging from 10 μm to submicron particles that are as little as < 0.1 μm. It is worth mentioning that, in this study, we can only present data on PM
10 and PM
2.5, because the monitoring stations that provide us with PM data do not evaluate the outdoor concentrations of particles with small diameters, which are generally classified as ultrafine particles. Regarding the ultrafine particles (UFP), these are considered to be particles with a diameter of less than 100 nm and due to their size, these particles can easily penetrate and diffuse throughout the body, leading to adverse health effects in different organs, such as the lung, heart, and brain, through activation of inflammatory and oxidative stress responses [
37]. Based on these pieces of information, it is clear that data regarding the UFP levels could provide us with useful information about the impact of air pollution on our volunteers. However, in this study, the monitoring stations that provide the PM data do not evaluate the ultrafine particles separately. In this regard, it has been pointed out that the lack of a standardized protocol for UFP data collection [
37,
38], especially in outdoor environments, impairs the progress of knowledge of the effects of UFP exposure on people’s health. Therefore, the need to develop additional PM metrics to improve knowledge of the impact of PM on people’s health, especially the role of ultrafine particles, has been debated. In this regard, Lowther et al. [
39] reported in their recent review that the two main metrics often used to measure the concentration of atmospheric PM are the particle mass and particle number. In addition, other additional metrics, such as particle size distribution and chemical composition of particles, can also be measured and used to provide valuable information on the nature of atmospheric PM. However, the same authors highlight that, so far, it is unclear “how each of these metrics relates to health effects and therefore which metric is the best suited to measuring health risk”. Furthermore, it is important to mention that the relative importance of each metric in terms of health is extremely closely associated with the composition, location, and time of PM exposure [
40].
Moreover, there is a huge debate concerning the amount of PM that can be deposited in the airways from the external environment, since, according to the literature, this evaluation is performed only with the use of an environment chamber which allows monitoring and regulation of exposure to pollutants.
Finally, another point that deserves some commentary is associated with the fact that all monitoring stations used in this study are located in the metropolitan region, an area in which it is estimated that more than 21 million people live and work currently. This area contains most of the urban traffic and industries responsible for the largest release of air pollutants in the state of São Paulo. In this way, we can suggest that this number of monitoring stations used in this study may represent the “worst case of urban background stations”. In addition, according to WHO Air Quality Guidelines [
18], the assessment of PM levels can affect health in terms of long- and short-term exposure. Regarding short-term exposure, WHO points out that the 24-h average is useful for identifying pollution peaks that may be associated with increased morbidity. Thus, we decided to evaluate the range of PM levels for 24 h, in order to verify the possible occurrence of a peak of PM levels during the study period, which could impact the health of the volunteers in an acute way. It is important to mention that we did not observe a peak in PM levels during the 10 weeks between samples. Based on these pieces of information, all the data obtained from the monitoring stations can be considered to be representative of volunteers’ pollutant exposure due to their urban background.