Selection of Appropriate Thermal Indices for Applications in Human Biometeorological Studies
Abstract
1. Introduction
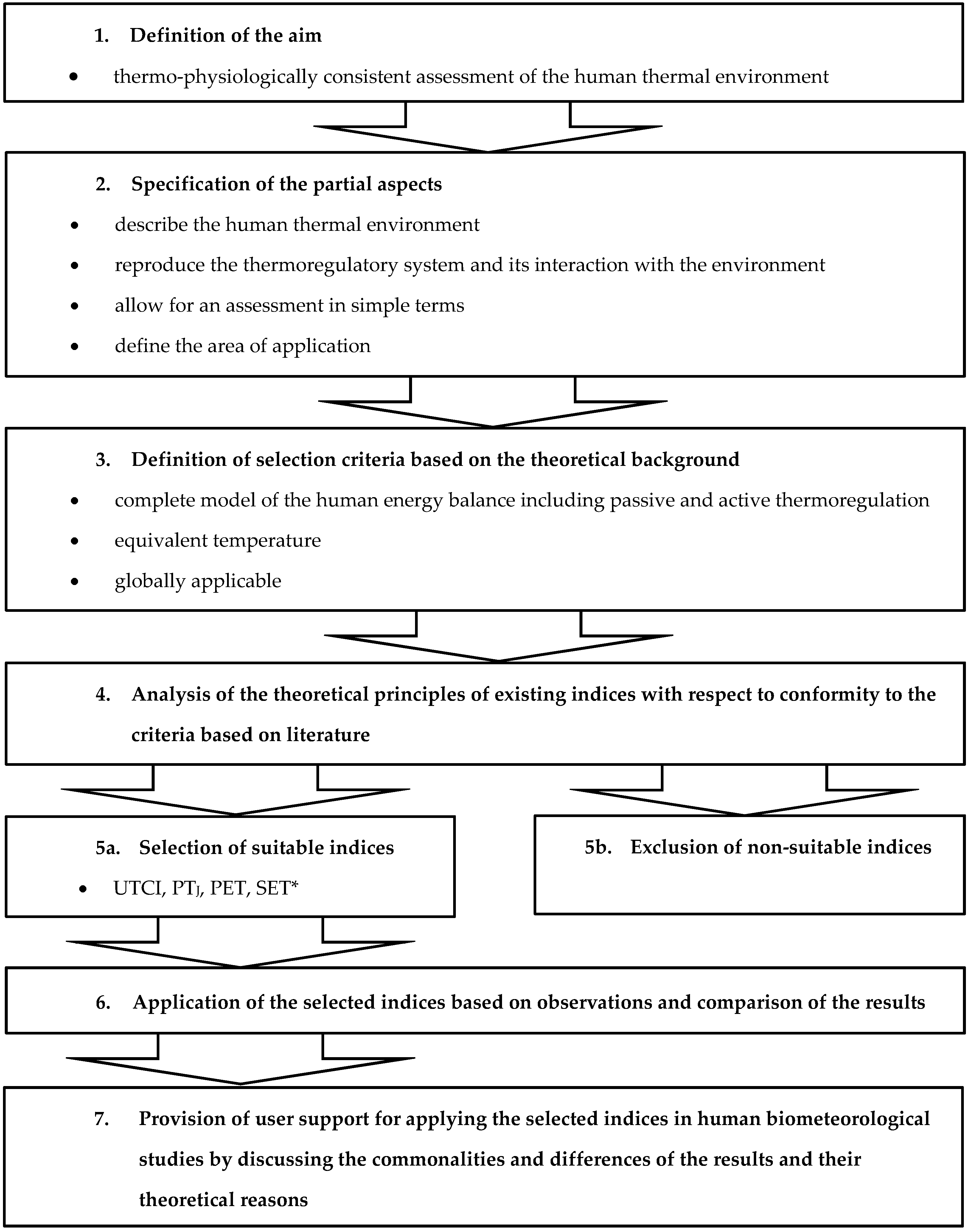
2. Method
- The index needs to be ascribable to models providing a “rational representation of the human body involving heat transfer between the body and the environment, the anthropometry and thermal properties of the body and a dynamic (transient) representation of the human thermoregulatory system [1,16]”. These are in first principles complete models of the human energy balance including passive and active thermoregulation which are integrated to steady state. If this is not achievable within an integration time of two hours [17], the physiological state at the end of the interval should be taken. In case this criterion is fulfilled the symbol ”M” is used in the further analysis, if not “m”.
- The index needs to take the form of an equivalent temperature, i.e., the air temperature of an isothermal (tmrt = ta) reference environment with minor wind velocity so that a reference subject will show identical (selected) thermo-physiological values in actual and in reference environment (symbol “T”, otherwise “t”). Concerning thermal sensation such an equivalent temperature has the advantage to be self-explanatory comparing it with the actual ambient temperature ta.
- The index needs to be worldwide applicable (symbol “W”, otherwise “w”), i.e., an index which not restricted to specific regions, such as the “Equatorial Comfort Index (ECI) [18]”.
- The index is non-suitable if it is not a whole body index, i.e., is restricted to only one part of the body (symbol “p”), such as the wind chill equivalent temperature (WCET) for the exposed facial skin [19].
- The index is non-suitable if it is a simulation device or a single meteorological parameter (symbol “s”), such as the “Kata Thermometer” [22] or the “Sultriness value” [23] for the dew-point temperature, because such physical or engineering approaches cannot account for the complex passive and active thermoregulation of man [1].
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Parsons, K.C. Environments. The Effects of Hot, Moderate, and Cold Environments on Human Health, Comfort and Performance, 2nd ed.; Taylor & Francis: London, UK; New York, NY, USA, 2003; p. 518. ISBN 0-415-23793-9. [Google Scholar]
- Herrmann, H. Die Schwüle—Eine Vergleichende Untersuchung. Ph.D. Thesis, Universität Köln, Köln, Germany, 1959; p. 76. [Google Scholar]
- Graveling, R.A.; Morris, L.A.; Graves, R.J. Working in Hot Conditions in Mining: A Literature Review; Historical Research Report TM/88/13; Institute of Occupational Medicine: Edinburgh, UK, 1988; p. 128. [Google Scholar]
- Epstein, Y.; Moran, D.S. Thermal comfort and the Heat Stress Indices. Ind. Health 2006, 44, 388–398. [Google Scholar] [CrossRef] [PubMed]
- Auliciems, A.; Szokolay, S.V. Thermal Comfort. PLEA Note 3; Second Revised Edition; University of Queensland: Brisbane, QLD, Austualia, 2007; p. 66. ISBN 0 86776 729 4. [Google Scholar]
- Pantavou, K.; Santamouris, M.; Asimakopoulos, D.; Theoharatos, G. Empirical calibration of thermal indices in an urban outdoor Mediterranean environment. Build. Environ. 2014, 80, 283–292. [Google Scholar] [CrossRef]
- De Freitas, C.R.; Grigorieva, E.A. A comprehensive catalogue and classification of human thermal climate indices. Int. J. Biometeorol. 2015, 59, 109–120. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, C.R.; Grigorieva, E.A. A comparison and appraisal of a comprehensive range of human thermal climate indices. Int. J. Biometeorol. 2017, 61, 487–512. [Google Scholar] [CrossRef] [PubMed]
- Potchter, O.; Cohen, P.; Lin, T.P.; Matzarakis, A. Outdoor human thermal perception in various climates: A comprehensive review of approaches, methods and quantification. Sci. Total Environ. 2018, 631–632, 390–406. [Google Scholar] [CrossRef] [PubMed]
- Guideline VDI 3787/Part 2. Environmental Meteorology, Methods for the Human Biometeorological Evaluation of Climate and Air Quality for Urban and Regional Planning at Regional Level: Part I: Climate. Kommission Reinhaltung der Luft im VDI und DIN-Normenausschuss KRdL; VDI/DIN Handbuch Reinhaltung der Luft, Band 1B: Umweltmeteorologie; Beuth-Verlag: Berlin, Germany, 2008.
- Aschoff, J.; Wever, R. Kern und Schale im Wärmehaushalt des Menschen. Naturwissenschaften 1958, 45, 477–485. [Google Scholar] [CrossRef]
- Pandolf, K.B.; Burr, R. (Eds.) Medical Aspects of Harsh Environments; Office of The Surgeon General at TMM Publications, Borden Institute, Walter Reed Army Medical Center: Washington, DC, USA, 2001; Volume 1, Available online: http://www.usariem.army.mil/pages/download/harshenvironmentsvol1.pdf (accessed on 28 July 2011).
- Hensel, H.; Schafer, K. Thermoreception and Temperature, Regulation in Man. In Recent Advances in Medical Thermology; Ring, E.F.J., Phillips, B., Eds.; Springer: Boston, MA, USA, 1984. [Google Scholar]
- Gagge, A.P.; Stolwijk, J.A.J.; Nishi, Y. An effective temperature scale based on a simple model of human physiological regulatory response. ASHRAE Trans. 1971, 77, 247–262. [Google Scholar]
- Fiala, D.; Lomas, K.J.; Stohrer, M. Computer prediction of human thermoregulatory and temperature responses to a wide range of environmental conditions. Int. J. Biometeorol. 2001, 45, 143–159. [Google Scholar] [CrossRef]
- Yokota, M.; Berglund, L.G.; Xu, X. Thermoregulatory modeling use and application in the military workforce. Appl. Ergon. 2014, 45, 663–670. [Google Scholar] [CrossRef]
- Höppe, P. Different aspects of assessing indoor and outdoor thermal comfort. Energy Build. 2002, 34, 661–665. [Google Scholar] [CrossRef]
- Webb, C.G. An analysis of some observations of thermal comfort in an equatorial climate. Br. J. Ind. Med. 1959, 16, 279–310. [Google Scholar] [CrossRef]
- OFCM. Report on Wind Chill Temperature and Extreme Heat Indices: Evaluation and Improvement Projects; FCM-R19-2003; US Department of Commerce, Federal Coordinator for Meteorological Services and Supporting Research: Washington, DC, USA, 2003; p. 75. Available online: http://www.ofcm.gov/jagti/r19-ti-plan/r19-ti-plan.htm (accessed on 15 November 2006).
- Rothfusz, L.P. The Heat Index “Equation” (or, more than you ever Wanted to Know about Heat Index). NWS Southern Region Technical Attachment 1990, SR/SSD 90-23; Fort Worth, TX, USA, 1990; p. 2. Available online: https://www.weather.gov/media/bgm/ta_htindx.PDF (accessed on 17 April 2010).
- Steadman, R.G. The Assessment of Sultriness. Part II: Effects of Wind, Extra Radiation and Barometric Pressure on Apparent Temperature. J. Appl. Meteor. 1979, 18, 874–885. [Google Scholar] [CrossRef]
- Hill, L.; Griffith, O.W.; Flack, M. The measurement of the rate of heat-loss at body temperature by convection, radiation, and evaporation. Philos. Trans. R. Soc. Lond. Ser. B Contain. Pap. Biol. Character 1916, 207, 183–220. [Google Scholar] [CrossRef]
- Scharlau, K. Die Schwüle als meßbare Größe. Bioklim. Beibl. 1943, 10, 19–23. [Google Scholar]
- IUPS Glossary of Terms for Thermal Physiology. 3rd Ed. revised by The Commission for Thermal Physiology of the International Union of Physiological Sciences (IUPS Thermal Commission). J. Ther. Biol. 2003, 28, 75–106. [CrossRef]
- Gallagher, M. Development of a perceptual hyperthermia index to evaluate heat strain during treadmill exercise. Eur. J. Appl. Physiol. 2012, 112, 2025–2034. [Google Scholar] [CrossRef] [PubMed]
- Upton, G.; Cook, I. A Dictionary of Statistics; University Press: Oxford, UK, 2002; p. 464. [Google Scholar]
- Blazejczyk, K.; Matzarakis, A. Assessment of bioclimatic differentiation of Poland based on the human heat balance. Geogr. Pol. 2007, 80, 63–82. [Google Scholar]
- Fanger, P.O. Thermal Comfort. Analysis and Applications in Environmental Engineering; McGraw-Hill Company: Detroit, MI, USA, 1972; p. 244. [Google Scholar]
- ASHRAE. ASHRAE Handbook: Fundamentals, 8; American Society of Heating and Air-Conditioning Engineers: Atlanta, GA, USA, 2001; ISBN 1-931862-70-2. [Google Scholar]
- Gagge, A.P.; Fobelets, A.P.; Berglund, P.E. A Standard Predictive Index of Human Response to the Thermal Environment. ASHRAE Trans. 1986, 92, 709–731. [Google Scholar]
- Staiger, H.; Laschewski, G.; Grätz, A. The perceived temperature – a versatile index for the assessment of the human thermal environment. Part A: Scientific basics. Int. J. Biometeorol. 2012, 56, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Nagano, K.; Horikoshi, T. New index indicating the universal and separate effects on human comfort under outdoor and non-uniform thermal conditions. Energy Build. 2011, 43, 1694–1701. [Google Scholar] [CrossRef]
- Steadman, R.G. A universal scale of apparent temperature. J. Appl. Meteorol. 1984, 23, 1677–1687. [Google Scholar] [CrossRef]
- Steadman, R.G. Indices of windchill of clothed persons. J. Appl. Meteorol. 1971, 10, 674–683. [Google Scholar] [CrossRef]
- Steadman, R.G. Norms of apparent temperature in Australia. Austr. Meteorol. Mag. 1994, 43, 1–16. [Google Scholar]
- De Freitas, C.R. Assessment of human bioclimate based on thermal response. Int. J. Biometeorol. 1985, 29, 97–119. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, C.R. Human Thermal Climates of New Zealand; New Zealand Meteorological Service, Miscellaneous Publication: Wellington, New Zealand, 1986. [Google Scholar]
- De Freitas, C.R.; Ryken, M.G. Climate and physiological heat strain during exercise. Int. J. Biometeorol. 1989, 33, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Fanger, P.O.; Melikov, A.K.; Hanzawa, H.; Ring, J. Air turbulence and sensation of draught. Energy Build. 1988, 12, 21–39. [Google Scholar] [CrossRef]
- Jendritzky, G.; Havenith, G.; Weihs, P.; Batchvarova, E. Towards a Universal Thermal Climate Index UTCI for Assessing the Thermal Environment of the Human Being; COST Action 730 on UTCI: Freiburg, Germany, 2009. [Google Scholar]
- Jendritzky, G.; de Dear, R.; Havenith, G. UTCI—Why another thermal index? Int. J. Biometeorol. 2012, 56, 421–428. [Google Scholar] [CrossRef] [PubMed]
- Fiala, D.; Havenith, G.; Bröde, P.; Kampmann, B.; Jendritzky, G. UTCI-Fiala multi-node model of human heat transfer and temperature regulation. Int. J. Biometeorol. 2012, 56, 429–441. [Google Scholar] [CrossRef]
- Havenith, G.; Fiala, D.; Blazejczyk, K.; Richards, M.; Bröde, P.; Holmer, I.; Rintanmaki, H.; Benshabat, Y.; Jendritzky, G. The UTCI-clothing model. Int. J. Biometeorol. 2012, 56, 461–470. [Google Scholar] [CrossRef]
- Bröde, P.; Fiala, D.; Blazejczyk, K.; Holmer, I.; Jendritzky, G.; Kampmann, B.; Tinz, B.; Havenith, G. Deriving the operational procedure for the Universal Thermal Climate Index (UTCI). Int. J. Biometeorol. 2012, 56, 481–494. [Google Scholar] [CrossRef]
- Jendritzky, G.; Staiger, H.; Bucher, K.; Graetz, A.; Laschewski, G. The Perceived Temperature—The Method of the Deutscher Wetterdienst for the Assessment of Cold Stress and Heat Load for the Human Body. In Proceedings of the Internet Workshop on Windchill, Windchill-Conference, Canada, 3–7 April 2000; Available online: http://ec.gc.ca/workshop/papers/pdf/session_1_paper_4_e.pdf (accessed on 8 April 2000).
- Mayer, H.; Höppe, P. Thermal comfort of man in different urban environments. Theor. Appl. Climatol. 1987, 38, 43–49. [Google Scholar] [CrossRef]
- Höppe, P. The physiological equivalent temperature—A universal index for the biometeorological assessment of the thermal environment. Int. J. Biometeorol. 1999, 43, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Höppe, P. Die Energiebilanz des Menschen; Universitat Munchen, Meteorologisches Institut: München, Germany, 1984; p. 194. [Google Scholar]
- Gonzalez, R.R.; Nishi, Y.; Gagge, A.P. Experimental evaluation of Standard Effective Temperature. A new biometeorological index of man’s thermal discomfort. Int. J. Biometeorol. 1974, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pickup, J.; de Dear, R.J. An outdoor thermal comfort index (OUT-SET*)—Part I—The model and its assumptions. In Biometeorology and Urban Climatology at the Turn of the Millennium, Proceedings of the Conference ICB-ICUC’99, Sydney, Australia, 8–12 November 1999; de Dear, R.J., Kalma, J.D., Oke, T.R., Auliciems, A., Eds.; World Meteorological Organization: Geneva, Switzerland, 2000; pp. 279–283. [Google Scholar]
- Park, S.; Tuller, S.E. Comparison of human radiation exchange models in outdoor areas. Theor. Appl. Climatol. 2011, 105, 357–370. [Google Scholar] [CrossRef]
- Nishi, Y.; Gagge, A.P. Humid operative temperature: A biophysical index of thermal sensation and discomfort. J. Physiol. (Paris) 1971, 63, 365–368. [Google Scholar]
- Stolwijk, J.A.J. A Mathematical Model of Physiological Temperature Regulation in Man. NASA Contract Report 1855; Maryland, 1971; p. 78. Available online: http://ntrs.nasa.gov/archive/nasa/casi.ntrs.nasa.gov/19710023925_1971023925.pdf (accessed on 2 August 2011).
- Stolwijk, J.A.J.; Hardy, J.D. Temperature regulation in man—A theoretical study. Pflügers Arch. 1966, 291, 129–162. [Google Scholar] [CrossRef]
- Jendritzky, G.; Fiala, D.; Havenith, G.; Koppe, C.; Laschewski, G.; Staiger, H.; Tinz, B. Thermische Umweltbedingungen. Promet 2007, 33, 83–94. [Google Scholar]
- Brown, R.D.; Gillespie, T.G. Estimating outdoor thermal comfort using a cylindrical radiation thermometer and an energy budget model. Int. J. Biometeorol. 1986, 30, 43–52. [Google Scholar] [CrossRef]
- Kenny, N.A.; Warland, J.S.; Brown, R.D.; Gillespie, T.G. Part A: Assessing the performance of the COMFA outdoor thermal comfort model on subjects performing physical activity, Part B: Revisions to the COMFA outdoor thermal comfort model for application to subjects performing physical activity. Int. J. Biometeorol. 2009, 53, 415–441. [Google Scholar] [CrossRef]
- Huizenga, C.; Hui, Z.; Arens, E. A model of human physiology and comfort for assessing complex thermal environments. Build. Environ. 2001, 36, 691–699. [Google Scholar] [CrossRef]
- Tanabe, S.-I.; Kobayashi, K.; Nakamo, J.; Ozeki, Y.; Konishi, M. Evaluation of thermal comfort using multi-node thermoregulation (65MN) and radiation models and computational fluid dynamics (CFD). Energy Build. 2002, 34, 637–646. [Google Scholar] [CrossRef]
- Fiala, D.; Lomas, K.J.; Stohrer, M. First principles modelling of thermal sensation response in steady-state and transient conditions. ASHRAE Trans. 2003, 109, 179–188. [Google Scholar]
- Zhang, H.; Arens, E.; Huizenga, C.; Han, T. Thermal sensation and comfort models for non-uniform and transient environments: Part I: Local sensation of individual body parts, Part II::Local comfort of individual body parts, Part III: Whole-body sensation and comfort. Building and Environment 2010, 45, 380–410. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Matzarakis, A. Modified physiologically equivalent temperature—Basics and applications for western European climate. Theor. Appl. Climatol. 2018, 132, 1275–1289. [Google Scholar] [CrossRef]
- Pennes, H.H. Analysis of tissue and arterial blood temperatures in the resting human forearm. J. Appl. Physiol. 1948, 85, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Koppe, C.; Jendritzky, G. Inclusion of short-term adaptation to thermal stresses in a heat load warning procedure. Meteorol. Z. 2005, 14, 271–278. [Google Scholar] [CrossRef]
- Jendritzky, G.; Tinz, B. The thermal environment of the human being on the global scale. Glob. Health Action 2009, 2, 1021. [Google Scholar] [CrossRef] [PubMed]
- Matzarakis, A.; Amelung, B. Physiologically equivalent temperature as indicator for impacts of climate change on thermal comfort of humans. In Seasonal Forecasts, Climatic Change and Human Health; Thomson, M.C., Garcia-Herrera, R., Beniston, M., Eds.; Springer: Dordrecht, The Netherlands, 2008; pp. 161–172. [Google Scholar]
- Giannaros, T.M.; Kotroni, V.; Lagouvardos, K.; Matzarakis, A. Climatology and trends of the Euro-Mediterranean thermal bioclimate. Int. J. Climatol. 2018, 38, 3290–3308. [Google Scholar] [CrossRef]

| Criterion | Symbol in Case Index Is Suitable | Symbol in Case Index Is Non-Suitable |
|---|---|---|
| complete model of the human energy balance including passive and active thermoregulation | M | m |
| equivalent temperature | T | t |
| worldwide applicable | W | w |
| restricted to only one part of the body | - | p |
| defined exclusively for warm/humid/dry or for cold environments (regional in climatological terms) | - | r |
| simulation device or a single meteorological parameter | - | s |
| Classification | Category | Amount | Not Suitable (Amount) | Reasons | Principally Suitable (Amount) | Reasons |
|---|---|---|---|---|---|---|
| Simulation devices for integrated measurements | A | 11 | 11 | s | -- | |
| Single sensor (parameter) index | B | 6 | 6 | s | -- | |
| Algebraic or statistical models | C | 37 | 37 | m, p, t, r | -- | |
| Proxy thermal strain index | D | 14 | 14 | m, t, r | -- | |
| Proxy thermal stress index | E | 16 | 16 | m(?), w, p, t, r | -- | |
| Energy balance strain index | F | 28 | 28 | m(?), r, t | -- | |
| Energy balance stress index | G | 42 | 30 | m(?), r, t | 7 | M, W, T |
| 1 | M, W, t | |||||
| 4 | M(?), W, t | |||||
| Special purpose index | H | 11 | 11 | m(?), w, r, t | -- | |
| Sum | 165 | 153 | 12 |
| Category | Index | Energy Balance Stress Index | Authors | Suitability | VDI Selected | Identical with/Included in | Adaptation |
|---|---|---|---|---|---|---|---|
| G | UTCI | Universal Thermal Climate Index | [40,41,42,43,44] | MWT | Y | Y | |
| G | PTj | Perceived Temperature | [31,45] | MWT | Y | Y | |
| G | PET | Physiologically Equivalent Temperature | [46,47] | MWT | Y | N | |
| G | SET* | Standard Effective Temperature | [30,49] | MWT | Y | N | |
| G | OUT_SET* | Standard Effective Temperature Outdoors | [30,49,50] | MWT | N | SET* | N |
| G | ET* | New Effective Temperature | [14] | MWT | N | ET*/SET*/PMV* | N |
| G | HToh | Humid Operative Temperature | [14,30,52] | MWT | N | ET*/SET* | N |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Staiger, H.; Laschewski, G.; Matzarakis, A. Selection of Appropriate Thermal Indices for Applications in Human Biometeorological Studies. Atmosphere 2019, 10, 18. https://doi.org/10.3390/atmos10010018
Staiger H, Laschewski G, Matzarakis A. Selection of Appropriate Thermal Indices for Applications in Human Biometeorological Studies. Atmosphere. 2019; 10(1):18. https://doi.org/10.3390/atmos10010018
Chicago/Turabian StyleStaiger, Henning, Gudrun Laschewski, and Andreas Matzarakis. 2019. "Selection of Appropriate Thermal Indices for Applications in Human Biometeorological Studies" Atmosphere 10, no. 1: 18. https://doi.org/10.3390/atmos10010018
APA StyleStaiger, H., Laschewski, G., & Matzarakis, A. (2019). Selection of Appropriate Thermal Indices for Applications in Human Biometeorological Studies. Atmosphere, 10(1), 18. https://doi.org/10.3390/atmos10010018





