A Concise Review on Tissue Engineered Artificial Skin Grafts for Chronic Wound Treatment: Can We Reconstruct Functional Skin Tissue In Vitro?
Abstract
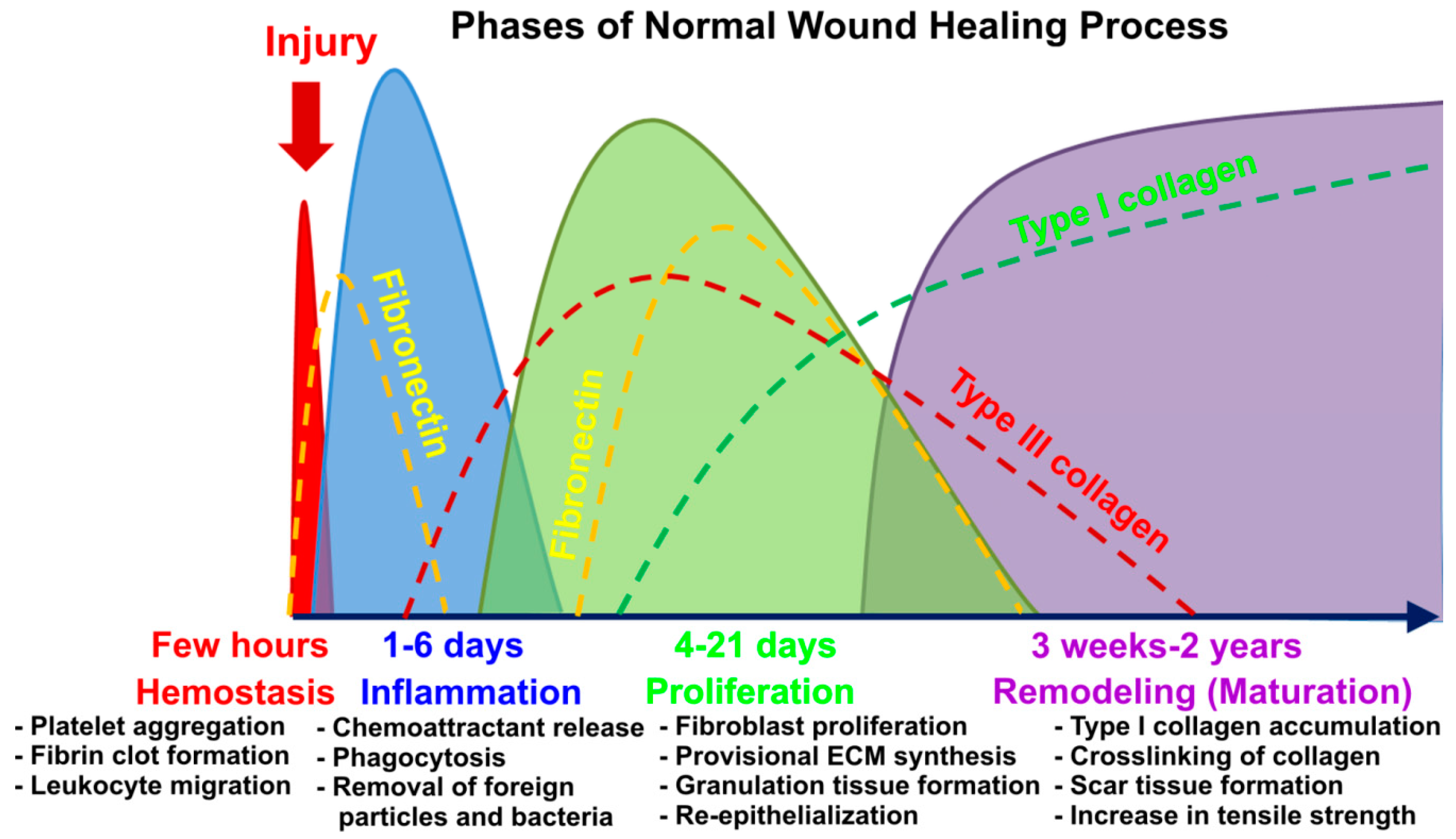
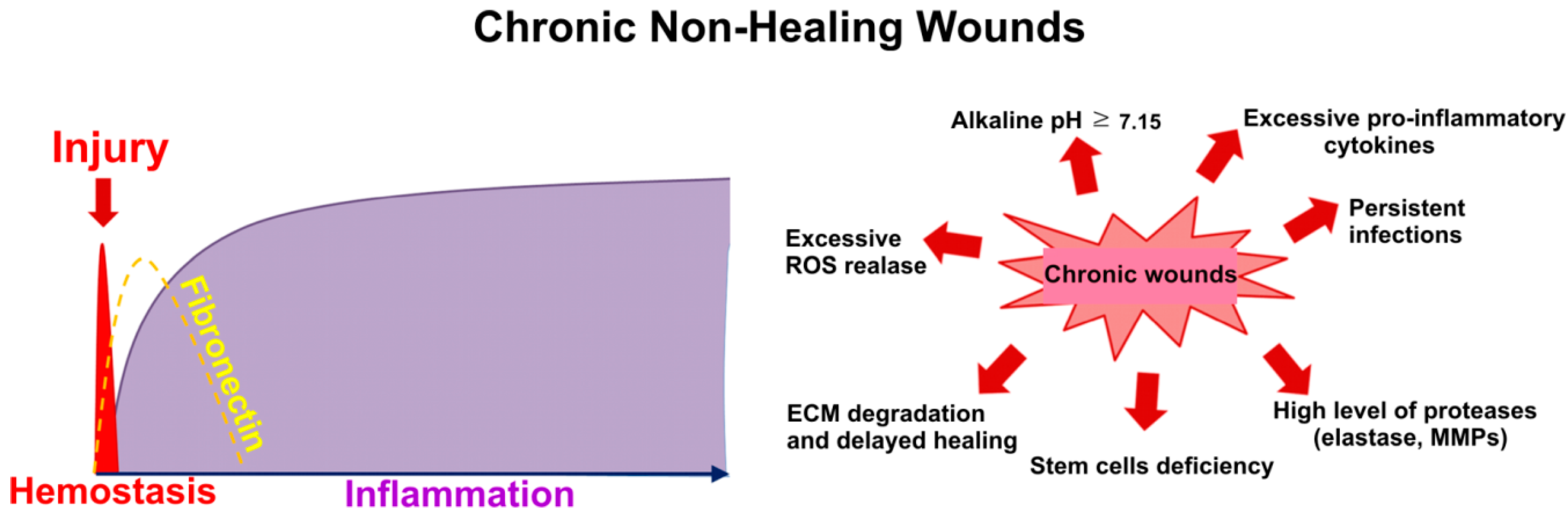
1. Introduction to the Problem of Chronic Wounds
2. Common Therapies for Chronic Wounds
2.1. Skin Transplantation
2.2. Administration of Anti-Inflammatory and Anti-Oxidant Agents
2.3. Administration of Growth Factors and Protease Inhibitors
3. Modern Approaches to Chronic Wound Treatment
3.1. Topical Delivery of Adult Stem Cells’ Suspension
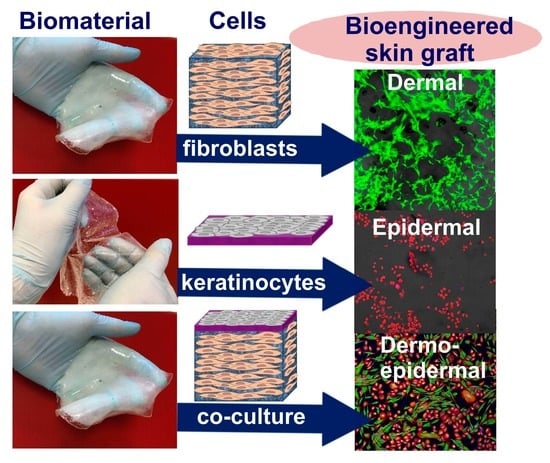
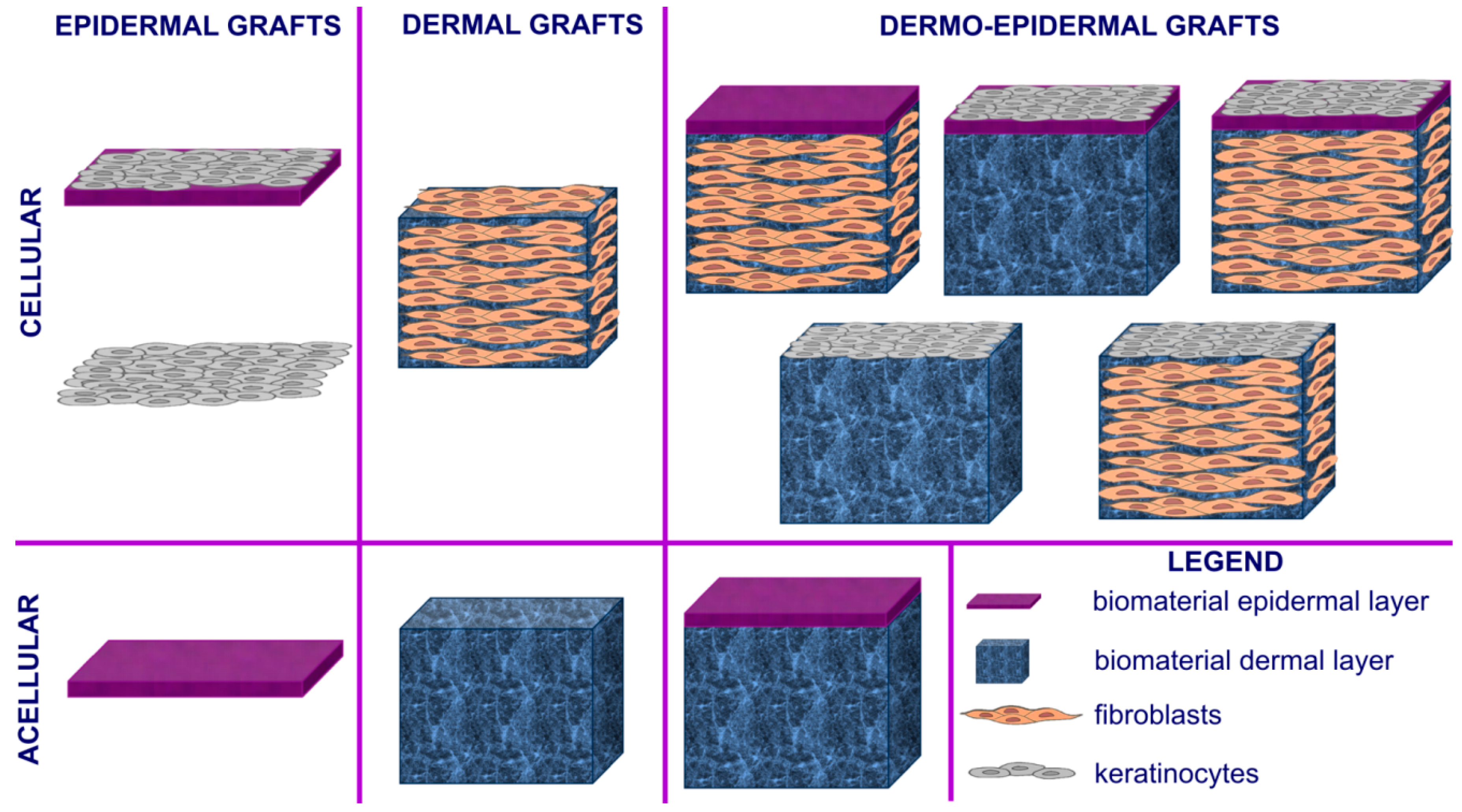
3.2. Skin Tissue Engineering
3.2.1. Cells Used for Cellular Skin Graft Production
3.2.2. Biomaterials Used for Skin Graft Production
3.2.3. Nanocomposite Artificial Skin Grafts with Antibacterial Properties
3.2.4. Reconstruction of Skin Appendages, Pigmentation, and Nerves Using Artificial Skin Grafts
3.2.5. Commercially Available Skin Grafts
4. Concluding Remarks
Funding
Acknowledgments
Conflicts of Interest
References
- Urciuolo, F.; Casale, C.; Imparato, G.; Netti, P.A. Bioengineered Skin Substitutes: The Role of Extracellular Matrix and Vascularization in the Healing of Deep Wounds. J. Clin. Med. 2019, 8, 2083. [Google Scholar] [CrossRef] [PubMed]
- Vig, K.; Chaudhari, A.; Tripathi, S.; Dixit, S.; Sahu, R.; Pillai, S.; Dennis, V.A.; Singh, S.R. Advances in skin regeneration using tissue engineering. Int. J. Mol. Sci. 2017, 18, 789. [Google Scholar] [CrossRef] [PubMed]
- Randall, M.J.; Jüngel, A.; Rimann, M.; Wuertz-Kozak, K. Advances in the biofabrication of 3D skin in vitro: Healthy and pathological models. Front. Bioeng. Biotechnol. 2018, 6, 154. [Google Scholar] [CrossRef] [PubMed]
- Sood, A.; Granick, M.S.; Tomaselli, N.L. Wound Dressings and Comparative Effectiveness Data. Adv. Wound Care 2014, 3, 511–529. [Google Scholar] [CrossRef]
- Dhivya, S.; Padma, V.V.; Santhini, E. Wound dressing—A review. BioMedicine 2015, 5, 24–28. [Google Scholar] [CrossRef]
- Laurens, N.; Koolwijk, P.; de Maat, M.P. Fibrin structure and wound healing. J. Thromb. Haemost. 2006, 4, 932–939. [Google Scholar] [CrossRef]
- Larouche, J.; Sheoran, S.; Maruyama, K.; Martino, M.M. Immune regulation of skin wound healing: Mechanisms and novel therapeutic targets. Adv. Wound Care 2018, 7, 209–231. [Google Scholar] [CrossRef]
- Frykberg, R.G.C.; Banks, J. Challenges in the Treatment of Chronic Wounds. Adv. Wound Care 2015, 4, 560–582. [Google Scholar] [CrossRef]
- Jaller, J.A.; Herskovitz, I.; Borda, L.J.; Mervis, J.; Darwin, E.; Hirt, P.A.; Lev-Tov, H.; Kirsner, R.S. Evaluation of Donor Site Pain after Fractional Autologous Full-Thickness Skin Grafting. Adv. Wound Care 2018, 7, 309–314. [Google Scholar] [CrossRef]
- Patterson, C.W.; Stark, M.; Sharma, S.; Mundinger, G.S. Regeneration and expansion of autologous full-thickness skin through a self-propagating autologous skin graft technology. Clin. Case Rep. 2019, 7, 2449–2455. [Google Scholar] [CrossRef]
- Everts, P.A.M.; Warbout, M.; de Veth, D.; Cirkel, M.; Spruijt, N.E.; Buth, J. Use of epidermal skin grafts in chronic wounds: A case series. Int. Wound J. 2017, 14, 1213–1218. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.C.; Chen, D.; Guo, D.; Liang, Y.Y.; Zhang, J.; Zhu, J.Y.; Tang, B. Randomized clinical trial of autologous skin cell suspension combined with skin grafting for chronic wounds. Br. J. Surg. 2015, 102, 117–123. [Google Scholar] [CrossRef]
- Pérez-Recalde, M.; Ruiz Arias, I.E.; Hermida, É.B. Could essential oils enhance biopolymers performance for wound healing? A systematic review. Phytomedicine 2018, 38, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Orhan, I.E.; Mesaik, M.A.; Jabeen, A.; Kan, Y. Immunomodulatory properties of various natural compounds and essential oils through modulation of human cellular immune response. Ind. Crops Prod. 2016, 81, 117–122. [Google Scholar] [CrossRef]
- Kim, D.S.; Lee, H.J.; Jeon, Y.D.; Han, Y.H.; Kee, J.Y.; Kim, H.J.; Shin, H.J.; Kang, J.; Lee, B.S.; Kim, S.H.; et al. Alpha-Pinene Exhibits Anti-Inflammatory Activity Through the Suppression of MAPKs and the NF-κB Pathway in Mouse Peritoneal Macrophages. Am. J. Chin. Med. 2015, 43, 731–742. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Yang, K.W.; Kim, S.S.; Park, S.M.; Park, K.J.; Kim, K.S.; Choi, Y.H.; Cho, K.K.; Lee, N.H.; Hyun, C.G. Chemical composition and anti-inflammatory effects of essential oil from Hallabong flower. EXCLI J. 2013, 12, 933–942. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Yan, J.; Sun, Z. D-limonene exhibits anti-inflammatory and antioxidant properties in an ulcerative colitis rat model via regulation of iNOS, COX-2, PGE2 and ERK signaling pathways. Mol. Med. Rep. 2017, 15, 2339–2346. [Google Scholar] [CrossRef]
- Da Silva, S.M.M.; Costa, C.R.R.; Gelfuso, G.M.; Guerra, E.N.S.; De Medeiros Nóbrega, Y.K.; Gomes, S.M.; Pic-Taylor, A.; Fonseca-Bazzo, Y.M.; Silveira, D.; De Oliveira Magalhães, P. Wound healing effect of essential oil extracted from eugenia dysenterica DC (Myrtaceae) leaves. Molecules 2019, 24, 2. [Google Scholar] [CrossRef]
- Mori, H.M.; Kawanami, H.; Kawahata, H.; Aoki, M. Wound healing potential of lavender oil by acceleration of granulation and wound contraction through induction of TGF-β in a rat model. BMC Complement. Altern. Med. 2016, 16, 144. [Google Scholar] [CrossRef]
- Costa, M.F.; Durço, A.O.; Rabelo, T.K.; Barreto, R.D.S.S.; Guimarães, A.G. Effects of Carvacrol, Thymol and essential oils containing such monoterpenes on wound healing: A systematic review. J. Pharm. Pharmacol. 2019, 71, 141–155. [Google Scholar] [CrossRef]
- Saporito, F.; Sandri, G.; Bonferoni, M.C.; Rossi, S.; Boselli, C.; Cornaglia, A.I.; Mannucci, B.; Grisoli, P.; Vigani, B.; Ferrari, F. Essential oil-loaded lipid nanoparticles for wound healing. Int. J. Nanomed. 2018, 13, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Maugeri, A.; Favara, G.; San Lio, R.M.; Evola, G.; Agodi, A.; Basile, G. Nutrition and wound healing: An overview focusing on the beneficial effects of curcumin. Int. J. Mol. Sci. 2019, 20, 1119. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, C.; Sahoo, S.K. Curcumin and its topical formulations for wound healing applications. Drug Discov. Today 2017, 22, 1582–1592. [Google Scholar] [CrossRef] [PubMed]
- Rosique, R.G.; Rosique, M.J.; Farina Junior, J.A. Curbing inflammation in skin wound healing: A review. Int. J. Inflam. 2015, 2015, 316235. [Google Scholar] [CrossRef]
- Kant, V.; Gopal, A.; Pathak, N.N.; Kumar, P.; Tandan, S.K.; Kumar, D. Antioxidant and anti-inflammatory potential of curcumin accelerated the cutaneous wound healing in streptozotocin-induced diabetic rats. Int. Immunopharmacol. 2014, 20, 322–330. [Google Scholar] [CrossRef]
- Moura, L.I.F.; Dias, A.M.A.; Suesca, E.; Casadiegos, S.; Leal, E.C.; Fontanilla, M.R.; Carvalho, L.; de Sousa, H.C.; Carvalho, E. Neurotensin-loaded collagen dressings reduce inflammation and improve wound healing in diabetic mice. Biochim. Biophys. Acta Mol. Basis Dis. 2014, 1842, 32–43. [Google Scholar] [CrossRef]
- Sandhu, V.K.; Alavi, A. The role of anti-tumour necrosis factor in wound healing: A case report of refractory ulcerated necrobiosis lipoidica treated with adalimumab and review of the literature. SAGE Open Med. Case Rep. 2019, 7. [Google Scholar] [CrossRef]
- Stacey, M. Combined topical growth factor and protease inhibitor in chronic wound healing: Protocol for a randomized controlled proof-of-concept study. J. Med. Internet Res. 2018, 7, e97. [Google Scholar] [CrossRef]
- Jones, I.; Nguyen, T.T.; Peng, Z.; Chang, M. Targeting MMP-9 in Diabetic Foot Ulcers. Pharmaceuticals 2019, 12, 79. [Google Scholar] [CrossRef]
- Han, G.; Ceilley, R. Chronic Wound Healing: A Review of Current Management and Treatments. Adv. Ther. 2017, 34, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Cullen, B.; Smith, R.; Mcculloch, E.; Silcock, D.; Morrison, L. Mechanism of action of PROMOGRAN, a protease modulating matrix, for the treatment of diabetic foot ulcers. Wound Repair Regen. 2002, 10, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.; Bernardo, M.M.; Li, Z.H.; Kotra, L.P.; Tanaka, Y.; Fridman, R.; Mobashery, S. Potent and selective mechanism-based inhibition of gelatinases. J. Am. Chem. Soc. 2000, 122, 6799–6800. [Google Scholar] [CrossRef]
- Gooyit, M.; Lee, M.; Schroeder, V.A.; Ikejiri, M.; Suckow, M.A.; Mobashery, S.; Chang, M. Selective water-soluble gelatinase inhibitor prodrugs. J. Med. Chem. 2011, 54, 6676–6690. [Google Scholar] [CrossRef][Green Version]
- Gao, M.; Nguyen, T.T.; Suckow, M.A.; Wolter, W.R.; Gooyit, M.; Mobashery, S.; Chang, M. Acceleration of diabetic wound healing using a novel proteaseanti-protease combination therapy. Proc. Natl. Acad. Sci. USA 2015, 112, 15226–15231. [Google Scholar] [CrossRef] [PubMed]
- Coalson, E.; Bishop, E.; Liu, W.; Feng, Y.; Spezia, M.; Liu, B.; Shen, Y.; Wu, D.; Du, S.; Li, A.J.; et al. Stem cell therapy for chronic skin wounds in the era of personalized medicine: From bench to bedside. Genes Dis. 2019, 6, 342–358. [Google Scholar] [CrossRef]
- Fathke, C. Contribution of Bone Marrow-Derived Cells to Skin: Collagen Deposition and Wound Repair. Stem Cells 2004, 22, 812–822. [Google Scholar] [CrossRef]
- Bluff, J.E.; Ferguson, M.W.J.; O’Kane, S.; Ireland, G. Bone marrow-derived endothelial progenitor cells do not contribute significantly to new vessels during incisional wound healing. Exp. Hematol. 2007, 35, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Rehman, J.; Li, J.; Orschell, C.M.; March, K.L. Peripheral blood “endothelial progenitor cells” are derived from monocyte/macrophages and secrete angiogenic growth factors. Circulation 2003, 107, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Kazimierczak, P.; Benko, A.; Nocun, M.; Przekora, A. Novel chitosan/agarose/hydroxyapatite nanocomposite scaffold for bone tissue engineering applications: Comprehensive evaluation of biocompatibility and osteoinductivity with the use of osteoblasts and mesenchymal stem cells. Int. J. Nanomed. 2019, 14, 6615–6630. [Google Scholar] [CrossRef] [PubMed]
- Atalay, S.; Coruh, A.; Deniz, K. Stromal vascular fraction improves deep partial thickness burn wound healing. Burns 2014, 40, 1375–1383. [Google Scholar] [CrossRef]
- Zhu, M.; Xue, J.; Lu, S.; Yuan, Y.; Liao, Y.; Qiu, J.; Liu, C.; Liao, Q. Anti-inflammatory effect of stromal vascular fraction cells in fat transplantation. Exp. Ther. Med. 2019, 17, 1435–1439. [Google Scholar] [CrossRef]
- Bowles, A.C.; Wise, R.M.; Gerstein, B.Y.; Thomas, R.C.; Ogelman, R.; Febbo, I.; Bunnell, B.A. Immunomodulatory Effects of Adipose Stromal Vascular Fraction Cells Promote Alternative Activation Macrophages to Repair Tissue Damage. Stem Cells 2017, 35, 2198–2207. [Google Scholar] [CrossRef]
- Karina, K.; Rosadi, I.; Sobariah, S.; Afini, I.; Widyastuti, T.; Rosliana, I. Comparable effect of adipose-derived stromal vascular fraction and mesenchymal stem cells for wound healing: An in vivo study. Biomed. Res. Ther. 2019, 6, 3412–3421. [Google Scholar] [CrossRef]
- Sun, M.; He, Y.; Zhou, T.; Zhang, P.; Gao, J.; Lu, F. Adipose Extracellular Matrix/Stromal Vascular Fraction Gel Secretes Angiogenic Factors and Enhances Skin Wound Healing in a Murine Model. Biomed. Res. Int. 2017, 2017, 3105780. [Google Scholar] [CrossRef]
- Deng, C.; Wang, L.; Feng, J.; Lu, F. Treatment of human chronic wounds with autologous extracellular matrix/stromal vascular fraction gel: A STROBE-compliant study. Medicine 2018, 97, e11667. [Google Scholar] [CrossRef] [PubMed]
- Dixit, S.; Baganizi, D.R.; Sahu, R.; Dosunmu, E.; Chaudhari, A.; Vig, K.; Pillai, S.R.; Singh, S.R.; Dennis, V.A. Immunological challenges associated with artificial skin grafts: Available solutions and stem cells in future design of synthetic skin. J. Biol. Eng. 2017, 11, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Varkey, M.; Ding, J.; Tredget, E. Advances in Skin Substitutes—Potential of Tissue Engineered Skin for Facilitating Anti-Fibrotic Healing. J. Funct. Biomater. 2015, 6, 547–563. [Google Scholar] [CrossRef] [PubMed]
- Nathoo, R.; Howe, N.; Cohen, G. Skin substitutes: An overview of the key players in wound management. J. Clin. Aesthet. Dermatol. 2014, 7, 44–48. [Google Scholar] [PubMed]
- Kaur, A.; Midha, S.; Giri, S.; Mohanty, S. Functional skin grafts: Where biomaterials meet stem cells. Stem Cells Int. 2019, 2019, 1286054. [Google Scholar] [CrossRef]
- Savoji, H.; Godau, B.; Hassani, M.S.; Akbari, M. Skin Tissue Substitutes and Biomaterial Risk Assessment and Testing. Front. Bioeng. Biotechnol. 2018, 6, 86. [Google Scholar] [CrossRef]
- Paggiaro, A.O.; Mathor, M.B.; Teodoro, W.R.; Isaac, C.; Capelozzi, V.L.; Gemperli, R. Evaluation of Radiosterilized Glyercerolated Amniotic Membranes as a Substrate for Cultured Human Epithelial Cells. Organogenesis 2020, 16, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Przekora-Kusmierz, A.; Vivcharenko, V.; Kazimierczak, P. Hydrożelowy Substytut Skóry na Bazie Agarozy i Chitozanu Oraz Sposób jego Wytwarzania. PL Patent Application P.430458, 1 July 2019. [Google Scholar]
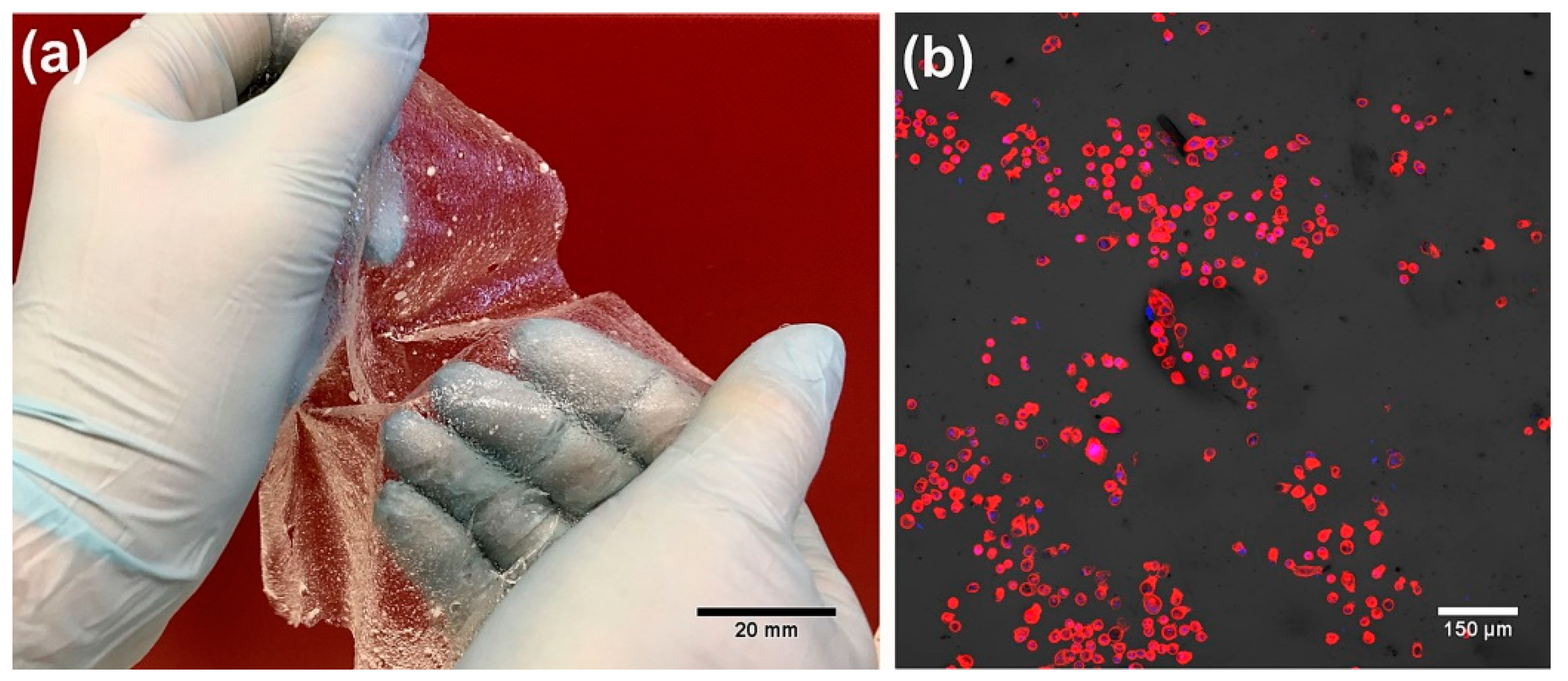
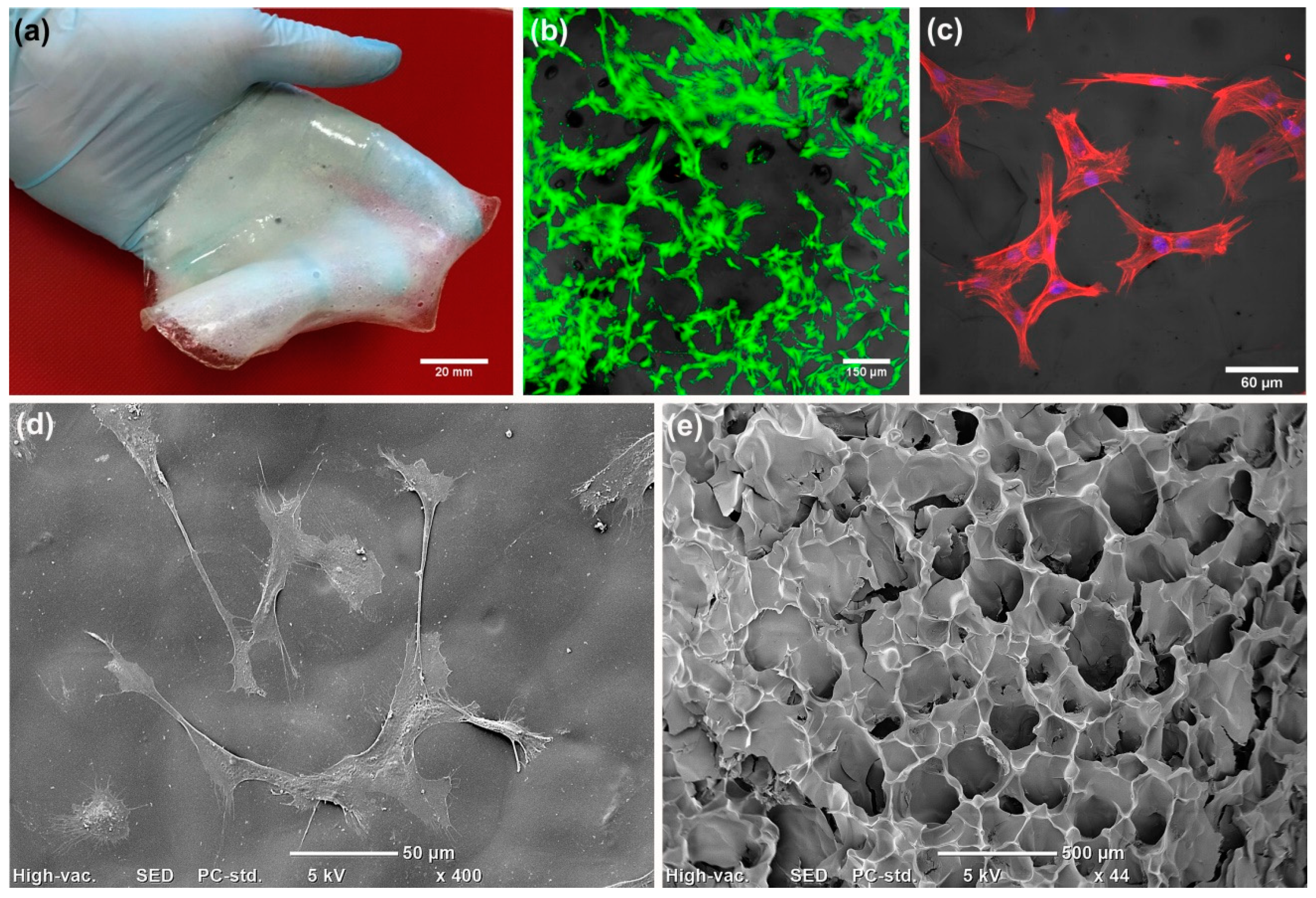
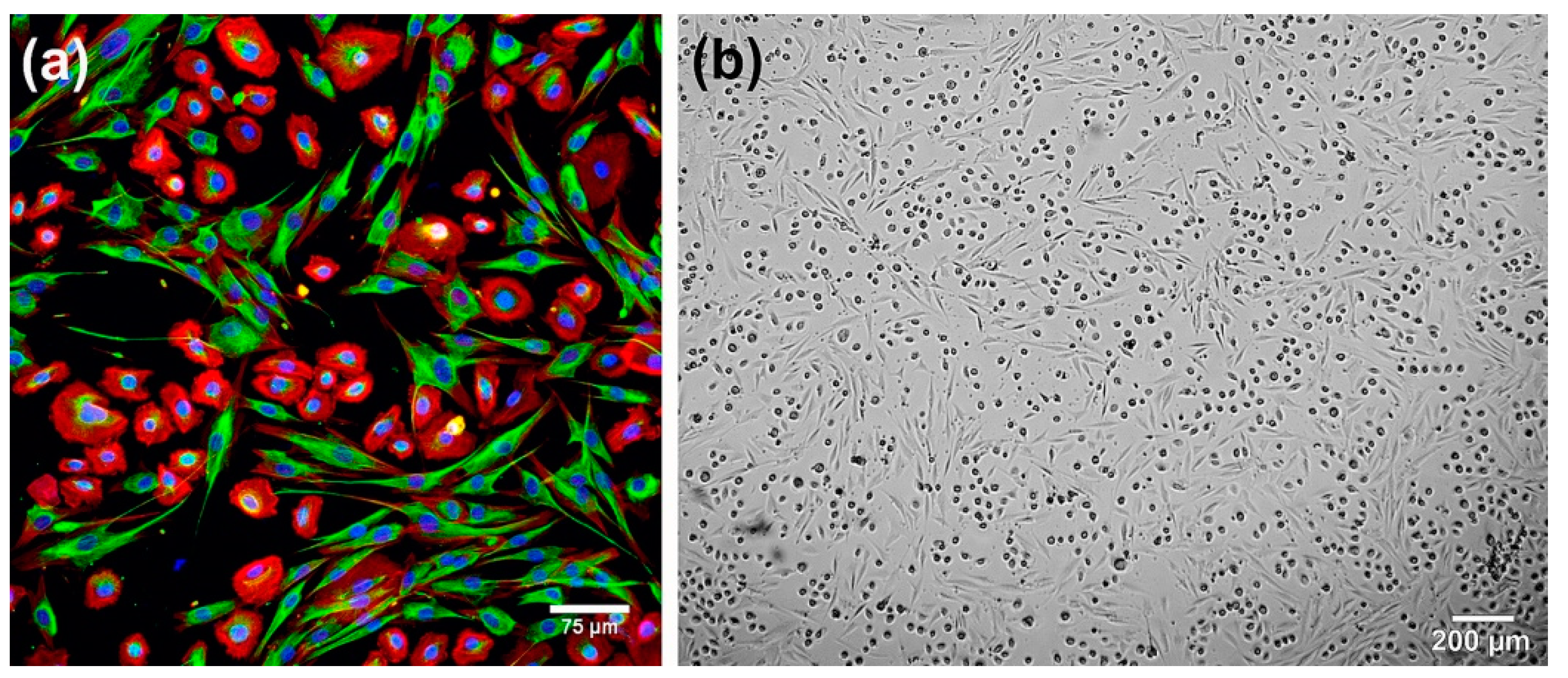
- Vivcharenko, V.; Wojcik, M.; Przekora, A. Cellular Response to Vitamin C-Enriched Chitosan/Agarose Film with Potential Application as Artificial Skin Substitute for Chronic Wound Treatment. Cells 2020, 9, 1185. [Google Scholar] [CrossRef]
- Kumar, R.J.; Kimble, R.M.; Boots, R.; Pegg, S.P. Treatment of Partial-Thickness Burns: A Prospective, Randomized Trial Using Transcyte. ANZ J. Surg. 2004, 74, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Myers, S.; Partha, V.; Soranzo, C.; Price, R.; Navsaria, H. Hyalomatrix: A temporary epidermal barrier, hyaluronan delivery, and neodermis induction system for keratinocyte stem cell therapy. Tissue Eng. 2007, 13, 2733–2741. [Google Scholar] [CrossRef] [PubMed]
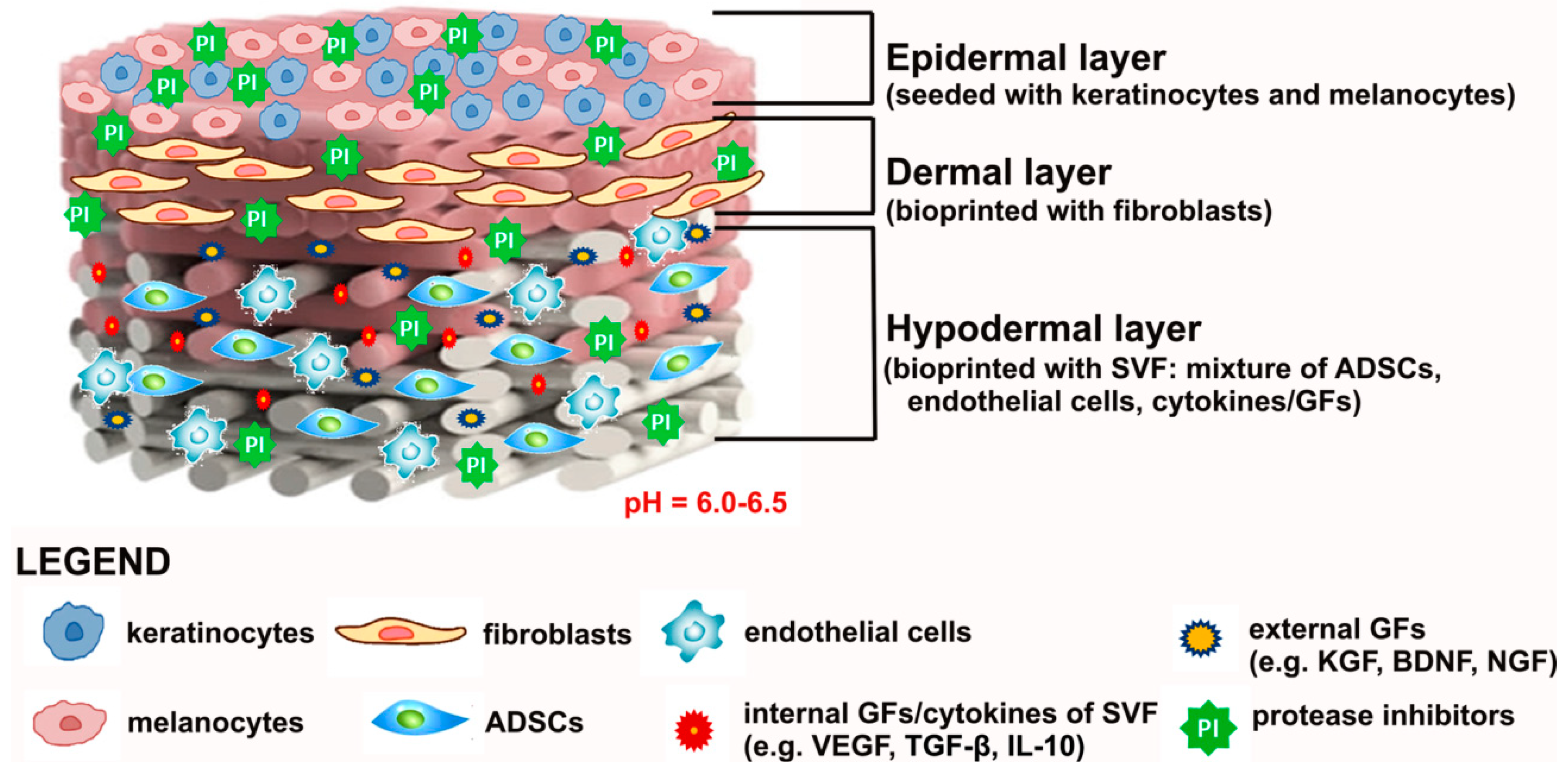
- Cubo, N.; Garcia, M.; Del Cañizo, J.; Velasco, D.; Jorcano, J. 3D bioprinting of functional human skin: Production and in vivo analysis. Biofabrication 2016, 9, 015006. [Google Scholar] [CrossRef]
- Baltazar, T.; Merola, J.; Catarino, C.; Xie, C.; Kirkiles-Smith, N.; Lee, V.; Hotta, S.; Dai, G.; Xu, X.; Ferreira, F.; et al. Three Dimensional Bioprinting of a Vascularized and Perfusable Skin Graft Using Human Keratinocytes, Fibroblasts, Pericytes, and Endothelial Cells. Tissue Eng Part A 2019. [Google Scholar] [CrossRef]
- Park, Y.R.; Ju, H.W.; Lee, J.M.; Kim, D.K.; Lee, O.J.; Moon, B.M.; Park, H.J.; Jeong, J.Y.; Yeon, Y.K.; Park, C.H. Three-dimensional electrospun silk-fibroin nanofiber for skin tissue engineering. Int. J. Biol. Macromol. 2016, 93, 1567–1574. [Google Scholar] [CrossRef] [PubMed]
- Przekora-Kusmierz, A.; Vivcharenko, V.; Kazimierczak, P.; Wojcik, M. Hydrożelowy Substytut Skóry na Bazie Chitozanu oraz Sposób jego Wytwarzania. PL Patent Application P.430456, 1 July 2019. [Google Scholar]
- Przekora Kusmierz, A.; Vivcharenko, V.; Kazimierczak, P.; Wojcik, M. Kriożelowy Materiał Opatrunkowy na Rany na Bazie Chitozanu oraz Sposób jego Wytwarzania. PL Patent Application P.430455, 1 July 2019. [Google Scholar]
- Reijnders, C.M.A.; Van Lier, A.; Roffel, S.; Kramer, D.; Scheper, R.J.; Gibbs, S. Development of a Full-Thickness Human Skin Equivalent in Vitro Model Derived from TERT-Immortalized Keratinocytes and Fibroblasts. Tissue Eng. Part A 2015, 21, 2448–2459. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.; Singh, G.; Trasatti, J.P.; Bjornsson, C.; Xu, X.; Tran, T.N.; Yoo, S.S.; Dai, G.; Karande, P. Design and fabrication of human skin by three-dimensional bioprinting. Tissue Eng. Part C Methods 2014, 20, 473–484. [Google Scholar] [CrossRef] [PubMed]
- Smits, J.P.H.; Niehues, H.; Rikken, G.; Van Vlijmen-Willems, I.M.J.J.; Van De Zande, G.W.H.J.F.; Zeeuwen, P.L.J.M.; Schalkwijk, J.; Van Den Bogaard, E.H. Immortalized N/TERT keratinocytes as an alternative cell source in 3D human epidermal models. Sci. Rep. 2017, 7, 11838. [Google Scholar] [CrossRef]
- Agarwal, R.; Ko, K.R.; Gratzer, P.F.; Frampton, J.P. Biopatterning of Keratinocytes in Aqueous Two-Phase Systems as a Potential Tool for Skin Tissue Engineering. MRS Adv. 2017, 357, 1–8. [Google Scholar] [CrossRef]
- Seo, M.D.; Kang, T.J.; Lee, C.H.; Lee, A.Y.; Noh, M. HaCa T keratinocytes and primary epidermal keratinocytes have different transcriptional profiles of cornified envelope-associated genes to T helper cell cytokines. Biomol. Ther. 2012, 20, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Przekora, A. The summary of the most important cell-biomaterial interactions that need to be considered during in vitro biocompatibility testing of bone scaffolds for tissue engineering applications. Mater. Sci. Eng. C 2019, 97, 1036–1051. [Google Scholar] [CrossRef]
- Meuli, M.; Hartmann-Fritsch, F.; Hüging, M.; Marino, D.; Saglini, M.; Hynes, S.; Neuhaus, K.; Manuel, E.; Middelkoop, E.; Reichmann, E.; et al. A Cultured Autologous Dermo-epidermal Skin Substitute for Full-Thickness Skin Defects: A Phase I, Open, Prospective Clinical Trial in Children. Plast. Reconstr. Surg. 2019, 144, 188–198. [Google Scholar] [CrossRef]
- Maarof, M.; Mh Busra, M.F.; Lokanathan, Y.; Bt Hj Idrus, R.; Rajab, N.F.; Chowdhury, S.R. Safety and efficacy of dermal fibroblast conditioned medium (DFCM) fortified collagen hydrogel as acellular 3D skin patch. Drug Deliv. Transl. Res. 2019, 9, 144–161. [Google Scholar] [CrossRef] [PubMed]
- Kouhbananinejad, S.M.; Derakhshani, A.; Vahidi, R.; Dabiri, S.; Fatemi, A.; Armin, F.; Farsinejad, A. A fibrinous and allogeneic fibroblast-enriched membrane as a biocompatible material can improve diabetic wound healing. Biomater. Sci. 2019, 7, 1949–1961. [Google Scholar] [CrossRef] [PubMed]
- Goyer, B.; Larouche, D.; Kim, D.H.; Veillette, N.; Pruneau, V.; Bernier, V.; Auger, F.A.; Germain, L. Immune tolerance of tissue-engineered skin produced with allogeneic or xenogeneic fibroblasts and syngeneic keratinocytes grafted on mice. Acta Biomater. 2019, 90, 192–204. [Google Scholar] [CrossRef] [PubMed]
- Bacakova, M.; Pajorova, J.; Broz, A.; Hadraba, D.; Lopot, F.; Zavadakova, A.; Vistejnova, L.; Beno, M.; Kostic, I.; Jencova, V.; et al. A two-layer skin construct consisting of a collagen hydrogel reinforced by a fibrin-coated polylactide nanofibrous membrane. Int. J. Nanomed. 2019, 14, 5033–5050. [Google Scholar] [CrossRef]
- Won, J.Y.; Lee, M.H.; Kim, M.J.; Min, K.H.; Ahn, G.; Han, J.S.; Jin, S.; Yun, W.S.; Shim, J.H. A potential dermal substitute using decellularized dermis extracellular matrix derived bio-ink. Artif. Cells Nanomed. Biotechnol. 2019, 47, 644–649. [Google Scholar] [CrossRef]
- Shamis, Y.; Hewitt, K.J.; Carlson, M.W.; Margvelashvilli, M.; Dong, S.; Kuo, C.K.; Daheron, L.; Egles, C.; Garlick, J.A. Fibroblasts derived from human embryonic stem cells direct development and repair of 3D human skin equivalents. Stem Cell Res. Ther. 2011, 2, 10. [Google Scholar] [CrossRef] [PubMed]
- Guenou, H.; Nissan, X.; Larcher, F.; Feteira, J.; Lemaitre, G.; Saidani, M.; Del Rio, M.; Barrault, C.C.; Bernard, F.X.; Peschanski, M.; et al. Human embryonic stem-cell derivatives for full reconstruction of the pluristratified epidermis: A preclinical study. Lancet 2009, 374, 1745–1753. [Google Scholar] [CrossRef]
- Kober, J.; Gugerell, A.; Schmid, M.; Kamolz, L.P.; Keck, M. Generation of a Fibrin Based Three-Layered Skin Substitute. Biomed Res. Int. 2015, 2015, 170427. [Google Scholar] [CrossRef] [PubMed]
- Gledhill, K.; Guo, Z.; Umegaki-Arao, N.; Higgins, C.A.; Itoh, M.; Christiano, A.M. Melanin transfer in human 3D skin equivalents generated exclusively from induced pluripotent stem cells. PLoS ONE 2015, 10, e0136713. [Google Scholar] [CrossRef]
- Itoh, M.; Umegaki-Arao, N.; Guo, Z.; Liu, L.; Higgins, C.A.; Christiano, A.M. Generation of 3D Skin Equivalents Fully Reconstituted from Human Induced Pluripotent Stem Cells (iPSCs). PLoS ONE 2013, 8, e77673. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J. Bioactive modification of poly(ethylene glycol) hydrogels for tissue engineering. Biomaterials 2010, 31, 4639–4656. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Michniak-Kohn, B.B. Tissue engineered human skin equivalents. Pharmaceutics 2012, 4, 26–41. [Google Scholar] [CrossRef]
- Zhang, K.; Wang, S.; Zhou, C.; Cheng, L.; Gao, X.; Xie, X.; Sun, J.; Wang, H.; Weir, M.D.; Reynolds, M.A.; et al. Advanced smart biomaterials and constructs for hard tissue engineering and regeneration. Bone Res. 2018, 6, 31. [Google Scholar] [CrossRef]
- Frisman, I.; Seliktar, D.; Bianco-Peled, H. Nanostructuring of PEG-fibrinogen polymeric scaffolds. Acta Biomater. 2010, 6, 2518–2524. [Google Scholar] [CrossRef]
- Lee, C.H.; Chang, S.H.; Chen, W.J.; Hung, K.C.; Lin, Y.H.; Liu, S.J.; Hsieh, M.J.; Pang, J.H.S.; Juang, J.H. Augmentation of diabetic wound healing and enhancement of collagen content using nanofibrous glucophage-loaded collagen/PLGA scaffold membranes. J. Colloid Interface Sci. 2015, 439, 88–97. [Google Scholar] [CrossRef]
- Dai, T.; Tanaka, M.; Huang, Y.-Y.; Hamblin, M.R. Chitosan Preparations for Wounds and Burns: Antimicrobial and Wound-Healing Effects. Exp. Rev. Anti. Infect. Ther. 2011, 9, 857–879. [Google Scholar] [CrossRef]
- Lu, B.; Wang, T.; Li, Z.; Dai, F.; Lv, L.; Tang, F.; Yu, K.; Liu, J.; Lan, G. Healing of skin wounds with a chitosan-gelatin sponge loaded with tannins and platelet-rich plasma. Int. J. Biol. Macromol. 2016, 82, 884–891. [Google Scholar] [CrossRef] [PubMed]
- Jayakumar, R.; Prabaharan, M.; Sudheesh Kumar, P.T.; Nair, S.V.; Tamura, H. Biomaterials based on chitin and chitosan in wound dressing applications. Biotechnol. Adv. 2011, 29, 322–337. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.; Niiyama, H.; Kondo, S.; Yamamoto, A.; Suzuki, R.; Kuroyanagi, Y. Wound dressing composed of hyaluronic acid and collagen containing EGF or bFGF: Comparative culture study. J. Biomater. Sci. Polym. Ed. 2013, 24, 1015–1026. [Google Scholar] [CrossRef]
- Mahmoud, A.A.; Salama, A.H. Norfloxacin-loaded collagen/chitosan scaffolds for skin reconstruction: Preparation, evaluation and in-vivo wound healing assessment. Eur. J. Pharm. Sci. 2016, 83, 155–165. [Google Scholar] [CrossRef]
- Jin, H.H.; Kim, D.H.; Kim, T.W.; Shin, K.K.; Jung, J.S.; Park, H.C.; Yoon, S.Y. In vivo evaluation of porous hydroxyapatite/chitosan-alginate composite scaffolds for bone tissue engineering. Int. J. Biol. Macromol. 2012, 51, 1079–1085. [Google Scholar] [CrossRef]
- Raafat, D.; Sahl, H.G. Chitosan and its antimicrobial potential—A critical literature survey. Microb. Biotechnol. 2009, 2, 186–201. [Google Scholar] [CrossRef]
- Ahmed, S.; Ikram, S. Chitosan Based Scaffolds and Their Applications in Wound Healing. Achiev. Life Sci. 2016, 10, 27–37. [Google Scholar] [CrossRef]
- Matsumine, H.; Fujimaki, H.; Takagi, M.; Mori, S.; Iwata, T.; Shimizu, M.; Takeuchi, M. Full-thickness skin reconstruction with basic fibroblast growth factor-impregnated collagen-gelatin sponge. Regen. Ther. 2019, 11, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, N.; Ishida, D.; Yamamoto, A.; Kuroyanagi, M.; Kuroyanagi, Y. Development of a functional wound dressing composed of hyaluronic acid spongy sheet containing bioactive components: Evaluation of wound healing potential in animal tests. J. Biomater. Sci. Polym. Ed. 2014, 25, 1278–1291. [Google Scholar] [CrossRef] [PubMed]
- Arasteh, S.; Khanjani, S.; Golshahi, H.; Mobini, S.; Jahed, M.T.; Heidari-Vala, H.; Edalatkhah, H.; Kazemnejad, S. Efficient Wound Healing Using a Synthetic Nanofibrous Bilayer Skin Substitute in Murine Model. J. Surg. Res. 2020, 245, 31–44. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekaran, A.; Venugopal, J.; Sundarrajan, S.; Ramakrishna, S. Fabrication of a nanofibrous scaffold with improved bioactivity for culture of human dermal fibroblasts for skin regeneration. Biomed. Mater. 2011, 6, 015001. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, S.; Venugopal, J.R.; Ramakrishna, S. Improved regeneration potential of fibroblasts using ascorbic acid-blended nanofibrous scaffolds. J. Biomed. Mater. Res. Part A 2015, 103, 3431–3440. [Google Scholar] [CrossRef] [PubMed]
- Sobhanian, P.; Khorram, M.; Hashemi, S.S.; Mohammadi, A. Development of nanofibrous collagen-grafted poly (vinyl alcohol)/gelatin/alginate scaffolds as potential skin substitute. Int. J. Biol. Macromol. 2019, 130, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Miguel, S.P.; Cabral, C.S.D.; Moreira, A.F.; Correia, I.J. Production and characterization of a novel asymmetric 3D printed construct aimed for skin tissue regeneration. Colloids Surf. B Biointerfaces 2019, 181, 994–1003. [Google Scholar] [CrossRef] [PubMed]
- Haldar, S.; Sharma, A.; Gupta, S.; Chauhan, S.; Roy, P.; Lahiri, D. Bioengineered smart trilayer skin tissue substitute for efficient deep wound healing. Mater. Sci. Eng. C 2019, 105, 110140. [Google Scholar] [CrossRef] [PubMed]
- Kubo, K.; Kuroyanagi, Y. Spongy matrix of hyaluronic acid and collagen as a cultured dermal substitute: Evaluation in an animal test. J. Artif. Organs 2003, 6, 64–70. [Google Scholar] [CrossRef]
- Karri, V.V.S.R.; Kuppusamy, G.; Talluri, S.V.; Mannemala, S.S.; Kollipara, R.; Wadhwani, A.D.; Mulukutla, S.; Raju, K.R.S.; Malayandi, R. Curcumin loaded chitosan nanoparticles impregnated into collagen-alginate scaffolds for diabetic wound healing. Int. J. Biol. Macromol. 2016, 93, 1519–1529. [Google Scholar] [CrossRef]
- Agarwal, T.; Narayan, R.; Maji, S.; Behera, S.; Kulanthaivel, S.; Maiti, T.K.; Banerjee, I.; Pal, K.; Giri, S. Gelatin/Carboxymethyl chitosan based scaffolds for dermal tissue engineering applications. Int. J. Biol. Macromol. 2016, 93, 1499–1506. [Google Scholar] [CrossRef]
- Haider, A.; Haider, S.; Han, S.S.; Kang, I.K. Recent advances in the synthesis, functionalization and biomedical applications of hydroxyapatite: A review. RSC Adv. 2017, 7, 7442–7458. [Google Scholar] [CrossRef]
- Basu, P.; Narendrakumar, U.; Arunachalam, R.; Devi, S.; Manjubala, I. Characterization and Evaluation of Carboxymethyl Cellulose-Based Films for Healing of Full-Thickness Wounds in Normal and Diabetic Rats. ACS Omega 2018, 3, 12622–12632. [Google Scholar] [CrossRef]
- Gandhimathi, C.; Venugopal, J.R.; Bhaarathy, V.; Ramakrishna, S.; Kumar, S.D. Biocomposite nanofibrous strategies for the controlled release of biomolecules for skin tissue regeneration. Int. J. Nanomed. 2014, 9, 4709–4722. [Google Scholar] [CrossRef] [PubMed]
- Kuroyanagi, M.; Yamamoto, A.; Shimizu, N.; Ishihara, E.; Ohno, H.; Takeda, A.; Kuroyanagi, Y. Development of cultured dermal substitute composed of hyaluronic acid and collagen spongy sheet containing fibroblasts and epidermal growth factor. J. Biomater. Sci. Polym. Ed. 2014, 25, 1133–1143. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, M.R.; Rabbani, S.; Bahrami, S.H.; Joghataei, M.T.; Moayer, F. Antibacterial performance and in vivo diabetic wound healing of curcumin loaded gum tragacanth/poly(ε-caprolactone) electrospun nanofibers. Mater. Sci. Eng. C 2016, 69, 1183–1191. [Google Scholar] [CrossRef] [PubMed]
- Mohd Hilmi, A.B.; Halim, A.S.; Jaafar, H.; Asiah, A.B.; Hassan, A. Chitosan dermal substitute and Chitosan skin substitute contribute to accelerated full-thickness wound healing in irradiated rats. Biomed Res. Int. 2013, 2013, 795458. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, A.R.; Bernstein, J.M. Chronic wound infection: Facts and controversies. Clin. Dermatol. 2010, 28, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Mohandas, A.; Deepthi, S.; Biswas, R.; Jayakumar, R. Chitosan based metallic nanocomposite scaffolds as antimicrobial wound dressings. Bioact. Mater. 2018, 3, 267–277. [Google Scholar] [CrossRef]
- Pérez-Díaz, M.; Alvarado-Gomez, E.; Magaña-Aquino, M.; Sánchez-Sánchez, R.; Velasquillo, C.; Gonzalez, C.; Ganem-Rondero, A.; Martínez-Castañon, G.; Zavala-Alonso, N.; Martinez-Gutierrez, F. Anti-biofilm activity of chitosan gels formulated with silver nanoparticles and their cytotoxic effect on human fibroblasts. Mater. Sci. Eng. C 2016, 60, 317–323. [Google Scholar] [CrossRef]
- Anisha, B.S.; Biswas, R.; Chennazhi, K.P.; Jayakumar, R. Chitosan-hyaluronic acid/nano silver composite sponges for drug resistant bacteria infected diabetic wounds. Int. J. Biol. Macromol. 2013, 62, 310–320. [Google Scholar] [CrossRef]
- Mihai, M.; Dima, M.; Dima, B.; Holban, A. Nanomaterials for Wound Healing and Infection Control. Materials 2019, 12, 2176. [Google Scholar] [CrossRef]
- Raghavendra, G.M.; Jayaramudu, T.; Varaprasad, K.; Sadiku, R.; Ray, S.S.; Mohana Raju, K. Cellulose-polymer-Ag nanocomposite fibers for antibacterial fabrics/skin scaffolds. Carbohydr. Polym. 2013, 93, 553–560. [Google Scholar] [CrossRef]
- Arya, G.; Kumari, R.M.; Sharma, N.; Gupta, N.; Kumar, A.; Chatterjee, S.; Nimesh, S. Catalytic, antibacterial and antibiofilm efficacy of biosynthesised silver nanoparticles using Prosopis juliflora leaf extract along with their wound healing potential. J. Photochem. Photobiol. B Biol. 2019, 190, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Sood, R.; Chopra, D.S. Optimization of reaction conditions to fabricate Ocimum sanctum synthesized silver nanoparticles and its application to nano-gel systems for burn wounds. Mater. Sci. Eng. C 2018, 92, 575–589. [Google Scholar] [CrossRef] [PubMed]
- Sudheesh Kumar, P.T.; Lakshmanan, V.K.; Anilkumar, T.V.; Ramya, C.; Reshmi, P.; Unnikrishnan, A.G.; Nair, S.V.; Jayakumar, R. Flexible and microporous chitosan hydrogel/nano ZnO composite bandages for wound dressing: In vitro and in vivo evaluation. ACS Appl. Mater. Interfaces 2012, 4, 2618–2629. [Google Scholar] [CrossRef] [PubMed]
- Shao, F.; Yang, A.J.; Yu, D.M.; Wang, J.; Gong, X.; Tian, H.X. Bio-synthesis of Barleria gibsoni leaf extract mediated zinc oxide nanoparticles and their formulation gel for wound therapy in nursing care of infants and children. J. Photochem. Photobiol. B Biol. 2018, 189, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Archana, D.; Dutta, J.; Dutta, P.K. Evaluation of chitosan nano dressing for wound healing: Characterization, in vitro and in vivo studies. Int. J. Biol. Macromol. 2013, 57, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.C.; Yang, M.H.; Chiu, W.T.; Chiu, C.H.; Yang, C.S.; Chen, Y.W.; Chen, K.C.; Peng, R.Y. Composite nano-titanium oxide-chitosan artificial skin exhibits strong wound-healing effect—An approach with anti-inflammatory and bactericidal kinetics. Macromol. Biosci. 2008, 8, 316–327. [Google Scholar] [CrossRef]
- Woo, C.H.; Choi, Y.C.; Choi, J.S.; Lee, H.Y.; Cho, Y.W. A bilayer composite composed of TiO2-incorporated electrospun chitosan membrane and human extracellular matrix sheet as a wound dressing. J. Biomater. Sci. Polym. Ed. 2015, 26, 841–854. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhou, Y.; Wu, X.; Wang, L.; Xu, L.; Wei, S. A facile method for electrospinning of Ag nanoparticles/poly (vinyl alcohol)/carboxymethyl-chitosan nanofibers. Appl. Surf. Sci. 2012, 258, 8867–8873. [Google Scholar] [CrossRef]
- Srivastava, R.; Tiwari, D.K.; Dutta, P.K. 4-(Ethoxycarbonyl) phenyl-1-amino-oxobutanoic acid-chitosan complex as a new matrix for silver nanocomposite film: Preparation, characterization and antibacterial activity. Int. J. Biol. Macromol. 2011, 49, 863–870. [Google Scholar] [CrossRef]
- Abdelgawad, A.M.; Hudson, S.M.; Rojas, O.J. Antimicrobial wound dressing nanofiber mats from multicomponent (chitosan/silver-NPs/polyvinyl alcohol) systems. Carbohydr. Polym. 2014, 100, 166–178. [Google Scholar] [CrossRef]
- Ye, H.; Cheng, J.; Yu, K. In Situ Reduction of Silver Nanoparticles by Gelatin to Obtain Porous Silver Nanoparticle/Chitosan Composites with Enhanced Antimicrobial and Wound-Healing Activity; Elsevier B.V.: Amsterdam, The Netherlands, 2019; Volume 121. [Google Scholar] [CrossRef]
- Moniri, M.; Moghaddam, A.B.; Azizi, S.; Rahim, R.A.; Zuhainis, S.W.; Navaderi, M.; Mohamad, R. In vitro molecular study of wound healing using biosynthesized bacteria nanocellulose/silver nanocomposite assisted by bioinformatics databases. Int. J. Nanomed. 2018, 13, 5097–5112. [Google Scholar] [CrossRef] [PubMed]
- Boonkaew, B.; Barber, P.M.; Rengpipat, S.; Supaphol, P.; Kempf, M.; He, J.; John, V.T.; Cuttle, L. Development and characterization of a novel, antimicrobial, sterile hydrogel dressing for burn wounds: Single-step production with gamma irradiation creates silver nanoparticles and radical polymerization. J. Pharm. Sci. 2014, 103, 3244–3253. [Google Scholar] [CrossRef] [PubMed]
- Bartel, M.; Markowska, K.; Strawski, M.; Wolska, K.; Mazur, M. Silver-decorated gel-shell nanobeads: Physicochemical characterization and evaluation of antibacterial properties. Beilstein J. Nanotechnol. 2020, 11, 620–630. [Google Scholar] [CrossRef] [PubMed]
- Regiel-Futyra, A.; Kus-Liśkiewicz, M.; Sebastian, V.; Irusta, S.; Arruebo, M.; Stochel, G.; Kyzioł, A. Development of noncytotoxic chitosan-gold nanocomposites as efficient antibacterial materials. ACS Appl. Mater. Interfaces 2015, 7, 1087–1099. [Google Scholar] [CrossRef]
- Li, Y.; Xu, T.; Tu, Z.; Dai, W.; Xue, Y.; Tang, C.; Gao, W.; Mao, C.; Lei, B.; Lin, C. Bioactive antibacterial silica-based nanocomposites hydrogel scaffolds with high angiogenesis for promoting diabetic wound healing and skin repair. Theranostics 2020, 10, 4929–4943. [Google Scholar] [CrossRef]
- Dang, L.H.; Nguyen, T.H.; Tran, H.L.B.; Doan, V.N.; Tran, N.Q. Injectable Nanocurcumin-Formulated Chitosan-g-Pluronic Hydrogel Exhibiting a Great Potential for Burn Treatment. J. Healthc. Eng. 2018, 2018, 5754890. [Google Scholar] [CrossRef]
- Cai, N.; Li, C.; Han, C.; Luo, X.; Shen, L.; Xue, Y.; Yu, F. Tailoring mechanical and antibacterial properties of chitosan/gelatin nanofiber membranes with Fe 3 O 4 nanoparticles for potential wound dressing application. Appl. Surf. Sci. 2016, 369, 492–500. [Google Scholar] [CrossRef]
- Farag, R.K.; Labena, A.; Fakhry, S.H.; Safwat, G.; Diab, A.; Atta, A.M. Antimicrobial activity of hybrids terpolymers based on magnetite hydrogel nanocomposites. Materials 2019, 12, 3604. [Google Scholar] [CrossRef]
- Archana, D.; Singh, B.K.; Dutta, J.; Dutta, P.K. In vivo evaluation of chitosan-PVP-titanium dioxide nanocomposite as wound dressing material. Carbohydr. Polym. 2013, 95, 530–539. [Google Scholar] [CrossRef]
- Timaeva, O.; Pashkin, I.; Mulakov, S.; Kuzmicheva, G.; Konarev, P.; Terekhova, R.; Sadovskaya, N.; Czakkel, O.; Prevost, S. Synthesis and physico-chemical properties of poly(N-vinyl pyrrolidone)-based hydrogels with titania nanoparticles. J. Mater. Sci. 2020, 55, 3005–3021. [Google Scholar] [CrossRef]
- Khalid, A.; Khan, R.; Ul-Islam, M.; Khan, T.; Wahid, F. Bacterial cellulose-zinc oxide nanocomposites as a novel dressing system for burn wounds. Carbohydr. Polym. 2017, 164, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Mohandas, A.; Kumar, P.; Raja, B.; Lakshmanan, V.; Jayakumar, R. Exploration of alginate hydrogel/nano zinc oxide composite bandages for infected wounds. Int. J. Nanomed. 2015, 10, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Arshad, R.; Sohail, M.F.; Sarwar, H.S.; Saeed, H.; Ali, I.; Akhtar, S.; Hussain, S.Z.; Afzal, I.; Jahan, S.; Anees-Ur-Rehman; et al. ZnO-NPs embedded biodegradable thiolated bandage for postoperative surgical site infection: In vitro and in vivo evaluation. PLoS ONE 2019, 14, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Weng, T.; Wu, P.; Zhang, W.; Zheng, Y.; Li, Q.; Jin, R.; Chen, H.; You, C.; Guo, S.; Han, C.; et al. Regeneration of skin appendages and nerves: Current status and further challenges. J. Transl. Med. 2020, 18, 53. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, K.; Medina, R.J.; Kageyama, T.; Miyazaki, M.; Yoshino, T.; Makino, T.; Huh, N.H. Participation of adult mouse bone marrow cells in reconstitution of skin. Am. J. Pathol. 2003, 163, 1227–1231. [Google Scholar] [CrossRef]
- Fang, L.J.; Fu, X.B.; Cheng, B.; Sun, T.Z.; Li, J.F.; Cao, R.; Wang, Y.X. Study on the potentiation of bone marrow mesenchymal stem cells involved in sebaceous duct formation. Zhonghua Wai Ke Za Zhi 2004, 42, 1136–1138. [Google Scholar]
- Xu, Y.; Hong, Y.; Xu, M.; Ma, K.; Fu, X.; Zhang, M.; Wang, G. Role of Keratinocyte Growth Factor in the Differentiation of Sweat Gland-Like Cells From Human Umbilical Cord-Derived Mesenchymal Stem Cells. Stem Cells Transl Med. 2016, 5, 106–116. [Google Scholar] [CrossRef]
- Sriwiriyanont, P.; Lynch, K.A.; Maier, E.A.; Hahn, J.M.; Supp, D.M.; Boyce, S.T. Morphogenesis of chimeric hair follicles in engineered skin substitutes with human keratinocytes and murine dermal papilla cells. Exp. Dermatol. 2012, 21, 783–785. [Google Scholar] [CrossRef]
- Abaci, H.E.; Coffman, A.; Doucet, Y.; Chen, J.; Jacków, J.; Wang, E.; Guo, Z.; Shin, J.U.; Jahoda, C.A.; Christiano, A.M. Tissue engineering of human hair follicles using a biomimetic developmental approach. Nat. Commun. 2018, 9, 5301. [Google Scholar] [CrossRef]
- Shu, S.; Chen, L.; Li, X.; Li, H. Three—Dimensional culture and morphological observation of human eccrine sweat gland cells. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2014, 28, 162–166. [Google Scholar]
- Li, H.; Chen, L.; Zeng, S.; Li, X.; Zhang, X.; Lin, C.; Zhang, M.; Xie, S.; He, Y.; Shu, S.; et al. Matrigel basement membrane matrix induces eccrine sweat gland cells to reconstitute sweat gland-like structures in nude mice. Exp. Cell Res. 2015, 332, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.; Xu, Y.; Wu, C.; Sha, D.; Fu, X. In vitro constitution and in vivo implantation of engineered skin constructs with sweat glands. Biomaterials 2010, 31, 5520–5525. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.L.; Qi, J.T.Z.; Yeong, W.Y.; Naing, M.W. Proof-of-concept: 3D bioprinting of pigmented human skin constructs. Biofabrication 2018, 10, 025005. [Google Scholar] [CrossRef] [PubMed]
- Dana Harriger, M.; Warden, G.D.; Greenhalgh, D.G.; Kagan, R.J.; Boyce, S.T. Pigmentation and microanatomy of skin regenerated from composite grafts of cultured cells and biopolymers applied to full-thickness burn wounds. Transplantation 1995, 59, 702–707. [Google Scholar] [CrossRef]
- McKenzie, I.A.; Biernaskie, J.; Toma, J.G.; Midha, R.; Miller, F.D. Skin-derived precursors generate myelinating Schwann cells for the injured and dysmyelinated nervous system. J. Neurosci. 2006, 26, 6651–6660. [Google Scholar] [CrossRef]
- Yannas, I.V. Emerging rules for inducing organ regeneration. Biomaterials 2013, 34, 321–330. [Google Scholar] [CrossRef]
- Soller, E.C.; Tzeranis, D.S.; Miu, K.; So, P.T.C.; Yannas, I.V. Common features of optimal collagen scaffolds that disrupt wound contraction and enhance regeneration both in peripheral nerves and in skin. Biomaterials 2012, 33, 4783–4791. [Google Scholar] [CrossRef]
- Wang, A.; Tang, Z.; Park, I.H.; Zhu, Y.; Patel, S.; Daley, G.Q.; Li, S. Induced pluripotent stem cells for neural tissue engineering. Biomaterials 2011, 32, 5023–5032. [Google Scholar] [CrossRef] [PubMed]
- Blais, M.; Grenier, M.; Berthod, F. Improvement of nerve regeneration in tissue-engineered skin enriched with schwann cells. J. Investig. Dermatol. 2009, 129, 2895–2900. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.F.; Jiang, T.X.; Garner, W.; Chuong, C.M. A simplified procedure to reconstitute hair-producing skin. Tissue Eng. Part C Methods 2011, 17, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Chen, L.; Zhang, M.; Tang, S.; Fu, X. Three-dimensional culture and identification of human eccrine sweat glands in matrigel basement membrane matrix. Cell Tissue Res. 2013, 354, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.C.; Paggiaro, A.O.; Isaac, C.; Teixeira Neto, N.; Santos, G.B.D. Substitutos cutâneos: Conceitos atuais e proposta de classificação. Rev. Bras. Cir. Plástica 2011, 26, 696–702. [Google Scholar] [CrossRef]
- Vana, L.P.M.; Battlehner, C.N.; Ferreira, M.A.; Caldini, E.G.; Gemperli, R.; Alonso, N. Comparative long-term study between two dermal regeneration templates for the reconstruction of burn scar contractures in humans: Clinical and histological results. Burns 2019. In Press. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.W.; Park, J.K.; Shon, H.C.; Choi, E.S.; Kim, D.S.; Min, K.T. Skin graft using MatriDerm® for plantar defects after excision of skin cancer. Cancer Manag. Res. 2019, 11, 2947–2950. [Google Scholar] [CrossRef]
- Cristofari, S.; Guenane, Y.; Atlan, M.; Hallier, A.; Revol, M.; Stivala, A. Coverage of radial forearm flap donor site with full thickness skin graft and Matriderm®: An alternative reliable solution? Ann. Chir. Plast. Esthet. 2019. In Press. [Google Scholar] [CrossRef] [PubMed]
- Lucas, D.; Di Rocco, D.; Müller, C.T.; Jurjus, A.R.; Raffoul, W.; Di Summa, P.G.; Watfa, W. Application of Dermal Skin Substitutes for Hand and Finger Palmar Soft Tissue Loss. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2551. [Google Scholar] [CrossRef] [PubMed]
- Hart, C.E.; Loewen-Rodriguez, A.; Lessem, J. Dermagraft: Use in the Treatment of Chronic Wounds. Adv. Wound Care 2012, 1, 138–141. [Google Scholar] [CrossRef]
- Vanscheidt, W.; Ukat, A.; Horak, V.; Brüning, H.; Hunyadi, J.; Pavlicek, R.; Emter, M.; Hartmann, A.; Bende, J.; Zwingers, T.; et al. Treatment of recalcitrant venous leg ulcers with autologous keratinocytes in fibrin sealant: A multinational randomized controlled clinical trial. Wound Repair Regen. 2007, 15, 308–315. [Google Scholar] [CrossRef]
- Lam, P.; Chan, E.; To, E.; Lau, C.; Yen, S.; King, W. Development and evaluation of a new composite Laserskin graft. J. Trauma 1999, 47, 918–922. [Google Scholar] [CrossRef]
- Grassner, L.; Marhold, F.; Yousif, M.; Grillhösl, A.; Ungersboeck, K.; Schulz, J.; Strowitzki, M. Experiences with a temporary synthetic skin substitute after decompressive craniectomy: A retrospective two-center analysis. Acta Neurochir. 2019, 161, 493–499. [Google Scholar] [CrossRef]
- Soejima, K.; Kashimura, T.; Kazama, T.; Matsumoto, T.; Nakazawa, H. Effect of Mature Adipocyte-Derived Dedifferentiated Fat Cells on Formation of Basement Membrane after Cultured Epithelial Autograft on Artificial Dermis. Plast. Reconstr. Surg. 2019, 143, 983e–992e. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Yoshitake, K.; Tokunaka, R.; Yoshida, Y.; Oshima, M.; Tatsuta, S.; Hamada, T.; Kamitomo, A.; Hamajima, A. Combination of meshed dermis graft and cultured epithelial autograft for massive burns: Three case reports. Medicine 2018, 97, 48. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Muramatsu, H.; Nakano, M.; Yamamoto, N.; Tokunaka, R.; Umezawa, K.; Hamajima, A.; Araki, N.; Yoshimoto, S. Changes in the dermal structure during cultured epidermal autograft engraftment process. Plast. Reconstr. Surg. Glob. Open 2016, 4, e870. [Google Scholar] [CrossRef]
- Hernon, C.A.; Dawson, R.A.; Freedlander, E.; Short, R.; Haddow, D.B.; Brotherston, M.; MacNeil, S. Clinical experience using cultured epithelial autografts leads to an alternative methodology for transferring skin cells from the laboratory to the patient. Regen. Med. 2006, 1, 809–821. [Google Scholar] [CrossRef] [PubMed]
- Yoon, D.; Cho, Y.S.; Joo, S.Y.; Seo, C.H.; Cho, Y.S. A clinical trial with a novel collagen dermal substitute for wound healing in burn patients. Biomater. Sci. 2020, 8, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, L.M.; Serras, R.; Guimarães, D.; Vilela, M.; Mouzinho, M.M. Bilateral third-degree burn of the legs: Lower limb salvage with dermal regenerative matrix. Ann. Burns Fire Disasters 2018, 31, 228–232. [Google Scholar]
- Yiğitbaş, H.; Yavuz, E.; Beken Özdemir, E.; Önen, Ö.; Pençe, H.; Meriç, S. Our Experience with Dermal Substitute Nevelia® in the Treatment of Severely Burned Patients. Ulus. Travma Acil Cerrahi Derg. 2019, 25, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Uccioli, L. A clinical investigation on the characteristics and outcomes of treating chronic lower extremity wounds using the tissuetech autograft system. Int. J. Low Extrem. Wounds 2003, 2, 140–151. [Google Scholar] [CrossRef]
- Fang, J.J.; Li, P.F.; Wu, J.J.; Zhou, H.Y.; Xie, L.P.; Lu, H. Reconstruction of massive skin avulsion of the scrota and penis by combined application of dermal regeneration template (Pelnac) and split-thickness skin graft with vacuum-assisted closure: A case report. World J. Clin. Cases 2019, 7, 4349–4354. [Google Scholar] [CrossRef]
- PELNACTM—Robust, Stable, Infection Resistant and Affordable—The Ideal Dermal Substitute. Available online: https://www.eurosurgical.co.uk/wound-care-burns/pelnac/ (accessed on 19 March 2020).
- Waymack, P.; Duff, R.G.; Sabolinski, M. The effect of a tissue engineered bilayered living skin analog, over meshed split-thickness autografts on the healing of excised burn wounds. Burns 2000, 26, 609–619. [Google Scholar] [CrossRef]
- Curran, M.P.; Plosker, G.L. Bilayered bioengineered skin substitute (Apligraf): A review of its use in the treatment of venous leg ulcers and diabetic foot ulcers. BioDrugs 2002, 16, 439–455. [Google Scholar] [CrossRef] [PubMed]
- Seet, W.T.; Maarof, M.; Khairul Anuar, K.; Chua, K.H.; Ahmad Irfan, A.W.; Ng, M.H.; Saim Aminuddin, B.; Idrus Ruszymah, B.H. Shelf-life evaluation of Bilayered human skin equivalent, MyDermTM. PLoS ONE 2012, 7, e40978. [Google Scholar] [CrossRef]
- Mohamed Haflah, N.; Ng, M.; Mohd Yunus, M.; Naicker, A.; Htwe, O.; Abdul Razak, K.; Idrus, R. Massive Traumatic Skin Defect Successfully Treated with Autologous, Bilayered, Tissue-Engineered MyDerm Skin Substitute. JBJS Case Connect. 2018, 8, e38. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.M.; Cochrane, C.A.; Percival, S.L. The Effect of pH on the Extracellular Matrix and Biofilms. Adv. Wound Care 2015, 4, 431–439. [Google Scholar] [CrossRef]
- Pereira, R.F.; Sousa, A.; Barrias, C.C.; Bártolo, P.J.; Granja, P.L. A single-component hydrogel bioink for bioprinting of bioengineered 3D constructs for dermal tissue engineering. Mater. Horizons 2018, 5, 1100–1111. [Google Scholar] [CrossRef]
- Dias, J.R.; Granja, P.L.; Bártolo, P.J. Advances in electrospun skin substitutes. Prog. Mater. Sci. 2016, 84, 314–334. [Google Scholar] [CrossRef]
- Rafieian, S.; Mirzadeh, H.; Mahdavi, H.; Masoumi, M.E. A review on nanocomposite hydrogels and their biomedical applications. IEEE J. Sel. Top. Quantum Electron. 2019, 26, 154–174. [Google Scholar] [CrossRef]
- Owczarczyk-Saczonek, A.; Krajewska-Włodarczyk, M.; Kruszewska, A.; Banasiak, Ł.; Placek, W.; Maksymowicz, W.; Wojtkiewicz, J. Therapeutic potential of stem cells in follicle regeneration. Stem Cells Int. 2018, 2018, 1049641. [Google Scholar] [CrossRef]
- Miyazaki, H.; Tsunoi, Y.; Akagi, T.; Sato, S.; Akashi, M.; Saitoh, D. A novel strategy to engineer pre-vascularized 3-dimensional skin substitutes to achieve efficient, functional engraftment. Sci. Rep. 2019, 9, 7797. [Google Scholar] [CrossRef]
- Ma, K.; Tan, Z.; Zhang, C.; Fu, X. Mesenchymal stem cells for sweat gland regeneration after burns: From possibility to reality. Burns 2016, 42, 492–499. [Google Scholar] [CrossRef]
- Marino, D.; Luginbühl, J.; Scola, S.; Meuli, M.; Reichmann, E. Bioengineering dermo-epidermal skin grafts with blood and lymphatic capillaries. Sci. Transl. Med. 2014, 6, 221ra14. [Google Scholar] [CrossRef] [PubMed]
- Briquez, P.S.; Hubbell, J.A.; Martino, M.M. Extracellular Matrix-Inspired Growth Factor Delivery Systems for Skin Wound Healing. Adv. Wound Care 2015, 4, 479–489. [Google Scholar] [CrossRef] [PubMed]
- Jackson, W.M.; Nesti, L.J.; Tuan, R.S. Mesenchymal stem cell therapy for attenuation of scar formation during wound healing. Stem Cell Res. Ther. 2012, 3, 20. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R. Skin bioprinting: A novel approach for creating artificial skin from synthetic and natural building blocks. Prog. Biomater. 2018, 7, 77–92. [Google Scholar] [CrossRef]
| Biomaterial Composition | Structural Type of Graft | Cellular Content | Demonstrated Effect In Vitro or In Vivo | Ref. |
|---|---|---|---|---|
| Collagen, PLGA, glucophage | Dermal | Acellular | Increased collagen content and accelerated healing of diabetic wounds in rats | [82] |
| Bovine type I collagen, HA | Dermal | Acellular | Improved granulation tissue formation in full-thickness skin defect rat model | [99] |
| Collagen, alginate, curcumin-loaded chitosan nanoparticles | Dermal | Acellular | Enhanced healing with complete re-epithelialization of diabetic wounds in a rat model | [100] |
| Gelatin, carboxymethyl chitosan | Dermal | Acellular | Expression of type I collagen and VEGF by mouse embryonic fibroblasts in vitro | [101] |
| Montmorillonite, bacterial cellulose | Dermal | Acellular | Enhanced wound healing, granulation tissue formation, and re-epithelialization of the burn wounds in murine model | [102] |
| Carboxymethyl cellulose, PEG | Dermal | Acellular | Accelerated healing of full-thickness wounds in diabetic rats | [103] |
| Silk fibroin, PLACL, vitamin E, curcumin | Dermal | Acellular | Enhanced fibroblast proliferation and collagen synthesis in vitro | [104] |
| Fibrin | Dermal | Cellular (fibroblasts) | Promotion of wound bed maturation in diabetic rats | [69] |
| Collagen, HA, EGF | Dermal | Cellular (fibroblasts) | Increased VEGF and HGF release by fibroblasts in vitro | [105] |
| PCL, gum tragacanth, curcumin | Dermal | Cellular (MSCs) | Accelerated healing, increased granulation tissue formation, and collagen deposition in diabetic rat model | [106] |
| Chitosan | Dermal | Cellular (fibroblasts, hair follicle stem cells) | Accelerated full-thickness wound healing in irradiated rats and reduced scarring | [107] |
| Bovine type I collagen | Dermo-epidermal | Cellular (fibroblasts, keratinocytes) | Formation of epidermis and dermis comparable to native skin in patients with acute partial- or full-thickness skin defects * | [67] |
| Fibrin-coated poly-l-lactide (PLLA), collagen | Dermo-epidermal | Cellular (fibroblasts, keratinocytes) | Promotion of fibroblast proliferation/migration as well as keratinocyte growth in vitro | [71] |
| Fibrin | Dermo-epidermal | Cellular (fibroblasts, keratinocytes, ADSCs) | In vitro development of trilayered skin substitute with dermal, epidermal, and hypodermal layer | [75] |
| Biomaterial Composition | Type of Nanoparticles | Tested Bacterial Strain | Demonstrated Effect In Vitro or In Vivo | Ref. |
|---|---|---|---|---|
| Chitosan, HA | nAg | E. coli, S. aureus, MRSA, P. aeruginosa, K. pneumonia | Antibacterial activity with low cytotoxicity against human dermal fibroblasts in vitro (at low concentrations of nAg) | [111] |
| Poly (vinyl alcohol) (PVA) carboxymethyl-chitosan | nAg | E. coli | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [121] |
| Chitosan, 4-(ethoxycarbonyl) phenyl-1-amino-oxobutanoic acid | nAg | E. coli, S. aureus, P. aeruginosa | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [122] |
| Chitosan, PVA | nAg | E. coli | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [123] |
| Chitosan, gelatin | nAg | E. coli, S. aureus | Antibacterial activity with no cytotoxic effect against mouse fibroblasts in vitro; accelerated wound healing in a rabbit model | [124] |
| Biosynthesized bacterial nanocellulose | nAg | S. aureus, P. aeruginosa, S. epidermidis | Antibacterial activity with no cytotoxic effect against human dermal fibroblasts in vitro (at low concentrations of nAg) | [125] |
| 2-acrylamido- 2-methylpropane sulfonic acid sodium salt | nAg | MRSA, P. aeruginosa | Antibacterial activity with no cytotoxic effect against human dermal fibroblasts in vitro; prevention of bacterial colonization in a porcine burn model | [126] |
| Sulfonated polystyrene | nAg | E. coli, S. aureus, P. aeruginosa, S. epidermidis | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [127] |
| Chitosan | nAu | S. aureus, P. aeruginosa | Bactericidal effect against biofilm forming antibiotic resistant strains with no cytotoxic effect against human dermal keratinocytes in vitro | [128] |
| Alginate, polyethylene glycol diacrylate | Cu-doped bioactive glass nanoparticles | E. coli, S. aureus | Antibacterial activity in vitro; accelerated collagen deposition and promoted early angiogenesis of diabetic full-thickness wounds in a mouse model | [129] |
| Chitosan-g-pluronic copolymer | nanocurcumin | E. coli, S. aureus, P. aeruginosa, S. typhimurium | Antibacterial activity with no cytotoxic effect against human dermal fibroblasts in vitro; enhanced collagen deposition, granulation, and wound maturity of burn wounds in a mouse model | [130] |
| Chitosan, gelatin | nFe3O4 | E. coli, S. aureus | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [131] |
| 2-acrylamido- 2-methylpropane sulfonic acid, acrylamide, acrylonitrile, acrylic acid | nFe3O4 | E. coli, B. subtilis | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [132] |
| Chitosan, pectin | nTiO2 | E. coli, S. aureus, P. aeruginosa, B. subtilis | Antibacterial activity with no cytotoxic effect against mouse fibroblasts in vitro; accelerated wound healing in a rat model | [118] |
| Chitosan | nTiO2 | S. aureus | Bactericidal effect in vitro; accelerated wound healing in a rat model | [119] |
| Chitosan, ECM sheet from human adipose tissue | nTiO2 | E. coli, S. aureus | Antibacterial activity in vitro; promotion of granulation tissue formation, re-epithelialization, and angiogenesis in a rat model | [120] |
| Chitosan, poly(N-vinylpyrrolidone) | nTiO2 | E. coli, S. aureus, P. aeruginosa, B. subtilis | Antibacterial activity with no cytotoxic effect against mouse fibroblasts in vitro; accelerated healing of open excision type wounds in a rat model | [133] |
| Poly(N-vinylpyrrolidone) | nTiO2 | S. aureus | Antibacterial activity in vitro; effect on eukaryotic cells was not tested | [134] |
| Chiotsan | nZnO | P. aeruginosa, S. intermedius, S. hyicus | Antibacterial activity with no cytotoxic effect against human dermal fibroblasts in vitro; accelerated wound healing and faster re-epithelialization in a rat model | [116] |
| Bacterial cellulose | nZnO | E. coli, S. aureus, P. aeruginosa, C. freundii | Antibacterial activity in vitro; accelerated wound healing in a burn mouse model | [135] |
| Alginate | nZnO | E. coli, S. aureus, MRSA | Antibacterial activity with low cytotoxicity against human dermal fibroblasts in vitro (at low concentrations of nZnO); re-epithelialization in ex-vivo porcine skin model | [136] |
| Chitosan, alginate | nZnO | S. aureus | Antibacterial activity with low cytotoxicity against human cervical cancer cells (HeLa cell line) in vitro; improved tissue generation and accelerated wound healing in a mouse model | [137] |
| Biomaterial Composition | Skin Appendage or Pigmentation or Nerves | Cellular Content | Demonstrated Effect In Vitro or In Vivo | Ref. |
|---|---|---|---|---|
| Chitosan | Hair follicles | Human fibroblasts and hair follicle stem cells | Accelerated healing and the presence of viable follicle stem cells in the irradiated wound of rats | [107] |
| Collagen, glycosaminoglycan | Hair follicles | Murine dermal papilla cells, human fibroblasts and keratinocytes | Successful generation of chimeric hair follicles in an athymic nude mouse model | [142] |
| Type I collagen | Hair follicles | Human neonatal dermal keratinocytes and fibroblasts, human dermal papilla cells | Differentiation of human keratinocytes into hair follicle lineage in vitro; hair growth after 4-6 weeks in an athymic nude mouse model | [143] |
| Bovine type I collagen, chondroitin-6-sulfate (Integra®) | Hair follicles | Murine newborn epidermal and dermal stem cells | Reconstruction of skin with proper proportions and topological organization, showing large amount of hair follicles (in vivo mouse model) | [154] |
| Matrigel™ matrix | Sweat glands | Human eccrine sweat gland cells | Formation of the 3D structures in vitro, resembling the morphology of eccrine sweat glands | [144] |
| Matrigel™ matrix | Sweat glands | Human eccrine sweat gland cells | Reconstruction of tubular-like structures in athymic nude mice (20% of the de novo formed tubular-like structures were coils and 80% were ducts) | [145] |
| Matrigel™ matrix mixed (1:2) with type I collagen, EGF-loaded gelatin microspheres | Sweat glands | Human skin fibroblasts and keratinocytes, human sweat gland cells | Formation of sweat gland-like structure in vitro; accelerated regeneration of full-thickness cutaneous wounds in an athymic mouse model | [146] |
| Matrigel™ matrix | Sweat glands | Human eccrine sweat gland cells | Formation of the 3D sweat gland-like structures under in vitro conditions | [155] |
| Collagen | Pigmentation | Human skin fibroblasts and keratinocytes, human melanocytes | Uniform skin pigmentation; tissue organization resembling native skin | [147] |
| PLACL, poly(propylene glycol) | Nerves | iPSC-derived neural crest stem cells | Regeneration of sciatic nerves and promoted axonal myelination in a rat model | [152] |
| Collagen, chitosan | Nerves | Human skin fibroblasts and keratinocytes, murine Schwann cells | Enhanced nerve migration and promoted myelin sheath formation in vitro; nerve function recovery in an athymic nude mouse model | [153] |
| Commercial Product | Biomaterial Composition | Structural Type of Graft | Cellular Content | Indications for Use | Ref. |
|---|---|---|---|---|---|
| Epigard® | Polytetrafluorethylen, polyurethane | Epidermal | Acellular | Preparation of wound bed before skin transplantation | [160,164] |
| JACE® | No biomaterial used (autologous keratinocyte sheet prepared based on Green method) | Epidermal | Cellular (keratinocytes) | Full-thickness skin defects, extensive burn wounds | [165,166,167] |
| MySkin™ | Silicone | Epidermal | Cellular (keratinocytes) | Diabetic foot ulcers | [168] |
| Insuregraf® | Porcine type I collagen | Dermal | Acellular | Burn wounds | [169] |
| Integra® | Bovine type I collagen, chondroitin-6-sulfate | Dermal | Acellular | Partial- and full-thickness burns, chronic ulcers | [157,170] |
| Nevelia® | Calf type I collagen | Dermal | Acellular | Burn wounds | [171] |
| Hyalograft 3D® | HA | Dermal | Cellular (fibroblasts) | Deep burns, foot ulcers | [172] |
| PELNAC™ | Porcine atelocollagen, silicone | Dermo-epidermal | Acellular | Partial- and full-thickness wounds, large acute burns | [173,174] |
| Apligraf® | Bovine type I collagen | Dermo-epidermal | Cellular (fibroblasts, keratinocytes) | Partial- and full-thickness burns, chronic ulcers | [175,176] |
| MyDerm™ | Fibrin | Dermo-epidermal | Cellular (fibroblasts, keratinocyte) | Full-thickness wounds | [177,178] |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Przekora, A. A Concise Review on Tissue Engineered Artificial Skin Grafts for Chronic Wound Treatment: Can We Reconstruct Functional Skin Tissue In Vitro? Cells 2020, 9, 1622. https://doi.org/10.3390/cells9071622
Przekora A. A Concise Review on Tissue Engineered Artificial Skin Grafts for Chronic Wound Treatment: Can We Reconstruct Functional Skin Tissue In Vitro? Cells. 2020; 9(7):1622. https://doi.org/10.3390/cells9071622
Chicago/Turabian StylePrzekora, Agata. 2020. "A Concise Review on Tissue Engineered Artificial Skin Grafts for Chronic Wound Treatment: Can We Reconstruct Functional Skin Tissue In Vitro?" Cells 9, no. 7: 1622. https://doi.org/10.3390/cells9071622
APA StylePrzekora, A. (2020). A Concise Review on Tissue Engineered Artificial Skin Grafts for Chronic Wound Treatment: Can We Reconstruct Functional Skin Tissue In Vitro? Cells, 9(7), 1622. https://doi.org/10.3390/cells9071622