The Functional Heterogeneity of Neutrophil-Derived Extracellular Vesicles Reflects the Status of the Parent Cell
Abstract
1. Introduction
1.1. EVs in Intercellular Communication
1.2. Non-Cellular Effects of EVs
1.3. EVs in Pathological Conditions
1.4. Diagnostics and Therapy
2. Neutrophil-Derived EVs
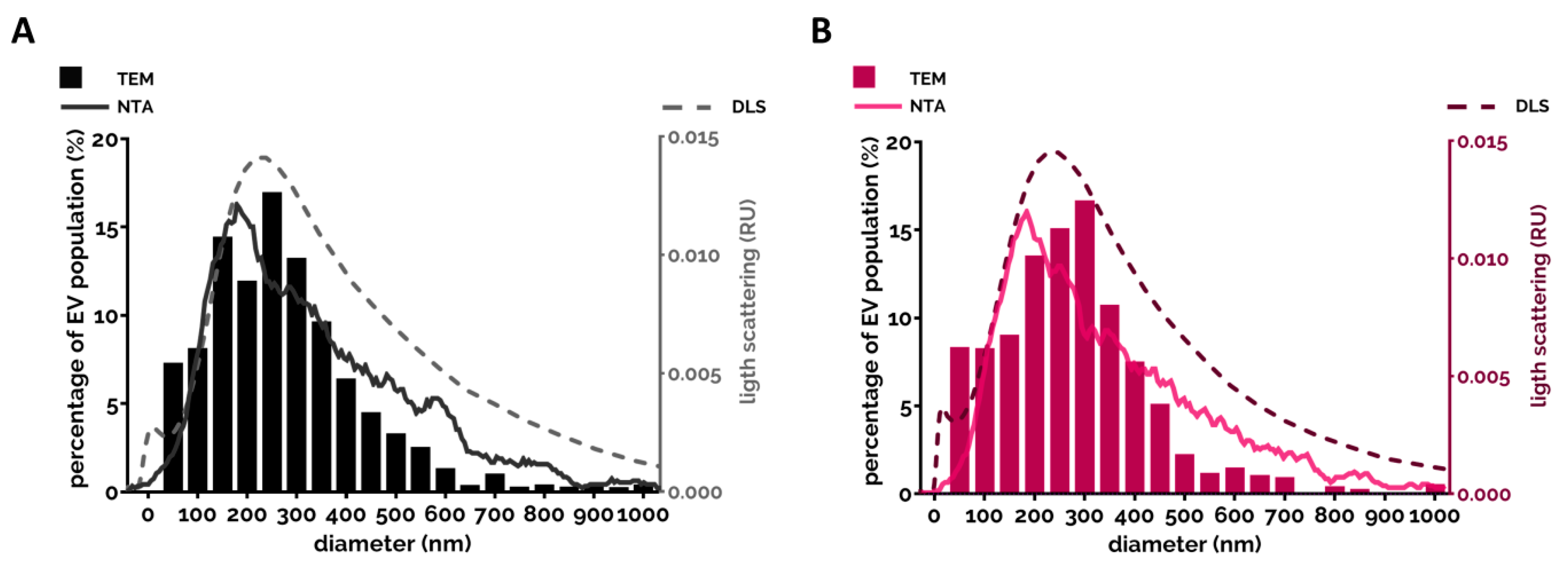
2.1. Characteristics of Neutrophil-Derived EVs
2.2. Neutrophil-Derived EVs in Intercellular Communication
2.2.1. Effect of PMN-EVs Released without Stimulation
2.2.2. Effect of PMN-EVs Released upon Stimulation with Bacterial Byproducts (fMLP and LPS)
2.2.3. Effect of PMN-EVs Released upon Stimulation with Endogenous Pro-Inflammatory Mediators
2.2.4. Effect of PMN-EVs Released upon Stimulation with Pathogens
2.2.5. Effect of PMN-EVs Released upon Stimulation with Pharmacological Stimuli
2.2.6. Effect of PMN-EVs Released in Pathophysiological Environments
2.3. Non-Cellular Effects of Neutrophil-Derived EVs
2.3.1. Effect of PMN-EVs on Hemostasis
2.3.2. Anti-Pathogenic Effect of PMN EVs
2.4. Role of PMN-EVs in Diagnostics and Therapy
3. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yanez-Mo, M.; Siljander, P.R.; Andreu, Z.; Zavec, A.B.; Borras, F.E.; Buzas, E.I.; Buzas, K.; Casal, E.; Cappello, F.; Carvalho, J.; et al. Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles 2015, 4, 27066. [Google Scholar] [CrossRef] [PubMed]
- Wolf, P. The nature and significance of platelet products in human plasma. Br. J. Haematol. 1967, 13, 269–288. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.; Samuel, M.; Kumar, S.; Mathivanan, S. Ticket to a bubble ride: Cargo sorting into exosomes and extracellular vesicles. Biochim. Biophys. Acta Proteins Proteom. 2019, 1867, 140203. [Google Scholar] [CrossRef]
- Colombo, M.; Raposo, G.; Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell. Dev. Biol. 2014, 30, 255–289. [Google Scholar] [CrossRef] [PubMed]
- Brisson, A.R.; Tan, S.; Linares, R.; Gounou, C.; Arraud, N. Extracellular vesicles from activated platelets: A semiquantitative cryo-electron microscopy and immuno-gold labeling study. Platelets 2017, 28, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Kowal, J.; Arras, G.; Colombo, M.; Jouve, M.; Morath, J.P.; Primdal-Bengtson, B.; Dingli, F.; Loew, D.; Tkach, M.; Thery, C. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proc. Natl. Acad. Sci. USA 2016, 113, E968–E977. [Google Scholar] [CrossRef] [PubMed]
- Zwaal, R.F.; Schroit, A.J. Pathophysiologic implications of membrane phospholipid asymmetry in blood cells. Blood 1997, 89, 1121–1132. [Google Scholar] [CrossRef] [PubMed]
- Hamon, Y.; Broccardo, C.; Chambenoit, O.; Luciani, M.F.; Toti, F.; Chaslin, S.; Freyssinet, J.M.; Devaux, P.F.; McNeish, J.; Marguet, D.; et al. ABC1 promotes engulfment of apoptotic cells and transbilayer redistribution of phosphatidylserine. Nat. Cell Biol. 2000, 2, 399–406. [Google Scholar] [CrossRef]
- Daleke, D.L. Regulation of transbilayer plasma membrane phospholipid asymmetry. J. Lipid Res. 2003, 44, 233–242. [Google Scholar] [CrossRef]
- Lorincz, A.M.; Schutte, M.; Timar, C.I.; Veres, D.S.; Kittel, A.; McLeish, K.R.; Merchant, M.L.; Ligeti, E. Functionally and morphologically distinct populations of extracellular vesicles produced by human neutrophilic granulocytes. J. Leukoc. Biol. 2015, 98, 583–589. [Google Scholar] [CrossRef]
- Zhang, Y.; Bi, J.; Huang, J.; Tang, Y.; Du, S.; Li, P. Exosome: A Review of Its Classification, Isolation Techniques, Storage, Diagnostic and Targeted Therapy Applications. Int. J. Nanomed. 2020, 15, 6917–6934. [Google Scholar] [CrossRef] [PubMed]
- Doyle, L.M.; Wang, M.Z. Overview of Extracellular Vesicles, Their Origin, Composition, Purpose, and Methods for Exosome Isolation and Analysis. Cells 2019, 8, 727. [Google Scholar] [CrossRef] [PubMed]
- Sidhom, K.; Obi, P.O.; Saleem, A. A Review of Exosomal Isolation Methods: Is Size Exclusion Chromatography the Best Option? Int. J. Mol. Sci. 2020, 21, 6466. [Google Scholar] [CrossRef] [PubMed]
- Hartjes, T.A.; Mytnyk, S.; Jenster, G.W.; van Steijn, V.; van Royen, M.E. Extracellular Vesicle Quantification and Characterization: Common Methods and Emerging Approaches. Bioengineering 2019, 6, 7. [Google Scholar] [CrossRef] [PubMed]
- Panagopoulou, M.S.; Wark, A.W.; Birch, D.J.S.; Gregory, C.D. Phenotypic analysis of extracellular vesicles: A review on the applications of fluorescence. J. Extracell. Vesicles 2020, 9, 1710020. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.; Seeger, R.C.; Fabbri, M.; Wang, L.; Wayne, A.S.; Jong, A.Y. Biological roles and potential applications of immune cell-derived extracellular vesicles. J. Extracell. Vesicles 2017, 6, 1400370. [Google Scholar] [CrossRef] [PubMed]
- Kalluri, R.; LeBleu, V.S. The biology, function, and biomedical applications of exosomes. Science 2020, 367, eaau6977. [Google Scholar] [CrossRef]
- Gutierrez-Vazquez, C.; Villarroya-Beltri, C.; Mittelbrunn, M.; Sanchez-Madrid, F. Transfer of extracellular vesicles during immune cell-cell interactions. Immunol. Rev. 2013, 251, 125–142. [Google Scholar] [CrossRef]
- Raposo, G.; Nijman, H.W.; Stoorvogel, W.; Liejendekker, R.; Harding, C.V.; Melief, C.J.; Geuze, H.J. B lymphocytes secrete antigen-presenting vesicles. J. Exp. Med. 1996, 183, 1161–1172. [Google Scholar] [CrossRef]
- Thery, C.; Regnault, A.; Garin, J.; Wolfers, J.; Zitvogel, L.; Ricciardi-Castagnoli, P.; Raposo, G.; Amigorena, S. Molecular characterization of dendritic cell-derived exosomes. Selective accumulation of the heat shock protein hsc73. J. Cell Biol. 1999, 147, 599–610. [Google Scholar] [CrossRef]
- Thery, C.; Ostrowski, M.; Segura, E. Membrane vesicles as conveyors of immune responses. Nat. Rev. Immunol. 2009, 9, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Al-Nedawi, K.; Meehan, B.; Micallef, J.; Lhotak, V.; May, L.; Guha, A.; Rak, J. Intercellular transfer of the oncogenic receptor EGFRvIII by microvesicles derived from tumour cells. Nat. Cell Biol. 2008, 10, 619–624. [Google Scholar] [CrossRef] [PubMed]
- Valadi, H.; Ekstrom, K.; Bossios, A.; Sjostrand, M.; Lee, J.J.; Lotvall, J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007, 9, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Skog, J.; Wurdinger, T.; van Rijn, S.; Meijer, D.H.; Gainche, L.; Sena-Esteves, M.; Curry, W.T., Jr.; Carter, B.S.; Krichevsky, A.M.; Breakefield, X.O. Glioblastoma microvesicles transport RNA and proteins that promote tumour growth and provide diagnostic biomarkers. Nat. Cell Biol. 2008, 10, 1470–1476. [Google Scholar] [CrossRef]
- Ratajczak, M.Z.; Zuba-Surma, E.; Kucia, M.; Reca, R.; Wojakowski, W.; Ratajczak, J. The pleiotropic effects of the SDF-1-CXCR4 axis in organogenesis, regeneration and tumorigenesis. Leukemia 2006, 20, 1915–1924. [Google Scholar] [CrossRef]
- Nolte-’t Hoen, E.N.; Wauben, M.H. Immune cell-derived vesicles: Modulators and mediators of inflammation. Curr. Pharm. Des. 2012, 18, 2357–2368. [Google Scholar] [CrossRef]
- Robbins, P.D.; Morelli, A.E. Regulation of immune responses by extracellular vesicles. Nat. Rev. Immunol. 2014, 14, 195–208. [Google Scholar] [CrossRef]
- Fernandez-Messina, L.; Gutierrez-Vazquez, C.; Rivas-Garcia, E.; Sanchez-Madrid, F.; de la Fuente, H. Immunomodulatory role of microRNAs transferred by extracellular vesicles. Biol. Cell 2015, 107, 61–77. [Google Scholar] [CrossRef]
- Cerri, C.; Chimenti, D.; Conti, I.; Neri, T.; Paggiaro, P.; Celi, A. Monocyte/macrophage-derived microparticles up-regulate inflammatory mediator synthesis by human airway epithelial cells. J. Immunol. 2006, 177, 1975–1980. [Google Scholar] [CrossRef]
- Eyre, J.; Burton, J.O.; Saleem, M.A.; Mathieson, P.W.; Topham, P.S.; Brunskill, N.J. Monocyte- and endothelial-derived microparticles induce an inflammatory phenotype in human podocytes. Nephron Exp. Nephrol. 2011, 119, e58–e66. [Google Scholar] [CrossRef]
- Bardelli, C.; Amoruso, A.; Federici Canova, D.; Fresu, L.; Balbo, P.; Neri, T.; Celi, A.; Brunelleschi, S. Autocrine activation of human monocyte/macrophages by monocyte-derived microparticles and modulation by PPARgamma ligands. Br. J. Pharm. 2012, 165, 716–728. [Google Scholar] [CrossRef] [PubMed]
- Scanu, A.; Molnarfi, N.; Brandt, K.J.; Gruaz, L.; Dayer, J.M.; Burger, D. Stimulated T cells generate microparticles, which mimic cellular contact activation of human monocytes: Differential regulation of pro- and anti-inflammatory cytokine production by high-density lipoproteins. J. Leukoc. Biol. 2008, 83, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Shefler, I.; Salamon, P.; Levi-Schaffer, F.; Mor, A.; Hershko, A.Y.; Mekori, Y.A. MicroRNA-4443 regulates mast cell activation by T cell-derived microvesicles. J. Allergy Clin. Immunol. 2018, 141, 2132–2141.e4. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.; Tesse, A.; Hugel, B.; Martinez, M.C.; Morel, O.; Freyssinet, J.M.; Andriantsitohaina, R. Shed membrane particles from T lymphocytes impair endothelial function and regulate endothelial protein expression. Circulation 2004, 109, 1653–1659. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, J.V.; de Castro, R.O.; da Silva, E.Z.; Silveira, P.P.; da Silva-Januario, M.E.; Arruda, E.; Jamur, M.C.; Oliver, C.; Aguiar, R.S.; daSilva, L.L. Nef neutralizes the ability of exosomes from CD4+ T cells to act as decoys during HIV-1 infection. PLoS ONE 2014, 9, e113691. [Google Scholar] [CrossRef]
- Canas, J.A.; Sastre, B.; Mazzeo, C.; Fernandez-Nieto, M.; Rodrigo-Munoz, J.M.; Gonzalez-Guerra, A.; Izquierdo, M.; Barranco, P.; Quirce, S.; Sastre, J.; et al. Exosomes from eosinophils autoregulate and promote eosinophil functions. J. Leukoc. Biol. 2017, 101, 1191–1199. [Google Scholar] [CrossRef]
- Bari, E.; Perteghella, S.; Catenacci, L.; Sorlini, M.; Croce, S.; Mantelli, M.; Avanzini, M.A.; Sorrenti, M.; Torre, M.L. Freeze-dried and GMP-compliant pharmaceuticals containing exosomes for acellular mesenchymal stromal cell immunomodulant therapy. Nanomedicine 2019, 14, 753–765. [Google Scholar] [CrossRef]
- Macia, L.; Nanan, R.; Hosseini-Beheshti, E.; Grau, G.E. Host- and Microbiota-Derived Extracellular Vesicles, Immune Function, and Disease Development. Int. J. Mol. Sci. 2019, 21, 107. [Google Scholar] [CrossRef]
- Gould, S.J.; Booth, A.M.; Hildreth, J.E. The Trojan exosome hypothesis. Proc. Natl. Acad. Sci. USA 2003, 100, 10592–10597. [Google Scholar] [CrossRef]
- Ali, S.; Toews, K.; Schwiebert, S.; Klaus, A.; Winkler, A.; Grunewald, L.; Oevermann, L.; Deubzer, H.E.; Tuns, A.; Jensen, M.C.; et al. Tumor-Derived Extracellular Vesicles Impair CD171-Specific CD4(+) CAR T Cell Efficacy. Front. Immunol. 2020, 11, 531. [Google Scholar] [CrossRef]
- Kerris, E.W.J.; Hoptay, C.; Calderon, T.; Freishtat, R.J. Platelets and platelet extracellular vesicles in hemostasis and sepsis. J. Investig. Med. 2020, 68, 813–820. [Google Scholar] [CrossRef]
- Owens, A.P., 3rd; Mackman, N. Microparticles in hemostasis and thrombosis. Circ. Res. 2011, 108, 1284–1297. [Google Scholar] [CrossRef]
- Van Der Meijden, P.E.; Van Schilfgaarde, M.; Van Oerle, R.; Renné, T.; ten Cate, H.; Spronk, H.M. Platelet- and erythrocyte-derived microparticles trigger thrombin generation via factor XIIa. J. Thromb. Haemost. 2012, 10, 1355–1362. [Google Scholar] [CrossRef]
- Steppich, B.; Mattisek, C.; Sobczyk, D.; Kastrati, A.; Schömig, A.; Ott, I. Tissue factor pathway inhibitor on circulating microparticles in acute myocardial infarction. Thromb. Haemost. 2005, 93, 35–39. [Google Scholar] [CrossRef]
- Kushak, R.I.; Nestoridi, E.; Lambert, J.; Selig, M.K.; Ingelfinger, J.R.; Grabowski, E.F. Detached endothelial cells and microparticles as sources of tissue factor activity. Thromb. Res. 2005, 116, 409–419. [Google Scholar] [CrossRef]
- Koshiar, R.L.; Somajo, S.; Norström, E.; Dahlbäck, B. Erythrocyte-derived microparticles supporting activated protein C-mediated regulation of blood coagulation. PLoS ONE 2014, 9, e104200. [Google Scholar] [CrossRef]
- Somajo, S.; Koshiar, R.L.; Norström, E.; Dahlbäck, B. Protein S and factor V in regulation of coagulation on platelet microparticles by activated protein C. Thromb. Res. 2014, 134, 144–152. [Google Scholar] [CrossRef]
- Lacroix, R.; Plawinski, L.; Robert, S.; Doeuvre, L.; Sabatier, F.; Martinez de Lizarrondo, S.; Mezzapesa, A.; Anfosso, F.; Leroyer, A.S.; Poullin, P.; et al. Leukocyte- and endothelial-derived microparticles: A circulating source for fibrinolysis. Haematologica 2012, 97, 1864–1872. [Google Scholar] [CrossRef]
- Kesimer, M.; Scull, M.; Brighton, B.; DeMaria, G.; Burns, K.; O’Neal, W.; Pickles, R.J.; Sheehan, J.K. Characterization of exosome-like vesicles released from human tracheobronchial ciliated epithelium: A possible role in innate defense. FASEB J. 2009, 23, 1858–1868. [Google Scholar] [CrossRef]
- Regente, M.; Pinedo, M.; San Clemente, H.; Balliau, T.; Jamet, E.; de la Canal, L. Plant extracellular vesicles are incorporated by a fungal pathogen and inhibit its growth. J. Exp. Bot. 2017, 68, 5485–5495. [Google Scholar] [CrossRef]
- Becker, A.; Thakur, B.K.; Weiss, J.M.; Kim, H.S.; Peinado, H.; Lyden, D. Extracellular Vesicles in Cancer: Cell-to-Cell Mediators of Metastasis. Cancer Cell 2016, 30, 836–848. [Google Scholar] [CrossRef]
- Xu, R.; Rai, A.; Chen, M.; Suwakulsiri, W.; Greening, D.W.; Simpson, R.J. Extracellular vesicles in cancer—Implications for future improvements in cancer care. Nat. Rev. Clin. Oncol. 2018, 15, 617–638. [Google Scholar] [CrossRef]
- Rak, J.; Guha, A. Extracellular vesicles–vehicles that spread cancer genes. Bioessays 2012, 34, 489–497. [Google Scholar] [CrossRef]
- House, I.G.; Petley, E.V.; Beavis, P.A. Tumor-derived exosomes modulate T cell function through transfer of RNA. FEBS J. 2018, 285, 1030–1032. [Google Scholar] [CrossRef]
- Fu, H.; Yang, H.; Zhang, X.; Xu, W. The emerging roles of exosomes in tumor-stroma interaction. J. Cancer Res. Clin. Oncol. 2016, 142, 1897–1907. [Google Scholar] [CrossRef]
- Guo, W.; Gao, Y.; Li, N.; Shao, F.; Wang, C.; Wang, P.; Yang, Z.; Li, R.; He, J. Exosomes: New players in cancer (Review). Oncol. Rep. 2017, 38, 665–675. [Google Scholar] [CrossRef]
- Cloutier, N.; Tan, S.; Boudreau, L.H.; Cramb, C.; Subbaiah, R.; Lahey, L.; Albert, A.; Shnayder, R.; Gobezie, R.; Nigrovic, P.A.; et al. The exposure of autoantigens by microparticles underlies the formation of potent inflammatory components: The microparticle-associated immune complexes. EMBO Mol. Med. 2013, 5, 235–249. [Google Scholar] [CrossRef]
- Fortin, P.R.; Cloutier, N.; Bissonnette, V.; Aghdassi, E.; Eder, L.; Simonyan, D.; Laflamme, N.; Boilard, E. Distinct Subtypes of Microparticle-containing Immune Complexes Are Associated with Disease Activity, Damage, and Carotid Intima-media Thickness in Systemic Lupus Erythematosus. J. Rheumatol. 2016, 43, 2019–2025. [Google Scholar] [CrossRef]
- Murao, A.; Brenner, M.; Aziz, M.; Wang, P. Exosomes in Sepsis. Front. Immunol. 2020, 11, 2140. [Google Scholar] [CrossRef]
- Azevedo, L.C.; Janiszewski, M.; Pontieri, V.; Pedro Mde, A.; Bassi, E.; Tucci, P.J.; Laurindo, F.R. Platelet-derived exosomes from septic shock patients induce myocardial dysfunction. Crit. Care 2007, 11, R120. [Google Scholar] [CrossRef]
- Loyer, X.; Zlatanova, I.; Devue, C.; Yin, M.; Howangyin, K.Y.; Klaihmon, P.; Guerin, C.L.; Kheloufi, M.; Vilar, J.; Zannis, K.; et al. Intra-Cardiac Release of Extracellular Vesicles Shapes Inflammation Following Myocardial Infarction. Circ. Res. 2018, 123, 100–106. [Google Scholar] [CrossRef] [PubMed]
- O’Farrell, H.E.; Yang, I.A. Extracellular vesicles in chronic obstructive pulmonary disease (COPD). J. Thorac. Dis. 2019, 11, S2141–S2154. [Google Scholar] [CrossRef] [PubMed]
- Mitsuhashi, S.; Feldbrugge, L.; Csizmadia, E.; Mitsuhashi, M.; Robson, S.C.; Moss, A.C. Luminal Extracellular Vesicles (EVs) in Inflammatory Bowel Disease (IBD) Exhibit Proinflammatory Effects on Epithelial Cells and Macrophages. Inflamm. Bowel Dis. 2016, 22, 1587–1595. [Google Scholar] [CrossRef] [PubMed]
- La Salvia, S.; Gunasekaran, P.M.; Byrd, J.B.; Erdbrugger, U. Extracellular Vesicles in Essential Hypertension: Hidden Messengers. Curr. Hypertens. Rep. 2020, 22, 76. [Google Scholar] [CrossRef]
- Xiao, Y.; Zheng, L.; Zou, X.; Wang, J.; Zhong, J.; Zhong, T. Extracellular vesicles in type 2 diabetes mellitus: Key roles in pathogenesis, complications, and therapy. J. Extracell. Vesicles 2019, 8, 1625677. [Google Scholar] [CrossRef]
- Emmanouilidou, E.; Melachroinou, K.; Roumeliotis, T.; Garbis, S.D.; Ntzouni, M.; Margaritis, L.H.; Stefanis, L.; Vekrellis, K. Cell-produced alpha-synuclein is secreted in a calcium-dependent manner by exosomes and impacts neuronal survival. J. Neurosci. 2010, 30, 6838–6851. [Google Scholar] [CrossRef]
- Bellingham, S.A.; Guo, B.B.; Coleman, B.M.; Hill, A.F. Exosomes: Vehicles for the transfer of toxic proteins associated with neurodegenerative diseases? Front. Physiol. 2012, 3, 124. [Google Scholar] [CrossRef]
- Garcia-Romero, N.; Esteban-Rubio, S.; Rackov, G.; Carrion-Navarro, J.; Belda-Iniesta, C.; Ayuso-Sacido, A. Extracellular vesicles compartment in liquid biopsies: Clinical application. Mol. Asp. Med. 2018, 60, 27–37. [Google Scholar] [CrossRef]
- Zhou, B.; Xu, K.; Zheng, X.; Chen, T.; Wang, J.; Song, Y.; Shao, Y.; Zheng, S. Application of exosomes as liquid biopsy in clinical diagnosis. Signal Transduct. Target. 2020, 5, 144. [Google Scholar] [CrossRef]
- Sluijter, J.P.G.; Davidson, S.M.; Boulanger, C.M.; Buzas, E.I.; de Kleijn, D.P.V.; Engel, F.B.; Giricz, Z.; Hausenloy, D.J.; Kishore, R.; Lecour, S.; et al. Extracellular vesicles in diagnostics and therapy of the ischaemic heart: Position Paper from the Working Group on Cellular Biology of the Heart of the European Society of Cardiology. Cardiovasc. Res. 2018, 114, 19–34. [Google Scholar] [CrossRef]
- McKiernan, J.; Donovan, M.J.; Margolis, E.; Partin, A.; Carter, B.; Brown, G.; Torkler, P.; Noerholm, M.; Skog, J.; Shore, N.; et al. A Prospective Adaptive Utility Trial to Validate Performance of a Novel Urine Exosome Gene Expression Assay to Predict High-grade Prostate Cancer in Patients with Prostate-specific Antigen 2-10ng/ml at Initial Biopsy. Eur. Urol. 2018, 74, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Crivelli, B.; Chlapanidas, T.; Perteghella, S.; Lucarelli, E.; Pascucci, L.; Brini, A.T.; Ferrero, I.; Marazzi, M.; Pessina, A.; Torre, M.L.; et al. Mesenchymal stem/stromal cell extracellular vesicles: From active principle to next generation drug delivery system. J. Control. Release 2017, 262, 104–117. [Google Scholar] [CrossRef]
- Gowen, A.; Shahjin, F.; Chand, S.; Odegaard, K.E.; Yelamanchili, S.V. Mesenchymal Stem Cell-Derived Extracellular Vesicles: Challenges in Clinical Applications. Front. Cell Dev. Biol. 2020, 8, 149. [Google Scholar] [CrossRef] [PubMed]
- Parfejevs, V.; Sagini, K.; Buss, A.; Sobolevska, K.; Llorente, A.; Riekstina, U.; Abols, A. Adult Stem Cell-Derived Extracellular Vesicles in Cancer Treatment: Opportunities and Challenges. Cells 2020, 9, 1171. [Google Scholar] [CrossRef] [PubMed]
- Lai, R.C.; Arslan, F.; Lee, M.M.; Sze, N.S.; Choo, A.; Chen, T.S.; Salto-Tellez, M.; Timmers, L.; Lee, C.N.; El Oakley, R.M.; et al. Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. Stem Cell Res. 2010, 4, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Timmers, L.; Lim, S.K.; Hoefer, I.E.; Arslan, F.; Lai, R.C.; van Oorschot, A.A.; Goumans, M.J.; Strijder, C.; Sze, S.K.; Choo, A.; et al. Human mesenchymal stem cell-conditioned medium improves cardiac function following myocardial infarction. Stem Cell Res. 2011, 6, 206–214. [Google Scholar] [CrossRef]
- Gatti, S.; Bruno, S.; Deregibus, M.C.; Sordi, A.; Cantaluppi, V.; Tetta, C.; Camussi, G. Microvesicles derived from human adult mesenchymal stem cells protect against ischaemia-reperfusion-induced acute and chronic kidney injury. Nephrol. Dial. Transplant. 2011, 26, 1474–1483. [Google Scholar] [CrossRef]
- Lai, R.C.; Chen, T.S.; Lim, S.K. Mesenchymal stem cell exosome: A novel stem cell-based therapy for cardiovascular disease. Regen. Med. 2011, 6, 481–492. [Google Scholar] [CrossRef]
- Heldring, N.; Mäger, I.; Wood, M.J.; Le Blanc, K.; Andaloussi, S.E. Therapeutic Potential of Multipotent Mesenchymal Stromal Cells and Their Extracellular Vesicles. Hum. Gene Ther. 2015, 26, 506–517. [Google Scholar] [CrossRef]
- Pi, F.; Binzel, D.W.; Lee, T.J.; Li, Z.; Sun, M.; Rychahou, P.; Li, H.; Haque, F.; Wang, S.; Croce, C.M.; et al. Nanoparticle orientation to control RNA loading and ligand display on extracellular vesicles for cancer regression. Nat. Nanotechnol. 2018, 13, 82–89. [Google Scholar] [CrossRef]
- Witwer, K.W.; Van Balkom, B.W.M.; Bruno, S.; Choo, A.; Dominici, M.; Gimona, M.; Hill, A.F.; De Kleijn, D.; Koh, M.; Lai, R.C.; et al. Defining mesenchymal stromal cell (MSC)-derived small extracellular vesicles for therapeutic applications. J. Extracell. Vesicles 2019, 8, 1609206. [Google Scholar] [CrossRef]
- Timar, C.I.; Lorincz, A.M.; Ligeti, E. Changing world of neutrophils. Pflügers Archiv 2013, 465, 1521–1533. [Google Scholar] [CrossRef]
- Mocsai, A. Diverse novel functions of neutrophils in immunity, inflammation, and beyond. J. Exp. Med. 2013, 210, 1283–1299. [Google Scholar] [CrossRef]
- Tecchio, C.; Cassatella, M.A. Neutrophil-derived chemokines on the road to immunity. Semin. Immunol. 2016, 28, 119–128. [Google Scholar] [CrossRef]
- Duarte, T.A.; Noronha-Dutra, A.A.; Nery, J.S.; Ribeiro, S.B.; Pitanga, T.N.; Lapa, E.S.J.R.; Arruda, S.; Boechat, N. Mycobacterium tuberculosis-induced neutrophil ectosomes decrease macrophage activation. Tuberculosis 2012, 92, 218–225. [Google Scholar] [CrossRef]
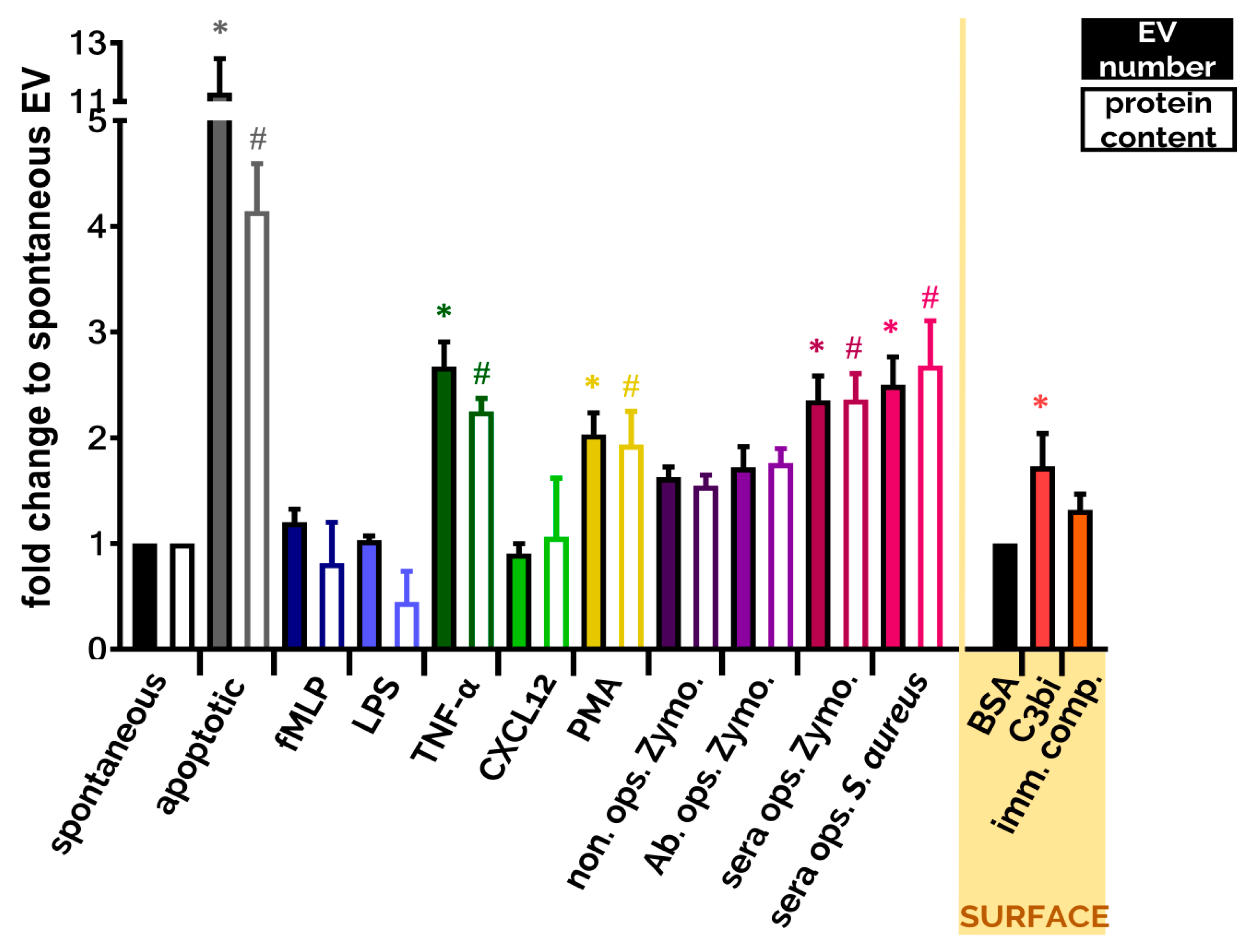
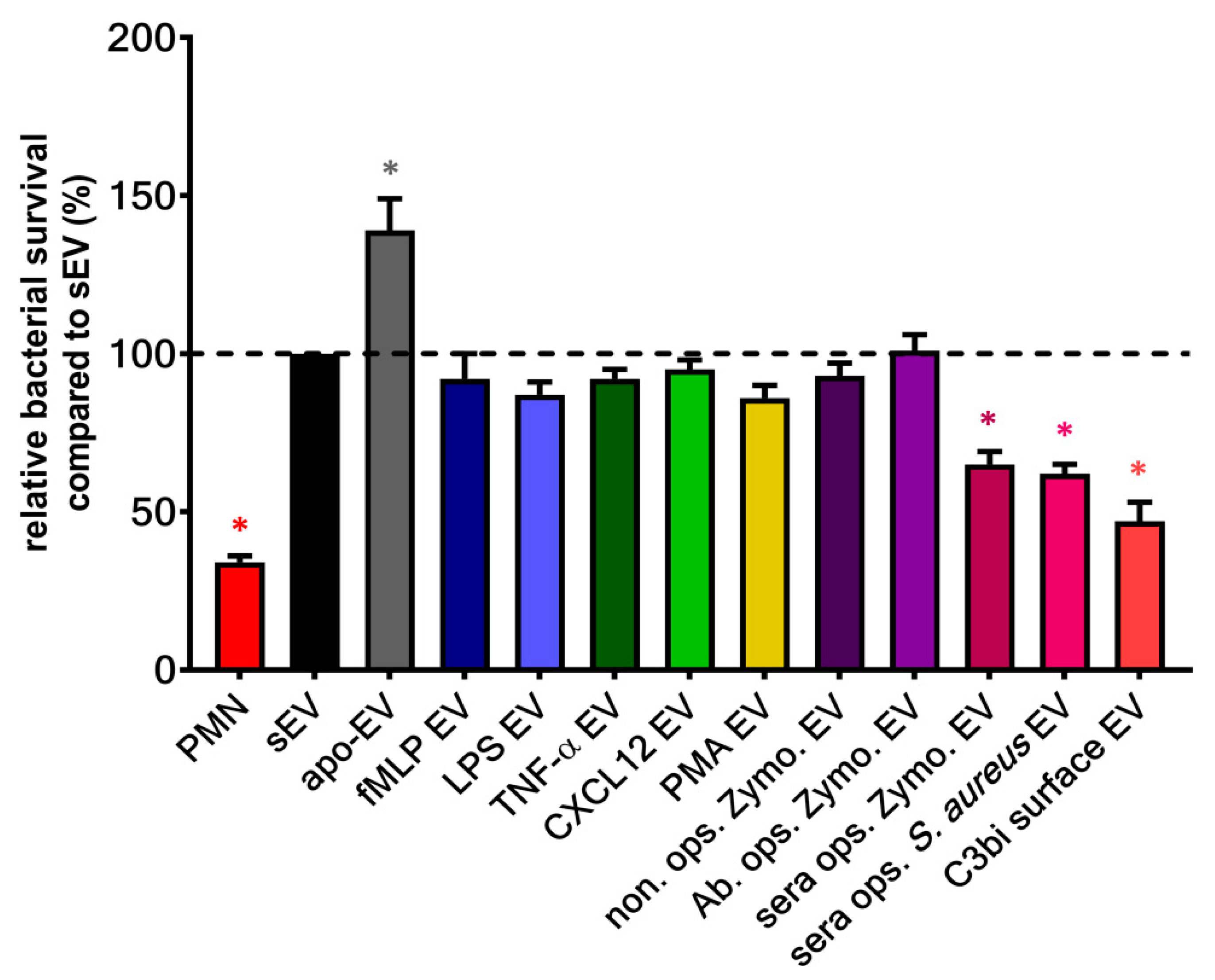
- Kolonics, F.; Kajdacsi, E.; Farkas, V.J.; Veres, D.S.; Khamari, D.; Kittel, A.; Merchant, M.L.; McLeish, K.R.; Lorincz, A.M.; Ligeti, E. Neutrophils produce proinflammatory or anti-inflammatory extracellular vesicles depending on the environmental conditions. J. Leukoc. Biol. 2020. [Google Scholar] [CrossRef]
- Ren, Y.; Stuart, L.; Lindberg, F.P.; Rosenkranz, A.R.; Chen, Y.; Mayadas, T.N.; Savill, J. Nonphlogistic clearance of late apoptotic neutrophils by macrophages: Efficient phagocytosis independent of beta 2 integrins. J. Immunol. 2001, 166, 4743–4750. [Google Scholar] [CrossRef]
- Byrne, A.; Reen, D.J. Lipopolysaccharide induces rapid production of IL-10 by monocytes in the presence of apoptotic neutrophils. J. Immunol. 2002, 168, 1968–1977. [Google Scholar] [CrossRef]
- Salei, N.; Hellberg, L.; Kohl, J.; Laskay, T. Enhanced survival of Leishmania major in neutrophil granulocytes in the presence of apoptotic cells. PLoS ONE 2017, 12, e0171850. [Google Scholar] [CrossRef]
- Shen, G.; Krienke, S.; Schiller, P.; Niessen, A.; Neu, S.; Eckstein, V.; Schiller, M.; Lorenz, H.M.; Tykocinski, L.O. Microvesicles released by apoptotic human neutrophils suppress proliferation and IL-2/IL-2 receptor expression of resting T helper cells. Eur. J. Immunol. 2017, 47, 900–910. [Google Scholar] [CrossRef]
- Ren, Y.; Xie, Y.; Jiang, G.; Fan, J.; Yeung, J.; Li, W.; Tam, P.K.; Savill, J. Apoptotic cells protect mice against lipopolysaccharide-induced shock. J. Immunol. 2008, 180, 4978–4985. [Google Scholar] [CrossRef] [PubMed]
- Eken, C.; Martin, P.J.; Sadallah, S.; Treves, S.; Schaller, M.; Schifferli, J.A. Ectosomes released by polymorphonuclear neutrophils induce a MerTK-dependent anti-inflammatory pathway in macrophages. J. Biol. Chem. 2010, 285, 39914–39921. [Google Scholar] [CrossRef] [PubMed]
- Eken, C.; Gasser, O.; Zenhaeusern, G.; Oehri, I.; Hess, C.; Schifferli, J.A. Polymorphonuclear neutrophil-derived ectosomes interfere with the maturation of monocyte-derived dendritic cells. J. Immunol. 2008, 180, 817–824. [Google Scholar] [CrossRef]
- Gasser, O.; Schifferli, J.A. Activated polymorphonuclear neutrophils disseminate anti-inflammatory microparticles by ectocytosis. Blood 2004, 104, 2543–2548. [Google Scholar] [CrossRef]
- Cumpelik, A.; Ankli, B.; Zecher, D.; Schifferli, J.A. Neutrophil microvesicles resolve gout by inhibiting C5a-mediated priming of the inflammasome. Ann. Rheum. Dis. 2016, 75, 1236–1245. [Google Scholar] [CrossRef] [PubMed]
- Pliyev, B.K.; Kalintseva, M.V.; Abdulaeva, S.V.; Yarygin, K.N.; Savchenko, V.G. Neutrophil microparticles modulate cytokine production by natural killer cells. Cytokine 2014, 65, 126–129. [Google Scholar] [CrossRef]
- Dalli, J.; Norling, L.V.; Renshaw, D.; Cooper, D.; Leung, K.Y.; Perretti, M. Annexin 1 mediates the rapid anti-inflammatory effects of neutrophil-derived microparticles. Blood 2008, 112, 2512–2519. [Google Scholar] [CrossRef]
- Mesri, M.; Altieri, D.C. Leukocyte microparticles stimulate endothelial cell cytokine release and tissue factor induction in a JNK1 signaling pathway. J. Biol. Chem. 1999, 274, 23111–23118. [Google Scholar] [CrossRef]
- Mesri, M.; Altieri, D.C. Endothelial cell activation by leukocyte microparticles. J. Immunol. 1998, 161, 4382–4387. [Google Scholar]
- Gomez, I.; Ward, B.; Souilhol, C.; Recarti, C.; Ariaans, M.; Johnston, J.; Burnett, A.; Mahmoud, M.; Luong, L.A.; West, L.; et al. Neutrophil microvesicles drive atherosclerosis by delivering miR-155 to atheroprone endothelium. Nat. Commun. 2020, 11, 214. [Google Scholar] [CrossRef]
- Ajikumar, A.; Long, M.B.; Heath, P.R.; Wharton, S.B.; Ince, P.G.; Ridger, V.C.; Simpson, J.E. Neutrophil-Derived Microvesicle Induced Dysfunction of Brain Microvascular Endothelial Cells In Vitro. Int. J. Mol. Sci. 2019, 20, 5227. [Google Scholar] [CrossRef] [PubMed]
- Butin-Israeli, V.; Bui, T.M.; Wiesolek, H.L.; Mascarenhas, L.; Lee, J.J.; Mehl, L.C.; Knutson, K.R.; Adam, S.A.; Goldman, R.D.; Beyder, A.; et al. Neutrophil-induced genomic instability impedes resolution of inflammation and wound healing. J. Clin. Investig. 2019, 129, 712–726. [Google Scholar] [CrossRef]
- Rossaint, J.; Kuhne, K.; Skupski, J.; Van Aken, H.; Looney, M.R.; Hidalgo, A.; Zarbock, A. Directed transport of neutrophil-derived extracellular vesicles enables platelet-mediated innate immune response. Nat. Commun. 2016, 7, 13464. [Google Scholar] [CrossRef]
- Dalli, J.; Montero-Melendez, T.; Norling, L.V.; Yin, X.; Hinds, C.; Haskard, D.; Mayr, M.; Perretti, M. Heterogeneity in neutrophil microparticles reveals distinct proteome and functional properties. Mol. Cell. Proteom. 2013, 12, 2205–2219. [Google Scholar] [CrossRef]
- Alvarez-Jimenez, V.D.; Leyva-Paredes, K.; Garcia-Martinez, M.; Vazquez-Flores, L.; Garcia-Paredes, V.G.; Campillo-Navarro, M.; Romo-Cruz, I.; Rosales-Garcia, V.H.; Castaneda-Casimiro, J.; Gonzalez-Pozos, S.; et al. Extracellular Vesicles Released from Mycobacterium tuberculosis-Infected Neutrophils Promote Macrophage Autophagy and Decrease Intracellular Mycobacterial Survival. Front. Immunol. 2018, 9, 272. [Google Scholar] [CrossRef]
- Dalli, J.; Norling, L.V.; Montero-Melendez, T.; Federici Canova, D.; Lashin, H.; Pavlov, A.M.; Sukhorukov, G.B.; Hinds, C.J.; Perretti, M. Microparticle alpha-2-macroglobulin enhances pro-resolving responses and promotes survival in sepsis. EMBO Mol. Med. 2014, 6, 27–42. [Google Scholar] [CrossRef]
- Genschmer, K.R.; Russell, D.W.; Lal, C.; Szul, T.; Bratcher, P.E.; Noerager, B.D.; Abdul Roda, M.; Xu, X.; Rezonzew, G.; Viera, L.; et al. Activated PMN Exosomes: Pathogenic Entities Causing Matrix Destruction and Disease in the Lung. Cell 2019, 176, 113–126.e15. [Google Scholar] [CrossRef]
- Butin-Israeli, V.; Houser, M.C.; Feng, M.; Thorp, E.B.; Nusrat, A.; Parkos, C.A.; Sumagin, R. Deposition of microparticles by neutrophils onto inflamed epithelium: A new mechanism to disrupt epithelial intercellular adhesions and promote transepithelial migration. FASEB J. 2016, 30, 4007–4020. [Google Scholar] [CrossRef]
- Lim, K.; Sumagin, R.; Hyun, Y.M. Extravasating Neutrophil-derived Microparticles Preserve Vascular Barrier Function in Inflamed Tissue. Immune Netw. 2013, 13, 102–106. [Google Scholar] [CrossRef][Green Version]
- Hess, C.; Sadallah, S.; Hefti, A.; Landmann, R.; Schifferli, J.A. Ectosomes released by human neutrophils are specialized functional units. J. Immunol. 1999, 163, 4564–4573. [Google Scholar] [CrossRef]
- Slater, T.W.; Finkielsztein, A.; Mascarenhas, L.A.; Mehl, L.C.; Butin-Israeli, V.; Sumagin, R. Neutrophil Microparticles Deliver Active Myeloperoxidase to Injured Mucosa To Inhibit Epithelial Wound Healing. J. Immunol. 2017, 198, 2886–2897. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, R.; Tavakoli Tameh, A.; Parent, C.A. Exosomes Mediate LTB4 Release during Neutrophil Chemotaxis. PLoS Biol. 2016, 14, e1002336. [Google Scholar] [CrossRef] [PubMed]
- Moraes, J.A.; Frony, A.C.; Barcellos-de-Souza, P.; Menezes da Cunha, M.; Brasil Barbosa Calcia, T.; Benjamim, C.F.; Boisson-Vidal, C.; Barja-Fidalgo, C. Downregulation of Microparticle Release and Pro-Inflammatory Properties of Activated Human Polymorphonuclear Neutrophils by LMW Fucoidan. J. Innate Immun. 2019, 11, 330–346. [Google Scholar] [CrossRef] [PubMed]
- El Habhab, A.; Altamimy, R.; Abbas, M.; Kassem, M.; Amoura, L.; Qureshi, A.W.; El Itawi, H.; Kreutter, G.; Khemais-Benkhiat, S.; Zobairi, F.; et al. Significance of neutrophil microparticles in ischaemia-reperfusion: Pro-inflammatory effectors of endothelial senescence and vascular dysfunction. J. Cell. Mol. Med. 2020, 24, 7266–7281. [Google Scholar] [CrossRef] [PubMed]
- Vargas, A.; Roux-Dalvai, F.; Droit, A.; Lavoie, J.P. Neutrophil-Derived Exosomes: A New Mechanism Contributing to Airway Smooth Muscle Remodeling. Am. J. Respir. Cell Mol. Biol. 2016, 55, 450–461. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, J.; Marathe, G.K.; Neilsen, P.O.; Weyrich, A.S.; Harrison, K.A.; Murphy, R.C.; Zimmerman, G.A.; McIntyre, T.M. Endotoxins stimulate neutrophil adhesion followed by synthesis and release of platelet-activating factor in microparticles. J. Biol. Chem. 2003, 278, 33161–33168. [Google Scholar] [CrossRef]
- Pluskota, E.; Woody, N.M.; Szpak, D.; Ballantyne, C.M.; Soloviev, D.A.; Simon, D.I.; Plow, E.F. Expression, activation, and function of integrin alphaMbeta2 (Mac-1) on neutrophil-derived microparticles. Blood 2008, 112, 2327–2335. [Google Scholar] [CrossRef]
- Rhys, H.I.; Dell’Accio, F.; Pitzalis, C.; Moore, A.; Norling, L.V.; Perretti, M. Neutrophil Microvesicles from Healthy Control and Rheumatoid Arthritis Patients Prevent the Inflammatory Activation of Macrophages. EBioMedicine 2018, 29, 60–69. [Google Scholar] [CrossRef]
- Kahn, R.; Mossberg, M.; Stahl, A.L.; Johansson, K.; Lopatko Lindman, I.; Heijl, C.; Segelmark, M.; Morgelin, M.; Leeb-Lundberg, L.M.; Karpman, D. Microvesicle transfer of kinin B1-receptors is a novel inflammatory mechanism in vasculitis. Kidney Int. 2017, 91, 96–105. [Google Scholar] [CrossRef]
- Lashin, H.M.S.; Nadkarni, S.; Oggero, S.; Jones, H.R.; Knight, J.C.; Hinds, C.J.; Perretti, M. Microvesicle Subsets in Sepsis Due to Community Acquired Pneumonia Compared to Faecal Peritonitis. Shock 2018, 49, 393–401. [Google Scholar] [CrossRef]
- Karasu, E.; Demmelmaier, J.; Kellermann, S.; Holzmann, K.; Kohl, J.; Schmidt, C.Q.; Kalbitz, M.; Gebhard, F.; Huber-Lang, M.S.; Halbgebauer, R. Complement C5a Induces Pro-inflammatory Microvesicle Shedding in Severely Injured Patients. Front. Immunol. 2020, 11, 1789. [Google Scholar] [CrossRef] [PubMed]
- Shopova, I.A.; Belyaev, I.; Dasari, P.; Jahreis, S.; Stroe, M.C.; Cseresnyes, Z.; Zimmermann, A.K.; Medyukhina, A.; Svensson, C.M.; Kruger, T.; et al. Human Neutrophils Produce Antifungal Extracellular Vesicles against Aspergillus fumigatus. mBio 2020, 11, e00596-20. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.A.; Li, X.; Seitz, A.; Steinmann, J.; Koch, A.; Schuchman, E.; Kamler, M.; Edwards, M.J.; Caldwell, C.C.; Gulbins, E. Neutrophils Kill Reactive Oxygen Species-Resistant Pseudomonas aeruginosa by Sphingosine. Cell. Physiol. Biochem. 2017, 43, 1603–1616. [Google Scholar] [CrossRef] [PubMed]
- Timar, C.I.; Lorincz, A.M.; Csepanyi-Komi, R.; Valyi-Nagy, A.; Nagy, G.; Buzas, E.I.; Ivanyi, Z.; Kittel, A.; Powell, D.W.; McLeish, K.R.; et al. Antibacterial effect of microvesicles released from human neutrophilic granulocytes. Blood 2013, 121, 510–518. [Google Scholar] [CrossRef]
- Lorincz, A.M.; Szeifert, V.; Bartos, B.; Szombath, D.; Mocsai, A.; Ligeti, E. Different Calcium and Src Family Kinase Signaling in Mac-1 Dependent Phagocytosis and Extracellular Vesicle Generation. Front. Immunol. 2019, 10, 2942. [Google Scholar] [CrossRef]
- Turbica, I.; Gallais, Y.; Gueguen, C.; Tharinger, H.; Al Sabbagh, C.; Gorges, R.; Gary-Gouy, H.; Kerdine-Romer, S.; Pallardy, M.; Mascarell, L.; et al. Ectosomes from neutrophil-like cells down-regulate nickel-induced dendritic cell maturation and promote Th2 polarization. J. Leukoc. Biol. 2015, 97, 737–749. [Google Scholar] [CrossRef]
- Wang, Y.; Luo, L.; Braun, O.O.; Westman, J.; Madhi, R.; Herwald, H.; Morgelin, M.; Thorlacius, H. Neutrophil extracellular trap-microparticle complexes enhance thrombin generation via the intrinsic pathway of coagulation in mice. Sci. Rep. 2018, 8, 4020. [Google Scholar] [CrossRef]
- Pitanga, T.N.; de Aragao Franca, L.; Rocha, V.C.; Meirelles, T.; Borges, V.M.; Goncalves, M.S.; Pontes-de-Carvalho, L.C.; Noronha-Dutra, A.A.; dos-Santos, W.L. Neutrophil-derived microparticles induce myeloperoxidase-mediated damage of vascular endothelial cells. BMC Cell Biol. 2014, 15, 21. [Google Scholar] [CrossRef]
- Nolan, S.; Dixon, R.; Norman, K.; Hellewell, P.; Ridger, V. Nitric oxide regulates neutrophil migration through microparticle formation. Am. J. Pathol. 2008, 172, 265–273. [Google Scholar] [CrossRef]
- Prakash, P.S.; Caldwell, C.C.; Lentsch, A.B.; Pritts, T.A.; Robinson, B.R. Human microparticles generated during sepsis in patients with critical illness are neutrophil-derived and modulate the immune response. J. Trauma Acute Care Surg. 2012, 73, 401–407. [Google Scholar] [CrossRef]
- Herrmann, I.K.; Bertazzo, S.; O’Callaghan, D.J.; Schlegel, A.A.; Kallepitis, C.; Antcliffe, D.B.; Gordon, A.C.; Stevens, M.M. Differentiating sepsis from non-infectious systemic inflammation based on microvesicle-bacteria aggregation. Nanoscale 2015, 7, 13511–13520. [Google Scholar] [CrossRef] [PubMed]
- Kumagai, Y.; Murakami, T.; Kuwahara, A.; Iba, T.; Reich, J.; Nagaoka, I. Antimicrobial peptide LL-37 ameliorates a murine sepsis model via the induction of microvesicle release from neutrophils. Innate Immun. 2020, 26, 565–579. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.L., 3rd; Midura, E.F.; Prakash, P.S.; Rice, T.C.; Kunz, N.; Kalies, K.; Caldwell, C.C. Neutrophil derived microparticles increase mortality and the counter-inflammatory response in a murine model of sepsis. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 2554–2563. [Google Scholar] [CrossRef] [PubMed]
- Porro, C.; Di Gioia, S.; Trotta, T.; Lepore, S.; Panaro, M.A.; Battaglino, A.; Ratclif, L.; Castellani, S.; Bufo, P.; Martinez, M.C.; et al. Pro-inflammatory effect of cystic fibrosis sputum microparticles in the murine lung. J. Cyst. Fibros. 2013, 12, 721–728. [Google Scholar] [CrossRef]
- Madhi, R.; Rahman, M.; Taha, D.; Linders, J.; Merza, M.; Wang, Y.; Morgelon, M.; Thorlacius, H. Platelet IP6K1 regulates neutrophil extracellular trap-microparticle complex formation in acute pancreatitis. JCI Insight 2019, 4, e135102. [Google Scholar] [CrossRef]
- Kambas, K.; Chrysanthopoulou, A.; Vassilopoulos, D.; Apostolidou, E.; Skendros, P.; Girod, A.; Arelaki, S.; Froudarakis, M.; Nakopoulou, L.; Giatromanolaki, A.; et al. Tissue factor expression in neutrophil extracellular traps and neutrophil derived microparticles in antineutrophil cytoplasmic antibody associated vasculitis may promote thromboinflammation and the thrombophilic state associated with the disease. Ann. Rheum. Dis. 2014, 73, 1854–1863. [Google Scholar] [CrossRef]
- Hong, Y.; Eleftheriou, D.; Hussain, A.A.; Price-Kuehne, F.E.; Savage, C.O.; Jayne, D.; Little, M.A.; Salama, A.D.; Klein, N.J.; Brogan, P.A. Anti-neutrophil cytoplasmic antibodies stimulate release of neutrophil microparticles. J. Am. Soc. Nephrol. 2012, 23, 49–62. [Google Scholar] [CrossRef]
- Thom, S.R.; Bhopale, V.M.; Yu, K.; Huang, W.; Kane, M.A.; Margolis, D.J. Neutrophil microparticle production and inflammasome activation by hyperglycemia due to cytoskeletal instability. J. Biol. Chem. 2017, 292, 18312–18324. [Google Scholar] [CrossRef]
- Gardiner, C.; Di Vizio, D.; Sahoo, S.; Thery, C.; Witwer, K.W.; Wauben, M.; Hill, A.F. Techniques used for the isolation and characterization of extracellular vesicles: Results of a worldwide survey. J. Extracell. Vesicles 2016, 5, 32945. [Google Scholar] [CrossRef]
- Lorincz, A.M.; Bartos, B.; Szombath, D.; Szeifert, V.; Timar, C.I.; Turiak, L.; Drahos, L.; Kittel, A.; Veres, D.S.; Kolonics, F.; et al. Role of Mac-1 integrin in generation of extracellular vesicles with antibacterial capacity from neutrophilic granulocytes. J. Extracell. Vesicles 2020, 9, 1698889. [Google Scholar] [CrossRef]
- Lorincz, A.M.; Timar, C.I.; Marosvari, K.A.; Veres, D.S.; Otrokocsi, L.; Kittel, A.; Ligeti, E. Effect of storage on physical and functional properties of extracellular vesicles derived from neutrophilic granulocytes. J. Extracell. Vesicles 2014, 3, 25465. [Google Scholar] [CrossRef] [PubMed]
- Théry, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 2018, 7, 1535750. [Google Scholar] [CrossRef]
- Gasser, O.; Hess, C.; Miot, S.; Deon, C.; Sanchez, J.C.; Schifferli, J.A. Characterisation and properties of ectosomes released by human polymorphonuclear neutrophils. Exp. Cell Res. 2003, 285, 243–257. [Google Scholar] [CrossRef]
- Allen, E.R.; Lempke, S.L.; Miller, M.M.; Bush, D.M.; Braswell, B.G.; Estes, C.L.; Benedict, E.L.; Mahon, A.R.; Sabo, S.L.; Greenlee-Wacker, M.C. Effect of extracellular vesicles from S. aureus-challenged human neutrophils on macrophages. J. Leukoc. Biol. 2020, 108, 1841–1850. [Google Scholar] [CrossRef] [PubMed]
- Fujimi, S.; Ogura, H.; Tanaka, H.; Koh, T.; Hosotsubo, H.; Nakamori, Y.; Kuwagata, Y.; Shimazu, T.; Sugimoto, H. Activated polymorphonuclear leukocytes enhance production of leukocyte microparticles with increased adhesion molecules in patients with sepsis. J. Trauma 2002, 52, 443–448. [Google Scholar] [CrossRef] [PubMed]
- Daniel, L.; Fakhouri, F.; Joly, D.; Mouthon, L.; Nusbaum, P.; Grunfeld, J.P.; Schifferli, J.; Guillevin, L.; Lesavre, P.; Halbwachs-Mecarelli, L. Increase of circulating neutrophil and platelet microparticles during acute vasculitis and hemodialysis. Kidney Int. 2006, 69, 1416–1423. [Google Scholar] [CrossRef]
- Martinez, G.J.; Barraclough, J.Y.; Nakhla, S.; Kienzle, V.; Robertson, S.; Mallat, Z.; Celermajer, D.S.; Patel, S. Neutrophil-derived microparticles are released into the coronary circulation following percutaneous coronary intervention in acute coronary syndrome patients. Biosci. Rep. 2017, 37. [Google Scholar] [CrossRef]
- Gyorgy, B.; Szabo, T.G.; Pasztoi, M.; Pal, Z.; Misjak, P.; Aradi, B.; Laszlo, V.; Pallinger, E.; Pap, E.; Kittel, A.; et al. Membrane vesicles, current state-of-the-art: Emerging role of extracellular vesicles. Cell. Mol. Life Sci. 2011, 68, 2667–2688. [Google Scholar] [CrossRef]
- Lorincz, A.M.; Szeifert, V.; Bartos, B.; Ligeti, E. New flow cytometry-based method for the assessment of the antibacterial effect of immune cells and subcellular particles. J. Leukoc. Biol. 2018, 103, 955–963. [Google Scholar] [CrossRef]
- Deng, S.; Wang, Y.; Liu, S.; Chen, T.; Hu, Y.; Zhang, G.; Zhang, X.; Yu, B. Extracellular Vesicles: A Potential Biomarker for Quick Identification of Infectious Osteomyelitis. Front. Cell. Infect. Microbiol. 2020, 10, 323. [Google Scholar] [CrossRef]
- Nieuwland, R.; Berckmans, R.J.; McGregor, S.; Boing, A.N.; Romijn, F.P.; Westendorp, R.G.; Hack, C.E.; Sturk, A. Cellular origin and procoagulant properties of microparticles in meningococcal sepsis. Blood 2000, 95, 930–935. [Google Scholar] [CrossRef]
- Joop, K.; Berckmans, R.J.; Nieuwland, R.; Berkhout, J.; Romijn, F.P.; Hack, C.E.; Sturk, A. Microparticles from patients with multiple organ dysfunction syndrome and sepsis support coagulation through multiple mechanisms. Thromb. Haemost. 2001, 85, 810–820. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zhou, X.; Zhang, H.; Yao, Q.; Liu, Y.; Dong, Z. Extracellular vesicles in diagnosis and therapy of kidney diseases. Am. J. Physiol. Ren. Physiol. 2016, 311, F844–F851. [Google Scholar] [CrossRef] [PubMed]
- O’Dea, K.P.; Porter, J.R.; Tirlapur, N.; Katbeh, U.; Singh, S.; Handy, J.M.; Takata, M. Circulating Microvesicles Are Elevated Acutely following Major Burns Injury and Associated with Clinical Severity. PLoS ONE 2016, 11, e0167801. [Google Scholar] [CrossRef] [PubMed]
- Raeven, P.; Zipperle, J.; Drechsler, S. Extracellular Vesicles as Markers and Mediators in Sepsis. Theranostics 2018, 8, 3348–3365. [Google Scholar] [CrossRef]
- Nadkarni, S.; Lashin, H.; Hollywood, J.; Dasgupta, B.; Mason, J.C.; Perretti, M. Identification of an activated neutrophil phenotype in polymyalgia rheumatica during steroid treatment: A potential involvement of immune cell cross-talk. Clin. Sci. 2019, 133, 839–851. [Google Scholar] [CrossRef]
- Guimaraes Junior, M.H.; Ferrari, T.C.A.; Teixeira-Carvalho, A.; Moreira, M.L.; de Souza Santos, L.J.; Costa-Silva, M.F.; Coelho, R.M.P.; Pinto, P.; Ris, T.H.; Salles, J.T.; et al. Cell-derived microvesicles in infective endocarditis: Role in diagnosis and potential for risk stratification at hospital admission. J. Infect. 2019, 79, 101–107. [Google Scholar] [CrossRef]
- Suades, R.; Padro, T.; Crespo, J.; Sionis, A.; Alonso, R.; Mata, P.; Badimon, L. Liquid Biopsy of Extracellular Microvesicles Predicts Future Major Ischemic Events in Genetically Characterized Familial Hypercholesterolemia Patients. Arter. Thromb. Vasc. Biol. 2019, 39, 1172–1181. [Google Scholar] [CrossRef]
- Gyorgy, B.; Hung, M.E.; Breakefield, X.O.; Leonard, J.N. Therapeutic applications of extracellular vesicles: Clinical promise and open questions. Annu. Rev. Pharm. Toxicol. 2015, 55, 439–464. [Google Scholar] [CrossRef]
- Wiklander, O.P.B.; Brennan, M.A.; Lotvall, J.; Breakefield, X.O.; El Andaloussi, S. Advances in therapeutic applications of extracellular vesicles. Sci. Transl. Med. 2019, 11, eaav8521. [Google Scholar] [CrossRef]
- Wang, S.; Dong, X.; Gao, J.; Wang, Z. Targeting Inflammatory Vasculature by Extracellular Vesicles. AAPS J. 2018, 20, 37. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Dong, X.; Wang, Z. Generation, purification and engineering of extracellular vesicles and their biomedical applications. Methods 2020, 177, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Gao, J.; Zhang, C.Y.; Hayworth, C.; Frank, M.; Wang, Z. Neutrophil Membrane-Derived Nanovesicles Alleviate Inflammation To Protect Mouse Brain Injury from Ischemic Stroke. ACS Nano 2019, 13, 1272–1283. [Google Scholar] [CrossRef] [PubMed]
- Lotvall, J.; Hill, A.F.; Hochberg, F.; Buzas, E.I.; Di Vizio, D.; Gardiner, C.; Gho, Y.S.; Kurochkin, I.V.; Mathivanan, S.; Quesenberry, P.; et al. Minimal experimental requirements for definition of extracellular vesicles and their functions: A position statement from the International Society for Extracellular Vesicles. J. Extracell. Vesicles 2014, 3, 26913. [Google Scholar] [CrossRef]
- Ayers, L.; Pink, R.; Carter, D.R.F.; Nieuwland, R. Clinical requirements for extracellular vesicle assays. J. Extracell. Vesicles 2019, 8, 1593755. [Google Scholar] [CrossRef]
- Boing, A.N.; van der Pol, E.; Grootemaat, A.E.; Coumans, F.A.; Sturk, A.; Nieuwland, R. Single-step isolation of extracellular vesicles by size-exclusion chromatography. J. Extracell. Vesicles 2014, 3, 23430. [Google Scholar] [CrossRef]
- Welsh, J.A.; Van Der Pol, E.; Arkesteijn, G.J.A.; Bremer, M.; Brisson, A.; Coumans, F.; Dignat-George, F.; Duggan, E.; Ghiran, I.; Giebel, B.; et al. MIFlowCyt-EV: A framework for standardized reporting of extracellular vesicle flow cytometry experiments. J. Extracell. Vesicles 2020, 9, 1713526. [Google Scholar] [CrossRef]
- Gandham, S.; Su, X.; Wood, J.; Nocera, A.L.; Alli, S.C.; Milane, L.; Zimmerman, A.; Amiji, M.; Ivanov, A.R. Technologies and Standardization in Research on Extracellular Vesicles. Trends Biotechnol. 2020, 38, 1066–1098. [Google Scholar] [CrossRef]
- Clayton, A.; Boilard, E.; Buzas, E.I.; Cheng, L.; Falcon-Perez, J.M.; Gardiner, C.; Gustafson, D.; Gualerzi, A.; Hendrix, A.; Hoffman, A.; et al. Considerations towards a roadmap for collection, handling and storage of blood extracellular vesicles. J. Extracell. Vesicles 2019, 8, 1647027. [Google Scholar] [CrossRef]
- Yuana, Y.; Boing, A.N.; Grootemaat, A.E.; van der Pol, E.; Hau, C.M.; Cizmar, P.; Buhr, E.; Sturk, A.; Nieuwland, R. Handling and storage of human body fluids for analysis of extracellular vesicles. J. Extracell. Vesicles 2015, 4, 29260. [Google Scholar] [CrossRef]
- Gyorgy, B.; Modos, K.; Pallinger, E.; Paloczi, K.; Pasztoi, M.; Misjak, P.; Deli, M.A.; Sipos, A.; Szalai, A.; Voszka, I.; et al. Detection and isolation of cell-derived microparticles are compromised by protein complexes resulting from shared biophysical parameters. Blood 2011, 117, e39–e48. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, M.I.; Amorim, M.G.; Gadelha, C.; Milic, I.; Welsh, J.A.; Freitas, V.M.; Nawaz, M.; Akbar, N.; Couch, Y.; Makin, L.; et al. Technical challenges of working with extracellular vesicles. Nanoscale 2018, 10, 881–906. [Google Scholar] [CrossRef] [PubMed]
- El Kebir, D.; Filep, J.G. Role of neutrophil apoptosis in the resolution of inflammation. ScientificWorldJournal 2010, 10, 1731–1748. [Google Scholar] [CrossRef] [PubMed]
- Dalli, J.; Serhan, C.N. Specific lipid mediator signatures of human phagocytes: Microparticles stimulate macrophage efferocytosis and pro-resolving mediators. Blood 2012, 120, e60–e72. [Google Scholar] [CrossRef]
- Poon, I.K.; Lucas, C.D.; Rossi, A.G.; Ravichandran, K.S. Apoptotic cell clearance: Basic biology and therapeutic potential. Nat. Rev. Immunol. 2014, 14, 166–180. [Google Scholar] [CrossRef]
- Boeltz, S.; Hagen, M.; Knopf, J.; Mahajan, A.; Schick, M.; Zhao, Y.; Erfurt-Berge, C.; Rech, J.; Munoz, L.E.; Herrmann, M. Towards a pro-resolving concept in systemic lupus erythematosus. Semin. Immunopathol. 2019, 41, 681–697. [Google Scholar] [CrossRef]
| PMN-EV Induction Stimulus | Target | Effect | PMN Purity | PMN Viability | EV Isolation Method | EV Characterization Method | EV Diameter [nm] | EV Storage | Ref. | |
|---|---|---|---|---|---|---|---|---|---|---|
| Unstimulated | Spontaneous release | HMDM | Bacterial killing ↓ | ? (nuclear morphology analyzed with light microscopy) | 95% (Trypan Blue) | DC | FC, EM | 50–300 | −80 °C | [85] |
| PMN, HUVEC, plasma | Anti-inflammatory, PMN ROS production ↓, pro-coagulant | >95% | ? | DC + F | FC, DLS, NTA, EM | 80–1000 | none | [86] | ||
| Apoptosis induction | none | No pro-inflammatory effect | ? | n/a | no isolation | FC | ? | ? | [87] | |
| Monocytes, HMDM | Mostly anti-inflammatory, but IL-10 production of HMDM ↓ | >90% (CD15 FC) | n/a | no isolation | FC | ? | −70 °C | [88] | ||
| PMN | ROS production ↓, Leishmania killing ↓ | >99.9% (Diff Quik) | n/a | no isolation | FC | ? | n/a | [89] | ||
| Th cells | Anti-inflammatory | ? | n/a | DC + F | FC, NTA | 100–400 | ? | [90] | ||
| HMDM | Anti-inflammatory | ? | n/a | no isolation | FC | ? | ? | [91] | ||
| PMN, HUVEC, plasma | PMN ROS production delayed, pro-coagulant | >95% | ? | DC + F | FC, DLS, NTA, EM | 80–1000 | none | [86] | ||
| Bacterial byproducts | fMLP | HMDM | Anti-inflammatory | ? | ? | DC + F | ? | ? | −80 °C | [92] |
| MoDC | Anti-inflammatory, anti-phagocytic | ? | ? | DC + F | FC | ? | −80 °C | [93] | ||
| HMDM | Anti-inflammatory | ? | ? | DC + F | none | ? | −80 °C | [94] | ||
| Peritoneal macrophages | Anti-inflammatory | ? | ? | DC | FC, EM | 50–500 | ? | [95] | ||
| NK cells | Anti-inflammatory | 95% or 99% (FC) | ? | DC | FC | 200–1000 | ? | [96] | ||
| PMN, systemic | PMN recruitment ↓, PMN-EC interaction ↓ | ? | ? | DC | FC | ? | ? | [97] | ||
| HUVEC | Pro-inflammatory, TF expression ↑ | ? | ? | F or DC | FC | ? | ? | [98] | ||
| HUVEC | Pro-inflammatory | ? | ? | DC + F | FC | ? | ? | [99] | ||
| Human coronary endothelial cells | Pro-inflammatory, pro-migratory | ? | ? | DC + dialysis | FC, TRPS—human, NTA—mouse | 280 (human), 165 (mouse) | ? | [100] | ||
| BMEC | Vascular permeability ↑ | ? | ? | DC | FC, NTA | 100–300 | ? | [101] | ||
| IEC | Delivers pro-inflammatory miR content, genomic instability, impaired wound healing | Human: ?, Mouse: 85–90% | ? | DC | EM | ? | ? | [102] | ||
| PLT | Arachidonic acid transfer to PLT, causing TXA2 release and subsequent pro-inflammatory EC activation | ? | ? | ExoQuick-TC kit | ? | ? | ? | [103] | ||
| HUVEC | Non-adherent PMN-derived EVs: anti-inflammatory, vasoprotective. Adherent PMN-derived EVs: pro-inflammatory, vasoreactive | ? | ? | DC | FC | ? | −80 °C | [104] | ||
| HMDM | Pro-inflammatory, bacterial killing ↑ | >98% | >98% | DC | FC, NTA, EM | 100–200 | 4 °C <24 h | [105] | ||
| HMDM, PMN, systemic | Pro- and anti-inflammatory, bacterial killing ↑, PMN and macrophage ROS production ↑ | ? | ? | DC | FC | 2000–3000 | −80 °C | [106] | ||
| ECM | Neutrophil elastase-dependent degradation of ECM | ? | >95% (Trypan Blue) | DC | FC, NTA, EM | 100 | −80 °C or fresh | [107] | ||
| IEC | Disruption of epithelial intercellular adhesion, enhanced transepithelial migration | Human: ?, Mouse: 85–90% | ? | DC | FC, EM | 100–800 | ? | [108] | ||
| Vascular permeability | Maintaining the integrity of the microvascular barrier | ? | ? | no isolation | FC | ? | ? | [109] | ||
| S. aureus | Binding to opsonized bacteria | >98% | >99% before and after stimulation (Trypan Blue) | DC + F | EM | ? | ? | [110] | ||
| fMLP or fMLP + LatrB | IEC | Inhibition of epithelial wound healing via MPO delivery | Human: ?, Mouse: 85–90% | ? | no isolation | FC, EM | 600 | ? | [111] | |
| GM-CSF + (?) fMLP | PMN | Pro-inflammatory | ? | ? | DC + F | FC, EM | 50–120 (purified from 50–500) | ? | [112] | |
| fMLP + LPS | PMN, HMDM | ROS production ↑ | ? | ? | DC | FC | ? | ? | [113] | |
| LPS | P1EC, artery rings | Pro-inflammatory, oxidative stress ↑, TF expression ↑ | n/a (splenocytes) | ? | DC | TRPS | 200–500 | ? | [114] | |
| Airway smooth muscle cells | Proliferation | 99.5% (Cytospin slide + Protocol Hema 3 staining) | 97.75% (ADAM cell counter) | Size-exclusion chromatography | DLS, EM | 30–80 | −80 °C | [115] | ||
| PLT | Platelet activation and co-aggregation with PMN, delivery of PAF receptor | ? | ? | DC | none | ? | ? | [116] | ||
| PLT | Platelet activation | ? | ? | DC + F | FC | <1000 | −80 °C | [117] | ||
| Endogenous pro-inflammatory mediators | TNFα | HDMD, joints, macrophage-FLS co-culture system | Anti-inflammatory | ? | ? | DC | FC, NTA | 70–400 | ? | [118] |
| IEC | Delivers pro-inflammatory miR content, genomic instability, impaired wound healing | Human: ?, Mouse: 85–90% | ? | DC | EM | ? | ? | [108] | ||
| Embryonic kidney cells | Transfer of kinin B1-receptors, calcium influx | ? | ? | DC | FC, EM | 150 | −80 °C | [119] | ||
| IFN-γ | IEC | Delivers pro-inflammatory miR content, genomic instability, impaired wound healing | Human: ?, Mouse: 85–90% | ? | DC | EM | ? | ? | [108] | |
| PMN, HUVEC | Mainly pro-inflammatory and pro-migratory, but reduced increase in EC permeability upon LPS treatment | n/a (stimulation in whole blood) | n/a (stimulation in whole blood) | ? (DC) | FC | ? | ? | [120] | ||
| GM-CSF | PMN, HUVEC | Mainly pro-inflammatory and pro-migratory, EC ROS production ↑, but reduced increase in EC permeability upon LPS treatment | n/a (stimulation in whole blood) | n/a (stimulation in whole blood) | ? (DC) | FC | ? | ? | [120] | |
| C5a | HMDM | Anti-inflammatory | ? | ? | DC + F | none | ? | −80 °C | [94] | |
| NK | Anti-inflammatory | 95% or 99% (FC) | ? | DC | FC | 200–1000 | ? | [96] | ||
| PMN, whole blood | Pro-inflammatory, ROS production ↑, MPO release ↑ | ? | ? | DC | FC | 300–1000 | −80 °C | [121] | ||
| PAF | PMN, systemic | PMN recruitment ↓, PMN-EC interaction ↓ | ? | ? | DC | FC | ? | ? | [97] | |
| PLT | Platelet activation | ? | ? | DC + F | FC | <1000 | −80 °C | [117] | ||
| IL-8 | NK | Anti-inflammatory | 95% or 99% (FC) | ? | DC | FC | 200–1000 | ? | [96] | |
| CXCL-2 | Vascular permeability | Maintaining the integrity of the microvascular barrier | ? | ? | no isolation | FC | ? | ? | [109] | |
| Pathogens | M. tuberculosis | HMDM | Bacterial killing ↓ | ?, but nuclear morphology analyzed with light microscopy | 95% (Trypan Blue) | DC | FC, EM | 50–300 | −80 °C | [85] |
| M. tuberculosis | HMDM | Pro-inflammatory, ROS production ↑, autophagy ↑, bacterial killing ↑ | >98% | >98% | DC | FC, NTA, EM | 100–700 | 4 °C <24h | [105] | |
| Ops. A. fumigatus | A. fumigatus | Antifungal effect | >95% | >98% | DC + F | FC, NTA, EM | ? | −80 °C or fresh | [122] | |
| P. aeruginosa | P. aeruginosa | Antibacterial effect | ? | ? | no isolation | none | ? | ? | [123] | |
| Ops. S. aureus | Ops. and non-ops. S. aureus, E. coli | Binding to bacteria, antibacterial effect | >95% | 80–85% (EB) | DC + F | FC, DLS, EM | 100, 200–800 | ? | [124] | |
| Ops. zymosan | S. aureus, E. coli | Antibacterial effect | >95% | ? | DC + F | FC | ? | ? | [125] | |
| PMN, HUVEC, plasma | Pro-inflammatory, PMN ROS production ↑ | >95% | ? | DC + F | FC, DLS, NTA, EM | 80–1000 | none | [86] | ||
| Pharmacological stimuli | PMA | MoDC | Anti-inflammatory, Th2 polarization | ? | ? | DC | FC, DLS | 50–600 | −80 °C | [126] |
| HMDM | Pro-inflammatory | >98% | >98% | DC | FC, NTA, EM | 100–300 | 4 °C <24 h | [105] | ||
| IEC | Inhibition of epithelial wound healing via MPO delivery | Human: ?, Mouse: 85–90% | ? | DC | FC, EM | 600 | ? | [111] | ||
| S. aureus | Binding to opsonized bacteria | >98% | >99% before and after stimulation (Trypan Blue) | DC + F | EM | ? | ? | [110] | ||
| Plasma, NET | Pro-coagulant (intrinsic), NET-binding | ? | ? | no isolation | FC, EM | ? | ? | [127] | ||
| PLT | Platelet activation | ? | ? | DC + F | FC | <1000 | −80 °C | [117] | ||
| PMA + A23187 | P1EC, artery rings | Pro-inflammatory, oxidative stress ↑, TF expression ↑ | n/a (splenocytes) | ? | DC | TRPS | 200–500 | ? | [114] | |
| A23187 | HUVEC | MPO-mediated cytotoxicity | >90% (FC CD66b) | ? | DC | FC, EM | <1000 | 4 °C | [128] | |
| Ionomycin | S. aureus | Binding to opsonized bacteria | >98% | >99% before and after stimulation (Trypan Blue) | DC + F | EM | ? | ? | [110] | |
| L-NAME | PMN | Pro-migratory | >97% (hemocytometer) | >95% (Trypan Blue) | DC | FC, EM | ? | ? | [129] | |
| Pathophysiological environment | Sepsis | THP-1 | Pro-inflammatory, pro-phagocytic | n/a (peritoneal and BAL EVs) | n/a (peritoneal and BAL EVs) | C | FC | 300–1100 | ? | [130] |
| HUVEC, Plasma, ops. S. aureus | Pro-inflammatory, pro-coagulant, binding to ops. bacteria | >95% (FC) | ? | DC | FC, NTA | 50–800 | ? | [131] | ||
| Ops. and non-ops. S. aureus, E. coli | Binding to bacteria | n/a (plasma EVs) | n/a (plasma EVs) | DC + F | FC | ? | ? | [124] | ||
| Sepsis + LL37 | E. coli | Antibacterial effect | 90% (Giemsa) | ? | DC | FC | 500–1000 | −80 °C | [132] | |
| Sepsis + thioglycolate i.p. | Peritoneal macrophages, systemic | Pro- and anti-inflammatory, bacterial clearance ↓, mortality ↑ | n/a (peritoneal EVs) | n/a (peritoneal EVs) | DC | FC | ? | ? | [133] | |
| Cystic fibrosis/primary ciliary dyskinesia | Airways | Pro-inflammatory | n/a (sputum EVs) | n/a (sputum EVs) | DC | FC | ? | 4 °C | [134] | |
| Pancreatitis | Pancreas acinar cells, systemic | Pro-inflammatory, tissue injury ↑ | n/a (pancreatic EVs) | n/a (pancreatic EVs) | DC | EM | ? | n/a (pancreatic EVs) | [135] | |
| ANCA vasculitis | none | Pro-coagulant (extrinsic) | ? | ? | DC | FC | ? | ? | [136] | |
| TNFα + ANCA | HUVEC | Pro-inflammatory, pro-coagulant, ROS production ↑ | ? | ? | DC | FC | ? | Frozen (no temp. data) | [137] | |
| Rheumatoid arthritis + TNFα | HDMD, joints, macrophage-FLS co-culture system | Anti-inflammatory | ? | ? | DC | FC, NTA | 70–400 | ? | [118] | |
| MSU i.p. | Peritoneal macrophages | Anti-inflammatory | n/a (peritoneal EVs) | n/a (peritoneal EVs) | DC | FC, EM | 50–500 | ? | [95] | |
| Gout | Peritoneal macrophages | Anti-inflammatory | n/a (synovial EVs) | n/a (synovial EVs) | DC | FC, EM | 50 | ? | [95] | |
| acLDL | Human coronary endothelial cells | Pro-inflammatory, pro-migratory | ? | ? | DC + dialysis | FC, TRPS—human, NTA—mouse | 280 (human), 165 (mouse) | ? | [100] | |
| Hyperglycemia | None | Release of EVs carrying IL-1β | ? | >78% after EV isolation (Trypan Blue) | no isolation | FC | 300–1000 | ? | [138] |
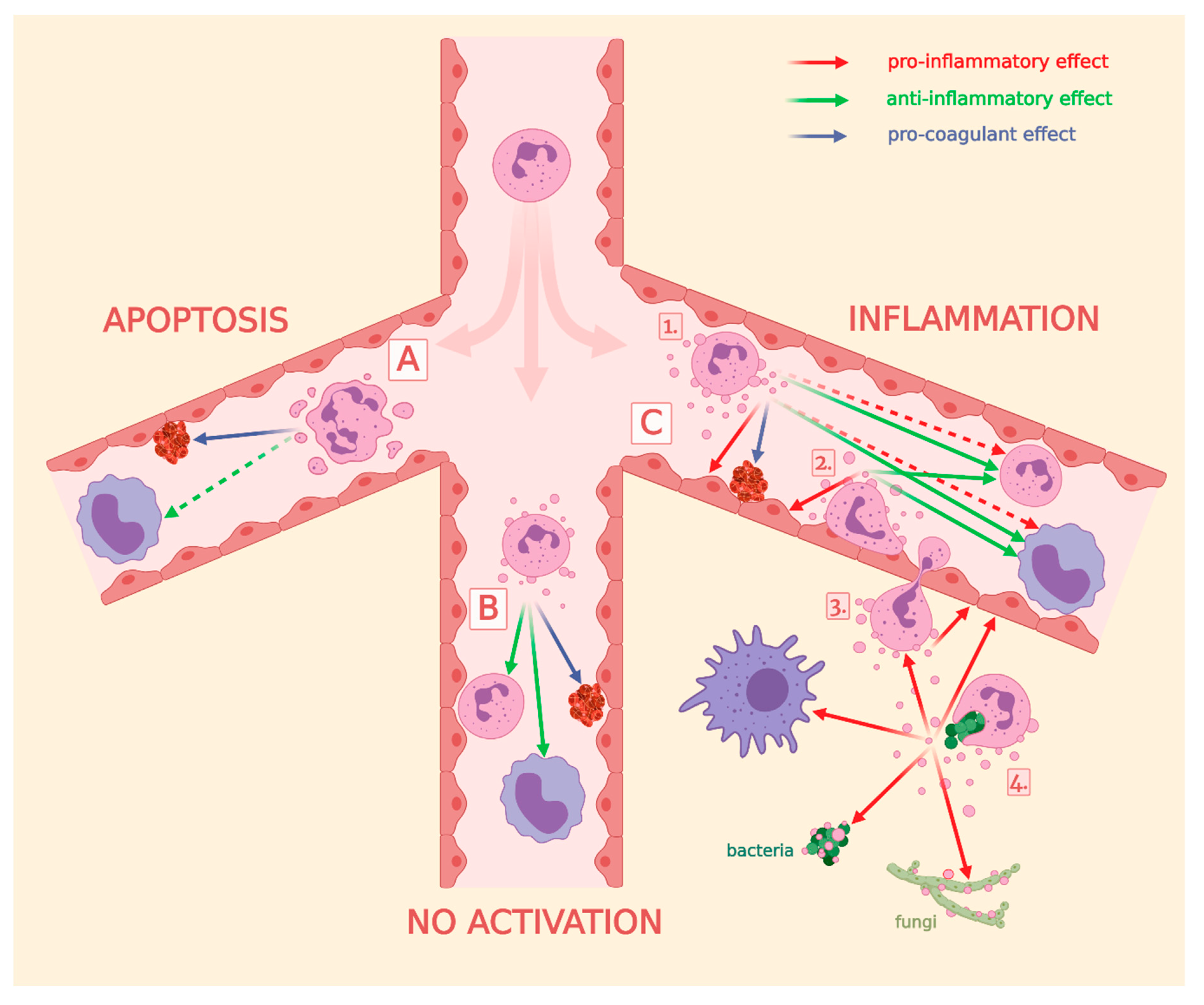
| Group (Figure 4) | Effect | PMN-EV Induction Stimulus | Target | References | |
|---|---|---|---|---|---|
| A | No effect | apoptosis | PMN | [86] | |
| [89] | |||||
| Monocyte/macrophage | [87] | ||||
| [91] | |||||
| T-cell | [90] | ||||
| Anti-inflammatory | Monocyte/macrophage | [88] | |||
| Pro-coagulant | Coagulation | [86] | |||
| B | Anti-inflammatory | spontaneous release | Monocyte/macrophage | [85] | |
| PMN | [86] | ||||
| Pro-coagulant | Coagulation | [86] | |||
| C | 1 | Anti-inflammatory | fMLP | Monocyte/macrophage | [92] |
| [95] | |||||
| [93] | |||||
| [104] | |||||
| [94] | |||||
| C5a | [94] | ||||
| TNFα | [118] | ||||
| fMLP, IL-8 | NK | [96] | |||
| PAF | PMN | [97] | |||
| Pro-inflammatory | fMLP | Endothelium/HUVEC | [99] | ||
| [98] | |||||
| [100] | |||||
| [101] | |||||
| LPS | [114] | ||||
| TNFα | [137] | ||||
| TNFa, GM-CSF, IFN-γ | [102] | ||||
| fMLP + GM-CSF | PMN | [112] | |||
| C5a | [121] | ||||
| fMLP+LPS | Phagocytes | [113] | |||
| Pro-coagulant | fMLP | Coagulation | [98] | ||
| TNFα + ANCA | [137] | ||||
| LPS | [117] | ||||
| [116] | |||||
| 2 | Anti-inflammatory | fMLP | Monocyte/macrophage | [97] | |
| Pro-inflammatory | Phagocytes | [106] | |||
| Endothelium/HUVEC | [104] | ||||
| [103] | |||||
| 3 | Pro-inflammatory | fMLP | Endothelium/HUVEC | [108] | |
| [111] | |||||
| [102] | |||||
| 4 | Pro-inflammatory | ops. zymosan | PMN | [86] | |
| Bacteria | [149] | ||||
| ops. bacteria | Bacteria | [124] | |||
| ops. fungi | Fungi | [122] | |||
| M. tuberculosis | Monocyte/macrophage | [105] | |||
| Anti-inflammatory | [85] | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolonics, F.; Szeifert, V.; Timár, C.I.; Ligeti, E.; Lőrincz, Á.M. The Functional Heterogeneity of Neutrophil-Derived Extracellular Vesicles Reflects the Status of the Parent Cell. Cells 2020, 9, 2718. https://doi.org/10.3390/cells9122718
Kolonics F, Szeifert V, Timár CI, Ligeti E, Lőrincz ÁM. The Functional Heterogeneity of Neutrophil-Derived Extracellular Vesicles Reflects the Status of the Parent Cell. Cells. 2020; 9(12):2718. https://doi.org/10.3390/cells9122718
Chicago/Turabian StyleKolonics, Ferenc, Viktória Szeifert, Csaba I. Timár, Erzsébet Ligeti, and Ákos M. Lőrincz. 2020. "The Functional Heterogeneity of Neutrophil-Derived Extracellular Vesicles Reflects the Status of the Parent Cell" Cells 9, no. 12: 2718. https://doi.org/10.3390/cells9122718
APA StyleKolonics, F., Szeifert, V., Timár, C. I., Ligeti, E., & Lőrincz, Á. M. (2020). The Functional Heterogeneity of Neutrophil-Derived Extracellular Vesicles Reflects the Status of the Parent Cell. Cells, 9(12), 2718. https://doi.org/10.3390/cells9122718





