Perinatal Brain Injury and Inflammation: Lessons from Experimental Murine Models
Abstract
1. Neonatal Encephalopathy and Neonatal Seizures
1.1. Aetiology
Classification of Neonatal Seizures in Murine Models of Neonatal Encephalopathy
1.2. Current Treatments for Neonatal Encephalopathy
Challenges of Current Drug Treatments in the Clinic
- Preclinical models have shown that ACDs can induce neurotoxicity and neuronal apoptosis in the immature brain [18,19,20]. With similar results to those observed in a mouse model of hypoxia, PhB itself induces neuronal damage in neonates; and when given as a treatment for hypoxia-induced seizures, it exacerbates the damage [20].
- Current ACDs affect neurogenesis, synaptogenesis and synaptic plasticity, resulting in unwanted neuropsychiatric outcomes [20,21,22]. Indeed, P7 mice pups receiving PhB presented anxiety-like behaviour and detrimental hippocampal function in adulthood [20]. Furthermore, PhB given as a treatment for neonatal seizures does not improve the lasting anxiety-like behaviour and hippocampal-dependent memory of the hypoxic mice [20]. Supporting the pre-clinical animal model, infants treated with PhB show a strong decrease in cognitive and motor scores at 24 months of age compared to untreated infants [23].
2. Experimental Animal Models of Hypoxia and Hypoxia–Ischemia
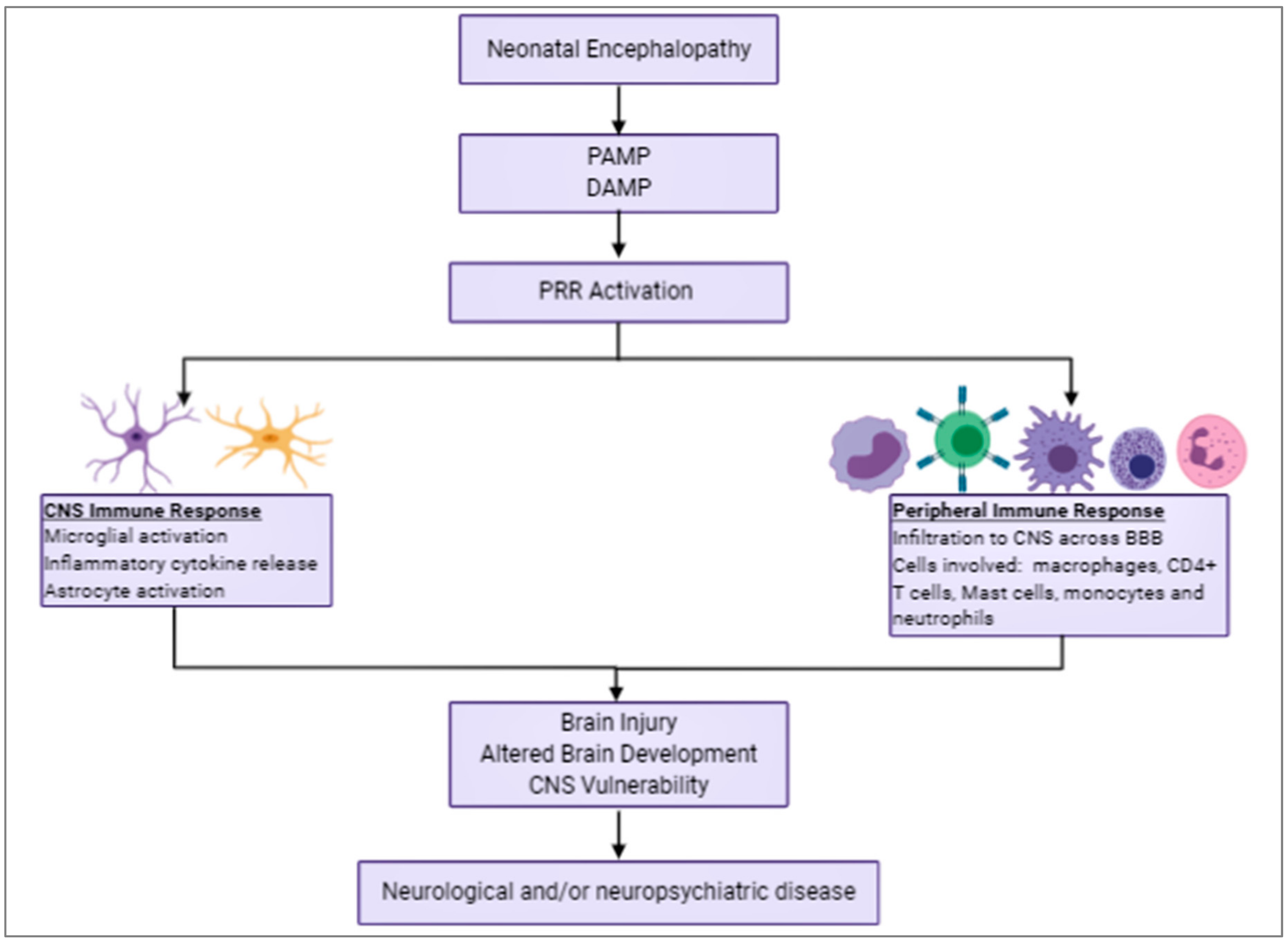
3. Inflammation in Neonatal Encephalopathy
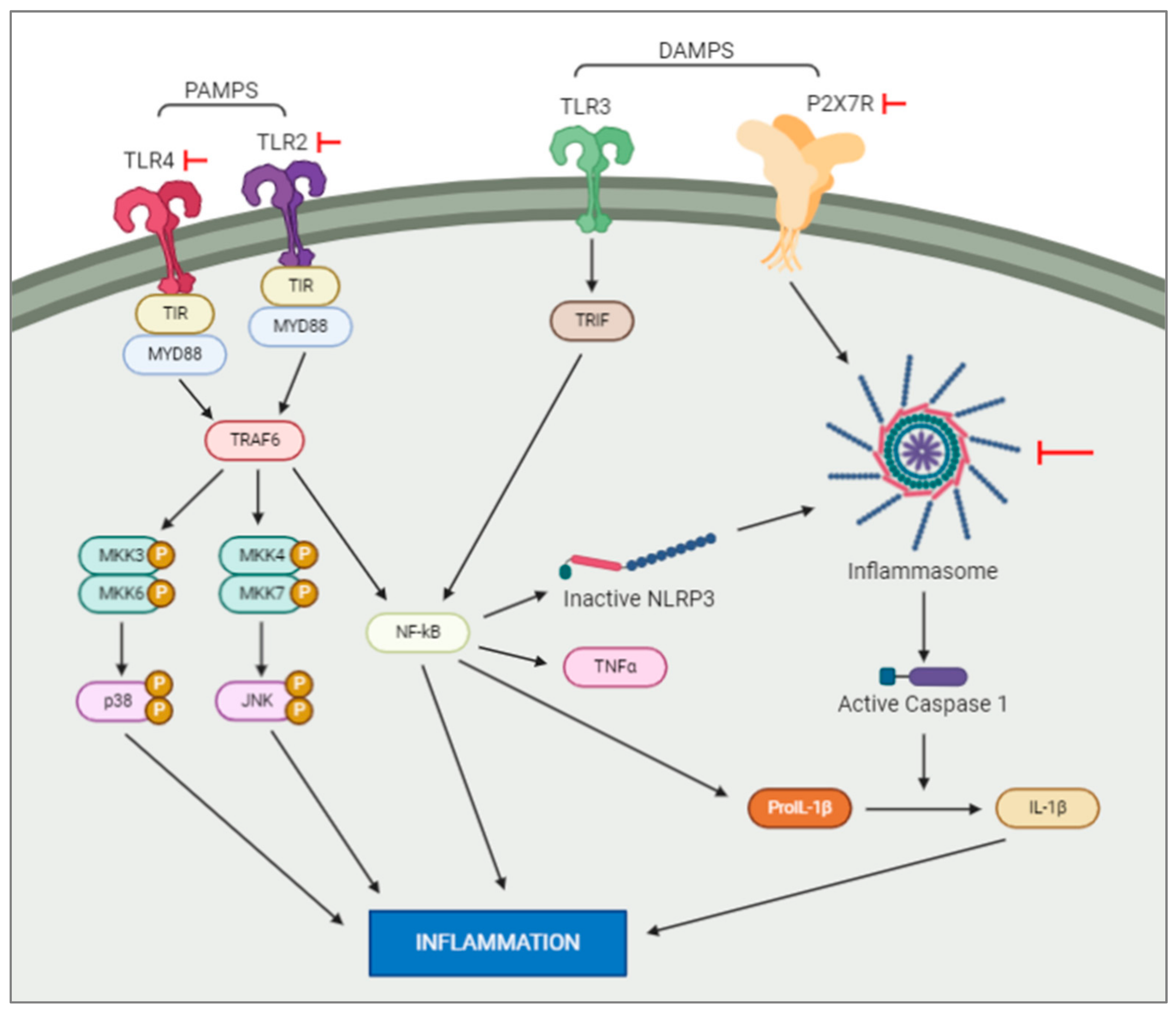
3.1. Pathogen-Associated Molecular Patterns (PAMPS) and Damage-Associated Molecular Patterns (DAMPS)
3.2. Toll-Like Receptors in Neonatal Encephalopathy
3.3. Purinergic Signalling Activation after Neonatal Encephalopathy
3.4. Cytokines and Chemokines in Neonatal Encephalopathy
3.4.1. Interleukin 1β, IL1β
3.4.2. Interleukin-6, IL6
3.4.3. Tumour Necrosis Factor, TNFα
4. Contributions of Central and Peripheral Cells to Neonatal Encephalopathy
4.1. Microglia
4.2. Astrocytes
4.3. Oligodendrocytes
4.4. Peripheral Immune Cells
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Aslam, S.; Strickland, T.; Molloy, E.J. Neonatal encephalopathy: Need for recognition of multiple etiologies for optimal management. Front. Pediatr. 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Yıldız, E.P.; Tatlı, B.; Ekici, B.; Eraslan, E.; Aydınlı, N.; Çalışkan, M.; Ozmen, M. Evaluation of etiologic and prognostic factors in neonatal convulsions. Pediatric Neurol. 2012, 47, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Pellegrin, S.; Munoz, F.M.; Padula, M.; Heath, P.T.; Meller, L.; Top, K.A.; Wilmshurst, J.; Wiznitzer, M.; Das, M.K.; Hahn, C.D.; et al. Neonatal seizures: Case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine 2019, 37, 7596–7609. [Google Scholar] [PubMed]
- Vasudevan, C.; Levene, M. Epidemiology and aetiology of neonatal seizures. Semin. Fetal Neonatal Med. 2013, 18, 185–191. [Google Scholar] [CrossRef]
- Mwaniki, M.K.; Mathenge, A.; Gwer, S.; Mturi, N.; Bauni, E.; Newton, C.R.; Berkley, J.A.; Idro, R. Neonatal seizures in a rural Kenyan District Hospital: Aetiology, incidence and outcome of hospitalization. BMC Med. 2010, 8, 16. [Google Scholar] [CrossRef]
- Boylan, G.B.; Kharoshankaya, L.; Wusthoff, C.J. Seizures and hypothermia: Importance of electroencephalographic monitoring and considerations for treatment. Semin. Fetal Neonatal Med. 2020, 103–108. [Google Scholar] [CrossRef]
- Rice, J.E., 3rd; Vannucci, R.C.; Brierley, J.B. The influence of immaturity on hypoxic-ischemic brain damage in the rat. Ann. Neurol. 1981, 9, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Morin, L.; Enderlin, J.; Leger, P.-L.; Perrotte, G.; Bonnin, P.; Dupuis, N.; Baud, O.; Charriaut-Marlangue, C.; Auvin, S. Different response to antiepileptic drugs according to the type of epileptic events in a neonatal ischemia-reperfusion model. Neurobiol. Dis. 2017, 99, 145–153. [Google Scholar] [CrossRef]
- Rodriguez-Alvarez, N.; Jimenez-Mateos, E.M.; Dunleavy, M.; Waddington, J.L.; Boylan, G.B.; Henshall, D.C. Effects of hypoxia-induced neonatal seizures on acute hippocampal injury and later-life seizure susceptibility and anxiety-related behavior in mice. Neurobiol. Dis. 2015, 83, 100–114. [Google Scholar] [CrossRef]
- Rodriguez-Alvarez, N.; Jimenez-Mateos, E.M.; Engel, T.; Quinlan, S.; Reschke, C.R.; Conroy, R.M.; Bhattacharya, A.; Boylan, G.B.; Henshall, D.C. Effects of P2X7 receptor antagonists on hypoxia-induced neonatal seizures in mice. Neuropharmacology 2017, 116, 351–363. [Google Scholar] [CrossRef]
- Quinlan, S.; Merino-Serrais, P.; Di Grande, A.; Dussmann, H.; Prehn, J.H.M.; Ní Chonghaile, T.; Henshall, D.C.; Jimenez-Mateos, E.M. The anti-inflammatory compound candesartan cilexetil improves neurological outcomes in a mouse model of neonatal hypoxia. Front. Immunol. 2019, 10, 1752. [Google Scholar] [CrossRef] [PubMed]
- Vezzani, A.; Conti, M.; De Luigi, A.; Ravizza, T.; Moneta, D.; Marchesi, F.; De Simoni, M.G. Interleukin-1β immunoreactivity and microglia are enhanced in the rat hippocampus by focal Kainate application: Functional evidence for enhancement of electrographic seizures. J. Neurosci. 1999, 19, 5054–5065. [Google Scholar] [CrossRef] [PubMed]
- Vezzani, A.; Moneta, D.; Conti, M.; Richichi, C.; Ravizza, T.; Luigi, A.D.; De Simoni, M.G.; Sperk, G.; Andell-Jonsson, S.; Lundkvist, J.; et al. Powerful anticonvulsant action of IL-1 receptor antagonist on intracerebral injection and astrocytic overexpression in mice. Proc. Natl. Acad. Sci. USA 2000, 97, 11534–11539. [Google Scholar] [CrossRef] [PubMed]
- Stellwagen, D.; Beattie, E.C.; Seo, J.Y.; Malenka, R.C. Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J. Neurosci. 2005, 25, 3219–3228. [Google Scholar] [CrossRef]
- Spagnoli, C.; Seri, S.; Pavlidis, E.; Mazzotta, S.; Pelosi, A.; Pisani, F. Phenobarbital for neonatal seizures: Response rate and predictors of refractoriness. Neuropediatrics 2016, 47, 318–326. [Google Scholar] [CrossRef]
- Donovan, M.D.; Griffin, B.T.; Kharoshankaya, L.; Cryan, J.F.; Boylan, G.B. Pharmacotherapy for neonatal seizures: Current knowledge and future perspectives. Drugs 2016, 76, 647–661. [Google Scholar] [CrossRef]
- Al-Muhtasib, N.; Sepulveda-Rodriguez, A.; Vicini, S.; Forcelli, P.A. Neonatal phenobarbital exposure disrupts GABAergic synaptic maturation in rat CA1 neurons. Epilepsia 2018, 59, 333–344. [Google Scholar] [CrossRef]
- Forcelli, P.A.; Kim, J.; Kondratyev, A.; Gale, K. Pattern of antiepileptic drug-induced cell death in limbic regions of the neonatal rat brain. Epilepsia 2011, 52, e207–e211. [Google Scholar] [CrossRef]
- Torolira, D.; Suchomelova, L.; Wasterlain, C.G.; Niquet, J. Phenobarbital and midazolam increase neonatal seizure-associated neuronal injury. Ann. Neurol. 2017, 82, 115–120. [Google Scholar] [CrossRef]
- Quinlan, S.M.M.; Rodriguez-Alvarez, N.; Molloy, E.J.; Madden, S.F.; Boylan, G.B.; Henshall, D.C.; Jimenez-Mateos, E.M. Complex spectrum of phenobarbital effects in a mouse model of neonatal hypoxia-induced seizures. Sci. Rep. 2018, 8, 9986. [Google Scholar] [CrossRef]
- Bhardwaj, S.K.; Forcelli, P.A.; Palchik, G.; Gale, K.; Srivastava, L.K.; Kondratyev, A. Neonatal exposure to phenobarbital potentiates schizophrenia-like behavioral outcomes in the rat. Neuropharmacology 2012, 62, 2337–2345. [Google Scholar] [CrossRef] [PubMed]
- Pisani, F.; Spagnoli, C. Neonatal seizures: A review of outcomes and outcome predictors. Neuropediatrics 2016, 47, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Maitre, N.L.; Smolinsky, C.; Slaughter, J.C.; Stark, A.R. Adverse neurodevelopmental outcomes after exposure to phenobarbital and levetiracetam for the treatment of neonatal seizures. J. Perinatol. Off. Calif. Perinat. Assoc. 2013, 33, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Pressler, R.M.; Boylan, G.B.; Marlow, N.; Blennow, M.; Chiron, C.; Cross, J.H.; de Vries, L.S.; Hallberg, B.; Hellstrom-Westas, L.; Jullien, V.; et al. Bumetanide for the treatment of seizures in newborn babies with hypoxic ischaemic encephalopathy (NEMO): An open-label, dose finding, and feasibility phase 1/2 trial. Lancet Neurol. 2015, 14, 469–477. [Google Scholar] [CrossRef]
- Shimomura, C.; Ohta, H. Behavioral abnormalities and seizure susceptibility in rat after neonatal anoxia. Brain Dev. 1988, 10, 160–163. [Google Scholar] [CrossRef]
- Ujházy, E.; Schmidtová, M.; Dubovický, M.; Navarova, J.; Brucknerová, I.; Mach, M. Neurobehavioural changes in rats after neonatal anoxia: Effect of antioxidant stobadine pretreatment. Neuro. Endocrinol. Lett. 2006, 27, 82–85. [Google Scholar]
- Samaiya, P.K.; Krishnamurthy, S. Characterization of mitochondrial bioenergetics in neonatal anoxic model of rats. J. Bioenerg. Biomembr. 2015, 47, 217–222. [Google Scholar] [CrossRef]
- Coq, J.O.; Strata, F.; Russier, M.; Safadi, F.F.; Merzenich, M.M.; Byl, N.N.; Barbe, M.F. Impact of neonatal asphyxia and hind limb immobilization on musculoskeletal tissues and S1 map organization: Implications for cerebral palsy. Exp. Neurol. 2008, 210, 95–108. [Google Scholar] [CrossRef]
- Rastogi, R.; Prichard, J.; Lowden, J. Elevation of phosphorus levels in serum and decreased brain content of gangliosides in rats following neonatal asphyxia. Pediatr. Res. 1968, 2, 125–130. [Google Scholar] [CrossRef]
- Buwalda, B.; Nyakas, C.; Jan Vosselman, H.; Luiten, P.G.M. Effects of early postnatal anoxia on adult learning and emotion in rats. Behav. Brain Res. 1995, 67, 85–90. [Google Scholar] [CrossRef][Green Version]
- Rogalska, J.; Caputa, M.; Wentowska, K.; Nowakowska, A. Stress-induced behaviour in juvenile rats: Effects of neonatal asphyxia, body temperature and chelation of iron. Behav. Brain Res. 2004, 154, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Casolini, P.; Zuena, A.R.; Cinque, C.; Matteucci, P.; Alema’, G.S.; Adriani, W.; Carpinelli, G.; Santoro, F.; Alleva, E.; Bosco, P.; et al. Sub-neurotoxic neonatal anoxia induces subtle behavioural changes and specific abnormalities in brain group-I metabotropic glutamate receptors in rats. J. Neurochem. 2005, 95, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Dell’Anna, M.E.; Calzolari, S.; Molinari, M.; Iuvone, L.; Calimici, R. Neonatal anoxia induces transitory hyperactivity, permanent spatial memory deficits and CA1 cell density reduction in developing rats. Behav. Brain Res. 1991, 45, 125–134. [Google Scholar] [CrossRef]
- Speiser, Z.; Uziel, J.; Defrin-Assa, R.; Gitter, S.; Urca, G. Different behavioral deficits are induced by anoxia/hypoxia in neonatal and senescent rats: Blockade by MK-801. Behav. Brain Res. 1991, 42, 181–186. [Google Scholar] [CrossRef]
- Iuvone, L.; Concetta Geloso, M.; Dell’Anna, E. Changes in open field behavior, spatial memory, and hippocampal parvalbumin immunoreactivity following enrichment in rats exposed to neonatal anoxia. Exp. Neurol. 1996, 139, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Pacary, E.; Freret, T.; Divoux, D.; Petit, E.; Schumann-Bard, P.; Bernaudin, M. Effect of hypoxic preconditioning on brain genomic response before and following ischemia in the adult mouse: Identification of potential neuroprotective candidates for stroke. Neurobiol. Dis. 2006, 21, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Rogalska, J.; Danielisova, V.; Caputa, M. Effect of neonatal body temperature on postanoxic, potentially neurotoxic iron accumulation in the rat brain. Neurosci. Lett. 2006, 393, 249–254. [Google Scholar] [CrossRef]
- Takada, S.; Haemmerle, C.D.S.; Motta-Teixeira, L.; Machado-Nils, A.; Lee, V.; Takase, L.; Cruz-Rizzolo, R.; Kihara, A.; Xavier, G.; Watanabe, I.-S.; et al. Neonatal anoxia in rats: Hippocampal cellular and subcellular changes related to cell death and spatial memory. Neuroscience 2015, 284, 247–259. [Google Scholar] [CrossRef]
- Takada, S.; Motta-Teixeira, L.C.; Machado-Nils, A.V.; Lee, V.Y.; Sampaio, C.A.; Polli, R.S.; Malheiros, J.M.; Takase, L.F.; Kihara, A.H.; Covolan, L.; et al. Impact of neonatal anoxia on adult rat hippocampal volume, neurogenesis and behavior. Behav. Brain Res. 2016, 296, 331–338. [Google Scholar] [CrossRef]
- Speiser, Z.; Katzir, O.; Rehavi, M.; Zabarski, T.; Cohen, S. Sparing by rasagiline (TVP-1012) of cholinergic functions and behavior in the postnatal anoxia rat. Pharmacol. Biochem. Behav. 1998, 60, 387–393. [Google Scholar] [CrossRef]
- Wasterlain, C.G. Does anoxemia play a role in the effects of neonatal seizures on brain growth? An experimental study in the rat. Eur. Neurol. 1979, 18, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Blaise, S.A.; Nédélec, E.; Alberto, J.M.; Schroeder, H.; Audonnet, S.; Bossenmeyer-Pourié, C.; Guéant, J.L.; Daval, J.L. Short hypoxia could attenuate the adverse effects of hyperhomocysteinemia on the developing rat brain by inducing neurogenesis. Exp. Neurol. 2009, 216, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.; Mozet, C.; Martin, H.; Welt, K.; Engel, C.; Fitzl, G. The effect of Ginkgo biloba extract (EGb 761) on parameters of oxidative stress in different regions of aging rat brains after acute hypoxia. Aging Clin. Exp. Res. 2011, 23, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Paulose, C.S.; Chathu, F.; Khan, S.R.; Krishnakumar, A. Neuroprotective role of Bacopa monnieri extract in epilepsy and effect of glucose supplementation during hypoxia: Glutamate receptor gene expression. Neurochem. Res. 2008, 33, 1663–1671. [Google Scholar] [CrossRef] [PubMed]
- Anju, T.R.; Abraham, P.M.; Antony, S.; Paulose, C.S. Alterations in cortical GABAB receptors in neonatal rats exposed to hypoxic stress: Role of glucose, oxygen, and epinephrine resuscitation. Mol. Cell Biochem. 2010, 343, 1–11. [Google Scholar] [CrossRef]
- Raveendran, A.T.; Skaria, P.C. Learning and cognitive deficits in hypoxic neonatal rats intensified by BAX mediated apoptosis: Protective role of glucose, oxygen, and epinephrine. Int. J. Neurosci. 2013, 123, 80–88. [Google Scholar] [CrossRef]
- Jensen, F.E.; Alvarado, S.; Firkusny, I.R.; Geary, C. NBQX blocks the acute and late epileptogenic effects of perinatal hypoxia. Epilepsia 1995, 36, 966–972. [Google Scholar] [CrossRef]
- Wang, C.T.; Lin, H.J.; Cheng, B.C.; Lin, M.T.; Chang, C.P. Attenuating systemic inflammatory markers in simulated high-altitude exposure by heat shock protein 70-mediated hypobaric hypoxia preconditioning in rats. J. Formos. Med. Assoc. 2015, 114, 328–338. [Google Scholar] [CrossRef][Green Version]
- Applegate, C.D.; Jensen, F.; Burchfiel, J.L.; Lombroso, C. The effects of neonatal hypoxia on kindled seizure development and electroconvulsive shock profiles. Epilepsia 1996, 37, 723–727. [Google Scholar] [CrossRef]
- Mikati, M.A.; Zeinieh, M.P.; Kurdi, R.M.; Harb, S.A.; El Hokayem, J.A.; Daderian, R.H.; Shamseddine, A.; Obeid, M.; Bitar, F.F.; El Sabban, M. Long-term effects of acute and of chronic hypoxia on behavior and on hippocampal histology in the developing brain. Brain Res. Dev. Brain Res. 2005, 157, 98–102. [Google Scholar] [CrossRef]
- Sampath, D.; Shmueli, D.; White, A.M.; Raol, Y.H. Flupirtine effectively prevents development of acute neonatal seizures in an animal model of global hypoxia. Neurosci. Lett. 2015, 607, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Mikati, M.A.; Hokayem, J.A.E.; Sabban, M.E.E. Effects of a single dose of erythropoietin on subsequent seizure susceptibility in rats exposed to acute hypoxia at P10. Epilepsia 2007, 48, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Li, J.; Li, Y.; Yang, X.; Feng, S.; Han, S.; Li, J. Downregulation of miR-181b in mouse brain following ischemic stroke induces neuroprotection against ischemic injury through targeting heat shock protein A5 and ubiquitin carboxyl-terminal hydrolase isozyme L1. J. Neurosci. Res. 2013, 91, 1349–1362. [Google Scholar] [CrossRef] [PubMed]
- Greggio, S.; Rosa, R.M.; Dolganov, A.; de Oliveira, I.M.; Menegat, F.D.; Henriques, J.A.; DaCosta, J.C. NAP prevents hippocampal oxidative damage in neonatal rats subjected to hypoxia-induced seizures. Neurobiol. Dis. 2009, 36, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.P.; Zhu, L.L.; Zhao, T.; Zhao, H.; Huang, X.; Ma, X.; Wang, H.; Fan, M. Characteristics of neural stem cells expanded in lowered oxygen and the potential role of hypoxia-inducible factor-1Alpha. Neurosignals 2006, 15, 259–265. [Google Scholar] [CrossRef]
- Aujla, P.K.; Fetell, M.R.; Jensen, F.E. Talampanel suppresses the acute and chronic effects of seizures in a rodent neonatal seizure model. Epilepsia 2009, 50, 694–701. [Google Scholar] [CrossRef]
- Rakhade, S.N.; Klein, P.M.; Huynh, T.; Hilario-Gomez, C.; Kosaras, B.; Rotenberg, A.; Jensen, F.E. Development of later life spontaneous seizures in a rodent model of hypoxia-induced neonatal seizures. Epilepsia 2011, 52, 753–765. [Google Scholar] [CrossRef]
- Sanchez, R.M.; Ribak, C.E.; Shapiro, L.A. Synaptic connections of hilar basal dendrites of dentate granule cells in a neonatal hypoxia model of epilepsy. Epilepsia 2012, 53, 98–108. [Google Scholar] [CrossRef]
- Mikhailenko, V.A.; Butkevich, I.P.; Bagaeva, T.R.; Makukhina, G.V.; Otellin, V.A. Short- and long-term influences of hypoxia during early postnatal period of development on behavioral and hormonal responses in rats. Neurosci. Lett. 2009, 464, 214–217. [Google Scholar] [CrossRef]
- Koh, S.; Jensen, F.E. Topiramate blocks perinatal hypoxia-induced seizures in rat pups. Ann. Neurol. 2001, 50, 366–372. [Google Scholar] [CrossRef]
- Laroia, N.; McBride, L.; Baggs, R.; Guillet, R. Dextromethorphan ameliorates effects of neonatal hypoxia on brain morphology and seizure threshold in rats. Dev. Brain Res. 1997, 100, 29–34. [Google Scholar] [CrossRef]
- Rotstein, M.; Bassan, H.; Kariv, N.; Speiser, Z.; Harel, S.; Gozes, I. NAP enhances neurodevelopment of newborn apolipoprotein E-deficient mice subjected to hypoxia. J. Pharmacol. Exp. Ther. 2006, 319, 332–339. [Google Scholar] [CrossRef]
- Decker, M.J.; Hue, G.; Caudle, W.; Miller, G.; Keating, G.; Rye, D. Episodic neonatal hypoxia evokes executive dysfunction and regionally specific alterations in markers of dopamine signaling. Neuroscience 2003, 117, 417–425. [Google Scholar] [CrossRef]
- Mortola, J.P.; Naso, L. Thermogenesis in newborn rats after prenatal or postnatal hypoxia. J. Appl. Physiol. 1998, 85, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Decker, M.J.; Jones, K.A.; Solomon, I.G.; Keating, G.L.; Rye, D.B. Reduced extracellular dopamine and increased responsiveness to novelty: Neurochemical and behavioral sequelae of intermittent hypoxia. Sleep 2005, 28, 169–176. [Google Scholar] [CrossRef]
- Caputa, M.; Rogalska, J.; Wentowska, K.; Nowakowska, A. Perinatal asphyxia, hyperthermia and hyperferremia as factors inducing behavioural disturbances in adulthood: A rat model. Behav. Brain Res. 2005, 163, 246–256. [Google Scholar] [CrossRef]
- Zanelli, S.; Goodkin, H.P.; Kowalski, S.; Kapur, J. Impact of transient acute hypoxia on the developing mouse EEG. Neurobiol. Dis. 2014, 68, 37–46. [Google Scholar] [CrossRef][Green Version]
- Wang, K.C.; Fan, L.W.; Kaizaki, A.; Pang, Y.; Cai, Z.; Tien, L.T. Neonatal lipopolysaccharide exposure induces long-lasting learning impairment, less anxiety-like response and hippocampal injury in adult rats. Neuroscience 2013, 234, 146–157. [Google Scholar] [CrossRef]
- Hagberg, H.; Mallard, C.; Ferriero, D.M.; Vannucci, S.J.; Levison, S.W.; Vexler, Z.S.; Gressens, P. The role of inflammation in perinatal brain injury. Nat. Rev. Neurol. 2015, 11, 192–208. [Google Scholar] [CrossRef]
- Mallard, C.; Tremblay, M.E.; Vexler, Z.S. Microglia and Neonatal Brain Injury. Neuroscience 2019, 1, 68–76. [Google Scholar] [CrossRef]
- Takemiya, T.; Fumizawa, K.; Yamagata, K.; Iwakura, Y.; Kawakami, M. Brain Interleukin-1 facilitates learning of a water maze spatial memory task in young mice. Front. Behav. Neurosci. 2017, 11, 202. [Google Scholar] [CrossRef] [PubMed]
- Al Mamun, A.; Yu, H.; Romana, S.; Liu, F. Inflammatory responses are sex specific in chronic hypoxic–ischemic encephalopathy. Cell Transplant. 2018, 1328–1339. [Google Scholar] [CrossRef] [PubMed]
- Manuck, T.A.; Rice, M.M.; Bailit, J.L.; Grobman, W.A.; Reddy, U.M.; Wapner, R.J.; Thorp, J.M.; Caritis, S.N.; Prasad, M.; Tita, A.T.N. Preterm neonatal morbidity and mortality by gestational age: A contemporary cohort. Am. J. Obstet. Gynecol. 2016, 215, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.W.; Walsh, W.F. Hypoxic-ischemic encephalopathy in preterm infants. J. Neonatal. Perinatal. Med. 2010, 3, 277–284. [Google Scholar] [CrossRef]
- Chalak, L.F.; Rollins, N.; Morriss, M.C.; Brion, L.P.; Heyne, R.; Sanchez, P.J. Perinatal acidosis and hypoxic-ischemic encephalopathy in preterm infants of 33 to 35 weeks’ gestation. J. Pediatr. 2012, 160, 388–394. [Google Scholar] [CrossRef]
- Garfinkle, J.; Wintermark, P.; Shevell, M.I.; Oskoui, M. Children born at 32 to 35 weeks with birth asphyxia and later cerebral palsy are different from those born after 35 weeks. J. Perinatol. 2017, 37, 963–968. [Google Scholar] [CrossRef]
- Woodward, L.J.; Anderson, P.J.; Austin, N.C.; Howard, K.; Inder, T.E. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N. Engl. J. Med. 2006, 355, 685–694. [Google Scholar] [CrossRef]
- Batalle, D.; Eixarch, E.; Figueras, F.; Muoz-Moreno, E.; Bargallo, N.; Illa, M.; Acosta-Rojas, R.; Amat-Roldan, I.; Gratacos, E. Altered smallworld topology of structural brain networks in infants with intrauterine growth restriction and its association with later neurodevelopmental outcome. NeuroImage 2012, 60, 1352–1366. [Google Scholar] [CrossRef]
- Mullen, K.M.; Vohr, B.R.; Katz, K.H.; Schneider, K.C.; Lacadie, C.; Hampson, M.; Makuch, R.W.; Reiss, A.L.; Constable, R.T.; Ment, L.R. Preterm birth results in alterations in neural connectivity at age 16 years. NeuroImage 2011, 54, 2563–2570. [Google Scholar] [CrossRef]
- Buser, J.R.; Maire, J.; Riddle, A.; Gong, X.; Nguyen, T.; Nelson, K.; Luo, N.L.; Ren, J.; Struve, J.; Sherman, L.S. Arrested preoligodendrocyte maturation contributes to myelination failure in premature infants. Ann. Neurol. 2012, 71, 93–109. [Google Scholar] [CrossRef]
- Bartha, A.I.; Foster-Barber, A.; Miller, S.P.; Vigneron, D.B.; Glidden, D.V.; Barkovich, A.J.; Ferriero, D.M. Neonatal encephalopathy: Association of cytokines with MR spectroscopy and outcome. Pediatr. Res. 2004, 56, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Zindel, J.; Kubes, P. DAMPs, PAMPs, and LAMPs in immunity and sterile inflammation. Annu. Rev. Pathol. Mech. Dis. 2020, 15, 493–518. [Google Scholar] [CrossRef] [PubMed]
- Serdar, M.; Kempe, K.; Rizazad, M.; Herz, J.; Bendix, I.; Felderhoff-Müser, U.; Sabir, H. Early pro-inflammatory microglia activation after inflammation-sensitized hypoxic-ischemic brain injury in neonatal rats. Front. Cell Neurosci. 2019, 13, 237. [Google Scholar] [CrossRef] [PubMed]
- Lalancette-Hébert, M.; Faustino, J.; Sampath Thammisetty, S.; Chip, S.; Vexler, Z.S.; Kriz, J. Live imaging of the innate immune response in neonates reveals differential TLR2 dependent activation patterns in sterile inflammation and infection. Brain Behav. Immun. 2017, 65, 312–327. [Google Scholar] [CrossRef]
- Stridh, L.; Smith, P.L.; Naylor, A.S.; Wang, X.; Mallard, C. Regulation of Toll-like receptor 1 and -2 in neonatal mice brains after hypoxia-ischemia. J. Neuroinflammation 2011, 8, 45. [Google Scholar] [CrossRef]
- Mottahedin, A.; Ardalan, M.; Chumak, T.; Riebe, I.; Ek, J.; Mallard, C. Effect of neuroinflammation on synaptic organization and function in the developing brain: Implications for neurodevelopmental and neurodegenerative disorders. Front. Cell. Neurosci. 2017, 11, 190. [Google Scholar] [CrossRef]
- Tang, Z.; Cheng, S.; Sun, Y.; Zhang, Y.; Xiang, X.; Ouyang, Z.; Zhu, X.; Wang, B.; Hei, M. Early TLR4 inhibition reduces hippocampal injury at puberty in a rat model of neonatal hypoxic-ischemic brain damage via regulation of neuroimmunity and synaptic plasticity. Exp. Neurol. 2019, 321, 113039. [Google Scholar] [CrossRef]
- Burnstock, G. Purinergic signalling and disorders of the central nervous system. Nat. Rev. Drug Dis. 2008, 7, 575–590. [Google Scholar] [CrossRef]
- Burnstock, G. Physiology and pathophysiology of purinergic neurotransmission. Physiol. Rev. 2007, 87, 659–797. [Google Scholar] [CrossRef]
- Sperlagh, B.; Illes, P. P2X7 receptor: An emerging target in central nervous system diseases. Trend Pharmacol. Sci. 2014, 35, 537–547. [Google Scholar] [CrossRef]
- Rappold, P.M.; Lynd-Balta, E.; Joseph, S.A. P2X7 receptor immunoreactive profile confined to resting and activated microglia in the epileptic brain. Brain Res. 2006, 1089, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Mingam, R.; De Smedt, V.; Amedee, T.; Bluthe, R.M.; Kelley, W.K.; Dantzer, R.; Laye, S. In vitro and in vivo evidence for a role of the P2X7 receptor in the release of IL-1 beta in the murine brain. Brain Behav. Immun. 2008, 22, 234–244. [Google Scholar] [CrossRef] [PubMed]
- Monif, M.; Reid, C.A.; Powell, K.L.; Smart, M.L.; Williams, D.A. The P2X7 receptor drives microglial activation and proliferation: A trophic role for P2X7R pore. J. Neurosci. 2009, 29, 3781–3791. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, J.N.; Brust, T.B.; Lewis, R.G.; MacVicar, B.A. Activation of presynaptic P2X7-like receptors depresses mossy fiber-CA3 synaptic transmission through p38 mitogen-activated protein kinase. J. Neurosci. 2002, 22, 5938–5945. [Google Scholar] [CrossRef]
- Sperlagh, B.; Köfalvi, A.; Deuchars, J.; Atkinson, L.; Milligan, C.J.; Buckley, N.J.; Vizi, E.S. Involvement of P2X7 receptors in the regulation of neurotransmitter release in the rat hippocampus. J. Neurochem. 2002, 81, 1196–1211. [Google Scholar] [CrossRef]
- Dale, N.; Frenguelli, B.G. Release of adenosine and ATP during ischemia and epilepsy. Curr. Neuropharmacol. 2009, 7, 160–179. [Google Scholar] [CrossRef]
- Ulrich, H.; Illes, P. P2X receptors in maintenance and differentiation of neural progenitor cells. Neural. Regen. Res. 2014, 9, 2040–2041. [Google Scholar] [CrossRef]
- Illes, P.; Messemer, N.; Rubini, P. P2Y receptors in neurogenesis. WIRES Membr. Transp. Signal 2013, 2, 43–48. [Google Scholar] [CrossRef]
- Rozmer, K.; Gao, P.; Araújo, M.G.L.; Tahir Khan, M.; Liu, J.; Rong, W.; Tang, Y.; Franke, H.; Krügel, U.; Fernandes, M.J.S.; et al. Pilocarpine-Induced Status Epilepticus Increases the Sensitivity of P2X7 and P2Y1 Receptors to Nucleotides at Neural Progenitor Cells of the Juvenile Rodent Hippocampus. Cereb. Cortex 2017, 27, 3568–3585. [Google Scholar] [CrossRef]
- Mesuret, G.; Engel, T.; Hessel, E.V.; Sanz-Rodriguez, A.; Jimenez-Pacheco, A.; Miras-Portugal, M.T.; Diaz-Hernandez, M.; Henshall, D.C. P2X7 receptor inhibition interrupts the progression of seizures in immature rats and reduces hippocampal damage. CNS Neurosci. Ther. 2014, 20, 556–564. [Google Scholar] [CrossRef]
- Tsimis, M.E.; Lei, J.; Rosenzweig, J.M.; Arif, H.; Shabi, Y.; Alshehri, W.; Talbot, C.C.; Baig-Ward, K.M.; Segars, J.; Graham, E.M.; et al. P2X7 receptor blockade prevents preterm birth and perinatal brain injury in a mouse model of intrauterine inflammation. Biol. Reprod. 2017, 97, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, C.S.; Longoni Calió, M.; Mosini, A.C.; Moreira Pires, J.; da Silva Bandeira Rêgo, D.; Mello, L.E.; Figueiredo Stochero Leslie, A.T. LPS-Induced systemic neonatal inflammation: Blockage of P2X7R by BBG decreases mortality on rat pups and oxidative stress in hippocampus of adult rats. Front. Behav. Neurosci. 2019, 13, 240. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.D.; Rollins, L.G.; Perkel, J.K.; Wagner, C.L.; Katikaneni, L.P.; Bass, W.T.; Kaufman, D.A.; Horgan, M.J.; Languani, S.; Givelichian, L.; et al. Serum cytokines in a clinical trial of hypothermia for neonatal hypoxic-ischemic encephalopathy. J. Cereb. Blood Flow Metab. 2012, 32, 1888–1896. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Feng, Z.C. Increased umbilical cord plasma interleukin-1 beta levels was correlated with adverse outcomes of neonatal hypoxic-ischemic encephalopathy. J. Trop. Pediatr. 2010, 56, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Mccullough, L.D. Inflammatory responses in hypoxic ischemic encephalopathy. Acta Pharmacol. Sin. 2013, 34, 1121–1130. [Google Scholar] [CrossRef] [PubMed]
- Bona, E.; Andersson, A.L.; Blomgren, K.; Gilland, E.; Puka-Sundvall, M.; Gustafson, K.; Hagberg, H. Chemokine and inflammatory cell response to hypoxia-ischemia in immature rats. Pediatr. Res. 1999, 45, 500–509. [Google Scholar] [CrossRef]
- Winerdal, M.; Winerdal, M.E.; Kinn, J.; Urmaliya, V.; Winqvist, O.; Ådén, U. Long lasting local and systemic inflammation after cerebral hypoxic ischemia in newborn mice. PLoS ONE 2012, 7, e36422. [Google Scholar] [CrossRef]
- Sofroniew, M.V. Molecular dissection of reactive astrogliosis and glial scar formation. Trends Neurosci. 2009, 32, 638–647. [Google Scholar] [CrossRef]
- Verkhratsky, A.; Sofroniew, M.V.; Messing, A.; deLanerolle, N.C.; Rempe, D.; Rodríguez, J.J.; Nedergaard, M. Neurological diseases as primary gliopathies: A reassessment of neurocentrism. ASN Neuro 2012. [Google Scholar] [CrossRef]
- Johnston, M.V.; Fatemi, A.; Wilson, M.A.; Northington, F. Treatment advances in neonatal neuroprotection and neurointensive care. Lancet Neurol. 2011, 10, 372–382. [Google Scholar] [CrossRef]
- Morken, T.S.; Brekke, E.; Håberg, A.; Widerøe, M.; Brubakk, A.-M.; Sonnewald, U. Altered astrocyte–neuronal interactions after hypoxia-ischemia in the neonatal brain in female and male rats. Stroke 2014, 45, 2777–2785. [Google Scholar] [CrossRef]
- Wang, X.; Yang, X.-L.; Kong, W.-L.; Zeng, M.-L.; Shao, L.; Jiang, G.-T.; Cheng, J.-J.; Kong, S.; He, X.-H.; Liu, W.-H.; et al. TRPV1 translocated to astrocytic membrane to promote migration and inflammatory infiltration thus promotes epilepsy after hypoxic ischemia in immature brain. J. Neuroinflammation 2019, 16, 214. [Google Scholar] [CrossRef] [PubMed]
- Hurtado-Zavala, J.I.; Ramachandran, B.; Ahmed, S.; Halder, R.; Bolleyer, C.; Awasthi, A.; Stahlberg, M.A.; Wagener, R.J.; Anderson, K.R.; Drenan, R.M.; et al. TRPV1 regulates excitatory innervation of OLM neurons in the hippocampus. Nat. Commun. 2017, 8, 15878. [Google Scholar] [CrossRef]
- He, M.L.; Lv, Z.Y.; Shi, X.; Yang, T.; Zhang, Y.; Li, T.-Y.; Chen, J. Interleukin-10 release from astrocytes suppresses neuronal apoptosis via the TLR2/NFκB pathway in a neonatal rat model of hypoxic-ischemic brain damage. J. Neurochem. 2017, 142, 920–933. [Google Scholar] [CrossRef] [PubMed]
- Jiao, M.; Li, X.; Chen, L.; Wang, X.; Yuan, B.; Liu, T. Neuroprotective effect of astrocyte-derived IL-33 in neonatal hypoxic-ischemic brain injury. J. Neuroinflammation 2020, 17, 251. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; He, M.; Zhou, X.; Liu, J.; Hou, N.; Bin, T.; Zhang, Y.; Li, T.; Chen, J. Endogenous IL-6 of mesenchymal stem cell improves behavioral outcome of hypoxic-ischemic brain damage neonatal rats by supressing apoptosis in astrocyte. Sci. Rep. 2016, 6, 18587. [Google Scholar] [CrossRef]
- He, M.; Shi, X.; Yang, M.; Yang, T.; Li, T.; Chen, J. Mesenchymal stem cells-derived IL-6 activates AMPK/mTOR signaling to inhibit the proliferation of reactive astrocytes induced by hypoxic-ischemic brain damage. Exp. Neurol. 2019, 311, 15–32. [Google Scholar] [CrossRef]
- Montaldo, P.; Ivain, P.; Lally, P.; Bassett, P.; Pant, S.; Oliveira, V. White matter injury after neonatal encephalopathy is associated with thalamic metabolite perturbations. EBioMedicine 2020, 52, 102663. [Google Scholar] [CrossRef]
- Haynes, R.L.; Folkerth, R.D.; Keefe, R.J.; Sung, I.; Swzeda, L.I.; Rosenberg, P.A.; Volpe, J.J.; Kinney, H.C. Nitrosative and oxidative injury to premyelinating oligodendrocytes in periventricular Leukomalacia. J. Neuropathol. Exp. Neurol. 2003, 62, 441–450. [Google Scholar] [CrossRef]
- Billiards, S.S.; Haynes, R.L.; Folkerth, R.D.; Borenstein, N.S.; Trachtenberg, F.L.; Rowitch, D.H.; Ligon, K.L.; Volpe, J.J.; Kinney, H.C. Myelin abnormalities without oligodendrocyte loss in periventricular Leukomalacia. Brain Pathol. 2008, 18, 153–163. [Google Scholar] [CrossRef]
- Favrais, G.; van de Looij, Y.; Fleiss, B.; Ramanantsoa, N.; Bonnin, P.; Stoltenburg-Didinger, G. Systemic inflammation disrupts the developmental program of white matter. Ann. Neurol. 2011, 70, 550–565. [Google Scholar] [CrossRef] [PubMed]
- Val, A.; Ferrario, M.; Dreano, M.; Garotta, G.; Spano, P.; Pizzi, M. Soluble Interleukin-6 (IL-6) Receptor/IL-6 fusion protein enhances in vitro differentiation of purified rat oligodendroglial lineage cells. Mol. Cell. Neurosci. 2002, 21, 602–615. [Google Scholar]
- Campbell, I.L.; Abraham, C.R.; Masliah, E.; Kemper, P.; Inglis, J.D.; Oldstone, M.B.; Mucke, L. Neurologic disease induced in transgenic mice by cerebral overexpression of interleukin 6. Proc. Natl. Acad. Sci. USA 1993, 90, 10061–10065. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.Y.; Rocha-Ferreira, E.; Ek, C.J.; Wang, X.; Hagberg, H.; Mallard, C. Immune responses in perinatal brain injury. Brain Behav. Immun. 2016, 63, 210–223. [Google Scholar] [CrossRef]
- Martín-Ancel, A.; García-Alix, A.; Salas, S.; Castillo F del Cabañas, F.; Quero, J. Cerebrospinal fluid leucocyte counts in healthy neonates. Arch. Dis. Child. Neonatal Ed. 2006, 91, F357–F358. [Google Scholar] [CrossRef]
- Hedtjärn, M.; Mallard, C.; Hagberg, H. Inflammatory Gene Profiling in the Developing Mouse Brain after Hypoxia-Ischemia. J. Cereb. Blood Flow Metab. 2004, 24, 1333–1551. [Google Scholar] [CrossRef]
- Shi, C.; Pamer, E.G. Monocyte recruitment during infection and inflammation. Nat. Rev. Immunol. 2011, 11, 762–774. [Google Scholar] [CrossRef]
- Palmer, C.; Roberts, R.L.; Young, P.I. Timing of neutrophil depletion influences long-term neuroprotection in neonatal rat hypoxic-ischemic brain injury. Pediatr. Res. 2004, 55, 549–556. [Google Scholar] [CrossRef]
- Mesplès, B.; Fontaine, R.H.; Lelièvre, V.; Launay, J.-M.; Gressens, P. Neuronal TGF-beta1 mediates IL-9/mast cell interaction and exacerbates excitotoxicity in newborn mice. Neurobiol. Dis. 2005, 18, 193–205. [Google Scholar] [CrossRef]
- Jin, Y.; Silverman, A.-J.; Vannucci, S.J. Mast cell stabilization limits hypoxic-ischemic brain damage in the immature rat. DNE 2007, 29, 373–384. [Google Scholar] [CrossRef]
- Jin, Y.; Silverman Ann, J.; Vannucci Susan, J. Mast cells are early responders after hypoxia-ischemia in immature rat brain. Stroke 2009, 40, 3107–3112. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.L.P.; Mottahedin, A.; Svedin, P.; Mohn, C.-J.; Hagberg, H.; Ek, J.; Mallard, C. Peripheral myeloid cells contribute to brain injury in male neonatal mice. J. Neuroinflammation 2018, 15, 301. [Google Scholar] [CrossRef] [PubMed]
- Albertsson, A.-M.; Bi, D.; Duan, L.; Zhang, X.; Leavenworth, J.W.; Qiao, L.; Zhu, C.; Cardell, S.; Cantor, H.; Hagberg, H.; et al. The immune response after hypoxia-ischemia in a mouse model of preterm brain injury. J. Neuroinflammation 2014, 11, 153. [Google Scholar] [CrossRef] [PubMed]
| O2 Levels | Age | Duration | Common Reported Behaviour | References |
|---|---|---|---|---|
| Rat | ||||
| 0% | P0–P11 | 5–30 min | Hyperactivity in open field, impaired memory, increase anxiety | [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44] |
| 2.5–5% | P0–P10 | 15–30 min | Seizures during hypoxia, worse water maze performance | [44,45,46,47,48,49,50,51,52] |
| 5–8% | P7–P10 | 15 min–3 h | Increase susceptibility to chemical induced seizures at adulthood | [53,54,55,56,57,58,59,60,61,62] |
| 10% | P7–P9 | 30 min–6 h | Hyperactivity in novel object task | [63,64,65] |
| Mouse | ||||
| 0% | P0–P15 | 20–25 min | Hyperactivity and seizures | [66,67] |
| 5% | P1–P7 | 15 min–2 h | Seizures, impaired learning | [9,68] |
| Species | O2 Partial Pressure | Age (Postnatal Day) | T (°C) | Duration of Hypoxia | Reported Behavioural Phenotype | References |
|---|---|---|---|---|---|---|
| C57 Mouse | 0% | P3–15 | RT | 20 min | Electrographic seizures without clinical manifestations. | [67] |
| Mouse | 0% | P0 | 33, 37, 39 | 25 min | Both open-field stress-induced and spontaneous motor activity reduced. Hyperactive in the plus maze test. Behavioural disturbances were prevented by the body temperature of 33 °C. | [66] |
| C57 Mouse | 5% | P7 | 34 | 15 min | Seizures in pups, reduced curiosity in novel object test, weight loss. | [9] |
| Mouse | 5% | P1 | - | 2 h | Melatonin improved learning and memory in the Morris water maze. | [68] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leavy, A.; Jimenez Mateos, E.M. Perinatal Brain Injury and Inflammation: Lessons from Experimental Murine Models. Cells 2020, 9, 2640. https://doi.org/10.3390/cells9122640
Leavy A, Jimenez Mateos EM. Perinatal Brain Injury and Inflammation: Lessons from Experimental Murine Models. Cells. 2020; 9(12):2640. https://doi.org/10.3390/cells9122640
Chicago/Turabian StyleLeavy, Aisling, and Eva M. Jimenez Mateos. 2020. "Perinatal Brain Injury and Inflammation: Lessons from Experimental Murine Models" Cells 9, no. 12: 2640. https://doi.org/10.3390/cells9122640
APA StyleLeavy, A., & Jimenez Mateos, E. M. (2020). Perinatal Brain Injury and Inflammation: Lessons from Experimental Murine Models. Cells, 9(12), 2640. https://doi.org/10.3390/cells9122640






