Inflammatory Bowel Disease: A Stressed “Gut/Feeling”
Abstract
1. Introduction
2. Search Strategy
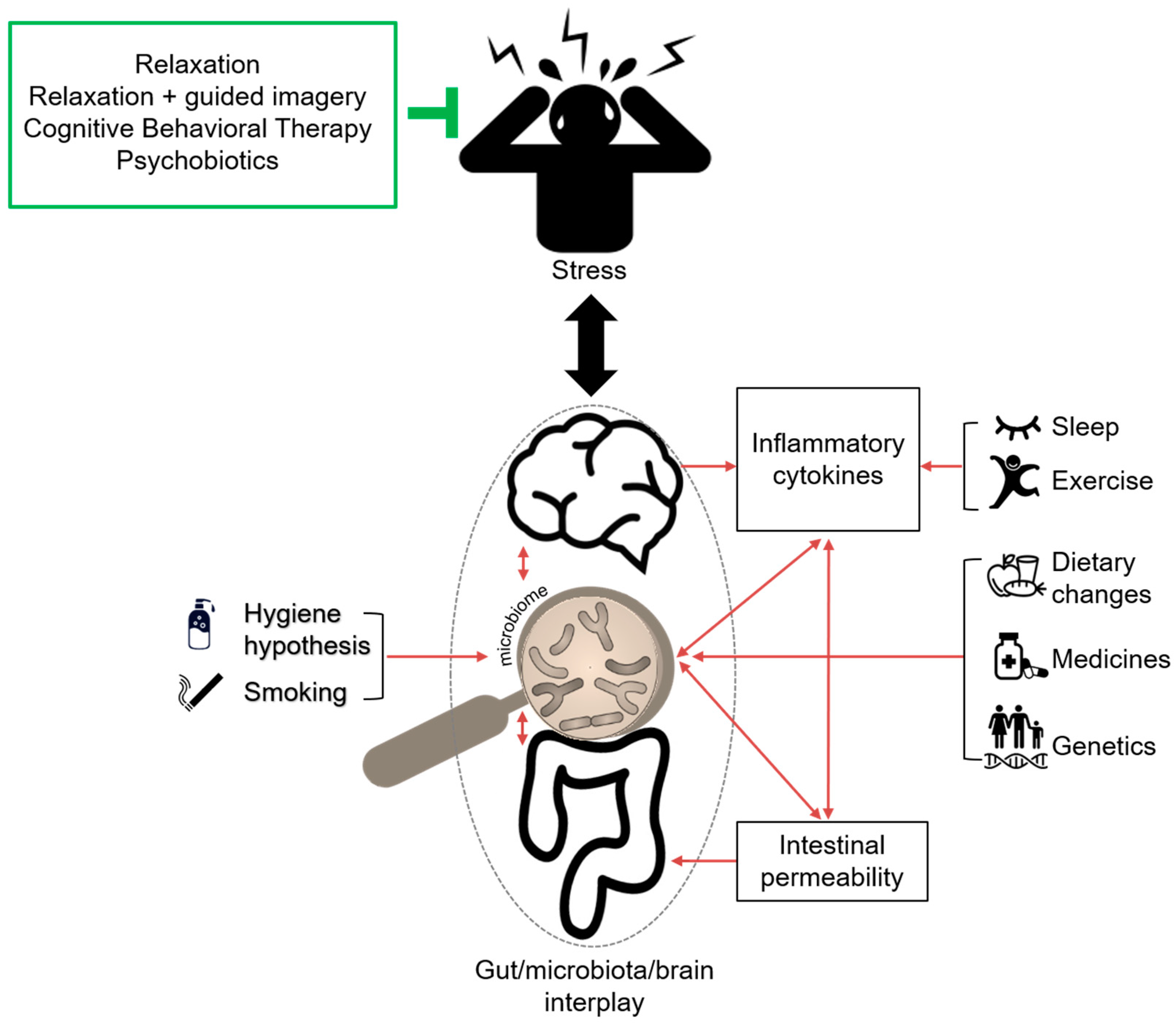
3. Gut/Microbiota/Brain Interplay
3.1. Brain/Gut Interaction
3.2. Gut Microbiota
4. Gut/Microbiota/Brain Interplay in IBD Development
5. Stress and Intestinal Microbiota: Bidirectional Relationship in IBD
5.1. Influence of Stress on Gut Microbiota
5.1.1. Preclinical Studies
5.1.2. Clinical Studies
5.2. Impact of Intestinal Microbiota on Stress Responsiveness
5.2.1. Preclinical Studies
5.2.2. Clinical Studies
5.3. Stress and Its Impact on Inflammation
5.3.1. Preclinical Studies
5.3.2. Clinical Studies
5.4. Stress and Inflammation in IBD
5.4.1. Preclinical Studies
5.4.2. Clinical Studies
6. Managing Stress in IBD: Does It Make the Gut Feel Better?
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACTH | Adrenocorticotropic hormone |
| ANS | Autonomic nervous system |
| CNS | Central nervous system |
| CRF | Corticotropin-releasing factor |
| CRP | C-reactive protein |
| ENS | Enteric nervous system |
| HPA | Hypothalamic pituitary adrenal |
| IBD | Inflammatory bowel disease |
| IBS | Irritable bowel syndrome |
| IFNγ | Interferon-gamma |
| IL | Interleukin |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| MCP1 | Monocyte chemotactic protein-1 |
| SCFA | Short-chain fatty acids |
| TNFα | Tumor necrosis factor alpha |
References
- Tontini, G.E.; Vecchi, M.; Pastorelli, L.; Neurath, M.F.; Neumann, H. Differential diagnosis in inflammatory bowel disease colitis: State of the art and future perspectives. World J. Gastroenterol. 2015, 21, 21–46. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N. Epidemiology and risk factors for IBD. Nat Rev. Gastroenterol. Hepatol. 2015, 12, 205–217. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Pang, Z.; Chen, W.; Ju, S.; Zhou, C. The epidemiology and risk factors of inflammatory bowel disease. Int J. Clin. Exp. Med. 2015, 8, 22529–22542. [Google Scholar] [PubMed]
- Camara, R.J.; Ziegler, R.; Begre, S.; Schoepfer, A.M.; von Kanel, R.; Swiss Inflammatory Bowel Disease Cohort Study Group. The role of psychological stress in inflammatory bowel disease: Quality assessment of methods of 18 prospective studies and suggestions for future research. Digestion 2009, 80, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Mawdsley, J.E.; Rampton, D.S. Psychological stress in IBD: New insights into pathogenic and therapeutic implications. Gut 2005, 54, 1481–1491. [Google Scholar] [CrossRef] [PubMed]
- Yeager, M.P.; Pioli, P.A.; Guyre, P.M. Cortisol exerts bi-phasic regulation of inflammation in humans. Dose Response 2011, 9, 332–347. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Victor Fon, G.; Meixner, W.; Creekmore, A.; Zong, Y.; M, K.D.; Colacino, J.; Dedhia, P.H.; Hong, S.; Wiley, J.W. Chronic stress and intestinal barrier dysfunction: Glucocorticoid receptor and transcription repressor HES1 regulate tight junction protein Claudin-1 promoter. Sci. Rep. 2017, 7, 4502. [Google Scholar] [CrossRef]
- Petrosus, E.; Silva, E.B.; Lay, D., Jr.; Eicher, S.D. Effects of orally administered cortisol and norepinephrine on weanling piglet gut microbial populations and Salmonella passage. J. Anim. Sci. 2018, 96, 4543–4551. [Google Scholar] [CrossRef]
- Gonzalez-Ariki, S.; Husband, A.J. The role of sympathetic innervation of the gut in regulating mucosal immune responses. Brain Behav. Immun. 1998, 12, 53–63. [Google Scholar] [CrossRef]
- Mourad, F.H.; Saade, N.E. Neural regulation of intestinal nutrient absorption. Prog. Neurobiol. 2011, 95, 149–162. [Google Scholar] [CrossRef]
- Cryan, J.F.; O’Mahony, S.M. The microbiome-gut-brain axis: From bowel to behavior. Neurogastroenterol. Motil. 2011, 23, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Clapp, M.; Aurora, N.; Herrera, L.; Bhatia, M.; Wilen, E.; Wakefield, S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin. Pract. 2017, 7, 987. [Google Scholar] [CrossRef] [PubMed]
- Yoo, B.B.; Mazmanian, S.K. The Enteric Network: Interactions between the Immune and Nervous Systems of the Gut. Immunity 2017, 46, 910–926. [Google Scholar] [CrossRef] [PubMed]
- Furness, J.B.; Costa, M. Types of nerves in the enteric nervous system. Neuroscience 1980, 5, 1–20. [Google Scholar] [CrossRef]
- Schneider, S.; Wright, C.M.; Heuckeroth, R.O. Unexpected Roles for the Second Brain: Enteric Nervous System as Master Regulator of Bowel Function. Annu. Rev. Physiol. 2019, 81, 235–259. [Google Scholar] [CrossRef] [PubMed]
- Gershon, M.D. The enteric nervous system: A second brain. Hosp. Pract. 1999, 34, 31–52. [Google Scholar] [CrossRef]
- Jandhyala, S.M.; Talukdar, R.; Subramanyam, C.; Vuyyuru, H.; Sasikala, M.; Nageshwar Reddy, D. Role of the normal gut microbiota. World J. Gastroenterol. 2015, 21, 8787–8803. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.N.; St Amand, A.L.; Feldman, R.A.; Boedeker, E.C.; Harpaz, N.; Pace, N.R. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc. Natl. Acad. Sci. USA 2007, 104, 13780–13785. [Google Scholar] [CrossRef]
- Haiser, H.J.; Turnbaugh, P.J. Developing a metagenomic view of xenobiotic metabolism. Pharmacol. Res. 2013, 69, 21–31. [Google Scholar] [CrossRef]
- Kuethe, J.W.; Armocida, S.M.; Midura, E.F.; Rice, T.C.; Hildeman, D.A.; Healy, D.P.; Caldwell, C.C. Fecal Microbiota Transplant Restores Mucosal Integrity in a Murine Model of Burn Injury. Shock 2015. [Google Scholar] [CrossRef]
- Donaldson, G.P.; Lee, S.M.; Mazmanian, S.K. Gut biogeography of the bacterial microbiota. Nat. Rev. Microbiol. 2016, 14, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Kamada, N.; Chen, G.Y.; Inohara, N.; Nunez, G. Control of pathogens and pathobionts by the gut microbiota. Nat. Immunol. 2013, 14, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Guida, F.; Turco, F.; Iannotta, M.; De Gregorio, D.; Palumbo, I.; Sarnelli, G.; Furiano, A.; Napolitano, F.; Boccella, S.; Luongo, L.; et al. Antibiotic-induced microbiota perturbation causes gut endocannabinoidome changes, hippocampal neuroglial reorganization and depression in mice. Brain Behav. Immun. 2018, 67, 230–245. [Google Scholar] [CrossRef] [PubMed]
- Zheng, P.; Zeng, B.; Zhou, C.; Liu, M.; Fang, Z.; Xu, X.; Zeng, L.; Chen, J.; Fan, S.; Du, X.; et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol. Psychiatry 2016. [Google Scholar] [CrossRef] [PubMed]
- Mi, G.L.; Zhao, L.; Qiao, D.D.; Kang, W.Q.; Tang, M.Q.; Xu, J.K. Effectiveness of Lactobacillus reuteri in infantile colic and colicky induced maternal depression: A prospective single blind randomized trial. Antonie Van Leeuwenhoek 2015, 107, 1547–1553. [Google Scholar] [CrossRef] [PubMed]
- Ni, J.; Wu, G.D.; Albenberg, L.; Tomov, V.T. Gut microbiota and IBD: Causation or correlation? Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 573–584. [Google Scholar] [CrossRef]
- Zhang, M.; Sun, K.; Wu, Y.; Yang, Y.; Tso, P.; Wu, Z. Interactions between Intestinal Microbiota and Host Immune Response in Inflammatory Bowel Disease. Front. Immunol. 2017, 8, 942. [Google Scholar] [CrossRef]
- Cryan, J.F.; Dinan, T.G. Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nat. Rev. Neurosci. 2012, 13, 701–712. [Google Scholar] [CrossRef]
- Waclawikova, B.; El Aidy, S. Role of Microbiota and Tryptophan Metabolites in the Remote Effect of Intestinal Inflammation on Brain and Depression. Pharmaceuticals 2018, 11, 63. [Google Scholar] [CrossRef]
- Takahashi, K.; Nishida, A.; Fujimoto, T.; Fujii, M.; Shioya, M.; Imaeda, H.; Inatomi, O.; Bamba, S.; Sugimoto, M.; Andoh, A. Reduced Abundance of Butyrate-Producing Bacteria Species in the Fecal Microbial Community in Crohn’s Disease. Digestion 2016, 93, 59–65. [Google Scholar] [CrossRef]
- Parada Venegas, D.; De la Fuente, M.K.; Landskron, G.; Gonzalez, M.J.; Quera, R.; Dijkstra, G.; Harmsen, H.J.M.; Faber, K.N.; Hermoso, M.A. Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Front. Immunol. 2019, 10, 277. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kotani, T.; Konno, T.; Setiawan, J.; Kitamura, Y.; Imada, S.; Usui, Y.; Hatano, N.; Shinohara, M.; Saito, Y.; et al. Promotion of Intestinal Epithelial Cell Turnover by Commensal Bacteria: Role of Short-Chain Fatty Acids. PLoS ONE 2016, 11, e0156334. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Kelly, C.J.; Battista, K.D.; Schaefer, R.; Lanis, J.M.; Alexeev, E.E.; Wang, R.X.; Onyiah, J.C.; Kominsky, D.J.; Colgan, S.P. Microbial-Derived Butyrate Promotes Epithelial Barrier Function through IL-10 Receptor-Dependent Repression of Claudin-2. J. Immunol. 2017, 199, 2976–2984. [Google Scholar] [CrossRef] [PubMed]
- Donohoe, D.R.; Garge, N.; Zhang, X.; Sun, W.; O’Connell, T.M.; Bunger, M.K.; Bultman, S.J. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 2011, 13, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Macia, L.; Tan, J.; Vieira, A.T.; Leach, K.; Stanley, D.; Luong, S.; Maruya, M.; Ian McKenzie, C.; Hijikata, A.; Wong, C.; et al. Metabolite-sensing receptors GPR43 and GPR109A facilitate dietary fibre-induced gut homeostasis through regulation of the inflammasome. Nat. Commun. 2015, 6, 6734. [Google Scholar] [CrossRef]
- Lydiard, R.B. The role of GABA in anxiety disorders. J. Clin. Psychiatry 2003, 64 (Suppl. 3), 21–27. [Google Scholar]
- Orholm, M.; Munkholm, P.; Langholz, E.; Nielsen, O.H.; Sorensen, T.I.; Binder, V. Familial occurrence of inflammatory bowel disease. N. Engl. J. Med. 1991, 324, 84–88. [Google Scholar] [CrossRef]
- Kostic, A.D.; Xavier, R.J.; Gevers, D. The microbiome in inflammatory bowel disease: Current status and the future ahead. Gastroenterology 2014, 146, 1489–1499. [Google Scholar] [CrossRef]
- Jostins, L.; Ripke, S.; Weersma, R.K.; Duerr, R.H.; McGovern, D.P.; Hui, K.Y.; Lee, J.C.; Schumm, L.P.; Sharma, Y.; Anderson, C.A.; et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 2012, 491, 119–124. [Google Scholar] [CrossRef]
- Liu, J.Z.; van Sommeren, S.; Huang, H.; Ng, S.C.; Alberts, R.; Takahashi, A.; Ripke, S.; Lee, J.C.; Jostins, L.; Shah, T.; et al. Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nat. Genet. 2015, 47, 979–986. [Google Scholar] [CrossRef]
- Cleynen, I.; Vazeille, E.; Artieda, M.; Verspaget, H.W.; Szczypiorska, M.; Bringer, M.A.; Lakatos, P.L.; Seibold, F.; Parnell, K.; Weersma, R.K.; et al. Genetic and microbial factors modulating the ubiquitin proteasome system in inflammatory bowel disease. Gut 2014, 63, 1265–1274. [Google Scholar] [CrossRef] [PubMed]
- Cleynen, I.; Boucher, G.; Jostins, L.; Schumm, L.P.; Zeissig, S.; Ahmad, T.; Andersen, V.; Andrews, J.M.; Annese, V.; Brand, S.; et al. Inherited determinants of Crohn’s disease and ulcerative colitis phenotypes: A genetic association study. Lancet 2016, 387, 156–167. [Google Scholar] [CrossRef]
- Momozawa, Y.; Dmitrieva, J.; Theatre, E.; Deffontaine, V.; Rahmouni, S.; Charloteaux, B.; Crins, F.; Docampo, E.; Elansary, M.; Gori, A.S.; et al. IBD risk loci are enriched in multigenic regulatory modules encompassing putative causative genes. Nat. Commun. 2018, 9, 2427. [Google Scholar] [CrossRef] [PubMed]
- Barthel, C.; Spalinger, M.R.; Brunner, J.; Lang, S.; Fried, M.; Rogler, G.; Scharl, M. A distinct pattern of disease-associated single nucleotide polymorphisms in IBD risk genes in a family with Crohn’s disease. Eur J. Gastroenterol. Hepatol. 2014, 26, 803–806. [Google Scholar] [CrossRef] [PubMed]
- Spehlmann, M.E.; Begun, A.Z.; Burghardt, J.; Lepage, P.; Raedler, A.; Schreiber, S. Epidemiology of inflammatory bowel disease in a German twin cohort: Results of a nationwide study. Inflamm. Bowel Dis. 2008, 14, 968–976. [Google Scholar] [CrossRef] [PubMed]
- Halfvarson, J.; Bodin, L.; Tysk, C.; Lindberg, E.; Jarnerot, G. Inflammatory bowel disease in a Swedish twin cohort: A long-term follow-up of concordance and clinical characteristics. Gastroenterology 2003, 124, 1767–1773. [Google Scholar] [CrossRef]
- Ardesia, M.; Ferlazzo, G.; Fries, W. Vitamin D and inflammatory bowel disease. Biomed. Res. Int. 2015, 2015, 470805. [Google Scholar] [CrossRef]
- Bashir, M.; Prietl, B.; Tauschmann, M.; Mautner, S.I.; Kump, P.K.; Treiber, G.; Wurm, P.; Gorkiewicz, G.; Hogenauer, C.; Pieber, T.R. Effects of high doses of vitamin D3 on mucosa-associated gut microbiome vary between regions of the human gastrointestinal tract. Eur. J. Nutr. 2016, 55, 1479–1489. [Google Scholar] [CrossRef]
- Lahiri, A.; Abraham, C. Activation of pattern recognition receptors up-regulates metallothioneins, thereby increasing intracellular accumulation of zinc, autophagy, and bacterial clearance by macrophages. Gastroenterology 2014, 147, 835–846. [Google Scholar] [CrossRef]
- Rogler, G.; Vavricka, S. Anemia in inflammatory bowel disease: An under-estimated problem? Front. Med. (Lausanne) 2014, 1, 58. [Google Scholar] [CrossRef]
- Mahid, S.S.; Minor, K.S.; Soto, R.E.; Hornung, C.A.; Galandiuk, S. Smoking and inflammatory bowel disease: A meta-analysis. Mayo Clin. Proc. 2006, 81, 1462–1471. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.E.; Morgan, J.M.; Jasani, B.; Green, J.T.; Rhodes, J.; Williams, G.T.; Lindstrom, J.; Wonnacott, S.; Peel, S.; Thomas, G.A. Effect of smoking and transdermal nicotine on colonic nicotinic acetylcholine receptors in ulcerative colitis. QJM 2003, 96, 57–65. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khor, B.; Gardet, A.; Xavier, R.J. Genetics and pathogenesis of inflammatory bowel disease. Nature 2011, 474, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Pituch-Zdanowska, A.; Banaszkiewicz, A.; Albrecht, P. The role of dietary fibre in inflammatory bowel disease. Prz. Gastroenterol. 2015, 10, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, M.A.; Hoffmann, C.; Sherrill-Mix, S.A.; Keilbaugh, S.A.; Hamady, M.; Chen, Y.Y.; Knight, R.; Ahima, R.S.; Bushman, F.; Wu, G.D. High-fat diet determines the composition of the murine gut microbiome independently of obesity. Gastroenterology 2009, 137, 1716–1724. [Google Scholar] [CrossRef] [PubMed]
- Parks, B.W.; Nam, E.; Org, E.; Kostem, E.; Norheim, F.; Hui, S.T.; Pan, C.; Civelek, M.; Rau, C.D.; Bennett, B.J.; et al. Genetic control of obesity and gut microbiota composition in response to high-fat, high-sucrose diet in mice. Cell Metab. 2013, 17, 141–152. [Google Scholar] [CrossRef] [PubMed]
- Geerling, B.J.; Dagnelie, P.C.; Badart-Smook, A.; Russel, M.G.; Stockbrugger, R.W.; Brummer, R.J. Diet as a risk factor for the development of ulcerative colitis. Am. J. Gastroenterol. 2000, 95, 1008–1013. [Google Scholar] [CrossRef]
- Aldini, R.; Micucci, M.; Cevenini, M.; Fato, R.; Bergamini, C.; Nanni, C.; Cont, M.; Camborata, C.; Spinozzi, S.; Montagnani, M.; et al. Antiinflammatory effect of phytosterols in experimental murine colitis model: Prevention, induction, remission study. PLoS ONE 2014, 9, e108112. [Google Scholar] [CrossRef]
- Brolinson, P.G.; Elliott, D. Exercise and the immune system. Clin. Sports Med. 2007, 26, 311–319. [Google Scholar] [CrossRef]
- Saxena, A.; Fletcher, E.; Larsen, B.; Baliga, M.S.; Durstine, J.L.; Fayad, R. Effect of exercise on chemically-induced colitis in adiponectin deficient mice. J. Inflamm. 2012, 9, 30. [Google Scholar] [CrossRef]
- Khalili, H.; Ananthakrishnan, A.N.; Konijeti, G.G.; Liao, X.; Higuchi, L.M.; Fuchs, C.S.; Spiegelman, D.; Richter, J.M.; Korzenik, J.R.; Chan, A.T. Physical activity and risk of inflammatory bowel disease: Prospective study from the Nurses’ Health Study cohorts. BMJ 2013, 347, f6633. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.C.; Tang, W.; Leong, R.W.; Chen, M.; Ko, Y.; Studd, C.; Niewiadomski, O.; Bell, S.; Kamm, M.A.; de Silva, H.J.; et al. Environmental risk factors in inflammatory bowel disease: A population-based case-control study in Asia-Pacific. Gut 2015, 64, 1063–1071. [Google Scholar] [CrossRef] [PubMed]
- Loudon, C.P.; Corroll, V.; Butcher, J.; Rawsthorne, P.; Bernstein, C.N. The effects of physical exercise on patients with Crohn’s disease. Am. J. Gastroenterol. 1999, 94, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Engels, M.; Cross, R.K.; Long, M.D. Exercise in patients with inflammatory bowel diseases: Current perspectives. Clin. Exp. Gastroenterol. 2018, 11, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bloomfield, S.F.; Stanwell-Smith, R.; Crevel, R.W.; Pickup, J. Too clean, or not too clean: The hygiene hypothesis and home hygiene. Clin. Exp. Allergy 2006, 36, 402–425. [Google Scholar] [CrossRef]
- Ng, S.C.; Bernstein, C.N.; Vatn, M.H.; Lakatos, P.L.; Loftus, E.V., Jr.; Tysk, C.; O’Morain, C.; Moum, B.; Colombel, J.F.; Epidemiology; et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut 2013, 62, 630–649. [Google Scholar] [CrossRef] [PubMed]
- Koloski, N.A.; Bret, L.; Radford-Smith, G. Hygiene hypothesis in inflammatory bowel disease: A critical review of the literature. World J. Gastroenterol. 2008, 14, 165–173. [Google Scholar] [CrossRef]
- Carpio, D.; Barreiro-de Acosta, M.; Echarri, A.; Pereira, S.; Castro, J.; Ferreiro, R.; Lorenzo, A.; Group, E. Influence of urban/rural and coastal/inland environment on the prevalence, phenotype, and clinical course of inflammatory bowel disease patients from northwest of Spain: A cross-sectional study. Eur J. Gastroenterol. Hepatol 2015, 27, 1030–1037. [Google Scholar] [CrossRef]
- Piovani, D.; Danese, S.; Peyrin-Biroulet, L.; Nikolopoulos, G.K.; Lytras, T.; Bonovas, S. Environmental Risk Factors for Inflammatory Bowel Diseases: An Umbrella Review of Meta-analyses. Gastroenterology 2019. [Google Scholar] [CrossRef]
- Ungaro, R.; Bernstein, C.N.; Gearry, R.; Hviid, A.; Kolho, K.L.; Kronman, M.P.; Shaw, S.; Van Kruiningen, H.; Colombel, J.F.; Atreja, A. Antibiotics associated with increased risk of new-onset Crohn’s disease but not ulcerative colitis: A meta-analysis. Am. J. Gastroenterol. 2014, 109, 1728–1738. [Google Scholar] [CrossRef]
- Ortizo, R.; Lee, S.Y.; Nguyen, E.T.; Jamal, M.M.; Bechtold, M.M.; Nguyen, D.L. Exposure to oral contraceptives increases the risk for development of inflammatory bowel disease: A meta-analysis of case-controlled and cohort studies. Eur J. Gastroenterol. Hepatol. 2017, 29, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Felder, J.B.; Korelitz, B.I.; Rajapakse, R.; Schwarz, S.; Horatagis, A.P.; Gleim, G. Effects of nonsteroidal antiinflammatory drugs on inflammatory bowel disease: A case-control study. Am. J. Gastroenterol. 2000, 95, 1949–1954. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Graff, L.A.; Bernstein, C.N. Do NSAIDs, antibiotics, infections, or stress trigger flares in IBD? Am. J. Gastroenterol. 2009, 104, 1298–1313. [Google Scholar] [CrossRef] [PubMed]
- Guslandi, M. Exacerbation of inflammatory bowel disease by nonsteroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors: Fact or fiction? World J. Gastroenterol. 2006, 12, 1509–1510. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N.; Long, M.D.; Martin, C.F.; Sandler, R.S.; Kappelman, M.D. Sleep disturbance and risk of active disease in patients with Crohn’s disease and ulcerative colitis. Clin. Gastroenterol. Hepatol. 2013, 11, 965–971. [Google Scholar] [CrossRef] [PubMed]
- Born, J.; Lange, T.; Hansen, K.; Molle, M.; Fehm, H.L. Effects of sleep and circadian rhythm on human circulating immune cells. J. Immunol. 1997, 158, 4454–4464. [Google Scholar]
- Mahlmann, L.; Gerber, M.; Furlano, R.I.; Legeret, C.; Kalak, N.; Holsboer-Trachsler, E.; Brand, S. Impaired objective and subjective sleep in children and adolescents with inflammatory bowel disease compared to healthy controls. Sleep Med. 2017, 39, 25–31. [Google Scholar] [CrossRef]
- Keefer, L.; Stepanski, E.J.; Ranjbaran, Z.; Benson, L.M.; Keshavarzian, A. An initial report of sleep disturbance in inactive inflammatory bowel disease. J. Clin. Sleep Med. 2006, 2, 409–416. [Google Scholar]
- Ali, T.; Madhoun, M.F.; Orr, W.C.; Rubin, D.T. Assessment of the relationship between quality of sleep and disease activity in inflammatory bowel disease patients. Inflamm. Bowel Dis. 2013, 19, 2440–2443. [Google Scholar] [CrossRef]
- Voigt, R.M.; Forsyth, C.B.; Green, S.J.; Mutlu, E.; Engen, P.; Vitaterna, M.H.; Turek, F.W.; Keshavarzian, A. Circadian disorganization alters intestinal microbiota. PLoS ONE 2014, 9, e97500. [Google Scholar] [CrossRef]
- Bharwani, A.; Mian, M.F.; Foster, J.A.; Surette, M.G.; Bienenstock, J.; Forsythe, P. Structural & functional consequences of chronic psychosocial stress on the microbiome & host. Psychoneuroendocrinology 2016, 63, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Bengmark, S. Gut microbiota, immune development and function. Pharmacol Res. 2013, 69, 87–113. [Google Scholar] [CrossRef] [PubMed]
- Xie, R.; Sun, Y.; Wu, J.; Huang, S.; Jin, G.; Guo, Z.; Zhang, Y.; Liu, T.; Liu, X.; Cao, X.; et al. Maternal High Fat Diet Alters Gut Microbiota of Offspring and Exacerbates DSS-Induced Colitis in Adulthood. Front. Immunol. 2018, 9, 2608. [Google Scholar] [CrossRef] [PubMed]
- Golubeva, A.V.; Crampton, S.; Desbonnet, L.; Edge, D.; O’Sullivan, O.; Lomasney, K.W.; Zhdanov, A.V.; Crispie, F.; Moloney, R.D.; Borre, Y.E.; et al. Prenatal stress-induced alterations in major physiological systems correlate with gut microbiota composition in adulthood. Psychoneuroendocrinology 2015, 60, 58–74. [Google Scholar] [CrossRef] [PubMed]
- Jasarevic, E.; Howerton, C.L.; Howard, C.D.; Bale, T.L. Alterations in the Vaginal Microbiome by Maternal Stress Are Associated With Metabolic Reprogramming of the Offspring Gut and Brain. Endocrinology 2015, 156, 3265–3276. [Google Scholar] [CrossRef] [PubMed]
- Collado, M.C.; Cernada, M.; Bauerl, C.; Vento, M.; Perez-Martinez, G. Microbial ecology and host-microbiota interactions during early life stages. Gut Microbes 2012, 3, 352–365. [Google Scholar] [CrossRef] [PubMed]
- Donnet-Hughes, A.; Perez, P.F.; Dore, J.; Leclerc, M.; Levenez, F.; Benyacoub, J.; Serrant, P.; Segura-Roggero, I.; Schiffrin, E.J. Potential role of the intestinal microbiota of the mother in neonatal immune education. Proc. Nutr Soc. 2010, 69, 407–415. [Google Scholar] [CrossRef]
- Bailey, M.T.; Dowd, S.E.; Galley, J.D.; Hufnagle, A.R.; Allen, R.G.; Lyte, M. Exposure to a social stressor alters the structure of the intestinal microbiota: Implications for stressor-induced immunomodulation. Brain Behav. Immun. 2011, 25, 397–407. [Google Scholar] [CrossRef]
- Marin, I.A.; Goertz, J.E.; Ren, T.; Rich, S.S.; Onengut-Gumuscu, S.; Farber, E.; Wu, M.; Overall, C.C.; Kipnis, J.; Gaultier, A. Microbiota alteration is associated with the development of stress-induced despair behavior. Sci. Rep. 2017, 7, 43859. [Google Scholar] [CrossRef]
- Galley, J.D.; Nelson, M.C.; Yu, Z.; Dowd, S.E.; Walter, J.; Kumar, P.S.; Lyte, M.; Bailey, M.T. Exposure to a social stressor disrupts the community structure of the colonic mucosa-associated microbiota. BMC Microbiol. 2014, 14, 189. [Google Scholar] [CrossRef]
- Bailey, M.T.; Coe, C.L. Maternal separation disrupts the integrity of the intestinal microflora in infant rhesus monkeys. Dev. Psychobiol. 1999, 35, 146–155. [Google Scholar] [CrossRef]
- O’Mahony, S.M.; Marchesi, J.R.; Scully, P.; Codling, C.; Ceolho, A.M.; Quigley, E.M.; Cryan, J.F.; Dinan, T.G. Early life stress alters behavior, immunity, and microbiota in rats: Implications for irritable bowel syndrome and psychiatric illnesses. Biol. Psychiatry 2009, 65, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Cao, Q.; Cheng, Y.; Zhao, D.; Wang, Z.; Yang, H.; Wu, Q.; You, L.; Wang, Y.; Lin, Y.; et al. Chronic stress promotes colitis by disturbing the gut microbiota and triggering immune system response. Proc. Natl. Acad. Sci. USA 2018, 115, E2960–E2969. [Google Scholar] [CrossRef] [PubMed]
- Soderholm, J.D.; Yang, P.C.; Ceponis, P.; Vohra, A.; Riddell, R.; Sherman, P.M.; Perdue, M.H. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology 2002, 123, 1099–1108. [Google Scholar] [CrossRef] [PubMed]
- Saunders, P.R.; Santos, J.; Hanssen, N.P.; Yates, D.; Groot, J.A.; Perdue, M.H. Physical and psychological stress in rats enhances colonic epithelial permeability via peripheral CRH. Dig. Dis. Sci. 2002, 47, 208–215. [Google Scholar] [CrossRef]
- Meddings, J.B.; Swain, M.G. Environmental stress-induced gastrointestinal permeability is mediated by endogenous glucocorticoids in the rat. Gastroenterology 2000, 119, 1019–1028. [Google Scholar] [CrossRef]
- Santos, J.; Yang, P.C.; Soderholm, J.D.; Benjamin, M.; Perdue, M.H. Role of mast cells in chronic stress induced colonic epithelial barrier dysfunction in the rat. Gut 2001, 48, 630–636. [Google Scholar] [CrossRef]
- Gareau, M.G.; Sherman, P.M.; Walker, W.A. Probiotics and the gut microbiota in intestinal health and disease. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 503–514. [Google Scholar] [CrossRef]
- Zareie, M.; Johnson-Henry, K.; Jury, J.; Yang, P.C.; Ngan, B.Y.; McKay, D.M.; Soderholm, J.D.; Perdue, M.H.; Sherman, P.M. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut 2006, 55, 1553–1560. [Google Scholar] [CrossRef]
- Garcia-Rodenas, C.L.; Bergonzelli, G.E.; Nutten, S.; Schumann, A.; Cherbut, C.; Turini, M.; Ornstein, K.; Rochat, F.; Corthesy-Theulaz, I. Nutritional approach to restore impaired intestinal barrier function and growth after neonatal stress in rats. J. Pediatr. Gastroenterol. Nutr. 2006, 43, 16–24. [Google Scholar] [CrossRef]
- Noguera, J.C.; Aira, M.; Perez-Losada, M.; Dominguez, J.; Velando, A. Glucocorticoids modulate gastrointestinal microbiome in a wild bird. R. Soc. Open Sci. 2018, 5, 171743. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, S.; Robbe-Masselot, C.; Ait-Belgnaoui, A.; Mancuso, A.; Mercade-Loubiere, M.; Salvador-Cartier, C.; Gillet, M.; Ferrier, L.; Loubiere, P.; Dague, E.; et al. Stress disrupts intestinal mucus barrier in rats via mucin O-glycosylation shift: Prevention by a probiotic treatment. Am. J. Physiol. Gastrointest. Liver Physiol. 2014, 307, G420–G429. [Google Scholar] [CrossRef] [PubMed]
- Walker, L.S.; Garber, J.; Smith, C.A.; Van Slyke, D.A.; Claar, R.L. The relation of daily stressors to somatic and emotional symptoms in children with and without recurrent abdominal pain. J. Consult. Clin. Psychol. 2001, 69, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Zijlmans, M.A.; Korpela, K.; Riksen-Walraven, J.M.; de Vos, W.M.; de Weerth, C. Maternal prenatal stress is associated with the infant intestinal microbiota. Psychoneuroendocrinology 2015, 53, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Kubera, M.; Leunis, J.C.; Berk, M. Increased IgA and IgM responses against gut commensals in chronic depression: Further evidence for increased bacterial translocation or leaky gut. J. Affect. Disord. 2012, 141, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Van der Zaag-Loonen, H.J.; Grootenhuis, M.A.; Last, B.F.; Derkx, H.H. Coping strategies and quality of life of adolescents with inflammatory bowel disease. Qual. Life Res. 2004, 13, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Gianaros, P.J. Central role of the brain in stress and adaptation: Links to socioeconomic status, health, and disease. Ann. N. Y. Acad. Sci. 2010, 1186, 190–222. [Google Scholar] [CrossRef]
- Sudo, N.; Chida, Y.; Aiba, Y.; Sonoda, J.; Oyama, N.; Yu, X.N.; Kubo, C.; Koga, Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J. Physiol. 2004, 558, 263–275. [Google Scholar] [CrossRef]
- Neufeld, K.M.; Kang, N.; Bienenstock, J.; Foster, J.A. Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol. Motil. 2011, 23, 255-e119. [Google Scholar] [CrossRef]
- Diaz Heijtz, R.; Wang, S.; Anuar, F.; Qian, Y.; Bjorkholm, B.; Samuelsson, A.; Hibberd, M.L.; Forssberg, H.; Pettersson, S. Normal gut microbiota modulates brain development and behavior. Proc. Natl. Acad. Sci. USA 2011, 108, 3047–3052. [Google Scholar] [CrossRef]
- Bravo, J.A.; Forsythe, P.; Chew, M.V.; Escaravage, E.; Savignac, H.M.; Dinan, T.G.; Bienenstock, J.; Cryan, J.F. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl. Acad. Sci. USA 2011, 108, 16050–16055. [Google Scholar] [CrossRef] [PubMed]
- Messaoudi, M.; Lalonde, R.; Violle, N.; Javelot, H.; Desor, D.; Nejdi, A.; Bisson, J.F.; Rougeot, C.; Pichelin, M.; Cazaubiel, M.; et al. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br. J. Nutr. 2011, 105, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Wang, Q.; Wang, Y.; Sun, A.; Lin, Y.; Jin, Y.; Li, X. Oral Probiotics Ameliorate the Behavioral Deficits Induced by Chronic Mild Stress in Mice via the Gut Microbiota-Inflammation Axis. Front. Behav. Neurosci. 2018, 12, 266. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Srinivasjois, R.; Patole, S. Prebiotic supplementation in full-term neonates: A systematic review of randomized controlled trials. Arch. Pediatr. Adolesc. Med. 2009, 163, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Dhabhar, F.S. Effects of stress on immune function: The good, the bad, and the beautiful. Immunol. Res. 2014, 58, 193–210. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, K.; Dhabhar, F.S. Stress-induced enhancement of leukocyte trafficking into sites of surgery or immune activation. Proc. Natl. Acad. Sci. USA 2005, 102, 5808–5813. [Google Scholar] [CrossRef]
- Dhabhar, F.S.; Miller, A.H.; McEwen, B.S.; Spencer, R.L. Stress-induced changes in blood leukocyte distribution. Role of adrenal steroid hormones. J. Immunol. 1996, 157, 1638–1644. [Google Scholar]
- Viswanathan, K.; Daugherty, C.; Dhabhar, F.S. Stress as an endogenous adjuvant: Augmentation of the immunization phase of cell-mediated immunity. Int. Immunol. 2005, 17, 1059–1069. [Google Scholar] [CrossRef]
- Maes, M.; Christophe, A.; Bosmans, E.; Lin, A.; Neels, H. In humans, serum polyunsaturated fatty acid levels predict the response of proinflammatory cytokines to psychologic stress. Biol. Psychiatry 2000, 47, 910–920. [Google Scholar] [CrossRef]
- Larson, M.R.; Ader, R.; Moynihan, J.A. Heart rate, neuroendocrine, and immunological reactivity in response to an acute laboratory stressor. Psychosom. Med. 2001, 63, 493–501. [Google Scholar] [CrossRef]
- Schmid-Ott, G.; Jaeger, B.; Meyer, S.; Stephan, E.; Kapp, A.; Werfel, T. Different expression of cytokine and membrane molecules by circulating lymphocytes on acute mental stress in patients with atopic dermatitis in comparison with healthy controls. J. Allergy Clin. Immunol. 2001, 108, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Alsulami, S.; Al Omar, Z.; Binnwejim, M.S.; Alhamdan, F.; Aldrees, A.; Al-Bawardi, A.; Alsohim, M.; Alhabeeb, M. Perception of academic stress among Health Science Preparatory Program students in two Saudi universities. Adv. Med. Educ. Pract. 2018, 9, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Connor, T.J.; Brewer, C.; Kelly, J.P.; Harkin, A. Acute stress suppresses pro-inflammatory cytokines TNF-alpha and IL-1 beta independent of a catecholamine-driven increase in IL-10 production. J. Neuroimmunol. 2005, 159, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Elenkov, I.J. Glucocorticoids and the Th1/Th2 balance. Ann. N. Y. Acad. Sci. 2004, 1024, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Frank, M.G.; Frank, J.L.W.; Hendricks, S.E.; Burke, W.J.; Johnson, D.R. Age at onset of major depressive disorder predicts reductions in NK cell number and activity. J. Affect. Disord. 2002, 71, 159–167. [Google Scholar] [CrossRef]
- Danner, M.; Kasl, S.V.; Abramson, J.L.; Vaccarino, V. Association between depression and elevated C-reactive protein. Psychosom. Med. 2003, 65, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.M.; El-Zaatari, M.; Kao, J.Y. Does stress induce bowel dysfunction? Expert. Rev. Gastroenterol. Hepatol. 2014, 8, 583–585. [Google Scholar] [CrossRef] [PubMed]
- Vrakas, S.; Mountzouris, K.C.; Michalopoulos, G.; Karamanolis, G.; Papatheodoridis, G.; Tzathas, C.; Gazouli, M. Intestinal Bacteria Composition and Translocation of Bacteria in Inflammatory Bowel Disease. PLoS ONE 2017, 12, e0170034. [Google Scholar] [CrossRef] [PubMed]
- Slyepchenko, A.; Maes, M.; Jacka, F.N.; Kohler, C.A.; Barichello, T.; McIntyre, R.S.; Berk, M.; Grande, I.; Foster, J.A.; Vieta, E.; et al. Gut Microbiota, Bacterial Translocation, and Interactions with Diet: Pathophysiological Links between Major Depressive Disorder and Non-Communicable Medical Comorbidities. Psychother. Psychosom. 2017, 86, 31–46. [Google Scholar] [CrossRef] [PubMed]
- Mizoguchi, A.; Takeuchi, T.; Himuro, H.; Okada, T.; Mizoguchi, E. Genetically engineered mouse models for studying inflammatory bowel disease. J. Pathol. 2016, 238, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Read, S.; Asseman, C.; Malmstrom, V.; Mottet, C.; Stephens, L.A.; Stepankova, R.; Tlaskalova, H.; Powrie, F. Control of intestinal inflammation by regulatory T cells. Immunol. Rev. 2001, 182, 190–200. [Google Scholar] [CrossRef] [PubMed]
- Tlaskalova-Hogenova, H.; Tuckova, L.; Stepankova, R.; Hudcovic, T.; Palova-Jelinkova, L.; Kozakova, H.; Rossmann, P.; Sanchez, D.; Cinova, J.; Hrncir, T.; et al. Involvement of innate immunity in the development of inflammatory and autoimmune diseases. Ann. N. Y. Acad. Sci. 2005, 1051, 787–798. [Google Scholar] [CrossRef] [PubMed]
- Rabizadeh, S.; Rhee, K.J.; Wu, S.; Huso, D.; Gan, C.M.; Golub, J.E.; Wu, X.; Zhang, M.; Sears, C.L. Enterotoxigenic bacteroides fragilis: A potential instigator of colitis. Inflamm. Bowel Dis. 2007, 13, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Mahida, Y.R.; Makh, S.; Hyde, S.; Gray, T.; Borriello, S.P. Effect of Clostridium difficile toxin A on human intestinal epithelial cells: Induction of interleukin 8 production and apoptosis after cell detachment. Gut 1996, 38, 337–347. [Google Scholar] [CrossRef] [PubMed]
- Brito, G.A.; Fujji, J.; Carneiro-Filho, B.A.; Lima, A.A.; Obrig, T.; Guerrant, R.L. Mechanism of Clostridium difficile toxin A-induced apoptosis in T84 cells. J. Infect. Dis. 2002, 186, 1438–1447. [Google Scholar] [CrossRef] [PubMed]
- Ghia, J.E.; Blennerhassett, P.; Deng, Y.; Verdu, E.F.; Khan, W.I.; Collins, S.M. Reactivation of inflammatory bowel disease in a mouse model of depression. Gastroenterology 2009, 136, 2280–2288. [Google Scholar] [CrossRef] [PubMed]
- Zamani, S.; Hesam Shariati, S.; Zali, M.R.; Asadzadeh Aghdaei, H.; Sarabi Asiabar, A.; Bokaie, S.; Nomanpour, B.; Sechi, L.A.; Feizabadi, M.M. Detection of enterotoxigenic Bacteroides fragilis in patients with ulcerative colitis. Gut Pathog. 2017, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Issa, M.; Vijayapal, A.; Graham, M.B.; Beaulieu, D.B.; Otterson, M.F.; Lundeen, S.; Skaros, S.; Weber, L.R.; Komorowski, R.A.; Knox, J.F.; et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 2007, 5, 345–351. [Google Scholar] [CrossRef]
- Baumgart, M.; Dogan, B.; Rishniw, M.; Weitzman, G.; Bosworth, B.; Yantiss, R.; Orsi, R.H.; Wiedmann, M.; McDonough, P.; Kim, S.G.; et al. Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn’s disease involving the ileum. ISME J. 2007, 1, 403–418. [Google Scholar] [CrossRef]
- Darfeuille-Michaud, A.; Boudeau, J.; Bulois, P.; Neut, C.; Glasser, A.L.; Barnich, N.; Bringer, M.A.; Swidsinski, A.; Beaugerie, L.; Colombel, J.F. High prevalence of adherent-invasive Escherichia coli associated with ileal mucosa in Crohn’s disease. Gastroenterology 2004, 127, 412–421. [Google Scholar] [CrossRef]
- Ford, D.E.; Erlinger, T.P. Depression and C-reactive protein in US adults: Data from the Third National Health and Nutrition Examination Survey. Arch. Intern. Med. 2004, 164, 1010–1014. [Google Scholar] [CrossRef] [PubMed]
- Tuglu, C.; Kara, S.H.; Caliyurt, O.; Vardar, E.; Abay, E. Increased serum tumor necrosis factor-alpha levels and treatment response in major depressive disorder. Psychopharmacology 2003, 170, 429–433. [Google Scholar] [CrossRef] [PubMed]
- De Punder, K.; Pruimboom, L. Stress induces endotoxemia and low-grade inflammation by increasing barrier permeability. Front. Immunol. 2015, 6, 223. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, W.E.; Palsson, O.; Jones, K.R. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: What are the causes and implications? Gastroenterology 2002, 122, 1140–1156. [Google Scholar] [CrossRef] [PubMed]
- Loftus, E.V., Jr.; Guerin, A.; Yu, A.P.; Wu, E.Q.; Yang, M.; Chao, J.; Mulani, P.M. Increased risks of developing anxiety and depression in young patients with Crohn’s disease. Am. J. Gastroenterol. 2011, 106, 1670–1677. [Google Scholar] [CrossRef] [PubMed]
- Targownik, L.E.; Sexton, K.A.; Bernstein, M.T.; Beatie, B.; Sargent, M.; Walker, J.R.; Graff, L.A. The Relationship Among Perceived Stress, Symptoms, and Inflammation in Persons With Inflammatory Bowel Disease. Am. J. Gastroenterol. 2015, 110, 1001–1012. [Google Scholar] [CrossRef] [PubMed]
- Coskun, M.; Vermeire, S.; Nielsen, O.H. Novel Targeted Therapies for Inflammatory Bowel Disease. Trends Pharmacol. Sci. 2017, 38, 127–142. [Google Scholar] [CrossRef]
- Torres, J.; Ellul, P.; Langhorst, J.; Mikocka-Walus, A.; Barreiro-de Acosta, M.; Basnayake, C.; Ding, N.J.S.; Gilardi, D.; Katsanos, K.; Moser, G.; et al. European Crohn’s and Colitis Organisation Topical Review on Complementary Medicine and Psychotherapy in Inflammatory Bowel Disease. J. Crohns Colitis 2019, 13, 673–685e. [Google Scholar] [CrossRef]
- Regueiro, M.; Greer, J.B.; Szigethy, E. Etiology and Treatment of Pain and Psychosocial Issues in Patients With Inflammatory Bowel Diseases. Gastroenterology 2017, 152, 430–439 e434. [Google Scholar] [CrossRef]
- Baird, C.L.; Sands, L.P. Effect of guided imagery with relaxation on health-related quality of life in older women with osteoarthritis. Res. Nurs. Health 2006, 29, 442–451. [Google Scholar] [CrossRef]
- Garcia-Vega, E.; Fernandez-Rodriguez, C. A stress management programme for Crohn’s disease. Behav. Res. Ther. 2004, 42, 367–383. [Google Scholar] [CrossRef]
- Keefer, L.; Kiebles, J.L.; Martinovich, Z.; Cohen, E.; Van Denburg, A.; Barrett, T.A. Behavioral interventions may prolong remission in patients with inflammatory bowel disease. Behav. Res. Ther. 2011, 49, 145–150. [Google Scholar] [CrossRef] [PubMed]
- McCombie, A.M.; Mulder, R.T.; Gearry, R.B. Psychotherapy for inflammatory bowel disease: A review and update. J. Crohns Colitis 2013, 7, 935–949. [Google Scholar] [CrossRef] [PubMed]
- Vermeire, S.; Van Assche, G.; Rutgeerts, P. C-reactive protein as a marker for inflammatory bowel disease. Inflamm. Bowel Dis. 2004, 10, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Gerbarg, P.L.; Jacob, V.E.; Stevens, L.; Bosworth, B.P.; Chabouni, F.; DeFilippis, E.M.; Warren, R.; Trivellas, M.; Patel, P.V.; Webb, C.D.; et al. The Effect of Breathing, Movement, and Meditation on Psychological and Physical Symptoms and Inflammatory Biomarkers in Inflammatory Bowel Disease: A Randomized Controlled Trial. Inflamm. Bowel Dis. 2015, 21, 2886–2896. [Google Scholar] [CrossRef] [PubMed]
- Neilson, K.; Ftanou, M.; Monshat, K.; Salzberg, M.; Bell, S.; Kamm, M.A.; Connell, W.; Knowles, S.R.; Sevar, K.; Mancuso, S.G.; et al. A Controlled Study of a Group Mindfulness Intervention for Individuals Living With Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2016, 22, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Langhorst, J.; Mueller, T.; Luedtke, R.; Franken, U.; Paul, A.; Michalsen, A.; Schedlowski, M.; Dobos, G.J.; Elsenbruch, S. Effects of a comprehensive lifestyle modification program on quality-of-life in patients with ulcerative colitis: A twelve-month follow-up. Scand. J. Gastroenterol. 2007, 42, 734–745. [Google Scholar] [CrossRef]
- Szigethy, E.; Kenney, E.; Carpenter, J.; Hardy, D.M.; Fairclough, D.; Bousvaros, A.; Keljo, D.; Weisz, J.; Beardslee, W.R.; Noll, R.; et al. Cognitive-behavioral therapy for adolescents with inflammatory bowel disease and subsyndromal depression. J. Am. Acad. Child. Adolesc Psychiatry 2007, 46, 1290–1298. [Google Scholar] [CrossRef]
- Keefer, L.; Kiebles, J.L.; Kwiatek, M.A.; Palsson, O.; Taft, T.H.; Martinovich, Z.; Barrett, T.A. The potential role of a self-management intervention for ulcerative colitis: A brief report from the ulcerative colitis hypnotherapy trial. Biol. Res. Nurs. 2012, 14, 71–77. [Google Scholar] [CrossRef]
- Larsson, K.; Sundberg Hjelm, M.; Karlbom, U.; Nordin, K.; Anderberg, U.M.; Loof, L. A group-based patient education programme for high-anxiety patients with Crohn disease or ulcerative colitis. Scand. J. Gastroenterol. 2003, 38, 763–769. [Google Scholar]
- Smith, G.D.; Watson, R.; Roger, D.; McRorie, E.; Hurst, N.; Luman, W.; Palmer, K.R. Impact of a nurse-led counselling service on quality of life in patients with inflammatory bowel disease. J. Adv. Nurs. 2002, 38, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Maunder, R.G.; Esplen, M.J. Supportive-expressive group psychotherapy for persons with inflammatory bowel disease. Can. J. Psychiatry 2001, 46, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Mizrahi, M.C.; Reicher-Atir, R.; Levy, S.; Haramati, S.; Wengrower, D.; Israeli, E.; Goldin, E. Effects of guided imagery with relaxation training on anxiety and quality of life among patients with inflammatory bowel disease. Psychol Health 2012, 27, 1463–1479. [Google Scholar] [CrossRef] [PubMed]
- Berrill, J.W.; Sadlier, M.; Hood, K.; Green, J.T. Mindfulness-based therapy for inflammatory bowel disease patients with functional abdominal symptoms or high perceived stress levels. J. Crohns Colitis 2014, 8, 945–955. [Google Scholar] [CrossRef] [PubMed]
- Perera, L.P.; Radigan, M.; Guilday, C.; Banerjee, I.; Eastwood, D.; Babygirija, R.; Massey, B.T. Presence of Irritable Bowel Syndrome Symptoms in Quiescent Inflammatory Bowel Disease Is Associated with High Rate of Anxiety and Depression. Dig. Dis. Sci. 2019. [Google Scholar] [CrossRef]
- Gracie, D.J.; Irvine, A.J.; Sood, R.; Mikocka-Walus, A.; Hamlin, P.J.; Ford, A.C. Effect of psychological therapy on disease activity, psychological comorbidity, and quality of life in inflammatory bowel disease: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2017, 2, 189–199. [Google Scholar] [CrossRef]
- Elsenbruch, S.; Langhorst, J.; Popkirowa, K.; Muller, T.; Luedtke, R.; Franken, U.; Paul, A.; Spahn, G.; Michalsen, A.; Janssen, O.E.; et al. Effects of mind-body therapy on quality of life and neuroendocrine and cellular immune functions in patients with ulcerative colitis. Psychother. Psychosom. 2005, 74, 277–287. [Google Scholar] [CrossRef]
- Cheifetz, A.S.; Gianotti, R.; Luber, R.; Gibson, P.R. Complementary and Alternative Medicines Used by Patients With Inflammatory Bowel Diseases. Gastroenterology 2017, 152, 415–429 e415. [Google Scholar] [CrossRef]
- Kimball, E.S.; Schneider, C.R.; Wallace, N.H.; Hornby, P.J. Agonists of cannabinoid receptor 1 and 2 inhibit experimental colitis induced by oil of mustard and by dextran sulfate sodium. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 291, G364–G371. [Google Scholar] [CrossRef]
- Massa, F.; Marsicano, G.; Hermann, H.; Cannich, A.; Monory, K.; Cravatt, B.F.; Ferri, G.L.; Sibaev, A.; Storr, M.; Lutz, B. The endogenous cannabinoid system protects against colonic inflammation. J. Clin. Investig. 2004, 113, 1202–1209. [Google Scholar] [CrossRef]
- Naftali, T.; Lev, L.B.; Yablecovitch, D.; Half, E.; Konikoff, F.M. Treatment of Crohn’s disease with cannabis: An observational study. Isr Med. Assoc. J. 2011, 13, 455–458. [Google Scholar] [PubMed]
- Naftali, T.; Bar-Lev Schleider, L.; Dotan, I.; Lansky, E.P.; Sklerovsky Benjaminov, F.; Konikoff, F.M. Cannabis induces a clinical response in patients with Crohn’s disease: A prospective placebo-controlled study. Clin. Gastroenterol. Hepatol. 2013, 11, 1276–1280 e1271. [Google Scholar] [CrossRef] [PubMed]
- Froicu, M.; Weaver, V.; Wynn, T.A.; McDowell, M.A.; Welsh, J.E.; Cantorna, M.T. A crucial role for the vitamin D receptor in experimental inflammatory bowel diseases. Mol. Endocrinol. 2003, 17, 2386–2392. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, S.P.; Agnholt, J.; Glerup, H.; Lyhne, S.; Villadsen, G.E.; Hvas, C.L.; Bartels, L.E.; Kelsen, J.; Christensen, L.A.; Dahlerup, J.F. Clinical trial: Vitamin D3 treatment in Crohn’s disease—A randomized double-blind placebo-controlled study. Aliment. Pharmacol. Ther. 2010, 32, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Miheller, P.; Muzes, G.; Hritz, I.; Lakatos, G.; Pregun, I.; Lakatos, P.L.; Herszenyi, L.; Tulassay, Z. Comparison of the effects of 1,25 dihydroxyvitamin D and 25 hydroxyvitamin D on bone pathology and disease activity in Crohn’s disease patients. Inflamm. Bowel Dis. 2009, 15, 1656–1662. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N. Vitamin D and Inflammatory Bowel Disease. Gastroenterol. Hepatol. 2016, 12, 513–515. [Google Scholar]
- Pan, Y.; Liu, Y.; Guo, H.; Jabir, M.S.; Liu, X.; Cui, W.; Li, D. Associations between Folate and Vitamin B12 Levels and Inflammatory Bowel Disease: A Meta-Analysis. Nutrients 2017, 9, 382. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, E.M.; Grealy, G.; McCarthy, J.; Desmond, A.; Craig, O.; Shanahan, F.; Cashman, K.D. Effect of phylloquinone (vitamin K1) supplementation for 12 months on the indices of vitamin K status and bone health in adult patients with Crohn’s disease. Br. J. Nutr. 2014, 112, 1163–1174. [Google Scholar] [CrossRef]
- Ng, V.; Millard, W.; Lebrun, C.; Howard, J. Low-intensity exercise improves quality of life in patients with Crohn’s disease. Clin. J. Sport Med. 2007, 17, 384–388. [Google Scholar] [CrossRef]
- Klare, P.; Nigg, J.; Nold, J.; Haller, B.; Krug, A.B.; Mair, S.; Thoeringer, C.K.; Christle, J.W.; Schmid, R.M.; Halle, M.; et al. The impact of a ten-week physical exercise program on health-related quality of life in patients with inflammatory bowel disease: A prospective randomized controlled trial. Digestion 2015, 91, 239–247. [Google Scholar] [CrossRef]
- Sarkar, A.; Lehto, S.M.; Harty, S.; Dinan, T.G.; Cryan, J.F.; Burnet, P.W.J. Psychobiotics and the Manipulation of Bacteria-Gut-Brain Signals. Trends Neurosci. 2016, 39, 763–781. [Google Scholar] [CrossRef] [PubMed]
- Akram, W.; Garud, N.; Joshi, R. Role of inulin as prebiotics on inflammatory bowel disease. Drug Discov. Ther. 2019, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
| Factor | Type of study | N | Intervention/Methodology | Outcome | Author(s) | Reference |
|---|---|---|---|---|---|---|
| Genetics | Clinical study | 637 | Questionnaire | First-degree relatives have 10-fold increased risk of IBD development | Orholm, M. et al. | 37 |
| Meta-analysis | >75,000 cases & controls | GWAS | Identified 30 gene loci for CD and 23 for UC | Jostins, L. et al. | 39 | |
| Trans-ancestry association studies | 238,401 | GWAS | Identified 38 susceptibility loci for IBD | Liu, J.Z. et al. | 40 | |
| Genetic association study | 6228 | Association studies | Identified UPS and CYLD gene are important in IBD pathogenesis | Cleynen, I. et al. | 41 | |
| Genotype association study | 34,819 | Association studies | Insights into genetic heterogeneity between ileal and colonic CD | Cleynen, I. et al. | 42 | |
| Clinical study | 323 | Array-based transcriptome data | Identified 99 strong positional candidate genes in 63 risk loci | Momozawa, Y. et al. | 43 | |
| Clinical study | 189 twin pairs | Questionnaire | Results highlight the importance of environmental triggers | Spehlmann, ME. et al. | 45 | |
| Clinical study | 80 twin pairs | Questionnaire | Genetic influence is stronger in CD than in UC | Halfvarson, J. et al. | 46 | |
| Diet | Interventional, open-label, pilot study | 16 | Vitamin D3 supplementation | Vitamin D3 modulates the gut microbiome | Bashir, M. et al. | 48 |
| In-vivo mouse study | 4–8 mice per group | Oral antibiotics | Increased levels of intracellular zinc led to bacterial clearance | Lahiri, A. et al. | 49 | |
| In-vivo mouse study | 4–5 mice per group | High-fat diet and oral antibiotics | High-fat diet alters gut microbiome composition | Hildebrandt, MA. | 55 | |
| In-vivo mouse study | >100 inbred mouse strains | High-fat/high-sucrose diet | High-fat/high-sucrose diet influences gut microbiota composition | Parks, BW. et al. | 56 | |
| Case-control study | 86 | Dietary intake | Mono- and polyunsaturated fats consumption is a risk factor for IBD | Geerling, BJ. et al. | 57 | |
| In-vivo mouse study | 4–5 mice per group | Diet enriched with phytosterols | Phytosterols are protective against IBD | Aldini, R. et al. | 58 | |
| Environment | Population-based case-control study | 1382 | Questionnaire on 25 different topics | Altered intestinal microbiota may modulate risk of IBD | Ng, SC. et al. | 62 |
| Retrospective case study | 1194 | Clinical history and questionnaire | Higher prevalence of CD in urban areas and UC in inland areas | Carpio, D. et al. | 68 | |
| Smoking | Meta-analysis | 245 articles | Smoking | Smoking is a risk factor for IBD | Mahid, SS. et al. | 51 |
| Prospective case-control study | 160 | Transdermal nicotine or placebo patches | Smoking effects gut microbiota composition | Richardson, CE. et al. | 52 | |
| Medication | Meta-analysis | 11 observational studies | Antibiotic exposure | Antibiotics increases the risk of new-onset CD than UC | Ungaro, R. et al. | 70 |
| Meta-analysis | 20 studies | OCP | Increased risk for development of CD and UC | Ortizo, R. et al. | 71 | |
| Case-control study | 122 | NSAIDs | Provoked disease activity in IBD | Felder, JB. et al. | 72 | |
| Exercise | In-vivo mouse study | 4 mice per group | Exercise training | Alleviated symptoms of acute colitis | Saxena, A. et al. | 60 |
| Prospective cohort study | 194,711 | Physical activity | Inversely associated with risk of CD | Khalili, H. | 61 | |
| Uncontrolled pilot study | 12 | 12-week walking program | Beneficial for IBD patients | Loudon, CP. et al. | 63 | |
| Sleep disturbances | Longitudinal,internet-based cohort data | 3173 | Questionnaire | Increased risk of disease flares in CD but not UC | Ananthakrishnan, AN. et al. | 75 |
| Clinical study | 10 | Disturbances in sleep-wake cycle | Sleep disturbances led to immunologic alterations | Born, J. et al. | 76 | |
| Clinical study | 47 | Questionnaire assessing sleep quality | Impaired sleep quality is associated with pediatric IBD | Mahlmann, L. et al. | 77 | |
| Clinical study | 32 | Questionnaire assessing sleep quality | Impaired quality of life in IBD | Keefer, L. et al. | 78 | |
| Prospective observational cohort study | 41 | Pittsburgh sleep quality index (PSQI) | Strong association between poor sleep quality and IBD | Ali, T. et al. | 79 | |
| In-vivo mouse study | 33 | Diet and sleep disturbances | Circadian disorganization impacts intestinal microbiota | Voigt, RM. et al. | 80 |
| Factor | Type of Study | N | Intervention/Methodology | Outcome | Author(s) | Reference |
|---|---|---|---|---|---|---|
| Prenatal/early life stress | In-vivo mouse study | 6–20 mice per group | Maternal high-fat diet | Dysbiosis and low-grade inflammation in the intestine | Xie, R. et al. | 83 |
| In-vivo rat study | 6–10 per group | Prenatal stress | Long-lasting alterations in the intestinal microbiota composition | Golubeva, AV. et al. | 84 | |
| In-vivo mouse study | 21–23 mice per group | Prenatal stress | Alterations in vaginal microbiota contributed to reprogramming of the developing brain | Jasarevic, E. et al. | 85 | |
| In vivo primates study | 20 | Maternal separation | Maternal separation-induced psychological disturbances altered intestinal microflora | Bailey, MT. et al. | 91 | |
| In-vivo rat study | 22 | Maternal separation | Early life stress induced alterations in gut-brain axis contributing to IBD symptoms | O’Mahony, SM. et al. | 92 | |
| Longitudinal clinical study | 192 children | Questionnaire | Prenatal stress is associated with microbial colonization patterns in infants | Zijlmans, MA. et al. | 104 | |
| Chronic/social/environmental stress | In-vivo mouse study | 7–20 mice per group | Chronic social defeat | Stress induced complex structural changes in the gut microbiota | Bharwani, A. et al. | 81 |
| In-vivo mouse study | 10 mice per group | Lactation | Cellular transfer of bacterial translocation occurred in pregnant and lactating mice | Donnet-Hughes, A. et al. | 87 | |
| In-vivo mouse study | 5 mice per group | SDR | Stress led to significant changes in intestinal microbiota colonization | Bailey, MT. et al. | 88 | |
| In-vivo mouse study | 10–12 (3 independent experiments) | Unpredictable chronic mild stress | Altered intestinal microbiota composition, specifically the lactobacillus compartment | Marin, IA. et al. | 89 | |
| In-vivo mouse study | 5 mice per group | SDR | Affected microbial populations that are closely associated with the colonic mucosa | Galley, JD. et al. | 90 | |
| In-vivo mouse study | 4–6 mice per group | Chronic restraint stress | Disturbed gut microbiota and subsequent activation of immune system led to colitis | Gao, X. et al. | 93 | |
| In-vivo rat study | 7–8 rats per group | WAS | Intestinal inflammation by impaired mucosal defenses against luminal bacteria | Soderholm, JD. et al. | 94 | |
| In-vivo rat study | 6 | Cold-restraint stress or WAS | Exacerbated intestinal inflammation due to increased uptake of immunogenic substances | Saunders, PR. et al. | 95 | |
| In-vivo rat study | not specified | Stress induction | Increased gastrointestinal permeability, allowing luminal constituents to the mucosal immune system | Meddings, JB. et al. | 96 | |
| In-vivo rat study | 4 rats per group | WAS | Stress-induced epithelial mitochondrial damage and mucosal mast cell activation | Santos, J. et al. | 97 | |
| Field experiment in wild birds | 64 | Corticosterone-implant | Altered gut microbiome in free-living birds | Noguera, JC. et al. | 101 | |
| In-vivo rat study | 13–14 rats per group | WAS | Altered intestinal mucus composition | Da Silva, S et al. | 102 | |
| In-vivo mouse study | 18–24 mice per group | Germ-free and specific-pathogen free; acute restraint stress | Commensal microbiota can affect the postnatal development of the HPA stress response | Sudo, N. et al. | 108 | |
| In-vivo mouse study | 12 mice per group | Germ-free and specific-pathogen free | Conventional intestinal microbiota influenced the development of behavior | Neufeld, KM. et al. | 109 | |
| In-vivo mouse study | 7–14 mice per group | Germ-free and specific-pathogen free | Gut microbiota affected mammalian brain development and subsequent adult behavior | Diaz Heijtz, R. et al. | 110 | |
| Clinical study | 263 | Daily interview assessment | Stress is associated with digestive problems and gastrointestinal health | Walker, LS. et al. | 103 | |
| Clinical study | 40 | Depression | Increased bacterial translocation and activated immune responses against commensal bacteria | Maes, M. et al. | 105 | |
| Clinical study | 65 | Coping style instrument | IBD adolescents used more avoidant coping styles compared to healthy controls | Van der Zaag-Loonen, HJ. et al. | 106 | |
| Pro/prebiotics | In-vivo rat study | 4–5 rats per group | WAS and probiotics | Probiotics prevented chronic stress-induced intestinal abnormalities | Zareie, M. et al. | 99 |
| In-vivo rat study | 84 | Maternal separationand prebiotics/probiotics/LC-PUFA | Nutritional intervention at weaning normalized gut permeability and restored growth rate | Garcia-Rodenas, CL. et al. | 100 | |
| In-vivo mouse study | 36 | Probiotic formulation | Suggested the importance of probiotics in gut/brain axis in stress-related disorders | Bravo, JA. et al. | 111 | |
| In-vivo mouse study | 8 mice per group | Chronic mild stress and probiotics | Decreased pro-inflammatory cytokines and altered stress-related behaviors | Li, N. et al. | 113 | |
| In-vivo rat study | 36 rats; | Probiotic formulation | Anxiolytic-like activity in rats | Messaoudi, M. et al. | 112 | |
| Double-blind, placebo-controlled, randomized parallel group study | 66 individuals | Probiotic formulation | Beneficial psychological effects in healthy human volunteers | Messaoudi, M. et al. | 112 | |
| Systematic review | 11 RCTs | Prebiotic supplementation | Short-term beneficial effects in intestinal microbiota composition | Rao, S. et al. | 114 |
| Factor | Type of Study | N | Intervention | Outcome in IBD Patients | Author(s) | Reference |
|---|---|---|---|---|---|---|
| Guided imagery/Relaxation training | Pilot RCT | 28 | Guided imagery with relaxation (GIR) | Improved QL in elderly women with osteoarthritis | Baird, CL. et al. | 150 |
| Prospective RCT | 39 | Relaxation-training | Beneficial effects on anxiety, pain and stress in IBD patients | Mizrahi, MC. et al. | 163 | |
| Self-directed stress management | Clinical study | 45 | 3 types of stress management, including self-directed and conventional medical treatment | Trained CD patients showed reduced fatigue, constipation and abdominal pain, whereas no beneficial effects in conventional-treated CD patients | García-Vega, E. et al. | 151 |
| Lifestyle management | Clinical study | 60 | 60-h training program in lifestyle modification over a period of 10 weeks | Short-term benefits in the QL in UC patients, whereas no long-term effects | Langhorst, J. et al. | 157 |
| Clinical study | 49 | 8-session information about QL and stress management | No effect on anxiety levels 6 months post-intervention | Larsson, K. et al. | 160 | |
| Prospective, randomized waiting-control group design | 30 | 60-h training program on life style management | Improved QL in patients with UC remission | Elsenbruch, S. et al. | 167 | |
| Prospective, randomized study | 32 | Low-intensity walking program | Improved QL of CD patients | Ng, V. et al. | 179 | |
| Prospective RCT | 30 | Moderate-intensity running | Improved QL of IBD patients | Klare, P. et al. | 180 | |
| Psychotherapy | Two clinical trials | 36 | 7-session behavioral protocol | 57% reduction in IBD relapse in the following 12 months | Keefer, L. et al. | 152 |
| RCT | 41 | Primary and Secondary Control Enhancement Therapy-Physical Illness | Beneficial effects on depression in IBD adolescents | Szigethy, E. et al. | 158 | |
| Clinical study | 178 | Nurse-led counselling | Improved QL over 6 rather than 12 months in IBD patients | Smith, GD. et al. | 161 | |
| Prospective, uncontrolled open trial | 30 | Supportive-expressive group psychotherapy | No changes in QL, anxiety, or depression over the course of treatment in UC/CD | Maunder, RG. et al. | 162 | |
| Meta-analysis | 1824 studies with 14 RCTs | Psychological therapy | Small short-term beneficial effects on QL and depression in IBD patients | Gracie, DJ. et al. | 166 | |
| RCT | 29 | Breath-Body-Mind Workshop; questionnaire | Significant long-lasting benefits for IBD symptoms, anxiety, depression and QL | Gerbarg, PL. et al. | 155 | |
| Control study | 60 | Mindfulness-based stress reduction | Improved mood and QL after six months of intervention | Neilson, K. et al. | 156 | |
| RCT | 36 | Gut-directed hypnotherapy | Gut-directed hypnotherapy may be one aspect in a disease-management program for IBD | Keefer, L. et al. | 159 | |
| Clinical trial | 66 | Multi-convergent therapy (psychotherapy) | Therapy is beneficial in the management of IBD symptoms | Berrill, JW. et al. | 164 | |
| Medication | Retrospective observational study | 30 | Herbal treatment | Positive effect of cannabis on disease activity in CD | Naftali, T. et al. | 171 |
| Prospective, placebo-controlled study | 21 | Herbal treatment | Short course of cannabis had beneficial effects in CD patients | Naftali, T. et al. | 172 | |
| Double-blind RCT | 108 | Placebo or vitamin D3 | Reduced relapse risk in CD | Jorgensen, SP. et al. | 174 | |
| Prospective | 37 | Active or plain vitamin D | Active form of vitamin D has short-term beneficial effects in CD | Miheller, P. et al. | 175 | |
| Meta-analysis | 12 studies | Serum folate and vitamin B12 | Low concentration of serum folate is a risk factor for IBD and supplementation may be beneficial | Pan, Y. et al. | 177 | |
| Double-blind RCT | 10 per group | Placebo/ phylloquinone/ vitamin D3 | No significant beneficial effects of phylloquinone on bone health in CD patients | O’Connor EM. et al. | 178 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oligschlaeger, Y.; Yadati, T.; Houben, T.; Condello Oliván, C.M.; Shiri-Sverdlov, R. Inflammatory Bowel Disease: A Stressed “Gut/Feeling”. Cells 2019, 8, 659. https://doi.org/10.3390/cells8070659
Oligschlaeger Y, Yadati T, Houben T, Condello Oliván CM, Shiri-Sverdlov R. Inflammatory Bowel Disease: A Stressed “Gut/Feeling”. Cells. 2019; 8(7):659. https://doi.org/10.3390/cells8070659
Chicago/Turabian StyleOligschlaeger, Yvonne, Tulasi Yadati, Tom Houben, Claudia Maria Condello Oliván, and Ronit Shiri-Sverdlov. 2019. "Inflammatory Bowel Disease: A Stressed “Gut/Feeling”" Cells 8, no. 7: 659. https://doi.org/10.3390/cells8070659
APA StyleOligschlaeger, Y., Yadati, T., Houben, T., Condello Oliván, C. M., & Shiri-Sverdlov, R. (2019). Inflammatory Bowel Disease: A Stressed “Gut/Feeling”. Cells, 8(7), 659. https://doi.org/10.3390/cells8070659





