Carbon Nanotubes as Excellent Adjuvants for Anticancer Therapeutics and Cancer Diagnosis: A Plethora of Laboratory Studies Versus Few Clinical Trials
Abstract
1. Introduction: Carbon Nanotubes in Cancer Therapy
2. Current Synthetic Methods to Obtain CNTs
3. Carbon Nanotubes as Delivery Systems for Anticancer Drugs
3.1. Carbon Nanotube-Based Drug Delivery Systems for Target Anticancer Therapy
3.1.1. Carbon Nanotubes-Based Drug Delivery Systems for the Tumour Microenvironment (TME) and Site-Specific Target Cancer Therapy
3.1.2. Carbon Nanotubes-Based Drug Delivery Systems for the Tumour Microenvironment (TME)-Responsive Release of Chemotherapeutics
4. Carbon Nanotubes Application in Anticancer Phototherapy
4.1. Anticancer Photothermal Therapy
4.2. Anticancer Photodynamic Therapy
4.3. Enhanced Anticancer Phototherapies by CNTs-Improved Drug Delivery
4.4. Application of CNTs for Enhanced Anticancer Combined PTT and PDT
5. Carbon Nanotubes Application in Anticancer Gene Therapy
6. Carbon Nanotubes Application in Anticancer Immunotherapy
7. Carbon Nanotubes Application in Cancer Diagnosis
7.1. Raman Imaging
7.2. Nuclear Magnetic Resonance Imaging
7.3. Ultrasonography
7.4. Photoacoustic Imaging
7.5. Radionuclide Imaging
7.6. Near-Infrared Fluorescence Imaging
7.7. CNTs in Nano Biosensors
7.8. CNTs Combination with Metallic Nanoparticles
7.9. CNTs Combination with Antibody
7.10. CNTs Combination with Peptide Reporter
7.11. CNTs Combination with Multiple Modifications
8. Clinical Translatability and Challenges Concerning CNTs
- The mechanisms of action of CNTs on normal cells and tissues are not fully unveiled.
- Potential toxic effects can occur due to their special structure.
- The mechanisms of CNT-induced toxicity are not fully clarified.
- The biodegradability of raw CNTs is too low because their hydrophobic properties prevent enzymes from approaching them, thus impeding enzymatic degradation.
 ”, “high risk
”, “high risk  ”, or “some concerns
”, or “some concerns  ”, based on specific criteria [319,320]. This assessment process emphasised the importance of transparency and rigour. Using the Cochrane Risk of Bias, two reviewers independently assessed the risk of bias (Table 16).
”, based on specific criteria [319,320]. This assessment process emphasised the importance of transparency and rigour. Using the Cochrane Risk of Bias, two reviewers independently assessed the risk of bias (Table 16).9. Interaction of CNTs with Biomolecules and Tactics to Reduce Their Toxicity
9.1. Interactions of CNTs with Biomolecules
9.2. Tactics to Reduce CNT Toxicity
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Goding Sauer, A.; Fedewa, S.A.; Butterly, L.F.; Anderson, J.C.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal Cancer Statistics, 2020. CA Cancer J. Clin. 2020, 70, 145–164. [Google Scholar] [CrossRef]
- Bray, F.; Laversanne, M.; Weiderpass, E.; Soerjomataram, I. The Ever-increasing Importance of Cancer as a Leading Cause of Premature Death Worldwide. Cancer 2021, 127, 3029–3030. [Google Scholar] [CrossRef]
- Chen, S.; Cao, Z.; Prettner, K.; Kuhn, M.; Yang, J.; Jiao, L.; Wang, Z.; Li, W.; Geldsetzer, P.; Bärnighausen, T.; et al. Estimates and Projections of the Global Economic Cost of 29 Cancers in 204 Countries and Territories from 2020 to 2050. JAMA Oncol. 2023, 9, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Naief, M.F.; Mohammed, S.N.; Mayouf, H.J.; Mohammed, A.M. A Review of the Role of Carbon Nanotubes for Cancer Treatment Based on Photothermal and Photodynamic Therapy Techniques. J. Organomet. Chem. 2023, 999, 122819. [Google Scholar] [CrossRef]
- Klochkov, S.G.; Neganova, M.E.; Nikolenko, V.N.; Chen, K.; Somasundaram, S.G.; Kirkland, C.E.; Aliev, G. Implications of Nanotechnology for the Treatment of Cancer: Recent Advances. Semin. Cancer Biol. 2021, 69, 190–199. [Google Scholar] [CrossRef]
- Chen, K.; Cao, X.; Li, M.; Su, Y.; Li, H.; Xie, M.; Zhang, Z.; Gao, H.; Xu, X.; Han, Y.; et al. A TRAIL-Delivered Lipoprotein-Bioinspired Nanovector Engineering Stem Cell-Based Platform for Inhibition of Lung Metastasis of Melanoma. Theranostics 2019, 9, 2984–2998. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global Cancer Statistics 2022: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef]
- Wang, W.; Chen, K.; Su, Y.; Zhang, J.; Li, M.; Zhou, J. Lysosome-Independent Intracellular Drug/Gene Codelivery by Lipoprotein-Derived Nanovector for Synergistic Apoptosis-Inducing Cancer-Targeted Therapy. Biomacromolecules 2018, 19, 438–448. [Google Scholar] [CrossRef]
- Ganesh, K.; Massagué, J. Targeting Metastatic Cancer. Nat. Med. 2021, 27, 34–44. [Google Scholar] [CrossRef]
- Shakibaie, M.; Hajighasemi, E.; Adeli-Sardou, M.; Doostmohammadi, M.; Forootanfar, H. Antimicrobial and Anti-Biofilm Activities of Bi Subnitrate and BiNPs Produced by Delftia Sp. SFG against Clinical Isolates of Staphylococcus Aureus, Pseudomonas Aeruginosa, and Proteus Mirabilis. IET Nanobiotechnol. 2019, 13, 377–381. [Google Scholar] [CrossRef]
- Mohammed, S.N.; Al-Rawi, K.F.; Mohammed, A.M. Kinetic Evaluation and Study of Gold-Based Nanoparticles and Multi-Walled Carbon Nanotubes as an Alkaline Phosphatase Inhibitor in Serum and Pure Form. Carbon Lett. 2023, 33, 1217–1229. [Google Scholar] [CrossRef]
- faiad naief, M.; Mishaal Mohammed, A.; Khalaf, Y.H. Kinetic and Thermodynamic Study of ALP Enzyme in the Presence and Absence MWCNTs and Pt-NPs Nanocomposites. Results Chem. 2023, 5, 100844. [Google Scholar] [CrossRef]
- Naief, M.F.; Mohammed, S.N.; Ahmed, Y.N.; Mohammed, A.M.; Mohammed, S.N.; Mohammed, S.N. Novel Preparation Method of Fullerene and Its Ability to Detect H2S and NO2 Gases. Results Chem. 2023, 5, 100924. [Google Scholar] [CrossRef]
- Naief, M.F.; Mohammed, S.N.; Ahmed, Y.N.; Mohammed, A.M. Synthesis and Characterisation of MWCNTCOOH and Investigation of Its Potential as Gas Sensor. Inorg. Chem. Commun. 2023, 157, 111338. [Google Scholar] [CrossRef]
- Latif, Z.A.A.; Mohammed, A.M.; Abbass, N.M. Synthesis and Characterization of Polymer Nanocomposites from Methyl Acrylate and Metal Chloride and Their Application. Polym. Bull. 2020, 77, 5879–5898. [Google Scholar] [CrossRef]
- Abdullah, O.H.; Mohammed, A.M. Green Synthesis of Aunps from the Leaf Extract of Prosopis Farcta for Antibacterial and Anti-Cancer Applications. Dig. J. Nanomater. Biostruct. 2020, 15, 943–951. [Google Scholar] [CrossRef]
- Nasir, G.A.; Najm, M.A.; Hussein, A.L. The Effect of Silver Nanoparticles on Braf Gene Expression. Syst. Rev. Pharm. 2020, 11, 570–575. [Google Scholar]
- Mohammed, A.M.; Saud, W.M.; Ali, M.M. Green Synthesis of Fe2O3 Nanoparticles Using Olea Europaea Leaf Extract and Their Antibacterial Activity. Dig. J. Nanomater. Biostruct. 2020, 15, 175–183. [Google Scholar] [CrossRef]
- Jwied, D.H.; Nayef, U.M.; Mutlak, F.A.H. Synthesis of C:Se Nanoparticles Ablated on Porous Silicon for Sensing NO2 and NH3 Gases. Optik 2021, 241, 167013. [Google Scholar] [CrossRef]
- Altaee, M.F.; Yaaqoob, L.A.; Kamona, Z.K. Evaluation of the Biological Activity of Nickel Oxide Nanoparticles as Antibacterial and Anticancer Agents. Iraqi J. Sci. 2020, 61, 2888–2896. [Google Scholar] [CrossRef]
- Ghdeeb, N.J.; AbdulMajeed, A.M.; Mohammed, A.H. Role of Extracted Nano-Metal Oxides from Factory Wastes In Medical Applications. Iraqi J. Sci. 2023, 64, 1704–1716. [Google Scholar] [CrossRef]
- Al-Ali, A.A.A.; Alsalami, K.A.S.; Athbi, A.M. Cytotoxic Effects of CeO2 NPs and β-Carotene and Their Ability to Induce Apoptosis in Human Breast Normal and Cancer Cell Lines. Iraqi J. Sci. 2022, 63, 923–937. [Google Scholar] [CrossRef]
- Salih, A.M.A.; Abdo, G.M. Water Conservation in the Arab Region. In Water, Energy and Food Sustainability in the Middle East: The Sustainability Triangle; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Jiang, D.; Rosenkrans, Z.T.; Ni, D.; Lin, J.; Huang, P.; Cai, W. Nanomedicines for Renal Management: From Imaging to Treatment. Acc. Chem. Res. 2020, 53, 1869–1880. [Google Scholar] [CrossRef]
- Kopeček, J.; Yang, J. Polymer Nanomedicines. Adv. Drug Deliv. Rev. 2020, 156, 40–64. [Google Scholar] [CrossRef]
- Lammers, T.; Sofias, A.M.; van der Meel, R.; Schiffelers, R.; Storm, G.; Tacke, F.; Koschmieder, S.; Brümmendorf, T.H.; Kiessling, F.; Metselaar, J.M. Dexamethasone Nanomedicines for COVID-19. Nat. Nanotechnol. 2020, 15, 622–624. [Google Scholar] [CrossRef] [PubMed]
- Pelaz, B.; Alexiou, C.; Alvarez-Puebla, R.A.; Alves, F.; Andrews, A.M.; Ashraf, S.; Balogh, L.P.; Ballerini, L.; Bestetti, A.; Brendel, C.; et al. Diverse Applications of Nanomedicine. ACS Nano 2017, 11, 2313–2381. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Kantoff, P.W.; Wooster, R.; Farokhzad, O.C. Cancer Nanomedicine: Progress, Challenges and Opportunities. Nat. Rev. Cancer 2017, 17, 20–37. [Google Scholar] [CrossRef]
- Kemp, J.A.; Kwon, Y.J. Cancer Nanotechnology: Current Status and Perspectives. Nano Converg. 2021, 8, 34. [Google Scholar] [CrossRef]
- Bhatia, S.N.; Chen, X.; Dobrovolskaia, M.A.; Lammers, T. Cancer Nanomedicine. Nat. Rev. Cancer 2022, 22, 550–556. [Google Scholar] [CrossRef]
- Zhen, W.; Weichselbaum, R.R.; Lin, W. Nanoparticle-Mediated Radiotherapy Remodels the Tumor Microenvironment to Enhance Antitumor Efficacy. Adv. Mater. 2023, 35, e2206370. [Google Scholar] [CrossRef]
- Su, Z.; Dong, S.; Zhao, S.C.; Liu, K.; Tan, Y.; Jiang, X.; Assaraf, Y.G.; Qin, B.; Chen, Z.S.; Zou, C. Novel Nanomedicines to Overcome Cancer Multidrug Resistance. Drug Resist. Updates 2021, 58, 100777. [Google Scholar] [CrossRef] [PubMed]
- Llop, J.; Lammers, T. Nanoparticles for Cancer Diagnosis, Radionuclide Therapy and Theranostics. ACS Nano 2021, 15, 16974–16981. [Google Scholar] [CrossRef]
- Gerken, L.R.H.; Gerdes, M.E.; Pruschy, M.; Herrmann, I.K. Prospects of Nanoparticle-Based Radioenhancement for Radiotherapy. Mater. Horiz. 2023, 10, 4059–4082. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.; Rashid, S.; Chaudhary, A.A.; Alawam, A.S.; Alghonaim, M.I.; Raza, S.S.; Khan, R. Nanomedicine as Potential Cancer Therapy via Targeting Dysregulated Transcription Factors. Semin. Cancer Biol. 2023, 89, 38–60. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, T.P.; Moreira, J.A.; Monterio, F.J.; Laranjeira, M.S. Nanomaterials in Cancer: Reviewing the Combination of Hyperthermia and Triggered Chemotherapy. J. Control. Release 2022, 347, 89–103. [Google Scholar] [CrossRef]
- Lei, W.; Yang, C.; Wu, Y.; Ru, G.; He, X.; Tong, X.; Wang, S. Nanocarriers Surface Engineered with Cell Membranes for Cancer Targeted Chemotherapy. J. Nanobiotechnol. 2022, 20, 45. [Google Scholar] [CrossRef]
- Bagherifar, R.; Kiaie, S.H.; Hatami, Z.; Ahmadi, A.; Sadeghnejad, A.; Baradaran, B.; Jafari, R.; Javadzadeh, Y. Nanoparticle-Mediated Synergistic Chemoimmunotherapy for Tailoring Cancer Therapy: Recent Advances and Perspectives. J. Nanobiotechnol. 2021, 19, 110. [Google Scholar] [CrossRef]
- Nevins, S.; McLoughlin, C.D.; Oliveros, A.; Stein, J.B.; Rashid, M.A.; Hou, Y.; Jang, M.H.; Lee, K.B. Nanotechnology Approaches for Prevention and Treatment of Chemotherapy-Induced Neurotoxicity, Neuropathy, and Cardiomyopathy in Breast and Ovarian Cancer Survivors. Small 2023, 20, e2300744. [Google Scholar] [CrossRef]
- Wu, W.; Pu, Y.; Shi, J. Nanomedicine-Enabled Chemotherapy-Based Synergetic Cancer Treatments. J. Nanobiotechnol. 2022, 20, 4. [Google Scholar] [CrossRef]
- Wei, G.; Wang, Y.; Yang, G.; Wang, Y.; Ju, R. Recent Progress in Nanomedicine for Enhanced Cancer Chemotherapy. Theranostics 2021, 11, 6370–6392. [Google Scholar] [CrossRef]
- Su, X.; Zhang, X.; Liu, W.; Yang, X.; An, N.; Yang, F.; Sun, J.; Xing, Y.; Shang, H. Advances in the Application of Nanotechnology in Reducing Cardiotoxicity Induced by Cancer Chemotherapy. Semin. Cancer Biol. 2022, 86, 929–942. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M. Cancer Nanotechnology: Opportunities and Challenges. Nat. Rev. Cancer 2005, 5, 161–171. [Google Scholar] [CrossRef] [PubMed]
- van der Meel, R.; Sulheim, E.; Shi, Y.; Kiessling, F.; Mulder, W.J.M.; Lammers, T. Smart Cancer Nanomedicine. Nat. Nanotechnol. 2019, 14, 1007–1017. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Gao, D.; Zhao, J.; Yang, G.; Guo, M.; Wang, Y.; Ren, X.; Kim, J.S.; Jin, L.; Tian, Z.; et al. Thermal Immuno-Nanomedicine in Cancer. Nat. Rev. Clin. Oncol. 2023, 20, 116–134. [Google Scholar] [CrossRef]
- Beg, S.; Kawish, S.M.; Panda, S.K.; Tarique, M.; Malik, A.; Afaq, S.; Al-Samghan, A.S.; Iqbal, J.; Alam, K.; Rahman, M. Nanomedicinal Strategies as Efficient Therapeutic Interventions for Delivery of Cancer Vaccines. Semin. Cancer Biol. 2021, 69, 43–51. [Google Scholar] [CrossRef]
- Rodríguez, F.; Caruana, P.; De la Fuente, N.; Español, P.; Gámez, M.; Balart, J.; Llurba, E.; Rovira, R.; Ruiz, R.; Martín-Lorente, C.; et al. Nano-Based Approved Pharmaceuticals for Cancer Treatment: Present and Future Challenges. Biomolecules 2022, 12, 784. [Google Scholar] [CrossRef]
- Wicki, A.; Witzigmann, D.; Balasubramanian, V.; Huwyler, J. Nanomedicine in Cancer Therapy: Challenges, Opportunities, and Clinical Applications. J. Control. Release 2015, 200, 138–157. [Google Scholar] [CrossRef]
- Blanco, E.; Shen, H.; Ferrari, M. Principles of Nanoparticle Design for Overcoming Biological Barriers to Drug Delivery. Nat. Biotechnol. 2015, 33, 941–951. [Google Scholar] [CrossRef]
- Handa, M.; Beg, S.; Shukla, R.; Barkat, M.A.; Choudhry, H.; Singh, K.K. Recent Advances in Lipid-Engineered Multifunctional Nanophytomedicines for Cancer Targeting. J. Control. Release 2021, 340, 48–59. [Google Scholar] [CrossRef]
- Li, S.; Xu, S.; Liang, X.; Xue, Y.; Mei, J.; Ma, Y.; Liu, Y.; Liu, Y. Nanotechnology: Breaking the Current Treatment Limits of Lung Cancer. Adv. Healthc. Mater. 2021, 10, 2100078. [Google Scholar] [CrossRef]
- Briolay, T.; Petithomme, T.; Fouet, M.; Nguyen-Pham, N.; Blanquart, C.; Boisgerault, N. Delivery of Cancer Therapies by Synthetic and Bio-Inspired Nanovectors. Mol. Cancer 2021, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Votruba, A.R.; Farokhzad, O.C.; Langer, R. Nanotechnology in Drug Delivery and Tissue Engineering: From Discovery to Applications. Nano Lett. 2010, 10, 3223–3230. [Google Scholar] [CrossRef]
- Iijima, S. Helical Microtubules of Graphitic Carbon. Nature 1991, 354, 56–58. [Google Scholar] [CrossRef]
- Alfei, S.; Schito, G.C. Antimicrobial Nanotubes: From Synthesis and Promising Antimicrobial Upshots to Unanticipated Toxicities, Strategies to Limit Them, and Regulatory Issues. Nanomaterials 2025, 15, 633. [Google Scholar] [CrossRef] [PubMed]
- Alfei, S.; Schito, G.C. Nanotubes: Carbon-Based Fibers and Bacterial Nano-Conduits Both Arousing a Global Interest and Conflicting Opinions. Fibers 2022, 10, 75. [Google Scholar] [CrossRef]
- Hussain, A.; Haider, Q.; Rehman, A.; Ahmad, H.; Baili, J.; Aljahdaly, N.H.; Hassan, A. A Thermal Conductivity Model for Hybrid Heat and Mass Transfer Investigation of Single and Multi-Wall Carbon Nano-Tubes Flow Induced by a Spinning Body. Case Stud. Therm. Eng. 2021, 28, 101449. [Google Scholar] [CrossRef]
- Sobamowo, M.G.; Akanmu, J.O.; Adeleye, O.A.; Akingbade, S.A.; Yinusa, A.A. Coupled Effects of Magnetic Field, Number of Walls, Geometric Imperfection, Temperature Change, and Boundary Conditions on Nonlocal Nonlinear Vibration of Carbon Nanotubes Resting on Elastic Foundations. Forces Mech. 2021, 3, 100010. [Google Scholar] [CrossRef]
- Abd-Elsalam, K.A. Carbon Nanomaterials: 30 Years of Research in Agroecosystems. In Carbon Nanomaterials for Agri-Food and Environmental Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 1–18. [Google Scholar]
- Aminul Islam, M.; Hasan, M.; Rahman, M.; Hosne Mobarak, M.; Akter Mimona, M.; Hossain, N. Advances and Significances of Carbon Nanotube Applications: A Comprehensive Review. Eur. Polym. J. 2024, 220, 113443. [Google Scholar] [CrossRef]
- Anzar, N.; Hasan, R.; Tyagi, M.; Yadav, N.; Narang, J. Carbon Nanotube—A Review on Synthesis, Properties and Plethora of Applications in the Field of Biomedical Science. Sens. Int. 2020, 1, 100003. [Google Scholar] [CrossRef]
- Negri, V.; Pacheco-Torres, J.; Calle, D.; López-Larrubia, P. Carbon Nanotubes in Biomedicine. Top. Curr. Chem. 2020, 378, 15. [Google Scholar] [CrossRef]
- Lamberti, M.; Pedata, P.; Sannolo, N.; Porto, S.; De Rosa, A.; Caraglia, M. Carbon Nanotubes: Properties, Biomedical Applications, Advantages and Risks in Patients and Occupationally-Exposed Workers. Int. J. Immunopathol. Pharmacol. 2015, 28, 4–13. [Google Scholar] [CrossRef]
- Kumar, S.; Rani, R.; Dilbaghi, N.; Tankeshwar, K.; Kim, K.-H. Carbon Nanotubes: A Novel Material for Multifaceted Applications in Human Healthcare. Chem. Soc. Rev. 2017, 46, 158–196. [Google Scholar] [CrossRef]
- Su, Q.; Gan, L.; Liu, J.; Yang, X. Carbon Dots Derived from Pea for Specifically Binding with Cryptococcus Neoformans. Anal. Biochem. 2020, 589, 113476. [Google Scholar] [CrossRef] [PubMed]
- Salari, S.; Jafari, S.M. Application of Nanofluids for Thermal Processing of Food Products. Trends Food Sci. Technol. 2020, 97, 100–113. [Google Scholar] [CrossRef]
- Chen, D.; Dougherty, C.A.; Zhu, K.; Hong, H. Theranostic Applications of Carbon Nanomaterials in Cancer: Focus on Imaging and Cargo Delivery. J. Control. Release 2015, 210, 230–245. [Google Scholar] [CrossRef] [PubMed]
- Law, S.K.; Leung, A.W.N.; Xu, C.; Au, D.C.T. Is It Possible for Curcumin to Conjugate with a Carbon Nanotube in Photodynamic Therapy? Photodiagnosis Photodyn. Ther. 2022, 40, 103189. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, M.A.; Jeon, J.Y.; Ha, T.J. Carbon Nanotubes: An Effective Platform for Biomedical Electronics. Biosens. Bioelectron. 2020, 150, 111919. [Google Scholar] [CrossRef]
- Ijaz, H.; Mahmood, A.; Abdel-Daim, M.M.; Sarfraz, R.M.; Zaman, M.; Zafar, N.; Alshehery, S.; Salem-Bekhit, M.M.; Ali, M.A.; Eltayeb, L.B.; et al. Review on carbon nanotubes (CNTs) and their chemical and physical characteristics, with particular emphasis on potential applications in biomedicine. Inorg. Chem. Commun. 2023, 155, 111020. [Google Scholar] [CrossRef]
- Vashist, A.; Kaushik, A.; Vashist, A.; Sagar, V.; Ghosal, A.; Gupta, Y.K.; Ahmad, S.; Nair, M. Advances in Carbon Nanotubes–Hydrogel Hybrids in Nanomedicine for Therapeutics. Adv. Healthc. Mater. 2018, 7, e1701213. [Google Scholar] [CrossRef]
- Zhang, J.; Liu, Z.; Zhou, S.; Teng, Y.; Zhang, X.; Li, J. Novel Span-PEG Multifunctional Ultrasound Contrast Agent Based on CNTs as a Magnetic Targeting Factor and a Drug Carrier. ACS Omega 2020, 5, 31525–31534. [Google Scholar] [CrossRef]
- Garriga, R.; Herrero-Continente, T.; Palos, M.; Cebolla, V.L.; Osada, J.; Muñoz, E.; Rodríguez-Yoldi, M.J. Toxicity of Carbon Nanomaterials and Their Potential Application as Drug Delivery Systems: In Vitro Studies in Caco-2 and Mcf-7 Cell Lines. Nanomaterials 2020, 10, 1617. [Google Scholar] [CrossRef] [PubMed]
- Corletto, A.; Shapter, J.G. Nanoscale Patterning of Carbon Nanotubes: Techniques, Applications, and Future. Adv. Sci. 2021, 8, 2001778. [Google Scholar] [CrossRef] [PubMed]
- Azizi-Lalabadi, M.; Hashemi, H.; Feng, J.; Jafari, S.M. Carbon Nanomaterials against Pathogens; the Antimicrobial Activity of Carbon Nanotubes, Graphene/Graphene Oxide, Fullerenes, and Their Nanocomposites. Adv. Colloid. Interface Sci. 2020, 284, 102250. [Google Scholar] [CrossRef]
- Alfei, S.; Zuccari, G. Carbon-Nanotube-Based Nanocomposites in Environmental Remediation: An Overview of Typologies and Applications and an Analysis of Their Paradoxical Double-Sided Effects. J. Xenobiot. 2025, 15, 76. [Google Scholar] [CrossRef]
- Griffiths, O.G.; O’Byrne, J.P.; Torrente-Murciano, L.; Jones, M.D.; Mattia, D.; McManus, M.C. Identifying the Largest Environmental Life Cycle Impacts during Carbon Nanotube Synthesis via Chemical Vapour Deposition. J. Clean. Prod. 2013, 42, 180–189. [Google Scholar] [CrossRef]
- Wang, Z.; Shen, D.; Wu, C.; Gu, S. State-of-the-Art on the Production and Application of Carbon Nanomaterials from Biomass. Green Chem. 2018, 20, 5031–5057. [Google Scholar] [CrossRef]
- Berber, M.R.; Elkhenany, H.; Hafez, I.H.; El-Badawy, A.; Essawy, M.; El-Badri, N. Efficient Tailoring of Platinum Nanoparticles Supported on Multiwalled Carbon Nanotubes for Cancer Therapy. Nanomedicine 2020, 15, 793–808. [Google Scholar] [CrossRef]
- Zhang, J.; Song, L.; Zhou, S.; Hu, M.; Jiao, Y.; Teng, Y.; Wang, Y.; Zhang, X. Enhanced Ultrasound Imaging and Anti-Tumor: In Vivo Properties of Span-Polyethylene Glycol with Folic Acid-Carbon Nanotube-Paclitaxel Multifunctional Microbubbles. RSC Adv. 2019, 9, 35345–35355. [Google Scholar] [CrossRef]
- Behzadpour, N.; Ranjbar, A.; Azarpira, N.; Sattarahmady, N. Development of a Composite of Polypyrrole-Coated Carbon Nanotubes as a Sonosensitizer for Treatment of Melanoma Cancer Under Multi-Step Ultrasound Irradiation. Ultrasound Med. Biol. 2020, 46, 2322–2334. [Google Scholar] [CrossRef]
- Zhang, B.; Wang, H.; Shen, S.; She, X.; Shi, W.; Chen, J.; Zhang, Q.; Hu, Y.; Pang, Z.; Jiang, X. Fibrin-Targeting Peptide CREKA-Conjugated Multi-Walled Carbon Nanotubes for Self-Amplified Photothermal Therapy of Tumor. Biomaterials 2016, 79, 46–55. [Google Scholar] [CrossRef]
- Sobhani, Z.; Behnam, M.A.; Emami, F.; Dehghanian, A.; Jamhiri, I. Photothermal Therapy of Melanoma Tumor Using Multiwalled Carbon Nanotubes. Int. J. Nanomed. 2017, 12, 4509–4517. [Google Scholar] [CrossRef]
- Bosca, F.; Corazzari, I.; Foglietta, F.; Canaparo, R.; Durando, G.; Pastero, L.; Arpicco, S.; Dosio, F.; Zonari, D.; Cravotto, G.; et al. SWCNT-Porphyrin Nano-Hybrids Selectively Activated by Ultrasound: An Interesting Model for Sonodynamic Applications. RSC Adv. 2020, 10, 21736–21744. [Google Scholar] [CrossRef]
- Singh, R.; Kumar, S. Cancer Targeting and Diagnosis: Recent Trends with Carbon Nanotubes. Nanomaterials 2022, 12, 2283. [Google Scholar] [CrossRef] [PubMed]
- Faraji Dizaji, B.; Khoshbakht, S.; Farboudi, A.; Azarbaijan, M.H.; Irani, M. Far-Reaching Advances in the Role of Carbon Nanotubes in Cancer Therapy. Life Sci. 2020, 257, 118059. [Google Scholar] [CrossRef]
- Yadav, P.; Ambudkar, S.V.; Rajendra Prasad, N. Emerging nanotechnology-based therapeutics to combat multidrug-resistant cancer. J. Nanobiotechnol. 2022, 20, 423. [Google Scholar] [CrossRef]
- Zhang, Y.R.; Lin, R.; Li, H.J.; He, W.L.; Du, J.Z.; Wang, J. Strategies to Improve Tumor Penetration of Nanomedicines through Nanoparticle Design. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2019, 11, e1519. [Google Scholar] [CrossRef]
- Zhang, A.; Meng, K.; Liu, Y.; Pan, Y.; Qu, W.; Chen, D.; Xie, S. Absorption, Distribution, Metabolism, and Excretion of Nanocarriers in Vivo and Their Influences. Adv. Colloid Interface Sci. 2020, 284, 102261. [Google Scholar] [CrossRef]
- Zare, H.; Ahmadi, S.; Ghasemi, A.; Ghanbari, M.; Rabiee, N.; Bagherzadeh, M.; Karimi, M.; Webster, T.J.; Hamblin, M.R.; Mostafavi, E. Carbon Nanotubes: Smart Drug/Gene Delivery Carriers. Int. J. Nanomed. 2021, 16, 1681–1706. [Google Scholar] [CrossRef]
- Taghavi, S.; Nia, A.H.; Abnous, K.; Ramezani, M. Polyethylenimine-Functionalized Carbon Nanotubes Tagged with AS1411 Aptamer for Combination Gene and Drug Delivery into Human Gastric Cancer Cells. Int. J. Pharm. 2017, 516, 301–312. [Google Scholar] [CrossRef]
- Huang, Y.P.; Lin, I.J.; Chen, C.C.; Hsu, Y.C.; Chang, C.C.; Lee, M.J. Delivery of Small Interfering RNAs in Human Cervical Cancer Cells by Polyethylenimine-Functionalized Carbon Nanotubes. Nanoscale Res. Lett. 2013, 8, 267. [Google Scholar] [CrossRef]
- Bhirde, A.A.; Chikkaveeraiah, B.V.; Srivatsan, A.; Niu, G.; Jin, A.J.; Kapoor, A.; Wang, Z.; Patel, S.; Patel, V.; Gorbach, A.M.; et al. Targeted Therapeutic Nanotubes Influence the Viscoelasticity of Cancer Cells to Overcome Drug Resistance. ACS Nano 2014, 8, 4177–4189. [Google Scholar] [CrossRef]
- Dong, X.; Liu, L.; Zhu, D.; Zhang, H.; Leng, X. Transactivator of Transcription (TAT) Peptide– Chitosan Functionalized Multiwalled Carbon Nanotubes as a Potential Drug Delivery Vehicle for Cancer Therapy. Int. J. Nanomed. 2015, 10, 3829–3841. [Google Scholar] [CrossRef]
- Cheng, Q.; Blais, M.O.; Harris, G.M.; Jabbarzadeh, E. Correction: PLGA-Carbon Nanotube Conjugates for Intercellular Delivery of Caspase-3 into Osteosarcoma Cells. PLoS ONE 2013, 8, e81947. [Google Scholar] [CrossRef]
- Wang, C.H.; Chiou, S.H.; Chou, C.P.; Chen, Y.C.; Huang, Y.J.; Peng, C.A. Photothermolysis of Glioblastoma Stem-like Cells Targeted by Carbon Nanotubes Conjugated with CD133 Monoclonal Antibody. Nanomedicine 2011, 7, 69–79. [Google Scholar] [CrossRef]
- Shao, N.; Lu, S.; Wickstrom, E.; Panchapakesan, B. Integrated Molecular Targeting of IGF1R and HER2 Surface Receptors and Destruction of Breast Cancer Cells Using Single Wall Carbon Nanotubes. Nanotechnology 2007, 18, 315101. [Google Scholar] [CrossRef]
- Koh, B.; Park, S.B.; Yoon, E.; Yoo, H.M.; Lee, D.; Heo, J.N.; Ahn, S. AVβ3-Targeted Delivery of Camptothecin-Encapsulated Carbon Nanotube-Cyclic RGD in 2D and 3D Cancer Cell Culture. J. Pharm. Sci. 2019, 108, 3704–3712. [Google Scholar] [CrossRef]
- Bhirde, A.A.; Patel, V.; Gavard, J.; Zhang, G.; Sousa, A.A.; Masedunskas, A.; Leapman, R.D.; Weigert, R.; Gutkind, J.S.; Rusling, J.F. Targeted Killing of Cancer Cells in Vivo and in Vitro with EGF-Directed Carbon Nanotube-Based Drug Delivery. ACS Nano 2009, 3, 307–316. [Google Scholar] [CrossRef]
- Yang, S.; Wang, Z.; Ping, Y.; Miao, Y.; Xiao, Y.; Qu, L.; Zhang, L.; Hu, Y.; Wang, J. PEG/PEI-Functionalized Single-Walled Carbon Nanotubes as Delivery Carriers for Doxorubicin: Synthesis, Characterization, and in Vitro Evaluation. Beilstein J. Nanotechnol. 2020, 11, 1728–1741. [Google Scholar] [CrossRef]
- Liu, Z.; Sun, X.; Nakayama-Ratchford, N.; Dai, H. Supramolecular Chemistry on Water-Soluble Carbon Nanotubes for Drug Loading and Delivery. ACS Nano 2007, 1, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Rahamathulla, M.; Bhosale, R.R.; Osmani, R.A.M.; Mahima, K.C.; Johnson, A.P.; Hani, U.; Ghazwani, M.; Begum, M.Y.; Alshehri, S.; Ghoneim, M.M.; et al. Carbon Nanotubes: Current Perspectives on Diverse Applications in Targeted Drug Delivery and Therapies. Materials 2021, 14, 6707. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, S.; Patharkar, A.; Kuche, K.; Maheshwari, R.; Deb, P.K.; Kalia, K.; Tekade, R.K. Functionalized Carbon Nanotubes as Emerging Delivery System for the Treatment of Cancer. Int. J. Pharm. 2018, 548, 540–558. [Google Scholar] [CrossRef] [PubMed]
- Barzegar, A.; Mansouri, A.; Azamat, J. Molecular Dynamics Simulation of Non-Covalent Single-Walled Carbon Nanotube Functionalization with Surfactant Peptides. J. Mol. Graph. Model. 2016, 64, 75–84. [Google Scholar] [CrossRef]
- Hasnain, M.S.; Ahmad, S.A.; Hoda, M.N.; Rishishwar, S.; Rishishwar, P.; Nayak, A.K. Stimuli-Responsive Carbon Nanotubes for Targeted Drug Delivery. In Stimuli Responsive Polymeric Nanocarriers for Drug Delivery Applications: Volume 2: Advanced Nanocarriers for Therapeutics; Elsevier: Amsterdam, The Netherlands, 2019; pp. 321–344. [Google Scholar] [CrossRef]
- Cao, X.; Tao, L.; Wen, S.; Hou, W.; Shi, X. Hyaluronic Acid-Modified Multiwalled Carbon Nanotubes for Targeted Delivery of Doxorubicin into Cancer Cells. Carbohydr. Res. 2015, 405, 70–77. [Google Scholar] [CrossRef]
- Gu, Y.J.; Cheng, J.; Jin, J.; Cheng, S.H.; Wong, W.T. Development and Evaluation of PH-Responsive Single-Walled Carbon Nanotube-Doxorubicin Complexes in Cancer Cells. Int. J. Nanomed. 2011, 6, 2889–2898. [Google Scholar] [CrossRef]
- Fernández, M.; Javaid, F.; Chudasama, V. Advances in Targeting the Folate Receptor in the Treatment/Imaging of Cancers. Chem. Sci. 2018, 9, 790–810. [Google Scholar] [CrossRef]
- Lu, Y.J.; Wei, K.C.; Ma, C.C.M.; Yang, S.Y.; Chen, J.P. Dual Targeted Delivery of Doxorubicin to Cancer Cells Using Folate-Conjugated Magnetic Multi-Walled Carbon Nanotubes. Colloids Surf. B Biointerfaces 2012, 89, 1–9. [Google Scholar] [CrossRef]
- Feazell, R.P.; Nakayama-Ratchford, N.; Dai, H.; Lippard, S.J. Soluble Single-Walled Carbon Nanotubes as Longboat Delivery Systems for Platinum(IV) Anticancer Drug Design. J. Am. Chem. Soc. 2007, 129, 8438–8439. [Google Scholar] [CrossRef]
- Hampel, S.; Kunze, D.; Haase, D.; Krämer, K.; Rauschenbach, M.; Ritschel, M.; Leonhardt, A.; Thomas, J.; Oswald, S.; Hoffmann, V.; et al. Carbon Nanotubes Filled with a Chemotherapeutic Agent: A Nanocarrier Mediates Inhibition of Tumor Cell Growth. Nanomedicine 2008, 3, 175–182. [Google Scholar] [CrossRef]
- Wu, L.; Man, C.; Wang, H.; Lu, X.; Ma, Q.; Cai, Y.; Ma, W. PEGylated Multi-Walled Carbon Nanotubes for Encapsulation and Sustained Release of Oxaliplatin. Pharm. Res. 2013, 30, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Xu, H.; Wang, Y.; He, Z.; Li, S. Effect of Intratumoral Injection on the Biodistribution and Therapeutic Potential of Novel Chemophor EL-Modified Single-Walled Nanotube Loading Doxorubicin. Drug Dev. Ind. Pharm. 2012, 38, 1031–1038. [Google Scholar] [CrossRef] [PubMed]
- Ali-Boucetta, H.; Al-Jamal, K.T.; McCarthy, D.; Prato, M.; Bianco, A.; Kostarelos, K. Multiwalled Carbon Nanotube-Doxorubicin Supramolecular Complexes for Cancer Therapeutics. Chem. Commun. 2002, 8, 459–461. [Google Scholar] [CrossRef]
- Li, R.; Wu, R.; Zhao, L.; Wu, M.; Yang, L.; Zou, H. P-Glycoprotein Antibody Functionalized Carbon Nanotube Overcomes the Multidrug Resistance of Human Leukemia Cells. ACS Nano 2010, 4, 1399–1408. [Google Scholar] [CrossRef]
- Arya, N.; Arora, A.; Vasu, K.S.; Sood, A.K.; Katti, D.S. Combination of Single Walled Carbon Nanotubes/Graphene Oxide with Paclitaxel: A Reactive Oxygen Species Mediated Synergism for Treatment of Lung Cancer. Nanoscale 2013, 5, 2818–2829. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Meng, L.; Lu, Q.; Fei, Z.; Dyson, P.J. Targeted Delivery and Controlled Release of Doxorubicin to Cancer Cells Using Modified Single Wall Carbon Nanotubes. Biomaterials 2009, 30, 6041–6047. [Google Scholar] [CrossRef] [PubMed]
- Atyabi, F.; Sobhani; Adeli, M.; Dinarvand, R. Ghahremani Increased Paclitaxel Cytotoxicity against Cancer Cell Lines Using a Novel Functionalized Carbon Nanotube. Int. J. Nanomed. 2011, 6, 705–719. [Google Scholar] [CrossRef]
- Liu, Z.; Chen, K.; Davis, C.; Sherlock, S.; Cao, Q.; Chen, X.; Dai, H. Drug Delivery with Carbon Nanotubes for in Vivo Cancer Treatment. Cancer Res. 2008, 68, 6652–6660. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Chen, S.; Zhao, X.; Kuznetsova, L.V.; Wong, S.S.; Ojima, I. Functionalized Single-Walled Carbon Nanotubes as Rationally Designed Vehicles for Tumor-Targeted Drug Delivery. J. Am. Chem. Soc. 2008, 130, 16778–16785. [Google Scholar] [CrossRef]
- Razzazan, A.; Atyabi, F.; Kazemi, B.; Dinarvand, R. In Vivo Drug Delivery of Gemcitabine with PEGylated Single-Walled Carbon Nanotubes. Mater. Sci. Eng. C 2016, 62, 614–625. [Google Scholar] [CrossRef]
- Bartholomeusz, G.; Cherukuri, P.; Kingston, J.; Cognet, L.; Lemos, R.; Leeuw, T.K.; Gumbiner-Russo, L.; Weisman, R.B.; Powis, G. In Vivo Therapeutic Silencing of Hypoxia-Inducible Factor 1 Alpha (HIF-1α) Using Single-Walled Carbon Nanotubes Noncovalently Coated with SiRNA. Nano Res. 2009, 2, 279–291. [Google Scholar] [CrossRef]
- Varkouhi, A.K.; Foillard, S.; Lammers, T.; Schiffelers, R.M.; Doris, E.; Hennink, W.E.; Storm, G. SiRNA Delivery with Functionalized Carbon Nanotubes. Int. J. Pharm. 2011, 416, 419–425. [Google Scholar] [CrossRef]
- Wang, X.; Ren, J.; Qu, X. Targeted RNA Interference of Cyclin A2 Mediated by Functionalized Single-Walled Carbon Nanotubes Induces Proliferation Arrest and Apoptosis in Chronic Myelogenous Leukemia K562 Cells. ChemMedChem 2008, 3, 940–945. [Google Scholar] [CrossRef]
- Guo, C.; Al-Jamal, W.T.; Toma, F.M.; Bianco, A.; Prato, M.; Al-Jamal, K.T.; Kostarelos, K. Design of Cationic Multiwalled Carbon Nanotubes as Efficient SiRNA Vectors for Lung Cancer Xenograft Eradication. Bioconjugate Chem. 2015, 26, 1370–1379. [Google Scholar] [CrossRef]
- Singh, P.; Samorì, C.; Toma, F.M.; Bussy, C.; Nunes, A.; Al-Jamal, K.T.; Ménard-Moyon, C.; Prato, M.; Kostarelos, K.; Bianco, A. Polyamine Functionalized Carbon Nanotubes: Synthesis, Characterization, Cytotoxicity and SiRNA Binding. J. Mater. Chem. 2011, 21, 4850–4860. [Google Scholar] [CrossRef]
- Mohammadi, M.; Salmasi, Z.; Hashemi, M.; Mosaffa, F.; Abnous, K.; Ramezani, M. Single-Walled Carbon Nanotubes Functionalized with Aptamer and Piperazine-Polyethylenimine Derivative for Targeted SiRNA Delivery into Breast Cancer Cells. Int. J. Pharm. 2015, 485, 50–60. [Google Scholar] [CrossRef]
- Al-Jamal, K.T.; Toma, F.M.; Yilmazer, A.; Ali-Boucetta, H.; Nunes, A.; Herrero, M.A.; Tian, B.; Eddaoui, A.; Al-Jamal, W.; Bianco, A.; et al. Enhanced Cellular Internalization and Gene Silencing with a Series of Cationic Dendron-Multiwalled Carbon Nanotube:SiRNA Complexes. FASEB J. 2010, 24, 4354–4365. [Google Scholar] [CrossRef]
- Podesta, J.E.; Al-Jamal, K.T.; Herrero, M.A.; Tian, B.; Ali-Boucetta, H.; Hegde, V.; Bianco, A.; Prato, M.; Kostarelos, K. Antitumor Activity and Prolonged Survival by Carbon-Nanotube-Mediated Therapeutic Sirna Silencing in a Human Lung Xenograft Model. Small 2009, 5, 1176–1185. [Google Scholar] [CrossRef]
- Battigelli, A.; Wang, J.T.W.; Russier, J.; Da Ros, T.; Kostarelos, K.; Al-Jamal, K.T.; Prato, M.; Bianco, A. Ammonium and Guanidinium Dendron-Carbon Nanotubes by Amidation and Click Chemistry and Their Use for SiRNA Delivery. Small 2013, 9, 3610–3619. [Google Scholar] [CrossRef]
- Ren, X.; Lin, J.; Wang, X.; Liu, X.; Meng, E.; Zhang, R.; Sang, Y.; Zhang, Z. Photoactivatable RNAi for cancer gene therapy triggered by near-infrared-irradiated single-walled carbon nanotubes. Int. J. Nanomed. 2017, 12, 7885–7896. [Google Scholar] [CrossRef]
- Ahmed, M.; Jiang, X.; Deng, Z.; Narain, R. Cationic Glyco-Functionalized Single-Walled Carbon Nanotubes as Efficient Gene Delivery Vehicles. Bioconjugate Chem. 2009, 20, 2017–2022. [Google Scholar] [CrossRef]
- Karmakar, A.; Braton, S.M.; Dervishi, E.; Ghosh, A.; Mahmood, M.; Xu, Y.; Saeed, L.M.; Mustafa, T.; Casciano, D.; Radominska-Pandya, A.; et al. Ethylenediamine Functionalized-Single-Walled Nanotube (f-SWNT)-Assisted in Vitro Delivery of the Oncogene Suppressor P53 Gene to Breast Cancer MCF-7 Cells. Int. J. Nanomed. 2011, 6, 1045–1055. [Google Scholar] [CrossRef]
- Pantarotto, D.; Singh, R.; McCarthy, D.; Erhardt, M.; Briand, J.P.; Prato, M.; Kostarelos, K.; Bianco, A. Functionalized Carbon Nanotubes for Plasmid DNA Gene Delivery. Angew. Chem. Int. Ed. 2004, 43, 5242–5246. [Google Scholar] [CrossRef]
- Qin, W.; Yang, K.; Tang, H.; Tan, L.; Xie, Q.; Ma, M.; Zhang, Y.; Yao, S. Improved GFP Gene Transfection Mediated by Polyamidoamine Dendrimer-Functionalized Multi-Walled Carbon Nanotubes with High Biocompatibility. Colloids Surf. B Biointerfaces 2011, 84, 206–213. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, Z.; Liu, Z.; Ma, Y.; Yang, R.; Chen, Y. Multi-Functionalized Single-Walled Carbon Nanotubes as Tumor Cell Targeting Biological Transporters. J. Nanoparticle Res. 2008, 10, 815–822. [Google Scholar] [CrossRef]
- Dong, H.; Ding, L.; Yan, F.; Ji, H.; Ju, H. The Use of Polyethylenimine-Grafted Graphene Nanoribbon for Cellular Delivery of Locked Nucleic Acid Modified Molecular Beacon for Recognition of MicroRNA. Biomaterials 2011, 32, 3875–3882. [Google Scholar] [CrossRef]
- Crinelli, R.; Carloni, E.; Menotta, M.; Giacomini, E.; Bianchi, M.; Ambrosi, G.; Giorgi, L.; Magnani, M. Oxidized Ultrashort Nanotubes as Carbon Scaffolds for the Construction of Cell-Penetrating NF-ΚB Decoy Molecules. ACS Nano 2010, 4, 2791–2803. [Google Scholar] [CrossRef]
- Pan, B.; Cui, D.; Xu, P.; Ozkan, C.; Feng, G.; Ozkan, M.; Huang, T.; Chu, B.; Li, Q.; He, R.; et al. Synthesis and Characterization of Polyamidoamine Dendrimer-Coated Multi-Walled Carbon Nanotubes and Their Application in Gene Delivery Systems. Nanotechnology 2009, 20, 125101. [Google Scholar] [CrossRef]
- Van Den Bossche, J.; Al-Jamal, W.T.; Tian, B.; Nunes, A.; Fabbro, C.; Bianco, A.; Prato, M.; Kostarelos, K. Efficient Receptor-Independent Intracellular Translocation of Aptamers Mediated by Conjugation to Carbon Nanotubes. Chem. Commun. 2010, 46, 7379–7381. [Google Scholar] [CrossRef]
- Yan, Y.; Wang, R.; Hu, Y.; Sun, R.; Song, T.; Shi, X.; Yin, S. Stacking of Doxorubicin on Folic Acid-Targeted Multiwalled Carbon Nanotubes for in Vivo Chemotherapy of Tumors. Drug Deliv. 2018, 25, 1607–1616. [Google Scholar] [CrossRef]
- Li, J.; Du, Y.; Su, H.; Cheng, S.; Zhou, Y.; Jin, Y.; Qi, X.R. Interfacial Properties and Micellization of Triblock Poly(Ethylene Glycol)-Poly(ε-Caprolactone)-Polyethyleneimine Copolymers. Acta Pharm. Sin. B 2020, 10, 1122–1133. [Google Scholar] [CrossRef]
- Sohrabi, N.; Alihosseini, A.; Pirouzfar, V.; Pedram, M.Z. Analysis of Dynamics Targeting CNT-Based Drug Delivery through Lung Cancer Cells: Design, Simulation, and Computational Approach. Membranes 2020, 10, 283. [Google Scholar] [CrossRef]
- Cao, Y.; Huang, H.Y.; Chen, L.Q.; Du, H.H.; Cui, J.H.; Zhang, L.W.; Lee, B.J.; Cao, Q.R. Enhanced Lysosomal Escape of PH-Responsive Polyethylenimine-Betaine Functionalized Carbon Nanotube for the Codelivery of Survivin Small Interfering RNA and Doxorubicin. ACS Appl. Mater. Interfaces 2019, 11, 9763–9776. [Google Scholar] [CrossRef]
- Chen, W.; Yang, S.; Wei, X.; Yang, Z.; Liu, D.; Pu, X.; He, S.; Zhang, Y. Construction of Aptamer-SiRNA Chimera/PEI/5-FU/Carbon Nanotube/Collagen Membranes for the Treatment of Peritoneal Dissemination of Drug-Resistant Gastric Cancer. Adv. Healthc. Mater. 2020, 9, e2001153. [Google Scholar] [CrossRef]
- González-Domínguez, J.M.; Grasa, L.; Frontiñán-Rubio, J.; Abás, E.; Domínguez-Alfaro, A.; Mesonero, J.E.; Criado, A.; Ansón-Casaos, A. Intrinsic and Selective Activity of Functionalized Carbon Nanotube/Nanocellulose Platforms against Colon Cancer Cells. Colloids Surf. B Biointerfaces 2022, 212, 112363. [Google Scholar] [CrossRef]
- Su, Y.; Hu, Y.; Wang, Y.; Xu, X.; Yuan, Y.; Li, Y.; Wang, Z.; Chen, K.; Zhang, F.; Ding, X.; et al. A Precision-Guided MWNT Mediated Reawakening the Sunk Synergy in RAS for Anti-Angiogenesis Lung Cancer Therapy. Biomaterials 2017, 139, 75–90. [Google Scholar] [CrossRef]
- Jwameer, M.R.; Salman, S.A.; Noori, F.T.M.; Sulaiman, G.M.; Jabir, M.S.; Khalil, K.A.A.; Ahmed, E.M.; Soliman, M.T.A. Antiproliferative Activity of PEG-PEI-SWCNTs against AMJ13 Breast Cancer Cells. J. Nanomater. 2023, 2023, 2855788. [Google Scholar] [CrossRef]
- Tang, L.; Li, J.; Pan, T.; Yin, Y.; Mei, Y.; Xiao, Q.; Wang, R.; Yan, Z.; Wang, W. Versatile Carbon Nanoplatforms for Cancer Treatment and Diagnosis: Strategies, Applications and Future Perspectives. Theranostics 2022, 12, 2290–2321. [Google Scholar] [CrossRef]
- Harisa, G.I.; Faris, T.M. Direct Drug Targeting into Intracellular Compartments: Issues, Limitations, and Future Outlook. J. Membr. Biol. 2019, 252, 527–539. [Google Scholar] [CrossRef]
- Tang, L.; Mei, Y.; Shen, Y.; He, S.; Xiao, Q.; Yin, Y.; Xu, Y.; Shao, J.; Wang, W.; Cai, Z. Nanoparticle-Mediated Targeted Drug Delivery to Remodel Tumor Microenvironment for Cancer Therapy. Int. J. Nanomed. 2021, 16, 5811–5829. [Google Scholar] [CrossRef]
- Li, M.; Zhang, F.; Su, Y.; Zhou, J.; Wang, W. Nanoparticles Designed to Regulate Tumor Microenvironment for Cancer Therapy. Life Sci. 2018, 201, 37–44. [Google Scholar] [CrossRef]
- Kaymak, I.; Williams, K.S.; Cantor, J.R.; Jones, R.G. Immunometabolic Interplay in the Tumor Microenvironment. Cancer Cell 2021, 39, 28–37. [Google Scholar] [CrossRef]
- Al Faraj, A.; Shaik, A.S.; Al Sayed, B.; Halwani, R.; Al Jammaz, I. Specific Targeting and Noninvasive Imaging of Breast Cancer Stem Cells Using Single-Walled Carbon Nanotubes as Novel Multimodality Nanoprobes. Nanomedicine 2016, 11, 31–46. [Google Scholar] [CrossRef]
- Fu, S.; Zhao, Y.; Sun, J.; Yang, T.; Zhi, D.; Zhang, E.; Zhong, F.; Zhen, Y.; Zhang, S.; Zhang, S. Integrin Avβ3-Targeted Liposomal Drug Delivery System for Enhanced Lung Cancer Therapy. Colloids Surf. B Biointerfaces 2021, 201, 111623. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, T.; Cao, Y.; Sun, J.; Zhou, Q.; Chen, H.; Guo, S.; Wang, Y.; Zhen, Y.; Liang, X.J.; et al. Temperature-Sensitive Lipid-Coated Carbon Nanotubes for Synergistic Photothermal Therapy and Gene Therapy. ACS Nano 2021, 15, 6517–6529. [Google Scholar] [CrossRef]
- Lu, G.H.; Shang, W.T.; Deng, H.; Han, Z.Y.; Hu, M.; Liang, X.Y.; Fang, C.H.; Zhu, X.H.; Fan, Y.F.; Tian, J. Targeting Carbon Nanotubes Based on IGF-1R for Photothermal Therapy of Orthotopic Pancreatic Cancer Guided by Optical Imaging. Biomaterials 2019, 195, 13–22. [Google Scholar] [CrossRef]
- Wen, L.; Ding, W.; Yang, S.; Xing, D. Microwave Pumped High-Efficient Thermoacoustic Tumor Therapy with Single Wall Carbon Nanotubes. Biomaterials 2016, 75, 163–173. [Google Scholar] [CrossRef]
- Hassan, H.A.F.M.; Smyth, L.; Wang, J.T.W.; Costa, P.M.; Ratnasothy, K.; Diebold, S.S.; Lombardi, G.; Al-Jamal, K.T. Dual Stimulation of Antigen Presenting Cells Using Carbon Nanotube-Based Vaccine Delivery System for Cancer Immunotherapy. Biomaterials 2016, 104, 310–322. [Google Scholar] [CrossRef]
- Gangrade, A.; Mandal, B.B. Injectable carbon nanotube impregnated silk based multifunctional hydrogel for localized targeted and on-demand anticancer drug delivery. ACS Biomater. Sci. Eng. 2019, 5, 2365–2381. [Google Scholar] [CrossRef]
- Neves, V.; Heister, E.; Costa, S.; Tîlmaciu, C.; Flahaut, E.; Soula, B.; Coley, H.M.; McFadden, J.; Silva, S.R.P. Design of Double-Walled Carbon Nanotubes for Biomedical Applications. Nanotechnology 2012, 23, 365102. [Google Scholar] [CrossRef]
- Oh, Y.; Jin, J.O.; Oh, J. Photothermal-Triggered Control of Sub-Cellular Drug Accumulation Using Doxorubicin-Loaded Single-Walled Carbon Nanotubes for the Effective Killing of Human Breast Cancer Cells. Nanotechnology 2017, 28, 125101. [Google Scholar] [CrossRef]
- Lee, P.C.; Chiou, Y.C.; Wong, J.M.; Peng, C.L.; Shieh, M.J. Targeting Colorectal Cancer Cells with Single-Walled Carbon Nanotubes Conjugated to Anticancer Agent SN-38 and EGFR Antibody. Biomaterials 2013, 34, 8756–8765. [Google Scholar] [CrossRef]
- Yoong, S.L.; Wong, B.S.; Zhou, Q.L.; Chin, C.F.; Li, J.; Venkatesan, T.; Ho, H.K.; Yu, V.; Ang, W.H.; Pastorin, G. Enhanced Cytotoxicity to Cancer Cells by Mitochondria-Targeting MWCNTs Containing Platinum(IV) Prodrug of Cisplatin. Biomaterials 2014, 35, 748–759. [Google Scholar] [CrossRef]
- Kim, S.W.; Kyung Lee, Y.; Yeon Lee, J.; Hee Hong, J.; Khang, D. PEGylated Anticancer-Carbon Nanotubes Complex Targeting Mitochondria of Lung Cancer Cells. Nanotechnology 2017, 28, 465102. [Google Scholar] [CrossRef]
- Wang, M.; Ruan, L.; Zheng, T.; Wang, D.; Zhou, M.; Lu, H.; Gao, J.; Chen, J.; Hu, Y. A Surface Convertible Nanoplatform with Enhanced Mitochondrial Targeting for Tumor Photothermal Therapy. Colloids Surf. B Biointerfaces 2020, 189, 110854. [Google Scholar] [CrossRef]
- Zhou, F.; Wu, S.; Yuan, Y.; Chen, W.R.; Xing, D. Mitochondria-Targeting Photoacoustic Therapy Using Single-Walled Carbon Nanotubes. Small 2012, 8, 1543–1550. [Google Scholar] [CrossRef]
- Marangon, I.; Silva, A.A.K.; Guilbert, T.; Kolosnjaj-Tabi, J.; Marchiol, C.; Natkhunarajah, S.; Chamming’s, F.; Ménard-Moyon, C.; Bianco, A.; Gennisson, J.L.; et al. Tumor Stiffening, a Key Determinant of Tumor Progression, Is Reversed by Nanomaterial-Induced Photothermal Therapy. Theranostics 2017, 7, 329–343. [Google Scholar] [CrossRef]
- Miao, Y.; Zhang, H.; Pan, Y.; Ren, J.; Ye, M.; Xia, F.; Huang, R.; Lin, Z.; Jiang, S.; Zhang, Y.; et al. Single-Walled Carbon Nanotube: One Specific Inhibitor of Cancer Stem Cells in Osteosarcoma upon Downregulation of the TGFβ1 Signaling. Biomaterials 2017, 149, 29–40. [Google Scholar] [CrossRef]
- Das, M.; Nariya, P.; Joshi, A.; Vohra, A.; Devkar, R.; Seshadri, S.; Thakore, S. Carbon Nanotube Embedded Cyclodextrin Polymer Derived Injectable Nanocarrier: A Multiple Faceted Platform for Stimulation of Multi-Drug Resistance Reversal. Carbohydr. Polym. 2020, 247, 116751. [Google Scholar] [CrossRef]
- Luo, X.; Wang, H.; Ji, D. Carbon Nanotubes (CNT)-Loaded Ginsenosides Rb3 Suppresses the PD-1/PD-L1 Pathway in Triple-Negative Breast Cancer. Aging 2021, 13, 17177–17189. [Google Scholar] [CrossRef]
- Wang, X.; Li, B.; Jing, H.; Dong, X.; Leng, X. MWCNT-Mediated Combinatorial Photothermal Ablation and Chemo-Immunotherapy Strategy for the Treatment of Melanoma. J. Mater. Chem. B 2020, 8, 4245–4258. [Google Scholar] [CrossRef]
- Nichols, J.W.; Bae, Y.H. EPR: Evidence and Fallacy. J. Control. Release 2014, 190, 451–464. [Google Scholar] [CrossRef]
- Danhier, F. To Exploit the Tumor Microenvironment: Since the EPR Effect Fails in the Clinic, What Is the Future of Nanomedicine? J. Control. Release 2016, 244, 108–121. [Google Scholar] [CrossRef]
- Vasey, P.A.; Kaye, S.B.; Morrison, R.; Twelves, C.; Wilson, P.; Duncan, R.; Thomson, A.H.; Murray, L.S.; Hilditch, T.E.; Murray, T.; et al. Phase I Clinical and Pharmacokinetic Study of PK1 [N-(2-Hydroxypropyl)Methacrylamide Copolymer Doxorubicin]: First Member of a New Class of Chemotherapeutic Agents-Drug-Polymer Conjugates. Cancer Research Campaign Phase I/II Committee. Clin. Cancer Res. 1999, 5, 83–94. [Google Scholar]
- Matsumura, Y.; Maeda, H. A New Concept for Macromolecular Therapeutics in Cancer Chemotherapy: Mechanism of Tumoritropic Accumulation of Proteins and the Antitumor Agent Smancs. Cancer Res. 1986, 46, 6387–6392. [Google Scholar]
- Thomas, R.G.; Surendran, S.P.; Jeong, Y.Y. Tumor Microenvironment-Stimuli Responsive Nanoparticles for Anticancer Therapy. Front. Mol. Biosci. 2020, 7, 610533. [Google Scholar] [CrossRef]
- Yang, T.; Wu, Z.; Wang, P.; Mu, T.; Qin, H.; Zhu, Z.; Wang, J.; Sui, L. A Large-Inner-Diameter Multi-Walled Carbon Nanotube-Based Dual-Drug Delivery System with PH-Sensitive Release Properties. J. Mater. Sci. Mater. Med. 2017, 28, 110. [Google Scholar] [CrossRef]
- Zhang, H.; Sun, X.; Hubbe, M.; Pal, L. Flexible and Pressure-Responsive Sensors from Cellulose Fibers Coated with Multiwalled Carbon Nanotubes. ACS Appl. Electron. Mater. 2019, 1, 1179–1188. [Google Scholar] [CrossRef]
- Qin, Y.; Chen, J.; Bi, Y.; Xu, X.; Zhou, H.; Gao, J.; Hu, Y.; Zhao, Y.; Chai, Z. Near-Infrared Light Remote-Controlled Intracellular Anti-Cancer Drug Delivery Using Thermo/PH Sensitive Nanovehicle. Acta Biomater. 2015, 17, 201–209. [Google Scholar] [CrossRef]
- Doughty, A.C.V.; Hoover, A.R.; Layton, E.; Murray, C.K.; Howard, E.W.; Chen, W.R. Nanomaterial Applications in Photothermal Therapy for Cancer. Materials 2019, 12, 779. [Google Scholar] [CrossRef]
- Moy, A.J.; Tunnell, J.W. Combinatorial Immunotherapy and Nanoparticle Mediated Hyperthermia. Adv. Drug Deliv. Rev. 2017, 114, 175–183. [Google Scholar] [CrossRef]
- Sundaram, P.; Abrahamse, H. Phototherapy Combined with Carbon Nanomaterials (1d and 2d) and Their Applications in Cancer Therapy. Materials 2020, 13, 4830. [Google Scholar] [CrossRef]
- Zhu, Y.; Sun, Q.; Liu, Y.; Ma, T.; Su, L.; Liu, S.; Shi, X.; Han, D.; Liang, F. Decorating Gold Nanostars with Multiwalled Carbon Nanotubes for Photothermal Therapy. R. Soc. Open Sci. 2018, 5, 180159. [Google Scholar] [CrossRef]
- McKernan, P.; Virani, N.A.; Faria, G.N.F.; Karch, C.G.; Prada Silvy, R.; Resasco, D.E.; Thompson, L.F.; Harrison, R.G. Targeted Single-Walled Carbon Nanotubes for Photothermal Therapy Combined with Immune Checkpoint Inhibition for the Treatment of Metastatic Breast Cancer. Nanoscale Res. Lett. 2021, 16, 9. [Google Scholar] [CrossRef] [PubMed]
- Bachilo, S.M.; Balzano, L.; Herrera, J.E.; Pompeo, F.; Resasco, D.E.; Weisman, R.B. Narrow (n,m)-Distribution of Single-Walled Carbon Nanotubes Grown Using a Solid Supported Catalyst. J. Am. Chem. Soc. 2003, 125, 11186–11187. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Xing, D.; Ou, Z.; Wu, B.; Resasco, D.E.; Chen, W.R. Cancer Photothermal Therapy in the Near-Infrared Region by Using Single-Walled Carbon Nanotubes. J. Biomed. Opt. 2009, 14, 021009. [Google Scholar] [CrossRef]
- Vilar, R.; Fish, R.J.; Casini, A.; Neerman-Arbez, M. Fibrin(Ogen) in Human Disease: Both Friend and Foe. Haematologica 2020, 105, 284–296. [Google Scholar] [CrossRef] [PubMed]
- Naser Mohammed, S.; Mishaal Mohammed, A.; Al-Rawi, K.F. Novel Combination of Multi-Walled Carbon Nanotubes and Gold Nanocomposite for Photothermal Therapy in Human Breast Cancer Model. Steroids 2022, 186, 109091. [Google Scholar] [CrossRef]
- Naief, M.F.; Khalaf, Y.H.; Mohammed, A.M. Novel Photothermal Therapy Using Multi-Walled Carbon Nanotubes and Platinum Nanocomposite for Human Prostate Cancer PC3 Cell Line. J. Organomet. Chem. 2022, 975, 122422. [Google Scholar] [CrossRef]
- Doix, B.; Trempolec, N.; Riant, O.; Feron, O. Low Photosensitizer Dose and Early Radiotherapy Enhance Antitumor Immune Response of Photodynamic Therapy-Based Dendritic Cell Vaccination. Front. Oncol. 2019, 9, 811. [Google Scholar] [CrossRef]
- Ogbodu, R.O.; Limson, J.L.; Prinsloo, E.; Nyokong, T. Photophysical Properties and Photodynamic Therapy Effect of Zinc Phthalocyanine-Spermine-Single Walled Carbon Nanotube Conjugate on MCF-7 Breast Cancer Cell Line. Synth. Met. 2015, 204, 122–132. [Google Scholar] [CrossRef]
- Ogbodu, R.O.; Nyokong, T. The Effect of Ascorbic Acid on the Photophysical Properties and Photodynamic Therapy Activities of Zinc Phthalocyanine-Single Walled Carbon Nanotube Conjugate on MCF-7 Cancer Cells. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2015, 151, 174–183. [Google Scholar] [CrossRef]
- Sundaram, P.; Abrahamse, H. Effective Photodynamic Therapy for Colon Cancer Cells Using Chlorin E6 Coated Hyaluronic Acid-Based Carbon Nanotubes. Int. J. Mol. Sci. 2020, 21, 4745. [Google Scholar] [CrossRef] [PubMed]
- Son, K.H.; Hong, J.H.; Lee, J.W. Carbon Nanotubes as Cancer Therapeutic Carriers and Mediators. Int. J. Nanomed. 2016, 11, 5163–5185. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Ma, R.; Wang, L.; Zhang, J.; Liu, R.; Li, L.; Liu, Y.; Hou, L.; Yu, X.; Gao, J.; et al. The Application of Hyaluronic Acid-Derivatized Carbon Nanotubes in Hematoporphyrin Monomethyl Ether-Based Photodynamic Therapy for in Vivo and in Vitro Cancer Treatment. Int. J. Nanomed. 2013, 8, 2361–2373. [Google Scholar] [CrossRef]
- Dheyab, M.A.; Aziz, A.A.; Khaniabadi, P.M.; Jameel, M.S.; Oladzadabbasabadi, N.; Rahman, A.A.; Braim, F.S.; Mehrdel, B. Gold Nanoparticles-Based Photothermal Therapy for Breast Cancer. Photodiagnosis Photodyn. Ther. 2023, 42, 103312. [Google Scholar] [CrossRef]
- Wang, D.; Ren, Y.; Shao, Y.; Yu, D.; Meng, L. Facile Preparation of Doxorubicin-Loaded and Folic Acid-Conjugated Carbon Nanotubes@Poly(N-Vinyl Pyrrole) for Targeted Synergistic Chemo-Photothermal Cancer Treatment. Bioconjugate Chem. 2017, 28, 2815–2822. [Google Scholar] [CrossRef]
- Karimi, A.; Erfan, M.; Mortazavi, S.A.; Ghorbani-Bidkorbeh, F.; Kobarfard, F.; Shirazi, F.H. Functionalisation of Carbon Nanotubes by Methotrexate and Study of Synchronous Photothermal Effect of Carbon Nanotube and Anticancer Drug on Cancer Cell Death. IET Nanobiotechnol. 2019, 13, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Yi, W.; Hou, J.; Yoo, S.; Jin, W.; Yang, Q. Acarbon Nanotube-Gemcitabine-Lentinan Three-Component Composite for Chemo-Photothermal Synergistic Therapy of Cancer. Int. J. Nanomed. 2018, 13, 3069–3080. [Google Scholar] [CrossRef]
- Saliev, T.; Akhmetova, A.; Kulsharova, G. Multifunctional Hybrid Nanoparticles for Theranostics. In Core-Shell Nanostructures for Drug Delivery and Theranostics: Challenges, Strategies and Prospects for Novel Carrier Systems; Elsevier: Amsterdam, The Netherlands, 2018; pp. 177–244. [Google Scholar] [CrossRef]
- Karimi, A.; Erfan, M.; Mortazavi, S.A.; Ghorbani-Bidkorbeh, F.; Landi, B.; Kobarfard, F.; Shirazi, F.H. The Photothermal Effect of Targeted Methotrexate-Functionalized Multi-Walled Carbon Nanotubes on MCF7 Cells. Iran J. Pharm. Res. 2019, 18, 221–236. [Google Scholar] [CrossRef]
- Gao, W.; Zhang, W.; Yu, H.; Xing, W.; Yang, X.; Zhang, Y.; Liang, C. 3D CNT/MXene Microspheres for Combined Photothermal/Photodynamic/Chemo for Cancer Treatment. Front. Bioeng. Biotechnol. 2022, 10, 996177. [Google Scholar] [CrossRef]
- Gao, C.; Dong, P.; Lin, Z.; Guo, X.; Jiang, B.P.; Ji, S.; Liang, H.; Shen, X.C. Near-Infrared Light Responsive Imaging-Guided Photothermal and Photodynamic Synergistic Therapy Nanoplatform Based on Carbon Nanohorns for Efficient Cancer Treatment. Chem.–A Eur. J. 2018, 24, 12827–12837. [Google Scholar] [CrossRef]
- Gao, C.; Jian, J.; Lin, Z.; Yu, Y.X.; Jiang, B.P.; Chen, H.; Shen, X.C. Hypericin-Loaded Carbon Nanohorn Hybrid for Combined Photodynamic and Photothermal Therapy in Vivo. Langmuir 2019, 35, 8228–8237. [Google Scholar] [CrossRef]
- Yang, J.; Hou, M.; Sun, W.; Wu, Q.; Xu, J.; Xiong, L.; Chai, Y.; Liu, Y.; Yu, M.; Wang, H.; et al. Sequential PDT and PTT Using Dual-Modal Single-Walled Carbon Nanohorns Synergistically Promote Systemic Immune Responses against Tumor Metastasis and Relapse. Adv. Sci. 2020, 7, 2001088. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.; Chen, D.; Zou, J.; Shao, J.; Tang, H.; Xu, H.; Si, W.; Dong, X. Tumor Microenvironment Responsive Oxygen-Self-Generating Nanoplatform for Dual-Imaging Guided Photodynamic and Photothermal Therapy. ChemistrySelect 2018, 3, 4366–4373. [Google Scholar] [CrossRef]
- Zhang, M.; Wang, W.; Cui, Y.; Chu, X.; Sun, B.; Zhou, N.; Shen, J. Magnetofluorescent Fe3O4/Carbon Quantum Dots Coated Single-Walled Carbon Nanotubes as Dual-Modal Targeted Imaging and Chemo/Photodynamic/Photothermal Triple-Modal Therapeutic Agents. Chem. Eng. J. 2018, 338, 526–538. [Google Scholar] [CrossRef]
- Marangon, I.; Ménard-Moyon, C.; Silva, A.K.A.; Bianco, A.; Luciani, N.; Gazeau, F. Synergic Mechanisms of Photothermal and Photodynamic Therapies Mediated by Photosensitizer/Carbon Nanotube Complexes. Carbon N. Y. 2016, 97, 110–123. [Google Scholar] [CrossRef]
- Behnam, M.A.; Emami, F.; Sobhani, Z.; Koohi-Hosseinabadi, O.; Dehghanian, A.R.; Zebarjad, S.M.; Moghim, M.H.; Oryan, A. Novel Combination of Silver Nanoparticles and Carbon Nanotubes for Plasmonic Photo Thermal Therapy in Melanoma Cancer Model. Adv. Pharm. Bull. 2018, 8, 49–55. [Google Scholar] [CrossRef]
- Lee, S.S.; Roche, P.J.R.; Giannopoulos, P.N.; Mitmaker, E.J.; Tamilia, M.; Paliouras, M.; Trifiro, M.A. Prostate-Specific Membrane Antigen–Directed Nanoparticle Targeting for Extreme Nearfield Ablation of Prostate Cancer Cells. Tumor Biol. 2017, 39, 1010428317695943. [Google Scholar] [CrossRef] [PubMed]
- Koohi Hosseinabadi, O.; Behnam, M.A.; Khoradmehr, A.; Emami, F.; Sobhani, Z.; Dehghanian, A.R.; Dehghani Firoozabadi, A.; Rahmanifar, F.; Vafaei, H.; Tamadon, A.; et al. Benign Prostatic Hyperplasia Treatment Using Plasmonic Nanoparticles Irradiated by Laser in a Rat Model. Biomed. Pharmacother. 2020, 127, 110118. [Google Scholar] [CrossRef] [PubMed]
- Asrar, A.; Sobhani, Z.; Behnam, M.A. Melanoma Cancer Therapy Using PEGylated Nanoparticles and Semiconductor Laser. Adv. Pharm. Bull. 2022, 12, 524–530. [Google Scholar] [CrossRef]
- Fan, J.P.; Xie, C.F.; Luo, Y.S.; Song, F.T.; Liu, X.Y.; Zhu, J.H.; Zhang, X.H. Solubilities of Betulin and Betulinic Acid in Sodium Hydroxide Aqueous Solutions of Varied Mole Fraction at Temperatures from 283.2 K to 323.2 K. J. Chem. Thermodyn. 2013, 67, 1–4. [Google Scholar] [CrossRef]
- Tu, X.; Wang, L.; Cao, Y.; Ma, Y.; Shen, H.; Zhang, M.; Zhang, Z. Efficient cancer ablation by combined photothermal and enhanced chemo-therapy based on carbon nanoparticles/doxorubicin@SiO2 nanocomposites. Carbon 2016, 97, 35–44. [Google Scholar] [CrossRef]
- Alfei, S. Cationic Materials for Gene Therapy: A Look Back to the Birth and Development of 2,2-Bis-(Hydroxymethyl)Propanoic Acid-Based Dendrimer Scaffolds. Int. J. Mol. Sci. 2023, 24, 16006. [Google Scholar] [CrossRef]
- Piña, M.J.; Girotti, A.; Serrano, S.; Muñoz, R.; Rodríguez-Cabello, J.C.; Arias, F.J. A Double Safety Lock Tumor-Specific Device for Suicide Gene Therapy in Breast Cancer. Cancer Lett. 2020, 470, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Cáceres, B.; Ramirez, A.; Carrillo, E.; Jimenez, G.; Griñán-Lisón, C.; López-Ruiz, E.; Jiménez-Martínez, Y.; Marchal, J.A.; Boulaiz, H. Deciphering the Mechanism of Action Involved in Enhanced Suicide Gene Colon Cancer Cell Killer Effect Mediated by Gef and Apoptin. Cancers 2019, 11, 264. [Google Scholar] [CrossRef]
- Lin, M.C.; Wang, M.; Chou, M.C.; Chao, C.N.; Fang, C.Y.; Chen, P.L.; Chang, D.; Shen, C.H. Gene Therapy for Castration-Resistant Prostate Cancer Cells Using JC Polyomavirus-like Particles Packaged with a PSA Promoter Driven-Suicide Gene. Cancer Gene Ther. 2019, 26, 208–215. [Google Scholar] [CrossRef]
- Hossain, J.A.; Marchini, A.; Fehse, B.; Bjerkvig, R.; Miletic, H. Suicide Gene Therapy for the Treatment of High-Grade Glioma: Past Lessons, Present Trends, and Future Prospects. Neuro-Oncol Adv. 2020, 2, vdaa013. [Google Scholar] [CrossRef]
- Chao, C.N.; Lin, M.C.; Fang, C.Y.; Chen, P.L.; Chang, D.; Shen, C.H.; Wang, M. Gene Therapy for Human Lung Adenocarcinoma Using a Suicide Gene Driven by a Lung-Specific Promoter Delivered by JC Virus-like Particles. PLoS ONE 2016, 11, e0157865. [Google Scholar] [CrossRef]
- Michaelsen, S.R.; Christensen, C.L.; Sehested, M.; Cramer, F.; Poulsen, T.T.; Patterson, A.V.; Poulsen, H.S. Single Agent- and Combination Treatment with Two Targeted Suicide Gene Therapy Systems Is Effective in Chemoresistant Small Cell Lung Cancer Cells. J. Gene Med. 2012, 14, 445–458. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Sutariya, V.; Gupta, S.V.; Bhatia, D. GADD45α-Targeted Suicide Gene Therapy Driven by Synthetic CArG Promoter E9NS Sensitizes NSCLC Cells to Cisplatin, Resveratrol, and Radiation Regardless of P53 Status. Onco Targets Ther. 2019, 12, 3161–3170. [Google Scholar] [CrossRef]
- Mohseni-Dargah, M.; Akbari-Birgani, S.; Madadi, Z.; Saghatchi, F.; Kaboudin, B. Carbon Nanotube-Delivered IC9 Suicide Gene Therapy for Killing Breast Cancer Cells in Vitro. Nanomedicine 2019, 14, 1033–1047. [Google Scholar] [CrossRef]
- Zhang, L.; Zheng, W.; Tang, R.; Wang, N.; Zhang, W.; Jiang, X. Gene Regulation with Carbon-Based SiRNA Conjugates for Cancer Therapy. Biomaterials 2016, 104, 269–278. [Google Scholar] [CrossRef]
- Anderson, T.; Hu, R.; Yang, C.; Yoon, H.S.; Yong, K.T. Pancreatic Cancer Gene Therapy Using an SiRNA-Functionalized Single Walled Carbon Nanotubes (SWNTs) Nanoplex. Biomater. Sci. 2014, 2, 1244–1253. [Google Scholar] [CrossRef] [PubMed]
- Koury, J.; Lucero, M.; Cato, C.; Chang, L.; Geiger, J.; Henry, D.; Hernandez, J.; Hung, F.; Kaur, P.; Teskey, G.; et al. Immunotherapies: Exploiting the Immune System for Cancer Treatment. J. Immunol. Res. 2018, 2018, 9585614. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Bevan, M.J. CD8+ T Cells: Foot Soldiers of the Immune System. Immunity 2011, 35, 161–168. [Google Scholar] [CrossRef]
- Singer, M.; Wang, C.; Cong, L.; Marjanovic, N.D.; Kowalczyk, M.S.; Zhang, H.; Nyman, J.; Sakuishi, K.; Kurtulus, S.; Gennert, D.; et al. A Distinct Gene Module for Dysfunction Uncoupled from Activation in Tumor-Infiltrating T Cells. Cell 2016, 166, 1500–1511.e9. [Google Scholar] [CrossRef]
- Wang, C.; Xu, L.; Liang, C.; Xiang, J.; Peng, R.; Liu, Z. Immunological Responses Triggered by Photothermal Therapy with Carbon Nanotubes in Combination with Anti-CTLA-4 Therapy to Inhibit Cancer Metastasis. Adv. Mater. 2014, 26, 8154–8162. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Xu, Z.; Qi, Z.; Huang, X.; Li, M.; Liu, S.; Yan, Y.; Gao, M. Application of Carbon Nanomaterials to Enhancing Tumor Immunotherapy: Current Advances and Prospects. Int. J. Nanomed. 2024, 19, 10899–10915. [Google Scholar] [CrossRef]
- Wang, F.; Ullah, A.; Fan, X.; Xu, Z.; Zong, R.; Wang, X.; Chen, G. Delivery of Nanoparticle Antigens to Antigen-Presenting Cells: From Extracellular Specific Targeting to Intracellular Responsive Presentation. J. Control. Release 2021, 333, 107–128. [Google Scholar] [CrossRef]
- Jang, D.I.; Lee, A.H.; Shin, H.Y.; Song, H.R.; Park, J.H.; Kang, T.B.; Lee, S.R.; Yang, S.H. The Role of Tumor Necrosis Factor Alpha (Tnf-α) in Autoimmune Disease and Current Tnf-α Inhibitors in Therapeutics. Int. J. Mol. Sci. 2021, 22, 2719. [Google Scholar] [CrossRef]
- Tau, G.; Rothman, P. Biologic Functions of the IFN-γ Receptors. Allergy Eur. J. Allergy Clin. Immunol. 1999, 54, 1233–1251. [Google Scholar] [CrossRef]
- Paul, S.; Lal, G. The Molecular Mechanism of Natural Killer Cells Function and Its Importance in Cancer Immunotherapy. Front. Immunol. 2017, 8, 1124. [Google Scholar] [CrossRef] [PubMed]
- Patrick, B.; Akhtar, T.; Kousar, R.; Huang, C.C.; Li, X.G. Carbon Nanomaterials: Emerging Roles in Immuno-Oncology. Int. J. Mol. Sci. 2023, 24, 6600. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Yang, M.; Jia, F.; Kong, H.; Zhang, W.; Wang, C.; Xing, J.; Xie, S.; Xu, H. Subcutaneous Injection of Water-Soluble Multi-Walled Carbon Nanotubes in Tumor-Bearing Mice Boosts the Host Immune Activity. Nanotechnology 2010, 21, 145104. [Google Scholar] [CrossRef] [PubMed]
- Jin, H.; Gao, S.; Song, D.; Liu, Y.; Chen, X. Intratumorally CpG Immunotherapy with Carbon Nanotubes Inhibits Local Tumor Growth and Liver Metastasis by Suppressing the Epithelial-Mesenchymal Transition of Colon Cancer Cells. Anti-Cancer Drugs 2021, 32, 278–285. [Google Scholar] [CrossRef]
- Dutt, T.S.; Saxena, R.K. Enhanced Antibody Response to Ovalbumin Coupled to Poly-Dispersed Acid Functionalized Single Walled Carbon Nanotubes. Immunol. Lett. 2020, 217, 77–83. [Google Scholar] [CrossRef]
- Li, D.; Ahmed, M.; Khan, A.; Xu, L.; Walters, A.A.; Ballesteros, B.; Al-Jamal, K.T. Tailoring the Architecture of Cationic Polymer Brush-Modified Carbon Nanotubes for Efficient SiRNA Delivery in Cancer Immunotherapy. ACS Appl. Mater. Interfaces 2021, 13, 30284–30294. [Google Scholar] [CrossRef]
- Xia, Q.; Gong, C.; Gu, F.; Wang, Z.; Hu, C.; Zhang, L.; Qiang, L.; Ding, X.; Gao, S.; Gao, Y. Functionalized Multi-Walled Carbon Nanotubes for Targeting Delivery of Immunostimulatory CpG Oligonucleotides against Prostate Cancer. J. Biomed. Nanotechnol. 2018, 14, 1613–1626. [Google Scholar] [CrossRef]
- Zhao, D.; Alizadeh, D.; Zhang, L.; Liu, W.; Farrukh, O.; Manuel, E.; Diamond, D.J.; Badie, B. Carbon Nanotubes Enhance CpG Uptake and Potentiate Antiglioma Immunity. Clin. Cancer Res. 2011, 17, 771–782. [Google Scholar] [CrossRef]
- Radzi, M.R.M.; Johari, N.A.; Zawawi, W.F.A.W.M.; Zawawi, N.A.; Latiff, N.A.; Malek, N.A.N.N.; Wahab, A.A.; Salim, M.I.; Jemon, K. In Vivo Evaluation of Oxidized Multiwalled-Carbon Nanotubes-Mediated Hyperthermia Treatment for Breast Cancer. Biomater. Adv. 2022, 134, 112586. [Google Scholar] [CrossRef]
- Villa, C.H.; Dao, T.; Ahearn, I.; Fehrenbacher, N.; Casey, E.; Rey, D.A.; Korontsvit, T.; Zakhaleva, V.; Batt, C.A.; Philips, M.R.; et al. Single-Walled Carbon Nanotubes Deliver Peptide Antigen into Dendritic Cells and Enhance IgG Responses to Tumor-Associated Antigens. ACS Nano 2011, 5, 5300–5311. [Google Scholar] [CrossRef]
- Fadel, T.R.; Steenblock, E.R.; Stern, E.; Li, N.; Wang, X.; Haller, G.L.; Pfefferle, L.D.; Fahmy, T.M. Enhanced Cellular Activation with Single Walled Carbon Nanotube Bundles Presenting Antibody Stimuli. Nano Lett. 2008, 8, 2070–2076. [Google Scholar] [CrossRef] [PubMed]
- Fadel, T.R.; Look, M.; Staffier, P.A.; Haller, G.L.; Pfefferle, L.D.; Fahmy, T.M. Clustering of Stimuli on Single-Walled Carbon Nanotube Bundles Enhances Cellular Activation. Langmuir 2010, 26, 5645–5654. [Google Scholar] [CrossRef]
- Fadel, T.R.; Li, N.; Shah, S.; Look, M.; Pfefferle, L.D.; Haller, G.L.; Justesen, S.; Wilson, C.J.; Fahmy, T.M. Adsorption of Multimeric T Cell Antigens on Carbon Nanotubes: Effect on Protein Structure and Antigen-Specific T Cell Stimulation. Small 2013, 9, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Burkert, S.C.; He, X.; Shurin, G.V.; Nefedova, Y.; Kagan, V.E.; Shurin, M.R.; Star, A. Nitrogen-Doped Carbon Nanotube Cups for Cancer Therapy. ACS Appl. Nano Mater. 2022, 5, 13685–13696. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ali, S.F.; Dervishi, E.; Xu, Y.; Li, Z.; Casciano, D.; Biris, A.S. Cytotoxicity Effects of Graphene and Single-Wall Carbon Nanotubes in Neural Phaeochromocytoma-Derived Pc12 Cells. ACS Nano 2010, 4, 3181–3186. [Google Scholar] [CrossRef]
- Tang, L.; Xiao, Q.; Mei, Y.; He, S.; Zhang, Z.; Wang, R.; Wang, W. Insights on Functionalized Carbon Nanotubes for Cancer Theranostics. J. Nanobiotechnol. 2021, 19, 423. [Google Scholar] [CrossRef]
- Sekiyama, S.; Umezawa, M.; Iizumi, Y.; Ube, T.; Okazaki, T.; Kamimura, M.; Soga, K. Delayed Increase in Near-Infrared Fluorescence in Cultured Murine Cancer Cells Labeled with Oxygen-Doped Single-Walled Carbon Nanotubes. Langmuir 2019, 35, 831–837. [Google Scholar] [CrossRef]
- Wang, X.; Wang, C.; Cheng, L.; Lee, S.T.; Liu, Z. Noble Metal Coated Single-Walled Carbon Nanotubes for Applications in Surface Enhanced Raman Scattering Imaging and Photothermal Therapy. J. Am. Chem. Soc. 2012, 134, 7414–7422. [Google Scholar] [CrossRef]
- Yan, C.; Chen, C.; Hou, L.; Zhang, H.; Che, Y.; Qi, Y.; Zhang, X.; Cheng, J.; Zhang, Z. Single-Walled Carbon Nanotube-Loaded Doxorubicin and Gd-DTPA for Targeted Drug Delivery and Magnetic Resonance Imaging. J. Drug Target. 2017, 25, 163–171. [Google Scholar] [CrossRef]
- Zhang, M.; Wang, W.; Cui, Y.; Zhou, N.; Shen, J. Magnetofluorescent Carbon Quantum Dot Decorated Multiwalled Carbon Nanotubes for Dual-Modal Targeted Imaging in Chemo-Photothermal Synergistic Therapy. ACS Biomater. Sci. Eng. 2018, 4, 151–162. [Google Scholar] [CrossRef]
- Saghatchi, F.; Mohseni-Dargah, M.; Akbari-Birgani, S.; Saghatchi, S.; Kaboudin, B. Cancer Therapy and Imaging Through Functionalized Carbon Nanotubes Decorated with Magnetite and Gold Nanoparticles as a Multimodal Tool. Appl. Biochem. Biotechnol. 2020, 191, 1280–1293. [Google Scholar] [CrossRef]
- Delogu, L.G.; Vidili, G.; Venturelli, E.; Ménard-Moyon, C.; Zoroddu, M.A.; Pilo, G.; Nicolussi, P.; Ligios, C.; Bedognetti, D.; Sgarrella, F.; et al. Functionalized Multiwalled Carbon Nanotubes as Ultrasound Contrast Agents. Proc. Natl. Acad. Sci. USA 2012, 109, 16612–16617. [Google Scholar] [CrossRef]
- Avti, P.K.; Hu, S.; Favazza, C.; Mikos, A.G.; Jansen, J.A.; Shroyer, K.R.; Wang, L.V.; Sitharaman, B. Detection, Mapping, and Quantification of Single Walled Carbon Nanotubes in Histological Specimens with Photoacoustic Microscopy. PLoS ONE 2012, 7, e35064. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Bao, C.; Liang, S.; Fu, H.; Wang, K.; Deng, M.; Liao, Q.; Cui, D. RGD-Conjugated Silica-Coated Gold Nanorods on the Surface of Carbon Nanotubes for Targeted Photoacoustic Imaging of Gastric Cancer. Nanoscale Res. Lett. 2014, 9, 264. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.T.W.; Fabbro, C.; Venturelli, E.; Ménard-Moyon, C.; Chaloin, O.; Da Ros, T.; Methven, L.; Nunes, A.; Sosabowski, J.K.; Mather, S.J.; et al. The Relationship between the Diameter of Chemically-Functionalized Multi-Walled Carbon Nanotubes and Their Organ Biodistribution Profiles in Vivo. Biomaterials 2014, 35, 9517–9528. [Google Scholar] [CrossRef]
- Zhao, H.; Chao, Y.; Liu, J.; Huang, J.; Pan, J.; Guo, W.; Wu, J.; Sheng, M.; Yang, K.; Wang, J.; et al. Polydopamine Coated Single-Walled Carbon Nanotubes as a Versatile Platform with Radionuclide Labeling for Multimodal Tumor Imaging and Therapy. Theranostics 2016, 6, 1833–1843. [Google Scholar] [CrossRef]
- Ghosh, D.; Bagley, A.F.; Na, Y.J.; Birrer, M.J.; Bhatia, S.N.; Belcher, A.M. Deep, Noninvasive Imaging and Surgical Guidance of Submillimeter Tumors Using Targeted M13-Stabilized Single-Walled Carbon Nanotubes. Proc. Natl. Acad. Sci. USA 2014, 111, 13948–13953. [Google Scholar] [CrossRef] [PubMed]
- Welsher, K.; Liu, Z.; Sherlock, S.P.; Robinson, J.T.; Chen, Z.; Daranciang, D.; Dai, H. A Route to Brightly Fluorescent Carbon Nanotubes for Near-Infrared Imaging in Mice. Nat. Nanotechnol. 2009, 4, 773–780. [Google Scholar] [CrossRef]
- Rawashdeh1, I.; Al-Fandi, M.G.; Makableh, Y.; Harahsha, T. Developing a Nano-Biosensor for Early Detection of Pancreatic Cancer. Sens. Rev. 2021, 41, 93–100. [Google Scholar] [CrossRef]
- Sharma, A.; Hong, S.; Singh, R.; Jang, J. Single-Walled Carbon Nanotube Based Transparent Immunosensor for Detection of a Prostate Cancer Biomarker Osteopontin. Anal. Chim. Acta 2015, 869, 68–73. [Google Scholar] [CrossRef]
- Tîlmaciu, C.M.; Dinesh, B.; Pellerano, M.; Diot, S.; Guidetti, M.; Vollaire, J.; Bianco, A.; Ménard-Moyon, C.; Josserand, V.; Morris, M.C. Nanobiosensor Reports on CDK1 Kinase Activity in Tumor Xenografts in Mice. Small 2021, 17, 2007177. [Google Scholar] [CrossRef] [PubMed]
- Mahmoodi, P.; Rezayi, M.; Rasouli, E.; Avan, A.; Gholami, M.; Ghayour Mobarhan, M.; Karimi, E.; Alias, Y. Early-Stage Cervical Cancer Diagnosis Based on an Ultra-Sensitive Electrochemical DNA Nanobiosensor for HPV-18 Detection in Real Samples. J. Nanobiotechnol. 2020, 18, 11. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Tabakman, S.; Welsher, K.; Dai, H. Carbon Nanotubes in Biology and Medicine: In Vitro and in Vivo Detection, Imaging and Drug Delivery. Nano Res. 2009, 2, 85–120. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Young, R.J.; MacPherson, J.V.; Wilson, N.R. Silver-Decorated Carbon Nanotube Networks as SERS Substrates. J. Raman Spectrosc. 2011, 42, 1255–1262. [Google Scholar] [CrossRef]
- Dai, Y.; Su, J.; Wu, K.; Ma, W.; Wang, B.; Li, M.; Sun, P.; Shen, Q.; Wang, Q.; Fan, Q. Multifunctional Thermosensitive Liposomes Based on Natural Phase-Change Material: Near-Infrared Light-Triggered Drug Release and Multimodal Imaging-Guided Cancer Combination Therapy. ACS Appl. Mater. Interfaces 2019, 11, 10540–10553. [Google Scholar] [CrossRef]
- Ghaghada, K.B.; Starosolski, Z.A.; Bhayana, S.; Stupin, I.; Patel, C.V.; Bhavane, R.C.; Gao, H.; Bednov, A.; Yallampalli, C.; Belfort, M.; et al. Pre-Clinical Evaluation of a Nanoparticle-Based Blood-Pool Contrast Agent for MR Imaging of the Placenta. Placenta 2017, 57, 60–70. [Google Scholar] [CrossRef]
- Sanginario, A.; Miccoli, B.; Demarchi, D. Carbon Nanotubes as an Effective Opportunity for Cancer Diagnosis and Treatment. Biosensors 2017, 7, 9. [Google Scholar] [CrossRef]
- Ji, Z.; Ding, W.; Ye, F.; Lou, C.; Xing, D. Shape-Adapting Thermoacoustic Imaging System Based on Flexible Multi-Element Transducer. Appl. Phys. Lett. 2015, 107, 094104. [Google Scholar] [CrossRef]
- De La Zerda, A.; Zavaleta, C.; Keren, S.; Vaithilingam, S.; Bodapati, S.; Liu, Z.; Levi, J.; Smith, B.R.; Ma, T.J.; Oralkan, O.; et al. Carbon Nanotubes as Photoacoustic Molecular Imaging Agents in Living Mice. Nat. Nanotechnol. 2008, 3, 557–562. [Google Scholar] [CrossRef]
- Tao, Y.; Sun, Y.; Shi, K.; Pei, P.; Ge, F.; Yang, K.; Liu, T. Versatile Labeling of Multiple Radionuclides onto a Nanoscale Metal-Organic Framework for Tumor Imaging and Radioisotope Therapy. Biomater. Sci. 2021, 9, 2947–2954. [Google Scholar] [CrossRef]
- Hernandez, R.; Grudzinski, J.J.; Aluicio-Sarduy, E.; Massey, C.F.; Pinchuk, A.N.; Bitton, A.N.; Patel, R.; Zhang, R.; Rao, A.V.; Iyer, G.; et al. 177Lu-NM600 Targeted Radionuclide Therapy Extends Survival in Syngeneic Murine Models of Triple-Negative Breast Cancer. J. Nucl. Med. 2020, 61, 1187–1194. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Peng, R.; Liu, Z. Carbon Nanotubes for Biomedical Imaging: The Recent Advances. Adv. Drug Deliv. Rev. 2013, 65, 1951–1963. [Google Scholar] [CrossRef]
- Mandal, A.K.; Wu, X.; Ferreira, J.S.; Kim, M.; Powell, L.R.; Kwon, H.; Groc, L.; Wang, Y.H.; Cognet, L. Fluorescent Sp3 Defect-Tailored Carbon Nanotubes Enable NIR-II Single Particle Imaging in Live Brain Slices at Ultra-Low Excitation Doses. Sci. Rep. 2020, 10, 5286. [Google Scholar] [CrossRef] [PubMed]
- Dang, X.; Bardhan, N.M.; Qi, J.; Gu, L.; Eze, N.A.; Lin, C.W.; Kataria, S.; Hammond, P.T.; Belcher, A.M. Deep-Tissue Optical Imaging of near Cellular-Sized Features. Sci. Rep. 2019, 9, 3873. [Google Scholar] [CrossRef] [PubMed]
- Silindir-Gunay, M.; Sarcan, E.T.; Ozer, A.Y. Near-Infrared Imaging of Diseases: A Nanocarrier Approach. Drug Dev. Res. 2019, 80, 521–534. [Google Scholar] [CrossRef]
- Clark, L.C.; Lyons, C. Electrode systems for continuous monitoring in cardiovascular surgery. Ann. N. Y. Acad. Sci. 1962, 102, 29–45. [Google Scholar] [CrossRef]
- Gupta, S.; Murthy, C.N.; Prabha, C.R. Recent Advances in Carbon Nanotube Based Electrochemical Biosensors. Int. J. Biol. Macromol. 2018, 108, 687–703. [Google Scholar] [CrossRef]
- Moon, D.; Cha, Y.K.; Kim, S.; Cho, S.; Ko, H.J.; Park, T.H. FET-Based Nanobiosensors for the Detection of Smell and Taste. Sci. China Life Sci. 2020, 63, 1159–1167. [Google Scholar] [CrossRef]
- Bellan, L.M.; Wu, D.; Langer, R.S. Current Trends in Nanobiosensor Technology. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2011, 3, 229–246. [Google Scholar] [CrossRef]
- Yoosefian, M.; Etminan, N. Leucine/Pd-Loaded (5,5) Single-Walled Carbon Nanotube Matrix as a Novel Nanobiosensors for in Silico Detection of Protein. Amino Acids 2018, 50, 653–661. [Google Scholar] [CrossRef]
- Popovics, P.; Awadallah, W.N.; Kohrt, S.E.; Case, T.C.; Miller, N.L.; Ricke, E.A.; Huang, W.; Ramirez-Solano, M.; Liu, Q.; Vezina, C.M.; et al. Prostatic Osteopontin Expression Is Associated with Symptomatic Benign Prostatic Hyperplasia. Prostate 2020, 80, 731–741. [Google Scholar] [CrossRef]
- Wisniewski, T.; Winiecki, J.; Makarewicz, R.; Zekanowska, E. The Effect of Radiotherapy and Hormone Therapy on Osteopontin Concentrations in Prostate Cancer Patients. J. BUON 2020, 25, 527–530. [Google Scholar] [PubMed]
- Hiraoka, D.; Hosoda, E.; Chiba, K.; Kishimoto, T. SGK Phosphorylates Cdc25 and Myt1 to Trigger Cyclin B-Cdk1 Activation at the Meiotic G2/M Transition. J. Cell Biol. 2019, 218, 3597–3611. [Google Scholar] [CrossRef]
- Li, C.; Curreli, M.; Lin, H.; Lei, B.; Ishikawa, F.N.; Datar, R.; Cote, R.J.; Thompson, M.E.; Zhou, C. Complementary Detection of Prostate-Specific Antigen Using In 2O3 Nanowires and Carbon Nanotubes. J. Am. Chem. Soc. 2005, 127, 12484–12485. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Munge, B.; Patel, V.; Jensen, G.; Bhirde, A.; Gong, J.D.; Kim, S.N.; Gillespie, J.; Gutkind, J.S.; Papadimitrakopoulos, F.; et al. Carbon Nanotube Amplification Strategies for Highly Sensitive Immunodetection of Cancer Biomarkers. J. Am. Chem. Soc. 2006, 128, 11199–11205. [Google Scholar] [CrossRef]
- Bi, S.; Zhou, H.; Zhang, S. Multilayers Enzyme-Coated Carbon Nanotubes as Biolabel for Ultrasensitive Chemiluminescence Immunoassay of Cancer Biomarker. Biosens. Bioelectron. 2009, 24, 2961–2966. [Google Scholar] [CrossRef] [PubMed]
- Ou, C.; Yuan, R.; Chai, Y.; Tang, M.; Chai, R.; He, X. A Novel Amperometric Immunosensor Based on Layer-by-Layer Assembly of Gold Nanoparticles-Multi-Walled Carbon Nanotubes-Thionine Multilayer Films on Polyelectrolyte Surface. Anal. Chim. Acta 2007, 603, 205–213. [Google Scholar] [CrossRef]
- Ou, C.; Chen, S.; Yuan, R.; Chai, Y.; Zhong, X. Layer-by-Layer Self-Assembled Multilayer Films of Multi-Walled Carbon Nanotubes and Platinum-Prussian Blue Hybrid Nanoparticles for the Fabrication of Amperometric Immunosensor. J. Electroanal. Chem. 2008, 624, 287–292. [Google Scholar] [CrossRef]
- Ding, Y.; Liu, J.; Jin, X.; Lu, H.; Shen, G.; Yu, R. Poly-L-Lysine/Hydroxyapatite/Carbon Nanotube Hybrid Nanocomposite Applied for Piezoelectric Immunoassay of Carbohydrate Antigen 19-9. Analyst 2008, 133, 184–190. [Google Scholar] [CrossRef]
- Sánchez, S.; Roldán, M.; Pérez, S.; Fàbregas, E. Toward a Fast, Easy, and Versatile Immobilization of Biomolecules into Carbon Nanotube/Polysulfone-Based Biosensors for the Detection of HCG Hormone. Anal. Chem. 2008, 80, 6508–6514. [Google Scholar] [CrossRef]
- Li, N.; Yuan, R.; Chai, Y.; Chen, S.; An, H. Sensitive Immunoassay of Human Chorionic Gonadotrophin Based on Multi-Walled Carbon Nanotube-Chitosan Matrix. Bioprocess Biosyst. Eng. 2008, 31, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.P.; Lee, B.Y.; Lee, J.; Hong, S.; Sim, S.J. Enhancement of Sensitivity and Specificity by Surface Modification of Carbon Nanotubes in Diagnosis of Prostate Cancer Based on Carbon Nanotube Field Effect Transistors. Biosens. Bioelectron. 2009, 24, 3372–3378. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Yuan, R.; Chai, Y.; Min, L.; Li, W.; Xu, Y. Electrochemical Sensing Platform Based on Tris(2,2′-Bipyridyl)Cobalt(III) and Multiwall Carbon Nanotubes–Nafion Composite for Immunoassay of Carcinoma Antigen-125. Electrochim. Acta 2009, 54, 7242–7247. [Google Scholar] [CrossRef]
- Lin, J.; He, C.; Zhang, L.; Zhang, S. Sensitive Amperometric Immunosensor for α-Fetoprotein Based on Carbon Nanotube/Gold Nanoparticle Doped Chitosan Film. Anal. Biochem. 2009, 384, 130–135. [Google Scholar] [CrossRef]
- Jin, W.; Zhang, R.; Dong, C.; Jiang, T.; Tian, Y.; Yang, Q.; Yi, W.; Hou, J. A Simple MWCNTs@paper Biosensor for CA19-9 Detection and Its Long-Term Preservation by Vacuum Freeze Drying. Int. J. Biol. Macromol. 2020, 144, 995–1003. [Google Scholar] [CrossRef]
- Hu, D.; Yang, L.; Deng, S.; Hao, Y.; Zhang, K.; Wang, X.; Liu, Y.; Liu, H.; Chen, Y.; Xie, M. Development of Nanosensor by Bioorthogonal Reaction for Multi-Detection of the Biomarkers of Hepatocellular Carcinoma. Sens. Actuators B Chem. 2021, 334, 129653. [Google Scholar] [CrossRef]
- Ma, S.; Zhang, Y.; Ren, Q.; Wang, X.; Zhu, J.; Yin, F.; Li, Z.; Zhang, M. Tetrahedral DNA Nanostructure Based Biosensor for High-Performance Detection of Circulating Tumor DNA Using All-Carbon Nanotube Transistor. Biosens. Bioelectron. 2022, 197, 113785. [Google Scholar] [CrossRef]
- Biswas, S.; Lan, Q.; Xie, Y.; Sun, X.; Wang, Y. Label-Free Electrochemical Immunosensor for Ultrasensitive Detection of Carbohydrate Antigen 125 Based on Antibody-Immobilized Biocompatible MOF-808/CNT. ACS Appl. Mater. Interfaces 2021, 13, 3295–3302. [Google Scholar] [CrossRef] [PubMed]
- Song, C.K.; Oh, E.; Kang, M.S.; Shin, B.S.; Han, S.Y.; Jung, M.; Lee, E.S.; Yoon, S.Y.; Sung, M.M.; Ng, W.B.; et al. Fluorescence-Based Immunosensor Using Three-Dimensional CNT Network Structure for Sensitive and Reproducible Detection of Oral Squamous Cell Carcinoma Biomarker. Anal. Chim. Acta 2018, 1027, 101–108. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, F.; Dan, W.; Fu, Y.; Liu, S. Construction of Carbon Nanotube Based Nanoarchitectures for Selective Impedimetric Detection of Cancer Cells in Whole Blood. Analyst 2014, 139, 5086–5092. [Google Scholar] [CrossRef]
- Liao, C.; Li, Y.; Tjong, S.C. Graphene Nanomaterials: Synthesis, Biocompatibility, and Cytotoxicity. Int. J. Mol. Sci. 2018, 19, 3564. [Google Scholar] [CrossRef] [PubMed]
- Devasena, T.; Francis, A.P.; Ramaprabhu, S. Toxicity of Graphene: An Update. In Reviews of Environmental Contamination and Toxicology; Springer: Cham, Switzerland, 2021; Volume 259. [Google Scholar]
- Zhao, C.; Song, X.; Liu, Y.; Fu, Y.; Ye, L.; Wang, N.; Wang, F.; Li, L.; Mohammadniaei, M.; Zhang, M.; et al. Synthesis of Graphene Quantum Dots and Their Applications in Drug Delivery. J. Nanobiotechnol. 2020, 18, 142. [Google Scholar] [CrossRef]
- Ye, L.; Kollie, L.; Liu, X.; Guo, W.; Ying, X.; Zhu, J.; Yang, S.; Yu, M. Antitumor Activity and Potential Mechanism of Novel Fullerene Derivative Nanoparticles. Molecules 2021, 26, 3252. [Google Scholar] [CrossRef]
- Malhotra, N.; Audira, G.; Castillo, A.L.; Siregar, P.; Ruallo, J.M.S.; Roldan, M.J.; Chen, J.R.; Lee, J.S.; Ger, T.R.; Hsiao, C.-D.; et al. An Update Report on the Biosafety and Potential Toxicity of Fullerene-Based Nanomaterials toward Aquatic Animals. Oxidative Med. Cell Longev. 2021, 2021, 7995223. [Google Scholar] [CrossRef]
- Dong, J.; Ma, Q. Advances in Mechanisms and Signaling Pathways of Carbon Nanotube Toxicity. Nanotoxicology 2015, 9, 658–676. [Google Scholar] [CrossRef]
- Chen, M.; Qin, X.; Zeng, G. Biodegradation of Carbon Nanotubes, Graphene, and Their Derivatives. Trends Biotechnol. 2017, 35, 836–846. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Deng, X.; Wang, L.; Liu, J.; Xu, K. Clinical Application of Carbon Nanoparticles in Lymphatic Mapping during Colorectal Cancer Surgeries: A Systematic Review and Meta-Analysis. Dig. Liver Dis. 2020, 52, 1445–1454. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.F.; Gu, J. The Application of Carbon Nanoparticles in the Lymph Node Biopsy of CN0 Papillary Thyroid Carcinoma: A Randomized Controlled Clinical Trial. Asian J. Surg. 2017, 40, 345–349. [Google Scholar] [CrossRef]
- Li, Z.; Ao, S.; Bu, Z.; Wu, A.; Wu, X.; Shan, F.; Ji, X.; Zhang, Y.; Xing, Z.; Ji, J. Clinical Study of Harvesting Lymph Nodes with Carbon Nanoparticles in Advanced Gastric Cancer: A Prospective Randomized Trial. World J. Surg. Oncol. 2016, 14, 88. [Google Scholar] [CrossRef]
- Qian, X.; Tucker, A.; Gidcumb, E.; Shan, J.; Yang, G.; Calderon-Colon, X.; Sultana, S.; Lu, J.; Zhou, O.; Spronk, D.; et al. High Resolution Stationary Digital Breast Tomosynthesis Using Distributed Carbon Nanotube X-Ray Source Array. Med. Phys. 2012, 39, 2090–2099. [Google Scholar] [CrossRef]
- Amal, H.; Leja, M.; Funka, K.; Skapars, R.; Sivins, A.; Ancans, G.; Liepniece-Karele, I.; Kikuste, I.; Lasina, I.; Haick, H. Detection of Precancerous Gastric Lesions and Gastric Cancer through Exhaled Breath. Gut 2016, 65, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.Q.; Broza, Y.Y.; Ionsecu, R.; Tisch, U.; Ding, L.; Liu, H.; Song, Q.; Pan, Y.Y.; Xiong, F.X.; Gu, K.S.; et al. A Nanomaterial-Based Breath Test for Distinguishing Gastric Cancer from Benign Gastric Conditions. Br. J. Cancer 2013, 108, 941–950. [Google Scholar] [CrossRef]
- Bittar, R.; Alves, N.G.P.; Bertoldo, C.; Brugnera, C.; Oiticica, J. Efficacy of Carbon Microcoils in Relieving Cervicogenic Dizziness. Int. Arch. Otorhinolaryngol. 2017, 21, 4–7. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The Cochrane Collaboration’s Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, S.; Lv, Z.; Wang, Z.; Zhao, Y.; Xie, Y.; Xu, Y.; Qian, L.; Yang, Y.; Zhao, Z.; et al. Transforming the Synthesis of Carbon Nanotubes with Machine Learning Models and Automation. Matter 2025, 8, 101913. [Google Scholar] [CrossRef]
- Li, X.; Chen, W.; Zhan, Q.; Dai, L.; Sowards, L.; Pender, M.; Naik, R.R. Direct Measurements of Interactions between Polypeptides and Carbon Nanotubes. J. Phys. Chem. B 2006, 110, 12621–12625. [Google Scholar] [CrossRef] [PubMed]
- Ezzeddine, A.; Chen, Z.; Schanze, K.S.; Khashab, N.M. Surface Modification of Multiwalled Carbon Nanotubes with Cationic Conjugated Polyelectrolytes: Fundamental Interactions and Intercalation into Conductive Poly(Methyl Methacrylate) Composites. ACS Appl. Mater. Interfaces 2015, 7, 12903–12913. [Google Scholar] [CrossRef]
- Chen, X.; Fang, J.; Cheng, Y.; Zheng, J.; Zhang, J.; Chen, T.; Ruan, B.H. Biomolecular Interaction Analysis for Carbon Nanotubes and for Biocompatibility Prediction. Anal. Biochem. 2016, 505, 1–7. [Google Scholar] [CrossRef]
- Takada, T.; Kurosaki, R.; Konno, Y.; Abe, S. Interaction of Multi-Walled Carbon Nanotubes with Water-Soluble Proteins: Effect of Sidewall Carboxylation. J. Nanosci. Nanotechnol. 2014, 14, 3216–3220. [Google Scholar] [CrossRef]
- Sen, F.; Boghossian, A.A.; Sen, S.; Ulissi, Z.W.; Zhang, J.; Strano, M.S. Observation of Oscillatory Surface Reactions of Riboflavin, Trolox, and Singlet Oxygen Using Single Carbon Nanotube Fluorescence Spectroscopy. ACS Nano 2012, 6, 10632–10645. [Google Scholar] [CrossRef]
- Lettiero, B.; Andersen, A.J.; Hunter, A.C.; Moghimi, S.M. Complement System and the Brain: Selected Pathologies and Avenues toward Engineering of Neurological Nanomedicines. J. Control. Release 2012, 161, 283–289. [Google Scholar] [CrossRef]
- Moghimi, S.M.; Peer, D.; Langer, R. Reshaping the Future of Nanopharmaceuticals: Ad Iudicium. ACS Nano 2011, 5, 8454–8458. [Google Scholar] [CrossRef]
- Liu, Z.; Davis, C.; Cai, W.; He, L.; Chen, X.; Dai, H. Circulation and Long-Term Fate of Functionalized, Biocompatible Single-Walled Carbon Nanotubes in Mice Probed by Raman Spectroscopy. Proc. Natl. Acad. Sci. USA 2008, 105, 1410–1415. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Fernando, K.A.S.; Liu, J.; Wang, J.; Sun, H.; Liu, Y.; Chen, M.; Huang, Y.; Wang, X.; Wang, H.; et al. Covalently PEGylated Carbon Nanotubes with Stealth Character In Vivo. Small 2008, 4, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Pondman, K.M.; Pednekar, L.; Paudyal, B.; Tsolaki, A.G.; Kouser, L.; Khan, H.A.; Shamji, M.H.; ten Haken, B.; Stenbeck, G.; Sim, R.B.; et al. Innate Immune Humoral Factors, C1q and Factor H, with Differential Pattern Recognition Properties, Alter Macrophage Response to Carbon Nanotubes. Nanomedicine 2015, 11, 2109–2118. [Google Scholar] [CrossRef]
- Sayes, C.M.; Liang, F.; Hudson, J.L.; Mendez, J.; Guo, W.; Beach, J.M.; Moore, V.C.; Doyle, C.D.; West, J.L.; Billups, W.E.; et al. Functionalization Density Dependence of Single-Walled Carbon Nanotubes Cytotoxicity in Vitro. Toxicol. Lett. 2006, 161, 135–142. [Google Scholar] [CrossRef]
- Alimohammadi, Z.; Zamansani, A.; Abreshteh, A.; Edalat, M.; Ebrahimi, Z. Formulation and in vitro evaluation of quercetin loaded carbon nanotubes for Cancer Targeting. Int. Res. J. Eng. Technol. (IRJET) 2023, 10, 962–967. [Google Scholar]
- Yang, H.; Yang, T.; Heng, C.; Zhou, Y.; Jiang, Z.; Qian, X.; Du, L.; Mao, S.; Yin, X.; Lu, Q. Quercetin Improves Nonalcoholic Fatty Liver by Ameliorating Inflammation, Oxidative Stress, and Lipid Metabolism in Db/Db Mice. Phytother. Res. 2019, 33, 3140–3152. [Google Scholar] [CrossRef]
- Di Petrillo, A.; Orrù, G.; Fais, A.; Fantini, M.C. Quercetin and Its Derivates as Antiviral Potentials: A Comprehensive Review. Phytother. Res. 2022, 36, 266–278. [Google Scholar] [CrossRef]
- Sallam, A.A.; Ahmed, M.M.; El-Magd, M.A.; Magdy, A.; Ghamry, H.I.; Alshahrani, M.Y.; Abou El-Fotoh, M.F. Quercetin-Ameliorated, Multi-Walled Carbon Nanotubes-Induced Immunotoxic, Inflammatory, and Oxidative Effects in Mice. Molecules 2022, 27, 2117. [Google Scholar] [CrossRef]
- Zhang, D.; Deng, X.; Ji, Z.; Shen, X.; Dong, L.; Wu, M.; Gu, T.; Liu, Y. Long-Term Hepatotoxicity of Polyethylene-Glycol Functionalized Multi-Walled Carbon Nanotubes in Mice. Nanotechnology 2010, 21, 175101. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Luna, V.; Moreno-Aguilar, C.; Arauz-Lara, J.L.; Aranda-Espinoza, S.; Quintana, M. Interactions of Functionalized Multi-Wall Carbon Nanotubes with Giant Phospholipid Vesicles as Model Cellular Membrane System. Sci. Rep. 2018, 8, 17998. [Google Scholar] [CrossRef] [PubMed]
- Awasthi, S.; De, S.; Pandey, S.K. Surface Grafting of Carbon Nanostructures. In Handbook of Functionalized Carbon Nanostructures; Springer International Publishing: Cham, Switzland, 2024; pp. 1–45. [Google Scholar]
- Yang, M.; Zhang, M. Biodegradation of Carbon Nanotubes by Macrophages. Front. Mater. 2019, 6, 225. [Google Scholar] [CrossRef]
- Liu, Y.; Zhao, Y.; Sun, B.; Chen, C. Understanding the Toxicity of Carbon Nanotubes. Acc. Chem. Res. 2013, 46, 702–713. [Google Scholar] [CrossRef]
- Zhu, Y.; Li, W.; Li, Q.; Li, Y.; Li, Y.; Zhang, X.; Huang, Q. Effects of Serum Proteins on Intracellular Uptake and Cytotoxicity of Carbon Nanoparticles. Carbon N. Y. 2009, 47, 1351–1358. [Google Scholar] [CrossRef]
- Dong, X.; Sun, Z.; Wang, X.; Leng, X. An Innovative MWCNTs/DOX/TC Nanosystem for Chemo-Photothermal Combination Therapy of Cancer. Nanomedicine 2017, 13, 2271–2280. [Google Scholar] [CrossRef]
- Rele, S.; Thakur, C.K.; Khan, F.; Baral, B.; Saini, V.; Karthikeyan, C.; Moorthy, N.S.H.N.; Jha, H.C. Curcumin Coating: A Novel Solution to Mitigate Inherent Carbon Nanotube Toxicity. J. Mater. Sci. Mater. Med. 2024, 35, 24. [Google Scholar] [CrossRef]
- Costa, P.M.; Bourgognon, M.; Wang, J.T.-W.; Al-Jamal, K.T. Functionalised Carbon Nanotubes: From Intracellular Uptake and Cell-Related Toxicity to Systemic Brain Delivery. J. Control. Release 2016, 241, 200–219. [Google Scholar] [CrossRef]
- Sohaebuddin, S.K.; Thevenot, P.T.; Baker, D.; Eaton, J.W.; Tang, L. Nanomaterial Cytotoxicity Is Composition, Size, and Cell Type Dependent. Part. Fibre Toxicol. 2010, 7, 22. [Google Scholar] [CrossRef]
- Heras, A.; Colina, A.; López-Palacios, J.; Ayala, P.; Sainio, J.; Ruiz, V.; Kauppinen, E.I. Electrochemical Purification of Carbon Nanotube Electrodes. Electrochem. Commun. 2009, 11, 1535–1538. [Google Scholar] [CrossRef]
- Mercier, G.; Hérold, C.; Marêché, J.-F.; Cahen, S.; Gleize, J.; Ghanbaja, J.; Lamura, G.; Bellouard, C.; Vigolo, B. Selective Removal of Metal Impurities from Single Walled Carbon Nanotube Samples. New J. Chem. 2013, 37, 790. [Google Scholar] [CrossRef]
- Pełech, I.; Narkiewicz, U.; Kaczmarek, A.; Jędrzejewska, A.; Pełech, R. Removal of Metal Particles from Carbon Nanotubes Using Conventional and Microwave Methods. Sep. Purif. Technol. 2014, 136, 105–110. [Google Scholar] [CrossRef]
- Madani, S.Y.; Mandel, A.; Seifalian, A.M. A Concise Review of Carbon Nanotube’s Toxicology. Nano Rev. 2013, 4, 21521. [Google Scholar] [CrossRef]
- Agnihotri, S.; Mota, J.P.B.; Rostam-Abadi, M.; Rood, M.J. Structural Characterization of Single-Walled Carbon Nanotube Bundles by Experiment and Molecular Simulation. Langmuir 2005, 21, 896–904. [Google Scholar] [CrossRef] [PubMed]
- Hemraj-Benny, T.; Bandosz, T.J.; Wong, S.S. Effect of Ozonolysis on the Pore Structure, Surface Chemistry, and Bundling of Single-Walled Carbon Nanotubes. J. Colloid Interface Sci. 2008, 317, 375–382. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, C.; Li, F.; Cheng, H.-M. Pore Structures of Multi-Walled Carbon Nanotubes Activated by Air, CO2 and KOH. J. Porous. Mater. 2006, 13, 141–146. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, S.C.; Jung, J.H.; Kim, H.J. Pore Characterization of Multi-Walled Carbon Nanotubes Modified by KOH. Chem. Phys. Lett. 2005, 416, 251–255. [Google Scholar] [CrossRef]
- Liu, Y.; Shen, Z.; Yokogawa, K. Investigation of Preparation and Structures of Activated Carbon Nanotubes. Mater. Res. Bull. 2006, 41, 1503–1512. [Google Scholar] [CrossRef]
- Niu, J.J.; Wang, J.N.; Jiang, Y.; Su, L.F.; Ma, J. An Approach to Carbon Nanotubes with High Surface Area and Large Pore Volume. Microporous and Mesoporous Mater. 2007, 100, 1–5. [Google Scholar] [CrossRef]
- Liao, Q.; Sun, J.; Gao, L. Adsorption of Chlorophenols by Multi-Walled Carbon Nanotubes Treated with HNO3 and NH3. Carbon N. Y. 2008, 46, 553–555. [Google Scholar] [CrossRef]
- LU, C.; SU, F. Adsorption of Natural Organic Matter by Carbon Nanotubes. Sep. Purif. Technol. 2007, 58, 113–121. [Google Scholar] [CrossRef]
- Ebbesen, T.W.; Ajayan, P.M. Large-Scale Synthesis of Carbon Nanotubes. Nature 1992, 358, 220–222. [Google Scholar] [CrossRef]
- Eatemadi, A.; Daraee, H.; Karimkhanloo, H.; Kouhi, M.; Zarghami, N.; Akbarzadeh, A.; Abasi, M.; Hanifehpour, Y.; Joo, S.W. Carbon Nanotubes: Properties, Synthesis, Purification, and Medical Applications. Nanoscale Res. Lett. 2014, 9, 393. [Google Scholar] [CrossRef]
- Guo, T.; Nikolaev, P.; Rinzler, A.G.; Tomanek, D.; Colbert, D.T.; Smalley, R.E. Self-Assembly of Tubular Fullerenes. J Phys. Chem. 1995, 99, 10694–10697. [Google Scholar] [CrossRef]
- Guo, T.; Nikolaev, P.; Thess, A.; Colbert, D.T.; Smalley, R.E. Catalytic Growth of Single-Walled Nanotubes by Laser Vaporization. Chem. Phys. Lett. 1995, 243, 49–54. [Google Scholar] [CrossRef]
- Kumar, M.; Ando, Y. Chemical Vapor Deposition of Carbon Nanotubes: A Review on Growth Mechanism and Mass Production. J. Nanosci. Nanotechnol. 2010, 10, 3739–3758. [Google Scholar] [CrossRef]
- Neupane, S.; Lastres, M.; Chiarella, M.; Li, W.; Su, Q.; Du, G. Synthesis and Field Emission Properties of Vertically Aligned Carbon Nanotube Arrays on Copper. Carbon N. Y. 2012, 50, 2641–2650. [Google Scholar] [CrossRef]
- Inami, N.; Mohamed, M.A.; Shikoh, E.; Fujiwara, A. Synthesis-Condition Dependence of Carbon Nanotube Growth by Alcohol Catalytic Chemical Vapor Deposition Method. Sci. Technol. Adv. Mater. 2007, 8, 292–295. [Google Scholar] [CrossRef]
- Ishigami, N.; Ago, H.; Imamoto, K.; Tsuji, M.; Iakoubovskii, K.; Minami, N. Crystal Plane Dependent Growth of Aligned Single-Walled Carbon Nanotubes on Sapphire. J. Am. Chem. Soc. 2008, 130, 9918–9924. [Google Scholar] [CrossRef]
- Naha, S.; Puri, I.K. A Model for Catalytic Growth of Carbon Nanotubes. J. Phys. D. Appl. Phys. 2008, 41, 065304. [Google Scholar] [CrossRef]
- Banerjee, S.; Naha, S.; Puri, I.K. Molecular Simulation of the Carbon Nanotube Growth Mode during Catalytic Synthesis. Appl. Phys. Lett. 2008, 92, 233121. [Google Scholar] [CrossRef]
- Eftekhari, A.; Jafarkhani, P.; Moztarzadeh, F. High-Yield Synthesis of Carbon Nanotubes Using a Water-Soluble Catalyst Support in Catalytic Chemical Vapor Deposition. Carbon N. Y. 2006, 44, 1343–1345. [Google Scholar] [CrossRef]
- Ren, Z.F.; Huang, Z.P.; Xu, J.W.; Wang, J.H.; Bush, P.; Siegal, M.P.; Provencio, P.N. Synthesis of Large Arrays of Well-Aligned Carbon Nanotubes on Glass. Science (1979) 1998, 282, 1105–1107. [Google Scholar] [CrossRef]
- Futaba, D.N.; Hata, K.; Yamada, T.; Hiraoka, T.; Hayamizu, Y.; Kakudate, Y.; Tanaike, O.; Hatori, H.; Yumura, M.; Iijima, S. Shape-Engineerable and Highly Densely Packed Single-Walled Carbon Nanotubes and Their Application as Super-Capacitor Electrodes. Nat. Mater. 2006, 5, 987–994. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Futaba, D.N.; Mizuno, K.; Namai, T.; Yumura, M.; Iijima, S. Water-Assisted Highly Efficient Synthesis of Impurity-Free Single-Walled Carbon Nanotubes. Science 2004, 306, 1362–1364. [Google Scholar] [CrossRef]
- Smiljanic, O.; Stansfield, B.L.; Dodelet, J.-P.; Serventi, A.; Désilets, S. Gas-Phase Synthesis of SWNT by an Atmospheric Pressure Plasma Jet. Chem. Phys. Lett. 2002, 356, 189–193. [Google Scholar] [CrossRef]
- Kim, K.S.; Cota-Sanchez, G.; Kingston, C.T.; Imris, M.; Simard, B.; Soucy, G. Large-Scale Production of Single-Walled Carbon Nanotubes by Induction Thermal Plasma. J. Phys. D Appl. Phys. 2007, 40, 2375–2387. [Google Scholar] [CrossRef]
- Ren, J.; Li, F.-F.; Lau, J.; González-Urbina, L.; Licht, S. One-Pot Synthesis of Carbon Nanofibers from CO 2. Nano Lett. 2015, 15, 6142–6148. [Google Scholar] [CrossRef]
- Service, R.F. Conjuring Chemical Cornucopias out of Thin Air. Science (1979) 2015, 349, 1160. [Google Scholar] [CrossRef]
- Yuan, L.; Saito, K.; Pan, C.; Williams, F.A.; Gordon, A.S. Nanotubes from Methane Flames. Chem. Phys. Lett. 2001, 340, 237–241. [Google Scholar] [CrossRef]
- Yuan, L.; Saito, K.; Hu, W.; Chen, Z. Ethylene Flame Synthesis of Well-Aligned Multi-Walled Carbon Nanotubes. Chem. Phys. Lett. 2001, 346, 23–28. [Google Scholar] [CrossRef]
- Duan, H.M.; McKinnon, J.T. Nanoclusters Produced in Flames. J. Phys. Chem. 1994, 98, 12815–12818. [Google Scholar] [CrossRef]
- Novikov, I.V.; Krasnikov, D.V.; Lee, I.H.; Agafonova, E.E.; Serebrennikova, S.I.; Lee, Y.; Kim, S.; Nam, J.; Kondrashov, V.A.; Han, J.; et al. Aerosol CVD Carbon Nanotube Thin Films: From Synthesis to Advanced Applications: A Comprehensive Review. Adv. Mater. 2025, 37, 2413777. [Google Scholar] [CrossRef] [PubMed]
- Khabushev, E.M.; Kolodiazhnaia, J.V.; Krasnikov, D.V.; Nasibulin, A.G. Activation of Catalyst Particles for Single-Walled Carbon Nanotube Synthesis. Chem. Eng. J. 2021, 413, 127475. [Google Scholar] [CrossRef]
- Nasibulin, A.G.; Moisala, A.; Brown, D.P.; Jiang, H.; Kauppinen, E.I. A Novel Aerosol Method for Single Walled Carbon Nanotube Synthesis. Chem. Phys. Lett. 2005, 402, 227–232. [Google Scholar] [CrossRef]
- Lotfy, V.F.; Fathy, N.A.; Basta, A.H. Novel Approach for Synthesizing Different Shapes of Carbon Nanotubes from Rice Straw Residue. J. Environ. Chem. Eng. 2018, 6, 6263–6274. [Google Scholar] [CrossRef]
- Hamid, Z.A.; Azim, A.A.; Mouez, F.A.; Rehim, S.S.A. Challenges on Synthesis of Carbon Nanotubes from Environmentally Friendly Green Oil Using Pyrolysis Technique. J. Anal. Appl. Pyrolysis 2017, 126, 218–229. [Google Scholar] [CrossRef]
- Ghosh, P.; Soga, T.; Afre, R.A.; Jimbo, T. Simplified Synthesis of Single-Walled Carbon Nanotubes from a Botanical Hydrocarbon: Turpentine Oil. J. Alloys Compd. 2008, 462, 289–293. [Google Scholar] [CrossRef]
- Paul, S.; Samdarshi, S.K. A Green Precursor for Carbon Nanotube Synthesis. New Carbon Mater. 2011, 26, 85–88. [Google Scholar] [CrossRef]
- Kumar, R.; Singh, R.K.; Tiwari, R.S. Growth Analysis and High-Yield Synthesis of Aligned-Stacked Branched Nitrogen-Doped Carbon Nanotubes Using Sesame Oil as a Natural Botanical Hydrocarbon Precursor. Mater. Des. 2016, 94, 166–175. [Google Scholar] [CrossRef]
- Suriani, A.B.; Azira, A.A.; Nik, S.F.; Md Nor, R.; Rusop, M. Synthesis of Vertically Aligned Carbon Nanotubes Using Natural Palm Oil as Carbon Precursor. Mater. Lett. 2009, 63, 2704–2706. [Google Scholar] [CrossRef]
- Moo, J.G.S.; Veksha, A.; Oh, W.D.; Giannis, A.; Udayanga, W.D.C.; Lin, S.X.; Ge, L.; Lisak, G. Plastic Derived Carbon Nanotubes for Electrocatalytic Oxygen Reduction Reaction: Effects of Plastic Feedstock and Synthesis Temperature. Electrochem. Commun. 2019, 101, 11–18. [Google Scholar] [CrossRef]
- Abdullayeva, S.H.; Musayeva, N.N.; Jabbarov, R.B.; Matsuda, T. Synthesis of Carbon Nanotubes from Byproducts of Oil Refiner. WJCMP 2014, 04, 93–100. [Google Scholar] [CrossRef]
- Wang, J.; Shen, B.; Lan, M.; Kang, D.; Wu, C. Carbon Nanotubes (CNTs) Production from Catalytic Pyrolysis of Waste Plastics: The Influence of Catalyst and Reaction Pressure. Catal. Today 2020, 351, 50–57. [Google Scholar] [CrossRef]
- Boufades, D.; Hammadou Née Mesdour, S.; Moussiden, A.; Benmebrouka, H.; Ghouti, M.; Kaddour, O. Optimization of Carbon Nanotubes Synthesis via Pyrolysis over Ni/Al2O3 Using Response Surface Methodology. Fuller. Nanotub. Car. N. 2022, 30, 467–475. [Google Scholar] [CrossRef]
- Ahmad, S.; Liao, Y.; Hussain, A.; Zhang, Q.; Ding, E.X.; Jiang, H.; Kauppinen, E.I. Systematic Investigation of the Catalyst Composition Effects on Single-Walled Carbon Nanotubes Synthesis in Floating-Catalyst CVD. Carbon N. Y. 2019, 149, 318–327. [Google Scholar] [CrossRef]
- Fathy, N.A. Carbon Nanotubes Synthesis Using Carbonization of Pretreated Rice Straw through Chemical Vapor Deposition of Camphor. RSC Adv. 2017, 7, 28535–28541. [Google Scholar] [CrossRef]
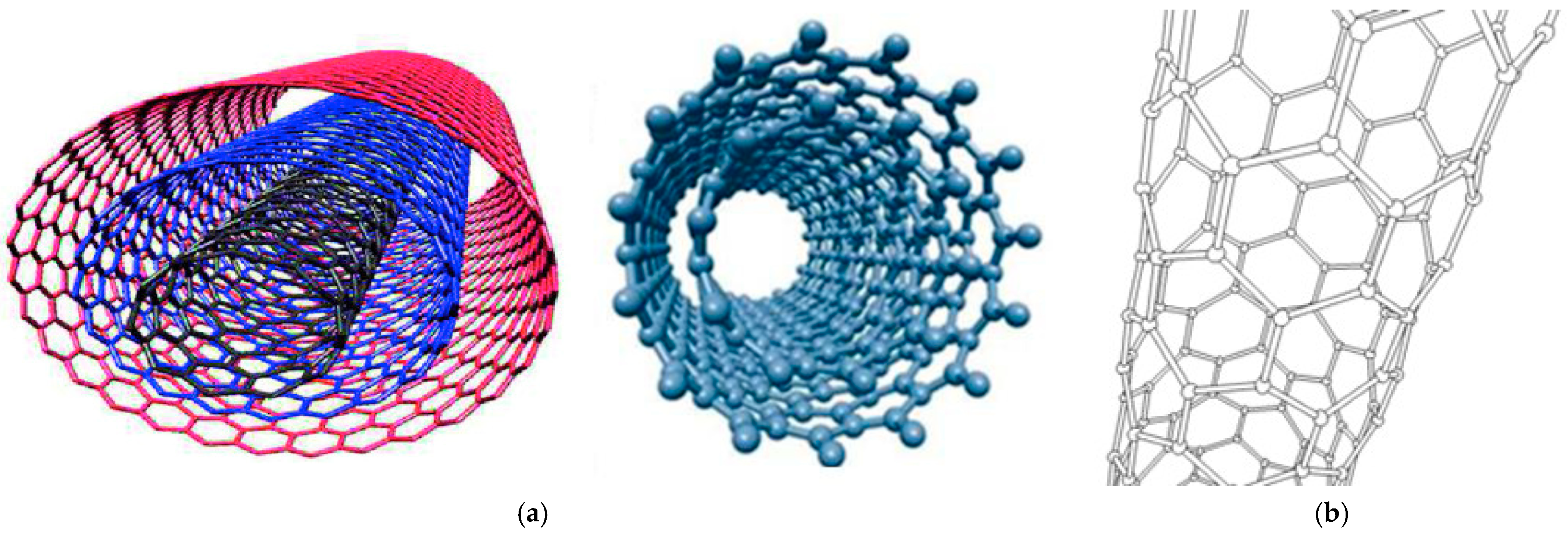
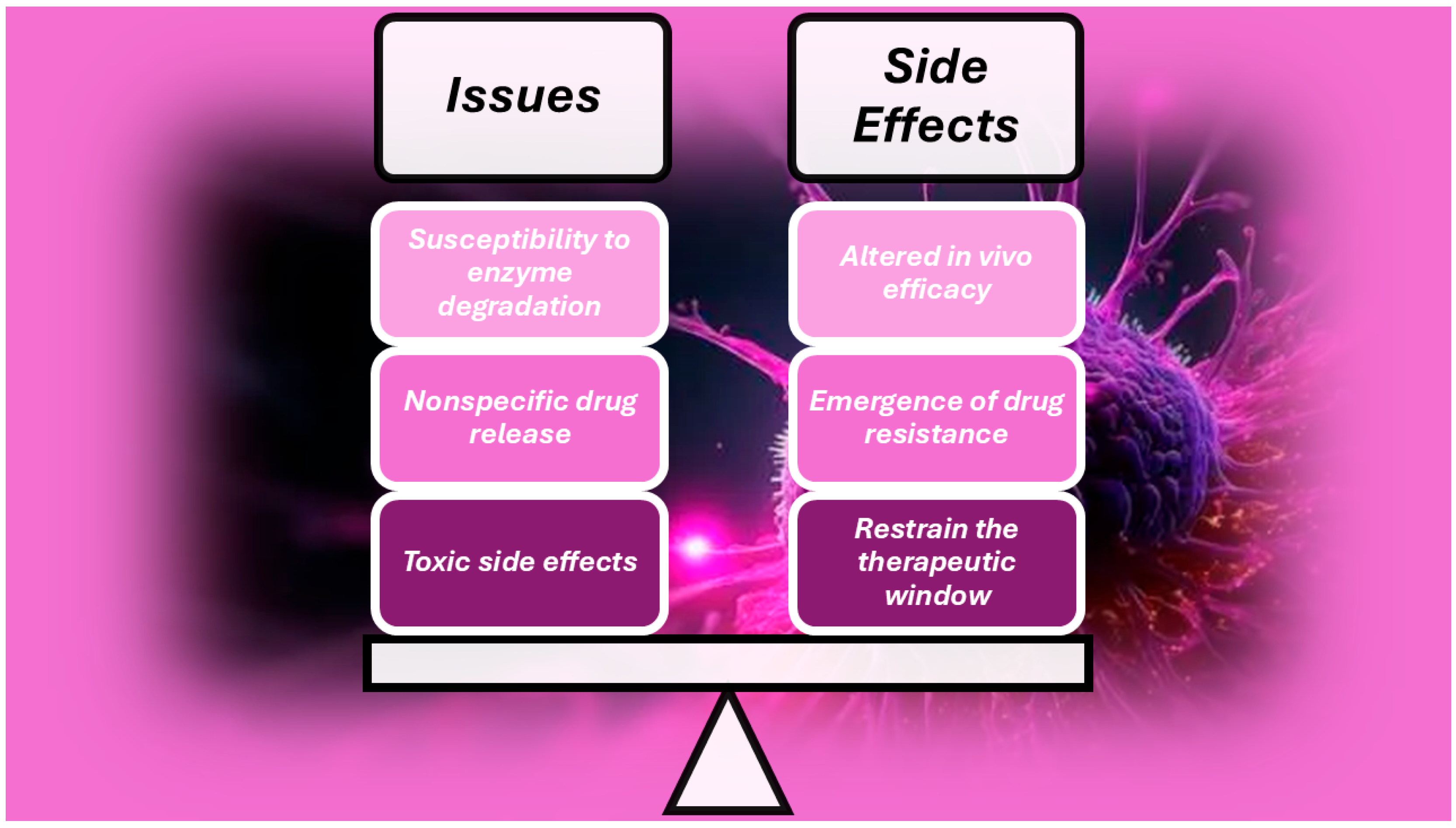
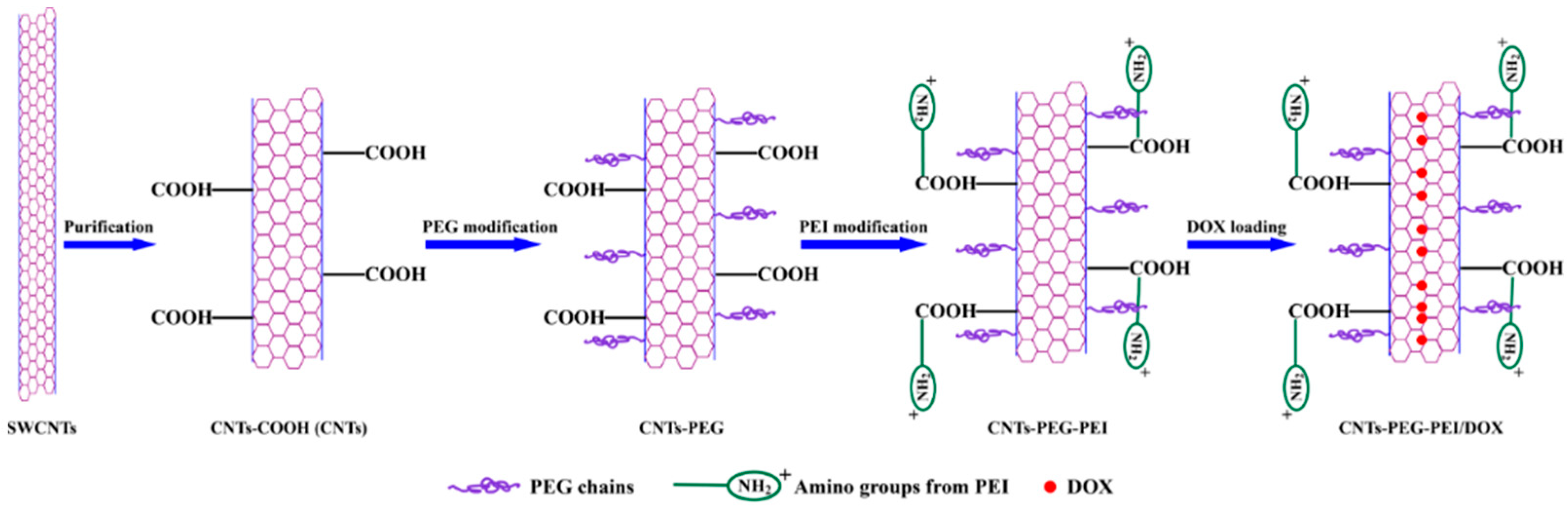
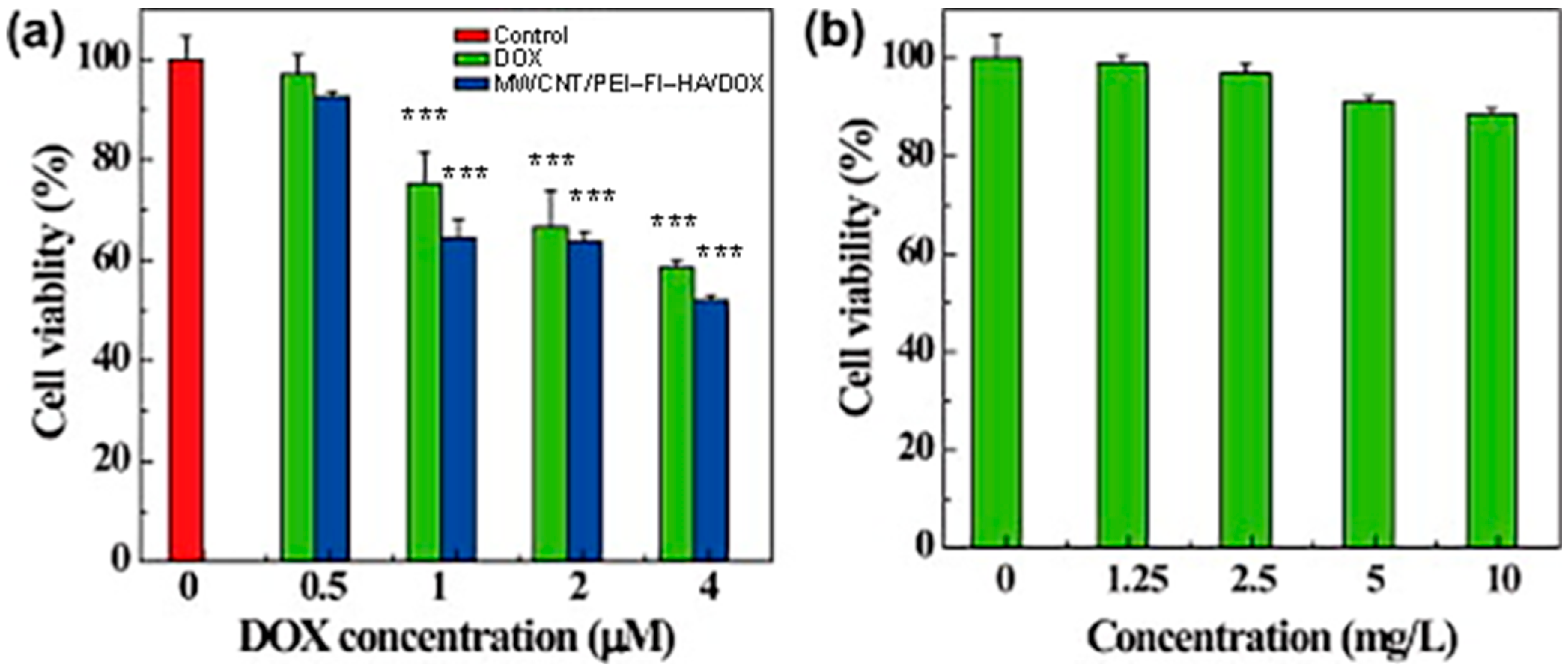



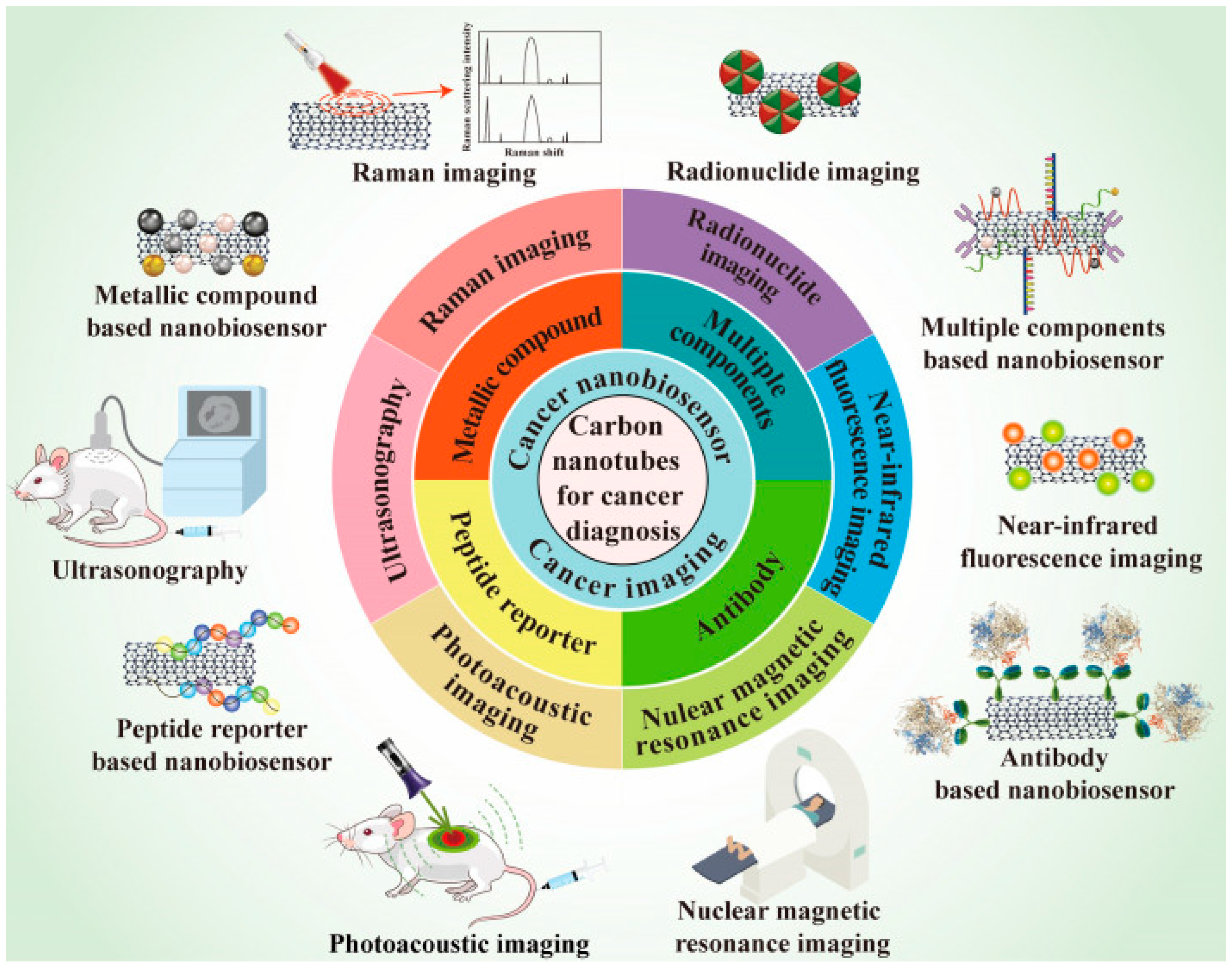
| CNTs | Measures | Cell Line/Animal Models | Drug(s) | Concentration/Dose | Results | Refs |
|---|---|---|---|---|---|---|
| MWCNTs | L = 330 nm Ø = 30 nm | BM-MSCs, MDA-MB-231 CD44high, CD24low CSCs | Pt-NPs, PBI | 100 µM | Cause cell cycle arrest, diminish drug resistance Impede DNA repair in breast CSCs. | [79] |
| CNTs | N.R. | Kunming mice | Span, PEG, FA Paclitaxel | 350 mg/kg | Penetrate breast tumours Inhibited development, induced tumour cell death | [80] |
| SWCNTs | N.R. | HT-29 | Porphyrin, PEG | 25 mg/mL | No antitumour activity | [84] |
| MWCNTs | Ø = 17.1 ± 3.0 nm | C540 Male Balb/c mice | Poly pyrrole | 250 mg/mL, 10 mg/kg | Concentration-dependent cytotoxicity under multi-step ultrasonic irradiation (8.9% cell viability for 250 mg/mL) 75% Necrosis and 50% TVR after 10 days of SDT | [81] |
| MWCNTs | Ø = 10 nm L = 5–15 µm | Male Balb/c mice | CREKA | MWNTs-PEG 2 mg/kg CMWNTs-PEG 4 mg/kg | 6.4 Times ⬆ accumulation in tumour tissue Xenograft eradicated after 4 cycles of illumination | [82] |
| MWCNTs | Ø = 5–20 nm L = 1–10 µm | HepG2, HeLa cells C57BL/6J female mice | PEG-O-CNTs | 0–1000 mL 1 mg/mL injected in tumour at 200 µL/cm3 | ⬆ Cell toxicity of PEG-O-CNTs, O-CNTs, pure CNTs Continuous-wave NIR laser diode (808 nm) for 10 min ⬆ TVR in animal group (PEG-O-CNTs) | [83] |
| CNTs | Functionalizing Molecules | Effectiveness | Tumour Model | Biocompatibility Test | Refs. |
|---|---|---|---|---|---|
| SWNTs | PEG | ⬆ Solubility, prevent particle aggregation, ⬇ side effects | Gastric cancer | ⬇ Toxicity towards normal tissue | [91] |
| SWNTs/MWNTs | PEI | ⬆ Solubility, homogeneity, dispersity, ⬇ particle size | Cervical cancer | N/A | [92] |
| ⬆ Positive charge to interact with siRNA | |||||
| SWNTs | HA | ⬆ Stability in serum, overcome MDR | Ovarian cancer | No cytotoxicity to normal tissue | [93] |
| Target CD44-overexpressing cancer cells | No drop in mice weight | ||||
| MWNTs | Chitosan | ⬆ Solubility, ⬆ cell-penetrating ability, ⬇ toxicity | Breast cancer | ⬇ Cytotoxicity | [94] |
| MWNTs | PLGA | ⬆ Dispersity, ⬇toxicity, provide, tune the temporal release | Osteosarcoma | ⬇ Cytotoxicity in normal cells | [95] |
| Provide attachment sites for drugs | |||||
| SWNTs | CD33 mAB | Recognize and specifically target the GNM-CD33+ cells | Glioblastoma | N/A | [96] |
| SWNTs | IGF1R mAB/HER2 mAB | Target IGF1R and HER2 surface receptors | Breast cancer | ⬇⬇⬇ In vitro toxicity in normal cells | [97] |
| SWNTs | RGD peptide | Target αvβ3-expressing cancer cells | MM | ⬇ Toxicity in vitro | [98] |
| SWNTs | EGF receptor | Active targeting ability, ⬆ uptake of drugs | HSC, NSC | ⬇⬇⬇ Toxicity in vitro and in vivo | [99] |
| Drug/Gene | Modified | Cancer Type | In Vitro | In Vivo | CNTs | Therapeutic Outcome | Refs |
|---|---|---|---|---|---|---|---|
| Pt (IV) drug, PD | PL-PEG F | Testicular cancer | Ntera-2 | N.R. | SWCNT | 25 Folds ⬆ cytotoxicity | [110] |
| CP | Covalent amide linkage | Head, neck cancer | HNCC | N.R. | SWCNT | ⬆ Effective than free CP and siRNA conjugate | [99] |
| CA | Interior filling | Bladder cancer | EJ28 | N.R. | SWCNT MWCNT | Controlled release properties | [111] |
| OP | PEG600 F | Colorectal cancer | HT29 | N.R. | MWCNT | Delayed cytotoxic activity | [112] |
| DOX | PEGylation F | N.R. | Ascites Sarcoma 180 | N.R. | SWCNT | ⬆ Retention of drug in situ | [113] |
| ⬇ Effect on other tissues | |||||||
| Not-F | Breast cancer | MCF-7 | N.R. | MWCNT | ⬆ Cytotoxicity | [114] | |
| P-gp F | Leukaemia | K562 | N.R. | SWCNT | ⬆ Cellular uptake | [115] | |
| 23 folds ⬆ cytotoxicity | |||||||
| PTX | PEGylated F | Lung cancers | A549, NCI–H460 | N.R. | SWCNT | ⬆ PTX activity | [116] |
| Ovarian cancer | OVCAR3 | N.R. | SWCNT | Chemosensitizer, ⬆ cell death | [117] | ||
| Poly citric acid F | Lung, ovary cancer | A549, SKOV3 | N.R. | MWCNT | ⬆ Potency | [118] | |
| PEGylated F | N.R. | N.R. | Murine 4T1 | SWCNT | ⬇⬇⬇ Tumour growth | [119] | |
| 10 folds ⬆ uptake | |||||||
| SB-T-1214, TAXO | Biotin F | Lung cancer, leukaemia | L1210FR, L1210 W138 | N.R. | SWCNT | ⬆ Target due to biotin | [120] |
| GEM | Folic acid F | Breast cancer | MCF-7 cells | N.R. | MWCNT | ⬆ Cytotoxic than free GEM | [121] |
| PEGylated F | Pancreatic cancer | N.R. | BxPC-3–B/c | ⬇ Metastatic lymph nodes | |||
| HIF-1α siRNA | Cationic F | N.R. | N.R. | MiaPaCa | SWCNT | ⬇⬇⬇ Tumour growth | [122] |
| 2/HRE MM | |||||||
| Anti-EGFP siRNA | PEI and Pyridinum F | Lung cancer | H1299 | N.R. | MWCNT | ⬆ Cytotoxicity | [123] |
| Cyclin A2 siRNA | Amine (NH3+) F | Leukaemia | K562 | N.R. | SWCNT | ⬇ Cell proliferation and | [124] |
| apoptosis | |||||||
| PLK 1 siRNA | NH3+ F | Lung cancer | Calu6 | LCXGM | MWCNT | ⬇⬇⬇ Tumour | [125] |
| siNEG siRNA | Amidation with PUT SPERD, SPER | Lung cancer | A549 | N.R. | SWCNT MWCNT | ⬇ Tumour proliferation | [126] |
| Bcl9l siRNA | Aptamer and Pyr-PEI F | Breast cancer | MDA-MB-231 | N.R. | SWCNT | Targeted silencing activity | [127] |
| GAPDH siRNA | PEI F | Cervical cancer | HeLa | N.R. | SWCNT | Induced cell death | [92] |
| siTOX, siNEG | Cationic DD F | Cervical, lung cancer | HeLa, A549 | N.R. | MWCNT | ⬇ Toxicity, effective delivery Gene silencing capabilities | [128] |
| siRNAs | |||||||
| PLK-1 & siTOX siRNAs | NH2-F or cationic liposomes | Breast, cervical, lung, melanoma, prostate, renal, kidney cancers | Calu6, A549, DU145 | LCXGM | MWCNT | Apoptosis, ⬇⬇⬇ tumour | [129] |
| C-33A, MCF-7, HEK293 HeLa, NIH 3T3 B16F10 | |||||||
| PLK1 siRNA | NH4+ and Guanidium DD | Cervical cancer | HeLa | N.R. | MWCNT | Significant silencing of PLK-1 | [130] |
| RNAi | PEHI-pHSP-shT, | Breast cancer | MCF-7 | Nude mice | SWCNT | Gene knockdown, ⬆AA | [131] |
| pDNA | Cationic glyP F | Cervical cancer | HeLa | N.R. | SWCNT | Biocompatible, ⬆ transfection * | [132] |
| p53 plasmids | Ethylenediamine F | Breast cancer | MCF-7 | N.R. | SWCNT | Induced apoptosis | [133] |
| pDNA | Ammonium F | Cervical cancer | HeLa, CHO | N.R. | SWCNT & MWCNT | First reported gene carrier | [134] |
| GFP gene | PAMAM | Cervical cancer | HeLa | N.R. | MWCNT | ⬆ GFP gene transfection | [135] |
| dsDNA | Multi-F | Epithelial cancer | Mouse ovarian epithelial | N.R. | SWCNT | Targeted drug delivery | [136] |
| miRNA | PEI-g-GNR | Cervical cancer | HeLa | N.R. | MWCNT | New nonviral vector for in situ detection | [137] |
| dsODN-NF-kB | Carbodiimide F | Cervical cancer | HeLa | N.R. | SWCNT | Targeted successful deliver | [138] |
| ANT c-myc ODNs | PAMAM | Breast, liver cancer | MCF-7, MDA-MB-435, HepG2 | N.R. | MWCNT | ⬆⬆⬆ Gene efficiency | [139] |
| MUC-1 Apt | Carboxylate F | Breast, lung cancer | MCF-7, Calu-6 | N.R. | MWCNT | Aptamer successful integration | [140] |
| CNTs | Functionalised Molecules | Effectiveness | Tumour Model | Biocompatibility Test | Refs. |
|---|---|---|---|---|---|
| MWCNTs | FA | Targeted and pH-sensible release of DOX | N.R. | N.R. | [141] |
| SWCNTs | PEG-10–10%PEI/pDNA | Allowed dosage 58-fold ⬇ conventional IC50 | AGS and L929 * | ⬇ Toxicity | [91] |
| ⬆ WS, ⬆ biological fluids dispersity | |||||
| SWCNTs | PEG-PCL and PEG-PCL-PEI | Faster acidic DOX release; ⬆ anticancer efficacy, ⬆ WS | MCF-7 * | ⬆ Biocompatibility | [142] |
| SWCNTs | ALG, CHI, FA, DOX | Precise magnetic field-dependent CNT vibration causing cancer cell membrane destruction and DOX release | Lung cancer * | ⬆ Biocompatibility | [143] |
| SWCNTs | COOH-, PEG- PEI- DOX | Faster acidic DOX release, ⬆ Antitumour activity | MCF-7 * | ⬇ Toxicity to normal cells | [100] |
| ⬆ Dispersibility, ⬆ Affinity for tumour cells. | |||||
| SWCNTs | PEI-BET-DOX and SUR siRNA | ⬆⬆⬆ pH-responsive lysosomal escape of siRNA | HeLa, A549 *,** | ⬇ Toxicity to normal cells | [144] |
| ⬆ Antitumour properties | |||||
| SWCNTs | Chim/PEI/5-FU/CNT | ⬆⬆⬆ Tissue penetrability, ⬆⬆⬆ DL, CT allowed | Gastric cancer * | ⬆ Biocompatibility | [145] |
| ⬇ Invasion and proliferation, apoptosis in 5-FU-RCCs | |||||
| SWCNTs | II-NCC | ⬆⬆⬆ SWCNTs water dispersion; ⬆ Anticancer effects of CAP | Caco-2 * | ⬆ Biocompatibility | [146] |
| MWNTs | iRGD-PEI-MWNT-SS-CD/pAT2 | ⬆ WS and complexation capacity by PEI, ⬇⬇⬇ Tumour growth | A549 *,** | ⬆ Biocompatibility | [147] |
| Target smart release in TRE by SS | |||||
| SWCNTs | PEG and PEI | ⬆ WS, ⬆ Cytotoxicity | AMJ13 * | ⬇ Cytotoxicity to normal cells | [148] |
| TT/Modulation | DDS | TM | Model | Effectiveness | Refs. |
|---|---|---|---|---|---|
| Cytoplasm | SWNT-PS/siRNA | PTT, GT | Hela | ⬆ Gene transport capacity, ⬆ antitumour activity Controlled gene release | [156] |
| Cytoplasm | SWNT-CY7-IGF-1Ra | PTT, IT | ASPC-1, BXPC-3 PANC-1 SW1990 * | Precise tumour-targeting therapy, ⬆ body weight ⬆ Survival rate of tumour-bearing mice | [157] |
| MITO | SWNTs-PL-PEG-NH2 | TAT | H22 liver cancer | Selective ⬇⬇⬇ of tumour mitochondria Tumour cell apoptosis | [158] |
| CSCs | N.R. | IT | MDA-MB-231 breast cancer | Realise active targetability towards breast CSCs | [154] |
| Antigen-presenting cells | MWNTs-CpG-αCD40-OVA | IT | B16F10 melanoma | ⬆ Co-loading ability of OVA, CpG, and anti-CD40 Ig ⬇ TG and metastasis | [159] |
| TV | iRGD-PEI-MWNT-SS-CD/pAT2 | CT | A549 lung cancer | ⬇⬇⬇ TG and neovascularization | [147] |
| Cytoplasm | SWCNT-FA/DOX | CT, NIR-I | Lung cancer A549 | External-stimuli-dependent DOX release, ⬆ anticancer effects | [160] |
| Cytoplasm | SWNT-HIF-1α/siRNA | GT | Pancreas | Transfected tumour, activated RNAi response, ⬇⬇⬇ TG | [122] |
| Cytoplasm | Ox-DWNT/siRNA | GT | Prostate | Prevent surviving creation and induce apoptosis by the release of siRNA into cytoplasm | [161] |
| Nucleus | PEG/SWNTs/DOX | PTT + CT | Breast | ⬆ Delivery effectiveness, ⬆ DOX localisation/accumulation inside nucleus, ⬆⬆ killing of cancer cells | [162] |
| Nucleus | SWNTs-carrier | CT | Colorectal | Targeted therapy, regulated medication release | [163] |
| Nucleus | f-SWNTs/p53 | GT | Breast | ⬆ Transport and targeting gene into the nucleus, apoptosis | [133] |
| MITO | MWNT-Rho (PtBzt + BP) | CT | Ovarian | Still ⬇ selective | [164] |
| MITO | PEG/CNTs/ABT737 | CT | Lung | ⬆ Cell targeting to mitochondria, apoptosis | [165] |
| MITO | P-D-CS-CNTs | PTT | Bladder | ⬆ Mito targeting with damage, ROS burst, cancer cells death | [166] |
| MITO | PL-PEG-SWNT | PAT | Breast | MITO malfunction, MITO outer membrane permeabilization | [167] |
| ECM | MWNTs | PTT | Epidermoid | ⬇⬇⬇ Tumours, ⬇ volume, collagen destruction, cell damage | [168] |
| CCSs | SWNT-Raw, SWNT-COOH | CT | Osteosarcoma | Activated TGFβR1, ⬇⬇⬇ its signalling, ⬇ OSCs population | [169] |
| TV | DOX/CD-CNT, CUR/CD-CNT | PTT + CT | Hepatocellular | ⬆ DEE and achieved sustained release of both drugs | [170] |
| TV | iRGD-PEI-MWNT-SS-CD/pAT2 | CT | Lung | ⬆ CU, TE, ⬇⬇⬇ angiogenesis, ⬇⬇⬇ TG | [147] |
| PD-1/PD-L1 | Rg3-CNT | IT | Breast | Inhibit PD-1/PD-L1 axis and the TNBC cell growth | [171] |
| IMs | MWNTs-DOX and MWNTs-CpG | IT + CT + PTT | Melanoma | ⬇⬇⬇ TG, ⬆ CD4+, CD8+ T cells, ⬆ TAM shifting ⬇ Tregs in TME | [172] |
| CNTs | Functionalizing Molecules | Effects | TM | Biocompatibility | Refs. |
|---|---|---|---|---|---|
| MWNT | DOX, Cis, PEG, FA | Stopped Cisplatin release, pH-sensitive release, synergic antitumour impact | L929, MCF-7 | ⬆ Biocompatibility | [178] |
| SWCNTs | DOX-CS/PNIPAAm | ⬆ Release at 40 °C than 25 °C, at pH 5.0 than pH 7.4 | HeLa | ⬆ Biocompatibility | [180] |
| ⬆ dual stimuli DOX release (NIR + AE of TME) | ⬆ Biocompatibility | ||||
| SWNTs | PEG | ⬆ WS, prevent PA | Gastric cancer | ⬇ Toxicity to NTs | [91] |
| SWNTs/MWNTs | PEI | ⬆ WS, homogeneity and dispersity, ⬇ particle size, ⬆ PC, ⬆ interaction with siRNA | Cervical cancer | N/A | [92] |
| SWNTs | HA | ⬆ SS, ⬆ target CD44-overexpressing cancer cells, overcome MDR | Ovarian cancer | No cytotoxicity to NTs | [93] |
| MWNTs | CS | ⬆ Water solubility and cell-penetrating ability | Breast cancer | ⬇ Cytotoxicity | [94] |
| MWNTs | PLGA | ⬆ Dispersity, ⬆ attachment sites, tuned temporal release | Osteosarcoma | ⬇ Cytotoxicity in NC | [95] |
| SWNTs | CD133 mAB | Recognise and specifically target the GNM-CD33+ cells | Glioblastoma | N/A | [96] |
| SWNTs | IGF1R mAB and HER2 mAB | Target IGF1R and HER2 surface receptors | Breast cancer | Negligible toxicity in NCs | [97] |
| SWNTs | RGD peptide | Target αvβ3-expressing cancer cells | MM | ⬇ Toxicity in vitro | [98] |
| SWNTs | EGF receptor | Active targeting ability and ⬆ uptake of drugs | HC, NC | Negligible toxicity | [99] |
| CNTs | Functional Molecules | Effectiveness | Tumour Model | Observations | Refs. |
|---|---|---|---|---|---|
| MWCNT | Ag NPs | ⬆ NIR LA at 670 nm | Melanoma B16/F10 cells | ⬆ CNT/Ag optical absorption to CNTs and Ag NPs | [210] |
| MWCNT | PEG | ⬆ MWCNTs WS | Melanoma | ⬇⬇⬇ Tumour size in the cancerous mice | [83] |
| MWCNT | –COO, –COOPt, –Pt NPs | –COO ⬆ CNTs WS, Pt NPs ⬆ LA at 1064nm | Cancer PC3 cells | PP ⬆ cytotoxicity due to ⬆ temperature of CCs | [190] |
| MWCNT | –COO, –COOAu, –Au NPs | –COO ⬆ CNTs WS, Au NPs ⬆ LA at 1064nm | MCF7 cells | PP ⬆ cytotoxicity due to ⬆ temperature of CCs | [189] |
| MWCNT | MTX, PEI, FA | MTX-based ACA, FA-based TP PEI-based hydrophilicity | MCF7 cells | ⬆ Synergistic effect of MTX and PTT (808 nm laser) MWCNT-MTX-PEI-FA are absorbed selectively | [202] |
| MWCNT | PS MAA | Antibody against prostate-specific MA | Prostate cancer LNCaP cells | > 80% cell ablation with a single 30-s (a 532-nm) | [211] |
| MWCNT | Au NSs | ⬆ Biocompatibility, ⬆ photothermal efficiency | Melanoma B16F10 mice | MWCNT/Au NSs have 12.4% ⬆ PE (808 nm) | [184] |
| MWCNT | PEG | ⬆ Photothermal transduction (NIR) | BPH | ⬇ Prostate size, apoptosis in PEC | [212] |
| SWCNTs/MWCNTs | PL, SL | BDS with ⬆ PE, TS | HeLa, MRC-5 cells | Muted surviving expression, ⬇⬇⬇ TG PE under 808 nm NIR light | [156] |
| MWCNT | TiO2 NPs | Absorb and scatter the 808 nm NIR light | Melanoma | Selective tumour death, ⬇ HR, ⬆ necrosis | [213] |
| SWCNT | anti-IGF-1R, CY7 | WS, BS, LT SWCNT-CY7-IGF-1R | PDCA | Target to PDCA for dye imaging-guided PTT | [157] |
| CNTs | Functionalized Molecules | Effectiveness | Tumour Model | Biocompatibility Test | Refs. |
|---|---|---|---|---|---|
| SWCNT | HA, Ce6 | ⬆ SWCNTs stability, WD (HA), Ce6-based ACA by PDT | Colon cancer cells | Colon cancer cell death, ⬆ PDT capacity | [194] |
| SWCNT | ZnMCPP | >50% ⬆ singlet and triplet oxygen quantum yields | MCF-7 breast cells | 64% ⬇ CV at 40 M (C1), 97-95% ⬇ CV (C2,3) | [192] |
| MWCNT | OEG, DOX, FA | OEG used to link DOX with CNT DOX used as anticancer drug FA act as the system’s targeted ligand | HeLa, L929, A549 | ⬆ Killing of cancer cells when exposed to light. | [214] |
| SWCNT | AA, ZnMCPP | ⬆ Lifetimes, quantum yields, singlet oxygen quantum yields | MCF-7 | 77% cytotoxicity by combined therapy | [193] |
| CNTs | FM | Effectiveness § | TM | Biocompatibility | NIR Laser | Refs. |
|---|---|---|---|---|---|---|
| MWCNTs | PVPy-S-PEG-FA, DOX | ⬆ ATA, ⬆ WD, ⬆ BCT, ⬆ DL, ⬆ PC of CNTs by PVPy, pH-sensitive | HeLa | ⬆ Biocompatibility | 808 | [198] |
| MWCNTs | ED | ⬆ ATA, ⬆ AA of MTX, ⬆ CD by SE, MWCNT-ED-MTX = MWCNT-ED-FA * | MCF7 | N.R. | 808 | [202] |
| MWCNTs | Ge, Le | ⬆ AA by LH, ⬆ biocompatibility, ⬆ HDP, ⬆ PC | MCF-7 | ⬇ Danger to NC | 808 | [200] |
| MWCNTs | MTX, PEI, FA | ⬆ ATA, ⬆ WD by PEI, ⬆ AA of MTX by SE with PPT | MCF-7 | N.R. | 808 | [202] |
| SWCNTs | ANXA5 | ⬆ Stimulation of IS, AE by SWCNT-ANXA5 SE | EMT6 BCCs | N.R. | 980 | [185] |
| CNTs | MXene | ⬇ CNT aggregation, DOX DL = 85.6%, ⬇⬇⬇ HeLa cells by PTT + DOX SE | HeLa | N.R. | 650/808 | [203] |
| CNTs | FM | Effectiveness | TM | Biocompatibility | Refs. |
|---|---|---|---|---|---|
| SWCNHs | ICG | ⬆ WD, ⬆ photostability, ⬆ AA by PTT + PDT SE | 4T1 BCCs * | ⬆ Photostability, ⬆ biocompatibility | [204] |
| SWCNHs | Ce6, Gd3+ | ⬆ IS, ⬆ ATA, ⬆ TP, ⬆ ISR by PTT + PDT SE in AMMs | 4T1 | N.R. | [206] |
| SWCNHs | Hyp | ⬆ WS ⬇ 4T1 growth by PDT + PTT SE | 4T1 * | ⬆ Photostability, ⬆ biocompatibility | [205] |
| MWCNT | MnO2, Ce6 | O2 + H+ production by MnO2 ⬇ TM, ⬆ potential for IG PDT + PTT SE | HeLa * | ⬆ Biocompatibility | [207] |
| SWCNT | PEG, Fe3O4, CQDs, DOX, sgc8c | ⬆ AA by PTT + PDT + CT by SE | HeLa mice | ⬆ Biocompatibility | [208] |
| CNP@SiO2 | DOX | pH responsive drug delivery, ⬆ PTT, ⬆ CT, ⬇⬇⬇ TD | 4T1 cells | N.R. | [215] |
| SWCNT | HA, HMME | ⬆ WS, HMME = PDT agent, ⬆ AA by PDT + PTT SE | B16F10, MMCs | ⬆ Biocompatibility | [196] |
| CNTs | FM | Effectiveness | TM | Biocompatibility | Refs. |
|---|---|---|---|---|---|
| MWCNTs | COOH | ⬆ WS, ⬆ CSA, ⬆ CP, ⬆ MA | H22 HCCs | N.F. | [237] |
| MWCNTs | Rg3 | Puffed ginseng, ACA, Apoptosis, ⬇ PD-L1 expression | TNBC | N.F. | [171] |
| SWCNTs | CpG | ACA in gliomas, ⬇ CCP, ⬇ invasion/migration | HCCsT116 | ⬆ Mice survival rate | [238] |
| MWCNTs | DOX/CpG | ⬆ WD; no change in MWCNTs PS, ⬇ TG, ⬆ CD4+, ⬆ CD8+, ⬆ T cells | B16 MCs | Biocompatible to normal cells | [172] |
| SWCNTs | COOH/OVA | Primary immunisation/mice, ⬆ anti-ovalbumin antibody response | AMBCs | ⬇ Toxicity, ⬇ inflammation | [239] |
| MWCNTs | PDAEMA | ⬆ Design flexibility, ⬆ control on SARs, ⬆ SE, ⬆ CU | B16-F10 | ⬆ Biocompatibility | [240] |
| CNTs | DM | Effect | Refs. |
|---|---|---|---|
| SWCNTs | RI | Spots of RSs were visible in colon-26 cells after 5 days of administration of o-SWNTs-PEG | [251] |
| SWCNTs | RI | ⬆ SERS-E suitable for labelling and fast RI of biological samples | [252] |
| SWCNTs | MRI | Excellent MRI functions for tumour diagnosis | [253] |
| MWCNTs | MRI | ⬆ Longitudinal proton relaxation process, T1 enhanced MRI effect | [254] |
| MWCNTs | US | ⬆ Contrast in ultrasonic imaging | [255] |
| MWCNTs | US | Strong, long-lived and ⬆-quality ultrasound signal after sonication treatment | [256] |
| SWCNTs | PAI | Clear and stable PA signals | [257] |
| MWCNTs | PAI | Precise target to the tumour site in vivo, ⬆ PA imaging effect | [258] |
| MWCNTs | RNI | Easy and direct SPECT/CT imaging | [259] |
| SWCNTs | RNI | ⬆ Tumour tissue accumulation for the subsequent radionuclide imaging | [260] |
| SWCNTs | NIR-FI | ⬆ Signal-to-noise performance, ⬆ specificity to ovarian tumour and tumor nodules | [261] |
| SWCNTs | NIR-FI | ⬆ Resolution intravital tumour vessel images through the thick skin in live mice | [262] |
| MWCNTs | NBSs | ⬆ Biosensing ability, wide linear range for detecting miR-21, ⬇⬇⬇ detection limit | [263] |
| SWCNTs | NBSs | Broad detection range, ⬇ detection limit, ⬆ specificity to only OPN in prostate cancer | [264] |
| MWCNTs | NBSs | Simple detection of CDK1, report the enzymatic activity of CDK1 for cancer diagnosis | [265] |
| MWCNTs | NBSs | ⬆ Selectivity/sensitivity to HPV-18, early, rapid, easy, and accurate diagnosis of cervical cancer | [266] |
| CNTs | Cell Line/Biomarkers | Linear Range | LoD | Techniques | Ref. |
|---|---|---|---|---|---|
| SWCNTs | PSA | N.R. | 250 pg/mL | Electrochemical | [288] |
| SWCNTs | PSA | 0.4–40 pg/mL | 4 pg/mL | Immune sensing | [289] |
| MWCNTs | AFP | 0.02–2.0 ng/mL | 8.0 pg/mL | Immune sensing | [290] |
| MWCNTs | CEA | 0.5–15.0 and 15.0–200 ng/mL | 0.01 ng/mL | Immune sensing | [291] |
| MWCNTs | AFP | 0.1–15.0 and 15.0–200.0 ng/mL | 0.08 ng/mL | Immune sensing | [292] |
| MWCNTs | CA 19-9 | 12.5–270.0 U/mL | 8.3 U/mL | Immune sensing | [293] |
| MWCNTs | hCG | Up to 600 mIU/mL | 14.6 mIU/mL | Electrochemical | [294] |
| MWCNTs | hCG | 0.8–500 mIU/mL | 0.3 mIU/mL | Electrochemical | [295] |
| CNTs | PSA | 1–100 ng/mL | 1.0 ng/mL | Electrochemical | [296] |
| MWCNTs | CA 125 | 1.0–30 and 30–150 U/mL | 0.36 U/mL | Electrochemical | [297] |
| CNTs | AFP | 1–55 ng/mL | 0.6 ng/mL | Immune sensing | [298] |
| MWCNTs | CA19-9 | 0–1000 U/mL | N.R. | Electrochemical | [299] |
| CNTs | GP73 | 0–80 ng/mL | 58.1 pg/mL | Immune sensing | [300] |
| CNTs | AFP | 0–64 ng/mL | 47.1 pg/mL | Immune sensing | [300] |
| CNTs | AKT2 gene | 1 pM–1 μM | 2 fM | Electrochemical | [301] |
| CNTs | CA 125 | 0.001–0.1 ng/mL/0.1–30 ng/mL | 0.5 pg/mL | Electrochemical | [302] |
| CNTs | Cyfra 21-1 | 0.1–10,000 ng/mL | 0.5 ng/mL | Fluorescence | [303] |
| CNTs | HepG2 | 10–105 cells/mL | 5 cells/mL | Electrochemical | [304] |
| Trial Number | Sponsor | Device/Intervention | Problem | Participants | Study Status | Ending Year | Ref |
|---|---|---|---|---|---|---|---|
| NCT01773850 * | UNC Lineberger Comprehensive Cancer Center | CNT x-ray source array for SDT of BN | BN | 54 | Completed | 2018 | [315] |
| NCT01420588 ** | Anhui Medical University | Of-AUNPs/CNT-based chemical nano sensors | PCGLs | 1000 | Completed | 2020 | [316,317] |
| Trial Number | Sponsor | Study Type | Ethics Approval | Status | Ref |
|---|---|---|---|---|---|
| NCT01773850 * | UNC Lineberger Comprehensive Cancer Center | OCPS |  | Completed | [315] |
| NCT01420588 ** | Anhui Medical University | OCPS |  | Completed | [316,317] |
 = positive ethical approval.
= positive ethical approval.| Trial Number | RSG | AC | BPP | BOA | IOD | SR | Ref |
|---|---|---|---|---|---|---|---|
| NCT01773850 |  |  |  |  |  |  | [315] |
| NCT01420588 |  |  |  |  |  |  | [316,317] |
| Strategy | Goal | Modifying Agents/Methods | Results | Refs |
|---|---|---|---|---|
| CNTs surface modification with biocompatible materials or other molecules | ⬆ Dispersion in biological fluids Influenced CU, ⬆ Solubility ⬇ Toxicity | Proteins, surfactants | ⬆ TT, ⬆ TB, ⬇ Toxicity | [341,342,343] |
| FA | ⬆ In vivo tumour targeting, ⬆ Therapeutic benefits ⬇ Toxicity | [141] | ||
| PA hydrogels *, biomaterial, TiO2 | 100% survival of L929 mouse fibroblast | [339] | ||
| Coatings of CNTs | ⬆ CNTs biocompatibility ⬇ Potential toxicity Prevent direct contact with BS ⬆ CNTs solubility | Curcumin lysine ** | ⬇ IL-6, IL-8, IL-1β, TNFα, N-FκB ⬆ Antioxidant enzyme catalase, ⬇ ROS generation Recovery of MM, ⬇ Cell death | [344] |
| CNTs encapsulation CNTs to entrap BAM | ⬇ Direct cells exposure to CNTs Control of CNTs release ⬇ CNTs impact on tissues | PEG (entrapping agent) Oxaliplatin (entrapped agent) | PEGylation delayed oxaliplatin release rate ⬆ Drug’s anticancer effects on HT-29 cells | [112] |
| Tailor Ø size and L | ⬇ Toxicity | N.A. | ⬆ SSA, ⬆ TM, ⬇ Toxicity, ⬇ Harm to lysosomes *** | [345,346] |
| Optimized PP | Remove MI Remove RC | Chemical/electrochemical oxidation [347] High chlorine partial pressure [348] MA digestion [349] Incandescent annealing [350] | ⬇ Lower harmful effects | [350] |
| Engineering controls Suitable PPE | ⬇ Inhalation | Proper ventilation/respiratory protection | ⬇ Respiratory toxicity | N.R. |
| CA with AO | ⬇ OS ⬇ Damage to cells | Quercetin | Prevention of the oxidative damage ⬇ Inflammatory effects, ⬇ Immuno-toxic effects | [336] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfei, S.; Reggio, C.; Zuccari, G. Carbon Nanotubes as Excellent Adjuvants for Anticancer Therapeutics and Cancer Diagnosis: A Plethora of Laboratory Studies Versus Few Clinical Trials. Cells 2025, 14, 1052. https://doi.org/10.3390/cells14141052
Alfei S, Reggio C, Zuccari G. Carbon Nanotubes as Excellent Adjuvants for Anticancer Therapeutics and Cancer Diagnosis: A Plethora of Laboratory Studies Versus Few Clinical Trials. Cells. 2025; 14(14):1052. https://doi.org/10.3390/cells14141052
Chicago/Turabian StyleAlfei, Silvana, Caterina Reggio, and Guendalina Zuccari. 2025. "Carbon Nanotubes as Excellent Adjuvants for Anticancer Therapeutics and Cancer Diagnosis: A Plethora of Laboratory Studies Versus Few Clinical Trials" Cells 14, no. 14: 1052. https://doi.org/10.3390/cells14141052
APA StyleAlfei, S., Reggio, C., & Zuccari, G. (2025). Carbon Nanotubes as Excellent Adjuvants for Anticancer Therapeutics and Cancer Diagnosis: A Plethora of Laboratory Studies Versus Few Clinical Trials. Cells, 14(14), 1052. https://doi.org/10.3390/cells14141052









