Gal-1 Expression Analysis in the GLIOCAT Multicenter Study: Role as a Prognostic Factor and an Immune-Suppressive Biomarker
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Ethical Details
2.3. Tissue Microarray Preparation
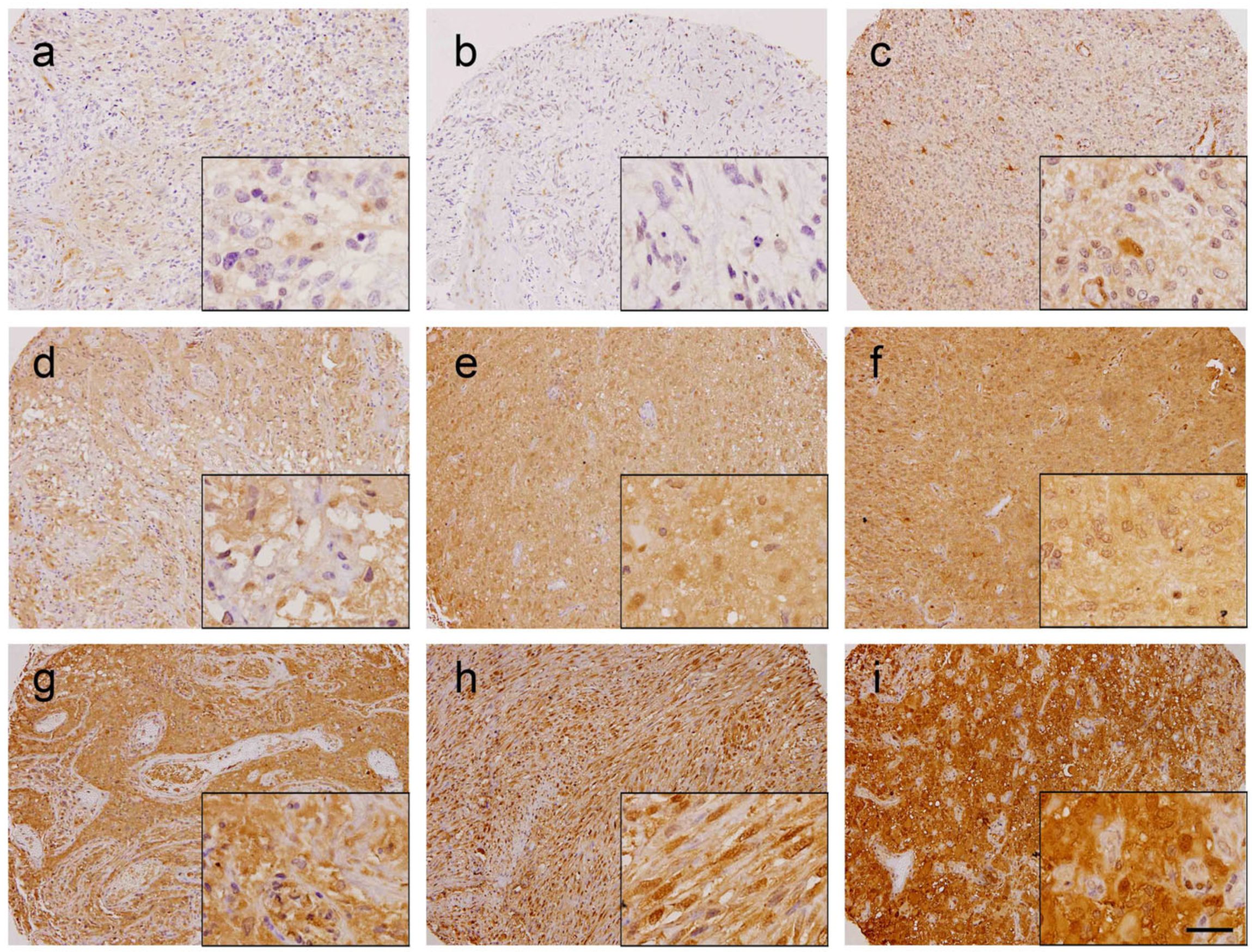
2.4. Immunohistochemistry Analysis
2.5. RNA Sequencing and GBM Molecular Subtypes
2.6. Cell-Type Deconvolution
2.7. Statistical Analysis
3. Results
3.1. Gal-1 Has Prognostic Value in GBM
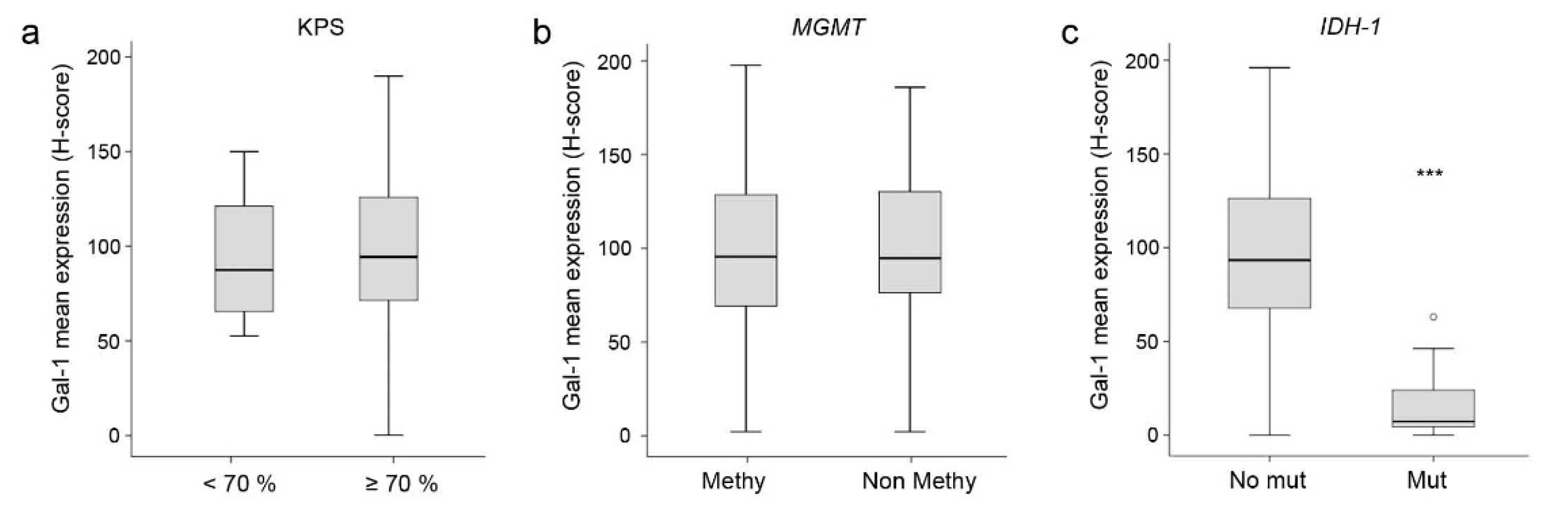
3.2. Correlation between Gal-1 and Clinical or Molecular Data
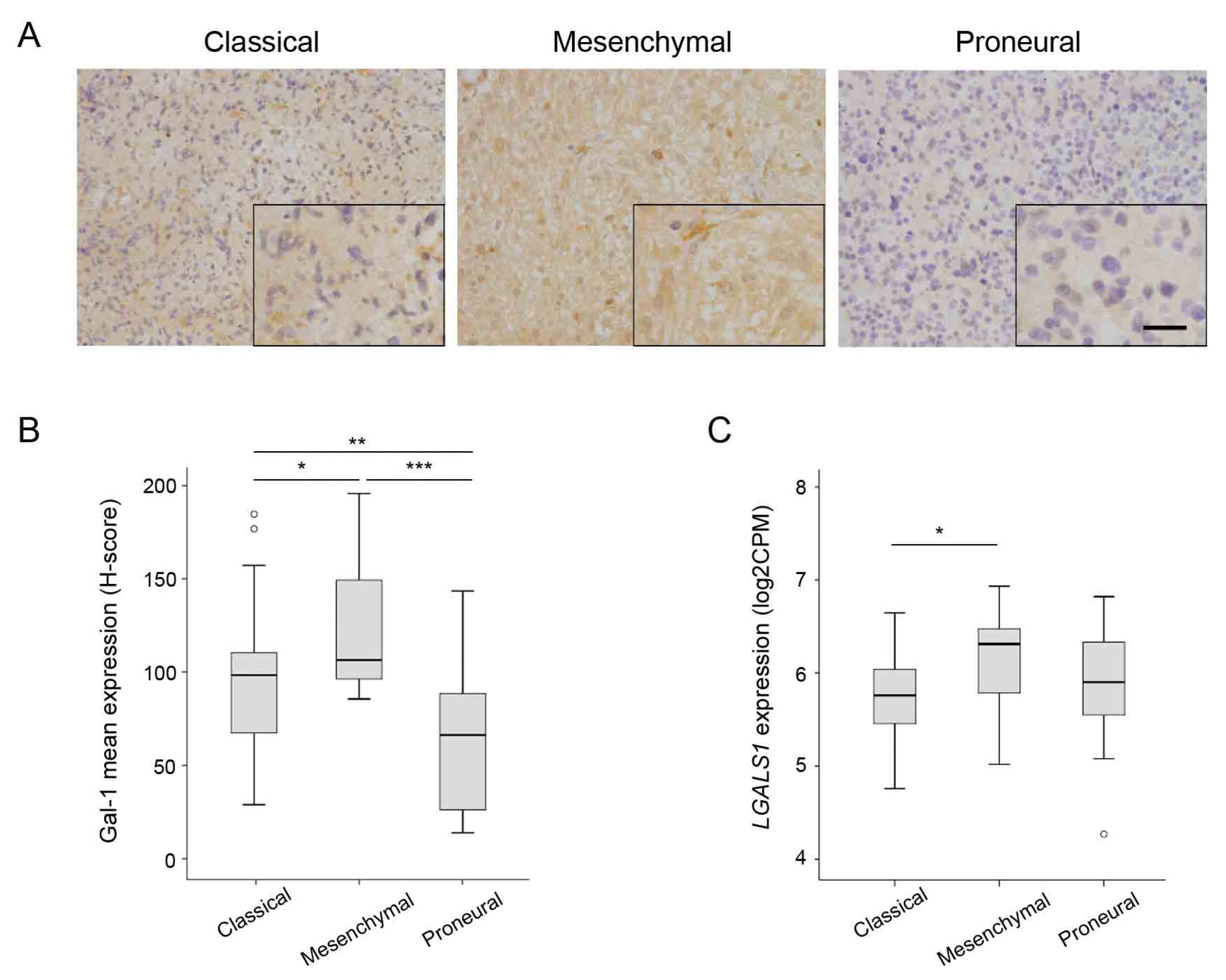
3.3. Correlation between Gal-1 and GBM Molecular Subtypes
3.4. Correlation between Gal-1 Expression and Markers of Inflammation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cruz, J.V.R.; Batista, C.; Afonso, B.d.H.; Alexandre-Moreira, M.S.; Dubois, L.G.; Pontes, B.; Neto, V.M.; Mendes, F.d.A. Obstacles to Glioblastoma Treatment Two Decades after Temozolomide. Cancers 2022, 14, 3203. [Google Scholar] [CrossRef] [PubMed]
- Ostrom, Q.T.; Cote, D.J.; Ascha, M.; Kruchko, C.; Barnholtz-Sloan, J.S. Adult Glioma Incidence and Survival by Race or Ethnicity in the United States from 2000 to 2014. JAMA Oncol. 2018, 4, 1254–1262. [Google Scholar] [CrossRef]
- Stupp, R.; Mason, W.P.; van den Bent, M.J.; Weller, M.; Fisher, B.; Taphoorn, M.J.B.; Belanger, K.; Brandes, A.A.; Marosi, C.; Bogdahn, U.; et al. Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma. N. Engl. J. Med. 2005, 352, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.M.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs. Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Waqas, M.; Shamim, M.S. Prognostic Significance of IDH 1 Mutation in Patients with Glioblastoma Multiforme. J. Pak. Med. Assoc. 2017, 67, 816–817. [Google Scholar] [PubMed]
- Louis, D.N.; Perry, A.; Wesseling, P.; Brat, D.J.; Cree, I.A.; Figarella-Branger, D.; Hawkins, C.; Ng, H.K.; Pfister, S.M.; Reifenberger, G.; et al. The 2021 WHO Classification of Tumors of the Central Nervous System: A Summary. Neuro Oncol. 2021, 23, 1231–1251. [Google Scholar] [CrossRef]
- Audureau, E.; Chivet, A.; Ursu, R.; Corns, R.; Metellus, P.; Noel, G.; Zouaoui, S.; Guyotat, J.; le Reste, P.J.; Faillot, T.; et al. Prognostic Factors for Survival in Adult Patients with Recurrent Glioblastoma: A Decision-Tree-Based Model. J. Neurooncol. 2018, 136, 565–576. [Google Scholar] [CrossRef]
- Wang, Q.; Hu, B.; Hu, X.; Kim, H.; Squatrito, M.; Scarpace, L.; deCarvalho, A.C.; Lyu, S.; Li, P.; Li, Y.; et al. Tumor Evolution of Glioma-Intrinsic Gene Expression Subtypes Associates with Immunological Changes in the Microenvironment. Cancer Cell 2017, 32, 42–56.e6. [Google Scholar] [CrossRef]
- Gravendeel, L.A.M.; Kouwenhoven, M.C.M.; Gevaert, O.; de Rooi, J.J.; Stubbs, A.P.; Duijm, J.E.; Daemen, A.; Bleeker, F.E.; Bralten, L.B.C.; Kloosterhof, N.K.; et al. Intrinsic Gene Expression Profiles of Gliomas Are a Better Predictor of Survival than Histology. Cancer Res. 2009, 69, 9065–9072. [Google Scholar] [CrossRef]
- Nagy, Á.; Garzuly, F.; Padányi, G.; Szűcs, I.; Feldmann, Á.; Murnyák, B.; Hortobágyi, T.; Kálmán, B. Molecular Subgroups of Glioblastoma- an Assessment by Immunohistochemical Markers. Pathol. Oncol. Res. 2019, 25, 21–31. [Google Scholar] [CrossRef]
- Carrato, C.; Alameda, F.; Esteve-Codina, A.; Pineda, E.; Arpí, O.; Martinez-García, M.; Mallo, M.; Gut, M.; Lopez-Martos, R.; Barco, S.d.; et al. Glioblastoma TCGA Mesenchymal and IGS 23 Tumors Are Identifiable by IHC and Have an Immune-Phenotype Indicating a Potential Benefit from Immunotherapy. Clin. Cancer Res. 2020, 26, 6600–6609. [Google Scholar] [CrossRef]
- Camby, I.; le Mercier, M.; Lefranc, F.; Kiss, R. Galectin-1: A Small Protein with Major Functions. Glycobiology 2006, 16, 137R–157R. [Google Scholar] [CrossRef]
- Liu, F.T.; Rabinovich, G.A. Galectins as Modulators of Tumour Progression. Nat. Rev. Cancer 2005, 5, 29–41. [Google Scholar] [CrossRef]
- Thijssen, V.L.; Heusschen, R.; Caers, J.; Griffioen, A.W. Galectin Expression in Cancer Diagnosis and Prognosis: A Systematic Review. Biochim. Biophys. Acta 2015, 1855, 235–247. [Google Scholar] [CrossRef]
- Girotti, M.R.; Salatino, M.; Dalotto-Moreno, T.; Rabinovich, G.A. Sweetening the Hallmarks of Cancer: Galectins as Multifunctional Mediators of Tumor Progression. J. Exp. Med. 2020, 217, e20182041. [Google Scholar] [CrossRef]
- Chou, S.Y.; Yen, S.L.; Huang, C.C.; Huang, E.Y. Galectin-1 Is a Poor Prognostic Factor in Patients with Glioblastoma Multiforme after Radiotherapy. BMC Cancer 2018, 18, 105. [Google Scholar] [CrossRef]
- Camby, I.; Belot, N.; Lefranc, F.; Sadeghi, N.; de Launoit, Y.; Kaltner, H.; Musette, S.; Darro, F.; Danguy, A.; Salmon, I.; et al. Galectin-1 Modulates Human Glioblastoma Cell Migration into the Brain through Modifications to the Actin Cytoskeleton and Levels of Expression of Small GTPases. J. Neuropathol. Exp. Neurol. 2002, 61, 585–596. [Google Scholar] [CrossRef]
- D’Haene, N.; Maris, C.; Rorive, S.; Decaestecker, C.; le Mercier, M.; Salmon, I. Galectins and Neovascularization in Central Nervous System Tumors. Glycobiology 2014, 24, 892–898. [Google Scholar] [CrossRef]
- Chen, Q.; Han, B.; Meng, X.; Duan, C.; Yang, C.; Wu, Z.; Magafurov, D.; Zhao, S.; Safin, S.; Jiang, C.; et al. Immunogenomic Analysis Reveals LGALS1 Contributes to the Immune Heterogeneity and Immunosuppression in Glioma. Int. J. Cancer 2019, 145, 517–530. [Google Scholar] [CrossRef]
- Videla-Richardson, G.A.; Morris-Hanon, O.; Torres, N.I.; Esquivel, M.I.; Vera, M.B.; Ripari, L.B.; Croci, D.O.; Sevlever, G.E.; Rabinovich, G.A. Galectins as Emerging Glyco-Checkpoints and Therapeutic Targets in Glioblastoma. Int. J. Mol. Sci. 2021, 23, 316. [Google Scholar] [CrossRef]
- Le Mercier, M.; Fortin, S.; Mathieu, V.; Kiss, R.; Lefranc, F. Galectins and Gliomas. Brain Pathol. 2010, 20, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Esteve-Codina, A.; Alameda, F.; Carrato, C.; Pineda, E.; Arpí, O.; Martinez-García, M.; Mallo, M.; Gut, M.; Dabad, M.; Tortosa, A.; et al. RNA Sequencing and Immunohistochemistry Reveal ZFN7 as a Stronger Marker of Survival than Molecular Subtypes in G-CIMP-Negative Glioblastoma. Clin. Cancer Res. 2021, 27, 645–655. [Google Scholar] [CrossRef]
- Martínez-Bosch, N.; Manero-Rupérez, N.; Moreno, M.; Navarro, P. Exploring the Role of Galectins in Cancer: In Vitro and In Vivo Approaches. Methods Mol. Biol. 2022, 2442, 685–711. [Google Scholar] [CrossRef] [PubMed]
- Detre, S.; Saclani Jotti, G.; Dowsett, M. A “Quickscore” Method for Immunohistochemical Semiquantitation: Validation for Oestrogen Receptor in Breast Carcinomas. J. Clin. Pathol. 1995, 48, 876–878. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.D.; Oshlack, A. A Scaling Normalization Method for Differential Expression Analysis of RNA-Seq Data. Genome Biol. 2010, 11, R25. [Google Scholar] [CrossRef]
- Chen, B.; Khodadoust, M.S.; Liu, C.L.; Newman, A.M.; Alizadeh, A.A. Profiling Tumor Infiltrating Immune Cells with CIBERSORT. Methods Mol. Biol. 2018, 1711, 243. [Google Scholar] [CrossRef]
- Hothorn, T.; Lausen, B. Maximally Selected Rank Statistics in R. R News, 1 February 2002; 3–5. [Google Scholar]
- Lausen, B.; Hothorn, T.; Bretz, F.; Schumacher, M. Assessment of Optimal Selected Prognostic Factors. Biom. J. 2004, 46, 364–374. [Google Scholar] [CrossRef]
- Budczies, J.; Klauschen, F.; Sinn, B.; Gyo Rffy, B.; Schmitt, W.D. Cutoff Finder: A Comprehensive and Straightforward Web Application Enabling Rapid Biomarker Cutoff Optimization. PLoS ONE 2012, 7, 51862. [Google Scholar] [CrossRef]
- Rabinovich, G.A. Galectin-1 as a Potential Cancer Target. Br. J. Cancer 2005, 92, 1188–1192. [Google Scholar] [CrossRef]
- Baker, G.J.; Chockley, P.; Yadav, V.N.; Doherty, R.; Ritt, M.; Sivaramakrishnan, S.; Castro, M.G.; Lowenstein, P.R. Natural Killer Cells Eradicate Galectin-1-Deficient Glioma in the Absence of Adaptive Immunity. Cancer Res. 2014, 74, 5079–5090. [Google Scholar] [CrossRef]
- Cooper, D.N.; Barondes, S.H. Evidence for Export of a Muscle Lectin from Cytosol to Extracellular Matrix and for a Novel Secretory Mechanism. J. Cell Biol. 1990, 110, 1681–1691. [Google Scholar] [CrossRef]
- Gao, Y.; Li, X.; Shu, Z.; Zhang, K.; Xue, X.; Li, W.; Hao, Q.; Wang, Z.; Zhang, W.; Wang, S.; et al. Nuclear Galectin-1-FOXP3 Interaction Dampens the Tumor-Suppressive Properties of FOXP3 in Breast Cancer. Cell Death Dis. 2018, 9, 416. [Google Scholar] [CrossRef]
- Patterson, R.J.; Wang, W.; Wang, J.L. Understanding the Biochemical Activities of Galectin-1 and Galectin-3 in the Nucleus. Glycoconj J. 2002, 19, 499–506. [Google Scholar] [CrossRef]
- Qi, C.; Lei, L.; Hu, J.; Wang, G.; Liu, J.; Ou, S. T Cell Immune Regulator 1 Is a Prognostic Marker Associated with Immune Infiltration in Glioblastoma Multiforme. Oncol. Lett. 2021, 21, 252. [Google Scholar] [CrossRef]
- Phillips, H.S.; Kharbanda, S.; Chen, R.; Forrest, W.F.; Soriano, R.H.; Wu, T.D.; Misra, A.; Nigro, J.M.; Colman, H.; Soroceanu, L.; et al. Molecular Subclasses of High-Grade Glioma Predict Prognosis, Delineate a Pattern of Disease Progression, and Resemble Stages in Neurogenesis. Cancer Cell 2006, 9, 157–173. [Google Scholar] [CrossRef]
- Verhaak, R.G.W.; Hoadley, K.A.; Purdom, E.; Wang, V.; Qi, Y.; Wilkerson, M.D.; Miller, C.R.; Ding, L.; Golub, T.; Mesirov, J.P.; et al. Integrated Genomic Analysis Identifies Clinically Relevant Subtypes of Glioblastoma Characterized by Abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 2010, 17, 98–110. [Google Scholar] [CrossRef]
- Van Woensel, M.; Mathivet, T.; Wauthoz, N.; Rosière, R.; Garg, A.D.; Agostinis, P.; Mathieu, V.; Kiss, R.; Lefranc, F.; Boon, L.; et al. Sensitization of Glioblastoma Tumor Micro-Environment to Chemo- and Immunotherapy by Galectin-1 Intranasal Knock-down Strategy. Sci. Rep. 2017, 7, 1217. [Google Scholar] [CrossRef]
- Correa, S.G.; Sotomayor, C.E.; Aoki, M.P.; Maldonado, C.A.; Rabinovich, G.A. Opposite Effects of Galectin-1 on Alternative Metabolic Pathways of L-Arginine in Resident, Inflammatory, and Activated Macrophages. Glycobiology 2003, 13, 119–128. [Google Scholar] [CrossRef]
- Barrionuevo, P.; Beigier-Bompadre, M.; Ilarregui, J.M.; Toscano, M.A.; Bianco, G.A.; Isturiz, M.A.; Rabinovich, G.A. A Novel Function for Galectin-1 at the Crossroad of Innate and Adaptive Immunity: Galectin-1 Regulates Monocyte/Macrophage Physiology through a Nonapoptotic ERK-Dependent Pathway. J. Immunol. 2007, 178, 436–445. [Google Scholar] [CrossRef]
- Rostoker, R.; Yaseen, H.; Schif-Zuck, S.; Lichtenstein, R.G.; Rabinovich, G.A.; Ariel, A. Galectin-1 Induces 12/15-Lipoxygenase Expression in Murine Macrophages and Favors Their Conversion toward a pro-Resolving Phenotype. Prostaglandins Other Lipid Mediat. 2013, 107, 85–94. [Google Scholar] [CrossRef]
- Malik, R.K.J.; Ghurye, R.R.; Lawrence-Watt, D.J.; Stewart, H.J.S. Galectin-1 Stimulates Monocyte Chemotaxis via the P44/42 MAP Kinase Pathway and a Pertussis Toxin-Sensitive Pathway. Glycobiology 2009, 19, 1402–1407. [Google Scholar] [CrossRef]
- Shao, R.; Taylor, S.L.; Oh, D.S.; Schwartz, L.M. Vascular Heterogeneity and Targeting: The Role of YKL-40 in Glioblastoma Vascularization. Oncotarget 2015, 6, 40507–40518. [Google Scholar] [CrossRef] [PubMed]
- Faibish, M.; Francescone, R.; Bentley, B.; Yan, W.; Shao, R. A YKL-40-Neutralizing Antibody Blocks Tumor Angiogenesis and Progression: A Potential Therapeutic Agent in Cancers. Mol. Cancer Ther. 2011, 10, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Francescone, R.A.; Scully, S.; Faibish, M.; Taylor, S.L.; Oh, D.; Moral, L.; Yan, W.; Bentley, B.; Shao, R. Role of YKL-40 in the Angiogenesis, Radioresistance, and Progression of Glioblastoma. J. Biol. Chem. 2011, 286, 15332–15343. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Jun, Y.J.; Kim, T.H.; Jung, J.Y.; Hwang, G.H.; Jung, K.J.; Lee, S.H.; Lee, H.M.; Lee, S.H. Increased Expression of YKL-40 in Mild and Moderate/Severe Persistent Allergic Rhinitis and Its Possible Contribution to Remodeling of Nasal Mucosa. Am. J. Rhinol. Allergy 2013, 27, 372–380. [Google Scholar] [CrossRef]



| HR | CI 95% | p Value | |
|---|---|---|---|
| Gal-1 mean H-score | |||
| <129.3 | 1 | ||
| ≥129.3 | 1.52 | 1.10–2.08 | 0.010 |
| Age | |||
| <70 | 1 | ||
| ≥70 | 1.45 | 1.06–1.98 | 0.019 |
| Gender | |||
| Male | 1 | ||
| Female | 0.90 | 0.69–1.17 | 0.428 |
| Clinical and Molecular Variables | n | Median Gal-1 | Percentiles (P25–P75) | p Value * |
|---|---|---|---|---|
| KPS | ||||
| <70% | 23 | 87.38 | (62.50–128.40) | 0.495 |
| ≥70% | 192 | 94.31 | (71.30–126.03) | |
| MGMT status | ||||
| Methylated | 123 | 93.63 | (66.88–127.92) | 0.503 |
| Non-methylated | 133 | 92.82 | (71.89–129.17) | |
| IDH-1 | ||||
| No mutated | 263 | 93.13 | (68.44–126.25) | <0.001 |
| Mutated | 10 | 7.28 | (3.68–29.57) | |
| Classical | Mesenchymal | Proneural | p Value * | |
|---|---|---|---|---|
| n | 36 | 13 | 22 | |
| Gal-1 median (P25-P75) | 98.60 (67.69–111.15) | 106.67 (93.28–151.46) | 66.58 (26.32–90.42) | <0.001 |
| Gal-1 Mean | Spearman Correlation Coefficient | p Value * |
|---|---|---|
| SHC1 | 0.230 | <0.001 |
| PD-L1 | 0.239 | <0.001 |
| PAX2 | 0.155 | 0.014 |
| MEOX2 | 0.159 | 0.012 |
| YKL-40 | 0.182 | 0.004 |
| TCIRG1 | 0.151 | 0.017 |
| YWHAG | 0.232 | <0.001 |
| OLIG2 | −0.313 | <0.001 |
| SOX2 | −0.192 | 0.003 |
| Ki-67 | −0.283 | <0.001 |
| SOX11 | −0.278 | <0.001 |
| Immune cell Type | LGALS1 Correlation | p Value * |
|---|---|---|
| B cells, naive | 0.032 | 0.733 |
| B cells, memory | −0.124 | 0.182 |
| Plasma cells | 0.038 | 0.681 |
| T cells CD8 | −0.062 | 0.505 |
| T cells CD4, naive | −0.193 | 0.036 |
| T cells CD4 memory, resting | 0.454 | <0.001 |
| T cells CD4 memory, activated | 0.105 | 0.255 |
| T cells folicular, helper | −0.035 | 0.707 |
| T cells regulatory | 0.104 | 0.263 |
| T cells gamma delta | −0.019 | 0.835 |
| NK cells resting | 0.116 | 0.212 |
| NK cells activated | −0.150 | 0.105 |
| Monocytes | 0.243 | 0.008 |
| Macrophages M0 | 0.119 | 0.198 |
| Macrophages M1 | 0.018 | 0.843 |
| Macrophages M2 | 0.437 | <0.001 |
| Dendritic cells, resting | 0.055 | 0.550 |
| Dendritic cells, activated | 0.163 | 0.078 |
| Mast cells, resting | 0.005 | 0.956 |
| Mast cells, activated | 0.106 | 0.253 |
| Eosinophils | 0.111 | 0.232 |
| Neutrophils | 0.067 | 0.474 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Bosch, N.; Vilariño, N.; Alameda, F.; Mojal, S.; Arumí-Uria, M.; Carrato, C.; Aldecoa, I.; Ribalta, T.; Vidal, N.; Bellosillo, B.; et al. Gal-1 Expression Analysis in the GLIOCAT Multicenter Study: Role as a Prognostic Factor and an Immune-Suppressive Biomarker. Cells 2023, 12, 843. https://doi.org/10.3390/cells12060843
Martínez-Bosch N, Vilariño N, Alameda F, Mojal S, Arumí-Uria M, Carrato C, Aldecoa I, Ribalta T, Vidal N, Bellosillo B, et al. Gal-1 Expression Analysis in the GLIOCAT Multicenter Study: Role as a Prognostic Factor and an Immune-Suppressive Biomarker. Cells. 2023; 12(6):843. https://doi.org/10.3390/cells12060843
Chicago/Turabian StyleMartínez-Bosch, Neus, Noelia Vilariño, Francesc Alameda, Sergi Mojal, Montserrat Arumí-Uria, Cristina Carrato, Iban Aldecoa, Teresa Ribalta, Noemí Vidal, Beatriz Bellosillo, and et al. 2023. "Gal-1 Expression Analysis in the GLIOCAT Multicenter Study: Role as a Prognostic Factor and an Immune-Suppressive Biomarker" Cells 12, no. 6: 843. https://doi.org/10.3390/cells12060843
APA StyleMartínez-Bosch, N., Vilariño, N., Alameda, F., Mojal, S., Arumí-Uria, M., Carrato, C., Aldecoa, I., Ribalta, T., Vidal, N., Bellosillo, B., Menéndez, S., Del Barco, S., Gallego, O., Pineda, E., López-Martos, R., Hernández, A., Mesia, C., Esteve-Codina, A., de la Iglesia, N., ... Navarro, P. (2023). Gal-1 Expression Analysis in the GLIOCAT Multicenter Study: Role as a Prognostic Factor and an Immune-Suppressive Biomarker. Cells, 12(6), 843. https://doi.org/10.3390/cells12060843









