FGF-2 Differentially Regulates Lens Epithelial Cell Behaviour during TGF-β-Induced EMT
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals and Tissue Culture
2.2. Lens Epithelial Explants
2.3. Assessment of Cell Morphology and Immunofluorescence
2.4. SDS-Page and Western Blotting
2.5. Statistical Analysis
3. Results
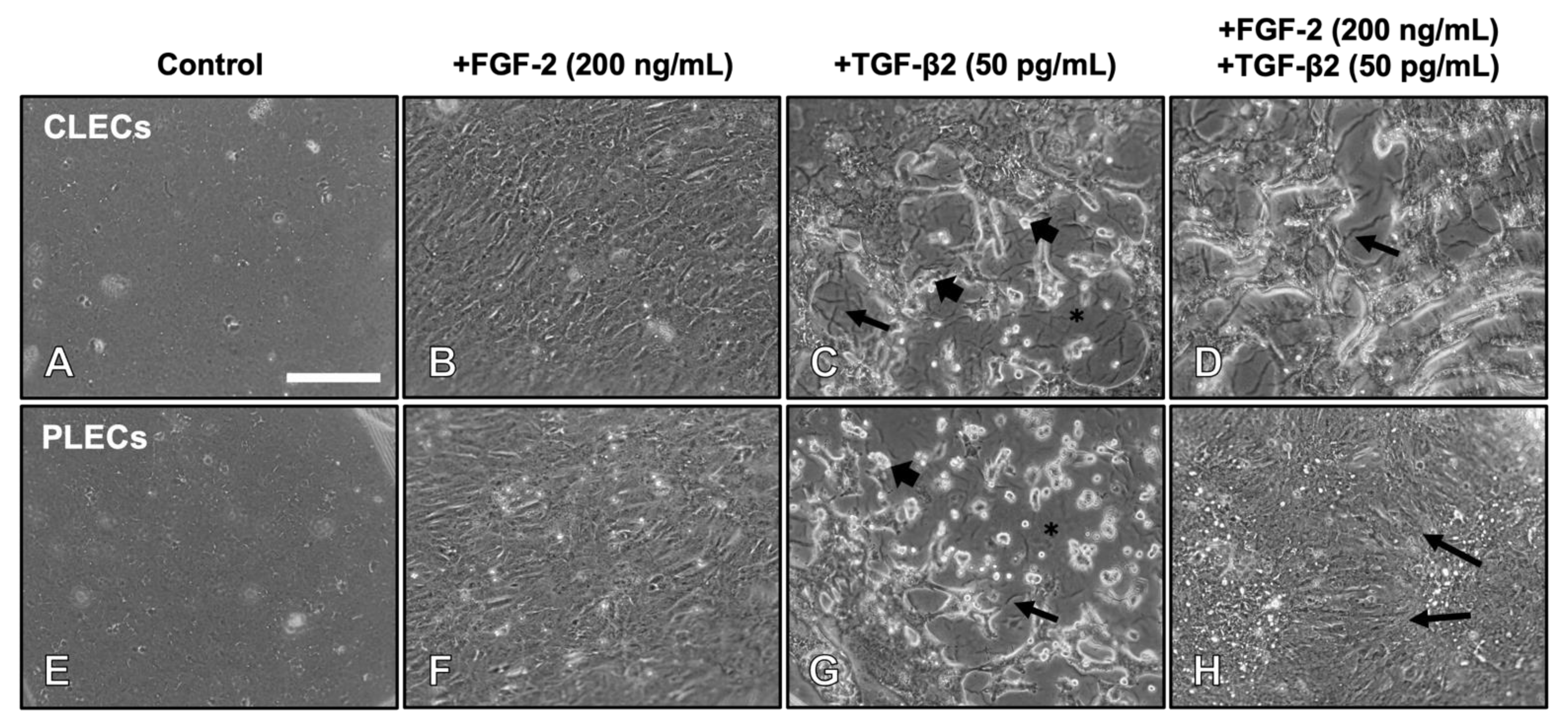
3.1. FGF-2 Promotes a Spatially Dependent TGF-β2-Induced EMT Response in Lens Epithelial Explants
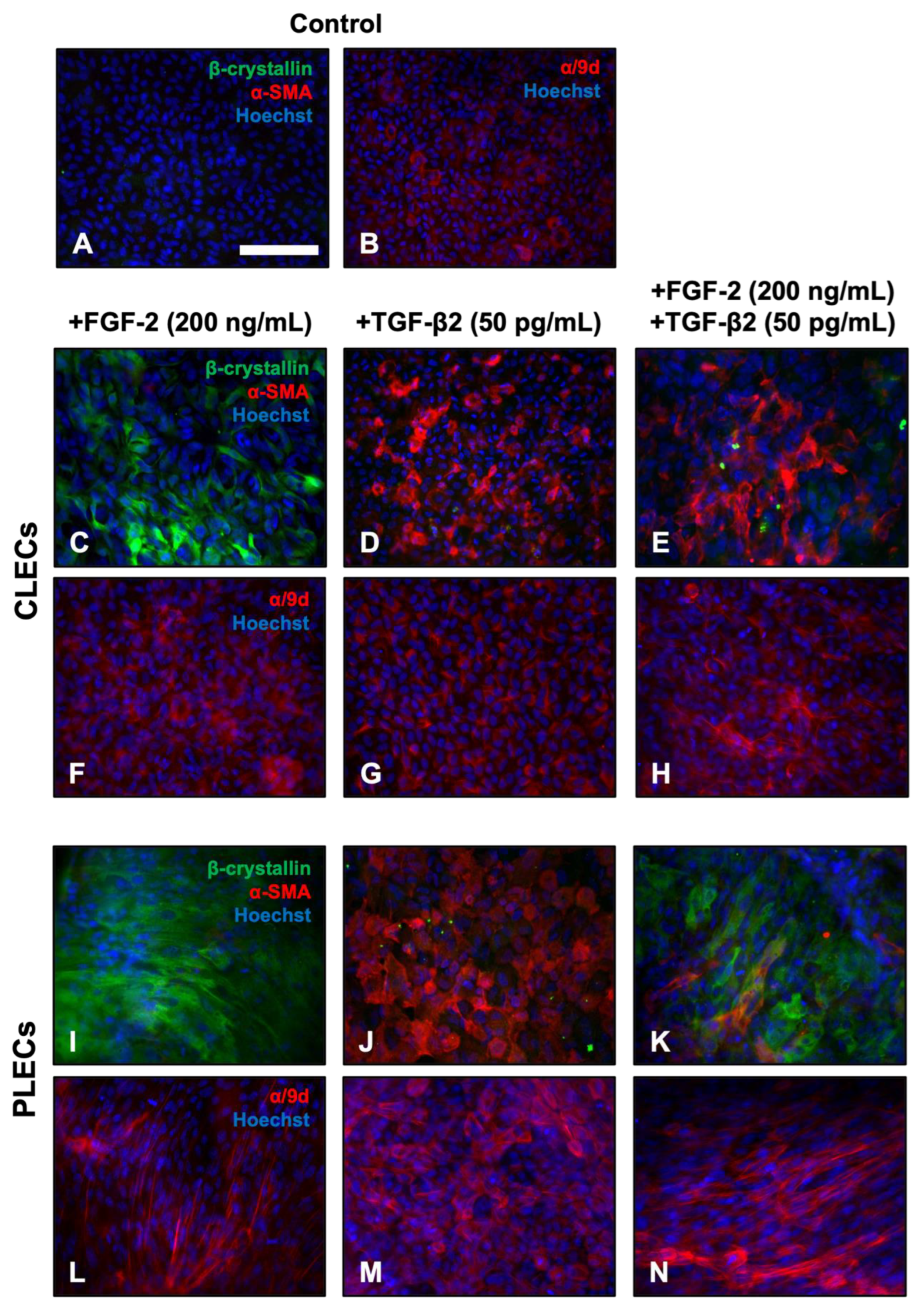
3.2. FGF-2 Promotes Spatial Differences in Labelling for EMT and Fibre Differentiation Markers in TGF-β2-Treated LECs
3.2.1. Immunofluorescent Labelling
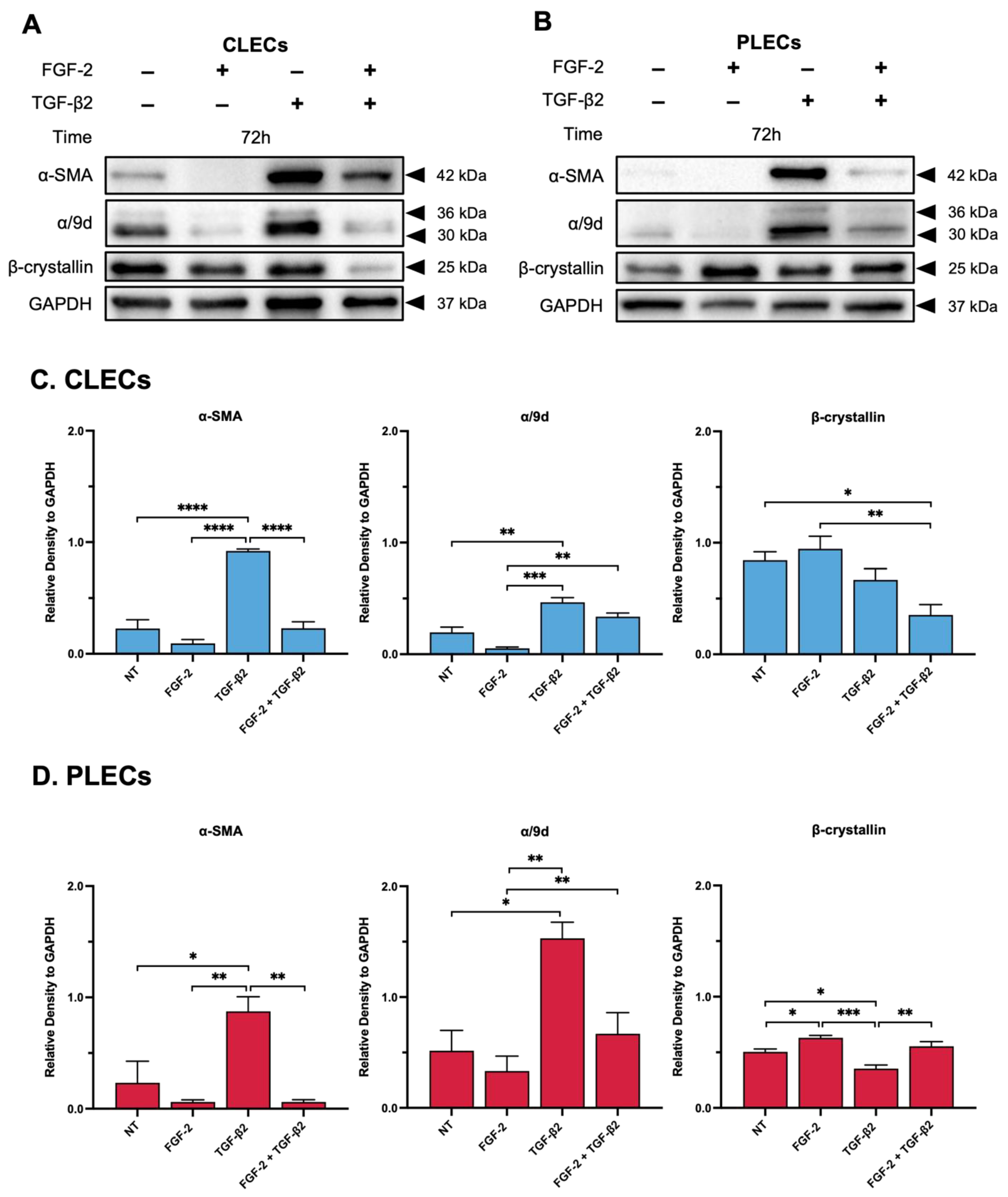
3.2.2. Western Blotting
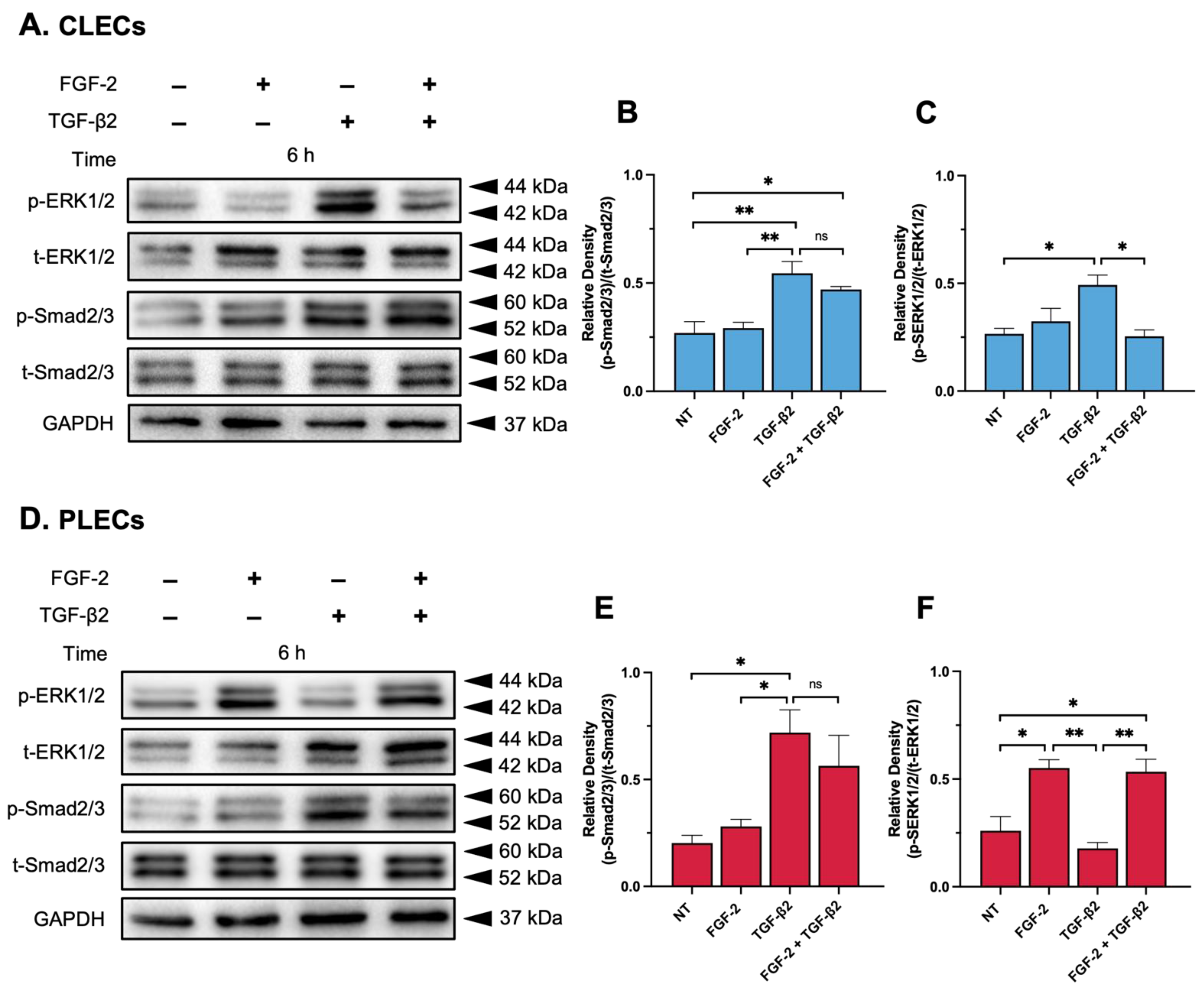
3.3. Impact of FGF-2 on TGF-β2-Mediated Intracellular Signalling
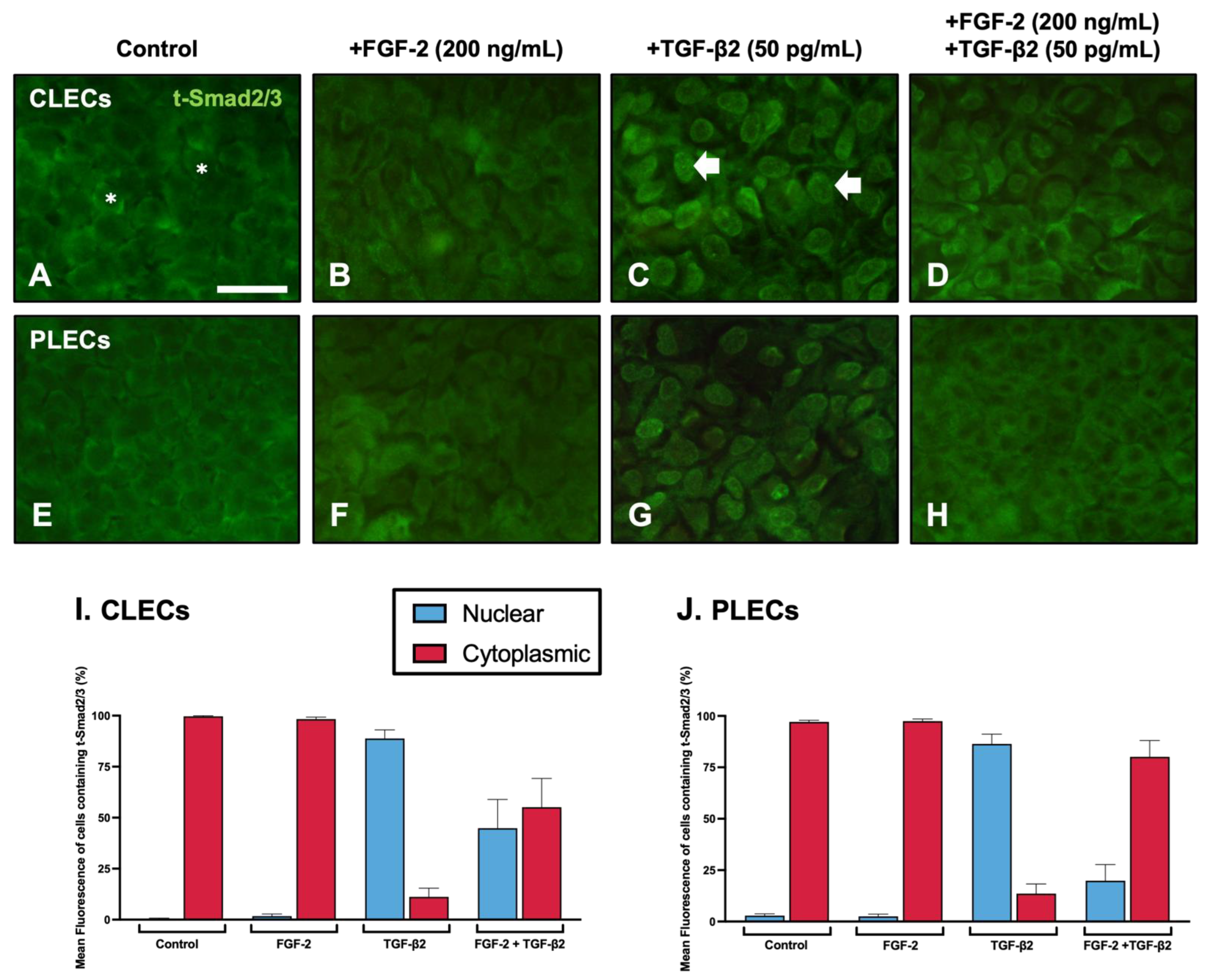
3.3.1. Nuclear Translocation of Smad2/3
3.3.2. Smad2/3-Signalling
3.3.3. MAPK/ERK1/2-Signalling
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ASC | Anterior subcapsular cataract |
| α-SMA | Alpha-smooth muscle actin |
| α/9d | Alpha tropomyosin 9d antibody |
| CLECs | Central lens epithelial cells |
| EMT | Epithelial–mesenchymal transition |
| ERK | Extracellular signal-regulated kinase |
| FGF | Fibroblast growth factor |
| LECs | Lens epithelial cells |
| MAPK | Mitogen-activated protein kinase |
| PLECs | Peripheral lens epithelial cells |
| PCO | Posterior capsular opacification |
| TGF-β | Transforming growth factor-beta |
| Tpm | Tropomyosin |
References
- Lovicu, F.J.; McAvoy, J.W. Growth factor regulation of lens development. Dev. Biol. 2005, 280, 1–14. [Google Scholar] [CrossRef]
- Iyengar, L.; Patkunanathan, B.; Mcavoy, J.W.; Lovicu, F.J. Growth factors involved in aqueous humour-induced lens cell proliferation. Growth Factors 2009, 27, 50–62. [Google Scholar] [CrossRef]
- Iyengar, L.; Wang, Q.; Rasko, J.E.J.; McAvoy, J.W.; Lovicu, F.J. Duration of ERK1/2 phosphorylation induced by FGF or ocular media determines lens cell fate. Differentiation 2007, 75, 662–668. [Google Scholar] [CrossRef]
- Lovicu, F.J.; McAvoy, J.W. FGF-induced lens cell proliferation and differentiation is dependent on MAPK (ERK1/2) signalling. Development 2001, 128, 5075–5084. [Google Scholar] [CrossRef]
- West-Mays, J.A.; Pino, G.; Lovicu, F.J. Development and use of the lens epithelial explant system to study lens differentiation and cataractogenesis. Prog. Retin. Eye Res. 2009, 29, 135–143. [Google Scholar] [CrossRef] [PubMed]
- De Iongh, R.U.; Lovicu, F.J.; Hanneken, A.; Baird, A.; McAvoy, J.W. FGF receptor-1 (flg) expression is correlated with fibre differentiation during rat lens morphogenesis and growth. Dev. Dyn. 1996, 206, 412–426. [Google Scholar] [CrossRef]
- Chamberlain, C.G.; McAvoy, J.W. Fibre differentiation and polarity in the mammalian lens: A key role for FGF. Prog. Retin. Eye Res. 1997, 16, 443–478. [Google Scholar] [CrossRef]
- Zhao, H.; Yang, T.; Madakashira, B.P.; Thiels, C.A.; Bechtle, C.A.; Garcia, C.M.; Zhang, H.; Yu, K.; Ornitz, D.M.; Beebe, D.C.; et al. Fibroblast growth factor receptor signaling is essential for lens fiber cell differentiation. Dev. Biol. 2008, 318, 276–288. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, C.G.; McAvoy, J.W. Induction of Lens Fibre Differentiation by Acidic and Basic Fibroblast Growth Factor (FGF). Growth Factors 1989, 1, 125–134. [Google Scholar] [CrossRef]
- Wang, D.; Wang, E.; Liu, K.; Xia, C.-H.; Li, S.; Gong, X. Roles of TGFβ and FGF signals during growth and differentiation of mouse lens epithelial cell in vitro. Sci. Rep. 2017, 7, 7274. [Google Scholar] [CrossRef] [PubMed]
- Wormstone, I.M.; Anderson, I.K.; Eldred, J.A.; Dawes, L.J.; Duncan, G. Short-term exposure to transforming growth factor β induces long-term fibrotic responses. Exp. Eye Res. 2006, 83, 1238–1245. [Google Scholar] [CrossRef]
- Wormstone, I.M.; Tamiya, S.; Anderson, I.; Duncan, G. TGF-beta2-induced matrix modification and cell transdif-ferentiation in the human lens capsular bag. Investig. Ophth. Vis. Sci. 2002, 43, 2301–2308. [Google Scholar]
- Boswell, B.A.; Korol, A.; West-Mays, J.A.; Musil, L.S. Dual function of TGFβ in lens epithelial cell fate: Implications for secondary cataract. Mol. Biol. Cell 2017, 28, 907–921. [Google Scholar] [CrossRef]
- Kubo, E.; Shibata, S.; Shibata, T.; Kiyokawa, E.; Sasaki, H.; Singh, D.P. FGF2 antagonizes aberrant TGFβ regulation of tropomyosin: Role for posterior capsule opacity. J. Cell. Mol. Med. 2017, 21, 916–928. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, K.J.; Cerra, A.; Chamberlain, C.G. FGF-2 counteracts loss of TGFbeta affected cells from rat lens explants: Implications for PCO (after cataract). Mol. Vis. 2004, 10, 521–532. [Google Scholar]
- Cerra, A.; Mansfield, K.J.; Chamberlain, C.G. Exacerbation of TGF-beta-induced cataract by FGF-2 in cultured rat lenses. Mol. Vis. 2003, 9, 689–700. [Google Scholar] [PubMed]
- de Iongh, R.U.; Wederell, E.; Lovicu, F.J.; McAvoy, J.W. Transforming Growth Factor-β-Induced Epithelial-Mesenchymal Transition in the Lens: A Model for Cataract Formation. Cells Tissues Organs 2005, 179, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Lovicu, F.J.; Flokis, M.; Wojciechowski, M.; Mao, B.; Shu, D. Understanding Fibrotic Cataract: Regulation of TGFβ-Mediated Pathways Leading to Lens Epithelial to Mesenchymal Transition (EMT). J. Jpn. Soc. Cataract. Res. 2020, 32, 23–32. [Google Scholar]
- Xu, J.; Lamouille, S.; Derynck, R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009, 19, 156–172. [Google Scholar] [CrossRef]
- Nieto, M.A.; Huang, R.Y.-J.; Jackson, R.A.; Thiery, J.P. EMT: 2016. Cell 2016, 166, 21–45. [Google Scholar] [CrossRef]
- Kalluri, R.; Neilson, E.G. Epithelial-mesenchymal transition and its implications for fibrosis. J. Clin. Investig. 2003, 112, 1776–1784. [Google Scholar] [CrossRef] [PubMed]
- Martinez, G.; de Iongh, R.U. The lens epithelium in ocular health and disease. Int. J. Biochem. Cell Biol. 2010, 42, 1945–1963. [Google Scholar] [CrossRef] [PubMed]
- Marcantonio, J.M.; Syam, P.P.; Liu, C.S.C.; Duncan, G. Epithelial transdifferentiation and cataract in the human lens. Exp. Eye Res. 2003, 77, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Lovicu, F.J.; Steven, P.; Saika, S.; McAvoy, J.W. Aberrant Lens Fiber Differentiation in Anterior Subcapsular Cataract Formation: A Process Dependent on Reduced Levels of Pax6. Investig. Ophthalmol. Vis. Sci. 2004, 45, 1946–1953. [Google Scholar] [CrossRef]
- Jiang, J.; Shihan, M.H.; Wang, Y.; Duncan, M.K. Lens Epithelial Cells Initiate an Inflammatory Response Following Cataract Surgery. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4986–4997. [Google Scholar] [CrossRef]
- Liu, Y.C.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef]
- Abdulhussein, D.; Hussein, M.A. WHO Vision 2020: Have We Done It? Ophthalmic Epidemiol. 2022, 1–9. [Google Scholar] [CrossRef]
- GBD Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: An analysis for the Global Burden of Disease Study. Lancet Glob. Health 2021, 9, e130–e143. [Google Scholar] [CrossRef]
- Vasavada, A.R.; Praveen, M.R. Posterior Capsule Opacification After Phacoemulsification: Annual Review. Asia-Pacific J. Ophthalmol. 2014, 3, 235–240. [Google Scholar] [CrossRef]
- Karahan, E.; Er, D.; Kaynak, S. An Overview of Nd:YAG Laser Capsulotomy. Med. Hypothesis Discov. Innov. Ophthalmol. 2014, 3, 45–50. [Google Scholar]
- Pandey, S.K.; Apple, D.J.; Werner, L.; Maloof, A.J.; Milverton, E.J. Posterior capsule opacification: A review of the aetiopathogenesis, experimental and clinical studies and factors for prevention. Indian J. Ophthalmol. 2004, 52, 99–112. [Google Scholar]
- Lovicu, F.J.; Shin, E.H.; McAvoy, J.W. Fibrosis in the lens. Sprouty regulation of TGFβ-signaling prevents lens EMT leading to cataract. Exp. Eye Res. 2015, 142, 92–101. [Google Scholar] [CrossRef]
- D’Antin, J.C.; Tresserra, F.; Barraquer, R.I.; Michael, R. Soemmerring’s Rings Developed around IOLs, in Human Donor Eyes, Can Present Internal Transparent Areas. Int. J. Mol. Sci. 2022, 23, 13294. [Google Scholar] [CrossRef]
- Wormstone, I.M.; Wormstone, Y.M.; Smith, A.J.O.; Eldred, J.A. Posterior capsule opacification: What’s in the bag? Prog. Retin. Eye Res. 2020, 82, 100905. [Google Scholar] [CrossRef]
- Wormstone, I.M.; Eldred, J.A. Experimental models for posterior capsule opacification research. Exp. Eye Res. 2016, 142, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Yu, S.; Song, H.; Zhao, Y.; Xie, S.; Tang, X.; Yuan, X. Posterior capsular opacification comparison between morphology and objective visual function. BMC Ophthalmol. 2019, 19, 40. [Google Scholar] [CrossRef] [PubMed]
- Aslam, T.M.; Aspinall, P.; Dhillon, B. Posterior capsule morphology determinants of visual function. Graefe’s Arch. Clin. Exp. Ophthalmol. 2003, 241, 208–212. [Google Scholar] [CrossRef]
- Boswell, B.A.; VanSlyke, J.K.; Musil, L.S. Regulation of Lens Gap Junctions by Transforming Growth Factor Beta. Mol. Biol. Cell 2010, 21, 1686–1697. [Google Scholar] [CrossRef] [PubMed]
- Shu, D.Y.; Wojciechowski, M.; Lovicu, F.J. ERK1/2-mediated EGFR-signaling is required for TGFβ-induced lens epithelial-mesenchymal transition. Exp. Eye Res. 2019, 178, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Musil, L.S. Primary Cultures of Embryonic Chick Lens Cells as a Model System to Study Lens Gap Junctions and Fiber Cell Differentiation. J. Membr. Biol. 2012, 245, 357–368. [Google Scholar] [CrossRef]
- Liu, J.; Hales, A.M.; Chamberlain, C.G.; McAvoy, J.W. Induction of cataract-like changes in rat lens epithelial explants by transforming growth factor beta. Investig. Ophthalmol. Vis. Sci. 1994, 35, 388–401. [Google Scholar]
- Shu, D.Y.; Wojciechowski, M.C.; Lovicu, F.J. Bone Morphogenetic Protein-7 Suppresses TGFβ2-Induced Epithelial-Mesenchymal Transition in the Lens: Implications for Cataract Prevention. Investig. Ophthalmol. Vis. Sci. 2017, 58, 781–796. [Google Scholar] [CrossRef]
- Lovicu, F.J.; Schulz, M.W.; Hales, A.M.; Vincent, L.N.; Overbeek, P.A.; Chamberlain, C.G.; McAvoy, J.W. TGFβ induces morphological and molecular changes similar to human anterior subcapsular cataract. Br. J. Ophthalmol. 2002, 86, 220. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, Y.; Lovicu, F.J.; A Overbeek, P. Lens-specific expression of transforming growth factor beta1 in transgenic mice causes anterior subcapsular cataracts. J. Clin. Investig. 1998, 101, 625–634. [Google Scholar] [CrossRef]
- Koike, Y.; Yozaki, M.; Utani, A.; Murota, H. Fibroblast growth factor 2 accelerates the epithelial–mesenchymal transition in keratinocytes during wound healing process. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Maruno, K.A.; Lovicu, F.J.; Chamberlain, C.G.; WMcAvoy, J. Apoptosis is a feature of TGFß-induced cataract. Clin. Exp. Optom. 2002, 85, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Strand, D.W.; Liang, Y.-Y.; Yang, F.; Barron, D.A.; Ressler, S.J.; Schauer, I.G.; Feng, X.-H.; Rowley, D.R. TGF-β in-duction of FGF-2 expression in stromal cells requires integrated smad3 and MAPK pathways. Am. J. Clin. Exp. Urol. 2014, 2, 239–248. [Google Scholar]
- Wojciechowski, M.C.; Mahmutovic, L.; Shu, D.Y.; Lovicu, F.J. ERK1/2 signaling is required for the initiation but not progression of TGFβ-induced lens epithelial to mesenchymal transition (EMT). Exp. Eye Res. 2017, 159, 98–113. [Google Scholar] [CrossRef]
- Shirakihara, T.; Horiguchi, K.; Miyazawa, K.; Ehata, S.; Shibata, T.; Morita, I.; Miyazono, K.; Saitoh, M. TGF-β regulates isoform switching of FGF receptors and epithelial-mesenchymal transition. EMBO J. 2011, 30, 783–795. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; McAvoy, J.W.; Lovicu, F.J. Growth Factor Signaling in Vitreous Humor–Induced Lens Fiber Differentiation. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3599–3610. [Google Scholar] [CrossRef]
- de Iongh, R.U.; Lovicu, F.J.; Overbeek, P.A.; Schneider, M.D.; Joya, J.; Hardeman, E.D.; McAvoy, J.W. Requirement for TGFbeta receptor signaling during terminal lens fiber differentiation. Development 2001, 128, 3995–4010. [Google Scholar] [CrossRef]
- Shu, D.Y.; Lovicu, F.J. Enhanced EGF receptor-signaling potentiates TGFβ-induced lens epithelial-mesenchymal transition. Exp. Eye Res. 2019, 185, 107693. [Google Scholar] [CrossRef] [PubMed]
- Kokawa, N.; Sotozono, C.; Nishida, K.; Kinoshita, S. High total TGF-β2 levels in normal human tears. Curr. Eye Res. 1996, 15, 341–343. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Itonaga, K.; Marunouchi, T.; Majima, K. Concentration of Transforming Growth Factor β2 in Aqueous Humor. Ophthalmic Res. 2005, 37, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, Y.; Ochiai, H. Higher Concentration of Transforming Growth Factor-β in Aqueous Humor of Glaucomatous Eyes and Diabetic Eyes. Jpn. J. Ophthalmol. 2002, 46, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.; Daher, A.M.; Agarwal, R. Aqueous humor TGF-β2 levels in patients with open-angle glaucoma: A meta-analysis. Mol. Vis. 2015, 21, 612–620. [Google Scholar] [PubMed]
- Cousins, S.W.; McCabe, M.M.; Danielpour, D.; Streilein, J.W. Identification of transforming growth factor-beta as an immunosuppressive factor in aqueous humor. Investig. Ophthalmol. Vis. Sci. 1991, 32, 2201–2211. [Google Scholar]
- de Iongh, R.U.; Lovicu, F.J.; Chamberlain, C.G.; McAvoy, J.W. Differential expression of fibroblast growth factor receptors during rat lens morphogenesis and growth. Investig. Ophthalmol. Vis. Sci. 1997, 38, 1688–1699. [Google Scholar]
- Dawes, L.J.; Sugiyama, Y.; Lovicu, F.J.; Harris, C.G.; Shelley, E.J.; McAvoy, J.W. Interactions between lens epithelial and fiber cells reveal an intrinsic self-assembly mechanism. Dev. Biol. 2014, 385, 291–303. [Google Scholar] [CrossRef]
- Kurosaka, D.; Kato, K.; Nagamoto, T.; Negishi, K. Growth factors influence contractility and alpha-smooth muscle actin expression in bovine lens epithelial cells. Investig. Ophthalmol. Vis. Sci. 1995, 36, 1701–1708. [Google Scholar]
- Cushing, M.C.; Mariner, P.D.; Liao, J.; Sims, E.A.; Anseth, K.S. Fibroblast growth factor represses Smad-mediated myofibroblast activation in aortic valvular interstitial cells. FASEB J. 2008, 22, 1769–1777. [Google Scholar] [CrossRef]
- Ramos, C.; Becerril, C.; Montaño, M.; García-De-Alba, C.; Ramírez, R.; Checa, M.; Pardo, A.; Selman, M. FGF-1 reverts epithelial-mesenchymal transition induced by TGF-β1 through MAPK/ERK kinase pathway. Am. J. Physiol. Cell. Mol. Physiol. 2010, 299, L222–L231. [Google Scholar] [CrossRef] [PubMed]
- Schevzov, G.; Whittaker, S.P.; Fath, T.; Lin, J.J.-C.; Gunning, P.W. Tropomyosin isoforms and reagents. Bioarchitecture 2011, 1, 135–164. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Nowak, R.B.; Amadeo, M.B.; Biswas, S.K.; Lo, W.-K.; Fowler, V.M. Tropomyosin 3.5 protects the F-actin networks required for tissue biomechanical properties. J. Cell Sci. 2018, 131, jcs222042. [Google Scholar] [CrossRef] [PubMed]
- Parreno, J.; Amadeo, M.B.; Kwon, E.H.; Fowler, V.M. Tropomyosin 3.1 association with actin stress fibers is required for lens epithelial to mesenchymal transition. Investig. Ophthalmol. Vis. Sci. 2020, 61, 2. [Google Scholar] [CrossRef] [PubMed]
- Gateva, G.; Kremneva, E.; Reindl, T.; Kotila, T.; Kogan, K.; Gressin, L.; Gunning, P.W.; Manstein, D.J.; Michelot, A.; Lappalainen, P. Tropomyosin Isoforms Specify Functionally Distinct Actin Filament Populations In Vitro. Curr. Biol. 2017, 27, 705–713. [Google Scholar] [CrossRef]
- Wang, Q.; Stump, R.; McAvoy, J.W.; Lovicu, F.J. MAPK/ERK1/2 and PI3-kinase signalling pathways are required for vitreous-induced lens fibre cell differentiation. Exp. Eye Res. 2008, 88, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Le, A.-C.N.; Musil, L.S. FGF Signaling in Chick Lens Development. Dev. Biol. 2001, 233, 394–411. [Google Scholar] [CrossRef]
- Shin, E.H.; Zhao, G.; Wang, Q.; Lovicu, F.J. Sprouty gain of function disrupts lens cellular processes and growth by restricting RTK signaling. Dev. Biol. 2015, 406, 129–146. [Google Scholar] [CrossRef]
- Susanto, A.; Zhao, G.; Wazin, F.; Feng, Y.; Rasko, J.E.; Bailey, C.G.; Lovicu, F.J. Spred negatively regulates lens growth by modulating epithelial cell proliferation and fiber differentiation. Exp. Eye Res. 2019, 178, 160–175. [Google Scholar] [CrossRef]
- Saika, S.; Kono-Saika, S.; Ohnishi, Y.; Sato, M.; Muragaki, Y.; Ooshima, A.; Flanders, K.C.; Yoo, J.; Anzano, M.; Liu, C.-Y.; et al. Smad3 Signaling Is Required for Epithelial-Mesenchymal Transition of Lens Epithelium after Injury. Am. J. Pathol. 2004, 164, 651–663. [Google Scholar] [CrossRef]
- Saika, S.; Miyamoto, T.; Ishida, I.; Shirai, K.; Ohnishi, Y.; Ooshima, A.; McAvoy, J.W. TGFbeta-Smad signalling in postoperative human lens epithelial cells. Br. J. Ophthalmol. 2002, 86, 1428–1433. [Google Scholar] [CrossRef] [PubMed]
- Stolen, C.M.; Jackson, M.W.; Griep, A.E. Overexpression of FGF-2 modulates fiber cell differentiation and survival in the mouse lens. Development 1997, 124, 4009–4017. [Google Scholar] [CrossRef]
- Kubo, E.; Shibata, T.; Singh, D.P.; Sasaki, H. Roles of TGF β and FGF Signals in the Lens: Tropomyosin Regulation for Posterior Capsule Opacity. Int. J. Mol. Sci. 2018, 19, 3093. [Google Scholar] [CrossRef] [PubMed]
- Akatsu, Y.; Takahashi, N.; Yoshimatsu, Y.; Kimuro, S.; Muramatsu, T.; Katsura, A.; Maishi, N.; Suzuki, H.; Inazawa, J.; Hida, K.; et al. Fibroblast growth factor signals regulate transforming growth factor-β-induced endothelial-to-myofibroblast transition of tumor endothelial cells via Elk1. Mol. Oncol. 2019, 13, 1706–1724. [Google Scholar] [CrossRef] [PubMed]
- Strutz, F.; Zeisberg, M.; Renziehausen, A.; Raschke, B.; Becker, V.; Kooten, C.V.; Müller, G.A. TGF-β1 induces proliferation in human renal fibroblasts via induction of basic fibroblast growth factor (FGF-2). Kidney Int. 2001, 59, 579–592. [Google Scholar] [CrossRef]
- Bordignon, P.; Bottoni, G.; Xu, X.; Popescu, A.S.; Truan, Z.; Guenova, E.; Kofler, L.; Jafari, P.; Ostano, P.; Röcken, M.; et al. Dualism of FGF and TGF-β Signaling in Heterogeneous Cancer-Associated Fibroblast Activation with ETV1 as a Critical Determinant. Cell Rep. 2019, 28, 2358–2372.e6. [Google Scholar] [CrossRef]
- Symonds, J.G.; Lovicu, F.J.; Chamberlain, C.G. Posterior capsule opacification-like changes in rat lens explants cultured with TGFβ and FGF: Effects of cell coverage and regional differences. Exp. Eye Res. 2006, 82, 693–699. [Google Scholar] [CrossRef]
- Lovicu, F.J.; Chamberlain, C.G.; McAvoy, J.W. Differential effects of aqueous and vitreous on fiber differentiation and extracellular matrix accumulation in lens epithelial explants. Investig. Ophthalmol. Vis. Sci. 1995, 36, 1459–1469. [Google Scholar]
- Kondo, T.; Ishiga-Hashimoto, N.; Nagai, H.; Takeshita, A.; Mino, M.; Morioka, H.; Kusakabe, K.T.; Okada, T. Expression of transforming growth factor β and fibroblast growth factor 2 in the lens epithelium of Morioka cataract mice. Congenit. Anom. 2014, 54, 104–109. [Google Scholar] [CrossRef]
- Lovicu, F.J.; McAvoy, J.W. The age of rats affects the response of lens epithelial explants to fibroblast growth factor. An ultrastructural analysis. Investig. Ophthalmol. Vis. Sci. 1992, 33, 2269–2278. [Google Scholar]
- Zhao, G.; Bailey, C.G.; Feng, Y.; Rasko, J.; Lovicu, F.J. Negative regulation of lens fiber cell differentiation by RTK antagonists Spry and Spred. Exp. Eye Res. 2018, 170, 148–159. [Google Scholar] [CrossRef] [PubMed]
- Newitt, P.; Boros, J.; Madakashira, B.P.; Robinson, M.L.; Reneker, L.W.; McAvoy, J.W.; Lovicu, F.J. Sef is a negative regulator of fiber cell differentiation in the ocular lens. Differentiation 2010, 80, 53–67. [Google Scholar] [CrossRef] [PubMed]

| Treatment | Concentration | Regional Cell Response in Explant | ||
|---|---|---|---|---|
| FGF-2 (ng/mL) | TGF-β2 (pg/mL) | FGF-2 (ng/mL) | TGF-β2 (pg/mL) | |
| f/t | 5 | 50 | EMT | EMT |
| f/T | 5 | 200 | EMT | EMT |
| F/t | 200 | 50 | EMT | Fibre Differentiation |
| F/T | 200 | 200 | EMT | EMT |
| Localisation of t-Smad2/3 (Total Mean % of Fluorescence) | ||||
|---|---|---|---|---|
| Treatment | CLECs | PLECs | ||
| Nuclear | Cytoplasmic | Nuclear | Cytoplasmic | |
| Control | 0.35 ± 0.351 | 99.65 ± 0.351 | 2.91 ± 0.833 | 97.09 ± 0.833 |
| FGF-2 (200 ng/mL) | 1.70 ± 0.988 | 98.30 ± 0.988 | 2.55 ± 1.047 | 97.45 ± 1.047 |
| TGF-β2 (50 pg/mL) | 88.80 ± 4.217 | 11.20 ± 4.217 | 86.40 ± 5.444 | 13.60 ± 5.444 |
| FGF-2 (200 ng/mL) + TGF-β2 (50 pg/mL) | 44.87 ± 14.058 | 55.13 ± 14.058 | 19.85 ± 9.090 | 80.15 ± 9.090 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flokis, M.; Lovicu, F.J. FGF-2 Differentially Regulates Lens Epithelial Cell Behaviour during TGF-β-Induced EMT. Cells 2023, 12, 827. https://doi.org/10.3390/cells12060827
Flokis M, Lovicu FJ. FGF-2 Differentially Regulates Lens Epithelial Cell Behaviour during TGF-β-Induced EMT. Cells. 2023; 12(6):827. https://doi.org/10.3390/cells12060827
Chicago/Turabian StyleFlokis, Mary, and Frank J. Lovicu. 2023. "FGF-2 Differentially Regulates Lens Epithelial Cell Behaviour during TGF-β-Induced EMT" Cells 12, no. 6: 827. https://doi.org/10.3390/cells12060827
APA StyleFlokis, M., & Lovicu, F. J. (2023). FGF-2 Differentially Regulates Lens Epithelial Cell Behaviour during TGF-β-Induced EMT. Cells, 12(6), 827. https://doi.org/10.3390/cells12060827







