The Research Progress in Transforming Growth Factor-β2
Abstract
1. Introduction
2. The Molecular Biology of TGF-β2
2.1. The Expression and Procession of TGF-β2
2.2. The Activation of TGF-β2
| Activators | TGF-β1 | TGF-β2 | TGF-β3 | Reference |
|---|---|---|---|---|
| Integrins | Activate | Unable to activate | Activate | [18,19] |
| Proteases | Activate | Activate | Activate | [24] |
| TSP-1 | Activate | Activate | NA | [26,27] |
| ROS | Activate | Unable to activate | Unable to activate | [28] |
| pH | ||||
| pH 3.1–4.1 pH 11.0–11.9 | Activate | Activate | NA | [30] |
| pH 2.5–3.1 | NA | NA | Activate | |
| pH 10.0–12.3 | ||||
| Heat | ||||
| 70 °C (10 min) | Fully activate | NA | NA | [30] |
| 75 °C (5 min) | Fully activate | Partially activate | Partially activate | |
| 85–90 °C (1 min) | Fully activate | NA | NA | |
| 100 °C (5 min) | Partially inactive | Fully activate | Fully activate | |
| Mechanical force | Activate | NA | NA | [31,32] |
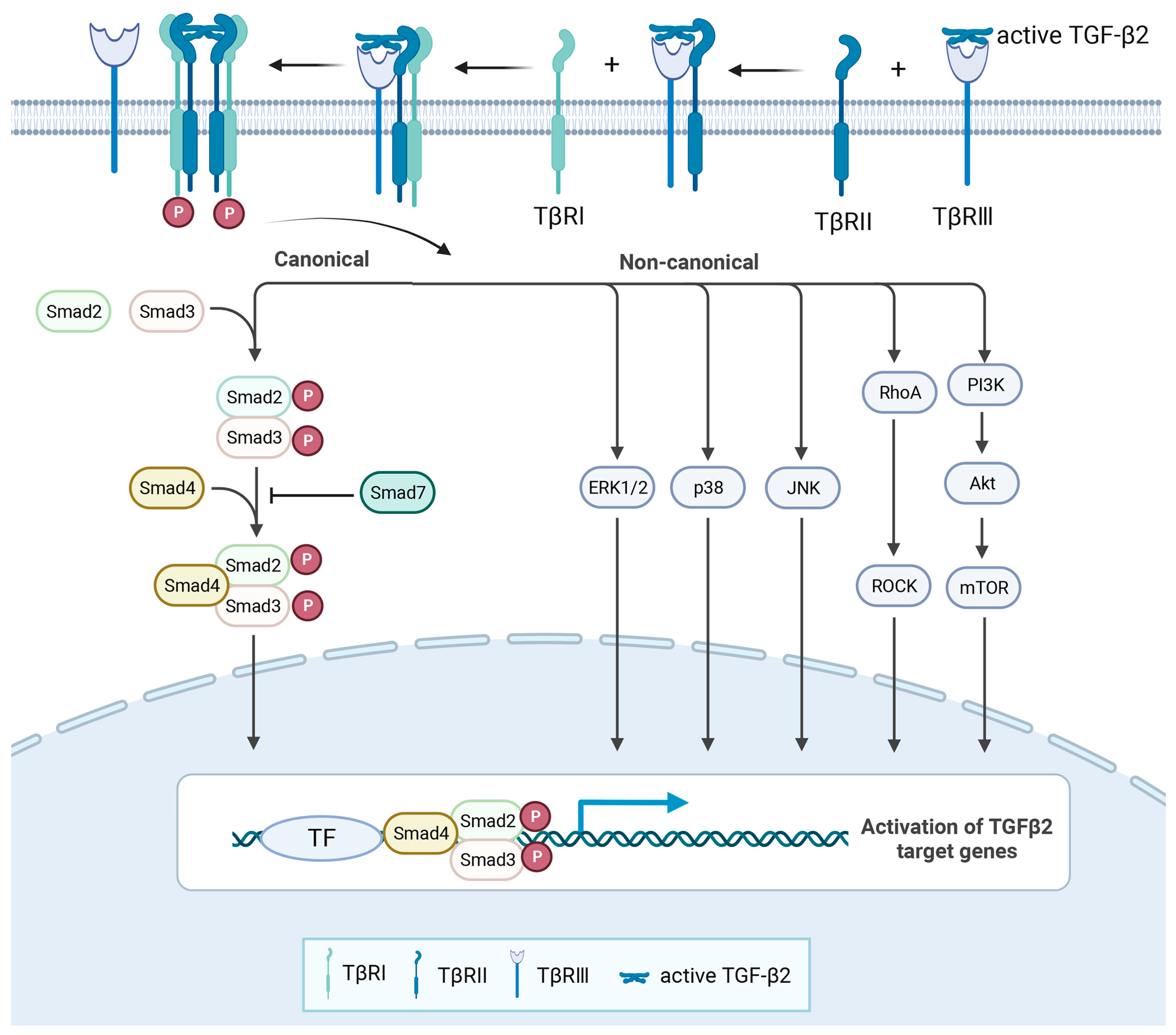
2.3. The Signalling Pathway of TGF-β2
Receptors
2.4. The Regulation of TGF-β2 Expression (Table 3)
2.4.1. Transcription Factors
2.4.2. Noncoding RNA
2.4.3. External Stimulus
| Effect | Mechanism | Diseases or Cell Types | Reference | |
|---|---|---|---|---|
| External stimulus | ||||
| Glypican 3 | Downregulate | NA | Hepatocellular carcinoma | [67] |
| Glycated- collagen | Upregulate | NA | Diabetic- cardiomyopathy | [68] |
| HDL | Upregulate | Activate PI3K/Akt | Atherosclerosis | [69] |
| TGF-β1 | Downregulate | NA | Fibroblastic cell | [77] |
| TGF-β2 | Upregulate | Inhibit Smad7 | Necrotising enterocolitis | [78] |
| IL-4 IL-13 | Upregulate | NA | Asthma | [70] |
| IFN-γ | Downregulate | Activate JAK-STAT | Retinal diseases | [71] |
| IL-1β | Upregulate | NA | Renal fibrosis | [72] |
| H2O2 | Upregulate | Activate p38 MAPK | Systemic inflammation | [73] |
| Hypoxia | Upregulate | Activate CAGA box | Endothelial cell | [74] |
| Lactate | Upregulate | Activate by thrombospondin-1 | Glioma | [27] |
| Cell density | Upregulate | NA | Corneal epithelial | [76] |
| Shear stress | Downregulate | NA | Tendon cell | [31] |
| Transcription factors | ||||
| CREBH | Upregulate | Bind promoter region at −49 to −43 | Hepatitis C | [42] |
| ERRγ | Upregulate | Bind promoter region at −1686 to −1676 | Acute liver injury | [43] |
| HOXB7 | Upregulate | Binding region unknown | Breast cancer | [44] |
| HOXA10 | Upregulate | Binding region unknown | Acute myeloid leukemia | [45] |
| Snail | Upregulate | Binding region unknown | Pancreatic cancer | [46] |
| ATF3 | Upregulate | Binding region unknown | Vascular diseases | [47] |
| ATF2 | Upregulate | Binding region unknown | Intestinal epithelial cells | [48] |
| PPARα | Upregulate | Binding region unknown | Glycolipid metabolism | [50] |
| PPARγ | Downregulate | Binding region unknown | Nonsmall cell lung cancer | [49] |
| RFX | Downregulate | Bind promoter region at −113 to −100 | Neuroblastoma | [51] |
| Noncoding RNA | ||||
| miR-7-5p | Downregulate | Bind 3′UTR | Lung cancer metastasis | [53] |
| miR-148a | Downregulate | Bind 3′UTR | Gastric cancer | [54] |
| miR-193a-3p | Downregulate | Bind 3′UTR | Congenital heart disease | [55] |
| miR-29b/ 29c-3p | Downregulate | Bind 3′UTR | Fibroblast | [56] |
| miR-200a | Downregulate | Bind 3′UTR | Renal fibrogenesis | [57] |
| miR-148b | Downregulate | Bind 3′UTR | Skin wound healing | [58] |
| miR-31 | Downregulate | Bind 3′UTR | Hairpoor | [59] |
| miR-193b | Downregulate | Bind 3′UTR | Chondrogenesis | [60] |
| miR-466a | Downregulate | Bind 3′UTR | Allogeneic transplantation | [61] |
| circUbe2k | Upregulate | Sponge miR-149-5p | Hepatic fibrosis | [62] |
| circ_0001293 | Upregulate | Sponge miR-8114 | Epilepsy | [63] |
| circRIP2 | Upregulate | Sponge miR-1305 | Bladder cancer | [64] |
| lncRNA CASC9 | Upregulate | Sponge miR-758-3p | Bladder cancer | [65] |
| LncMIAT | Upregulate | Sponge miR-16-5p | Liver fibrosis | [66] |
3. The Physiological and Pathological Roles of TGF-β2
3.1. Eye System
3.2. Cardiovascular System
3.3. Motor System
3.4. Immune System
3.5. Tumorigenesis
4. Conclusions and Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morikawa, M.; Derynck, R.; Miyazono, K. TGF-β and the TGF-β Family: Context-Dependent Roles in Cell and Tissue Physiology. Cold Spring Harb. Perspect. Biol. 2016, 8, a021873. [Google Scholar] [CrossRef] [PubMed]
- Derynck, R.; Jarrett, J.A.; Chen, E.Y.; Eaton, D.H.; Bell, J.R.; Assoian, R.K.; Roberts, A.B.; Sporn, M.B.; Goeddel, D.V. Human transforming growth factor-beta complementary DNA sequence and expression in normal and transformed cells. Nature 1985, 316, 701–705. [Google Scholar] [CrossRef] [PubMed]
- Moses, H.L.; Roberts, A.B.; Derynck, R. The Discovery and Early Days of TGF-β: A Historical Perspective. Cold Spring Harb. Perspect. Biol. 2016, 8, a021865. [Google Scholar] [CrossRef] [PubMed]
- Derynck, R.; Budi, E.H. Specificity, versatility, and control of TGF-β family signaling. Sci. Signal. 2019, 12, eaav5183. [Google Scholar] [CrossRef] [PubMed]
- Baardsnes, J.; Hinck, C.S.; Hinck, A.P.; O’Connor-McCourt, M.D. TbetaR-II discriminates the high- and low-affinity TGF-beta isoforms via two hydrogen-bonded ion pairs. Biochemistry 2009, 48, 2146–2155. [Google Scholar] [CrossRef]
- Shull, M.M.; Ormsby, I.; Kier, A.B.; Pawlowski, S.; Diebold, R.J.; Yin, M.; Allen, R.; Sidman, C.; Proetzel, G.; Calvin, D.; et al. Targeted disruption of the mouse transforming growth factor-beta 1 gene results in multifocal inflammatory disease. Nature 1992, 359, 693–699. [Google Scholar] [CrossRef] [PubMed]
- Kaartinen, V.; Voncken, J.W.; Shuler, C.; Warburton, D.; Bu, D.; Heisterkamp, N.; Groffen, J. Abnormal lung development and cleft palate in mice lacking TGF-beta 3 indicates defects of epithelial-mesenchymal interaction. Nat. Genet. 1995, 11, 415–421. [Google Scholar] [CrossRef]
- Sanford, L.P.; Ormsby, I.; Gittenberger-de Groot, A.C.; Sariola, H.; Friedman, R.; Boivin, G.P.; Cardell, E.L.; Doetschman, T. TGFbeta2 knockout mice have multiple developmental defects that are non-overlapping with other TGFbeta knockout phenotypes. Development 1997, 124, 2659–2670. [Google Scholar] [CrossRef]
- Foitzik, K.; Paus, R.; Doetschman, T.; Dotto, G.P. The TGF-beta2 isoform is both a required and sufficient inducer of murine hair follicle morphogenesis. Dev. Biol. 1999, 212, 278–289. [Google Scholar] [CrossRef]
- Webb, N.R.; Madisen, L.; Rose, T.M.; Purchio, A.F. Structural and sequence analysis of TGF-beta 2 cDNA clones predicts two different precursor proteins produced by alternative mRNA splicing. DNA 1988, 7, 493–497. [Google Scholar] [CrossRef]
- Robertson, I.B.; Rifkin, D.B. Regulation of the Bioavailability of TGF-β and TGF-β-Related Proteins. Cold Spring Harb. Perspect. Biol. 2016, 8, a021907. [Google Scholar] [CrossRef]
- Stockis, J.; Colau, D.; Coulie, P.G.; Lucas, S. Membrane protein GARP is a receptor for latent TGF-beta on the surface of activated human Treg. Eur. J. Immunol. 2009, 39, 3315–3322. [Google Scholar] [CrossRef]
- Rifkin, D.B. Latent transforming growth factor-beta (TGF-beta) binding proteins: Orchestrators of TGF-beta availability. J. Biol. Chem. 2005, 280, 7409–7412. [Google Scholar] [CrossRef]
- Tran, D.Q.; Andersson, J.; Wang, R.; Ramsey, H.; Unutmaz, D.; Shevach, E.M. GARP (LRRC32) is essential for the surface expression of latent TGF-beta on platelets and activated FOXP3+ regulatory T cells. Proc. Natl. Acad. Sci. USA 2009, 106, 13445–13450. [Google Scholar] [CrossRef]
- Annes, J.P.; Munger, J.S.; Rifkin, D.B. Making sense of latent TGFbeta activation. J. Cell Sci. 2003, 116, 217–224. [Google Scholar] [CrossRef]
- Saharinen, J.; Keski-Oja, J. Specific sequence motif of 8-Cys repeats of TGF-beta binding proteins, LTBPs, creates a hydrophobic interaction surface for binding of small latent TGF-beta. Mol. Biol. Cell 2000, 11, 2691–2704. [Google Scholar] [CrossRef]
- Tzavlaki, K.; Moustakas, A. TGF-β Signaling. Biomolecules 2020, 10, 487. [Google Scholar] [CrossRef]
- Aluwihare, P.; Mu, Z.; Zhao, Z.; Yu, D.; Weinreb, P.H.; Horan, G.S.; Violette, S.M.; Munger, J.S. Mice that lack activity of alphavbeta6- and alphavbeta8-integrins reproduce the abnormalities of Tgfb1- and Tgfb3-null mice. J. Cell Sci. 2009, 122, 227–232. [Google Scholar] [CrossRef]
- Noma, T.; Glick, A.B.; Geiser, A.G.; O’Reilly, M.A.; Miller, J.; Roberts, A.B.; Sporn, M.B. Molecular cloning and structure of the human transforming growth factor-beta 2 gene promoter. Growth Factors 1991, 4, 247–255. [Google Scholar] [CrossRef]
- Jenkins, G. The role of proteases in transforming growth factor-beta activation. Int. J. Biochem. Cell Biol. 2008, 40, 1068–1078. [Google Scholar] [CrossRef]
- Sato, Y.; Rifkin, D.B. Inhibition of endothelial cell movement by pericytes and smooth muscle cells: Activation of a latent transforming growth factor-beta 1-like molecule by plasmin during co-culture. J. Cell Biol. 1989, 109, 309–315. [Google Scholar] [CrossRef]
- Akita, K.; Okuno, M.; Enya, M.; Imai, S.; Moriwaki, H.; Kawada, N.; Suzuki, Y.; Kojima, S. Impaired liver regeneration in mice by lipopolysaccharide via TNF-alpha/kallikrein-mediated activation of latent TGF-beta. Gastroenterology 2002, 123, 352–364. [Google Scholar] [CrossRef]
- Yu, Q.; Stamenkovic, I. Cell surface-localized matrix metalloproteinase-9 proteolytically activates TGF-beta and promotes tumor invasion and angiogenesis. Genes. Dev. 2000, 14, 163–176. [Google Scholar] [CrossRef]
- Dallas, S.L.; Zhao, S.; Cramer, S.D.; Chen, Z.; Peehl, D.M.; Bonewald, L.F. Preferential production of latent transforming growth factor beta-2 by primary prostatic epithelial cells and its activation by prostate-specific antigen. J. Cell Physiol. 2005, 202, 361–370. [Google Scholar] [CrossRef]
- Adams, J.C. Thrombospondins: Multifunctional regulators of cell interactions. Annu. Rev. Cell Dev. Biol. 2001, 17, 25–51. [Google Scholar] [CrossRef]
- Mir, F.A.; Contreras-Ruiz, L.; Masli, S. Thrombospondin-1-dependent immune regulation by transforming growth factor-β2-exposed antigen-presenting cells. Immunology 2015, 146, 547–556. [Google Scholar] [CrossRef]
- Seliger, C.; Leukel, P.; Moeckel, S.; Jachnik, B.; Lottaz, C.; Kreutz, M.; Brawanski, A.; Proescholdt, M.; Bogdahn, U.; Bosserhoff, A.K.; et al. Lactate-modulated induction of THBS-1 activates transforming growth factor (TGF)-beta2 and migration of glioma cells in vitro. PLoS ONE 2013, 8, e78935. [Google Scholar] [CrossRef]
- Jobling, M.F.; Mott, J.D.; Finnegan, M.T.; Jurukovski, V.; Erickson, A.C.; Walian, P.J.; Taylor, S.E.; Ledbetter, S.; Lawrence, C.M.; Rifkin, D.B.; et al. Isoform-specific activation of latent transforming growth factor beta (LTGF-beta) by reactive oxygen species. Radiat. Res. 2006, 166, 839–848. [Google Scholar] [CrossRef]
- Lyons, R.M.; Keski-Oja, J.; Moses, H.L. Proteolytic activation of latent transforming growth factor-beta from fibroblast-conditioned medium. J. Cell Biol. 1988, 106, 1659–1665. [Google Scholar] [CrossRef]
- Brown, P.D.; Wakefield, L.M.; Levinson, A.D.; Sporn, M.B. Physicochemical activation of recombinant latent transforming growth factor-beta’s 1, 2, and 3. Growth Factors 1990, 3, 35–43. [Google Scholar] [CrossRef]
- Fong, K.D.; Trindade, M.C.; Wang, Z.; Nacamuli, R.P.; Pham, H.; Fang, T.D.; Song, H.M.; Smith, R.L.; Longaker, M.T.; Chang, J. Microarray analysis of mechanical shear effects on flexor tendon cells. Plast. Reconstr. Surg. 2005, 116, 1393–1404. [Google Scholar] [CrossRef]
- Ahamed, J.; Burg, N.; Yoshinaga, K.; Janczak, C.A.; Rifkin, D.B.; Coller, B.S. In vitro and in vivo evidence for shear-induced activation of latent transforming growth factor-beta1. Blood 2008, 112, 3650–3660. [Google Scholar] [CrossRef] [PubMed]
- Cheifetz, S.; Hernandez, H.; Laiho, M.; ten Dijke, P.; Iwata, K.K.; Massagué, J. Distinct transforming growth factor-beta (TGF-beta) receptor subsets as determinants of cellular responsiveness to three TGF-beta isoforms. J. Biol. Chem. 1990, 265, 20533–20538. [Google Scholar] [CrossRef]
- De Crescenzo, G.; Hinck, C.S.; Shu, Z.; Zúñiga, J.; Yang, J.; Tang, Y.; Baardsnes, J.; Mendoza, V.; Sun, L.; López-Casillas, F.; et al. Three key residues underlie the differential affinity of the TGFbeta isoforms for the TGFbeta type II receptor. J. Mol. Biol. 2006, 355, 47–62. [Google Scholar] [CrossRef]
- Sankar, S.; Mahooti-Brooks, N.; Centrella, M.; McCarthy, T.L.; Madri, J.A. Expression of transforming growth factor type III receptor in vascular endothelial cells increases their responsiveness to transforming growth factor beta 2. J. Biol. Chem. 1995, 270, 13567–13572. [Google Scholar] [CrossRef]
- Brown, C.B.; Boyer, A.S.; Runyan, R.B.; Barnett, J.V. Requirement of type III TGF-beta receptor for endocardial cell transformation in the heart. Science 1999, 283, 2080–2082. [Google Scholar] [CrossRef]
- López-Casillas, F.; Wrana, J.L.; Massagué, J. Betaglycan presents ligand to the TGF beta signaling receptor. Cell 1993, 73, 1435–1444. [Google Scholar] [CrossRef]
- Stenvers, K.L.; Tursky, M.L.; Harder, K.W.; Kountouri, N.; Amatayakul-Chantler, S.; Grail, D.; Small, C.; Weinberg, R.A.; Sizeland, A.M.; Zhu, H.J. Heart and liver defects and reduced transforming growth factor beta2 sensitivity in transforming growth factor beta type III receptor-deficient embryos. Mol. Cell Biol. 2003, 23, 4371–4385. [Google Scholar] [CrossRef]
- Bartram, U.; Molin, D.G.; Wisse, L.J.; Mohamad, A.; Sanford, L.P.; Doetschman, T.; Speer, C.P.; Poelmann, R.E.; Gittenberger-de Groot, A.C. Double-outlet right ventricle and overriding tricuspid valve reflect disturbances of looping, myocardialization, endocardial cushion differentiation, and apoptosis in TGF-beta(2)-knockout mice. Circulation 2001, 103, 2745–2752. [Google Scholar] [CrossRef]
- López-Casillas, F.; Payne, H.M.; Andres, J.L.; Massagué, J. Betaglycan can act as a dual modulator of TGF-beta access to signaling receptors: Mapping of ligand binding and GAG attachment sites. J. Cell Biol. 1994, 124, 557–568. [Google Scholar] [CrossRef]
- Rotzer, D.; Roth, M.; Lutz, M.; Lindemann, D.; Sebald, W.; Knaus, P. Type III TGF-beta receptor-independent signalling of TGF-beta2 via TbetaRII-B, an alternatively spliced TGF-beta type II receptor. Embo J. 2001, 20, 480–490. [Google Scholar] [CrossRef]
- Chida, T.; Ito, M.; Nakashima, K.; Kanegae, Y.; Aoshima, T.; Takabayashi, S.; Kawata, K.; Nakagawa, Y.; Yamamoto, M.; Shimano, H.; et al. Critical role of CREBH-mediated induction of transforming growth factor β2 by hepatitis C virus infection in fibrogenic responses in hepatic stellate cells. Hepatology 2017, 66, 1430–1443. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y.S.; Kim, Y.H.; Radhakrishnan, K.; Kim, J.; Lee, I.K.; Cho, S.J.; Kim, D.K.; Dooley, S.; Lee, C.H.; Choi, H.S. Orphan nuclear receptor ERRγ regulates hepatic TGF-β2 expression and fibrogenic response in CCl(4)-induced acute liver injury. Arch. Toxicol. 2021, 95, 3071–3084. [Google Scholar] [CrossRef]
- Liu, S.; Jin, K.; Hui, Y.; Fu, J.; Jie, C.; Feng, S.; Reisman, D.; Wang, Q.; Fan, D.; Sukumar, S.; et al. HOXB7 promotes malignant progression by activating the TGFβ signaling pathway. Cancer Res. 2015, 75, 709–719. [Google Scholar] [CrossRef]
- Shah, C.A.; Wang, H.; Bei, L.; Platanias, L.C.; Eklund, E.A. HoxA10 regulates transcription of the gene encoding transforming growth factor beta2 (TGFbeta2) in myeloid cells. J. Biol. Chem. 2011, 286, 3161–3176. [Google Scholar] [CrossRef]
- Shields, M.A.; Ebine, K.; Sahai, V.; Kumar, K.; Siddiqui, K.; Hwang, R.F.; Grippo, P.J.; Munshi, H.G. Snail cooperates with KrasG12D to promote pancreatic fibrosis. Mol. Cancer Res. 2013, 11, 1078–1087. [Google Scholar] [CrossRef]
- Hong, L.; Li, F.; Tang, C.; Li, L.; Sun, L.; Li, X.; Zhu, L. Semaphorin 7A promotes endothelial to mesenchymal transition through ATF3 mediated TGF-β2/Smad signaling. Cell Death Dis. 2020, 11, 695. [Google Scholar] [CrossRef]
- Namachivayam, K.; MohanKumar, K.; Arbach, D.; Jagadeeswaran, R.; Jain, S.K.; Natarajan, V.; Mehta, D.; Jankov, R.P.; Maheshwari, A. All-Trans Retinoic Acid Induces TGF-β2 in Intestinal Epithelial Cells via RhoA- and p38α MAPK-Mediated Activation of the Transcription Factor ATF2. PLoS ONE 2015, 10, e0134003. [Google Scholar] [CrossRef]
- Serizawa, M.; Murakami, H.; Watanabe, M.; Takahashi, T.; Yamamoto, N.; Koh, Y. Peroxisome proliferator-activated receptor γ agonist efatutazone impairs transforming growth factor β2-induced motility of epidermal growth factor receptor tyrosine kinase inhibitor-resistant lung cancer cells. Cancer Sci. 2014, 105, 683–689. [Google Scholar] [CrossRef]
- Takahashi, H.; Alves, C.R.R.; Stanford, K.I.; Middelbeek, R.J.W.; Nigro, P.; Ryan, R.E.; Xue, R.; Sakaguchi, M.; Lynes, M.D.; So, K.; et al. TGF-β2 is an exercise-induced adipokine that regulates glucose and fatty acid metabolism. Nat. Metab. 2019, 1, 291–303. [Google Scholar] [CrossRef]
- Feng, C.; Zuo, Z. Regulatory factor X1-induced down-regulation of transforming growth factor β2 transcription in human neuroblastoma cells. J. Biol. Chem. 2012, 287, 22730–22739. [Google Scholar] [CrossRef]
- Bartel, D.P. Metazoan MicroRNAs. Cell 2018, 173, 20–51. [Google Scholar] [CrossRef] [PubMed]
- Su, T.; Huang, S.; Zhang, Y.; Guo, Y.; Zhang, S.; Guan, J.; Meng, M.; Liu, L.; Wang, C.; Yu, D.; et al. miR-7/TGF-β2 axis sustains acidic tumor microenvironment-induced lung cancer metastasis. Acta Pharm. Sin. B 2022, 12, 821–837. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, Y. miR-148a downregulates the expression of transforming growth factor-β2 and SMAD2 in gastric cancer. Int. J. Oncol. 2016, 48, 1877–1885. [Google Scholar] [CrossRef]
- Zhong, L.; Yang, H.; Zhu, B.; Zhao, X.; Xie, M.; Cao, M.; Liu, C.; Zhao, D.; Lyu, Y.; Shang, W.; et al. The TBX1/miR-193a-3p/TGF-β2 Axis Mediates CHD by Promoting Ferroptosis. Oxid. Med. Cell Longev. 2022, 2022, 5130546. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.N.; Zou, X.; Fang, X.H.; Xu, J.D.; Xiao, Z.; Zhu, J.N.; Li, H.; Yang, J.; Zeng, N.; Yuan, S.J.; et al. The Smad3-miR-29b/miR-29c axis mediates the protective effect of macrophage migration inhibitory factor against cardiac fibrosis. Biochim. Biophys. Acta Mol. Basis Dis. 2019, 1865, 2441–2450. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Koh, P.; Winbanks, C.; Coughlan, M.T.; McClelland, A.; Watson, A.; Jandeleit-Dahm, K.; Burns, W.C.; Thomas, M.C.; Cooper, M.E.; et al. miR-200a Prevents renal fibrogenesis through repression of TGF-β2 expression. Diabetes 2011, 60, 280–287. [Google Scholar] [CrossRef]
- Miscianinov, V.; Martello, A.; Rose, L.; Parish, E.; Cathcart, B.; Mitić, T.; Gray, G.A.; Meloni, M.; Al Haj Zen, A.; Caporali, A. MicroRNA-148b Targets the TGF-β Pathway to Regulate Angiogenesis and Endothelial-to-Mesenchymal Transition during Skin Wound Healing. Mol. Ther. 2018, 26, 1996–2007. [Google Scholar] [CrossRef]
- Kim, B.K.; Yoon, S.K. Hairless Up-Regulates Tgf-β2 Expression via Down-Regulation of miR-31 in the Skin of “Hairpoor” (HrHp) Mice. J. Cell Physiol. 2015, 230, 2075–2085. [Google Scholar] [CrossRef]
- Hou, C.; Yang, Z.; Kang, Y.; Zhang, Z.; Fu, M.; He, A.; Zhang, Z.; Liao, W. MiR-193b regulates early chondrogenesis by inhibiting the TGF-beta2 signaling pathway. FEBS Lett. 2015, 589, 1040–1047. [Google Scholar] [CrossRef]
- Becker, W.; Nagarkatti, M.; Nagarkatti, P.S. miR-466a Targeting of TGF-β2 Contributes to FoxP3(+) Regulatory T Cell Differentiation in a Murine Model of Allogeneic Transplantation. Front. Immunol. 2018, 9, 688. [Google Scholar] [CrossRef]
- Zhu, S.; Chen, X.; Wang, J.N.; Xu, J.J.; Wang, A.; Li, J.J.; Wu, S.; Wu, Y.Y.; Li, X.F.; Huang, C.; et al. Circular RNA circUbe2k promotes hepatic fibrosis via sponging miR-149-5p/TGF-β2 axis. Faseb J. 2021, 35, e21622. [Google Scholar] [CrossRef]
- Hu, Y.; Meng, B.; Yin, S.; Yang, M.; Li, Y.; Liu, N.; Li, S.; Liu, Y.; Sun, D.; Wang, S.; et al. Scorpion venom peptide HsTx2 suppressed PTZ-induced seizures in mice via the circ_0001293/miR-8114/TGF-β2 axis. J. Neuroinflamm. 2022, 19, 284. [Google Scholar] [CrossRef]
- Su, Y.; Feng, W.; Shi, J.; Chen, L.; Huang, J.; Lin, T. circRIP2 accelerates bladder cancer progression via miR-1305/Tgf-β2/smad3 pathway. Mol. Cancer 2020, 19, 23. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Chen, F.; Zhan, H.; Chen, L.; Deng, Q.; Xiong, T.; Li, Y.; Ye, J. lncRNA CASC9 sponges miR-758-3p to promote proliferation and EMT in bladder cancer by upregulating TGF-β2. Oncol. Rep. 2021, 45, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Zhu, X.L.; Xu, D.H.; Li, S.; Yang, Q.; Feng, X.; Wei, Y.G.; Li, H.; Yang, L.; Zhang, Y.J.; et al. NPM promotes hepatotoxin-induced fibrosis by inhibiting ROS-induced apoptosis of hepatic stellate cells and upregulating lncMIAT-induced TGF-β2. Cell Death Dis. 2023, 14, 575. [Google Scholar] [CrossRef]
- Sun, C.K.; Chua, M.S.; He, J.; So, S.K. Suppression of glypican 3 inhibits growth of hepatocellular carcinoma cells through up-regulation of TGF-β2. Neoplasia 2011, 13, 735–747. [Google Scholar] [CrossRef] [PubMed]
- Talior-Volodarsky, I.; Arora, P.D.; Wang, Y.; Zeltz, C.; Connelly, K.A.; Gullberg, D.; McCulloch, C.A. Glycated Collagen Induces α11 Integrin Expression Through TGF-β2 and Smad3. J. Cell Physiol. 2015, 230, 327–336. [Google Scholar] [CrossRef]
- Norata, G.D.; Callegari, E.; Marchesi, M.; Chiesa, G.; Eriksson, P.; Catapano, A.L. High-density lipoproteins induce transforming growth factor-beta2 expression in endothelial cells. Circulation 2005, 111, 2805–2811. [Google Scholar] [CrossRef]
- Wen, F.Q.; Kohyama, T.; Liu, X.; Zhu, Y.K.; Wang, H.; Kim, H.J.; Kobayashi, T.; Abe, S.; Spurzem, J.R.; Rennard, S.I. Interleukin-4- and interleukin-13-enhanced transforming growth factor-beta2 production in cultured human bronchial epithelial cells is attenuated by interferon-gamma. Am. J. Respir. Cell Mol. Biol. 2002, 26, 484–490. [Google Scholar] [CrossRef]
- Nagineni, C.N.; Cherukuri, K.S.; Kutty, V.; Detrick, B.; Hooks, J.J. Interferon-gamma differentially regulates TGF-beta1 and TGF-beta2 expression in human retinal pigment epithelial cells through JAK-STAT pathway. J. Cell Physiol. 2007, 210, 192–200. [Google Scholar] [CrossRef]
- Felisaz, N.; Boumediene, K.; Ghayor, C.; Herrouin, J.F.; Bogdanowicz, P.; Galerra, P.; Pujol, J.P. Stimulating effect of diacerein on TGF-beta1 and beta2 expression in articular chondrocytes cultured with and without interleukin-1. Osteoarthr. Cartil. 1999, 7, 255–264. [Google Scholar] [CrossRef][Green Version]
- Montorfano, I.; Becerra, A.; Cerro, R.; Echeverría, C.; Sáez, E.; Morales, M.G.; Fernández, R.; Cabello-Verrugio, C.; Simon, F. Oxidative stress mediates the conversion of endothelial cells into myofibroblasts via a TGF-β1 and TGF-β2-dependent pathway. Lab. Investig. 2014, 94, 1068–1082. [Google Scholar] [CrossRef]
- Akman, H.O.; Zhang, H.; Siddiqui, M.A.; Solomon, W.; Smith, E.L.; Batuman, O.A. Response to hypoxia involves transforming growth factor-beta2 and Smad proteins in human endothelial cells. Blood 2001, 98, 3324–3331. [Google Scholar] [CrossRef]
- Baumann, F.; Leukel, P.; Doerfelt, A.; Beier, C.P.; Dettmer, K.; Oefner, P.J.; Kastenberger, M.; Kreutz, M.; Nickl-Jockschat, T.; Bogdahn, U.; et al. Lactate promotes glioma migration by TGF-beta2-dependent regulation of matrix metalloproteinase-2. Neuro Oncol. 2009, 11, 368–380. [Google Scholar] [CrossRef]
- Kawakita, T.; Espana, E.M.; Higa, K.; Kato, N.; Li, W.; Tseng, S.C. Activation of Smad-mediated TGF-β signaling triggers epithelial-mesenchymal transitions in murine cloned corneal progenitor cells. J. Cell Physiol. 2013, 228, 225–234. [Google Scholar] [CrossRef]
- Bascom, C.C.; Wolfshohl, J.R.; Coffey, R.J., Jr.; Madisen, L.; Webb, N.R.; Purchio, A.R.; Derynck, R.; Moses, H.L. Complex regulation of transforming growth factor beta 1, beta 2, and beta 3 mRNA expression in mouse fibroblasts and keratinocytes by transforming growth factors beta 1 and beta 2. Mol. Cell Biol. 1989, 9, 5508–5515. [Google Scholar] [CrossRef] [PubMed]
- Namachivayam, K.; Blanco, C.L.; MohanKumar, K.; Jagadeeswaran, R.; Vasquez, M.; McGill-Vargas, L.; Garzon, S.A.; Jain, S.K.; Gill, R.K.; Freitag, N.E.; et al. Smad7 inhibits autocrine expression of TGF-β2 in intestinal epithelial cells in baboon necrotizing enterocolitis. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 304, G167–G180. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Suzuki, S.; Sato, T.; Watanabe, M.; Higashide, M.; Tsugeno, Y.; Umetsu, A.; Furuhashi, M.; Ida, Y.; Hikage, F.; Ohguro, H. Hypoxia Differently Affects TGF-β2-Induced Epithelial Mesenchymal Transitions in the 2D and 3D Culture of the Human Retinal Pigment Epithelium Cells. Int. J. Mol. Sci. 2022, 23, 5473. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Liu, S.; Pu, L.; Luo, J.; Liu, H.; Wu, W. Nintedanib prevents TGF-β2-induced epithelial-mesenchymal transition in retinal pigment epithelial cells. Biomed. Pharmacother. 2023, 161, 114543. [Google Scholar] [CrossRef]
- Jang, H.Y.; Kim, S.J.; Park, K.S.; Kim, J.H. Klotho prevents transforming growth factor-β2-induced senescent-like morphological changes in the retinal pigment epithelium. Cell Death Dis. 2023, 14, 334. [Google Scholar] [CrossRef] [PubMed]
- Yao, L.; Yang, L.; Song, H.; Liu, T.; Yan, H. MicroRNA miR-29c-3p modulates FOS expression to repress EMT and cell proliferation while induces apoptosis in TGF-β2-treated lens epithelial cells regulated by lncRNA KCNQ1OT1. Biomed. Pharmacother. 2020, 129, 110290. [Google Scholar] [CrossRef]
- Sun, Y.; Xiong, L.; Wang, X.; Wang, L.; Chen, B.; Huang, J.; Huang, M.; Chen, J.; Wu, J.; Huang, S.; et al. Autophagy inhibition attenuates TGF-β2-induced epithelial-mesenchymal transition in lens epithelial cells. Life Sci. 2021, 265, 118741. [Google Scholar] [CrossRef]
- Cui, Y.; Yang, H.; Shi, S.; Ping, X.; Zheng, S.; Tang, X.; Yu, X.; Shentu, X. TP53INP2 Contributes to TGF-β2-Induced Autophagy during the Epithelial-Mesenchymal Transition in Posterior Capsular Opacification Development. Cells 2022, 11, 2385. [Google Scholar] [CrossRef]
- Yang, J.; Savvatis, K.; Kang, J.S.; Fan, P.; Zhong, H.; Schwartz, K.; Barry, V.; Mikels-Vigdal, A.; Karpinski, S.; Kornyeyev, D.; et al. Targeting LOXL2 for cardiac interstitial fibrosis and heart failure treatment. Nat. Commun. 2016, 7, 13710. [Google Scholar] [CrossRef]
- Ramnath, N.W.; Hawinkels, L.J.; van Heijningen, P.M.; te Riet, L.; Paauwe, M.; Vermeij, M.; Danser, A.H.; Kanaar, R.; ten Dijke, P.; Essers, J. Fibulin-4 deficiency increases TGF-β signalling in aortic smooth muscle cells due to elevated TGF-β2 levels. Sci. Rep. 2015, 5, 16872. [Google Scholar] [CrossRef]
- Edsfeldt, A.; Singh, P.; Matthes, F.; Tengryd, C.; Cavalera, M.; Bengtsson, E.; Dunér, P.; Volkov, P.; Karadimou, G.; Gisterå, A.; et al. Transforming growth factor-β2 is associated with atherosclerotic plaque stability and lower risk for cardiovascular events. Cardiovasc. Res. 2023, 119, 2061–2073. [Google Scholar] [CrossRef]
- Duan, M.; Liu, Y.; Guo, D.; Kan, S.; Niu, Z.; Pu, X.; Bai, M.; Zhang, D.; Du, W.; Xie, J. TGF-β2 increases cell-cell communication in chondrocytes via p-Smad3 signalling. Biochim. Biophys. Acta Mol. Cell Res. 2022, 1869, 119175. [Google Scholar] [CrossRef] [PubMed]
- Das, R.; Timur, U.T.; Edip, S.; Haak, E.; Wruck, C.; Weinans, H.; Jahr, H. TGF-β2 is involved in the preservation of the chondrocyte phenotype under hypoxic conditions. Ann. Anat. Anat. Anz. Off. Organ. Anat. Ges. 2015, 198, 1–10. [Google Scholar] [CrossRef]
- Tchetina, E.V.; Antoniou, J.; Tanzer, M.; Zukor, D.J.; Poole, A.R. Transforming growth factor-beta2 suppresses collagen cleavage in cultured human osteoarthritic cartilage, reduces expression of genes associated with chondrocyte hypertrophy and degradation, and increases prostaglandin E(2) production. Am. J. Pathol. 2006, 168, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; He, H.; Shen, X.; Tang, S.; Zhao, J.; Cao, X.; Han, S.; Cui, C.; Chen, Y.; Wei, Y.; et al. MicroRNA Profiling Reveals an Abundant miR-200a-3p Promotes Skeletal Muscle Satellite Cell Development by Targeting TGF-β2 and Regulating the TGF-β2/SMAD Signaling Pathway. Int. J. Mol. Sci. 2020, 21, 3274. [Google Scholar] [CrossRef]
- Um, S.; Lee, J.H.; Seo, B.M. TGF-β2 downregulates osteogenesis under inflammatory conditions in dental follicle stem cells. Int. J. Oral. Sci. 2018, 10, 29. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Feng, L.; Xu, J.; Yang, Z.; Wu, T.; Zhang, J.; Shi, L.; Zhu, D.; Zhang, J.; Li, G. MiR-378a suppresses tenogenic differentiation and tendon repair by targeting at TGF-β2. Stem Cell Res. Ther. 2019, 10, 108. [Google Scholar] [CrossRef]
- Koch, D.W.; Schnabel, L.V.; Ellis, I.M.; Bates, R.E.; Berglund, A.K. TGF-β2 enhances expression of equine bone marrow-derived mesenchymal stem cell paracrine factors with known associations to tendon healing. Stem Cell Res. Ther. 2022, 13, 477. [Google Scholar] [CrossRef]
- Liu, S.; Guo, J.; Cheng, X.; Li, W.; Lyu, S.; Chen, X.; Li, Q.; Wang, H. Molecular Evolution of Transforming Growth Factor-β (TGF-β) Gene Family and the Functional Characterization of Lamprey TGF-β2. Front. Immunol. 2022, 13, 836226. [Google Scholar] [CrossRef]
- Zhang, S.Z.; Wang, Q.Q.; Yang, Q.Q.; Gu, H.Y.; Yin, Y.Q.; Li, Y.D.; Hou, J.C.; Chen, R.; Sun, Q.Q.; Sun, Y.F.; et al. NG2 glia regulate brain innate immunity via TGF-β2/TGFBR2 axis. BMC Med. 2019, 17, 204. [Google Scholar] [CrossRef] [PubMed]
- De Feo, D.; Merlini, A.; Brambilla, E.; Ottoboni, L.; Laterza, C.; Menon, R.; Srinivasan, S.; Farina, C.; Garcia Manteiga, J.M.; Butti, E.; et al. Neural precursor cell-secreted TGF-β2 redirects inflammatory monocyte-derived cells in CNS autoimmunity. J. Clin. Investig. 2017, 127, 3937–3953. [Google Scholar] [CrossRef]
- Torres-Castro, P.; Grases-Pintó, B.; Abril-Gil, M.; Castell, M.; Rodríguez-Lagunas, M.J.; Pérez-Cano, F.J.; Franch, À. Modulation of the Systemic Immune Response in Suckling Rats by Breast Milk TGF-β2, EGF and FGF21 Supplementation. Nutrients 2020, 12, 1888. [Google Scholar] [CrossRef] [PubMed]
- Mabaya, L.; Matarira, H.T.; Tanyanyiwa, D.M.; Musarurwa, C.; Mukwembi, J. Levels of Total Antioxidant Capacity, sCD14, and TGF-β2 in Breast Milk Plasma of HIV-Infected and HIV-Uninfected Lactating Women. Breastfeed. Med. Off. J. Acad. Breastfeed. Med. 2021, 16, 821–826. [Google Scholar] [CrossRef]
- Corbet, C.; Bastien, E.; Santiago de Jesus, J.P.; Dierge, E.; Martherus, R.; Vander Linden, C.; Doix, B.; Degavre, C.; Guilbaud, C.; Petit, L.; et al. TGFβ2-induced formation of lipid droplets supports acidosis-driven EMT and the metastatic spreading of cancer cells. Nat. Commun. 2020, 11, 454. [Google Scholar] [CrossRef]
- Trempolec, N.; Degavre, C.; Doix, B.; Brusa, D.; Corbet, C.; Feron, O. Acidosis-Induced TGF-β2 Production Promotes Lipid Droplet Formation in Dendritic Cells and Alters Their Potential to Support Anti-Mesothelioma T Cell Response. Cancers 2020, 12, 1284. [Google Scholar] [CrossRef] [PubMed]
- Reithmeier, A.; Panizza, E.; Krumpel, M.; Orre, L.M.; Branca, R.M.M.; Lehtiö, J.; Ek-Rylander, B.; Andersson, G. Tartrate-resistant acid phosphatase (TRAP/ACP5) promotes metastasis-related properties via TGFβ2/TβR and CD44 in MDA-MB-231 breast cancer cells. BMC Cancer 2017, 17, 650. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Dai, C.Y.; Mei, Z.; Jiang, M.J.; Gu, D.N.; Huang, Q.; Tian, L. microRNA-193a stimulates pancreatic cancer cell repopulation and metastasis through modulating TGF-β2/TGF-βRIII signalings. J. Exp. Clin. Cancer Res. 2018, 37, 25. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, B.A.; Flanders, K.C.; Guérin, C.J.; Danielpour, D.; Anderson, D.H. Transforming growth factor beta 2 is the predominant isoform in the neural retina, retinal pigment epithelium-choroid and vitreous of the monkey eye. Exp. Eye Res. 1994, 59, 323–333. [Google Scholar] [CrossRef] [PubMed]
- Azhar, M.; Runyan, R.B.; Gard, C.; Sanford, L.P.; Miller, M.L.; Andringa, A.; Pawlowski, S.; Rajan, S.; Doetschman, T. Ligand-specific function of transforming growth factor beta in epithelial-mesenchymal transition in heart development. Dev. Dyn. 2009, 238, 431–442. [Google Scholar] [CrossRef] [PubMed]
- Sachan, N.; Phoon, C.K.L.; Zilberberg, L.; Kugler, M.C.; Ene, T.; Mintz, S.B.; Murtada, S.I.; Weiss, D.; Fishman, G.I.; Humphrey, J.D.; et al. TGFβ-2 haploinsufficiency causes early death in mice with Marfan syndrome. Matrix Biol. J. Int. Soc. Matrix Biol. 2023, 121, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Caja, L.; Dituri, F.; Mancarella, S.; Caballero-Diaz, D.; Moustakas, A.; Giannelli, G.; Fabregat, I. TGF-β and the Tissue Microenvironment: Relevance in Fibrosis and Cancer. Int. J. Mol. Sci. 2018, 19, 1294. [Google Scholar] [CrossRef]
- Colak, S.; Ten Dijke, P. Targeting TGF-β Signaling in Cancer. Trends Cancer 2017, 3, 56–71. [Google Scholar] [CrossRef]
- Peng, D.; Fu, M.; Wang, M.; Wei, Y.; Wei, X. Targeting TGF-β signal transduction for fibrosis and cancer therapy. Mol. Cancer 2022, 21, 104. [Google Scholar] [CrossRef]
- Corbet, C.; Feron, O. Tumour acidosis: From the passenger to the driver’s seat. Nat. Rev. Cancer 2017, 17, 577–593. [Google Scholar] [CrossRef]



| Organ | Tgfb1−/− | Tgfb2−/− | Tgfb3−/− |
|---|---|---|---|
| Heart | Generalised and extensive infiltration of inflammatory cells involving the pericardium, the myocardium, and the endocardium of the atria and ventricles | Congenital structural defects of the heart, including the arterial outflow tract, aortic and pulmonary orifices, atrioventricular valves, ventricular septum, and myocardium | NA |
| Lung | Lymphocytic and plasmacytic infiltration | Conducting airways collapsed | Branching morphogenesis and respiratory epithelial cell differentiation defects |
| Liver | Granulocyte and lymphocyte infiltration, multifocal hepatic necrosis and microgranulomas | NA | NA |
| Pancreas | Lymphocytic and plasmacytic infiltration | NA | NA |
| Stomach | Neutrophil and eosinophil cell infiltration | NA | NA |
| Salivary gland | Lymphocytic and plasmacytic infiltration | NA | NA |
| Striated muscle | Lymphocytic and plasmacytic infiltration | NA | NA |
| Brain | Granulocyte and lymphocyte infiltration | NA | NA |
| Eye | Conjunctivitis, ocular striated muscle inflammation, lacrimal gland inflammation | Hypercellular infusion in the posterior chamber, hyperplastic retina | NA |
| Skeletal | NA | Limb laxity, spina bifida occulta, sternum malformations, abnormal curvature of the ribs | NA |
| Craniofacial | NA | Retrognathia, dysmorphic calvaria | NA |
| Urogenital | NA | Agenesis renal pelvis, testicular ectopia and hypoplasia, ectopia of the uterine horns, degeneration of kidney tubular epithelium, adrenal ectopia | NA |
| Palate | NA | Cleft palate (partial penetrance, extensive palate cleft) | Cleft palate (full penetrance, soft palate cleft not involved) |
| Inner ear | NA | Absent spiral limbus and Rosenthal’s canal, undifferentiated inter-dental cells, partially canalised scala vestibuli | NA |
| Hair follicle | Slightly advanced hair follicle formation | Profound delay in hair follicle morphogenesis | NA |
| Other phenotypes | Slight enlargement of lymph nodes, smaller spleen and less distinct white pulp | Congenital cyanosis | NA |
| Organs | Consequences | Treatments | Reference |
|---|---|---|---|
| Eye system | Induces EMT (EMT of retinal pigment epithelial cells is a key mechanism in proliferative retinal diseases) | Human retinal pigment epithelium cells (20 ng/mL TGF-β2) | [79,80] |
| Induces senescence and EMT (Degenerative changes in the retinal pigment epithelium play a critical role in the progression of age-related macular degeneration) | Human retinal pigment epithelial cell and human lens epithelial cells (10 ng/mL or 12.5 ng/mL TGF-β2) | [81,82] | |
| Promote autophagy and EMT (Autophagy plays an important role in fibrotic cataracts) | Rabbit lens epithelial cells and human lens epithelial cells (5 ng/mL or 10 ng/mL TGF-β2) | [83,84] | |
| Cardiovascular system | Promote cardiac fibrosis (Loxl2 stimulates cardiac fibrosis by inducing TGF-β2; MiR-29b-3p and miR-29c-3p inhibit cardiac fibrosis by targeting Tgfb2) | Loxl2-treated TAC hearts and mouse cardiac fibroblasts from Ang-II-infused Mif-KO mice | [56,85] |
| Be associated with aortic aneurysm formation | TGF-β2 is elevated at higher levels in the conditioned medium from fibulin-4 deficient mice aortic smooth muscle cells, aortic lysates, and blood | [86] | |
| Reduce inflammation and matrix degradation and may be involved in maintaining plaque stability | RAW 264.7 cells and human THP-1 blood monocytes (5 ng/mL TGF-β2) | [87] | |
| Motor system | Increase chondrocyte communication, early chondrogenesis, maintain phenotype, and inhibit differentiation | Mouse chondrocytes and human osteoarthritic cartilage (5/10/25 ng/mL TGF-β2) | [60,88,89,90] |
| Inhibit skeletal muscle satellite cell differentiation and proliferation and promote apoptosis | Chicken skeletal muscle satellite cells (Inhibition of TGF-β2 by miR-200a-3p) | [91] | |
| Downregulate bone formation | Human dental follicle stem cells (1 μg/mL TGF-β2 inhibitor) | [92] | |
| Upregulate gene expression of collagens, extracellular matrix molecules, and growth factors associated with tendon healing | Mouse tendon-derived stem cells and equine bone marrow-derived mesenchymal stem cells (1 ng/mL TGF-β2) | [93,94] | |
| Immune system | Affect immune cell proliferation and apoptosis | MCF-7 cells, RAW 264.7 cells, lamprey supraneural myeloid body cells, and peripheral blood leukocytes (0.01/0.1/1/10 ng/mL TGF-β2) | [95] |
| Maintain brain immune homeostasis by regulating the chemokine receptor-modulated immune response in microglia | Mouse NG2 glial cells (5 ng/mL or 10 ng/mL TGF-β2) | [96] | |
| Redirect inflammatory monocyte-derived cells in central nervous system autoimmunity | Neural precursor cells from Tgfb2tm1Doe mice (Tgfb2−/−) and bone marrow-derived dendritic cells (0.01/1/10/100 ng/mL TGF-β2) | [97] | |
| Promote the maturation of immune development | G15 pregnant Wistar rats (TGF-β2 at 35 μg/kg/day) | [98] | |
| Have an impact on antiviral immunity | HIV breast feeding women | [99] | |
| Tumor | Sustain acidic tumor microenvironment- induced lung cancer metastasis | Human lung cancer cells (5 μg/mL of anti-TGF-β2 antibody) | [53] |
| Inhibit growth of hepatocellular carcinoma cells | Human hepatocellular carcinoma cells (1 ng/mL or 5 ng/mL TGF-β2) | [67] | |
| Support acidosis-driven EMT and the metastatic spreading of cancer cells | Human cervix SiHa, pharynx FaDu, colorectal HCT-116, and HT-29 cancer cell lines (10 µM TGFβ2-specific antisense oligonucleotide) | [100] | |
| Decrease dendritic cells migratory potential and activation and the anticancer immune response | Mouse bone marrow-derived dendritic cells (5 µM TGF-β receptor inhibitor) | [101] | |
| Mediate the effects of TRAP-dependent proliferation and migration in breast cancer cells | MDA-MB-231 breast cancer cell line (0.25 μg/mL TGF-β2 neutralising antibody) | [102] | |
| Block pancreatic cancer repopulation and metastasis | Human pancreatic cancer cell lines (Inhibition of TGF-β2 by miR-193a) | [103] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, M.-Y.; Liu, W.-J.; Wu, L.-Y.; Wang, G.; Zhang, C.-L.; Liu, J. The Research Progress in Transforming Growth Factor-β2. Cells 2023, 12, 2739. https://doi.org/10.3390/cells12232739
Wang M-Y, Liu W-J, Wu L-Y, Wang G, Zhang C-L, Liu J. The Research Progress in Transforming Growth Factor-β2. Cells. 2023; 12(23):2739. https://doi.org/10.3390/cells12232739
Chicago/Turabian StyleWang, Meng-Yan, Wen-Juan Liu, Le-Yi Wu, Gang Wang, Cheng-Lin Zhang, and Jie Liu. 2023. "The Research Progress in Transforming Growth Factor-β2" Cells 12, no. 23: 2739. https://doi.org/10.3390/cells12232739
APA StyleWang, M.-Y., Liu, W.-J., Wu, L.-Y., Wang, G., Zhang, C.-L., & Liu, J. (2023). The Research Progress in Transforming Growth Factor-β2. Cells, 12(23), 2739. https://doi.org/10.3390/cells12232739






