Using a Topical Formulation of Vitamin D for the Treatment of Vitiligo: A Systematic Review
Abstract
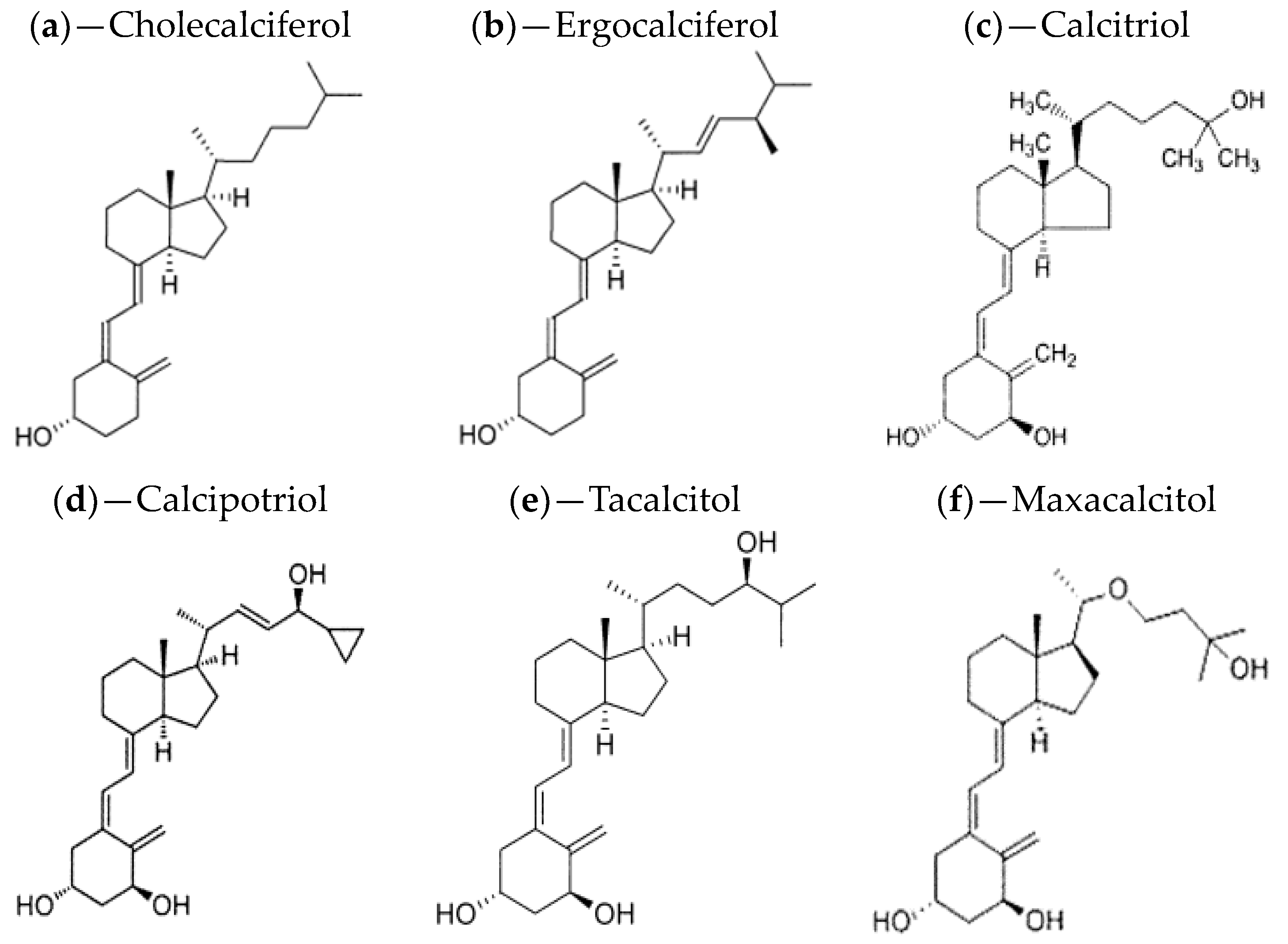
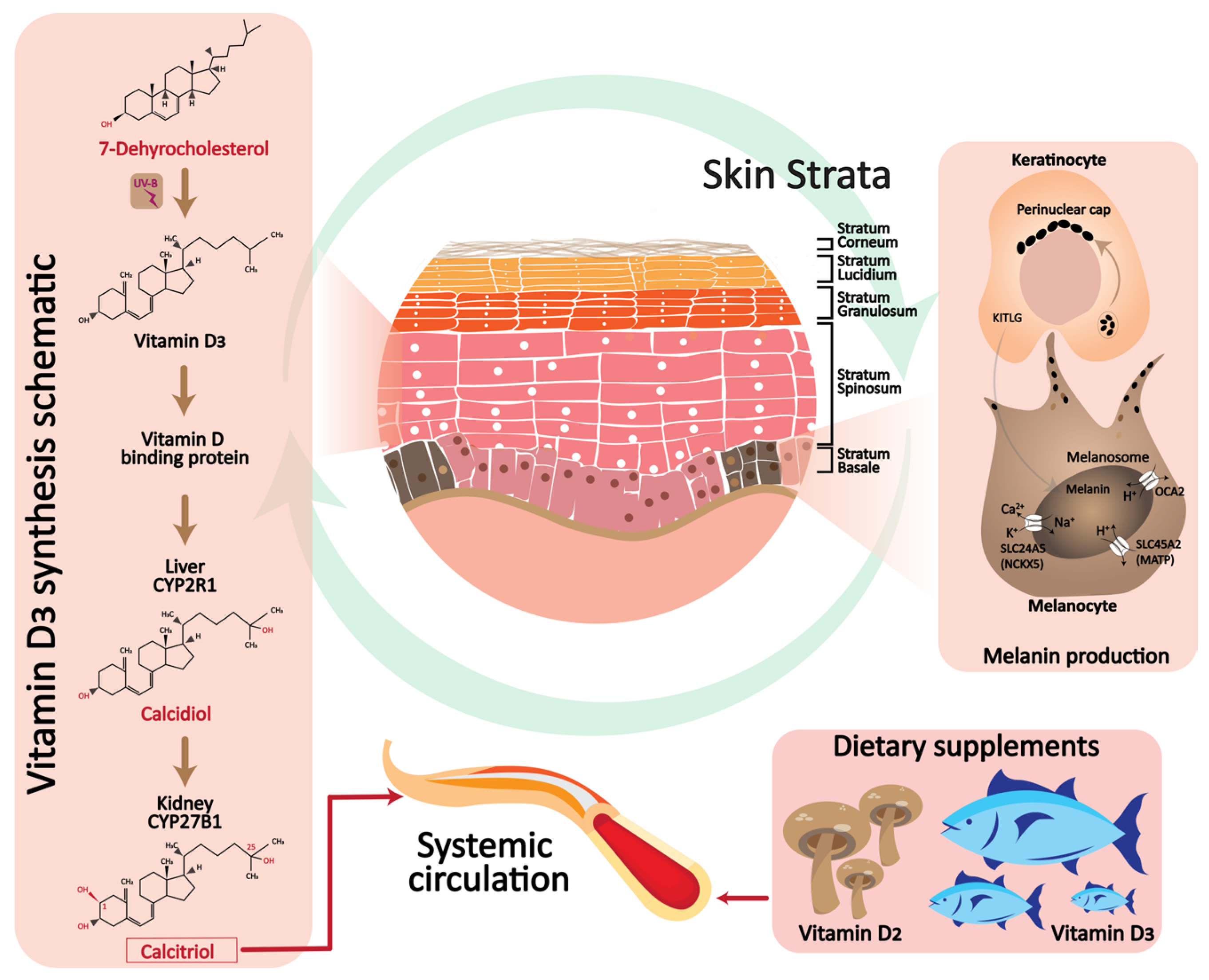
:1. Introduction
2. Melanin and Vitamin D Relation
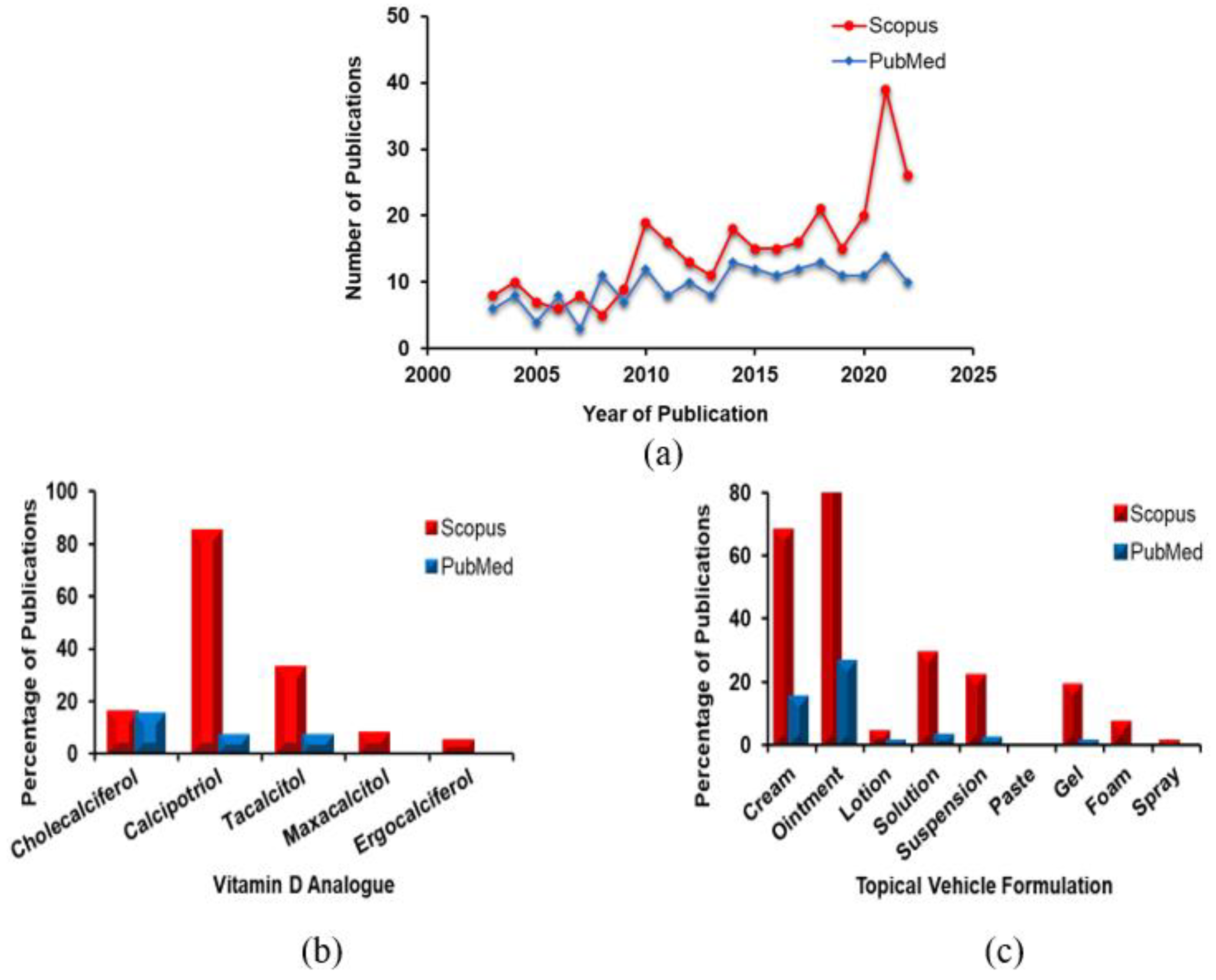
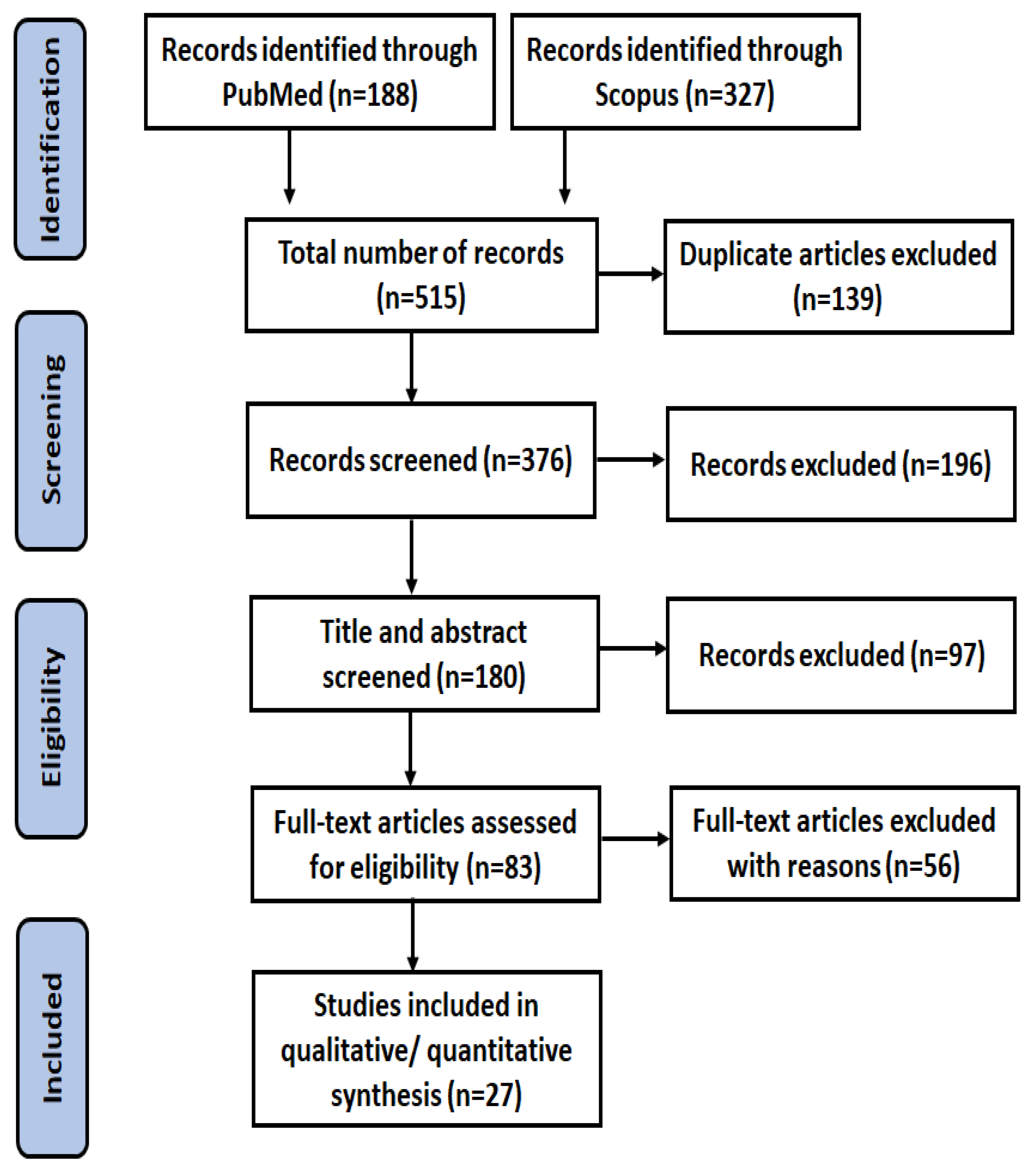
3. Methods
3.1. Search Strategy
3.2. Study Screening and Data Extraction
3.3. Inclusion and Exclusion Criteria
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Norman, A. Vitamin D; Elsevier: Amsterdam, The Netherlands, 2012; pp. 1–101. [Google Scholar]
- Agostini, D.; Donati Zeppa, S. Vitamin D, Diet and Musculoskeletal Health. Nutrients 2023, 15, 2902. [Google Scholar] [CrossRef]
- Mostafa, W.Z.; Hegazy, R.A. Vitamin D and the skin: Focus on a complex relationship: A review. J. Adv. Res. 2015, 6, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Illescas-Montes, R.; Melguizo-Rodríguez, L.; Ruiz, C.; Costela-Ruiz, V.J. Vitamin D and autoimmune diseases. Life Sci. 2019, 233, 116744. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F.; Chen, T.C. Vitamin D deficiency: A worldwide problem with health consequences. Am. J. Clin. Nutr. 2008, 87, 1080S–1086S. [Google Scholar] [CrossRef] [PubMed]
- Charoenngam, N.; Shirvani, A.; Holick, M.F. Vitamin D for skeletal and non-skeletal health: What we should know. J. Clin. Orthop. Trauma 2019, 10, 1082–1093. [Google Scholar] [CrossRef] [PubMed]
- Narvaez, J.; Maldonado, G.; Guerrero, R.; Messina, O.D.; Rios, C. Vitamin D megadose: Definition, efficacy in bone metabolism, risk of falls and fractures. Open Access Rheumatol. Res. Rev. 2020, 12, 105–115. [Google Scholar] [CrossRef]
- Sawarkar, S.; Ashtekar, A. Transdermal vitamin D supplementation—A potential vitamin D deficiency treatment. J. Cosmet. Dermatol. 2020, 19, 28–32. [Google Scholar] [CrossRef]
- Alsaqr, A.; Rasoully, M.; Musteata, F.M. Investigating transdermal delivery of vitamin D3. AAPS PharmSciTech 2015, 16, 963–972. [Google Scholar] [CrossRef]
- Yamagishi, N.; Namioka, T.; Okura, N.; Sato, S.; Kim, D.; Furuhama, K.; Naito, Y. Application of a reservoir-type calcitriol transdermal patch in dairy cattle. J. Vet. Med. Sci. 2009, 71, 845–848. [Google Scholar] [CrossRef]
- Wang, Z.; Ding, R.; Wang, J. The association between vitamin D status and autism spectrum disorder (ASD): A systematic review and meta-analysis. Nutrients 2020, 13, 86. [Google Scholar] [CrossRef]
- Al-smadi, K.; Imran, M.; Leite-Silva, V.R.; Mohammed, Y. Vitiligo: A Review of Aetiology, Pathogenesis, Treatment, and Psychosocial Impact. Cosmetics 2023, 10, 84. [Google Scholar] [CrossRef]
- Sharquie, K.E.; Sharquie, I.K.; Al Hamza, A.N. Psoriasis, pityriasis alba, and vitiligo (PPV) are a triad of one disease: New observation. Our Dermatol. Online/Nasza Dermatol. Online 2021, 12, 314–323. [Google Scholar]
- AlGhamdi, K.; Kumar, A.; Moussa, N. The role of vitamin D in melanogenesis with an emphasis on vitiligo. Indian J. Dermatol. Venereol. Leprol. 2013, 79, 750. [Google Scholar] [CrossRef] [PubMed]
- Okoro, U.; Usatine, R.P.; Heath, C.R. DX across the Skin Color Spectrum; Quadrant Healthcom Inc.: Parsippany, NJ, USA, 2023; Volume 111, pp. 106–107. [Google Scholar]
- Wolff, K.; Goldsmith, L.A.; Katz, S.I.; Gilchrest, B.A.; Paller, A.S.; Leffell, D.J. Fitzpatrick’s Dermatology in General Medicine; McGraw-Hill: New York, NY, USA, 2008. [Google Scholar]
- Ortonne, J.-P.; Passeron, T. Vitiligo and other disorders of hypopigmentation. Dermatology 2008, 1, 4–5. [Google Scholar]
- Boniface, K.; Seneschal, J.; Picardo, M.; Taïeb, A. Vitiligo: Focus on clinical aspects, immunopathogenesis, and therapy. Clin. Rev. Allergy Immunol. 2018, 54, 52–67. [Google Scholar] [CrossRef]
- Saniee, S.; Zare, A.G.; Radmehr, A. Zinc, vitamin D, and TSH levels in patients with vitiligo. Erciyes Med. J. 2019, 41, 148–152. [Google Scholar] [CrossRef]
- Hassan, I.; Bhat, Y.J.; Majid, S.; Sajad, P.; Rasool, F.; Malik, R.A.; Haq, I.U. Association of vitamin D receptor gene polymorphisms and serum 25-hydroxy vitamin D levels in vitiligo–A case-control study. Indian Dermatol. Online J. 2019, 10, 131. [Google Scholar]
- Saputra, M.A.R.; Purwoko, I.H.; Toruan, T.L. The Role of Topical Vitamin D in Vitiligo: A Narrative Literature Review. Biosci. Med. J. Biomed. Transl. Res. 2022, 6, 2516–2526. [Google Scholar]
- Naik, P.P.; Farrukh, S.N. Influence of ethnicities and skin color variations in different populations: A review. Ski. Pharmacol. Physiol. 2022, 35, 65–76. [Google Scholar] [CrossRef]
- Hawker, N.P.; Pennypacker, S.D.; Chang, S.M.; Bikle, D.D. Regulation of human epidermal keratinocyte differentiation by the vitamin D receptor and its coactivators DRIP205, SRC2, and SRC3. J. Investig. Dermatol. 2007, 127, 874–880. [Google Scholar] [CrossRef]
- Birlea, S.A.; Costin, G.E.; Norris, D.A. Cellular and molecular mechanisms involved in the action of vitamin D analogs targeting vitiligo depigmentation. Curr. Drug Targets 2008, 9, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Lotti, T.; Gori, A.; Zanieri, F.; Colucci, R.; Moretti, S. Vitiligo: New and emerging treatments. Dermatol. Ther. 2008, 21, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Travis, L.B.; Silverberg, N.B. Calcipotriene and corticosteroid combination therapy for vitiligo. Pediatr. Dermatol. 2004, 21, 495–498. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, Y.H.; Yamada, M.; Lin, L.L.; Grice, J.E.; Roberts, M.S.; Raphael, A.P.; Benson, H.A.E.; Prow, T.W. Microneedle enhanced delivery of cosmeceutically relevant peptides in human skin. PLoS ONE 2014, 9, e101956. [Google Scholar] [CrossRef]
- Vitamin D–Fact Sheet for Health Professionals. Available online: https://manoxblog.com/2018/05/01/vitamin-d-fact-sheet-for-health-professionals/ (accessed on 21 September 2023).
- Buttriss, J.L.; Lanham-New, S.A. Is a vitamin D fortification strategy needed? Nutr. Bull. 2020, 45, 115. [Google Scholar] [CrossRef]
- Itkonen, S.T.; Andersen, R.; Björk, A.K.; Brugård Konde, Å.; Eneroth, H.; Erkkola, M.; Holvik, K.; Madar, A.A.; Meyer, H.E.; Tetens, I. Vitamin D status and current policies to achieve adequate vitamin D intake in the Nordic countries. Scand. J. Public Health 2021, 49, 616–627. [Google Scholar] [CrossRef]
- Wessels, I.; Rink, L. Micronutrients in autoimmune diseases: Possible therapeutic benefits of zinc and vitamin D. J. Nutr. Biochem. 2020, 77, 108240. [Google Scholar] [CrossRef]
- Murdaca, G.; Greco, M.; Borro, M.; Gangemi, S. Hygiene hypothesis and autoimmune diseases: A narrative review of clinical evidences and mechanisms. Autoimmun. Rev. 2021, 20, 102845. [Google Scholar] [CrossRef]
- Garg, B.J.; Saraswat, A.; Bhatia, A.; Katare, O.P. Topical treatment in vitiligo and the potential uses of new drug delivery systems. Indian J. Dermatol. Venereol. Leprol. 2010, 76, 231. [Google Scholar]
- Bilal, A.; Anwar, I. Guidelines for the management of vitiligo. J. Pak. Assoc. Dermatol. 2014, 24, 68–78. [Google Scholar]
- Bouceiro Mendes, R.; Alpalhão, M.; Filipe, P. UVB phototherapy in the treatment of vitiligo: State of the art and clinical perspectives. Photodermatol. Photoimmunol. Photomed. 2022, 38, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D.D. Vitamin D metabolism, mechanism of action, and clinical applications. Chem. Biol. 2014, 21, 319–329. [Google Scholar] [CrossRef] [PubMed]
- Donnarumma, D.; Arena, A.; Trovato, E.; Rigano, F.; Zoccali, M.; Mondello, L. A miniaturized comprehensive approach for total lipidome analysis and vitamin D metabolite quantification in human serum. Anal. Bioanal. Chem. 2023, 415, 4579–4590. [Google Scholar] [CrossRef] [PubMed]
- Makris, K.; Bhattoa, H.P.; Cavalier, E.; Phinney, K.; Sempos, C.T.; Ulmer, C.Z.; Vasikaran, S.D.; Vesper, H.; Heijboer, A.C. Recommendations on the measurement and the clinical use of vitamin D metabolites and vitamin D binding protein–A position paper from the IFCC Committee on bone metabolism. Clin. Chim. Acta 2021, 517, 171–197. [Google Scholar] [CrossRef]
- Janoušek, J.; Pilařová, V.; Macáková, K.; Nomura, A.; Veiga-Matos, J.; Silva, D.D.d.; Remiao, F.; Saso, L.; Malá-Ládová, K.; Malý, J. Vitamin D: Sources, physiological role, biokinetics, deficiency, therapeutic use, toxicity, and overview of analytical methods for detection of vitamin D and its metabolites. Crit. Rev. Clin. Lab. Sci. 2022, 59, 517–554. [Google Scholar] [CrossRef] [PubMed]
- Joseph, M. Vitamin D2 vs. D3: An Evidence-Based Comparison. Available online: https://www.nutritionadvance.com/vitamin-d2-vs-d3/ (accessed on 29 December 2020).
- Shieh, A.; Chun, R.F.; Ma, C.; Witzel, S.; Meyer, B.; Rafison, B.; Swinkels, L.; Huijs, T.; Pepkowitz, S.; Holmquist, B. Effects of high-dose vitamin D2 versus D3 on total and free 25-hydroxyvitamin D and markers of calcium balance. J. Clin. Endocrinol. Metab. 2016, 101, 3070–3078. [Google Scholar] [CrossRef] [PubMed]
- Olmos-Ortiz, A.; Avila, E.; Durand-Carbajal, M.; Díaz, L. Regulation of calcitriol biosynthesis and activity: Focus on gestational vitamin D deficiency and adverse pregnancy outcomes. Nutrients 2015, 7, 443–480. [Google Scholar] [CrossRef] [PubMed]
- Brożyna, A.A.; Slominski, R.M.; Nedoszytko, B.; Zmijewski, M.A.; Slominski, A.T. Vitamin D signaling in psoriasis: Pathogenesis and therapy. Int. J. Mol. Sci. 2022, 23, 8575. [Google Scholar] [CrossRef]
- Wat, H.; Dytoc, M. Off-label uses of topical vitamin D in dermatology: A systematic review. J. Cutan. Med. Surg. 2014, 18, 91–108. [Google Scholar] [CrossRef] [PubMed]
- De Rie, M.A.; De Hoop, D.; Jönsson, L.; Bakkers, E.J.M.; Sørensen, M. Pharmacoeconomic evaluation of calcipotriol (Daivonex®/Dovonex®) and UVB phototherapy in the treatment of psoriasis: A Markov model for the Netherlands. Dermatology 2001, 202, 38–43. [Google Scholar] [CrossRef]
- Yalçin, B.; Şahin, S.; Bükülmez, G.; Karaduman, A.; Atakan, N.; Akan, T.; Kölemen, F. Experience with calcipotriol as adjunctive treatment for vitiligo in patients who do not respond to PUVA alone: A preliminary study. J. Am. Acad. Dermatol. 2001, 44, 634–637. [Google Scholar] [CrossRef] [PubMed]
- Baysal, V.; Yildirim, M.; Erel, A.; Kesici, D. Is the combination of calcipotriol and PUVA effective in vitiligo? J. Eur. Acad. Dermatol. Venereol. 2003, 17, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Glowka, E.; Stasiak, J.; Lulek, J. Drug delivery systems for vitamin D supplementation and therapy. Pharmaceutics 2019, 11, 347. [Google Scholar] [CrossRef] [PubMed]
- Dua, I.; Aggarwal, K.; Jain, V.K. Comparative evaluation of efficacy and safety of calcipotriol versus tacalcitol ointment, both in combination with NBUVB phototherapy in the treatment of stable plaque psoriasis. Photodermatol. Photoimmunol. Photomed. 2017, 33, 275–281. [Google Scholar] [CrossRef]
- Nagpal, S.; Lu, J.; Boehm, M.F. Vitamin D analogs: Mechanism of action and therapeutic applications. Curr. Med. Chem. 2001, 8, 1661–1679. [Google Scholar] [CrossRef]
- Trémezaygues, L.; Reichrath, J. Vitamin D analogs in the treatment of psoriasis: Where are we standing and where will we be going? Derm. Endocrinol. 2011, 3, 180–186. [Google Scholar] [CrossRef]
- Tapfumaneyi, P.; Imran, M.; Alavi, S.E.; Mohammed, Y. Science of, and insights into, thermodynamic principles for dermal formulations. Drug Discov. Today 2023, 6, 103521. [Google Scholar] [CrossRef]
- Yousef, S.A.; Mohammed, Y.H.; Namjoshi, S.; Grice, J.E.; Benson, H.A.E.; Sakran, W.; Roberts, M.S. Mechanistic evaluation of enhanced curcumin delivery through human skin in vitro from optimised nanoemulsion formulations fabricated with different penetration enhancers. Pharmaceutics 2019, 11, 639. [Google Scholar] [CrossRef]
- Leite-Silva, V.R.; Grice, J.E.; Mohammed, Y.; Moghimi, H.R.; Roberts, M.S. The Influence of emollients on dermal and transdermal drug delivery. In Percutaneous Penetration Enhancers Drug Penetration into/through the Skin: Methodology and General Considerations; Springer: Berlin/Heidelberg, Germany, 2017; pp. 77–93. [Google Scholar]
- Prausnitz, M.R.; Langer, R. Transdermal drug delivery. Nat. Biotechnol. 2008, 26, 1261–1268. [Google Scholar] [CrossRef]
- Kalluri, H.; Banga, A.K. Transdermal delivery of proteins. Aaps Pharmscitech 2011, 12, 431–441. [Google Scholar] [CrossRef]
- Jin, X.; Imran, M.; Mohammed, Y. Topical Semisolid Products—Understanding the Impact of Metamorphosis on Skin Penetration and Physicochemical Properties. Pharmaceutics 2022, 14, 2487. [Google Scholar] [CrossRef] [PubMed]
- Boshrouyeh, R.; Amari, S.; Boshrouyeh Ghandashtani, M.; Alavi, S.E.; Ebrahimi Shahmabadi, H. A topical gel nanoformulation of amphotericin B (AmB) for the treatment of cutaneous leishmaniasis (CL). J. Sol-Gel Sci. Technol. 2023, 105, 768–780. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.G.; Gkiouras, K.; Nigdelis, M.P.; Bogdanos, D.P.; Goulis, D.G. Efficacy of vitamin D3 buccal spray supplementation compared to other delivery methods: A systematic review of superiority randomized controlled trials. Nutrients 2020, 12, 691. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Alavi, S.E.; Shafiee, A.; Leite-Silva, V.R.; Khosrotehrani, K.; Mohammed, Y. Metamorphosis of Topical Semisolid Products—Understanding the Role of Rheological Properties in Drug Permeation under the “in Use” Condition. Pharmaceutics 2023, 15, 1707. [Google Scholar] [CrossRef]
- Adepu, S.; Ramakrishna, S. Controlled drug delivery systems: Current status and future directions. Molecules 2021, 26, 5905. [Google Scholar] [CrossRef]
- Kompella, U.B.; Lee, V.H.L. Delivery systems for penetration enhancement of peptide and protein drugs: Design considerations. Adv. Drug Deliv. Rev. 2001, 46, 211–245. [Google Scholar] [CrossRef]
- Parish, J.L. Topical vitamin D3 analogues: Unapproved uses, dosages, or indications. Clin. Dermatol. 2002, 20, 558–562. [Google Scholar] [CrossRef]
- Akgül, Z. Biological properties of vitamin D and its effect on the pathogenesis of periodontal. In Theory and Research in Health Sciences; Serüven Publishing: Güzelbahçe, Turkey, 2022. [Google Scholar]
- Hanel, A.; Carlberg, C. Vitamin D and evolution: Pharmacologic implications. Biochem. Pharmacol. 2020, 173, 113595. [Google Scholar] [CrossRef]
- Wan, M. What Dose of Vitamin D Is Required to Achieve Target Serum 25-Hydroxyvitamin D Levels in Children? Ph.D. Thesis, King’s College London, London, UK, 2021. [Google Scholar]
- Chen, T.C.; Lu, Z.; Holick, M.F. Photobiology of vitamin D. In Vitamin D: Physiology, Molecular Biology, and Clinical Applications; Springer Science & Business Media: Berlin, Germany, 2010; pp. 35–60. [Google Scholar]
- Milliken, S.V.I.; Wassall, H.; Lewis, B.J.; Logie, J.; Barker, R.N.; Macdonald, H.; Vickers, M.A.; Ormerod, A.D. Effects of ultraviolet light on human serum 25-hydroxyvitamin D and systemic immune function. J. Allergy Clin. Immunol. 2012, 129, 1554–1561. [Google Scholar] [CrossRef]
- Cichorek, M.; Wachulska, M.; Stasiewicz, A.; Tymińska, A. Skin melanocytes: Biology and development. Adv. Dermatol. Allergol. 2013, 30, 30–41. [Google Scholar] [CrossRef]
- Yousef, H.; Alhajj, M.; Sharma, S. Anatomy, Skin (Integument), Epidermis; StatPearls Publishing: Treasure Island, FL, USA, 2017. [Google Scholar]
- Costin, G.-E.; Hearing, V.J. Human skin pigmentation: Melanocytes modulate skin color in response to stress. FASEB J. 2007, 21, 976–994. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, B.; Chauhan, D.; Singh, A.K.; Chatterjee, M. Melanin based classification of skin types and their susceptibility to UV-induced cancer. In Skin Cancer: Pathogenesis and Diagnosis; Springer: Singapore, 2021; pp. 41–67. [Google Scholar]
- Karagün, E.; Ergin, C.; Baysak, S.; Erden, G.; Aktaş, H.; Ekiz, Ö. The role of serum Vitamin D levels in vitiligo. Postep. Dermatol. Alergol. 2016, 33, 300–302. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Jin, X.; Ali, M.; Tapfumaneyi, P.; Lelasseur, P.; Carlo, L.; Jude, A.; Bourg, A.L.; Panchal, B.; Dick, A. The Pandemic and Your Skin—Direct and Indirect Impact of COVID-19. Cosmetics 2023, 10, 34. [Google Scholar] [CrossRef]
- Goktas, E.O.; Aydin, F.; Senturk, N.; Canturk, M.T.; Turanli, A.Y. Combination of narrow band UVB and topical calcipotriol for the treatment of vitiligo. J. Eur. Acad. Dermatol. Venereol. 2006, 20, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Forschner, T.; Buchholtz, S.; Stockfleth, E. Current state of vitiligo therapy–evidence-based analysis of the literature. JDDG J. Der Dtsch. Dermatol. Ges. 2007, 5, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wan, Y.; Lin, Y.; Jiang, H. Current art of combination therapy with autologous platelet-rich plasma for stable vitiligo: A meta-analysis. Int. Wound J. 2021, 18, 251–260. [Google Scholar] [CrossRef] [PubMed]
- Abdel Latif, A.A.; Ibrahim, S.M. Monochromatic excimer light versus combination of topical steroid with vitamin D3 analogue in the treatment of nonsegmental vitiligo: A randomized blinded comparative study. Dermatol. Ther. 2015, 28, 383–389. [Google Scholar] [CrossRef]
- Ada, S.; Sahin, S.; Boztepe, G.; Karaduman, A.; Kölemen, F. No additional effect of topical calcipotriol on narrow-band UVB phototherapy in patients with generalized vitiligo. Photodermatol. Photoimmunol. Photomed. 2005, 21, 79–83. [Google Scholar] [CrossRef]
- Akdeniz, N.; Yavuz, I.H.; Gunes Bilgili, S.; Ozaydın Yavuz, G.; Calka, O. Comparison of efficacy of narrow band UVB therapies with UVB alone, in combination with calcipotriol, and with betamethasone and calcipotriol in vitiligo. J. Dermatol. Treat. 2014, 25, 196–199. [Google Scholar] [CrossRef]
- Arca, E.; Taştan, H.B.; Erbil, A.H.; Sezer, E.; Koç, E.; Kurumlu, Z. Narrow-band ultraviolet B as monotherapy and in combination with topical calcipotriol in the treatment of vitiligo. J. Dermatol. 2006, 33, 338–343. [Google Scholar] [CrossRef]
- Bakr, R.M.; Abdel-Gaber, R.M.; Tawfik, Y.M. A comparative study on the use of fractional CO2 laser with tacrolimus or calcipotriol or narrow band ultraviolet-B in treatment of stable nonsegmental vitiligo. Dermatol. Ther. 2021, 34, e14604. [Google Scholar] [CrossRef]
- Cherif, F.; Azaiz, M.I.; Ben Hamida, A.; Ben, O.; Dhari, A. Calcipotriol and PUVA as treatment for vitiligo. Dermatol. Online J. 2003, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Gargoom, A.M.; Duweb, G.A.; Elzorghany, A.H.; Benghazil, M.; Bugrein, O.O. Calcipotriol in the treatment of childhood vitiligo. Int. J. Clin. Pharmacol. Res. 2004, 24, 11–14. [Google Scholar]
- Goldinger, S.M.; Dummer, R.; Schmid, P.; Burg, G.; Seifert, B.; Läuchli, S. Combination of 308-nm xenon chloride excimer laser and topical calcipotriol in vitiligo. J. Eur. Acad. Dermatol. Venereol. 2007, 21, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, A.; Lurz, C.; Hamm, H.; Bröcker, E.B.; Hofmann, U.B. Narrow-band UVB311 nm vs. broad-band UVB therapy in combination with topical calcipotriol vs. placebo in vitiligo. Int. J. Dermatol. 2005, 44, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, Z.A.; Hassan, G.F.; Elgendy, H.Y.; Al-Shenawy, H.A. Evaluation of the efficacy of transdermal drug delivery of calcipotriol plus betamethasone versus tacrolimus in the treatment of vitiligo. J. Cosmet. Dermatol. 2019, 18, 581–588. [Google Scholar] [CrossRef]
- Juntongjin, P.; Sangganjanavanich, P. Efficacy of the combined excimer light and topical calcipotriol for acral vitiligo: A randomized double-blind comparative study. Dermatol. Ther. 2021, 34, e14886. [Google Scholar] [CrossRef]
- Katayama, I.; Ashida, M.; Maeda, A.; Eishi, K.; Murota, H.; Bae, S.J. Open trial of topical tacalcitol [1 alpha 24(OH)2D3] and solar irradiation for vitiligo vulgaris: Upregulation of c-Kit mRNA by cultured melanocytes. Eur. J. Dermatol. 2003, 13, 372–376. [Google Scholar]
- Khullar, G.; Kanwar, A.J.; Singh, S.; Parsad, D. Comparison of efficacy and safety profile of topical calcipotriol ointment in combination with NB-UVB vs. NB-UVB alone in the treatment of vitiligo: A 24-week prospective right-left comparative clinical trial. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 925–932. [Google Scholar] [CrossRef]
- Kullavanijaya, P.; Lim, H.W. Topical calcipotriene and narrowband ultraviolet B in the treatment of vitiligo. Photodermatol. Photoimmunol. Photomed. 2004, 20, 248–251. [Google Scholar] [CrossRef]
- Kumaran, M.S.; Kaur, I.; Kumar, B. Effect of topical calcipotriol, betamethasone dipropionate and their combination in the treatment of localized vitiligo. J. Eur. Acad. Dermatol. Venereol. 2006, 20, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Leone, G.; Pacifico, A.; Iacovelli, P.; Paro Vidolin, A.; Picardo, M. Tacalcitol and narrow-band phototherapy in patients with vitiligo. Clin. Exp. Dermatol. 2006, 31, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Lotti, T.; Buggiani, G.; Troiano, M.; Assad, G.B.; Delescluse, J.; De Giorgi, V.; Hercogova, J. Targeted and combination treatments for vitiligo. Comparative evaluation of different current modalities in 458 subjects. Dermatol. Ther. 2008, 21 (Suppl. S1), S20–S26. [Google Scholar] [CrossRef] [PubMed]
- Lu-Yan, T.; Wen-Wen, F.; Lei-Hong, X.; Yi, J.; Zhi-Zhong, Z. Topical tacalcitol and 308-nm monochromatic excimer light: A synergistic combination for the treatment of vitiligo. Photodermatol. Photoimmunol. Photomed. 2006, 22, 310–314. [Google Scholar] [CrossRef]
- Oh, S.H.; Kim, T.; Jee, H.; Do, J.E.; Lee, J.H. Combination treatment of non-segmental vitiligo with a 308-nm xenon chloride excimer laser and topical high-concentration tacalcitol: A prospective, single-blinded, paired, comparative study. J. Am. Acad. Dermatol. 2011, 65, 428–430. [Google Scholar] [CrossRef]
- Onita, A. New aspects on vitamin D3 ointment: Vitamin D3 therapy for vitiligo. Clin. Calcium 2004, 14, 137–140. [Google Scholar]
- Rodríguez-Martín, M.; García Bustínduy, M.; Sáez Rodríguez, M.; Noda Cabrera, A. Randomized, double-blind clinical trial to evaluate the efficacy of topical tacalcitol and sunlight exposure in the treatment of adult nonsegmental vitiligo. Br. J. Dermatol. 2009, 160, 409–414. [Google Scholar] [CrossRef]
- Sahu, P.; Jain, V.K.; Aggarwal, K.; Kaur, S.; Dayal, S. Tacalcitol: A useful adjunct to narrow-band ultraviolet-B phototherapy in vitiligo. Photodermatol. Photoimmunol. Photomed. 2016, 32, 262–268. [Google Scholar] [CrossRef]
- Salem, M.W.; Adel Abd El Azim, A.; Galal, S.A. Efficacy of topical vitamin D combined with microneedling in the treatment of vitiligo: A comparative study. J. Cosmet. Dermatol. 2023, 22, 1521–1527. [Google Scholar] [CrossRef]
- Vázquez-López, F.; López-Escobar, M.; Pérez-Oliva, N. Calcipotriene and Vitiligo. Arch. Dermatol. 2003, 139, 1656–1657. [Google Scholar] [CrossRef]
- Xing, C.; Xu, A. The effect of combined calcipotriol and betamethasone dipropionate ointment in the treatment of vitiligo: An open, uncontrolled trial. J. Drugs Dermatol. 2012, 11, e52–e54. [Google Scholar] [PubMed]
- Parsad, D.; Saini, R.; Verma, N. Combination of PUVAsol and topical calcipotriol in vitiligo. Dermatology 1998, 197, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Rütter, A.; Schwarz, T. Market hyperpigmentation in psoriatic plaque as a sequelae of combination therapy with UVB-311 and calcipotriol. In Der Hautarzt; Zeitschrift fur Dermatologie, Venerologie, und Verwandte Gebiete; Springer: Berlin/Heidelberg, Germany, 2000; Volume 51, pp. 431–433. [Google Scholar] [CrossRef]
- Schiener, R.; Behrens-Williams, S.C.; Pillekamp, H.; Kaskel, P.; Peter, R.U.; Kerscher, M. Calcipotriol vs. tazarotene as combination therapy with narrowband ultraviolet B (311 nm): Efficacy in patients with severe psoriasis. Br. J. Dermatol. 2000, 143, 1275–1278. [Google Scholar] [CrossRef] [PubMed]
- Pacifico, A.; Leone, G. Photo(chemo)therapy for vitiligo. Photodermatol. Photoimmunol. Photomed. 2011, 27, 261–277. [Google Scholar] [CrossRef]
- Novák, Z.; Bónis, B.; Baltás, E.; Ocsovszki, I.; Ignácz, F.; Dobozy, A.; Kemény, L. Xenon chloride ultraviolet B laser is more effective in treating psoriasis and in inducing T cell apoptosis than narrow-band ultraviolet B. J. Photochem. Photobiol. B Biol. 2002, 67, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Manstein, D.; Herron, G.S.; Sink, R.K.; Tanner, H.; Anderson, R.R. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg. Med. Off. J. Am. Soc. Laser Med. Surg. 2004, 34, 426–438. [Google Scholar] [CrossRef] [PubMed]
- Bogdan Allemann, I.; Kaufman, J. Fractional photothermolysis—An update. Lasers Med. Sci. 2010, 25, 137–144. [Google Scholar] [CrossRef]
- Lu, G.W.; Gao, P. Emulsions and microemulsions for topical and transdermal drug delivery. In Handbook of Non-Invasive Drug Delivery Systems; Elsevier: Amsterdam, The Netherlands, 2010; pp. 59–94. [Google Scholar] [CrossRef]
- Karadzovska, D.; Brooks, J.D.; Monteiro-Riviere, N.A.; Riviere, J.E. Predicting skin permeability from complex vehicles. Adv. Drug Deliv. Rev. 2013, 65, 265–277. [Google Scholar] [CrossRef]
- Kim, B.; Cho, H.-E.; Moon, S.H.; Ahn, H.-J.; Bae, S.; Cho, H.-D.; An, S. Transdermal delivery systems in cosmetics. Biomed. Dermatol. 2020, 4, 1–12. [Google Scholar] [CrossRef]
- Haque, T.; Talukder, M.M.U. Chemical enhancer: A simplistic way to modulate barrier function of the stratum corneum. Adv. Pharm. Bull. 2018, 8, 169. [Google Scholar] [CrossRef]
- Manconi, M.; Caddeo, C.; Sinico, C.; Valenti, D.; Mostallino, M.C.; Lampis, S.; Monduzzi, M.; Fadda, A.M. Penetration enhancer-containing vesicles: Composition dependence of structural features and skin penetration ability. Eur. J. Pharm. Biopharm. 2012, 82, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Yao, Z.; Wang, Y.; Chai, L.; Zhou, X. Vitamin D analogs combined with different types of phototherapy in the treatment of vitiligo: A systematic review of randomized trials and within-patient studies. Int. Immunopharmacol. 2022, 109, 108789. [Google Scholar] [CrossRef] [PubMed]
| Source | Study Design | Types of Vitiligo | No. of Patients | Subtype | Treatment Duration | Intervention | Fitzpatrick Skin Type | Types of Topical Vit-D | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Abdel 2015 [78] | Randomized blinded comparative study | Non-segmental | 44 | Localized and stable | 3 months |
| NR | Ointment |
|
| Ada 2005 [79] | Right-left comparison prospective single-blinded study | Non-segmental | 20 | Generalized vitiligo | 12 months |
| NR | Cream |
|
| Akdeniz [80] 2014 | Randomized double-blind comparative study | Non-segmental | 45 | NR | 6 months |
| NR | Ointment |
|
| Arca 2006 [81] | Comparative prospective study | Non-segmental | 40 | Stable | 4 months |
| NR | Ointment |
|
| Bakr 2021 [82] | Prospective randomized comparative study | Non-segmental | 30 | Stable | 3 months |
| NR | Ointment |
|
| Baysal 2003 [47] | Prospective right/left comparative, open study | Non-segmental | 22 | Generalized | 9 months |
| NR | Cream |
|
| Cherif 2003 [83] | Prospective study | Non-segmental | 23 | Bilateral symmetrical | 15 weeks |
| IV, V | Ointment |
|
| Gargoom 2004 [84] | Prospective right/left comparison study | Segmental and non-segmental | 18 | Focal/mucosal | 4–6 months |
| NR | Cream/Ointment |
|
| Goktas 2006 [75] | Prospective right/left comparison study | Non-segmental | 24 | Generalized | 6 months |
| II, III | Cream |
|
| Goldinger 2007 [85] | Prospective right/left comparative single-blinded trial | Non-segmental | 10 | Bilateral symmetrical | 15 months |
| II, III, IV | Ointment |
|
| Hartmann 2005 [86] | Prospective right/left comparative study | Non-segmental | 10 | Symmetrical (vulgaris/acrofacial /localized) | 12 months |
| II, III | Ointment |
|
| Ibrahim 2019 [87] | Prospective right/left comparative study | Segmental and non-segmental | 25 | Stable and symmetrical, focal and generalized | 6 months |
| III, IV | Ointment | 60% showed excellent improvement for the calcipotriol combination compared to 32% for tacrolimus |
| Juntongjin 2021 [88] | Prospective randomized double-blind comparative study | Non-segmental | 13 | Acral vitiligo | 24 weeks |
| IV | Ointment |
|
| Katayama 2003 [89] | Prospective uncontrolled open trial | Segmental and non-segmental | 15 | Vulgaris vitiligo | 3 months |
| NR | Ointment | 40% of patients responded in a good to excellent way clinically |
| Khullar 2015 [90] | Prospective right-left comparative study | Non-segmental | 27 | Generalized vitiligo (vulgaris and acrofacial | 24 weeks |
| III, IV, V | Ointment | 51.4% reduction in the lesions for NB and 49% for combination (good repigmentation) |
| Kullavanija-ya 2004 [91] | Prospective open bilateral comparison study | Non-segmental | 20 | Symmetrical vitiligo | 15 months |
| NR | Ointment |
|
| Kumaran 2006 [92] | Randomized trial | Non-segmental | 49 | Localized vitiligo | 3 months |
| NR | Ointment |
|
| Leone 2006 [93] | Prospective randomized open-label study | Non-segmental | 32 | Generalized and symmetrical | 12 months |
| II, III, IV | Ointment |
|
| Lotti 2008 [94] | Prospective open study | Segmental and non-segmental | 470 | Vulgaris vitiligo | 6 months |
| I, II, III, IV | Ointment |
|
| Lu-Yan 2006 [95] | Randomized single-blind within a patient-controlled trial | Segmental and non-segmental | 38 | Symmetrical, localized, vulgaris | 8 weeks |
| NR | Cream | 25.7% excellent repigmentation in the combination (early pigmentation with lower total dosage) to 5.7% for excimer monotherapy |
| Oh 2011 [96] | Prospective randomized single-blinded paired comparative study | Non-segmental | 20 | Localized | 16 weeks |
| NR | Ointment |
|
| Onita 2004 [97] | Prospective open trial | Segmental and non-segmental | 27 | Vulgaris vitiligo | NR |
| NR | Ointment | 48% of patients improved > 30%(moderate) |
| Rodriguez 2009 [98] | Randomized double-blind placebo-controlled study | Non-segmental | 80 | NR | 4 months |
| NR | Ointment | There was no reduction of the size of the lesion < 25% (poor repigmentation) |
| Sahu 2016 [99] | Prospective open label right/left intraindividual trial | Non-segmental | 30 | Symmetrical vitiligo | 24 weeks |
| NR | Ointment | 16.6% had moderate. 53.3% good 30% excellent repigmentation at the end of therapy |
| Salem 2023 [100] | Prospective comparative study | Segmental and non-segmental | 25 | Stable vitiligo | 19 months |
| II, III, IV | Solution | 52% excellent to good response in the combination |
| Vazquez 2003 [101] | Prospective open pilot study | Non-segmental | 10 | NR | NR |
| NR | Ointment |
|
| Xing 2012 [102] | Prospective open uncontrolled trial | Segmental and non-segmental | 31 | Focal or generalized | 12 weeks |
| NR | Ointment |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Smadi, K.; Ali, M.; Alavi, S.E.; Jin, X.; Imran, M.; Leite-Silva, V.R.; Mohammed, Y. Using a Topical Formulation of Vitamin D for the Treatment of Vitiligo: A Systematic Review. Cells 2023, 12, 2387. https://doi.org/10.3390/cells12192387
Al-Smadi K, Ali M, Alavi SE, Jin X, Imran M, Leite-Silva VR, Mohammed Y. Using a Topical Formulation of Vitamin D for the Treatment of Vitiligo: A Systematic Review. Cells. 2023; 12(19):2387. https://doi.org/10.3390/cells12192387
Chicago/Turabian StyleAl-Smadi, Khadeejeh, Masood Ali, Seyed Ebrahim Alavi, Xuping Jin, Mohammad Imran, Vania R. Leite-Silva, and Yousuf Mohammed. 2023. "Using a Topical Formulation of Vitamin D for the Treatment of Vitiligo: A Systematic Review" Cells 12, no. 19: 2387. https://doi.org/10.3390/cells12192387
APA StyleAl-Smadi, K., Ali, M., Alavi, S. E., Jin, X., Imran, M., Leite-Silva, V. R., & Mohammed, Y. (2023). Using a Topical Formulation of Vitamin D for the Treatment of Vitiligo: A Systematic Review. Cells, 12(19), 2387. https://doi.org/10.3390/cells12192387








