Decellularization of Dense Regular Connective Tissue—Cellular and Molecular Modification with Applications in Regenerative Medicine
Abstract
1. Introduction
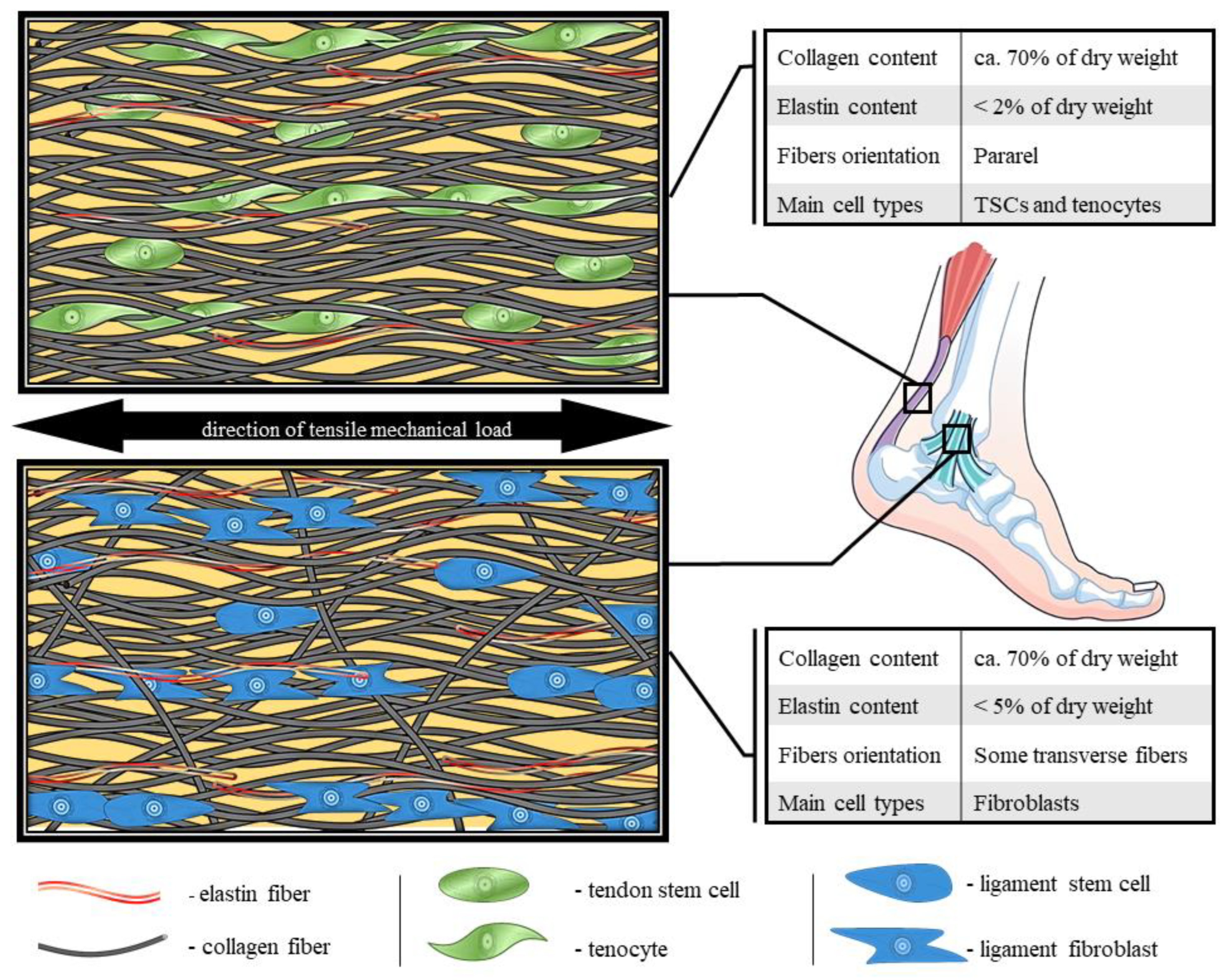
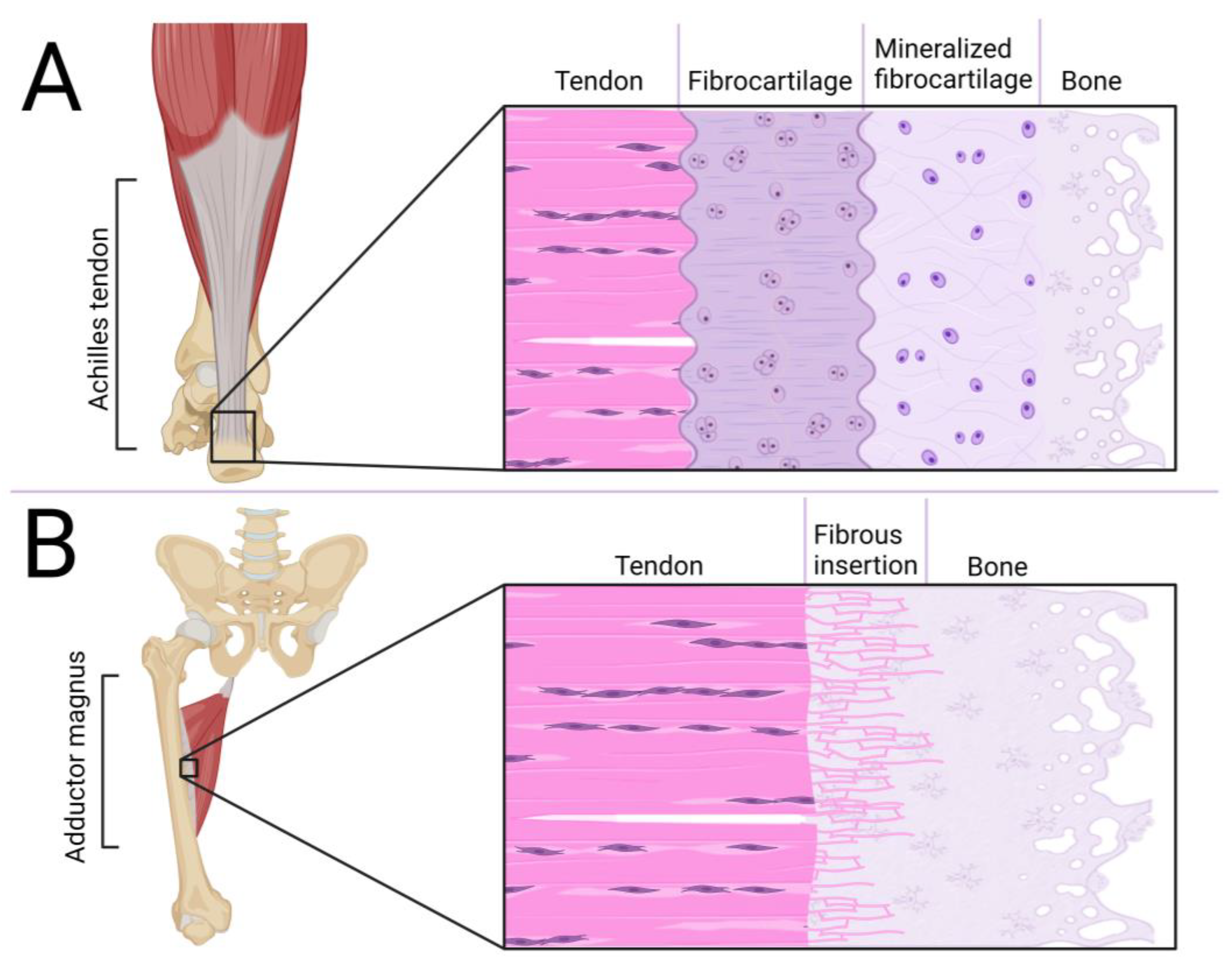
2. Essential Morphological and Molecular Features of Dense Regular Connective Tissue (DRCT)
3. Decellularization Methods
3.1. Physical Methods
3.1.1. Electroporation
3.1.2. Sonication
3.1.3. Freeze–Thaw
3.1.4. High Hydrostatic Pressure
3.2. Chemical Methods
3.2.1. Triton-X 100
3.2.2. Sodium Dodecyl Sulfate (SDS)
3.2.3. Sodium Azide
3.2.4. Latrunculin B
3.2.5. EDTA
3.2.6. Trypsin
3.2.7. Nucleases
4. Modifications of dECM Scaffolds
4.1. Cell Seeding
4.2. Native Structure
4.3. Structure Modifications
4.4. 3D Bioprinting
4.5. Enrichment of the Scaffold Composition
5. Therapeutic Potential—Current Preclinical Success
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Harvey, T.; Flamenco, S.; Fan, C.-M. A Tppp3+Pdgfra+ tendon stem cell population contributes to regeneration and reveals a shared role for PDGF signalling in regeneration and fibrosis. Nat. Cell Biol. 2019, 21, 1490–1503. [Google Scholar] [CrossRef] [PubMed]
- McAuley, S.; Dobbin, N.; Morgan, C.; Goodwin, P.C. Predictors of time to return to play and re-injury following hamstring injury with and without intramuscular tendon involvement in adult professional footballers: A retrospective cohort study. J. Sci. Med. Sport 2022, 25, 216–221. [Google Scholar] [CrossRef]
- Korntner, S.; Lehner, C.; Gehwolf, R.; Wagner, A.; Grütz, M.; Kunkel, N.; Tempfer, H.; Traweger, A. Limiting angiogenesis to modulate scar formation. Adv. Drug Deliv. Rev. 2019, 146, 170–189. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, J.E.; Best, K.T.; Muscat, S.N.; Loiselle, A.E. Metabolic regulation of tendon inflammation and healing following injury. Curr. Rheumatol. Rep. 2021, 23, 15. [Google Scholar] [CrossRef] [PubMed]
- Teh, T.K.H.; Goh, J.C.H. Tissue Engineering Approaches to Regeneration of Anterior Cruciate Ligament. In Comprehensive Biomaterials II; Ducheyne, P., Ed.; Elsevier: Oxford, UK, 2017; pp. 194–215. ISBN 978-0-08-100692-4. [Google Scholar]
- Vidal, A.F.; Joyce, C.D.; Mayo, M. Anterior Cruciate Ligament Graft Choices in the Female Athlete. In ACL Injuries in Female Athletes; West, R., Bryant, B., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 31–36. ISBN 978-0-323-54839-7. [Google Scholar]
- Henriksen, N.A.; Montgomery, A.; Kaufmann, R.; Berrevoet, F.; East, B.; Fischer, J.; Hope, W.; Klassen, D.; Lorenz, R.; Renard, Y.; et al. Guidelines for treatment of umbilical and epigastric hernias from the European Hernia Society and Americas Hernia Society. Br. J. Surg. 2020, 107, 171–190. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, J.C.; Díaz, D.M.; Sánchez, L.V.; Valencia-Vásquez, A.; Quintero, J.F.; Muñoz, L.V.; Bernal, A.F.; Osorio, G.; Guerra, Á.; Buitrago, J. Decellularization and In Vivo Recellularization of Abdominal Porcine Fascial Tissue. Tissue Eng. Regen. Med. 2020, 18, 369–376. [Google Scholar] [CrossRef]
- Song, H.; Yin, Z.; Wu, T.; Li, Y.; Luo, X.; Xu, M.; Duan, L.; Li, J. Enhanced Effect of Tendon Stem/Progenitor Cells Combined with Tendon-Derived Decellularized Extracellular Matrix on Tendon Regeneration. Cell Transplant. 2018, 27, 1634–1643. [Google Scholar] [CrossRef]
- Ahn, W.B.; Lee, Y.B.; Ji, Y.-H.; Moon, K.-S.; Jang, H.-S.; Kang, S.-W. Decellularized Human Adipose Tissue as an Alternative Graft Material for Bone Regeneration. Tissue Eng. Regen. Med. 2022, 19, 1089–1098. [Google Scholar] [CrossRef]
- Hudson, D.M.; Archer, M.; Rai, J.; Weis, M.; Fernandes, R.J.; Eyre, D.R. Age-related type I collagen modifications reveal tissue-defining differences between ligament and tendon. Matrix Biol. Plus 2021, 12, 100070. [Google Scholar] [CrossRef]
- Eisner, L.E.; Rosario, R.; Andarawis-Puri, N.; Arruda, E.M. The Role of the Non-Collagenous Extracellular Matrix in Tendon and Ligament Mechanical Behavior: A Review. J. Biomech. Eng. 2021, 144, 050801. [Google Scholar] [CrossRef]
- Zhang, C.; Svensson, R.B.; Montagna, C.; Carstensen, H.; Buhl, R.; Schoof, E.M.; Kjaer, M.; Magnusson, S.P.; Yeung, C.-Y.C. Comparison of Tenocyte Populations from the Core and Periphery of Equine Tendons. J. Proteome Res. 2020, 19, 4137–4144. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zhang, Y.; Xing, F.; Kong, Y.; Zhang, G. Changes of collagen and MMP-1 in liver, lung and kidney during growth of mice. Sheng Wu Gong Cheng Xue Bao Chin. J. Biotechnol. 2021, 37, 646–654. [Google Scholar] [CrossRef]
- Creze, M.; Soubeyrand, M.; Nyangoh Timoh, K.; Gagey, O. Organization of the fascia and aponeurosis in the lumbar paraspinal compartment. Surg. Radiol. Anat. 2018, 40, 1231–1242. [Google Scholar] [CrossRef] [PubMed]
- Sawadkar, P.; Player, D.; Bozec, L.; Mudera, V. The mechanobiology of tendon fibroblasts under static and uniaxial cyclic load in a 3D tissue engineered model mimicking native extracellular matrix. J. Tissue Eng. Regen. Med. 2020, 14, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Donahue, T.L.; Pauly, H.M. Osteoarthritic meniscal entheses exhibit altered collagen fiber orientation. Connect. Tissue Res. 2022, 63, 151–155. [Google Scholar] [CrossRef]
- Ellingson, A.; Pancheri, N.; Schiele, N. Regulators of collagen crosslinking in developing and adult tendons. Eur. Cell. Mater. 2022, 43, 130–152. [Google Scholar] [CrossRef]
- Salo, A.M.; Myllyharju, J. Prolyl and lysyl hydroxylases in collagen synthesis. Exp. Dermatol. 2021, 30, 38–49. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Taga, Y.; Zientek, K.; Mizuno, N.; Salo, A.M.; Semenova, O.; Tufa, S.; Keene, D.R.; Holden, P.; Mizuno, K.; et al. Type I and type V procollagen triple helix uses different subsets of the molecular ensemble for lysine posttranslational modifications in the rER. J. Biol. Chem. 2021, 296, 100453. [Google Scholar] [CrossRef]
- Terajima, M.; Taga, Y.; Nakamura, T.; Guo, H.-F.; Kayashima, Y.; Maeda-Smithies, N.; Parag-Sharma, K.; Kim, J.S.; Amelio, A.L.; Mizuno, K.; et al. Lysyl hydroxylase 2 mediated collagen post-translational modifications and functional outcomes. Sci. Rep. 2022, 12, 14256. [Google Scholar] [CrossRef]
- Ide, K.; Takahashi, S.; Sakai, K.; Taga, Y.; Ueno, T.; Dickens, D.; Jenkins, R.; Falciani, F.; Sasaki, T.; Ooi, K.; et al. The dipeptide prolyl-hydroxyproline promotes cellular homeostasis and lamellipodia-driven motility via active β1-integrin in adult tendon cells. J. Biol. Chem. 2021, 297, 100819. [Google Scholar] [CrossRef]
- Structure and function of tendon and ligament tissues. In Biomechanics of Tendons and Ligaments; Buschmann, J., Meier Bürgisser, G., Eds.; Woodhead Publishing: Thorston, UK, 2017; pp. 3–29. ISBN 978-0-08-100489-0. [Google Scholar]
- Luesma, M.J.; Cantarero, I.; Sánchez-Cano, A.I.; Rodellar, C.; Junquera, C. Ultrastructural evidence for telocytes in equine tendon. J. Anat. 2021, 238, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Dunkman, A.A.; Buckley, M.R.; Mienaltowski, M.J.; Adams, S.M.; Thomas, S.J.; Satchell, L.; Kumar, A.; Pathmanathan, L.; Beason, D.P.; Iozzo, R.V.; et al. Decorin expression is important for age-related changes in tendon structure and mechanical properties. Matrix Biol. J. Int. Soc. Matrix Biol. 2013, 32, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.H.-C.; Thampatty, B.P. Advances in tendon mechanobiology. In Mechanobiology in Health and Disease; Verbruggen, S.W., Ed.; Academic Press: Cambridge, MA, USA, 2018; pp. 127–155. ISBN 978-0-12-812952-4. [Google Scholar]
- Stecco, C.; Fede, C.; Macchi, V.; Porzionato, A.; Petrelli, L.; Biz, C.; Stern, R.; De Caro, R. The fasciacytes: A new cell devoted to fascial gliding regulation. Clin. Anat. 2018, 31, 667–676. [Google Scholar] [CrossRef]
- Thankam, F.G.; Chandra, I.; Diaz, C.; Dilisio, M.F.; Fleegel, J.; Gross, R.M.; Agrawal, D.K. Matrix regeneration proteins in the hypoxia-triggered exosomes of shoulder tenocytes and adipose-derived mesenchymal stem cells. Mol. Cell. Biochem. 2020, 465, 75–87. [Google Scholar] [CrossRef] [PubMed]
- De Micheli, A.J.; Swanson, J.B.; Disser, N.P.; Martinez, L.M.; Walker, N.R.; Oliver, D.J.; Cosgrove, B.D.; Mendias, C.L. Single-cell transcriptomic analysis identifies extensive heterogeneity in the cellular composition of mouse Achilles tendons. Am. J. Physiol.-Cell Physiol. 2020, 319, C885–C894. [Google Scholar] [CrossRef] [PubMed]
- Jadamba, B.; Urnukhsaikhan, E.; Gantulga, A.; Lkhagvachuluun, S.; Enkhsaikhan, L.; Tsolmon, B.; Damdindorj, L. The Characterization of Acid Soluble Collagen from Sheep Tail Tendon; Atlantis Press: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Svärd, A.; Hammerman, M.; Eliasson, P. Elastin levels are higher in healing tendons than in intact tendons and influence tissue compliance. FASEB J. 2020, 34, 13409–13418. [Google Scholar] [CrossRef]
- Ishigaki, T.; Kubo, K. Mechanical properties and collagen fiber orientation of tendon in young and elderly. Clin. Biomech. 2020, 71, 5–10. [Google Scholar] [CrossRef]
- Kharaz, Y.A.; Canty-Laird, E.G.; Tew, S.R.; Comerford, E.J. Variations in internal structure, composition and protein distribution between intra- and extra-articular knee ligaments and tendons. J. Anat. 2018, 232, 943–955. [Google Scholar] [CrossRef]
- Puetzer, J.L.; Ma, T.; Sallent, I.; Gelmi, A.; Stevens, M.M. Driving Hierarchical Collagen Fiber Formation for Functional Tendon, Ligament, and Meniscus Replacement. Biomaterials 2021, 269, 120527. [Google Scholar] [CrossRef]
- Wang, C.; Sha, Y.; Wang, S.; Chi, Q.; Sung, K.L.P.; Xu, K.; Yang, L. Lysyl oxidase suppresses the inflammatory response in anterior cruciate ligament fibroblasts and promotes tissue regeneration by targeting myotrophin via the nuclear factor-kappa B pathway. J. Tissue Eng. Regen. Med. 2020, 14, 1063–1076. [Google Scholar] [CrossRef]
- Sang, R.; Liu, Y.; Kong, L.; Qian, L.; Liu, C. Effect of Acellular Amnion with Increased TGF-β and bFGF Levels on the Biological Behavior of Tenocytes. Front. Bioeng. Biotechnol. 2020, 8, 446. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Liu, L.; Li, R.; Wei, X.; Luan, W.; Liu, P.; Zhao, J. Hypoxia-Inducible Factor 1-α (HIF-1α) Induces Apoptosis of Human Uterosacral Ligament Fibroblasts Through the Death Receptor and Mitochondrial Pathways. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2018, 24, 8722–8733. [Google Scholar] [CrossRef] [PubMed]
- Sono, T.; Hsu, C.-Y.; Wang, Y.; Xu, J.; Cherief, M.; Marini, S.; Huber, A.; Miller, S.; Péault, B.; Levi, B.; et al. Perivascular Fibro-Adipogenic Progenitor Tracing during Post-Traumatic Osteoarthritis. Am. J. Pathol. 2020, 190, 1909–1920. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xu, J.; Meyers, C.A.; Gao, Y.; Tian, Y.; Broderick, K.; Peault, B.; James, A.W. PDGFRα marks distinct perivascular populations with different osteogenic potential within adipose tissue. Stem Cells 2020, 38, 276–290. [Google Scholar] [CrossRef]
- Best, K.T.; Loiselle, A.E. Scleraxis lineage cells contribute to organized bridging tissue during tendon healing and identify a subpopulation of resident tendon cells. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2019, 33, 8578–8587. [Google Scholar] [CrossRef] [PubMed]
- Sima, Y.; Li, J.; Xiao, C.; Xu, L.; Wang, L.; Chen, Y. CD106/VCAM-1 distinguishes a fibroblast subpopulation with high colony-forming capacity and distinct protein expression from the uterosacral ligament. Ann. Transl. Med. 2022, 10, 511. [Google Scholar] [CrossRef] [PubMed]
- Thierbach, M.; Heyne, E.; Schwarzer, M.; Koch, L.G.; Britton, S.L.; Wildemann, B. Age and Intrinsic Fitness Affect the Female Rotator Cuff Tendon Tissue. Biomedicines 2022, 10, 509. [Google Scholar] [CrossRef]
- Fantoni, I.; Biz, C.; Fan, C.; Pirri, C.; Fede, C.; Lucia, P.; Ruggieri, P.; Caro, R.; Stecco, C. Fascia Lata Alterations in Hip Osteoarthritis: An Observational Cross-Sectional Study. Life 2021, 11, 1136. [Google Scholar] [CrossRef]
- Popowski, E.; Kohl, B.; Schneider, T.; Jankowski, J.; Schulze-Tanzil, G. Uremic Toxins and Ciprofloxacin Affect Human Tenocytes In Vitro. Int. J. Mol. Sci. 2020, 21, 4241. [Google Scholar] [CrossRef]
- Isik, A.; Gursul, C.; Peker, K.; Aydın, M.; Fırat, D.; Yılmaz, İ. Metalloproteinases and Their Inhibitors in Patients with Inguinal Hernia. World J. Surg. 2017, 41, 1259–1266. [Google Scholar] [CrossRef]
- Shukunami, C.; Takimoto, A.; Nishizaki, Y.; Yoshimoto, Y.; Tanaka, S.; Miura, S.; Watanabe, H.; Sakuma, T.; Yamamoto, T.; Kondoh, G.; et al. Scleraxis is a transcriptional activator that regulates the expression of Tenomodulin, a marker of mature tenocytes and ligamentocytes. Sci. Rep. 2018, 8, 3155. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.-D.; Zhu, Y.-B.; Wang, T.-R.; Zhang, W.-F.; Zhang, Y.-Z. Irradiated allograft versus autograft for anterior cruciate ligament reconstruction: A meta-analysis and systematic review of prospective studies. Int. J. Surg. 2018, 49, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Bednarski, P.; Piekarska, K. Traumatic Knee Injuries: Analysis of Reporting Data from the Period 2016-2018 Using API Interface of Polish National Health Fund Statistics. Ortop. Traumatol. Rehabil. 2020, 22, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Cherla, D.V.; Poulose, B.; Prabhu, A.S. Epidemiology and Disparities in Care: The Impact of Socioeconomic Status, Gender, and Race on the Presentation, Management, and Outcomes of Patients Undergoing Ventral Hernia Repair. Surg. Clin. N. Am. 2018, 98, 431–440. [Google Scholar] [CrossRef]
- Huang, L.; Chen, L.; Chen, H.; Wang, M.; Jin, L.; Zhou, S.; Gao, L.; Li, R.; Li, Q.; Wang, H.; et al. Biomimetic Scaffolds for Tendon Tissue Regeneration. Biomimetics 2023, 8, 246. [Google Scholar] [CrossRef]
- Oshiro, W.; Lou, J.; Xing, X.; Tu, Y.; Manske, P.R. Flexor tendon healing in the rat: A histologic and gene expression study. J. Hand Surg. 2003, 28, 814–823. [Google Scholar] [CrossRef]
- Inoue, H.; Arai, Y.; Nakagawa, S.; Fujii, Y.; Kaihara, K.; Takahashi, K. Analysis of Hemodynamic Changes After Medial Patellofemoral Ligament Reconstruction. Sports Med. Int. Open 2022, 6, E25–E31. [Google Scholar] [CrossRef]
- Genin, G.M.; Thomopoulos, S. Unification through disarray. Nat. Mater. 2017, 16, 607–608. [Google Scholar] [CrossRef]
- Apostolakos, J.; Durant, T.J.; Dwyer, C.R.; Russell, R.P.; Weinreb, J.H.; Alaee, F.; Beitzel, K.; McCarthy, M.B.; Cote, M.P.; Mazzocca, A.D. The enthesis: A review of the tendon-to-bone insertion. Muscles Ligaments Tendons J. 2014, 4, 333–342. [Google Scholar] [CrossRef]
- Felsenthal, N.; Rubin, S.; Stern, T.; Krief, S.; Pal, D.; Pryce, B.A.; Schweitzer, R.; Zelzer, E. Development of migrating tendon-bone attachments involves replacement of progenitor populations. Development 2018, 145, dev165381. [Google Scholar] [CrossRef]
- Notermans, T.; Isaksson, H. Predicting the formation of different tissue types during Achilles tendon healing using mechanoregulated and oxygen-regulated frameworks. Biomech. Model. Mechanobiol. 2023, 22, 655–667. [Google Scholar] [CrossRef] [PubMed]
- Delgado Caceres, M.; Angerpointner, K.; Galler, M.; Lin, D.; Michel, P.A.; Brochhausen, C.; Lu, X.; Varadarajan, A.R.; Warfsmann, J.; Stange, R.; et al. Tenomodulin knockout mice exhibit worse late healing outcomes with augmented trauma-induced heterotopic ossification of Achilles tendon. Cell Death Dis. 2021, 12, 1049. [Google Scholar] [CrossRef] [PubMed]
- Freedman, B.R.; Rodriguez, A.B.; Leiphart, R.J.; Newton, J.B.; Ban, E.; Sarver, J.J.; Mauck, R.L.; Shenoy, V.B.; Soslowsky, L.J. Dynamic Loading and Tendon Healing Affect Multiscale Tendon Properties and ECM Stress Transmission. Sci. Rep. 2018, 8, 10854. [Google Scholar] [CrossRef]
- Li, J.; Zhang, X.; Sun, Q.; Li, W.; Yu, A.; Fu, H.; Chen, K. Circulating matrix metalloproteinases and procollagen propeptides in inguinal hernia. Hernia J. Hernias Abdom. Wall Surg. 2018, 22, 541–547. [Google Scholar] [CrossRef]
- Deerenberg, E.B.; Henriksen, N.A.; Antoniou, G.A.; Antoniou, S.A.; Bramer, W.M.; Fischer, J.P.; Fortelny, R.H.; Gök, H.; Harris, H.W.; Hope, W.; et al. Updated guideline for closure of abdominal wall incisions from the European and American Hernia Societies. Br. J. Surg. 2022, 109, 1239–1250. [Google Scholar] [CrossRef]
- Crapo, P.M.; Gilbert, T.W.; Badylak, S.F. An overview of tissue and whole organ decellularization processes. Biomaterials 2011, 32, 3233–3243. [Google Scholar] [CrossRef] [PubMed]
- Padma, A.M.; Alsheikh, A.B.; Song, M.J.; Akouri, R.; Akyürek, L.M.; Oltean, M.; Brännström, M.; Hellström, M. Immune response after allogeneic transplantation of decellularized uterine scaffolds in the rat. Biomed. Mater. 2021, 16, 045021. [Google Scholar] [CrossRef]
- Jones, G.; Herbert, A.; Berry, H.; Edwards, J.H.; Fisher, J.; Ingham, E. Decellularization and Characterization of Porcine Superflexor Tendon: A Potential Anterior Cruciate Ligament Replacement. Tissue Eng. Part A 2017, 23, 124–134. [Google Scholar] [CrossRef]
- Hanai, H.; Jacob, G.; Nakagawa, S.; Tuan, R.S.; Nakamura, N.; Shimomura, K. Potential of Soluble Decellularized Extracellular Matrix for Musculoskeletal Tissue Engineering—Comparison of Various Mesenchymal Tissues. Front. Cell Dev. Biol. 2020, 8, 581972. [Google Scholar] [CrossRef]
- Takahashi, S.; Shimizu, R.; Sasadai, J.; Nakajima, K. Comprehensive inpatient rehabilitation for elite athletes after anterior cruciate ligament reconstruction. J. Phys. Ther. Sci. 2023, 35, 435–439. [Google Scholar] [CrossRef]
- Yanke, A.B.; Dandu, N.; Trasolini, N.A.; Darbandi, A.D.; Walsh, J.M.; Rice, R.; Huddleston, H.P.; Forsythe, B.; Verma, N.N.; Cole, B.J. Suture Anchor-Based Quadriceps Tendon Repair May Result in Improved Patient-Reported Outcomes but Similar Failure Rates Compared to the Transosseous Tunnel Technique. Arthrosc. J. Arthrosc. Relat. Surg. 2023, 39, 1483–1489.e1. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Wang, R.; Dong, W.; Yang, D.; Song, H.; Gu, Y. Synthetic Versus Biological Mesh in Ventral Hernia Repair and Abdominal Wall Reconstruction: A Systematic Review and Recommendations from Evidence-Based Medicine. World J. Surg. 2023, 47, 2416–2424. [Google Scholar] [CrossRef]
- Kotsifaki, R.; Sideris, V.; King, E.; Bahr, R.; Whiteley, R. Performance and symmetry measures during vertical jump testing at return to sport after ACL reconstruction. Br. J. Sports Med. 2023. [Google Scholar] [CrossRef]
- Poszepczyński, J.; Pietrusiński, M.; Borowiec, M.; Edward Domżalski, M. Assessment of fibrillin-2 and elastin gene polymorphisms in patients with a traumatic Achilles tendon rupture: Is Achilles tendon rupture a genetic disease? Acta Orthop. Traumatol. Turc. 2023, 57, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.S.; Li, J.; Brown, E.B.; Kuo, C.K. Embryo movements regulate tendon mechanical property development. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2018, 373, 20170325. [Google Scholar] [CrossRef] [PubMed]
- Gouarderes, S.; Ober, C.; Doumard, L.; Dandurand, J.; Vicendo, P.; Fourquaux, I.; Golberg, A.; Samouillan, V.; Gibot, L. Pulsed Electric Fields Induce Extracellular Matrix Remodeling through Matrix Metalloproteinases Activation and Decreased Collagen Production. J. Investig. Dermatol. 2022, 142, 1326–1337.e9. [Google Scholar] [CrossRef] [PubMed]
- Forouzesh, F.; Rabbani, M.; Bonakdar, S. A Comparison between Ultrasonic Bath and Direct Sonicator on Osteochondral Tissue Decellularization. J. Med. Signals Sens. 2019, 9, 227–233. [Google Scholar] [CrossRef]
- Farag, A.; Hashimi, S.M.; Vaquette, C.; Volpato, F.Z.; Hutmacher, D.W.; Ivanovski, S. Assessment of static and perfusion methods for decellularization of PCL membrane-supported periodontal ligament cell sheet constructs. Arch. Oral Biol. 2018, 88, 67–76. [Google Scholar] [CrossRef]
- Aeberhard, P.-A.; Grognuz, A.; Peneveyre, C.; McCallin, S.; Hirt-Burri, N.; Antons, J.; Pioletti, D.; Raffoul, W.; Applegate, L.A. Efficient decellularization of equine tendon with preserved biomechanical properties and cytocompatibility for human tendon surgery indications. Artif. Organs 2020, 44, E161–E171. [Google Scholar] [CrossRef]
- Santoso, E.G.; Yoshida, K.; Hirota, Y.; Aizawa, M.; Yoshino, O.; Kishida, A.; Osuga, Y.; Saito, S.; Ushida, T.; Furukawa, K.S. Application of detergents or high hydrostatic pressure as decellularization processes in uterine tissues and their subsequent effects on in vivo uterine regeneration in murine models. PLoS ONE 2014, 9, e103201. [Google Scholar] [CrossRef]
- Wu, P.; Nakamura, N.; Kimura, T.; Nam, K.; Fujisato, T.; Funamoto, S.; Higami, T.; Kishida, A. Decellularized porcine aortic intima-media as a potential cardiovascular biomaterial. Interact. Cardiovasc. Thorac. Surg. 2015, 21, 189–194. [Google Scholar] [CrossRef]
- Xing, S.; Liu, C.; Xu, B.; Chen, J.; Yin, D.; Zhang, C. Effects of various decellularization methods on histological and biomechanical properties of rabbit tendons. Exp. Ther. Med. 2014, 8, 628–634. [Google Scholar] [CrossRef]
- Burk, J.; Erbe, I.; Berner, D.; Kacza, J.; Kasper, C.; Pfeiffer, B.; Winter, K.; Brehm, W. Freeze-Thaw Cycles Enhance Decellularization of Large Tendons. Tissue Eng. Part C Methods 2014, 20, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Rothrauff, B.B.; Lin, H.; Gottardi, R.; Alexander, P.G.; Tuan, R.S. Enhancement of tenogenic differentiation of human adipose stem cells by tendon-derived extracellular matrix. Biomaterials 2013, 34, 9295–9306. [Google Scholar] [CrossRef] [PubMed]
- Narciso, M.; Ulldemolins, A.; Júnior, C.; Otero, J.; Navajas, D.; Farré, R.; Gavara, N.; Almendros, I. Novel Decellularization Method for Tissue Slices. Front. Bioeng. Biotechnol. 2022, 10, 832178. [Google Scholar] [CrossRef] [PubMed]
- White, L.J.; Taylor, A.J.; Faulk, D.M.; Keane, T.J.; Saldin, L.T.; Reing, J.E.; Swinehart, I.T.; Turner, N.J.; Ratner, B.D.; Badylak, S.F. The impact of detergents on the tissue decellularization process: A ToF-SIMS study. Acta Biomater. 2017, 50, 207–219. [Google Scholar] [CrossRef] [PubMed]
- Lohan, A.; Kohl, B.; Meier, C.; Schulze-Tanzil, G. Tenogenesis of Decellularized Porcine Achilles Tendon Matrix Reseeded with Human Tenocytes in the Nude Mice Xenograft Model. Int. J. Mol. Sci. 2018, 19, 2059. [Google Scholar] [CrossRef]
- Blaha, L.; Zhang, C.; Cabodi, M.; Wong, J.Y. A microfluidic platform for modeling metastatic cancer cell matrix invasion. Biofabrication 2017, 9, 045001. [Google Scholar] [CrossRef]
- Marvin, J.C.; Mochida, A.; Paredes, J.; Vaughn, B.; Andarawis-Puri, N. Detergent-Free Decellularization Preserves the Mechanical and Biological Integrity of Murine Tendon. Tissue Eng. Part C Methods 2022, 28, 646–655. [Google Scholar] [CrossRef]
- Reyna, W.E.; Pichika, R.; Ludvig, D.; Perreault, E.J. Efficiency of skeletal muscle decellularization methods and their effects on the extracellular matrix. J. Biomech. 2020, 110, 109961. [Google Scholar] [CrossRef]
- Hopkinson, A.; Shanmuganathan, V.A.; Gray, T.; Yeung, A.M.; Lowe, J.; James, D.K.; Dua, H.S. Optimization of Amniotic Membrane (AM) Denuding for Tissue Engineering. Tissue Eng. Part C Methods 2008, 14, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Maghsoudlou, P.; Georgiades, F.; Smith, H.; Milan, A.; Shangaris, P.; Urbani, L.; Loukogeorgakis, S.P.; Lombardi, B.; Mazza, G.; Hagen, C.; et al. Optimization of Liver Decellularization Maintains Extracellular Matrix Micro-Architecture and Composition Predisposing to Effective Cell Seeding. PLoS ONE 2016, 11, e0155324. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Cai, Z.; Cheng, J.; Wang, C.; Fang, Z.; Xiao, Y.; Feng, Z.-G.; Gu, Y. Characterization of a heparinized decellularized scaffold and its effects on mechanical and structural properties. J. Biomater. Sci. Polym. Ed. 2020, 31, 999–1023. [Google Scholar] [CrossRef]
- Zhou, S.; Yuan, B.; Huang, W.; Tang, Y.; Chen, X. Preparation and biological characteristics of a bovine acellular tendon fiber material. J. Biomed. Mater. Res. A 2021, 109, 1931–1941. [Google Scholar] [CrossRef]
- Arakelian, L.; Caille, C.; Faivre, L.; Corté, L.; Bruneval, P.; Shamdani, S.; Flageollet, C.; Albanese, P.; Domet, T.; Jarraya, M.; et al. A clinical-grade acellular matrix for esophageal replacement. J. Tissue Eng. Regen. Med. 2019, 13, 2191–2203. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, N.; Ito, A.; Kimura, T.; Kishida, A. Extracellular Matrix Induces Periodontal Ligament Reconstruction In Vivo. Int. J. Mol. Sci. 2019, 20, 3277. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.P. Tissue Engineering with Electroporation. In Handbook of Electroporation; Miklavcic, D., Ed.; Springer International Publishing: Cham, Germany, 2016; pp. 1–21. ISBN 978-3-319-26779-1. [Google Scholar]
- Chang, T.T.; Zhou, V.X.; Rubinsky, B. Using non-thermal irreversible electroporation to create an in vivo niche for exogenous cell engraftment. BioTechniques 2017, 62, 229–231. [Google Scholar] [CrossRef]
- Zhang, Y.; Lv, Y.; Wang, Y.; Chang, T.T.; Rubinsky, B. Pancreatic Islets Implanted in an Irreversible Electroporation Generated Extracellular Matrix in the Liver. Radiol. Oncol. 2023, 57, 51–58. [Google Scholar] [CrossRef]
- Song, Y.; Zheng, J.; Yan, M.; Ding, W.; Xu, K.; Fan, Q.; Li, Z. The Effects of Irreversible Electroporation on the Achilles Tendon: An Experimental Study in a Rabbit Model. PLoS ONE 2015, 10, e0131404. [Google Scholar] [CrossRef][Green Version]
- Wang, X.; Xu, K.; Zhang, E.; Bai, Q.; Ma, B.; Zhao, C.; Zhang, K.; Liu, T.; Ma, Z.; Zeng, H.; et al. Irreversible Electroporation Improves Tendon Healing in a Rat Model of Collagenase-Induced Achilles Tendinopathy. Am. J. Sports Med. 2023, 51, 1831–1843. [Google Scholar] [CrossRef]
- Koo, M.-A.; Jeong, H.; Hong, S.H.; Seon, G.M.; Lee, M.H.; Park, J.-C. Preconditioning process for dermal tissue decellularization using electroporation with sonication. Regen. Biomater. 2021, 9, rbab071. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.-H.; Hsia, K.; Su, C.-K.; Chen, C.-C.; Yeh, C.-C.; Ma, H.; Lu, J.-H. Sonication-Assisted Method for Decellularization of Human Umbilical Artery for Small-Caliber Vascular Tissue Engineering. Polymers 2021, 13, 1699. [Google Scholar] [CrossRef] [PubMed]
- Suss, P.H.; Ribeiro, V.S.T.; Motooka, C.E.; de Melo, L.C.; Tuon, F.F. Comparative study of decellularization techniques to obtain natural extracellular matrix scaffolds of human peripheral-nerve allografts. Cell Tissue Bank. 2022, 23, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Fitriatul, N.; Sha’ban, M.; Azhim, A. Evaluation of recellularization on decellularized aorta scaffolds engineered by ultrasonication treatment. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Republic of Korea, 11–15 July 2017; pp. 2072–2075. [Google Scholar] [CrossRef]
- Roth, S.P.; Glauche, S.M.; Plenge, A.; Erbe, I.; Heller, S.; Burk, J. Automated freeze-thaw cycles for decellularization of tendon tissue—A pilot study. BMC Biotechnol. 2017, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Khakpour, E.; Tavassoli, A.; Mahdavi-Shahri, N.; Matin, M.M. Assessing the biocompatibility of bovine tendon scaffold, a step forward in tendon tissue engineering. Cell Tissue Bank. 2023, 24, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Zemmyo, D.; Yamamoto, M.; Miyata, S. Efficient Decellularization by Application of Moderate High Hydrostatic Pressure with Supercooling Pretreatment. Micromachines 2021, 12, 1486. [Google Scholar] [CrossRef] [PubMed]
- Zemmyo, D.; Yamamoto, M.; Miyata, S. Fundamental Study of Decellularization Method Using Cyclic Application of High Hydrostatic Pressure. Micromachines 2020, 11, 1008. [Google Scholar] [CrossRef]
- Xu, K.; Kuntz, L.A.; Foehr, P.; Kuempel, K.; Wagner, A.; Tuebel, J.; Deimling, C.V.; Burgkart, R.H. Efficient decellularization for tissue engineering of the tendon-bone interface with preservation of biomechanics. PLoS ONE 2017, 12, e0171577. [Google Scholar] [CrossRef]
- Topuz, B.; Aydin, H.M. Preparation of decellularized optic nerve grafts. Artif. Organs 2022, 46, 618–632. [Google Scholar] [CrossRef]
- Bakhtiar, H.; Rajabi, S.; Pezeshki-Modaress, M.; Ellini, M.R.; Panahinia, M.; Alijani, S.; Mazidi, A.; Kamali, A.; Azarpazhooh, A.; Kishen, A. Optimizing Methods for Bovine Dental Pulp Decellularization. J. Endod. 2021, 47, 62–68. [Google Scholar] [CrossRef]
- Roth, S.P.; Erbe, I.; Burk, J. Decellularization of Large Tendon Specimens: Combination of Manually Performed Freeze-Thaw Cycles and Detergent Treatment. In Decellularized Scaffolds and Organogenesis: Methods and Protocols; Turksen, K., Ed.; Methods in Molecular Biology; Springer: New York, NY, USA, 2018; pp. 227–237. ISBN 978-1-4939-7656-0. [Google Scholar]
- Luo, Z.; Bian, Y.; Su, W.; Shi, L.; Li, S.; Song, Y.; Zheng, G.; Xie, A.; Xue, J. Comparison of various reagents for preparing a decellularized porcine cartilage scaffold. Am. J. Transl. Res. 2019, 11, 1417–1427. [Google Scholar] [PubMed]
- Hwang, J.; San, B.H.; Turner, N.J.; White, L.J.; Faulk, D.M.; Badylak, S.F.; Li, Y.; Yu, S.M. Molecular assessment of collagen denaturation in decellularized tissues using a collagen hybridizing peptide. Acta Biomater. 2017, 53, 268–278. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Pérez, J.; Ahearne, M. The impact of decellularization methods on extracellular matrix derived hydrogels. Sci. Rep. 2019, 9, 14933. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani, F.; Ekhtiari, M.; Moeini Chaghervand, B.; Moradi, L.; Mohammadi, B.; Kajbafzadeh, A.-M. Detection of the residual concentration of sodium dodecyl sulfate in the decellularized whole rabbit kidney extracellular matrix. Cell Tissue Bank. 2022, 23, 119–128. [Google Scholar] [CrossRef]
- Friedrich, E.E.; Lanier, S.T.; Niknam-Bienia, S.; Arenas, G.A.; Rajendran, D.; Wertheim, J.A.; Galiano, R.D. Residual sodium dodecyl sulfate in decellularized muscle matrices leads to fibroblast activation in vitro and foreign body response in vivo. J. Tissue Eng. Regen. Med. 2018, 12, e1704–e1715. [Google Scholar] [CrossRef]
- Kim, W.J.; Kim, G.H. A bioprinted complex tissue model for myotendinous junction with biochemical and biophysical cues. Bioeng. Transl. Med. 2022, 7, e10321. [Google Scholar] [CrossRef]
- Gillies, A.R.; Smith, L.R.; Lieber, R.L.; Varghese, S. Method for Decellularizing Skeletal Muscle Without Detergents or Proteolytic Enzymes. Tissue Eng. Part C Methods 2011, 17, 383–389. [Google Scholar] [CrossRef]
- Gaffney, L.S.; Davis, Z.G.; Mora-Navarro, C.; Fisher, M.B.; Freytes, D.O. Extracellular Matrix Hydrogels Promote Expression of Muscle-Tendon Junction Proteins. Tissue Eng. 2021, 28, 270–282. [Google Scholar] [CrossRef]
- Giraldo-Gomez, D.M.; Leon-Mancilla, B.; Del Prado-Audelo, M.L.; Sotres-Vega, A.; Villalba-Caloca, J.; Garciadiego-Cazares, D.; Piña-Barba, M.C. Trypsin as enhancement in cyclical tracheal decellularization: Morphological and biophysical characterization. Mater. Sci. Eng. C 2016, 59, 930–937. [Google Scholar] [CrossRef]
- Tachibana, K. N-cadherin-mediated aggregate formation; cell detachment by Trypsin-EDTA loses N-cadherin and delays aggregate formation. Biochem. Biophys. Res. Commun. 2019, 516, 414–418. [Google Scholar] [CrossRef]
- Ye, X.; Wang, H.; Gong, W.; Li, S.; Li, H.; Wang, Z.; Zhao, Q. Impact of decellularization on porcine myocardium as scaffold for tissue engineered heart tissue. J. Mater. Sci. Mater. Med. 2016, 27, 70. [Google Scholar] [CrossRef] [PubMed]
- Ozasa, Y.; Amadio, P.C.; Thoreson, A.R.; An, K.-N.; Zhao, C. Repopulation of Intrasynovial Flexor Tendon Allograft with Bone Marrow Stromal Cells: An Ex Vivo Model. Tissue Eng. Part A 2014, 20, 566–574. [Google Scholar] [CrossRef] [PubMed]
- EMA Use of Porcine Trypsin Used in the Manufacture Human Biological Medicinal Products—Scientific Guideline. Available online: https://www.ema.europa.eu/en/use-porcine-trypsin-used-manufacture-human-biological-medicinal-products-scientific-guideline (accessed on 2 July 2023).
- Ramanathan, A.; Karuri, N. Proteolysis of decellularized extracellular matrices results in loss of fibronectin and cell binding activity. Biochem. Biophys. Res. Commun. 2015, 459, 246–251. [Google Scholar] [CrossRef] [PubMed]
- Guéroult, M.; Picot, D.; Abi-Ghanem, J.; Hartmann, B.; Baaden, M. How Cations Can Assist DNase I in DNA Binding and Hydrolysis. PLoS Comput. Biol. 2010, 6, e1001000. [Google Scholar] [CrossRef] [PubMed]
- Su, M.; Zhang, Q.; Zhu, Y.; Wang, S.; Lv, J.; Sun, J.; Qiu, P.; Fan, S.; Jin, K.; Chen, L.; et al. Preparation of Decellularized Triphasic Hierarchical Bone-Fibrocartilage-Tendon Composite Extracellular Matrix for Enthesis Regeneration. Adv. Healthc. Mater. 2019, 8, 1900831. [Google Scholar] [CrossRef]
- Santos, A. de L.; Silva, C.G. da; Barreto, L.S. de S.; Tamaoki, M.J.S.; Almeida, F.G. de; Faloppa, F. Automated Assessment of Cell Infiltration and Removal in Decellularized Scaffolds—Experimental Study in Rabbits. Rev. Bras. Ortop. 2021, 57, 992–1000. [Google Scholar] [CrossRef]
- Edwards, J.H.; Jones, G.L.; Herbert, A.; Fisher, J.; Ingham, E. Integration and functional performance of a decellularised porcine superflexor tendon graft in an ovine model of anterior cruciate ligament reconstruction. Biomaterials 2021, 279, 121204. [Google Scholar] [CrossRef]
- Lafosse, A.; Desmet, C.; Aouassar, N.; André, W.; Hanet, M.-S.; Beauloye, C.; Vanwijck, R.; Poirel, H.A.; Gallez, B.; Dufrane, D. Autologous Adipose Stromal Cells Seeded onto a Human Collagen Matrix for Dermal Regeneration in Chronic Wounds: Clinical Proof of Concept. Plast. Reconstr. Surg. 2015, 136, 279. [Google Scholar] [CrossRef]
- Sabetkish, S.; Kajbafzadeh, A.-M.; Sabetkish, N.; Khorramirouz, R.; Akbarzadeh, A.; Seyedian, S.L.; Pasalar, P.; Orangian, S.; Beigi, R.S.H.; Aryan, Z.; et al. Whole-organ tissue engineering: Decellularization and recellularization of three-dimensional matrix liver scaffolds. J. Biomed. Mater. Res. A 2015, 103, 1498–1508. [Google Scholar] [CrossRef]
- Yao, S.; Liang, Z.; Lee, Y.W.; Yung, P.S.H.; Lui, P.P.Y. Bioactive Decellularized Tendon-Derived Stem Cell Sheet for Promoting Graft Healing After Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2023, 51, 66–80. [Google Scholar] [CrossRef]
- Park, J.; Jo, S.; Lee, M.-K.; Kim, T.-H.; Sung, I.-H.; Lee, J.K. Comparison of ligamentization potential between anterior cruciate ligament-derived cells and adipose-derived mesenchymal stem cells reseeded to acellularized tendon allograft. Bone Jt. Res. 2022, 11, 777–786. [Google Scholar] [CrossRef]
- Long, C.; Galvez, M.G.; Legrand, A.; Joubert, L.-M.; Wang, Z.; Chattopadhyay, A.; Chang, J.; Fox, P.M. Intratendinous Injection of Hydrogel for Reseeding Decellularized Human Flexor Tendons. Plast. Reconstr. Surg. 2017, 139, 1305e. [Google Scholar] [CrossRef]
- Li, W.; Midgley, A.C.; Bai, Y.; Zhu, M.; Chang, H.; Zhu, W.; Wang, L.; Wang, Y.; Wang, H.; Kong, D. Subcutaneously engineered autologous extracellular matrix scaffolds with aligned microchannels for enhanced tendon regeneration: Aligned microchannel scaffolds for tendon repair. Biomaterials 2019, 224, 119488. [Google Scholar] [CrossRef] [PubMed]
- Ning, L.-J.; Zhang, Y.-J.; Zhang, Y.-J.; Zhu, M.; Ding, W.; Jiang, Y.-L.; Zhang, Y.; Luo, J.-C.; Qin, T.-W. Enhancement of Migration and Tenogenic Differentiation of Macaca Mulatta Tendon-Derived Stem Cells by Decellularized Tendon Hydrogel. Front. Cell Dev. Biol. 2021, 9, 651583. [Google Scholar] [CrossRef] [PubMed]
- McGoldrick, R.; Chattopadhyay, A.; Crowe, C.; Chiou, G.; Hui, K.; Farnebo, S.; Davis, C.; Le Grand, A.; Jacobs, M.; Pham, H.; et al. The Tissue-Engineered Tendon-Bone Interface: In Vitro and In Vivo Synergistic Effects of Adipose-Derived Stem Cells, Platelet-Rich Plasma, and Extracellular Matrix Hydrogel. Plast. Reconstr. Surg. 2017, 140, 1169–1184. [Google Scholar] [CrossRef] [PubMed]
- Tao, M.; Liang, F.; He, J.; Ye, W.; Javed, R.; Wang, W.; Yu, T.; Fan, J.; Tian, X.; Wang, X.; et al. Decellularized tendon matrix membranes prevent post-surgical tendon adhesion and promote functional repair. Acta Biomater. 2021, 134, 160–176. [Google Scholar] [CrossRef]
- Crowe, C.S.; Chiou, G.; McGoldrick, R.; Hui, K.; Pham, H.; Hollenbeck, E.; Chang, J. In Vitro Characteristics of Porcine Tendon Hydrogel for Tendon Regeneration. Ann. Plast. Surg. 2016, 77, 47–53. [Google Scholar] [CrossRef]
- Toprakhisar, B.; Nadernezhad, A.; Bakirci, E.; Khani, N.; Skvortsov, G.A.; Koc, B. Development of Bioink from Decellularized Tendon Extracellular Matrix for 3D Bioprinting. Macromol. Biosci. 2018, 18, e1800024. [Google Scholar] [CrossRef]
- Zhao, F.; Cheng, J.; Zhang, J.; Yu, H.; Dai, W.; Yan, W.; Sun, M.; Ding, G.; Li, Q.; Meng, Q.; et al. Comparison of three different acidic solutions in tendon decellularized extracellular matrix bio-ink fabrication for 3D cell printing. Acta Biomater. 2021, 131, 262–275. [Google Scholar] [CrossRef]
- Chae, S.; Yong, U.; Park, W.; Choi, Y.; Jeon, I.-H.; Kang, H.; Jang, J.; Choi, H.S.; Cho, D.-W. 3D cell-printing of gradient multi-tissue interfaces for rotator cuff regeneration. Bioact. Mater. 2022, 19, 611–625. [Google Scholar] [CrossRef]
- Kara, A.; Distler, T.; Polley, C.; Schneidereit, D.; Seitz, H.; Friedrich, O.; Tihminlioglu, F.; Boccaccini, A.R. 3D printed gelatin/decellularized bone composite scaffolds for bone tissue engineering: Fabrication, characterization and cytocompatibility study. Mater. Today Bio 2022, 15, 100309. [Google Scholar] [CrossRef] [PubMed]
- Guler, S.; Aydin, H.M.; Lü, L.-X.; Yang, Y. Improvement of Decellularization Efficiency of Porcine Aorta Using Dimethyl Sulfoxide as a Penetration Enhancer. Artif. Organs 2018, 42, 219–230. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Qiu, H.; Wang, D.; Miao, H.; Zhu, Y.; Guo, Q.; Guo, Y.; Wang, Z. Enhanced vascularization and biocompatibility of rat pancreatic decellularized scaffolds loaded with platelet-rich plasma. J. Biomater. Appl. 2020, 35, 313–330. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Liu, D.; Chu, G.; Yu, Q.; Liu, Z.; Li, J.; Meng, Q.; Wang, W.; Han, F.; Li, B. TGF-β1-supplemented decellularized annulus fibrosus matrix hydrogels promote annulus fibrosus repair. Bioact. Mater. 2022, 19, 581–593. [Google Scholar] [CrossRef]
- Cheng, C.; Peng, X.; Xi, L.; Luo, Y.; Wang, Y.; Zhou, Y.; Yu, X. Feasibility study of oxidized naringin as a novel crosslinking agent for crosslinking decellularized porcine Achilles tendon and its potential application for anterior cruciate ligament repair. J. Biomed. Mater. Res. A 2023, 111, 170–184. [Google Scholar] [CrossRef]
- Evrova, O.; Kellenberger, D.; Calcagni, M.; Vogel, V.; Buschmann, J. Supporting Cell-Based Tendon Therapy: Effect of PDGF-BB and Ascorbic Acid on Rabbit Achilles Tenocytes in Vitro. Int. J. Mol. Sci. 2020, 21, 458. [Google Scholar] [CrossRef]
- Sukhorukova, I.V.; Sheveyko, A.N.; Firestein, K.L.; Kiryukhantsev-Korneev, P.V.; Golberg, D.; Shtansky, D.V. Mechanical properties of decellularized extracellular matrix coated with TiCaPCON film. Biomed. Mater. Bristol Engl. 2017, 12, 035014. [Google Scholar] [CrossRef]
- Yang, J.-L.; Yao, X.; Qing, Q.; Zhang, Y.; Jiang, Y.-L.; Ning, L.-J.; Luo, J.-C.; Qin, T.-W. An engineered tendon/ligament bioscaffold derived from decellularized and demineralized cortical bone matrix. J. Biomed. Mater. Res. A 2018, 106, 468–478. [Google Scholar] [CrossRef]
- Fu, S.-C.; Yeung, M.-Y.; Rolf, C.G.; Yung, P.S.-H.; Chan, K.-M.; Hung, L.-K. Hydrogen peroxide induced tendinopathic changes in a rat model of patellar tendon injury. J. Orthop. Res. 2018, 36, 3268–3274. [Google Scholar] [CrossRef]
- Kim, R.J.; An, S.H.; Gwark, J.Y.; Park, H.B. Antioxidant effects on hypoxia-induced oxidative stress and apoptosis in rat rotator cuff fibroblasts. Eur. Cell. Mater. 2021, 41, 680–693. [Google Scholar] [CrossRef]
- Chen, B.; Liang, Y.; Zhang, J.; Bai, L.; Xu, M.; Han, Q.; Han, X.; Xiu, J.; Li, M.; Zhou, X.; et al. Synergistic enhancement of tendon-to-bone healing via anti-inflammatory and pro-differentiation effects caused by sustained release of Mg2+/curcumin from injectable self-healing hydrogels. Theranostics 2021, 11, 5911–5925. [Google Scholar] [CrossRef] [PubMed]
- Yamaura, K.; Mifune, Y.; Inui, A.; Nishimoto, H.; Kurosawa, T.; Mukohara, S.; Hoshino, Y.; Niikura, T.; Kuroda, R. Antioxidant effect of nicotinamide mononucleotide in tendinopathy. BMC Musculoskelet. Disord. 2022, 23, 249. [Google Scholar] [CrossRef] [PubMed]
- Data, K.; Marcinkowska, K.; Buś, K.; Valihrach, L.; Pawlak, E.; Śmieszek, A. β-Lactoglobulin affects the oxidative status and viability of equine endometrial progenitor cells via lncRNA-mRNA-miRNA regulatory associations. J. Cell. Mol. Med. 2023, 27, 927–938. [Google Scholar] [CrossRef] [PubMed]
- Roth, S.P.; Schubert, S.; Scheibe, P.; Groß, C.; Brehm, W.; Burk, J. Growth Factor-Mediated Tenogenic Induction of Multipotent Mesenchymal Stromal Cells Is Altered by the Microenvironment of Tendon Matrix. Cell Transplant. 2018, 27, 1434–1450. [Google Scholar] [CrossRef]
- Chen, C.; Shi, Q.; Li, M.; Chen, Y.; Zhang, T.; Xu, Y.; Liao, Y.; Ding, S.; Wang, Z.; Li, X.; et al. Engineering an enthesis-like graft for rotator cuff repair: An approach to fabricate highly biomimetic scaffold capable of zone-specifically releasing stem cell differentiation inducers. Bioact. Mater. 2022, 16, 451–471. [Google Scholar] [CrossRef]
- Cao, R.; Zhan, A.; Ci, Z.; Wang, C.; She, Y.; Xu, Y.; Xiao, K.; Xia, H.; Shen, L.; Meng, D.; et al. A Biomimetic Biphasic Scaffold Consisting of Decellularized Cartilage and Decalcified Bone Matrixes for Osteochondral Defect Repair. Front. Cell Dev. Biol. 2021, 9, 639006. [Google Scholar] [CrossRef]
- Rothrauff, B.B.; Coluccino, L.; Gottardi, R.; Ceseracciu, L.; Scaglione, S.; Goldoni, L.; Tuan, R.S. Efficacy of thermoresponsive, photocrosslinkable hydrogels derived from decellularized tendon and cartilage extracellular matrix for cartilage tissue engineering. J. Tissue Eng. Regen. Med. 2018, 12, e159–e170. [Google Scholar] [CrossRef]
- Song, K.; Jiang, T.; Pan, P.; Yao, Y.; Jiang, Q. Exosomes from tendon derived stem cells promote tendon repair through miR-144-3p-regulated tenocyte proliferation and migration. Stem Cell Res. Ther. 2022, 13, 80. [Google Scholar] [CrossRef]
- Yu, H.; Cheng, J.; Shi, W.; Ren, B.; Zhao, F.; Shi, Y.; Yang, P.; Duan, X.; Zhang, J.; Fu, X.; et al. Bone marrow mesenchymal stem cell-derived exosomes promote tendon regeneration by facilitating the proliferation and migration of endogenous tendon stem/progenitor cells. Acta Biomater. 2020, 106, 328–341. [Google Scholar] [CrossRef]
- Liu, H.; Zhang, M.; Shi, M.; Zhang, T.; Lu, W.; Yang, S.; Cui, Q.; Li, Z. Adipose-derived mesenchymal stromal cell-derived exosomes promote tendon healing by activating both SMAD1/5/9 and SMAD2/3. Stem Cell Res. Ther. 2021, 12, 338. [Google Scholar] [CrossRef]
- Graça, A.L.; Domingues, R.M.A.; Calejo, I.; Gómez-Florit, M.; Gomes, M.E. Therapeutic Effects of Platelet-Derived Extracellular Vesicles in a Bioengineered Tendon Disease Model. Int. J. Mol. Sci. 2022, 23, 2948. [Google Scholar] [CrossRef]
- Graça, A.L.; Domingues, R.M.A.; Gomez-Florit, M.; Gomes, M.E. Platelet-Derived Extracellular Vesicles Promote Tenogenic Differentiation of Stem Cells on Bioengineered Living Fibers. Int. J. Mol. Sci. 2023, 24, 3516. [Google Scholar] [CrossRef] [PubMed]
- Antich-Rosselló, M.; Forteza-Genestra, M.A.; Calvo, J.; Gayà, A.; Monjo, M.; Ramis, J.M. Platelet-derived extracellular vesicles promote osteoinduction of mesenchymal stromal cells. Bone Jt. Res. 2020, 9, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Sadallah, S.; Amicarella, F.; Eken, C.; Iezzi, G.; Schifferli, J.A. Ectosomes released by platelets induce differentiation of CD4+T cells into T regulatory cells. Thromb. Haemost. 2014, 112, 1219–1229. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Xu, J.; Dong, S.; Xie, G.; Yang, S.; Huangfu, X.; Li, X.; Zhang, Y.; Shen, P.; Yan, Z.; et al. Anterior Cruciate Ligament Reconstruction in a Rabbit Model Using a Decellularized Allogenic Semitendinous Tendon Combined with Autologous Bone Marrow-Derived Mesenchymal Stem Cells. Stem Cells Transl. Med. 2019, 8, 971–982. [Google Scholar] [CrossRef] [PubMed]
- Mathes, T.; Prediger, B.; Walgenbach, M.; Siegel, R. Mesh fixation techniques in primary ventral or incisional hernia repair. Cochrane Database Syst. Rev. 2021, 2021, CD011563. [Google Scholar] [CrossRef]
- Buell, J.F.; Helm, J.; Mckillop, I.H.; Iglesias, B.; Pashos, N.; Hooper, P. Decellularized biologic muscle-fascia abdominal wall scaffold graft. Surgery 2021, 169, 595–602. [Google Scholar] [CrossRef]
- de Lima Santos, A.; da Silva, C.G.; de Sá Barreto, L.S.; Leite, K.R.M.; Tamaoki, M.J.S.; Ferreira, L.M.; de Almeida, F.G.; Faloppa, F. A new decellularized tendon scaffold for rotator cuff tears—Evaluation in rabbits. BMC Musculoskelet. Disord. 2020, 21, 689. [Google Scholar] [CrossRef]
- Uquillas, J.A.; Spierings, J.; van der Lande, A.; Eren, A.D.; Bertrand, M.; Yuan, H.; Yuan, H.; van Groningen, B.; Janssen, R.; Ito, K.; et al. An off-the-shelf decellularized and sterilized human bone-ACL-bone allograft for anterior cruciate ligament reconstruction. J. Mech. Behav. Biomed. Mater. 2022, 135, 105452. [Google Scholar] [CrossRef]
- Bottagisio, M.; D’Arrigo, D.; Talò, G.; Bongio, M.; Ferroni, M.; Boschetti, F.; Moretti, M.; Lovati, A.B. Achilles Tendon Repair by Decellularized and Engineered Xenografts in a Rabbit Model. Stem Cells Int. 2019, 2019, 5267479. [Google Scholar] [CrossRef]

| Tenocytes | Ligament Fibroblasts | Fasciacytes | Fascial Fibroblasts | |
|---|---|---|---|---|
| VIM | + | + | + | + |
| [36] | [37] | [27] | [27] | |
| PDGFRA | + | + | NA | + |
| [1] | [38] | [39] | ||
| FSP-1 | + | + | + | − |
| [40] | [41] | [27] | [27] | |
| COL1 | + | + | NA | + |
| [42] | [41] | [43] | ||
| MMP-1 | + | + | NA | + |
| [44] | [41] | [45] | ||
| SCX | + | + | NA | NA |
| [40] | [46] |
| Method | Mechanism of Action | Efficiency | Effect on ECM | Comments | Source | |
|---|---|---|---|---|---|---|
| Physical | Electroporation | Poration of cell membrane through destabilizing its electric potential | Insufficient | Forms microcavities that do not affect the strength of sample | Can be processed in situ | [59,60,61] |
| Sonication | Disrupting cell membrane by high-frequency sound waves | Low | Loosening of the collagen fibers, but used with lower intensity preserves ECM structure | Lack of information about using it in DRCT | [71,72] | |
| Freeze–Thaw | Disruption of cell membranes by freezing ice crystals | High | Preserves native structure | Rinsing sample even with distilled water increase the effectiveness of procedure | [63,73,74] | |
| High Hydrostatic Pressure | Loosening of the phospholipid bilayer | High | Preserves native structure | There is a lack of information about efficiency in DRCT | [75,76] | |
| Chemical | Triton X-100 | Disruption of lipid bilayer of cell membrane | Insufficient | Loosening of the fibers, but using low concentration can preserve the ECM structure | The most commonly used procedure in DRCT | [77,78,79] |
| SDS | Disruption of covalent bonds between membrane proteins | High | Dissolves the fibers leading to merging into a homogeneous mass | Has a long-lasting cytotoxic effect and requires advanced washing | [80,81] | |
| Sodium Azide | Inhibition of cytochrome C oxidase | High | Preserves native structure | Commonly used bacteriostatic agent | [82,83] | |
| Latrunculin | Depolymerization of actin filaments to destroy cell cytoskeleton | High | Preserves native structure | There is a lack of information about efficiency in DRCT | [84,85] | |
| EDTA | Reducing cell adhesion to ECM by binding to metal cations | Low | Reduces the number of proteins in some samples | Commonly used as supplement increasing trypsin activity | [86,87] | |
| Trypsin | Digesting membrane proteins leading to membrane permeability | High | Dissolves the fibers, but used with low concentration preserves the native structure | Demonstrates high efficiency even in low concentration | [88,89] | |
| Nucleases | Cleaving DNA or RNA released from the cells disrupted by other agents | Low | Preserves native structure | As supplement to protocol, greatly increases efficiency of other methods | [90,91] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Data, K.; Kulus, M.; Ziemak, H.; Chwarzyński, M.; Piotrowska-Kempisty, H.; Bukowska, D.; Antosik, P.; Mozdziak, P.; Kempisty, B. Decellularization of Dense Regular Connective Tissue—Cellular and Molecular Modification with Applications in Regenerative Medicine. Cells 2023, 12, 2293. https://doi.org/10.3390/cells12182293
Data K, Kulus M, Ziemak H, Chwarzyński M, Piotrowska-Kempisty H, Bukowska D, Antosik P, Mozdziak P, Kempisty B. Decellularization of Dense Regular Connective Tissue—Cellular and Molecular Modification with Applications in Regenerative Medicine. Cells. 2023; 12(18):2293. https://doi.org/10.3390/cells12182293
Chicago/Turabian StyleData, Krzysztof, Magdalena Kulus, Hanna Ziemak, Mikołaj Chwarzyński, Hanna Piotrowska-Kempisty, Dorota Bukowska, Paweł Antosik, Paul Mozdziak, and Bartosz Kempisty. 2023. "Decellularization of Dense Regular Connective Tissue—Cellular and Molecular Modification with Applications in Regenerative Medicine" Cells 12, no. 18: 2293. https://doi.org/10.3390/cells12182293
APA StyleData, K., Kulus, M., Ziemak, H., Chwarzyński, M., Piotrowska-Kempisty, H., Bukowska, D., Antosik, P., Mozdziak, P., & Kempisty, B. (2023). Decellularization of Dense Regular Connective Tissue—Cellular and Molecular Modification with Applications in Regenerative Medicine. Cells, 12(18), 2293. https://doi.org/10.3390/cells12182293






