Organ Abnormalities Caused by Turner Syndrome
Abstract
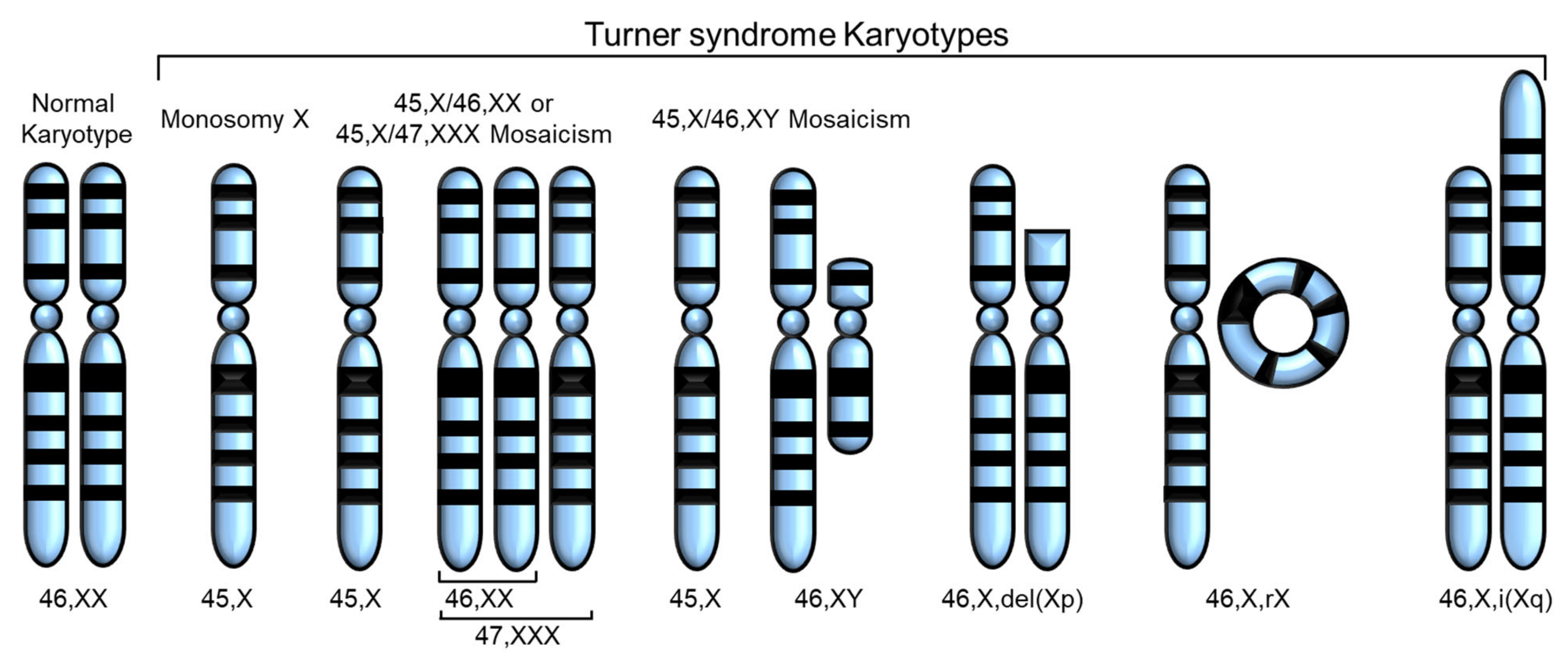
1. Introduction
2. Fertility Problems
3. Heart and Cardiovascular Disease
4. Liver Abnormalities
5. Kidney Abnormalities
6. Skeletal Abnormalities and Short Stature
7. Brain Abnormalities
8. Relevance to X Chromosome Inactivation and Escape Genes
9. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saenger, P. Turner’s syndrome. N. Engl. J. Med. 1996, 335, 1749–1754. [Google Scholar] [CrossRef] [PubMed]
- Turner, H.H. A syndrome of infantilism, congenital webbed neck, and cubitus valgus. Endocrinology 1938, 23, 566–574. [Google Scholar] [CrossRef]
- Ford, C.E.; Jones, K.W.; Polani, P.E.; De Almeida, J.C.; Briggs, J.H. A sex-chromosome anomaly in a case of gonadal dysgenesis (Turner’s syndrome). Lancet 1959, 1, 711–713. [Google Scholar] [CrossRef] [PubMed]
- Bollig, K.J.; Mainigi, M.; Senapati, S.; Lin, A.E.; Levitsky, L.L.; Bamba, V. Turner syndrome: Fertility counselling in childhood and through the reproductive lifespan. Curr. Opin. Endocrinol. Diabetes Obes. 2023, 30, 16–26. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Viuff, M.; Just, J.; Sandahl, K.; Brun, S.; van der Velden, J.; Andersen, N.H.; Skakkebaek, A. The Changing Face of Turner Syndrome. Endocr. Rev. 2023, 44, 33–69. [Google Scholar] [CrossRef] [PubMed]
- Rao, E.; Weiss, B.; Fukami, M.; Rump, A.; Niesler, B.; Mertz, A.; Muroya, K.; Binder, G.; Kirsch, S.; Winkelmann, M.; et al. Pseudoautosomal deletions encompassing a novel homeobox gene cause growth failure in idiopathic short stature and Turner syndrome. Nat. Genet. 1997, 16, 54–63. [Google Scholar] [CrossRef]
- Ellison, J.W.; Wardak, Z.; Young, M.F.; Gehron Robey, P.; Laig-Webster, M.; Chiong, W. PHOG, a candidate gene for involvement in the short stature of Turner syndrome. Hum. Mol. Genet. 1997, 6, 1341–1347. [Google Scholar] [CrossRef]
- Huang, A.C.; Olson, S.B.; Maslen, C.L. A Review of Recent Developments in Turner Syndrome Research. J. Cardiovasc. Dev. Dis. 2021, 8, 138. [Google Scholar] [CrossRef]
- Binder, G.; Fritsch, H.; Schweizer, R.; Ranke, M.B. Radiological signs of Leri-Weill dyschondrosteosis in Turner syndrome. Horm. Res. 2001, 55, 71–76. [Google Scholar] [CrossRef]
- Marchini, A.; Ogata, T.; Rappold, G.A. A Track Record on SHOX: From Basic Research to Complex Models and Therapy. Endocr. Rev. 2016, 37, 417–448. [Google Scholar] [CrossRef]
- Ottesen, A.M.; Aksglaede, L.; Garn, I.; Tartaglia, N.; Tassone, F.; Gravholt, C.H.; Bojesen, A.; Sorensen, K.; Jorgensen, N.; Rajpert-De Meyts, E.; et al. Increased number of sex chromosomes affects height in a nonlinear fashion: A study of 305 patients with sex chromosome aneuploidy. Am. J. Med. Genet. A 2010, 152A, 1206–1212. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.J.; Lafreniere, R.G.; Powers, V.E.; Sebastio, G.; Ballabio, A.; Pettigrew, A.L.; Ledbetter, D.H.; Levy, E.; Craig, I.W.; Willard, H.F. Localization of the X inactivation centre on the human X chromosome in Xq13. Nature 1991, 349, 82–84. [Google Scholar] [CrossRef] [PubMed]
- Ahern, D.T.; Bansal, P.; Armillei, M.K.; Faustino, I.V.; Kondaveeti, Y.; Glatt-Deeley, H.R.; Banda, E.C.; Pinter, S.F. Monosomy X in isogenic human iPSC-derived trophoblast model impacts expression modules preserved in human placenta. Proc. Natl. Acad. Sci. USA 2022, 119, e2211073119. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Castillo-Morales, A.; Jiang, M.; Zhu, Y.; Hu, L.; Urrutia, A.O.; Kong, X.; Hurst, L.D. Genes That Escape X-Inactivation in Humans Have High Intraspecific Variability in Expression, Are Associated with Mental Impairment but Are Not Slow Evolving. Mol. Biol. Evol. 2013, 30, 2588–2601. [Google Scholar] [CrossRef]
- Binder, G. Short stature due to SHOX deficiency: Genotype, phenotype, and therapy. Horm. Res. Paediatr. 2011, 75, 81–89. [Google Scholar] [CrossRef]
- Davies, W. The contribution of Xp22.31 gene dosage to Turner and Klinefelter syndromes and sex-biased phenotypes. Eur. J. Med. Genet. 2021, 64, 104169. [Google Scholar] [CrossRef]
- Rajpathak, S.N.; Vellarikkal, S.K.; Patowary, A.; Scaria, V.; Sivasubbu, S.; Deobagkar, D.D. Human 45,X fibroblast transcriptome reveals distinct differentially expressed genes including long noncoding RNAs potentially associated with the pathophysiology of Turner syndrome. PLoS ONE 2014, 9, e100076. [Google Scholar] [CrossRef]
- Zhang, R.; Hao, L.; Wang, L.; Chen, M.; Li, W.; Li, R.; Yu, J.; Xiao, J.; Wu, J. Gene expression analysis of induced pluripotent stem cells from aneuploid chromosomal syndromes. BMC Genom. 2013, 14, S8. [Google Scholar] [CrossRef]
- Zhang, X.; Hong, D.; Ma, S.; Ward, T.; Ho, M.; Pattni, R.; Duren, Z.; Stankov, A.; Bade Shrestha, S.; Hallmayer, J.; et al. Integrated functional genomic analyses of Klinefelter and Turner syndromes reveal global network effects of altered X chromosome dosage. Proc. Natl. Acad. Sci. USA 2020, 117, 4864–4873. [Google Scholar] [CrossRef]
- Wang, H.; Zhu, H.; Zhu, W.; Xu, Y.; Wang, N.; Han, B.; Song, H.; Qiao, J. Bioinformatic Analysis Identifies Potential Key Genes in the Pathogenesis of Turner Syndrome. Front Endocrinol. 2020, 11, 104. [Google Scholar] [CrossRef]
- Urbach, A.; Benvenisty, N. Studying early lethality of 45,XO (Turner’s syndrome) embryos using human embryonic stem cells. PLoS ONE 2009, 4, e4175. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Wang, Q.; Yu, M.; Kong, Y.; Shi, F.; Wang, S. Bioinformatic analysis identifies the immunological profile of turner syndrome with different X chromosome origins. Front Endocrinol. 2023, 14, 1024244. [Google Scholar] [CrossRef] [PubMed]
- Viuff, M.H.; Berglund, A.; Juul, S.; Andersen, N.H.; Stochholm, K.; Gravholt, C.H. Sex Hormone Replacement Therapy in Turner Syndrome: Impact on Morbidity and Mortality. J. Clin. Endocrinol. Metab. 2020, 105, 468–478. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Juul, S.; Naeraa, R.W.; Hansen, J. Morbidity in Turner syndrome. J. Clin. Epidemiol. 1998, 51, 147–158. [Google Scholar] [CrossRef]
- Schoemaker, M.J.; Swerdlow, A.J.; Higgins, C.D.; Wright, A.F.; Jacobs, P.A.; United Kingdom Clinical Cytogenetics, G. Mortality in women with turner syndrome in Great Britain: A national cohort study. J. Clin. Endocrinol. Metab. 2008, 93, 4735–4742. [Google Scholar] [CrossRef]
- Tuke, M.A.; Ruth, K.S.; Wood, A.R.; Beaumont, R.N.; Tyrrell, J.; Jones, S.E.; Yaghootkar, H.; Turner, C.L.S.; Donohoe, M.E.; Brooke, A.M.; et al. Mosaic Turner syndrome shows reduced penetrance in an adult population study. Genet. Med. 2019, 21, 877–886. [Google Scholar] [CrossRef]
- Cameron-Pimblett, A.; La Rosa, C.; King, T.F.J.; Davies, M.C.; Conway, G.S. The Turner syndrome life course project: Karyotype-phenotype analyses across the lifespan. Clin. Endocrinol. 2017, 87, 532–538. [Google Scholar] [CrossRef]
- Bernard, V.; Donadille, B.; Zenaty, D.; Courtillot, C.; Salenave, S.; Brac de la Perriere, A.; Albarel, F.; Fevre, A.; Kerlan, V.; Brue, T.; et al. Spontaneous fertility and pregnancy outcomes amongst 480 women with Turner syndrome. Hum. Reprod. 2016, 31, 782–788. [Google Scholar] [CrossRef]
- Denes, A.M.; Landin-Wilhelmsen, K.; Wettergren, Y.; Bryman, I.; Hanson, C. The proportion of diploid 46,XX cells increases with time in women with Turner syndrome–A 10-year follow-up study. Genet. Test Mol. Biomark. 2015, 19, 82–87. [Google Scholar] [CrossRef]
- El-Mansoury, M.; Barrenas, M.L.; Bryman, I.; Hanson, C.; Larsson, C.; Wilhelmsen, L.; Landin-Wilhelmsen, K. Chromosomal mosaicism mitigates stigmata and cardiovascular risk factors in Turner syndrome. Clin. Endocrinol. 2007, 66, 744–751. [Google Scholar] [CrossRef]
- Bryman, I.; Sylven, L.; Berntorp, K.; Innala, E.; Bergstrom, I.; Hanson, C.; Oxholm, M.; Landin-Wilhelmsen, K. Pregnancy rate and outcome in Swedish women with Turner syndrome. Fertil. Steril. 2011, 95, 2507–2510. [Google Scholar] [CrossRef] [PubMed]
- Sybert, V.P. Phenotypic effects of mosaicism for a 47,XXX cell line in Turner syndrome. J. Med. Genet. 2002, 39, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Snyder, E.A.; San Roman, A.K.; Pina-Aguilar, R.E.; Steeves, M.A.; McNamara, E.A.; Souter, I.; Hayes, F.J.; Levitsky, L.L.; Lin, A.E. Genetic counseling for women with 45,X/46,XX mosaicism: Towards more personalized management. Eur. J. Med. Genet. 2021, 64, 104140. [Google Scholar] [CrossRef]
- Luo, Y.; Zhu, D.; Du, R.; Gong, Y.; Xie, C.; Xu, X.; Fan, Y.; Yu, B.; Sun, X.; Chen, Y. Uniparental disomy of the entire X chromosome in Turner syndrome patient-specific induced pluripotent stem cells. Cell Discov. 2015, 1, 15022. [Google Scholar] [CrossRef] [PubMed]
- Hovatta, O. Pregnancies in women with Turner’s syndrome. Ann. Med. 1999, 31, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Birkebaek, N.H.; Cruger, D.; Hansen, J.; Nielsen, J.; Bruun-Petersen, G. Fertility and pregnancy outcome in Danish women with Turner syndrome. Clin. Genet. 2002, 61, 35–39. [Google Scholar] [CrossRef]
- Hadnott, T.N.; Gould, H.N.; Gharib, A.M.; Bondy, C.A. Outcomes of spontaneous and assisted pregnancies in Turner syndrome: The U.S. National Institutes of Health experience. Fertil. Steril. 2011, 95, 2251–2256. [Google Scholar] [CrossRef]
- Lippe, B. Turner syndrome. Endocrinol. Metab. Clin. N. Am. 1991, 20, 121–152. [Google Scholar] [CrossRef]
- Cleemann, L.; Holm, K.; Fallentin, E.; Skouby, S.O.; Smedegaard, H.; Moller, N.; Borch-Christensen, H.; Jeppesen, E.M.; Wieslander, S.B.; Andersson, A.M.; et al. Uterus and ovaries in girls and young women with Turner syndrome evaluated by ultrasound and magnetic resonance imaging. Clin. Endocrinol. 2011, 74, 756–761. [Google Scholar] [CrossRef]
- Weiss, L. Additional evidence of gradual loss of germ cells in the pathogenesis of streak ovaries in Turner’s syndrome. J. Med. Genet. 1971, 8, 540–544. [Google Scholar] [CrossRef]
- Prakash, S.K.; Crenshaw, M.L.; Backeljauw, P.F.; Silberbach, M.; Scurlock, C.; Culin, D.D.; Ranallo, K.C.; Lin, A.E. 45,X mosaicism in a population-based biobank: Implications for Turner syndrome. Genet. Med. 2019, 21, 1882–1883. [Google Scholar] [CrossRef] [PubMed]
- Negreiros, L.P.; Bolina, E.R.; Guimaraes, M.M. Pubertal development profile in patients with Turner syndrome. J. Pediatr. Endocrinol. Metab. 2014, 27, 845–849. [Google Scholar] [CrossRef] [PubMed]
- Viuff, M.; Gravholt, C.H. Turner Syndrome and Fertility. Ann. Endocrinol. 2022, 83, 244–249. [Google Scholar] [CrossRef]
- Reynaud, K.; Cortvrindt, R.; Verlinde, F.; De Schepper, J.; Bourgain, C.; Smitz, J. Number of ovarian follicles in human fetuses with the 45,X karyotype. Fertil. Steril. 2004, 81, 1112–1119. [Google Scholar] [CrossRef] [PubMed]
- Hovatta, O. Ovarian function and in vitro fertilization (IVF) in Turner syndrome. Pediatr. Endocrinol. Rev. 2012, 9, 713–717. [Google Scholar]
- Bakalov, V.K.; Shawker, T.; Ceniceros, I.; Bondy, C.A. Uterine development in Turner syndrome. J. Pediatr. 2007, 151, 528–531. [Google Scholar] [CrossRef]
- Viuff, M.H.; Just, J.; Brun, S.; Dam, T.V.; Hansen, M.; Melgaard, L.; Hougaard, D.M.; Lappe, M.; Gravholt, C.H. Women with Turner Syndrome Are Both Estrogen and Androgen Deficient: The Impact of Hormone Replacement Therapy. J. Clin. Endocrinol. Metab. 2022, 107, 1983–1993. [Google Scholar] [CrossRef]
- Hagen, C.P.; Main, K.M.; Kjaergaard, S.; Juul, A. FSH, LH, inhibin B and estradiol levels in Turner syndrome depend on age and karyotype: Longitudinal study of 70 Turner girls with or without spontaneous puberty. Hum. Reprod. 2010, 25, 3134–3141. [Google Scholar] [CrossRef]
- Ljubicic, M.L.; Busch, A.S.; Upners, E.N.; Fischer, M.B.; Petersen, J.H.; Raket, L.L.; Frederiksen, H.; Johannsen, T.H.; Juul, A.; Hagen, C.P. A Biphasic Pattern of Reproductive Hormones in Healthy Female Infants: The COPENHAGEN Minipuberty Study. J. Clin. Endocrinol. Metab. 2022, 107, 2598–2605. [Google Scholar] [CrossRef]
- Paterson, W.F.; Hollman, A.S.; Donaldson, M.D. Poor uterine development in Turner syndrome with oral oestrogen therapy. Clin. Endocrinol. 2002, 56, 359–365. [Google Scholar] [CrossRef]
- Practice Committee of American Society for Reproductive Medicine. Increased maternal cardiovascular mortality associated with pregnancy in women with Turner syndrome. Fertil. Steril. 2012, 97, 282–284. [Google Scholar] [CrossRef]
- Cauldwell, M.; Steer, P.J.; Adamson, D.; Alexander, C.; Allen, L.; Bhagra, C.; Bolger, A.; Bonner, S.; Calanchini, M.; Carroll, A.; et al. Pregnancies in women with Turner syndrome: A retrospective multicentre UK study. BJOG 2022, 129, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.H.; Furlong, R.A.; Burkin, H.; Chalmers, I.J.; Brown, G.M.; Khwaja, O.; Affara, N.A. The Drosophila developmental gene fat facets has a human homologue in Xp11.4 which escapes X-inactivation and has related sequences on Yq11.2. Hum. Mol. Genet. 1996, 5, 1695–1701. [Google Scholar] [CrossRef] [PubMed]
- Quilter, C.R.; Karcanias, A.C.; Bagga, M.R.; Duncan, S.; Murray, A.; Conway, G.S.; Sargent, C.A.; Affara, N.A. Analysis of X chromosome genomic DNA sequence copy number variation associated with premature ovarian failure (POF). Hum. Reprod. 2010, 25, 2139–2150. [Google Scholar] [CrossRef] [PubMed]
- Silberbach, M.; Roos-Hesselink, J.W.; Andersen, N.H.; Braverman, A.C.; Brown, N.; Collins, R.T.; De Backer, J.; Eagle, K.A.; Hiratzka, L.F.; Johnson, W.H., Jr.; et al. Cardiovascular Health in Turner Syndrome: A Scientific Statement from the American Heart Association. Circ. Genom. Precis. Med. 2018, 11, e000048. [Google Scholar] [CrossRef] [PubMed]
- Miyabara, S.; Nakayama, M.; Suzumori, K.; Yonemitsu, N.; Sugihara, H. Developmental analysis of cardiovascular system of 45,X fetuses with cystic hygroma. Am. J. Med. Genet. 1997, 68, 135–141. [Google Scholar] [CrossRef]
- Angelini, P. Coronary artery anomalies: An entity in search of an identity. Circulation 2007, 115, 1296–1305. [Google Scholar] [CrossRef]
- Koenraadt, W.M.C.; Siebelink, H.J.; Bartelings, M.M.; Schalij, M.J.; van der Vlugt, M.J.; van den Bosch, A.E.; Budde, R.P.J.; Roos-Hesselink, J.W.; Duijnhouwer, A.L.; van den Hoven, A.T.; et al. Coronary anatomy in Turner syndrome versus patients with isolated bicuspid aortic valves. Heart 2019, 105, 701–707. [Google Scholar] [CrossRef]
- Viuff, M.H.; Trolle, C.; Wen, J.; Jensen, J.M.; Norgaard, B.L.; Gutmark, E.J.; Gutmark-Little, I.; Mortensen, K.H.; Gravholt, C.H.; Andersen, N.H. Coronary artery anomalies in Turner Syndrome. J. Cardiovasc. Comput. Tomogr. 2016, 10, 480–484. [Google Scholar] [CrossRef]
- Zakaria, D.; Tang, X.; Bhakta, R.; ElHassan, N.O.; Prodhan, P. Chromosomal Abnormalities Affect the Surgical Outcome in Infants with Hypoplastic Left Heart Syndrome: A Large Cohort Analysis. Pediatr. Cardiol. 2018, 39, 11–18. [Google Scholar] [CrossRef]
- Phillips, H.M.; Mahendran, P.; Singh, E.; Anderson, R.H.; Chaudhry, B.; Henderson, D.J. Neural crest cells are required for correct positioning of the developing outflow cushions and pattern the arterial valve leaflets. Cardiovasc. Res. 2013, 99, 452–460. [Google Scholar] [CrossRef]
- Van Nisselrooij, A.E.L.; Lugthart, M.A.; Clur, S.A.; Linskens, I.H.; Pajkrt, E.; Rammeloo, L.A.; Rozendaal, L.; Blom, N.A.; van Lith, J.M.M.; Knegt, A.C.; et al. The prevalence of genetic diagnoses in fetuses with severe congenital heart defects. Genet. Med. 2020, 22, 1206–1214. [Google Scholar] [CrossRef] [PubMed]
- Sawada, H.; Rateri, D.L.; Moorleghen, J.J.; Majesky, M.W.; Daugherty, A. Smooth Muscle Cells Derived from Second Heart Field and Cardiac Neural Crest Reside in Spatially Distinct Domains in the Media of the Ascending Aorta-Brief Report. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1722–1726. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, K.H.; Hjerrild, B.E.; Andersen, N.H.; Sorensen, K.E.; Horlyck, A.; Pedersen, E.M.; Lundorf, E.; Christiansen, J.S.; Gravholt, C.H. Abnormalities of the major intrathoracic arteries in Turner syndrome as revealed by magnetic resonance imaging. Cardiol. Young 2010, 20, 191–200. [Google Scholar] [CrossRef]
- Kim, H.K.; Gottliebson, W.; Hor, K.; Backeljauw, P.; Gutmark-Little, I.; Salisbury, S.R.; Racadio, J.M.; Helton-Skally, K.; Fleck, R. Cardiovascular anomalies in Turner syndrome: Spectrum, prevalence, and cardiac MRI findings in a pediatric and young adult population. AJR Am. J. Roentgenol. 2011, 196, 454–460. [Google Scholar] [CrossRef]
- Ghazi Sherbaf, F.; Mohajer, B.; Ashraf-Ganjouei, A.; Mojtahed Zadeh, M.; Javinani, A.; Sanjari Moghaddam, H.; Shirin Shandiz, M.; Aarabi, M.H. Serum Insulin-Like Growth Factor-1 in Parkinson’s Disease; Study of Cerebrospinal Fluid Biomarkers and White Matter Microstructure. Front. Endocrinol. 2018, 9, 608. [Google Scholar] [CrossRef] [PubMed]
- Kruger, T.; Forkavets, O.; Veseli, K.; Lausberg, H.; Vohringer, L.; Schneider, W.; Bamberg, F.; Schlensak, C. Ascending aortic elongation and the risk of dissection. Eur. J. Cardiothorac. Surg. 2016, 50, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Costello, J.M.; Backer, C.L.; Pasquali, S.K.; Hill, K.D.; Wallace, A.S.; Jacobs, J.P.; Jacobs, M.L. Prevalence of Noncardiac and Genetic Abnormalities in Neonates Undergoing Cardiac Operations: Analysis of The Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann. Thorac. Surg. 2016, 102, 1607–1614. [Google Scholar] [CrossRef]
- Mortensen, K.H.; Hjerrild, B.E.; Stochholm, K.; Andersen, N.H.; Sorensen, K.E.; Lundorf, E.; Horlyck, A.; Pedersen, E.M.; Christiansen, J.S.; Gravholt, C.H. Dilation of the ascending aorta in Turner syndrome–a prospective cardiovascular magnetic resonance study. J. Cardiovasc. Magn. Reson. 2011, 13, 24. [Google Scholar] [CrossRef]
- Ostberg, J.E.; Donald, A.E.; Halcox, J.P.; Storry, C.; McCarthy, C.; Conway, G.S. Vasculopathy in Turner syndrome: Arterial dilatation and intimal thickening without endothelial dysfunction. J. Clin. Endocrinol. Metab. 2005, 90, 5161–5166. [Google Scholar] [CrossRef]
- Dulac, Y.; Pienkowski, C.; Abadir, S.; Tauber, M.; Acar, P. Cardiovascular abnormalities in Turner’s syndrome: What prevention? Arch. Cardiovasc. Dis. 2008, 101, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Roulot, D.; Degott, C.; Chazouilleres, O.; Oberti, F.; Cales, P.; Carbonell, N.; Benferhat, S.; Bresson-Hadni, S.; Valla, D. Vascular involvement of the liver in Turner’s syndrome. Hepatology 2004, 39, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Nathwani, N.C.; Unwin, R.; Brook, C.G.; Hindmarsh, P.C. Blood pressure and Turner syndrome. Clin. Endocrinol. 2000, 52, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Elsheikh, M.; Bird, R.; Casadei, B.; Conway, G.S.; Wass, J.A. The effect of hormone replacement therapy on cardiovascular hemodynamics in women with Turner’s syndrome. J. Clin. Endocrinol. Metab. 2000, 85, 614–618. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ounpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Stochholm, K.; Juul, S.; Juel, K.; Naeraa, R.W.; Gravholt, C.H. Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 3897–3902. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Viuff, M.H.; Brun, S.; Stochholm, K.; Andersen, N.H. Turner syndrome: Mechanisms and management. Nat. Rev. Endocrinol. 2019, 15, 601–614. [Google Scholar] [CrossRef]
- Allybocus, Z.A.; Wang, C.; Shi, H.; Wu, Q. Endocrinopathies and cardiopathies in patients with Turner syndrome. Climacteric 2018, 21, 536–541. [Google Scholar] [CrossRef]
- Sachdev, V.; Matura, L.A.; Sidenko, S.; Ho, V.B.; Arai, A.E.; Rosing, D.R.; Bondy, C.A. Aortic valve disease in Turner syndrome. J. Am. Coll. Cardiol. 2008, 51, 1904–1909. [Google Scholar] [CrossRef]
- Shah, S.Y.; Higgins, A.; Desai, M.Y. Bicuspid aortic valve: Basics and beyond. Cleve Clin. J. Med. 2018, 85, 779–784. [Google Scholar] [CrossRef]
- Mortensen, K.H.; Gopalan, D.; Norgaard, B.L.; Andersen, N.H.; Gravholt, C.H. Multimodality cardiac imaging in Turner syndrome. Cardiol. Young 2016, 26, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Aslam, S.; Khairy, P.; Shohoudi, A.; Mercier, L.A.; Dore, A.; Marcotte, F.; Miro, J.; Avila-Alonso, P.; Ibrahim, R.; Asgar, A.; et al. Shone Complex: An Under-recognized Congenital Heart Disease with Substantial Morbidity in Adulthood. Can. J. Cardiol. 2017, 33, 253–259. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Landin-Wilhelmsen, K.; Stochholm, K.; Hjerrild, B.E.; Ledet, T.; Djurhuus, C.B.; Sylven, L.; Baandrup, U.; Kristensen, B.O.; Christiansen, J.S. Clinical and epidemiological description of aortic dissection in Turner’s syndrome. Cardiol. Young 2006, 16, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Silberbach, M. Aortic dissection in Turner’s syndrome: A “perfect storm”? Cardiol. Young 2006, 16, 428–429. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, K.H.; Andersen, N.H.; Gravholt, C.H. Cardiovascular phenotype in Turner syndrome–Integrating cardiology, genetics, and endocrinology. Endocr. Rev. 2012, 33, 677–714. [Google Scholar] [CrossRef] [PubMed]
- Bondy, C.A.; Turner Syndrome Study, G. Care of girls and women with Turner syndrome: A guideline of the Turner Syndrome Study Group. J. Clin. Endocrinol. Metab. 2007, 92, 10–25. [Google Scholar] [CrossRef]
- Choi, Y.; Hoffman, J.; Alarcon, L.; Pfau, J.; Bolourchi, M. Neonatal arrhythmias in Turner syndrome: A case report and review of the literature. Eur. Heart J. Case Rep. 2021, 5, ytab160. [Google Scholar] [CrossRef]
- Corbitt, H.; Morris, S.A.; Gravholt, C.H.; Mortensen, K.H.; Tippner-Hedges, R.; Silberbach, M.; Maslen, C.L.; Gen, T.A.C.R.I. TIMP3 and TIMP1 are risk genes for bicuspid aortic valve and aortopathy in Turner syndrome. PLoS Genet. 2018, 14, e1007692. [Google Scholar] [CrossRef]
- Rabkin, S.W. Differential expression of MMP-2, MMP-9 and TIMP proteins in thoracic aortic aneurysm–comparison with and without bicuspid aortic valve: A meta-analysis. Vasa 2014, 43, 433–442. [Google Scholar] [CrossRef]
- Trolle, C.; Nielsen, M.M.; Skakkebaek, A.; Lamy, P.; Vang, S.; Hedegaard, J.; Nordentoft, I.; Orntoft, T.F.; Pedersen, J.S.; Gravholt, C.H. Widespread DNA hypomethylation and differential gene expression in Turner syndrome. Sci. Rep. 2016, 6, 34220. [Google Scholar] [CrossRef]
- Albareda, M.M.; Gallego, A.; Enriquez, J.; Rodriguez, J.L.; Webb, S.M. Biochemical liver abnormalities in Turner’s syndrome. Eur. J. Gastroenterol. Hepatol. 1999, 11, 1037–1039. [Google Scholar] [CrossRef] [PubMed]
- Floreani, A.; Molaro, M.; Baragiotta, A.; Naccarato, R. Chronic cholestasis associated with Turner’s syndrome. Digestion 1999, 60, 587–589. [Google Scholar] [CrossRef] [PubMed]
- Salerno, M.; Di Maio, S.; Gasparini, N.; Rizzo, M.; Ferri, P.; Vajro, P. Liver abnormalities in Turner syndrome. Eur. J. Pediatr. 1999, 158, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Gardner, L.I. Letter: Intrahepatic bile stasis in 45,X Turner’s syndrome. N. Engl. J. Med. 1974, 290, 406. [Google Scholar] [CrossRef]
- Krivosheev, A.B. Development of liver cirrhosis in a female patient with Shereshevskii-Turner syndrome. Klin. Med. 1990, 68, 95–96. [Google Scholar]
- Garavelli, L.; Donadio, A.; Banchini, G.; Fornaciari, G.; Plancher, A.C.; Franchi, F.; Gardini, G. Liver abnormalities and portal hypertension in Ullrich-Turner syndrome. Am. J. Med. Genet. 1998, 80, 180–182. [Google Scholar] [CrossRef]
- Singh, I.; Noel, G.; Barker, J.M.; Chatfield, K.C.; Furniss, A.; Khanna, A.D.; Nokoff, N.J.; Patel, S.; Pyle, L.; Nahata, L.; et al. Hepatic abnormalities in youth with Turner syndrome. Liver Int. 2022, 42, 2237–2246. [Google Scholar] [CrossRef]
- Machlab, S.; Miquel, M.; Volta, T.; Escoda, M.R.; Vergara, M. Turner syndrome as a cause of liver cirrhosis. Gastroenterol. Hepatol. 2018, 41, 308–309. [Google Scholar] [CrossRef]
- El-Mansoury, M.; Berntorp, K.; Bryman, I.; Hanson, C.; Innala, E.; Karlsson, A.; Landin-Wilhelmsen, K. Elevated liver enzymes in Turner syndrome during a 5-year follow-up study. Clin. Endocrinol. 2008, 68, 485–490. [Google Scholar] [CrossRef]
- Larizza, D.; Locatelli, M.; Vitali, L.; Vigano, C.; Calcaterra, V.; Tinelli, C.; Sommaruga, M.G.; Bozzini, A.; Campani, R.; Severi, F. Serum liver enzymes in Turner syndrome. Eur. J. Pediatr. 2000, 159, 143–148. [Google Scholar] [CrossRef]
- Blackett, P.R.; Rundle, A.C.; Frane, J.; Blethen, S.L. Body mass index (BMI) in Turner Syndrome before and during growth hormone (GH) therapy. Int. J. Obes. Relat. Metab. Disord. 2000, 24, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Wojcik, M.; Ruszala, A.; Janus, D.; Starzyk, J.B. Liver Biochemical Abnormalities in Adolescent Patients with Turner Syndrome. J. Clin. Res. Pediatr. Endocrinol. 2019, 11, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Ratziu, V.; Giral, P.; Charlotte, F.; Bruckert, E.; Thibault, V.; Theodorou, I.; Khalil, L.; Turpin, G.; Opolon, P.; Poynard, T. Liver fibrosis in overweight patients. Gastroenterology 2000, 118, 1117–1123. [Google Scholar] [CrossRef] [PubMed]
- Roulot, D. Liver involvement in Turner syndrome. Liver Int. 2013, 33, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, S.; Sakamoto, S.; Honda, M.; Hayashida, S.; Yamamoto, H.; Mikami, Y.; Inomata, Y. Liver transplantation for a patient with Turner syndrome presenting severe portal hypertension: A case report and literature review. Surg. Case Rep. 2016, 2, 68. [Google Scholar] [CrossRef]
- Viuff, M.H.; Stochholm, K.; Gronbaek, H.; Berglund, A.; Juul, S.; Gravholt, C.H. Increased occurrence of liver and gastrointestinal diseases and anaemia in women with Turner syndrome–a nationwide cohort study. Aliment Pharmacol. Ther. 2021, 53, 821–829. [Google Scholar] [CrossRef]
- Yamaguti, D.C.; Patricio, F.R. Morphometrical and immunohistochemical study of intrahepatic bile ducts in biliary atresia. Eur. J. Gastroenterol. Hepatol. 2011, 23, 759–765. [Google Scholar] [CrossRef]
- Elizondo-Montemayor, L.; Ugalde-Casas, P.A.; Lam-Franco, L.; Bustamante-Careaga, H.; Serrano-Gonzalez, M.; Gutierrez, N.G.; Martinez, U. Association of ALT and the metabolic syndrome among Mexican children. Obes. Res. Clin. Pract. 2014, 8, e79–e87. [Google Scholar] [CrossRef]
- Bianchi, I.; Lleo, A.; Bernuzzi, F.; Caliari, L.; Smyk, D.S.; Invernizzi, P. The X-factor in primary biliary cirrhosis: Monosomy X and xenobiotics. Auto Immun. Highlights 2012, 3, 127–132. [Google Scholar] [CrossRef]
- Milkiewicz, P.; Heathcote, J. Primary biliary cirrhosis in a patient with Turner syndrome. Can. J. Gastroenterol. 2005, 19, 631–633. [Google Scholar] [CrossRef]
- Sybert, V.P.; McCauley, E. Turner’s syndrome. N. Engl. J. Med. 2004, 351, 1227–1238. [Google Scholar] [CrossRef] [PubMed]
- Izumita, Y.; Nishigaki, S.; Satoh, M.; Takubo, N.; Numakura, C.; Takahashi, I.; Soneda, S.; Abe, Y.; Kamasaki, H.; Ohtsu, Y.; et al. Retrospective study of the renal function using estimated glomerular filtration rate and congenital anomalies of the kidney-urinary tract in pediatric Turner syndrome. Congenit. Anom. 2020, 60, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Gravholt, C.H.; Andersen, N.H.; Conway, G.S.; Dekkers, O.M.; Geffner, M.E.; Klein, K.O.; Lin, A.E.; Mauras, N.; Quigley, C.A.; Rubin, K.; et al. Clinical practice guidelines for the care of girls and women with Turner syndrome: Proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur. J. Endocrinol. 2017, 177, G1–G70. [Google Scholar] [CrossRef] [PubMed]
- Fanos, V.; Schena, S.; Dal Moro, A.; Portuese, A.; Antoniazzi, F. Multicystic kidney dysplasia and Turner syndrome: Two cases and a literature review. Pediatr. Nephrol. 2000, 14, 754–757. [Google Scholar] [CrossRef] [PubMed]
- Pritti, K.; Mishra, V.; Patel, H. A Rare Case of Mosaic Ring Turner Syndrome with Horseshoe Kidney. J. Hum. Reprod. Sci. 2022, 15, 318–320. [Google Scholar] [CrossRef] [PubMed]
- Bilge, I.; Kayserili, H.; Emre, S.; Nayir, A.; Sirin, A.; Tukel, T.; Bas, F.; Kilic, G.; Basaran, S.; Gunoz, H.; et al. Frequency of renal malformations in Turner syndrome: Analysis of 82 Turkish children. Pediatr. Nephrol. 2000, 14, 1111–1114. [Google Scholar] [CrossRef]
- Ogawa, T.; Takizawa, F.; Mukoyama, Y.; Ogawa, A.; Ito, J. Renal morphology and function from childhood to adulthood in Turner syndrome. Clin. Exp. Nephrol. 2021, 25, 633–640. [Google Scholar] [CrossRef]
- Pasquali, L.; d’Annunzio, G.; Gastaldi, R.; Di Battista, E.; Calcaterra, V.; Larizza, D.; Lorini, R.; D’Amato, E. Collectrin gene screening in Turner syndrome patients with kidney malformation. J. Genet. 2009, 88, 105–108. [Google Scholar] [CrossRef]
- Horita, S.; Simsek, E.; Simsek, T.; Yildirim, N.; Ishiura, H.; Nakamura, M.; Satoh, N.; Suzuki, A.; Tsukada, H.; Mizuno, T.; et al. SLC4A4 compound heterozygous mutations in exon-intron boundary regions presenting with severe proximal renal tubular acidosis and extrarenal symptoms coexisting with Turner’s syndrome: A case report. BMC Med. Genet. 2018, 19, 103. [Google Scholar] [CrossRef]
- Holroyd, C.R.; Davies, J.H.; Taylor, P.; Jameson, K.; Rivett, C.; Cooper, C.; Dennison, E.M. Reduced cortical bone density with normal trabecular bone density in girls with Turner syndrome. Osteoporos Int. 2010, 21, 2093–2099. [Google Scholar] [CrossRef]
- Wasserman, H.; Backeljauw, P.F.; Khoury, J.C.; Kalkwarf, H.J.; Gordon, C.M. Bone fragility in Turner syndrome: Fracture prevalence and risk factors determined by a national patient survey. Clin. Endocrinol. 2018, 89, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Bakalov, V.K.; Chen, M.L.; Baron, J.; Hanton, L.B.; Reynolds, J.C.; Stratakis, C.A.; Axelrod, L.E.; Bondy, C.A. Bone mineral density and fractures in Turner syndrome. Am. J. Med. 2003, 115, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Soucek, O.; Lebl, J.; Snajderova, M.; Kolouskova, S.; Rocek, M.; Hlavka, Z.; Cinek, O.; Rittweger, J.; Sumnik, Z. Bone geometry and volumetric bone mineral density in girls with Turner syndrome of different pubertal stages. Clin. Endocrinol. 2011, 74, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Bakalov, V.K.; Axelrod, L.; Baron, J.; Hanton, L.; Nelson, L.M.; Reynolds, J.C.; Hill, S.; Troendle, J.; Bondy, C.A. Selective reduction in cortical bone mineral density in turner syndrome independent of ovarian hormone deficiency. J. Clin. Endocrinol. Metab. 2003, 88, 5717–5722. [Google Scholar] [CrossRef]
- Even, L.; Bronstein, V.; Hochberg, Z. Bone maturation in girls with Turner’s syndrome. Eur. J. Endocrinol. 1998, 138, 59–62. [Google Scholar] [CrossRef]
- Cintron, D.; Rodriguez-Gutierrez, R.; Serrano, V.; Latortue-Albino, P.; Erwin, P.J.; Murad, M.H. Effect of estrogen replacement therapy on bone and cardiovascular outcomes in women with turner syndrome: A systematic review and meta-analysis. Endocrine 2017, 55, 366–375. [Google Scholar] [CrossRef]
- Gussinye, M.; Terrades, P.; Yeste, D.; Vicens-Calvet, E.; Carrascosa, A. Low areal bone mineral density values in adolescents and young adult turner syndrome patients increase after long-term transdermal estradiol therapy. Horm. Res. 2000, 54, 131–135. [Google Scholar] [CrossRef]
- Elsheikh, M.; Conway, G.S.; Wass, J.A. Medical problems in adult women with Turner’s syndrome. Ann. Med. 1999, 31, 99–105. [Google Scholar] [CrossRef]
- Saenger, P.; Wikland, K.A.; Conway, G.S.; Davenport, M.; Gravholt, C.H.; Hintz, R.; Hovatta, O.; Hultcrantz, M.; Landin-Wilhelmsen, K.; Lin, A.; et al. Recommendations for the diagnosis and management of Turner syndrome. J. Clin. Endocrinol. Metab. 2001, 86, 3061–3069. [Google Scholar] [CrossRef]
- Landin-Wilhelmsen, K.; Bryman, I.; Windh, M.; Wilhelmsen, L. Osteoporosis and fractures in Turner syndrome-importance of growth promoting and oestrogen therapy. Clin. Endocrinol. 1999, 51, 497–502. [Google Scholar] [CrossRef]
- Elsheikh, M.; Dunger, D.B.; Conway, G.S.; Wass, J.A. Turner’s syndrome in adulthood. Endocr. Rev. 2002, 23, 120–140. [Google Scholar] [CrossRef] [PubMed]
- Makishima, T.; King, K.; Brewer, C.C.; Zalewski, C.K.; Butman, J.; Bakalov, V.K.; Bondy, C.; Griffith, A.J. Otolaryngologic markers for the early diagnosis of Turner syndrome. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Leheup, B.P.; Perrin, P.; Perrin, C.; Pierson, M. Otologic signs and early diagnosis of Turner syndrome. Reevaluation of 30 cases. J. Genet. Hum. 1988, 36, 315–321. [Google Scholar] [PubMed]
- Parkin, M.; Walker, P. Hearing loss in Turner syndrome. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, N.; Tanaka, T.; Taiji, H.; Horikawa, R.; Naiki, Y.; Morimoto, Y.; Kawashiro, N. Hearing loss in Turner syndrome. J. Pediatr. 2006, 149, 697–701. [Google Scholar] [CrossRef]
- Palmisano, B.T.; Zhu, L.; Stafford, J.M. Role of Estrogens in the Regulation of Liver Lipid Metabolism. Adv. Exp. Med. Biol. 2017, 1043, 227–256. [Google Scholar] [CrossRef]
- Brady, C.W. Liver disease in menopause. World J. Gastroenterol. 2015, 21, 7613–7620. [Google Scholar] [CrossRef]
- Florio, A.A.; Graubard, B.I.; Yang, B.; Thistle, J.E.; Bradley, M.C.; McGlynn, K.A.; Petrick, J.L. Oophorectomy and risk of non-alcoholic fatty liver disease and primary liver cancer in the Clinical Practice Research Datalink. Eur. J. Epidemiol. 2019, 34, 871–878. [Google Scholar] [CrossRef]
- Elsheikh, M.; Hodgson, H.J.; Wass, J.A.; Conway, G.S. Hormone replacement therapy may improve hepatic function in women with Turner’s syndrome. Clin. Endocrinol. 2001, 55, 227–231. [Google Scholar] [CrossRef]
- Liebe, R.; Esposito, I.; Bock, H.H.; Vom Dahl, S.; Stindt, J.; Baumann, U.; Luedde, T.; Keitel, V. Diagnosis and management of secondary causes of steatohepatitis. J. Hepatol. 2021, 74, 1455–1471. [Google Scholar] [CrossRef]
- Egli, F.; Stalder, G. Malformations of kidney and urinary tract in common chromosomal aberrations. I. Clinical studies. Humangenetik 1973, 18, 1–15. [Google Scholar] [CrossRef]
- Gregoir, W. Conservative Surgery in Horseshoe-Kidney. Urol. Int. 1963, 16, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Farooqui, A.; Tazyeen, S.; Ahmed, M.M.; Alam, A.; Ali, S.; Malik, M.Z.; Ali, S.; Ishrat, R. Assessment of the key regulatory genes and their Interologs for Turner Syndrome employing network approach. Sci. Rep. 2018, 8, 10091. [Google Scholar] [CrossRef] [PubMed]
- Pajenda, S.; Wagner, L.; Gerges, D.; Herkner, H.; Tevdoradze, T.; Mechtler, K.; Schmidt, A.; Winnicki, W. Urinary Collectrin (TMEM27) as Novel Marker for Acute Kidney Injury. Life 2022, 12, 1391. [Google Scholar] [CrossRef]
- Gravholt, C.H. Aspects of the treatment of Turner syndrome. Expert Opin. Pharmacother. 2001, 2, 1633–1647. [Google Scholar] [CrossRef] [PubMed]
- Watkin, P. The age of onset and progression of sensorineural hearing loss in Turner’s syndrome and its relationship to SHOX deficiency: A case report. Hear. Balance Commun. 2013, 11, 39–46. [Google Scholar] [CrossRef]
- Cameron-Pimblett, A.; Davies, M.C.; Burt, E.; Talaulikar, V.S.; La Rosa, C.; King, T.F.J.; Conway, G.S. Effects of Estrogen Therapies on Outcomes in Turner Syndrome: Assessment of Induction of Puberty and Adult Estrogen Use. J. Clin. Endocrinol. Metab. 2019, 104, 2820–2826. [Google Scholar] [CrossRef]
- Itonaga, T.; Koga, E.; Nishigaki, S.; Kawai, M.; Sakakibara, H.; Hasegawa, Y. A retrospective multicenter study of bone mineral density in adolescents and adults with Turner syndrome in Japan. Endocr. J. 2020, 67, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.H.; Wong, P.; Strauss, B.J.; Jones, G.; Ebeling, P.R.; Milat, F.; Vincent, A. Delay in estrogen commencement is associated with lower bone mineral density in Turner syndrome. Climacteric 2017, 20, 436–441. [Google Scholar] [CrossRef]
- Nishigaki, S.; Itonaga, T.; Hasegawa, Y.; Kawai, M. Starting age of oestrogen-progestin therapy is negatively associated with bone mineral density in young adults with Turner syndrome independent of age and body mass index. Clin. Endocrinol. 2021, 95, 84–91. [Google Scholar] [CrossRef]
- Nakamura, T.; Tsuburai, T.; Tokinaga, A.; Nakajima, I.; Kitayama, R.; Imai, Y.; Nagata, T.; Yoshida, H.; Hirahara, F.; Sakakibara, H. Efficacy of estrogen replacement therapy (ERT) on uterine growth and acquisition of bone mass in patients with Turner syndrome. Endocr. J. 2015, 62, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Ranke, M.B.; Grauer, M.L. Adult height in Turner syndrome: Results of a multinational survey 1993. Horm. Res. 1994, 42, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Isojima, T.; Yokoya, S. Growth in girls with Turner syndrome. Front. Endocrinol. 2022, 13, 1068128. [Google Scholar] [CrossRef] [PubMed]
- Helena Mangs, A.; Morris, B.J. The Human Pseudoautosomal Region (PAR): Origin, Function and Future. Curr. Genom. 2007, 8, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Backeljauw, P.; Chernausek, S.D.; Gravholt, C.H.; Kruszka, P. Turner syndrome. In Sperling Pediatric Endocrinology; Elsevier: Amsterdam, The Netherlands, 2021; pp. 627–660. [Google Scholar]
- Fedor, I.; Zold, E.; Barta, Z. Liver Abnormalities in Turner Syndrome: The Importance of Estrogen Replacement. J. Endocr. Soc. 2022, 6, bvac124. [Google Scholar] [CrossRef]
- Carel, J.C.; Mathivon, L.; Gendrel, C.; Ducret, J.P.; Chaussain, J.L. Near normalization of final height with adapted doses of growth hormone in Turner’s syndrome. J. Clin. Endocrinol. Metab. 1998, 83, 1462–1466. [Google Scholar] [CrossRef]
- Sas, T.C.; de Muinck Keizer-Schrama, S.M.; Stijnen, T.; Jansen, M.; Otten, B.J.; Hoorweg-Nijman, J.J.; Vulsma, T.; Massa, G.G.; Rouwe, C.W.; Reeser, H.M.; et al. Normalization of height in girls with Turner syndrome after long-term growth hormone treatment: Results of a randomized dose-response trial. J. Clin. Endocrinol. Metab. 1999, 84, 4607–4612. [Google Scholar] [CrossRef]
- Van Pareren, Y.K.; de Muinck Keizer-Schrama, S.M.; Stijnen, T.; Sas, T.C.; Jansen, M.; Otten, B.J.; Hoorweg-Nijman, J.J.; Vulsma, T.; Stokvis-Brantsma, W.H.; Rouwe, C.W.; et al. Final height in girls with turner syndrome after long-term growth hormone treatment in three dosages and low dose estrogens. J. Clin. Endocrinol. Metab. 2003, 88, 1119–1125. [Google Scholar] [CrossRef] [PubMed]
- Reiss, A.L.; Mazzocco, M.M.; Greenlaw, R.; Freund, L.S.; Ross, J.L. Neurodevelopmental effects of X monosomy: A volumetric imaging study. Ann. Neurol. 1995, 38, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.G.; DeCarli, C.; Daly, E.; Haxby, J.V.; Allen, G.; White, B.J.; McIntosh, A.R.; Powell, C.M.; Horwitz, B.; Rapoport, S.I.; et al. X-chromosome effects on female brain: A magnetic resonance imaging study of Turner’s syndrome. Lancet 1993, 342, 1197–1200. [Google Scholar] [CrossRef] [PubMed]
- Reiss, A.L.; Freund, L.; Plotnick, L.; Baumgardner, T.; Green, K.; Sozer, A.C.; Reader, M.; Boehm, C.; Denckla, M.B. The effects of X monosomy on brain development: Monozygotic twins discordant for Turner’s syndrome. Ann. Neurol. 1993, 34, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Kesler, S.R.; Blasey, C.M.; Brown, W.E.; Yankowitz, J.; Zeng, S.M.; Bender, B.G.; Reiss, A.L. Effects of X-monosomy and X-linked imprinting on superior temporal gyrus morphology in Turner syndrome. Biol. Psychiatry 2003, 54, 636–646. [Google Scholar] [CrossRef]
- Lepage, J.F.; Mazaika, P.K.; Hong, D.S.; Raman, M.; Reiss, A.L. Cortical brain morphology in young, estrogen-naive, and adolescent, estrogen-treated girls with Turner syndrome. Cereb. Cortex 2013, 23, 2159–2168. [Google Scholar] [CrossRef]
- Marzelli, M.J.; Hoeft, F.; Hong, D.S.; Reiss, A.L. Neuroanatomical spatial patterns in Turner syndrome. Neuroimage 2011, 55, 439–447. [Google Scholar] [CrossRef] [PubMed]
- Knickmeyer, R.C. Turner syndrome: Advances in understanding altered cognition, brain structure and function. Curr. Opin. Neurol. 2012, 25, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Brown, W.E.; Kesler, S.R.; Eliez, S.; Warsofsky, I.S.; Haberecht, M.; Patwardhan, A.; Ross, J.L.; Neely, E.K.; Zeng, S.M.; Yankowitz, J.; et al. Brain development in Turner syndrome: A magnetic resonance imaging study. Psychiatry Res. 2002, 116, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Kesler, S.R.; Garrett, A.; Bender, B.; Yankowitz, J.; Zeng, S.M.; Reiss, A.L. Amygdala and hippocampal volumes in Turner syndrome: A high-resolution MRI study of X-monosomy. Neuropsychologia 2004, 42, 1971–1978. [Google Scholar] [CrossRef]
- Cutter, W.J.; Daly, E.M.; Robertson, D.M.; Chitnis, X.A.; van Amelsvoort, T.A.; Simmons, A.; Ng, V.W.; Williams, B.S.; Shaw, P.; Conway, G.S.; et al. Influence of X chromosome and hormones on human brain development: A magnetic resonance imaging and proton magnetic resonance spectroscopy study of Turner syndrome. Biol. Psychiatry 2006, 59, 273–283. [Google Scholar] [CrossRef]
- Davenport, M.L.; Cornea, E.; Xia, K.; Crowley, J.J.; Halvorsen, M.W.; Goldman, B.D.; Reinhartsen, D.; DeRamus, M.; Pretzel, R.; Styner, M.; et al. Altered Brain Structure in Infants with Turner Syndrome. Cereb. Cortex 2020, 30, 587–596. [Google Scholar] [CrossRef]
- Molko, N.; Cachia, A.; Riviere, D.; Mangin, J.F.; Bruandet, M.; LeBihan, D.; Cohen, L.; Dehaene, S. Brain anatomy in Turner syndrome: Evidence for impaired social and spatial-numerical networks. Cereb. Cortex 2004, 14, 840–850. [Google Scholar] [CrossRef]
- Brown, W.E.; Kesler, S.R.; Eliez, S.; Warsofsky, I.S.; Haberecht, M.; Reiss, A.L. A volumetric study of parietal lobe subregions in Turner syndrome. Dev. Med. Child. Neurol. 2004, 46, 607–609. [Google Scholar] [CrossRef]
- Ross, J.; Zinn, A.; McCauley, E. Neurodevelopmental and psychosocial aspects of Turner syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 2000, 6, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Rovet, J.F. The psychoeducational characteristics of children with Turner syndrome. J. Learn Disabil. 1993, 26, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.; Klonoff, H.; Hayden, M. Regional cerebral glucose metabolism in Turner syndrome. Can. J. Neurol. Sci. 1990, 17, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.G.; Mentis, M.J.; Pietrini, P.; Grady, C.; Daly, E.; Haxby, J.V.; De La Granja, M.; Allen, G.; Largay, K.; White, B.J.; et al. A PET study of Turner’s syndrome: Effects of sex steroids and the X chromosome on brain. Biol. Psychiatry 1997, 41, 285–298. [Google Scholar] [CrossRef] [PubMed]
- Kuntsi, J.; Skuse, D.; Elgar, K.; Morris, E.; Turner, C. Ring-X chromosomes: Their cognitive and behavioural phenotype. Ann. Hum. Genet. 2000, 64, 295–305. [Google Scholar] [CrossRef]
- Walter, E.; Mazaika, P.K.; Reiss, A.L. Insights into brain development from neurogenetic syndromes: Evidence from fragile X syndrome, Williams syndrome, Turner syndrome and velocardiofacial syndrome. Neuroscience 2009, 164, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Good, C.D.; Lawrence, K.; Thomas, N.S.; Price, C.J.; Ashburner, J.; Friston, K.J.; Frackowiak, R.S.; Oreland, L.; Skuse, D.H. Dosage-sensitive X-linked locus influences the development of amygdala and orbitofrontal cortex, and fear recognition in humans. Brain 2003, 126, 2431–2446. [Google Scholar] [CrossRef]
- Molko, N.; Cachia, A.; Riviere, D.; Mangin, J.F.; Bruandet, M.; Le Bihan, D.; Cohen, L.; Dehaene, S. Functional and structural alterations of the intraparietal sulcus in a developmental dyscalculia of genetic origin. Neuron 2003, 40, 847–858. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R., Jr.; Rohrbaugh, J.W.; Ross, J.L. Altered brain development in Turner’s syndrome: An event-related potential study. Neurology 1993, 43, 801–808. [Google Scholar] [CrossRef]
- Tsuboi, T.; Nielsen, J.; Nagayama, I. Turner’s syndrome: A qualitative and quantitative analysis of EEG background activity. Hum. Genet. 1988, 78, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Skuse, D.H.; James, R.S.; Bishop, D.V.; Coppin, B.; Dalton, P.; Aamodt-Leeper, G.; Bacarese-Hamilton, M.; Creswell, C.; McGurk, R.; Jacobs, P.A. Evidence from Turner’s syndrome of an imprinted X-linked locus affecting cognitive function. Nature 1997, 387, 705–708. [Google Scholar] [CrossRef] [PubMed]
- Skuse, D.H. Imprinting, the X-chromosome, and the male brain: Explaining sex differences in the liability to autism. Pediatr. Res. 2000, 47, 9–16. [Google Scholar] [CrossRef]
- Heard, E.; Chaumeil, J.; Masui, O.; Okamoto, I. Mammalian X-chromosome inactivation: An epigenetics paradigm. Cold Spring Harb. Symp. Quant. Biol. 2004, 69, 89–102. [Google Scholar] [CrossRef]
- Sahakyan, A.; Kim, R.; Chronis, C.; Sabri, S.; Bonora, G.; Theunissen, T.W.; Kuoy, E.; Langerman, J.; Clark, A.T.; Jaenisch, R.; et al. Human Naive Pluripotent Stem Cells Model X Chromosome Dampening and X Inactivation. Cell Stem. Cell 2017, 20, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Berletch, J.B.; Yang, F.; Disteche, C.M. Escape from X inactivation in mice and humans. Genome. Biol. 2010, 11, 213. [Google Scholar] [CrossRef] [PubMed]
- Berletch, J.B.; Yang, F.; Xu, J.; Carrel, L.; Disteche, C.M. Genes that escape from X inactivation. Hum. Genet. 2011, 130, 237–245. [Google Scholar] [CrossRef]
- Laupacis, A.; Bourne, R.; Rorabeck, C.; Feeny, D.; Tugwell, P.; Wong, C. Comparison of total hip arthroplasty performed with and without cement: A randomized trial. J. Bone Joint Surg. Am. 2002, 84, 1823–1828. [Google Scholar] [CrossRef]
- Miyake, N.; Mizuno, S.; Okamoto, N.; Ohashi, H.; Shiina, M.; Ogata, K.; Tsurusaki, Y.; Nakashima, M.; Saitsu, H.; Niikawa, N.; et al. KDM6A point mutations cause Kabuki syndrome. Hum. Mutat. 2013, 34, 108–110. [Google Scholar] [CrossRef]
- Alvarez-Nava, F.; Lanes, R. Epigenetics in Turner syndrome. Clin. Epigenetics 2018, 10, 45. [Google Scholar] [CrossRef]
- Probst, F.J.; Cooper, M.L.; Cheung, S.W.; Justice, M.J. Genotype, phenotype, and karyotype correlation in the XO mouse model of Turner Syndrome. J. Hered. 2008, 99, 512–517. [Google Scholar] [CrossRef] [PubMed]
| Gene | Location | Expression in TS | Associated Phenotype | Reference |
|---|---|---|---|---|
| SHOX | Xp22.33 and Y chromosome (PAR1) | Decreased expression | Short stature, Madelung wrist deformity, Intellectual disabilities | [9,10,11,12,13] |
| ARSD, ARSE, ARSF | Xp22.3 | Loss owing to contiguous gene deletion syndrome | Chondrodysplasia punctata | [14,15,16] |
| STS | Xp22.31 | Loss owing to contiguous gene deletion syndrome | X-linked ichthyosis | [13,14,15,16] |
| GPR143 | Xp22.2 | Loss owing to contiguous gene deletion syndrome | Ocular albinism type I | [14,15,16] |
| ANOS1 | Xp23.3 | Loss owing to contiguous gene deletion syndrome | Kallmann syndrome | [14,15,16] |
| RPS4X | Xq13.1 | Downregulation | N/A | [13,17,18,19] |
| CD99 | X and Y chromosomes (PAR1) | Downregulation | N/A | [13,20] |
| CSF2RA | X and Y chromosomes (PAR1) | Downregulation | N/A | [13,20,21,22] |
| MYL9 | 20q11.23 | Downregulated | N/A | [20] |
| MYLPF | 16p11.2 | Downregulated | N/A | [20] |
| IGFBP2 | 2q35 | Downregulated | N/A | [20] |
| Organ | Symptom | Prevalence Rate | Reference |
|---|---|---|---|
| Liver | Steatosis | 33.3% of all patients with TS (no changes in liver structure) | [72,96,98] |
| Steatohepatitis | 4.8–12% of all patients with TS | [103] | |
| Liver cirrhosis | 6.7–16.5% of all patients with TS (20% of patients with liver structural changes) | [72,95,98,104,105,106] | |
| Bile stasis, biliary involvement | 43.7% of all patients with TS | [91,92,94,107] | |
| Nodular regenerative hyperplasia (NRH) | 33% of all patients with TS (60% of liver structure change group) | [72,98,104] | |
| Liver enzyme elevation (alanine aminotransferase and aspartate aminotransferase) | 20% of all patients with TS | [93,97,100,103,108] | |
| Higher total cholesterol, triglycerides, and apolipoproteins a and b | 59% of all patients with TS (36% of patients were initially high, 23% of patients were added as a result of follow-up for 5 years) | [99] | |
| Non-alcoholic fatty liver disease (NAFLD) | 36.7% of all patients with TS (64.7% of group patients without changes in liver structure) | [72,96] | |
| Moderate portal fibrosis | 50% of all patients with TS (88.2% of group patients without changes in liver structure) | [72] | |
| Periductal fibrosis | 70% of all patients with TS (80% of patients in the liver structure change group, 76.4% of the group without liver structure change) | [72] | |
| Bile duct abnormalities | 66.6% of all patients with TS (95.2% of patients with periductal fibrosis) | [72] | |
| Portal hypertension | 13% of all patients with TS (40% of liver structure change group patients) | [72,96] | |
| Aortic bicuspid, coarctation, stenosis | 20% of all patients with TS (50% of liver structure change group patients) | [72] | |
| Multiple focal nodular hyperplasia (FNH) | 6.7% of all patients with TS (20% of patients with liver structural changes) | [72,104] | |
| Primary sclerosing cholangitis (PSC) | N/A | [107,109] | |
| Primary biliary cirrhosis (PBC) | 78% of all patients with TS | [109,110] | |
| Kidney | Horseshoe kidneys of different sizes | 7–29% (13.5% of patients with TS had renal abnormalities) | [111,112,113,114,115,116,117] |
| Renal aplasia | 3% of all patients with TS | [113] | |
| Simple cilia and cysts | 16% of all patients with TS | [118] | |
| Hydronephrosis | 17.5% of all patients with TS | [117] | |
| Urinary tract infections and kidney stones | N/A | [116,119] | |
| Skeletal | Reduced bone density | N/A | [120,121,122,123,124] |
| Delayed bone formation | N/A | [122,125] | |
| Osteopenia or osteoporosis | N/A | [126,127,128,129,130] | |
| Face skeletal malformations (including micrognathia, outer corners of the eyes and epicanthic folds, high-arched palate, and low-set ears) | More than 60% of all patients with TS | [131,132] | |
| Hearing loss | 63–70% of all patients with TS | [132,133,134,135] | |
| Sensorineural hearing loss (SNHL) | 9–63% of all patients with TS | [132,134] | |
| Middle ear disease | 91% of all patients with TS | [134] |
| Abnormal Structure | Site of Occurrence | Reference | |
|---|---|---|---|
| More than normal controls | Gray matter | Right superior temporal gyrus | [163] |
| Between the cerebellum | [167] | ||
| Inferior temporal | [164] | ||
| Superior temporal | [164] | ||
| Subcortical | [164] | ||
| Left amygdala | [168] | ||
| White matter | Left superior temporal gyrus | [163] | |
| Temporal lobes | [169] | ||
| Superior temporal | [164] | ||
| Superior frontal | [164] | ||
| Precentral | [164] | ||
| Right parahippocampal cortex | [170] | ||
| Right superior temporal gyrus | [170] | ||
| Left Heschl’s gyrus | [170] | ||
| Left middle and superior temporal gyri | [165] | ||
| Lesser than normal control | Gray matter | Symmetrical location of the right intraparietal sulcus | [171] |
| Precentral | [165,166] | ||
| Caudate nuclei | [169] | ||
| Postcentral | [164,165] | ||
| Supramarginal gyri | [165] | ||
| Cuneus | [164] | ||
| Lingual gyrus | [164] | ||
| Pericalcarine | [164] | ||
| Superior parietal | [164] | ||
| Rostral anterior portion of the cingulate cortex | [164] | ||
| White matter | Occipital lobe | [167] | |
| Pericalcarine | [164] | ||
| Postcentral | [164] | ||
| Precuneus | [164] | ||
| Entorhinal cortex | [164] | ||
| Pars opercularis | [164] | ||
| Frontal pole | [164] | ||
| Rostral anterior portion of the cingulate cortex | [164] | ||
| Surface area | [164] | ||
| Average cortical thickness | [164] | ||
| Parietal lobe | [164,167,172] | ||
| Hippocampus | [161,168] | ||
| Caudate | [161] | ||
| Lenticular | [161] | ||
| Thalamic nuclei | [161] | ||
| Parieto-occipital brain matter | [161] | ||
| Superior parietal | [172] | ||
| Postcentral gyri | [172] | ||
| Calcarine cortex | [170] | ||
| Lingual cortex | [170] | ||
| Precentral gyrus | [170] | ||
| Middle temporal gyrus | [170] | ||
| Left frontal inferior operon | [170] | ||
| Left frontal inferior trigonal | [170] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, S.H.; Kim, G.Y.; Choi, G.T.; Do, J.T. Organ Abnormalities Caused by Turner Syndrome. Cells 2023, 12, 1365. https://doi.org/10.3390/cells12101365
Yoon SH, Kim GY, Choi GT, Do JT. Organ Abnormalities Caused by Turner Syndrome. Cells. 2023; 12(10):1365. https://doi.org/10.3390/cells12101365
Chicago/Turabian StyleYoon, Sang Hoon, Ga Yeon Kim, Gyu Tae Choi, and Jeong Tae Do. 2023. "Organ Abnormalities Caused by Turner Syndrome" Cells 12, no. 10: 1365. https://doi.org/10.3390/cells12101365
APA StyleYoon, S. H., Kim, G. Y., Choi, G. T., & Do, J. T. (2023). Organ Abnormalities Caused by Turner Syndrome. Cells, 12(10), 1365. https://doi.org/10.3390/cells12101365



.png)



