Detoxification Cytochrome P450s (CYPs) in Families 1–3 Produce Functional Oxylipins from Polyunsaturated Fatty Acids
Abstract
1. Introduction
1.1. Background
1.2. CYPs and Changes in CYP Expression and Activity
1.3. CYP Expression, Obesity, and Oxylipins
2. Oxylipin Production by CYPs
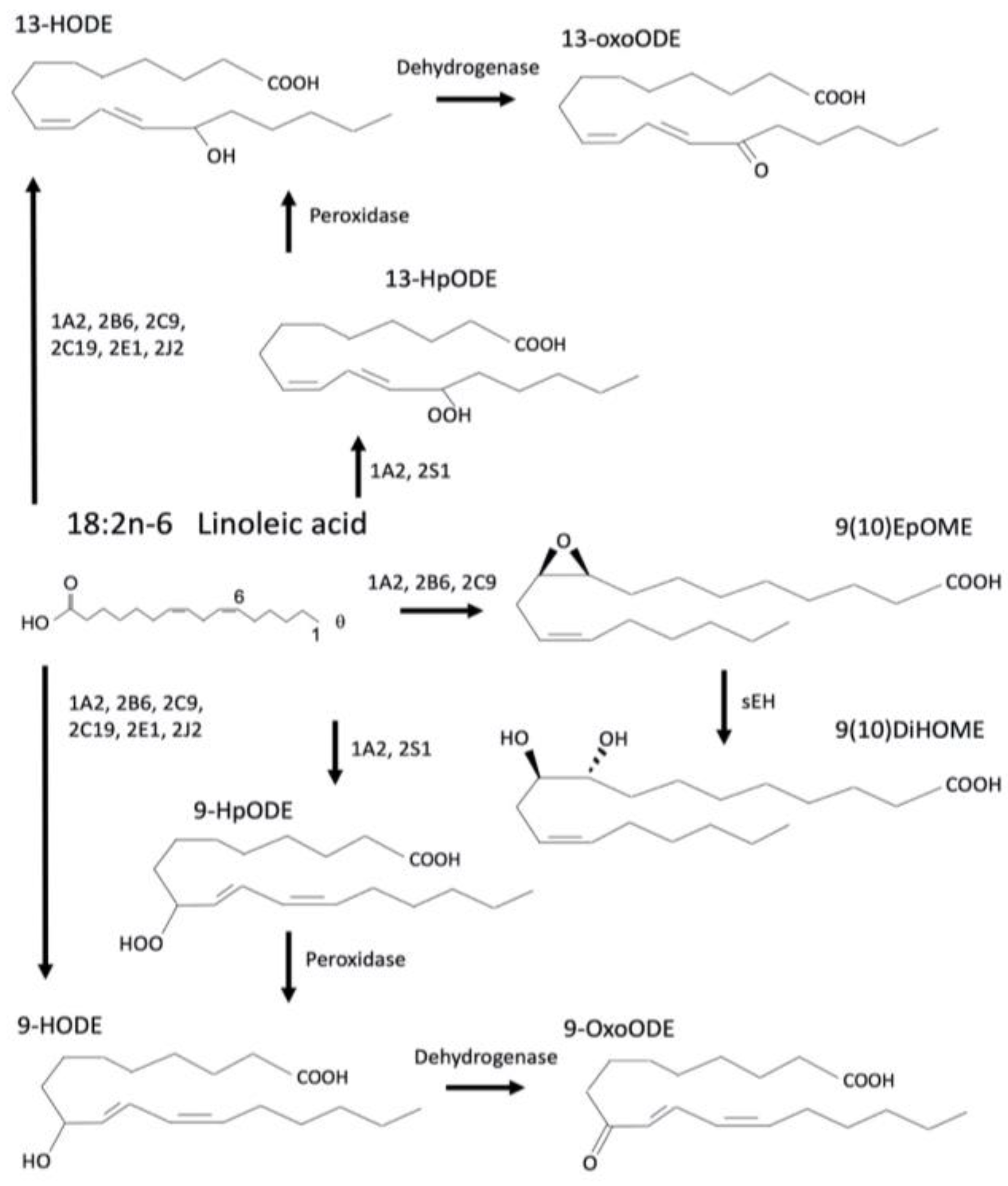
2.1. Linoleic Acid Metabolism
- CYPs primarily metabolize LA into the epoxinated EpOMEs that will be further metabolized by sEH into the DiHOMEs. HpODEs and HODEs may also be produced.
- LA oxylipins activate nuclear and cytosolic receptors such as PPARγ, GPR132, G2A, and TRPV1.
- In turn, most LA-oxylipins are pro-inflammatory, but anti-inflammatory effects potentially mediated by PPARγ have also been observed.
| Oxylipin | CAS Number | CYPs/Enzymes | References | Effects | References |
|---|---|---|---|---|---|
| 9,10-EpOME | 6814-52-4 | 1A2, 2B6, 2C9 | [8,84] |
| [2,76,85] |
| 9,10-DiHOME | 263399-34-4 | sEH |
| [76] | |
| 12,13-EpOME | Not found | 1A2, 2C9, 2E1, 2J2, | [68,84] |
| [2,85] |
| 12,13-DiHOME | 263399-35-5 | sEH |
| [7,16,52,86,87,88] | |
| 9-HpODE | 63121-49-3 | 1A2, 2S1 | [68,69] |
| [70] |
| 9-HODE | 98524-19-7 | 1A2, 2B6, 2C9, 2C19, 2E1, 2J2 Peroxidase | [8,73,75] |
| [8,76,83] |
| 9-oxoODE | 54232-59-6 | Dehydrogenase |
| [89] | |
| 13-HpODE | 23017-93-8 | 1A2, 2S1 | [68,69] |
| [71,72] |
| 13-HODE | 18104-45-5 | 1A2, 2B6, 2C9, 2C19, 2E1, 2J2 Peroxidase | [8,75,90] |
| [79,80,82,83,91] |
| 13-oxoODE | 29623-29-8 | Dehydrogenase |
| [8,92,93] |
2.2. Arachidonic Acid Metabolism
- AA is metabolized by the CYPs to a number of distinct oxylipins including the HETEs and the EETs that are subsequently metabolized by sEH into the DiHETs (also seen as DHETs).
- There are a large number of AA oxylipins that activate a number of GPCRs or act as second messengers
- AA-oxylipins are involved in a variety of processes, including inflammation, vascularization, vasoconstriction, oxidative stress, and apoptosis
| Oxylipin | CAS Number | CYPs/Enzymes | References | Effects | References |
|---|---|---|---|---|---|
| 5-HETE | 330796-62-8 | 1B1, 2B6 | [139,140] |
| [99,106,110] |
| 9-HETE | 79495-85-5 | 2B6 | [140] |
| [114] |
| 12-HETE | 71030-37-0 | 1B1, 2B6 | [8,139,140] |
| [112] |
| 15-HETE | 71030-36-9 | 1B1 | [139] |
| [107] |
| 18-HETE | 133268-58-3 | 2E1 | [141] |
| [115] |
| 19-HETE | 79551-85-2 | 2E1, 2U1 | [141,142] |
| [98] |
| 20-HETE | 79551-86-3 | 2U1 | [142] |
| [108,143,144] |
| 5,6-EET | 81246-84-6 | 2B6, 2D6, 2J2, 3A4 | [8,138,145,146] |
| [122,123] |
| 8,9-EET | 184488-44-6 | 1A2, 2B6, 2C9, 2D6, 2J2 3A4 | [8,138,140,145,146,147,148] |
| [116,118,149] |
| 11,12-EET | 200960-01-6 | 2C8, 2C9, 2D6, 2J2, 2S1, 3A4, 2B | [104,138,145,148,150] |
| [83,116,118,151] |
| 14,15-EET | 197508-62-6 | 2C8, 2C9, 2D6, 2J2, 2S1, 3A4 | [138,145,148,150] |
| [83,116,118,120] |
| 5,6-EET-EA * | N/A | 2D6, 2J2, 3A4 | [152,153] |
| [133,137] |
| 8,9-EET-EA * | N/A | 2D6, 2J2, 3A4 | [152,153] |
| [137] |
| 11,12-EET-EA * | N/A | 2D6, 2J2, 3A4 | [152,153] |
| [134] |
| 14,15-EET-EA * | N/A | 2D6, 2J2, 3A4 | [152,153] |
| [137] |
| 19-HETE-EA * | N/A | 2D6, 3A4 | [152,153] |
| |
| 20-HETE-EA * | 942069-11-6 | 2D6, 3A4 | [34,152,153] |
| [135] |
2.3. α–Linolenic Acid Metabolism
- ALA is metabolized by the CYPs into a number of distinct oxylipins including the EpODEs and HOTrEs
- Less is known about the individual CYPs responsible for metabolism of ALA
- There are several ALA-derived oxylipins about which little is known or little confirmation of its activity.
| Oxylipin | CAS Number | CYPs/Enzymes | References | Effects | References |
|---|---|---|---|---|---|
| 9,10-EpODE | N/A | 2B6 | [8] |
| [157] |
| 12,13-EpODE | N/A | unknown |
| [157] | |
| 15,16-EpODE | N/A | 2B6 | [8] |
| [157] |
| 9,10-DiHODE | N/A | sEH | [1] |
| [156,158,159] |
| 12,13-DiHODE | N/A | sEH | [1] |
| [156] |
| 15,16-DiHODE | N/A | sEH | [1] |
| [156,158] |
| 9-HpOTrE | 111004-08-1 | 2B6 | [8] |
| |
| 13-HpOTrE | 67597-26-6 | 2B6 | [8] |
| [160] |
| 9-HOTrE | 89886-42-0 | 2B6 | [8] |
| [162,164] |
| 13-HOTrE | 87984-82-5 | 2B6 | [8] |
| [160,162,163,164] |
| 9-oxoOTrE | 125559-74-2 | dehydrogenase | [1] |
| [165] |
| 13-oxoOTrE | N/A | dehydrogenase | [1] |
|
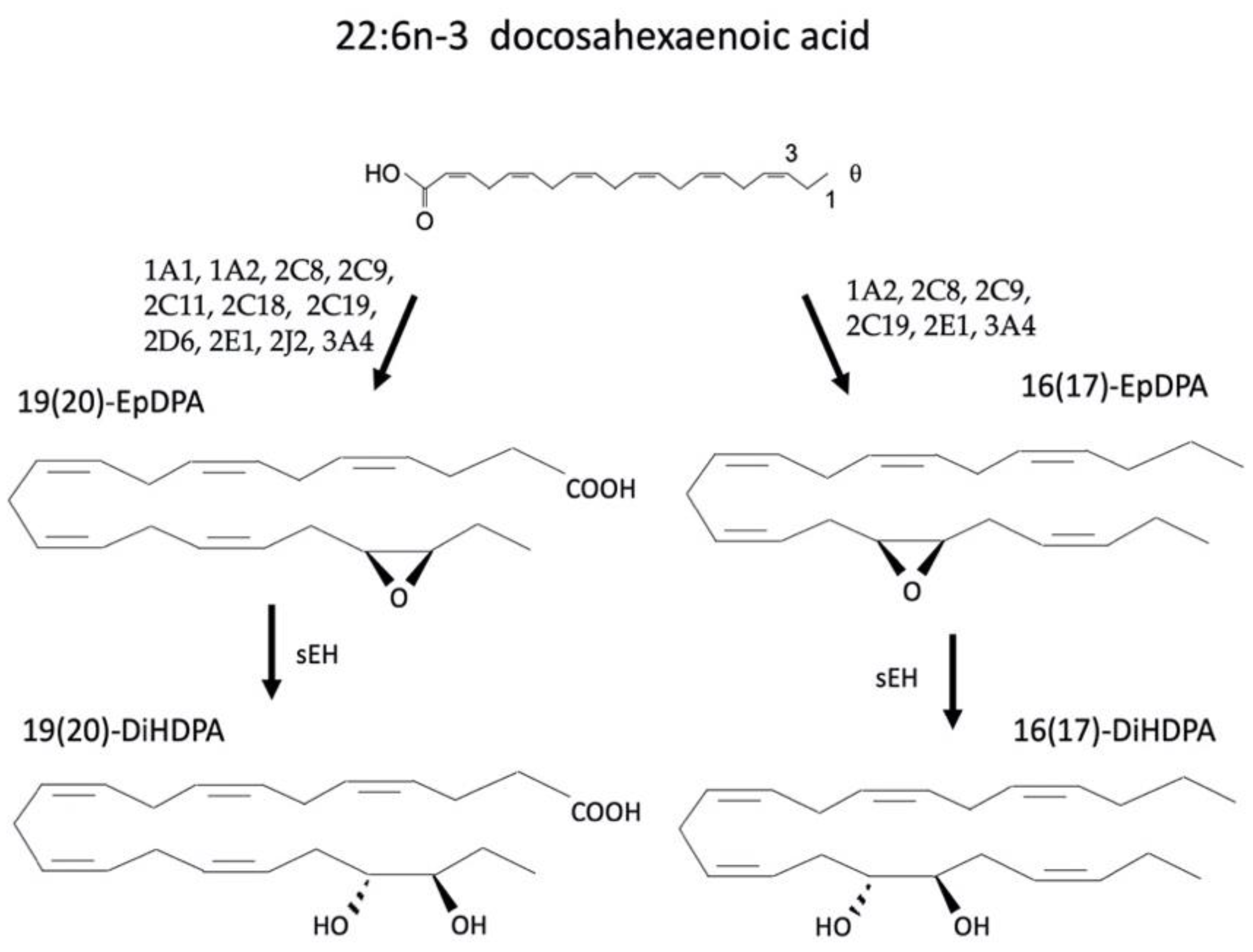
2.4. Eicosapentaenoic and Docosahexaenoic Acid Metabolism
- DHA and EPA are metabolized by CYPs, including CYP2C, CYP2J, and CYP3A subfamily members. EPA is metabolized into the HEPEs, epoxidated to the EpETEs and in turn the diols, DiHETEs (DHETEs) by sEH; DHA is metabolized to the epoxidated EpDPAs and in turn the DiHDPAs by sEH.
- DHA and EPA often function as anti-inflammatory and perceived as beneficial; however there are examples of negative effects of their oxylipins, especially DHA.
- Some of DHA and EPA’s beneficial effects are probably due to competitive inhibition of AA metabolism.
| Oxylipin | CAS Number | CYPs/Enzymes | References | Effects | References |
|---|---|---|---|---|---|
| 7,8-EpDPA | 895127-66-9 | 1A2, 2C9, 2C19, 2J2, 3A4 | [179] |
| [189] |
| 10,11-EpDPA | 895127-65-8 | 1A2, 2C8, 2C9, 2C19, 2J2, 3A4 | [179] |
| [189] |
| 13,14-EpDPA | 895127-64-7 | 1A2, 2C8, 2C9, 2C19, 2J2, 3A4 | [179] |
| [189,190] |
| 16,17-EpDPA | 155073-46-4 | 1A2, 2C8, 2C9, 2C19, 2E1, 3A4 | [179] |
| [177,189] |
| 19,20-EpDPA | N/A | 1A1, 1A2, 2C8, 2C9, 2C11, 2C18, 2C19, 2D6, 2E1, 2J2, 3A4 | [179,191] |
| [173,177,178,189,192] |
| 7,8-DiHDPA | 168111-93-1 | sEH |
| [193] | |
| 10,11-DiHDPA | 1345275-22-0 | sEH |
| ||
| 13,14-DiHDPA | 1345275-24-2 | sEH |
| [176] | |
| 16,17-DiHDPA | 1345275-27-5 | sEH |
| [188] | |
| 19,20-DiHDPA | N/A | sEH |
| [194] |
3. Discussion—Potential Interactions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gabbs, M.; Leng, S.; Devassy, J.G.; Monirujjaman, M.; Aukema, H.M. Advances in Our Understanding of Oxylipins Derived from Dietary PUFAs. Adv. Nutr. 2015, 6, 513–540. [Google Scholar] [CrossRef] [PubMed]
- Deol, P.; Fahrmann, J.; Yang, J.; Evans, J.R.; Rizo, A.; Grapov, D.; Salemi, M.; Wanichthanarak, K.; Fiehn, O.; PHinney, B.; et al. Omega-6 and omega-3 oxylipins are implicated in soybean oil induced obesity in mice. Sci. Rep. 2017, 7, 12488. [Google Scholar] [CrossRef] [PubMed]
- Dyall, S.C.; Balas, L.; Bazan, N.G.; Brenna, J.T.; Chiang, N.; da Costa Souza, F.; Dalli, J.; Durand, T.; Galano, J.M.; Lein, P.J.; et al. Polyunsaturated fatty acids and fatty acid-derived lipid mediators: Recent advances in the understanding of their biosynthesis, structures, and functions. Prog. Lipid Res. 2022, 86, 101165. [Google Scholar] [CrossRef] [PubMed]
- Caramia, G. Essential fatty acids and lipid mediators. Endocannabinoids. Pediatr. Med. Chir. 2012, 34, 65–72. [Google Scholar] [CrossRef]
- Moreira, F.A.; Lutz, B. The endocannabinoid system: Emotion, learning and addiction. Addict. Biol. 2008, 13, 196–212. [Google Scholar] [CrossRef]
- Barquissau, V.; Ghandour, R.A.; Ailhaud, G.; Klingenspor, M.; Langin, D.; Amri, E.Z.; Pisani, D.F. Control of adipogenesis by oxylipins, GPCRs and PPARs. Biochimie 2017, 136, 3–11. [Google Scholar] [CrossRef]
- Stanford, K.I.; Lynes, M.D.; Takahashi, H.; Baer, L.A.; Arts, P.J.; May, F.J.; Lehnig, A.C.; Middelbeek, R.J.W.; Richard, J.J.; So, K.; et al. 12,13-diHOME: An Exercise-Induced Lipokine that Increases Skeletal Muscle Fatty Acid Uptake. Cell Metab. 2018, 27, 1111–1120. [Google Scholar] [CrossRef]
- Heintz, M.M.; Eccles, J.A.; Olack, E.M.; Maner-Smith, K.M.; Ortlund, E.A.; Baldwin, W.S. Human CYP2B6 is an anti-obesity enzyme that produces active oxylipins from polyunsaturated fatty acids. PLoS ONE 2022, 17, e0277053. [Google Scholar] [CrossRef]
- Rahman, M.; Halade, G.V.; Bhattacharya, A.; Fernandes, G. The fat-1 transgene in mice increases antioxidant potential, reduces pro-inflammatory cytokine levels, and enhances PPAR-gamma and SIRT-1 expression on a calorie restricted diet. Oxid. Med. Cell Longev 2009, 2, 307–316. [Google Scholar] [CrossRef]
- Hohos, N.M.; Cho, K.J.; Swindle, D.C.; Allshouse, A.A.; Rudolph, M.C.; Skaznik-Wikiel, M.E. Fat-1 Transgene Is Associated With Improved Reproductive Outcomes. Endocrinology 2018, 159, 3981–3992. [Google Scholar] [CrossRef]
- Chansela, P.; Goto-Inoue, N.; Zaima, N.; Hayasaka, T.; Sroyraya, M.; Kornthong, N.; Engsusophon, A.; Tamtin, M.; Chaisri, C.; Sobhon, P.; et al. Composition and localization of lipids in Penaeus merguiensis ovaries during the ovarian maturation cycle as revealed by imaging mass spectrometry. PLoS ONE 2012, 7, e33154. [Google Scholar] [CrossRef] [PubMed]
- Ginjupalli, G.K.; Gerard, P.D.; Baldwin, W.S. Arachidonic acid enhances reproduction in Daphnia magna and mitigates changes in sex ratios induced by pyriproxyfen. Environ. Tox. Chem. 2015, 34, 527–535. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp. Biol. Med. 2008, 233, 674–688. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. An increase in the omega-6/omega-3 fatty acid ratio increases the risk for obesity. Nutrients 2016, 8, 128. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, R.C.; Gonçalves, T.T.; Leiria, L.O. Exploiting oxidized lipids and the lipid-binding GPCRs against cardiometabolic diseases. Br. J. Pharmacol. 2020, 178, 531–549. [Google Scholar] [CrossRef]
- Zimmer, B.; Angioni, C.; Osthues, T.; Toewe, A.; Thomas, D.B.; Pierre, S.C.; Geisslinger, G.; Scholich, K.; Sisignano, M. The oxidized linoleic acid metabolite 12,13-DiHOME mediates thermalhyperalgesia during inflammatory pain. BBA-Mol. Cell Biol. Lipids 2018, 1863, 669–678. [Google Scholar] [CrossRef]
- Yuan, X.; Ta, T.C.; Lin, M.; Evans, J.R.; Dong, Y.; Bolotin, E.; Sherman, M.A.; Forman, B.M.; Sladek, F.M. Identification of an endogenous ligand bound to a native orphan nuclear receptor. PLoS ONE 2009, 4, e5609. [Google Scholar] [CrossRef]
- Gilroy, D.W.; Edin, M.L.; DeMaeyer, R.P.H.; Tystrom, J.; Newson, J.; Lih, F.B.; Stables, M.; Zeldin, D.C.; Bishop-Bailey, D. CYP450-derived oxyipins mediate inflammatory resolution. Proc. Natl. Acad. Sci. USA 2016, 113, E3240–E3249. [Google Scholar] [CrossRef]
- Baldwin, W.S. Phase 0 of the Xenobiotic Response: Nuclear Receptors and Other Transcription Factors as a First Step in Protection from Xenobiotics. Nucl. Recept. Res. 2019, 6, 101447. [Google Scholar] [CrossRef]
- Nelson, D.R.; Zeldin, D.C.; Hoffman, S.M.G.; Maltais, L.J.; Wain, H.M.; Nebert, D.W. Comparison of cytochrome P450 (CYP) genes from the mouse and human genomes, including nomenclature recommendations for genes, pseudogenes and alternative splice variants. Pharmacogenetics 2004, 14, 1–18. [Google Scholar] [CrossRef]
- Waxman, D.J. Interactions of hepatic cytochromes P-450 with steroid hormones: Regioselectivity and stereoselectivity of steroid metabolism and hormonal regulation of rat P-450 enzyme expression. Biochem. Pharmcol. 1988, 37, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, W.S.; Marko, P.B.; Nelson, D.R. The Cytochrome P450 (CYP) gene superfamily in Daphnia pulex. BMC Genom. 2009, 10, 169. [Google Scholar] [CrossRef] [PubMed]
- David, P.; Dauphin-Villemant, D.; Mesneau, A.; Meyran, C. Molecular approach to aquatic environmental bioreporting: Differential response to environmental inducers of cytochrome P450 monooxygenase genes in the detritivorous subalpine planktonic Crustacea, Daphnia pulex. Mol. Ecol. 2003, 12, 2473–2481. [Google Scholar] [CrossRef] [PubMed]
- Wojnowski, L.; Kamdem, L.K. Clinical implications of CYP3A polymorphisms. Expert. Opin. Drug Metab. Toxicol. 2006, 2, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.C.; Ho, I.K.; Tsou, H.H.; Tian, J.N.; Hsiao, C.F.; Chen, C.H.; Tan, H.K.; Lin, L.; Wu, C.S.; Su, L.W.; et al. CYP2B6 polymorphisms influence the plasma concentration and clearance of the methadone S-enantiomer. J. Clin. Psychopharmacol. 2011, 31, 463–469. [Google Scholar] [CrossRef]
- Hernandez, J.P.; Mota, L.C.; Baldwin, W.S. Activation of CAR and PXR by dietary, environmental and occupational chemicals alters drug metabolism, intermediary metabolism, and cell proliferation. Curr. Pharm. Personal. Med. 2009, 7, 81–105. [Google Scholar] [CrossRef]
- Sonoda, J.; Evans, R.M. Biological function and mode of action of nuclear xenobiotic receptors. Pure Appl. Chem. 2003, 75, 1733–1742. [Google Scholar] [CrossRef]
- Kudo, T.; Shimada, T.; Toda, T.; Igeta, S.; Suzuki, W.; Ikarashi, N.; Ochiai, W.; Ito, K.; Aburada, M.; Sugiyama, K. Altered expression of CYP in TSOD mice: A model of type 2 diabetes and obesity. Xenobiotica 2009, 39, 889–902. [Google Scholar] [CrossRef]
- Dong, B.; Qatanani, M.; Moore, D.D. Constitutive androstane receptor mediates the induction of drug metabolism in mouse models of type 1 diabetes. Hepatology 2009, 50, 622–629. [Google Scholar] [CrossRef]
- Lang, T.; Klein, K.; Fischer, J.; Nussler, A.K.; Neuhaus, P.; Hofmann, U.; Eichelbaum, M.; Schwab, M.; Zanger, U.M. Extensive genetic polymorphism in the human CYP2B6 gene with impact on expression and function in human liver. Pharmacogenetics 2001, 11, 399–415. [Google Scholar] [CrossRef]
- Wang, C.J.; Shao, H.; Shang, M.; Zhang, W. Association between CYP2B6, CYP2D6, GSTP1 genetic polymorphisms and urinary styrene metabolites in professional workers. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2009, 27, 589–592. [Google Scholar] [PubMed]
- Bumpus, N.N.; Kent, U.M.; Hollenberg, P.F. Metabolism of efavirenz and 8-hydroxyefavirenz by P450 2B6 leads to inactivation by two distinct mechanisms. J. Pharmacol. Exp. Ther. 2013, 319, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Scheer, N.; Kapelyukh, Y.; McEwan, J.; Beuger, V.; Stanley, L.A.; Rode, A.; Wolf, C.R. Modeling human cytochrome P450 2D6 metabolism and drug-drug interaction by a novel panel of knockout and humanized mouse lines. Mol. Pharmacol. 2012, 81, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Sridar, C.; Snider, N.T.; Hollenberg, P.F. Anandamide oxidation by wild-type and polymorphically expressed CYP2B6 and CYP2D6. Drug Metab. Dispos. 2011, 39, 782–788. [Google Scholar] [CrossRef]
- Hankinson, O. The role of AHR-inducible cytochrome P450s in metabolism of polyunsaturated fatty acids. Drug Metab. Rev. 2016, 48, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Olack, E.M.; Heintz, M.M.; Baldwin, W.S. Dataset of Endo- and Xenobiotic Inhibition of CYP2B6: Comparison to CYP3A4. Data Brief. 2022, 41, 108013. [Google Scholar] [CrossRef] [PubMed]
- Usmani, K.A.; Rose, R.L.; Hodgson, E. Inhibition and activation of the human liver microsomal and human cytochrome P450 3A4 metabolism of testosterone by deployment-related chemicals. Drug Metab. Dispos. 2003, 31, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Usmani, K.A.; Cho, T.M.; Rose, R.L.; Hodgson, E. Inhibition of the human liver microsomal and human cytochrome P450 1A2 and 3A4 metabolism of estradiol by deployment-related and other chemicals. Drug Metab. Dispos. 2006, 34, 1606–1614. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Liu, X.; Hennighausen, L.; Davey, H.W.; Waxman, D.J. Distinctive roles of STAT5a and STAT5b in sexual dimorphism of hepatic P450 gene expression. Impact of STAT5a gene disruption. J. Biol. Chem. 1999, 274, 7421–7430. [Google Scholar] [CrossRef]
- Oshida, K.; Waxman, D.J.; Corton, J.C. Chemical and hormonal effects on STAT5b-dependent sexual dimorphism of the liver transcriptome. PLoS ONE 2016, 11, e0150284. [Google Scholar]
- Wiwi, C.A.; Gupte, M.; Waxman, D.J. Sexually dimorphic P450 gene expression in liver-specific hepatocyte nuclear factor 4a-deficient mice. Mol. Endocrinol. 2004, 18, 1975–1987. [Google Scholar] [CrossRef] [PubMed]
- Wiwi, C.A.; Waxman, D.J. Role of hepatocyte nuclear factors in growth hormone-regulated, sexually dimorphic expression of liver cytochromes P450. Growth Factors 2004, 22, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, J.P.; Mota, L.C.; Huang, W.; Moore, D.D.; Baldwin, W.S. Sexually dimorphic regulation and induction of P450s by the constitutive androstane receptor (CAR). Toxicology 2009, 256, 53–64. [Google Scholar] [CrossRef] [PubMed]
- Heintz, M.M.; Kumar, R.; Rutledge, M.M.; Baldwin, W.S. Cyp2b-null male mice are susceptible to diet-induced obesity and perturbations in lipid homeostasis. J. Nutr. Biochem. 2019, 70, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Heintz, M.M.; Kumar, R.; Maner-Smith, K.M.; Ortlund, E.A.; Baldwin, W.S. Age- and Diet-Dependent Changes in Hepatic Lipidomic Profiles of Phospholipids in Male Mice: Age Acceleration in Cyp2b-Null Mice. J. Lipids 2022, 2022, 7122738. [Google Scholar] [CrossRef]
- Oteng, A.-B.; Higuchi, S.; Banks, A.S.; Haeusler, R.A. Cyp2c-deficiency depletes muricholic acids and protects against high-fat diet-induced obesity in male mice but promotes liver damage. Mol. Metab. 2021, 53, 101326. [Google Scholar] [CrossRef]
- Kumar, R.; Litoff, E.J.; Boswell, W.T.; Baldwin, W.S. High fat diet induced obesity is mitigated in Cyp3a-null female mice. Chem.-Biol. Interact. 2018, 289, 129–140. [Google Scholar] [CrossRef]
- Nakagawa, K.; Marji, J.S.; Schwartzman, M.L.; Waterman, M.R.; Capdevila, J.H. Androgen-mediated induction of the kidney arachidonate hydroxylases is associated with the development of hypertension. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003, 284, R1055–R1062. [Google Scholar] [CrossRef]
- Holla, V.R.; Adas, F.; Imig, J.D.; Hao, H.; Price, E.J.; Olsen, N.; Kovacs, W.J.; Magnuson, M.A.; Keeney, D.S.; Breyer, M.D.; et al. Alterations in the regulation of androgen-sensitive Cyp 4a monooxygenases cause hypertension. Proc. Natl. Acad. Sci. USA 2001, 98, 5211–5216. [Google Scholar] [CrossRef]
- Sun, D.; Yang, Y.M.; Jiang, H.; Wu, H.; Ojaimi, C.; Kaley, G.; Huang, A. Roles of CYP2C29 and RXR gamma in vascular EET synthesis of female mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2010, 298, R862–R869. [Google Scholar] [CrossRef][Green Version]
- Athirakul, K.; Bradbury, J.A.; Graves, J.P.; DeGraff, L.M.; Ma, J.; Zhao, Y.; Couse, J.F.; Quigley, R.; Harder, D.R.; Zhao, X.; et al. Increased blood pressure in mice lacking cytochrome P450 2J5. FASEB J. 2008, 22, 4096–4108. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, K.L.; Darwash, A.M.; Sosnowski, K.A.; Zhang, H.; Shah, S.; Zhabyeyev, P.; Yang, J.; Hammock, B.D.; Edin, M.L.; Zeldin, D.C.; et al. Soluble epoxide hydrolase in aged female mice and human explanted hearts following ischemic injury. Int. J. Mol. Sci. 2021, 22, 1691. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.M.; Barraj, L.M.; Rampersaud, G.C. Consumption of grapefruit is associated with higher nutrient intakes and diet quality among adults, and more favorable anthropometrics in women, NHANES 2003–2008. Food Nutr. Res. 2014, 58, 22179. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.A.; Subhan, N.; Rahman, M.M.; Uddin, S.J.; Reza, H.M.; Sarker, S.D. Effect of Citrus Flavonoids, Naringin and Naringenin, on Metabolic Syndrome and Their Mechanisms of Action. Adv. Nutr. 2014, 5, 404–417. [Google Scholar] [CrossRef]
- Wang, K.; Chen, X.; Ward, S.C.; Liu, Y.; Ouedraogo, Y.; Xu, C.; Cederbaum, A.; Lu, Y. CYP2A6 is associated with obesity: Studies in human samples and a high fat diet mouse model. Int. J. Obes. 2019, 43, 475–486. [Google Scholar] [CrossRef]
- Krogstad, V.; Peric, A.; Robertsen, I.; Kringen, M.K.; Wegler, C.; Angeles, P.C.; Hjelmesaeth, J.; Karlsson, C.; Andersson, S.; Artursson, P.; et al. A comparative analysis of cytochrome P450 activities in paired liver and small intestinal samples from patients with obesity. Drug Metab. Dispos. 2020, 48, 8–17. [Google Scholar] [CrossRef]
- Heintz, M.M.; McRee, R.; Kumar, R.; Baldwin, W.S. Gender differences in diet-induced steatotic disease in Cyp2b-null mice. PLoS ONE 2020, 15, e0229896. [Google Scholar] [CrossRef]
- Finn, R.D.; Henderson, C.J.; Scott, C.L.; Wolf, C.R. Unsaturated fatty acid regulation of cytochrome P450 expression via a CAR-dependent pathway. Biochem. J. 2009, 417, 43–54. [Google Scholar] [CrossRef]
- Norman, J.E.; Aung, H.H.; Otoki, Y.; Zhang, Z.; Taha, A.Y.; Rutledge, J.C. A single meal has the potential to alter brain oxylipin content. Prostaglandins Leukot Essent Fat. Acids 2020, 154, 102062. [Google Scholar] [CrossRef]
- Cho, S.J.; Kim, S.B.; Cho, H.J.; Chong, S.; Chung, S.J.; Kang, I.M.; Lee, J.I.; Yoon, I.S.; Kim, D.D. Effects of Nonalcoholic Fatty Liver Disease on Hepatic CYP2B1 and in Vivo Bupropion Disposition in Rats Fed a High-Fat or Methionine/Choline-Deficient Diet. J. Agric. Food Chem. 2016, 64, 5598–5606. [Google Scholar] [CrossRef]
- Patoine, D.; Petit, M.; Pilote, S.; Picard, F.; Drolet, B.; Simard, C. Modulation of CYP3a expression and activity in mice models of type 1 and type 2 diabetes. Pharmacol. Res. Perspect. 2014, 2, e00082. [Google Scholar] [CrossRef] [PubMed]
- Shoieb, S.S.; El-Ghiaty, M.A.; Alqahtani, M.A.; El-Kadi, A.O.S. Cytochrome P450-derived eicosanoids and inflammation in liver diseases. Prostaglandins Other Lipid Med. 2020, 147, 106400. [Google Scholar] [CrossRef] [PubMed]
- Konkel, A.; Schunck, W.H. Role of cytochrome P450 enzymes in the bioactivation of polyunsaturated fatty acids. Biochim. Biophys. Acta 2011, 1814, 210–222. [Google Scholar] [CrossRef] [PubMed]
- Whelan, J.; Fritsche, K. Linoleic Acid. Adv. Nutr. 2013, 4, 311–312. [Google Scholar] [CrossRef] [PubMed]
- Blasbalg, T.L.; Hibbeln, J.R.; Ramsden, C.E.; Majchrzak, S.F.; Rawlings, R.R. Changes in consumption of omega-3 and omega-6 fatty acids in the United States during the 20th century. Am. J. Clin. Nutr. 2011, 93, 950–962. [Google Scholar] [CrossRef]
- Hildreth, K.; Kodani, S.D.; Hammock, B.D.; Zhao, L. Cytochrome P450-derived linoleic acid metabolites EpOMEs and DiHOMEs: A review of recent studies. J. Nutr. Biochem. 2020, 86, 108484. [Google Scholar] [CrossRef]
- Vangaveti, V.; Shashidhar, V.; Collier, F.; Hodge, J.; Rush, C.; Malabu, U.; Baune, B.; Kennedy, R.L. 9- and 13-HODE regulate fatty acid binding protein-4 in human macrophages, but does not involve HODE/GPR132 axis in PPAR-γ regulation of FABP4. Ther. Adv. Endocrinol. Metab. 2018, 9, 137–150. [Google Scholar] [CrossRef]
- Lu, J.; Shang, X.; Zhong, W.; Xu, Y.; Shi, R.; Wang, X. New insights of CYP1A in endogenous metabolism: A focus on single nucleotide polymorphisms and diseases. Acta Pharm. Sin. B 2020, 10, 91–104. [Google Scholar] [CrossRef]
- Bui, P.; Imaizumi, S.; Beedanagari, S.R.; Reddy, S.T.; Hankinson, O. Human CYP2S1 metabolizes cyclooxygenase- and lipoxygenase-derived eicosanoids. Drug Metab. Dispos. 2011, 39, 180–190. [Google Scholar] [CrossRef]
- Corteselli, E.M.; Gibbs-Flournoy, E.; Simmons, S.O.; Bromberg, P.; Gold, A.; Samet, J.M. Long chain lipid hydroperoxides increase the glutathione redox potential through glutathione peroxidase 4. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2019, 1863, 950–959. [Google Scholar] [CrossRef]
- Li, W.-G.; Stoll, L.L.; Rice, J.B.; Xu, S.-P.; Miller, F.J., Jr.; Chatterjee, P.; Hu, L.; Oberley, L.W.; Spector, A.A.; Weintraub, N.L. Activation of NAD(P)H oxidase by lipid hydroperoxides: Mechanism of oxidant-mediated smooth muscle cytotoxicity. Free Radic Biol. Med. 2003, 34, 937–946. [Google Scholar] [CrossRef] [PubMed]
- Rohr, M.; Narasimhulu, C.A.; Keewan, E.A.; Hamid, S.; Parthasarathy, S. The dietary peroxidized lipid, 13-HPODE, promotes intestinal inflammation by mediating granzyme B secretion from natural killer cells. Food Funct. 2020, 11, 9526–9534. [Google Scholar] [CrossRef] [PubMed]
- Moran, J.H.; Nowak, G.; Grant, D.F. Analysis of the toxic effects of linoleic acid, 12,13-cis-epoxyoctadecenoic acid, and 12,13-dihydroxyoctadecenoic acid in rabbit renal cortical mitochondria. Toxicol. Appl. Pharmacol. 2001, 172, 150–161. [Google Scholar] [CrossRef]
- Moran, J.H.; Weise, R.; Schnellmann, R.G.; Freeman, J.P.; Grant, D.F. Cytotoxicity of linoleic acid diols to renal proximal tubular cells. Toxicol. Appl. Pharmacol. 1997, 146, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Bylund, J.; Kunz, T.; Valmsen, K.; Oliw, E.H. Cytochromes P450 with bisallylic hydroxylation activity on arachidonic and linoleic acids studied with human recombinant enzymes and with human and rat liver microsomes. J. Pharmacol. Exp. Ther. 1998, 284, 51–60. [Google Scholar] [PubMed]
- Lecka-Czernik, B.; Moerman, E.J.; Grant, D.F.; Lehmann, M., Jr.; Manolagas, S.C.; Jilka, R.L. Divergent Effects of Selective Peroxisome Proliferator-Activated Receptor-γ2 Ligands on Adipocyte Versus Osteoblast Differentiation. Endocrinology 2002, 143, 2376–2384. [Google Scholar] [CrossRef] [PubMed]
- Hennebelle, M.; Morgan, R.K.; Sethi, S.; Zhang, Z.; Chen, H.; Grodzki, A.C.; Lein, P.J.; Taha, A.Y. Linoleic acid-derived metabolites constitute the majority of oxylipins in the rat pup brain and stimulate axonal growth in primary rat cortical neuron-glia co-cultures in a sex-dependent manner. J. Neurochem. 2020, 152, 195–207. [Google Scholar] [CrossRef]
- Hattori, T.; Obinata, H.; Ogawa, A.; Kishi, M.; Tatei, K.; Ishikawa, O.; Izumi, T. G2A Plays Proinflammatory Roles in Human Keratinocytes under Oxidative Stress as a Receptor for 9-Hydroxyoctadecadienoic Acid. J. Investig. Dermatol. 2008, 128, 1123–1133. [Google Scholar] [CrossRef]
- Setty, B.N.Y.; Berger, M.; Stuart, M.J. 13-Hydroxyoctadecadienoic acid (13-HODE) stimulates prostacyclin production by endothelial cells. Biochem. Biophys. Res. Commun. 1987, 146, 502–509. [Google Scholar] [CrossRef]
- Umeno, A.; Sakashita, M.; Sugino, S.; Murotomi, K.; Okuzawa, T.; Morita, N.; Tomii, K.; Tsuchya, Y.; Yamasaki, I.; Horie, M.; et al. Comprehensive analysis of PPARγ agonist activities of stereo-, regio-, and enantio-isomers of hydroxyoctadecadienoic acids. Biosci. Rep. 2020, 40, BSR20193767. [Google Scholar] [CrossRef]
- Szczuko, M.; Kotlęga, D.; Palma, J.; Zembroń-Łacny, A.; Tylutka, A.; Gołąb-Janowska, M.; Drozd, A. Lipoxins, RevD1 and 9, 13 HODE as the most important derivatives after an early incident of ischemic stroke. Sci. Rep. 2020, 10, 12849. [Google Scholar] [CrossRef] [PubMed]
- Camp, R.D.; Fincham, N.J. Inhibition of ionophore-stimulated leukotriene B4 production in human leucocytes by monohydroxy fatty acids. Br. J. Pharmacol. 1985, 85, 837–841. [Google Scholar] [CrossRef] [PubMed]
- Hanif, A.; Edin, M.L.; Zeldin, D.C.; Morisseau, C.; Falck, J.R.; Nayeem, M.A. Vascular endothelial overexpression of human CYP2J2 (Tie2-CYP2J2 Tr) modulates cardiac oxylipin profiles and enhances coronary reactive hyperemia in mice. PLoS ONE 2017, 12, e0174137. [Google Scholar] [CrossRef]
- Draper, A.J.; Hammock, B.D. Identification of CYP2C9 as a Human Liver Microsomal Linoleic Acid Epoxygenase. Arch. Biochem. Biophys. 2000, 376, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, S.; Hammock, B.D.; Newman, J.W.; Meerarani, P.; Toborek, M.; Hennig, B. Involvement of CYP 2C9 in Mediating the Proinflammatory Effects of Linoleic Acid in Vascular Endothelial Cells. J. Am. Coll. Nutr. 2003, 22, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Lynes, M.D.; Leiria, L.O.; Lundh, M.; Barlelt, A.; Shamsi, F.; Huang, T.L.; Takahashi, H.; Hirshman, M.F.; Schlein, C.; Lee, A.; et al. The cold-induced lipokine 12,13-diHOME promotes fatty acid transport into brown adipose tissue. Nat. Med. 2017, 23, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Markaverich, B.M.; Crowley, J.R.; Alejandro, M.A.; Shoulars, K.; Casajuna, N.; Mani, S.; Reyna, A.; Sharp, J. Leukotoxin diols from ground corncob bedding disrupt estrous cyclicity in rats and stimulate MCF-7 breast cancer cell proliferation. Environ. Health Perspect. 2005, 113, 1698–1704. [Google Scholar] [CrossRef] [PubMed]
- Sisemore, M.F.; Zheng, J.; Yang, J.C.; Thompson, D.A.; Plopper, C.G.; Cortopassi, G.A.; Hammock, B.D. Cellular Characterization of Leukotoxin Diol-Induced Mitochondrial Dysfunction. Arch. Biochem. Biophys. 2001, 392, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, A.M.; Akopian, A.N.; Ruparel, N.B.; Diogenes, A.; Weintraub, S.T.; Uhlson, C.; Murphy, R.C.; Hargreaves, K.M. Heat generates oxidized linoleic acid metabolites that activate TRPV1 and produce pain in rodents. J. Clin. Investig. 2010, 120, 1617–1626. [Google Scholar] [CrossRef]
- Moran, J.H.; Mitchell, L.A.; Bradbury, J.A.; Qu, W.; Zeldin, D.C.; Schnellmann, R.G.; Grant, D.F. Analysis of the Cytotoxic Properties of Linoleic Acid Metabolites Produced by Renal and Hepatic P450s. Toxicol. Appl. Pharmacol. 2000, 168, 268–279. [Google Scholar] [CrossRef]
- Haas, T.A.; Bastida, E.; Nakamura, K.; Hullin, F.; Admirall, L.; Buchanan, M.R. Binding of 13-HODE and 5-, 12- and 15-HETE to endothelial cells and subsequent platelet, neutrophil and tumor cell adhesion. Biochim. Biophys. Acta (BBA)-Lipids Lipid Metab. 1988, 961, 153–159. [Google Scholar] [CrossRef]
- Nagy, L.; Tontonoz, P.; Alvarez, J.G.A.; Chen, H.; Evans, R.M. Oxidized LDL Regulates Macrophage Gene Expression through Ligand Activation of PPARγ. Cell 1998, 93, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Altmann, R.; Hausmann, M.; Spottl, T.; Gruber, M.; Bulld, A.W.; Menzel, K.; Vogl, D.; Herfarth, H.; Scholmerich, J.; Falk, W.; et al. 13-oxo-ODE is an endogenous ligand for PPARg in human colonic epithelial cells. Biochem. Pharmacol. 2007, 74, 612–622. [Google Scholar] [CrossRef] [PubMed]
- Ramsden, C.E.; Ringel, A.; Feldstein, A.E.; Taha, A.Y.; MacIntosh, B.A.; Hibbeln, J.R.; Majchrzak-Hong, S.F.; Faurot, K.R.; Rapoport, S.I.; Cheon, Y.; et al. Lowering dietary linoleic acid reduces bioactive oxidized linoleic acid metabolites in humans. Prostaglandins Leukot Essent Fat. Acids 2012, 87, 135–141. [Google Scholar] [CrossRef] [PubMed]
- DiNicolantonio, J.J.; O’Keefe, J.H. Omega-6 vegetable oils as a driver of coronary heart disease: The oxidized linoleic acid hypothesis. Open Heart 2018, 5, e000898. [Google Scholar] [CrossRef]
- Tallima, H.; El Ridi, R. Arachidonic acid: Physiological roles and potential health benefits—A review. J. Adv. Res. 2018, 11, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Taber, L.; Chiu, C.-H.; Whelan, J. Assessment of the arachidonic acid content in foods commonly consumed in the American diet. Lipids 1998, 33, 1151–1157. [Google Scholar] [CrossRef]
- Tunaru, S.; Chennupati, R.; Nüsing, R.M.; Offermanns, S. Arachidonic Acid Metabolite 19(S)-HETE Induces Vasorelaxation and Platelet Inhibition by Activating Prostacyclin (IP) Receptor. PLoS ONE 2016, 11, e0163633. [Google Scholar] [CrossRef]
- Powell, W.S.; Rokach, J. The eosinophil chemoattractant 5-oxo-ETE and the OXE receptor. Prog. Lipid Res. 2013, 52, 651–665. [Google Scholar] [CrossRef]
- Oliw, E.H.; Bylund, J.; Herman, C. Bisallylic hydroxylation and epoxidation of polyunsaturated fatty acids by cytochrome P450. Lipids 1996, 31, 1003–1021. [Google Scholar] [CrossRef]
- Ayajiki, K.; Okamura, T.; Fujioka, H.; Imaoka, S.; Funae, Y.; Toda, N. Involvement of CYP3A-derived arachidonic acid metabolite(s) in responses to endothelium-derived K+ channel opening substance in monkey lingual artery. Br. J. Pharmacol. 1999, 128, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Grant, G.E.; Rokach, J.; Powell, W.S. 5-Oxo-ETE and the OXE receptor. Prostaglandins Other Lipid Med. 2009, 89, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Capdevila, J.H.; Falck, J.R.; Harris, R.C. Cytochrome P450 and arachidonic acid bioactivation: Molecular and functional properties of the arachidonate monooxygenase. J. Lipid Res. 2000, 41, 163–181. [Google Scholar] [CrossRef] [PubMed]
- El-Sherbeni, A.A.; Aboutabl, M.E.; Zordoky, B.N.M.; Anwar-Mohamed, A.; El-Kadi, A.O.S. Determination of the dominant arachidonic acid cytochrome P450 monooxygenases in rat heart, lung, kidney, and liver: Protein expression and metabolite kinetics. AAPS J. 2013, 15, 112–122. [Google Scholar] [CrossRef]
- Spector, A.A. Arachidonic acid cytochrome P450 epoxygenase pathway. J. Lipid Res. 2009, 50, S52–S66. [Google Scholar] [CrossRef]
- Bittleman, D.B.; Casale, T.B. 5-Hydroxyeicosatetraenoic acid (HETE)-induced neutrophil transcellular migration is dependent upon enantiomeric structure. Am. J. Respir. Cell Mol. Biol. 1998, 12, 260–267. [Google Scholar] [CrossRef]
- Zhu, D.; Medhora, M.; Campbell, W.B.; Spitzbarth, N.; Baker, J.E.; Jacobs, E.R. Chronic Hypoxia Activates Lung 15-Lipoxygenase, Which Catalyzes Production of 15-HETE and Enhances Constriction in Neonatal Rabbit Pulmonary Arteries. Circ. Res. 2003, 92, 992–1000. [Google Scholar] [CrossRef]
- Shekhar, S.; Varghese, K.; Li, M.; Fan, L.; Booz, G.W.; Roman, R.J.; Fan, F. Conflicting Roles of 20-HETE in Hypertension and Stroke. Int. J. Mol. Sci. 2019, 20, 4500. [Google Scholar] [CrossRef]
- Alexanian, A.; Sorokin, A. Targeting 20-HETE producing enzymes in cancer—Rationale, pharmacology, and clinical potential. Onco Targets Ther. 2013, 6, 243–255. [Google Scholar] [CrossRef]
- Nagahora, N.; Yamada, H.; Kikuchi, S.; Hakozaki, M.; Yano, A. Nrf2 Activation by 5-lipoxygenase Metabolites in Human Umbilical Vascular Endothelial Cells. Nutrients 2017, 9, 1001. [Google Scholar] [CrossRef]
- Ma, Q. Role of nrf2 in oxidative stress and toxicity. Annu. Rev. Pharmacol. Toxicol. 2013, 53, 401–426. [Google Scholar] [CrossRef]
- van Doren, L.; Nguyen, N.; Garzia, C.; Fletcher, E.K.; Stevenson, R.; Jaramillo, D.; Kuliopulos, A.; Covic, L. Lipid Receptor GPR31 (G-Protein–Coupled Receptor 31) Regulates Platelet Reactivity and Thrombosis Without Affecting Hemostasis. Arterioscler. Thromb. Vasc. Biol. 2021, 41, e33–e45. [Google Scholar] [CrossRef]
- Hanif, A.; Edin, M.L.; Zeldin, D.C.; Morisseau, C.; Falck, J.R.; Nayeem, M.A. Vascular Endothelial Over-Expression of Human Soluble Epoxide Hydrolase (Tie2-sEH Tr) Attenuates Coronary Reactive Hyperemia in Mice: Role of Oxylipins and ω-Hydroxylases. PLoS ONE 2017, 12, e0169584. [Google Scholar] [CrossRef] [PubMed]
- Shishehbor, M.H.; Zhang, R.; Medina, H.; Brennan, M.-L.; Brennan, D.M.; Ellis, S.G.; Topol, E.J.; Hazen, S.L. Systemic elevations of free radical oxidation products of arachidonic acid are associated with angiographic evidence of coronary artery disease. Free Radic Biol. Med. 2006, 41, 1678–1683. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.A.; Balazy, M.; Margiotta, P.; Huang, D.D.; Falck, J.R.; McGiff, J.C. Cytochrome P-450-dependent HETEs: Profile of biological activity and stimulation by vasoactive peptides. Am. J. Physiol.-Reg. Ing. Comp. Physiol. 1996, 271, R863–R869. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Zhang, L.; Han, W.; Shen, T.; Ma, C.; Liu, Y.; Nie, X.; Liu, M.; Ran, Y.; Zhu, D. Activation of JNK/c-Jun is required for the proliferation, survival, and angiogenesis induced by EET in pulmonary artery endothelial cells. J. Lipid Res. 2012, 53, 1093–1105. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.L.; Nakamura, K. The c-jun kinase/stress-activated pathway: Regulation, function and role in human disease. Biochim. Biophys. Acta 2007, 1773, 1341–1348. [Google Scholar] [CrossRef] [PubMed]
- Pavlov, T.S.; Ilatovskaya, D.V.; Levchenko, V.; Mattson, D.L.; Roman, R.J.; Staruschenko, A. Effects of cytochrome P-450 metabolites of arachidonic acid on the epithelial sodium channel (ENaC). Am. J. Physiol.-Ren. Physiol. 2011, 301, F672–F681. [Google Scholar] [CrossRef] [PubMed]
- O’Shaughnessy, K.M.; Karet, F.E. Salt handling and hypertension. J. Clin. Investig. 2004, 113, 1075–1081. [Google Scholar] [CrossRef]
- Geng, H.-X.; Li, R.-P.; Li, Y.-G.; Wang, X.-Q.; Zhang, L.; Deng, J.-B.; Deng, J.-X. 14,15-EET Suppresses Neuronal Apoptosis in Ischemia–Reperfusion Through the Mitochondrial Pathway. Neurochem. Res. 2017, 42, 2841–2849. [Google Scholar] [CrossRef]
- Peterson, J.M.; Bryner, R.W.; Sindler, A.; Frisbee, J.C.; Alway, S.E. Mitochondrial apoptotic signaling is elevated in cardiac but not skeletal muscle in the obese Zucker rat and is reduced with aerobic exercise. J. Appl. Physiol. 2008, 105, 1934–1943. [Google Scholar] [CrossRef]
- Lamounier-Zepter, V.; Look, C.; Schunck, W.H.; Schlottmann, I.; Woischwill, C.; Bornstein, S.R.; Xu, A.; Morano, I. Interaction of epoxyeicosatrienoic acids and adipocyte fatty acid-binding protein in the modulation of cardiomyocyte contractility. Int. J. Obes. 2015, 39, 755–761. [Google Scholar] [CrossRef]
- Cazade, M.; Bidaud, I.; Hansen, P.B.; Lory, P.; Chemin, J. 5,6-EET potently inhibits T-type calcium channels: Implication in the regulation of the vascular tone. Pflüg. Arch.-Eur. J. Physiol. 2014, 466, 1759–1768. [Google Scholar] [CrossRef]
- Keeney, D.S.; Skinner, S.; Weii, S.; Friedberg, T.; Waterman, M.R. A Keratinocyte-specific epoxygenase, CYP2B12, metabolizes arachidonic acid with unusual selectivity, producing a single major epoxyeicosatrienoic acid. J. Biol. Chem. 1998, 273, 9279–9284. [Google Scholar] [CrossRef]
- Du, L.; Yermalitsky, V.; Ladd, P.A.; Capdevila, J.H.; Mernaugh, R.; Keeney, D.S. Evidence that cytochrome P450 CYP2B19 is the major source of epoxyeicosatrienoic acids in mouse skin. Arch. Biochem. Biophys. 2005, 435, 125–133. [Google Scholar] [CrossRef]
- Ladd, P.A.; Du, L.; Capdevila, J.H.; Mernaugh, R.; Keeney, D.S. Epoxyeicosatrienoic acids activate transglutaminases in situ and induce cornification of epidermal keratinocytes. J. Biol. Chem. 2003, 278, 35184–35192. [Google Scholar] [CrossRef]
- Schuck, R.N.; Zha, W.; Edin, M.L.; Gruzdev, A.; Vendrov, K.C.; Miller, T.M.; Xu, Z.; Lih, F.B.; DeGraft, L.M.; Tomer, K.B.; et al. The Cytochrome P450 Epoxygenase Pathway Regulates the Hepatic Inflammatory Response in Fatty Liver Disease. PLoS ONE 2014, 9, e110162. [Google Scholar] [CrossRef]
- Iliff, J.J.; Alkayed, N.J. Soluble epoxide hydrolase inhibition: Targeting multiple mechanisms of ischemic brain injury with a single agent. Future Neurol. 2009, 4, 179–199. [Google Scholar] [CrossRef]
- Sudhahara, V.; Shawa, S.; Imiga, J.D. Epoxyeicosatrienoic Acid Analogs and Vascular Function. Curr. Med. Chem. 2010, 17, 1181–1190. [Google Scholar] [CrossRef]
- Iliff, J.J.; Jia, J.; Nelson, J.; Goyagi, T.; Klaus, J.; Alkayed, N.J. Epoxyeicosanoid Signaling in CNS Function and Disease. Prostaglandins Other Lipid Mediat. 2010, 91, 68–84. [Google Scholar] [CrossRef]
- Strauss, K.I.; Gruzdev, A.; Zeldin, D.C. Altered behavioral phenotypes in soluble epoxide hydrolase knockout mice: Effects of traumatic brain injury. Prostaglandins Other Lipid Mediat. 2013, 104–105, 18–24. [Google Scholar] [CrossRef][Green Version]
- Sugiura, T.; Kobayashi, Y.; Oka, S.; Waku, K. Biosynthesis and degradation of anandamide and 2-arachidonoylglycerol and their possible physiological significance. Prostaglandins Leuko Essen Fat. Acids (PLEFA) 2002, 66, 173–192. [Google Scholar] [CrossRef]
- Snider, N.T.; Nast, J.A.; Tesmer, L.A.; Hollenberg, P.F. A cytochrome P450-derived epoxygenated metabolite of anandamide is a potent cannabinoid receptor 2-selective agonist. Mol. Pharmacol. 2009, 75, 965–972. [Google Scholar] [CrossRef]
- Kim, M.J.; McCollum, G.W.; Penn, J.S. In-silico comparison of CB2 selectivity among endocannabinoid ω-6 and -3 epoxyethanolamides. Investig. Opthamol. Vis. Sci. 2021, 62, 3017. [Google Scholar]
- Zendulka, O.; Dovrtelova, G.; Nosková, K.; Turjap, M.; Sulcova, A.; Hanus, L.; Jurica, J. Cannabinoids and cytochrome P450 interactions. Current drug metabolism. Curr. Drug Metab. 2016, 17, 206–226. [Google Scholar] [CrossRef]
- Overton, H.A.; Fyfe, M.C.; Reynet, C. GPR119, a novel G protein-coupled receptor target for the treatment of type 2 diabetes and obesity. Br. J. Pharmacol. 2008, 153, S76–S81. [Google Scholar] [CrossRef]
- Syed, S.K.; Bui, H.H.; Beavers, L.S.; Farb, T.B.; Ficorilli, J.; Chesterfield, A.K.; Kuo, M.-S.; Bokvist, K.; Barrett, D.G.; Efanov, A.M. Regulation of GPR119 receptor activity with endocannabinoid-like lipids. Am. J. Physiol.-Endocrinol. Metab. 2012, 303, E1469–E1478. [Google Scholar] [CrossRef]
- Snider, N.T.; Sikora, M.J.; Sridar, C.; Feuerstein, T.J.; Rae, J.M.; Hollenberg, P.F. The endocannabinoid anandamide is a substrate for the human polymorphic cytochrome P450 2D6. J. Pharmacol. Exp. Ther. 2008, 327, 538–545. [Google Scholar] [CrossRef]
- Maayah, Z.H.; Althurwi, H.N.; Abdelhamid, G.; Lesyk, G.; Jurasz, P.; El-Kadi, A.O.S. CYP1B1 inhibition attenuates doxorubicin-induced cardiotoxicity through a mid-chain HETEs-dependent mechanism. Pharmacol. Res. 2016, 105, 28–43. [Google Scholar] [CrossRef]
- Heintz, M.M. Role of Cyp2b in Unsaturated Fatty Acid Metabolism, Obesity, and Non-Alcoholic Fatty Liver Disease. Ph.D. Thesis, Clemson University, Ann Arbor, MI, USA, 2020. [Google Scholar]
- Laethem, R.M.; Balazy, M.; Falck, J.R.; Laethem, C.L.; Koop, D.R. Formation of 19(S)-, 19(R)-, and 18(R)-hydroxyeicosatetraenoic acids by alcohol-inducible cytochrome P450 2E1. J. Biol. Chem. 1993, 268, 12912–12918. [Google Scholar] [CrossRef]
- Devos, A.; Lino Cardenas, C.L.; Glowacki, F.; Engels, A.; Lo-Guidice, J.-M.; Chevalier, D.; Allorge, D.; Broly, F.; Cauffiez, C. Genetic polymorphism of CYP2U1, a cytochrome P450 involved in fatty acids hydroxylation. Prostaglandins Leukot Essent Fat. Acids 2010, 83, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Zou, A.P.; Imig, J.D.; de Montellano, P.R.O.; Sui, Z.; Falck, J.R.; Roman, R.J. Effect of P-450 omega-hydroxylase metabolites of arachidonic acid on tubuloglomerular feedback. Am. J. Physiol.-Ren. Physiol. 1994, 266, F934–F941. [Google Scholar] [CrossRef] [PubMed]
- Hoff, U.; Lukitsch, I.; Chaykovska, L.; Ladwig, M.; Arnold, C.; Manthati, V.L.; Schunck, W.-H. Inhibition of 20-HETE synthesis and action protects the kidney from ischemia/reperfusion injury. Kidney Int. 2011, 79, 57–65. [Google Scholar] [CrossRef]
- Wu, S.; Moomaw, C.R.; Tomer, K.B.; Falck, J.R.; Zeldin, D.C. Molecular Cloning and Expression of CYP2J2, a Human Cytochrome P450 Arachidonic Acid Epoxygenase Highly Expressed in Heart (∗). J. Biol. Chem. 1996, 271, 3460–3468. [Google Scholar] [CrossRef]
- Thuy Phuong, N.T.; Kim, J.W.; Kim, J.A.; Jeon, J.S.; Lee, J.Y.; Xu, W.J.; Yang, J.W.; Kim, S.K.; Kang, K.W. Role of the CYP3A4-mediated 11,12-epoxyeicosatrienoic acid pathway in the development of tamoxifen-resistant breast cancer. Oncotarget 2017, 8, 71054–71069. [Google Scholar] [CrossRef] [PubMed]
- Rifkind, A.B.; Lee, C.; Chang, T.K.; Waxman, D.J. Arachidonic acid metabolism by human cytochrome P450s 2C8, 2C9, 2E1, and 1A2: Regioselective oxygenation and evidence for a role for CYP2C enzymes in arachidonic acid epoxygenation in human liver microsomes. Arch. Biochem. Biophys. 1995, 320, 380–389. [Google Scholar] [CrossRef]
- Daikh, B.E.; Lasker, J.M.; Raucy, J.L.; Koop, D.R. Regio- and stereoselective epoxidation of arachidonic acid by human cytochromes P450 2C8 and 2C9. J. Pharmacol. Exp. Ther. 1994, 271, 1427–1433. [Google Scholar]
- Gao, Y.; Feng, J.; Ma, K.; Zhou, Z.; Zhu, Y.; Xu, Q.; Wang, X. 8,9-Epoxyeicosatrienoic Acid Inhibits Antibody Production of B Lymphocytes in Mice. PLoS ONE 2012, 7, e40258. [Google Scholar] [CrossRef]
- Mitra, R.; Guo, Z.; Milani, M.; Mesaros, C.; Rodriguez, M.; Nguyen, J.; Luo, X.; Clarke, D.; Lamba, J.; Schuetz, E.; et al. CYP3A4 Mediates Growth of Estrogen Receptor-positive Breast Cancer Cells in Part by Inducing Nuclear Translocation of Phospho-Stat3 through Biosynthesis of (±)-14,15-Epoxyeicosatrienoic Acid (EET)*. J. Biol. Chem. 2011, 286, 17543–17559. [Google Scholar] [CrossRef]
- Loot, A.E.; Moneke, I.; Keserü, B.; Oelze, M.; Syzonenko, T.; Daiber, A.; Fleming, I. 11,12-EET Stimulates the Association of BK Channel α and β1 Subunits in Mitochondria to Induce Pulmonary Vasoconstriction. PLoS ONE 2012, 7, e46065. [Google Scholar] [CrossRef]
- Walker, V.; Hollenberg, P.F. Cytochrome P450 2J2 metabolizes the endocannabinoid, anandamide. FASEB J. 2012, 26, 850.7. [Google Scholar] [CrossRef]
- Walker, V.J.; Griffin, A.P.; Hammar, D.K.; Hollenberg, P.F. Metabolism of Anandamide by Human Cytochrome P450 2J2 in the Reconstituted System and Human Intestinal Microsomes. J. Pharmacol. Exp. Ther. 2016, 357, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-B.; Nam, Y.A.; Kim, H.S.; Hayes, A.W.; Lee, B.-M. α-Linolenic acid: Nutraceutical, pharmacological and toxicological evaluation. Food Chem. Toxicol. 2014, 70, 163–178. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Leyva, D.; Bassett, C.M.C.; McCullough, R.; Pierce, G.N. The cardiovascular effects of flaxseed and its omega-3 fatty acid, alpha-linolenic acid. Can. J. Cardiol. 2010, 26, 489–496. [Google Scholar] [CrossRef]
- Schuchardt, J.P.; Schmidt, S.; Kressel, G.; Dong, H.; Willenberg, I.; Hammock, B.D.; Hahn, A.; Schebb, N.H. Comparison of free serum oxylipin concentrations in hyper- vs. normolipidemic men. Prostaglandins Leukot Essent Fat. Acids 2013, 89, 19–29. [Google Scholar] [CrossRef]
- Tiwari, S.; Yang, J.; Morisseau, C.; Durbin-Johnson, B.; Hammock, B.D.; Gomes, A.V. Ibuprofen alters epoxide hydrolase activity and epoxy-oxylipin metabolites associated with different metabolic pathways in murine livers. Sci. Rep. 2021, 11, 7042. [Google Scholar] [CrossRef]
- Owen, M.P.T.; Northrop, E.J.; Rich, J.J.J.; Perry, G.A.; Messman, R.D.; Dinh, T.T.N.; McCarty, K.J.; Yang, J.; Wan, D.; Lemley, C.O. Oxylipin concentrations in bovine corpora lutea during maternal recognition of pregnancy. Theriogenology 2020, 142, 384–389. [Google Scholar] [CrossRef]
- Svenvik, M.; Raffetseder, J.; Brudin, L.; Lindberg, R.; Blomberg, M.; Axelsson, D.; Jenmalm, M.C.; Ernerudh, J.; Nording, M.L. Plasma oxylipin levels associated with preterm birth in preterm labor. Prostaglandins Leuko Essen Fat. Acids (PLEFA) 2021, 166, 102251. [Google Scholar] [CrossRef]
- Kumar, N.; Gupta, G.; Anilkumar, K.; Fatima, N.; Karnati, R.; Reddy, G.V.; Giri, P.V.; Reddanna, P. 15-Lipoxygenase metabolites of α-linolenic acid, [13-(S)-HPOTrE and 13-(S)-HOTrE], mediate anti-inflammatory effects by inactivating NLRP3 inflammasome. Sci. Rep. 2016, 6, 31649. [Google Scholar] [CrossRef]
- Swanson, K.V.; Deng, M.; Ting, J.P.Y. The NLRP3 inflammasome: Molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 2019, 19, 477–489. [Google Scholar] [CrossRef]
- Zahradka, P.; Neumann, S.; Aukema, H.M.; Taylor, C.G. Adipocyte lipid storage and adipokine production are modulated by lipoxygenase-derived oxylipins generated from 18-carbon fatty acids. Int. J. Biochem. Cell Biol. 2017, 88, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Eccles, J.A. Activation of the PPAR Nuclear Receptors by Oxyliins and Their Potential Effects on Differentiation and Gene Expression in Myocytes. Master’s Thesis, Clemson University, Clemson, SC, USA, 2022. [Google Scholar]
- Chistyakov, D.V.; Azbukina, N.V.; Astakhova, A.A.; Goriainov, S.V.; Chistyakov, V.V.; Tiulina, V.V.; Gancharova, O.S.; Baksheeva, V.E.; Zamyatnin, A.A.J.; Phillippov, P.P.; et al. Alterations in Tear Content of Inflammatory Oxylipines Associated with Perioperative Dry Eye Syndrome. Biochem. (Mosc.) Suppl. Ser. A Membr. Cell Biol. 2020, 14, 134–139. [Google Scholar] [CrossRef]
- Prost, I.; Dhondt, S.; Rothe, G.; Vicente, J.; Rodriguez, M.J.; Kift, N.; Carbonne, F.; Griffiths, G.; Esquerre-Tugaye, M.-T.; Sosahl, S.; et al. Evaluation of the Antimicrobial Activities of Plant Oxylipins Supports Their Involvement in Defense against Pathogens. Plant Physiol. 2005, 139, 1902–1913. [Google Scholar] [CrossRef]
- de Bus, I.; Witkamp, R.; Zuilhof, H.; Albada, B.; Balvers, M. The role of n-3 PUFA-derived fatty acid derivatives and their oxygenated metabolites in the modulation of inflammation. Prostaglandins Other Lipid Mediat. 2019, 144, 106351. [Google Scholar] [CrossRef]
- Ostermann, A.I.; West, A.L.; Schoenfeld, K.; Browning, L.M.; Walker, C.G.; Jebb, S.A.; Calder, P.C.; Schebb, N.H. Plasma oxylipins respond in a linear dose-response manner with increased intake of EPA and DHA: Results from a randomized controlled trial in healthy humans. Am. J. Clin. Nutr. 2019, 109, 1251–1263. [Google Scholar] [CrossRef] [PubMed]
- Schuster, G.U.; Bratt, J.M.; Jiang, X.; Pedersen, T.L.; Grapov, D.; Adkins, Y.; Kelley, D.S.; Newman, J.W.; Kenyon, N.J.; Stephensen, C.B. Dietary long-chain omega-3 fatty acids do not diminish eosinophilic pulmonary inflammation in mice. Am. J. Respir. Cell Mol. Biol. 2014, 50, 626–636. [Google Scholar] [CrossRef]
- Isobe, Y.; Itagaki, M.; Ito, Y.; Naoe, S.; Kojima, K.; Ikeguchi, M.; Arita, M. Comprehensive analysis of the mouse cytochrome P450 family responsible for omega-3 epoxidation of eicosapentaenoic acid. Sci. Rep. 2018, 8, 7954. [Google Scholar] [CrossRef] [PubMed]
- van Waterschoot, R.A.; Rooswinkel, R.W.; Wagenaar, E.; van der Kruijssen, C.M.; van Herwaarden, A.E.; Schinkel, A.H. Intestinal cytochrome P450 3A plays an important role in the regulation of detoxifying systems in the liver. FASEB J. 2009, 23, 1. [Google Scholar] [CrossRef]
- Ulu, A.; Stephen Lee, K.S.; Miyabe, C.; Yang, J.; Hammock, B.G.; Dong, H.; Hammock, B.D. An omega-3 epoxide of docosahexaenoic acid lowers blood pressure in angiotensin-II-dependent hypertension. J. Cardiovasc. Pharmacol. 2014, 64, 87–99. [Google Scholar] [CrossRef]
- D’Angelo, S.; Motti, M.L.; Meccariello, R. ω-3 and ω-6 Polyunsaturated Fatty Acids, Obesity and Cancer. Nutrients 2020, 12, 2751. [Google Scholar] [CrossRef]
- Yang, X.; Yi, X.; Zhang, F.; Li, F.; Lang, L.; Ling, M.; Lai, X.; Chen, L.; Quan, L.; Fu, Y.; et al. Cytochrome P450 epoxygenase-derived EPA and DHA oxylipins 17,18-epoxyeicosatetraenoic acid and 19,20-epoxydocosapentaenoic acid promote BAT thermogenesis and WAT browning through the GPR120-AMPKα signaling pathway. Food Funct. 2022, 13, 1232–1245. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Fasoli, L.; Di, X.; Kohler, I.; Osuna-Prieto, F.J.; Hankemeier, T.; Krekels, E.; Harms, A.C.; Yang, W.; Garcia-Lario, J.V.; Fernandez-Veledo, S.; et al. Omega-6 and omega-3 oxylipins as potential markers of cardiometabolic risk in young adults. Obesity 2022, 30, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, C.-Y.; Arita, M.; Kim, K.; Li, X.; Zhang, H.; Kang, J.X. An omega-3 polyunsaturated fatty acid derivative, 18-HEPE, protects against CXCR4-associated melanoma metastasis. Carcinogenesis 2018, 39, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Wiest, E.F.; Walsh-Wilcox, M.T.; Walker, M.K. Omega-3 polyunsaturated fatty acids protect against cigarette smoke-induced oxidative stress and vascular dysfunction. Toxicol. Sci. 2017, 156, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Panigrahy, D.; Mahakian, L.M.; Yang, J.; Liu, J.-Y.; Stephen Lee, K.S.; Wettersten, H.I.; Ulu, A.; Hu, X.; Tam, S.; et al. Epoxy metabolites of docosahexaenoic acid (DHA) inhibit angiogenesis, tumor growth, and metastasis. Proc. Natl. Acad. Sci. USA 2013, 110, 6530–6535. [Google Scholar] [CrossRef] [PubMed]
- Samokhvalov, V.; Jamieson, K.L.; Vriend, J.; Quan, S.; Seubert, J.M. CYP epoxygenase metabolites of docosahexaenoic acid protect HL-1 cardiac cells against LPS-induced cytotoxicity through SIRT1. Cell Death Discov. 2015, 1, 15054. [Google Scholar] [CrossRef]
- Lucas, D.; Goulitquer, S.; Marienhagen, J.; Fer, M.; Dreano, Y.; Schwaneberg, U.; Amet, Y.; Corcos, L. Stereoselective epoxidation of the last double bond of polyunsaturated fatty acids by human cytochromes P450. J. Lipid Res. 2010, 51, 1125–1133. [Google Scholar] [CrossRef]
- Bonafini, S.; Giontella, A.; Tagetti, A.; Marcon, D.; Montagnana, M.; Benati, M.; Gaudino, R.; Cavarzere, P.; Karber, M.; Rothe, M.; et al. Possible Role of CYP450 Generated Omega-3/Omega-6 PUFA Metabolites in the Modulation of Blood Pressure and Vascular Function in Obese Children. Nutrients 2018, 10, 1689. [Google Scholar] [CrossRef]
- Schäfer, S.M.G.; Sendetski, M.; Angioni, C.; Nüsing, R.; Geisslinger, G.; Scholich, K.; Sisignano, M. The omega-3 lipid 17,18-EEQ sensitizes TRPV1 and TRPA1 in sensory neurons through the prostacyclin receptor (IP). Neuropharmacology 2020, 166, 107952. [Google Scholar] [CrossRef]
- Adebesin, A.M.; Wesser, T.; Vjaykumar, J.; Konkel, A.; Paudyal, M.P.; Lossie, J.; Zhu, C.; Westphal, C.; Puli, N.; Fischer, R.; et al. Development of robust 17(R), 18(S) epoxyeicosatetraenoic acid (17,18-EEQ) analogues as potential clinical antiarrhythmic agents. J. Med. Chem. 2019, 62, 10124–10143. [Google Scholar] [CrossRef]
- Arnold, C.; Markovic, M.; Blossey, K.; Wallukat, G.; Fischer, R.; Dechend, R.; Konkel, A.; von Schacky, C.; Luft, F.C.; Muller, D.N.; et al. Arachidonic acid-metabolizing cytochrome P450 enzymes are targets of {omega}-3 fatty acids. J. Biol. Chem. 2010, 285, 32720–32733. [Google Scholar] [CrossRef] [PubMed]
- Hamabata, T.; Nakamura, T.; Tachibana, Y.; Horikami, D.; Murata, T. 5,6-DiHETE attenuates vascular hyperpermeability by inhibiting Ca2+ elevation in endothelial cells. J. Lipid Res. 2018, 59, 1864–1870. [Google Scholar] [CrossRef]
- Kobayashi, K.; Ashina, K.; Derouiche, S.; Hamabata, T.; Nakamura, T.; Nagata, N.; Takenouchi, S.; Tominaga, M.; Murata, T. 5,6-dihydroxy-8Z,11Z,14Z,17Z-eicosatetraenoic acid accelerates the healing of colitis by inhibiting transient receptor potential vanilloid 4-mediated signaling. FASEB J. 2021, 35, e21238. [Google Scholar] [CrossRef] [PubMed]
- Warner, J.B.; Hardesty, J.; Warner, D.; Song, Y.; McClain, C.; Kirpich, I. Effects of Dihydroxylated Fatty Acid Mediators on Ethanol-Induced Liver Injury in a Mouse Model of Alcoholic Liver Disease. FASEB J. 2020, 34, 1. [Google Scholar] [CrossRef]
- Caussy, C.; Chuang, J.-C.; Billin, A.; Hu, T.; Wang, Y.; Subramanian, G.M.; Djedjos, C.S.; Myers, R.P.; Dennis, E.A.; Loomba, R. Plasma eicosanoids as noninvasive biomarkers of liver fibrosis in patients with nonalcoholic steatohepatitis. Ther. Adv. Gastroenterol. 2020, 13, 1756284820923904. [Google Scholar] [CrossRef]
- Borsini, A. The role of soluble epoxide hydrolase and its inhibitors in depression. Brain Behav. Immun.-Health 2021, 16, 100325. [Google Scholar] [CrossRef]
- Liu, T.; Dogan, I.; Rothe, M.; Kunz, J.V.; Knauf, F.; Gollasch, M.; Luft, F.C.; Gollasch, B. Hemodialysis and Plasma Oxylipin Biotransformation in Peripheral Tissue. Metabolites 2022, 12, 34. [Google Scholar] [CrossRef]
- Ye, D.; Zhang, D.; Oltman, C.; Dellsperger, K.; Lee, H.-C.; VanRollins, M. Cytochrome P-450 Epoxygenase Metabolites of Docosahexaenoate Potently Dilate Coronary Arterioles by Activating Large-Conductance Calcium-Activated Potassium Channels. J. Pharmacol. Exp. Ther. 2002, 303, 768–776. [Google Scholar] [CrossRef]
- Westphal, C.; Konkel, A.; Schunck, W.-H. CYP-eicosanoids—A new link between omega-3 fatty acids and cardiac disease? Prostaglandins Other Lipid Med. 2011, 96, 99–108. [Google Scholar] [CrossRef]
- Agbor, L.N.; Walsh, M.T.; Boberg, J.R.; Walker, M.K. Elevated blood pressure in cytochrome P4501A1 knockout mice is associated with reduced vasodilation to omega−3 polyunsaturated fatty acids. Toxicol. Appl. Pharmacol. 2012, 263, 351–360. [Google Scholar] [CrossRef]
- Bah, T.M.; Allen, E.M.; Garcia-Jaramillo, M.; Perez, R.; Zarnegarnia, Y.; Davis, C.M.; Bloom, M.B.; Magana, A.A.; Choi, J.M.; Bobe, G.; et al. GPR39 Deficiency Impairs Memory and Alters Oxylipins and Inflammatory Cytokines Without Affecting Cerebral Blood Flow in a High-Fat Diet Mouse Model of Cognitive Impairment. Front. Cell Neurosci. 2022, 16, 893030. [Google Scholar] [CrossRef] [PubMed]
- Camacho-Muñoz, D.; Kiezel-Tsugunova, M.; Kiss, O.; Uddin, M.; Sundén, M.; Ryaboshapkina, M.; Lind, L.; Oscarsson, J.; Nicolaou, A. Omega-3 carboxylic acids and fenofibrate differentially alter plasma lipid mediators in patients with non-alcoholic fatty liver disease. FASEB J. 2021, 35, e21976. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Fu, Z.; Edin, M.L.; Liu, C.-H.; Wang, Z.; Shao, Z.; Fredrick, T.W.; Saba, N.J.; Morss, P.C.; Burnim, S.B.; et al. Cytochrome P450 Oxidase 2C inhibition adds to omega-3 long-chain polyunsaturated fatty acids protection against retinal and choroidal neovascularization. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 1919–1927. [Google Scholar] [CrossRef] [PubMed]
- Nieman, D.C.; Gillitt, N.D.; Chen, G.Y.; Zhang, Q.; Sakaguchi, C.A.; Stephan, E.H. Carbohydrate intake attenuates post-exercise plasma levels of cytochrome P450-generated oxylipins. PLoS ONE 2019, 14, e0213676. [Google Scholar] [CrossRef] [PubMed]
- Hu, N.; Hu, M.; Duan, R.; Liu, C.; Guo, H.; Zhang, M.; Yu, Y.; Wang, X.; Liu, L.; Liu, X. Increased levels of fatty acids contributed to induction of hepatic CYP3A4 activity induced by diabetes—In vitro evidence from HepG2 cell and Fa2N-4 cell lines. J. Phamacol. Sci. 2014, 124, 433–444. [Google Scholar] [CrossRef]
- Deol, P.; Evans, J.R.; Dhahbi, J.; Chellappa, K.; Han, D.S.; Spindler, S.; Sladek, F.M. Soybean oil is more obesogenic and diabetogenic than coconut oil and fructose in mouse: Potential role for the liver. PLoS ONE 2015, 10, e0132672. [Google Scholar] [CrossRef]
- Zangar, R.C.; Novak, R.F. Effects of fatty acids and ketone bodies on cytochromes P450 2B, 4A, and 2E1 expression in primary cultured rat hepatocytes. Arch. Biochem. Biophys. 1997, 337, 217–224. [Google Scholar] [CrossRef]
- Hoek-van den Hil, E.F.; van Schothorst, E.M.; van der Stelt, I.; Swarts, H.J.; van Vliet, M.; Amolo, T.; Vervoort, J.J.; Venema, D.; Hollman, P.C.; Rietjens, I.M.; et al. Direct comparison of metabolic health effects of the flavonoids quercetin, hesperetin, epicatechin, apigenin and anthocyanins in high-fat-diet-fed mice. Genes Nutr. 2015, 10, 23. [Google Scholar] [CrossRef]
- Maximos, S.; Chaumoun, M.; Gravel, S.; Turgeon, J.; Michaud, V. Tissue Specific Modulation of cyp2c and cyp3a mRNA Levels and Activities by Diet-Induced Obesity in Mice: The Impact of Type 2 Diabetes on Drug Metabolizing Enzymes in Liver and Extra-Hepatic Tissues. Pharmaceutics 2017, 9, 40. [Google Scholar] [CrossRef]
- Li, C.-C.; Lii, C.-K.; Liu, K.-L.; Yang, J.-J.; Chen, H.-W. DHA down-regulates phenobarbital-induced cytochrome P450 2B1 gene expression in rat primary hepatocytes by attenuating CAR translocation. Toxicol. Appl. Pharmacol. 2007, 225, 329–336. [Google Scholar] [CrossRef]
- McDougle, D.R.; Watson, J.E.; Abdeen, A.A.; Adili, R.; Caputo, M.P.; Krapf, J.E.; Johnson, R.W.; Kilian, K.A.; Holinstat, M.; Das, A. Anti-inflammatory omega-3 endocannabinoid epoxides. Proc. Natl. Acad. Sci. USA 2017, 114, E6034–E6043. [Google Scholar] [CrossRef] [PubMed]
- Brown, I.; Cascio, M.G.; Rotondo, D.; Pertwee, R.G.; Heys, S.D.; Wahle, K.W. Cannabinoids and omega-3/6 endocannabinoids as cell death and anticancer modulators. Prog. Lipid Res. 2013, 52, 80–109. [Google Scholar] [CrossRef] [PubMed]
- Larrieu, T.; Layé, S. Food for Mood: Relevance of Nutritional Omega-3 Fatty Acids for Depression and Anxiety. Front. Physiol. 2018, 9, 1047. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.E.; Kim, J.S.; Das, A. Emerging class of omega-3 fatty acid endocannabinoids & their derivatives. Prostaglandins Other Lipid Mediat. 2019, 143, 106337. [Google Scholar] [CrossRef]
- Kliewer, S.A.; Sundseth, S.S.; Jones, S.A.; Brown, P.J.; Wisely, G.B.; Koble, C.S.; Devchand, P.; Wahli, W.; Willson, T.M.; Lenhard, J.M.; et al. Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors alpha and gamma. Proc. Natl. Acad. Sci. USA 1997, 94, 4318–4323. [Google Scholar] [CrossRef]
- Yang, J.; Solaimani, P.; Dong, H.; Hammock, B.; Hankinson, O. Treatment of mice with 2,3,7,8-Tetrachlorodibenzo-p-dioxin markedly increases the levels of a number of cytochrome P450 metabolites of omega-3 polyunsaturated fatty acids in the liver and lung. J. Toxicol. Sci. 2013, 38, 833–836. [Google Scholar] [CrossRef]
- Hoek-van den Hil, E.F.; van Schothorst, E.M.; van der Stelt, I.; Swarts, H.J.M.; Venema, D.; Sailer, M.; Vervoort, J.J.M.; Hollman, P.C.H.; Rietjens, I.M.C.M.; Keijer, J. Quercetin decreases high-fat diet induced body weight gain and accumulation of hepatic and circulating lipids in mice. Genes Nutr. 2014, 9, 418. [Google Scholar] [CrossRef]
- Wang, T.; Han, Y.; Li, H.; Wang, Y.; Xue, T.; Che, N.X.; Chen, W.; Fan, Y.; Qiu, X.; Gong, J.; et al. Changes in bioactive lipid mediators in response to short-term exposure to ambient air particulate matter: A targeted lipidomic analysis of oxylipin signaling pathways. Environ. Int. 2021, 147, 106314. [Google Scholar] [CrossRef]
- Yao, H.-T.; Chang, Y.-W.; Lan, S.-J.; Chen, C.-T.; Hsu, J.T.A.; Yeh, T.-K. The inhibitory effect of polyunsaturated fatty acids on human CYP enzymes. Life Sci. 2006, 79, 2432–2440. [Google Scholar] [CrossRef]
- Hirunpanich, V.; Murakoso, K.; Sato, H. Inhibitory effect of docosahexaenoic acid (DHA) on the intestinal metabolism of midazolam: In vitro and in vivo studies in rat. Int. J. Pharm. 2008, 351, 133–143. [Google Scholar] [CrossRef]
- Hirunpanich, V.; Katagi, J.; Sethabouppha, B.; Sato, H. Demonstration of docosahexaenoic acid as a bioavailability enhancer for CYP3A substrates: In vitro and in vivo evidence using cyclosporin in rats. Drug Metab. Dispos. 2006, 34, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Ruparel, S.; Green, D.; Chen, P.; Hargreaves, K.M. The cytochrome P450 inhibitor, ketoconazole, inhibits oxidized linoleic acid metabolite-mediated peripheral inflammatory pain. Mol. Pain 2012, 8, 73. [Google Scholar] [CrossRef] [PubMed]




| CYP Subfamily | Human | Mouse | Rat |
|---|---|---|---|
| CYP1A | CYP1A1, 1A2 | Cyp1a1, 1a2 | Cyp1a1, 1a2 |
| CYP1B | CYP1B1 | Cyp1b1 | Cyp1b1 |
| CYP2A | CYP2A6, 2A7, 2A13 | Cyp2a4, 2a5, 2a12, 2a22 | Cyp2a1, 2a2, 2a3 |
| CYP2B | CYP2B6 | Cyp2b9, 2b10, 2b13, 2b19, 2b23 | Cyp2b1, 2b2, 2b3, 2b12, 2b15, 2b21 |
| CYP2C | CYP2C8, 2C9, 2C18, 2C19 | Cyp2c29, 2c37, 2c38, 2c39, 2c40, 2c44, 2c50, 2c54, 2c55, 2c65, 2c66, 2c67, 2c68, 2c69, 2c70 | Cyp2c6, 2c7, 2c11, 2c12, 2c13, 2c22, 2c23, 2c24, 2c78, 2c80 |
| CYP2D | CYP2D6 | Cyp2d9, 2d10, 2d11, 2d12, 2d13, 2d22, 2d26, 2d34, 2d40 | Cyp2d1, 2d2, 2d3, 2d4, 2d5 |
| CYP2E | CYP2E1 | Cyp2e1 | Cyp2e1 |
| CYP2J | CYP2J2 | Cyp2j5, 2j6, 2j7, 2j8, 2j9, 2j11, 2j12, 2j13 | Cyp2j3, 2j4, 2j10, 2j13, 2j16 |
| CYP2S | CYP2S1 | Cyp2s1 | Cyp2s1 |
| CYP2U | CYP2U1 | Cyp2u1 | Cyp2u1 |
| CYP3A | CYP3A4, 3A5, 3A7, 3A43 | Cyp3a11, 3a13, 3a16, 3a25, 3a41, 3a44, 3a57, 3a59 | Cyp3a1, 3a2, 3a9, 3a18, 3a23, 3a62, 3a73 |
| PUFA | Abbreviation | PUFA Type | Oxylipins Produced by CYPs |
|---|---|---|---|
| Linoleic acid | LA | n-6 | EpOME, DiHOME, HpODE, HODE, oxoODE |
| Arachidonic acid | AA | n-6 | HETE, oxoETE, EET, DiHET |
| alpha-linolenic acid | ALA | n-3 | EpODE, DiHODE, HpOTrE, HOTrE, oxoOTrE |
| Eicosapentaenoic acid | EPA | n-3 | EpETE, DiHETE, HEPE |
| Docosahexaenoic acid | DHA | n-3 | EpDPA, DiHDPA |
| Oxylipin | CAS Number | CYPs/Enzymes | References | Effects | References |
|---|---|---|---|---|---|
| 5,6-EpETE | N/A | 2C9, 2J2 | [179] |
| |
| 8,9-EpETE | 851378-93-3 | 1A2, 2C9, 2C19, 2E1, 2J2, 3A4 | [179] |
| |
| 11,12-EpETE | 504435-15-8 | 1A2, 2C8, 2C9, 2C19, 2E1, 2J2, 3A4 | [179] |
| [180] |
| 14,15-EpETE | 131339-24-7 | 1A2, 2C8, 2C9, 2C19, 2E1, 2J2, 3A4 | [179] |
| |
| 17,18-EpETE | 131339-23-6 | 1A1, 1A2, 2C8, 2C9, 2C19, 2D6, 2E1, 2J2, 3A4 | [179] |
| [173,181,182] |
| 5,6-DiHETE | 845673-97-4 | sEH | [183] |
| [184,185] |
| 8,9-DiHETE | 867350-87-6 | sEH | [183] |
| [186] |
| 11,12-DiHETE | 867350-92-3 | sEH | [183] |
| [187] |
| 14,15-DiHETE | N/A | sEH | [183] |
| [174] |
| 17,18-DiHETE | N/A | sEH | [183] |
| [174] |
| 18-HEPE | 141110-17-0 | CYP2C, 1A2, 2B | [169] |
| [175] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eccles, J.A.; Baldwin, W.S. Detoxification Cytochrome P450s (CYPs) in Families 1–3 Produce Functional Oxylipins from Polyunsaturated Fatty Acids. Cells 2023, 12, 82. https://doi.org/10.3390/cells12010082
Eccles JA, Baldwin WS. Detoxification Cytochrome P450s (CYPs) in Families 1–3 Produce Functional Oxylipins from Polyunsaturated Fatty Acids. Cells. 2023; 12(1):82. https://doi.org/10.3390/cells12010082
Chicago/Turabian StyleEccles, Jazmine A., and William S. Baldwin. 2023. "Detoxification Cytochrome P450s (CYPs) in Families 1–3 Produce Functional Oxylipins from Polyunsaturated Fatty Acids" Cells 12, no. 1: 82. https://doi.org/10.3390/cells12010082
APA StyleEccles, J. A., & Baldwin, W. S. (2023). Detoxification Cytochrome P450s (CYPs) in Families 1–3 Produce Functional Oxylipins from Polyunsaturated Fatty Acids. Cells, 12(1), 82. https://doi.org/10.3390/cells12010082








