Could Endogenous Glucocorticoids Influence SARS-CoV-2 Infectivity?
Abstract
1. Introduction
2. Various Lines of Research Suggest That Endogenous Glucocorticoids and Synthetic Analogs Thereof May Impact SARS-CoV-2 Infectivity by Interacting with the Host and Viral Components
2.1. Dexamethasone May Interact with the Host to Reduce ACE2 Expression
2.2. Dexamethasone May Directly Interact with SARS-CoV-2 Components
2.3. Dxamethasone and Cortisol Bind to Multiple Sites on SARS-CoV-2 S1 Protein to Cooperatively Inhibit S1-ACE2 Interaction
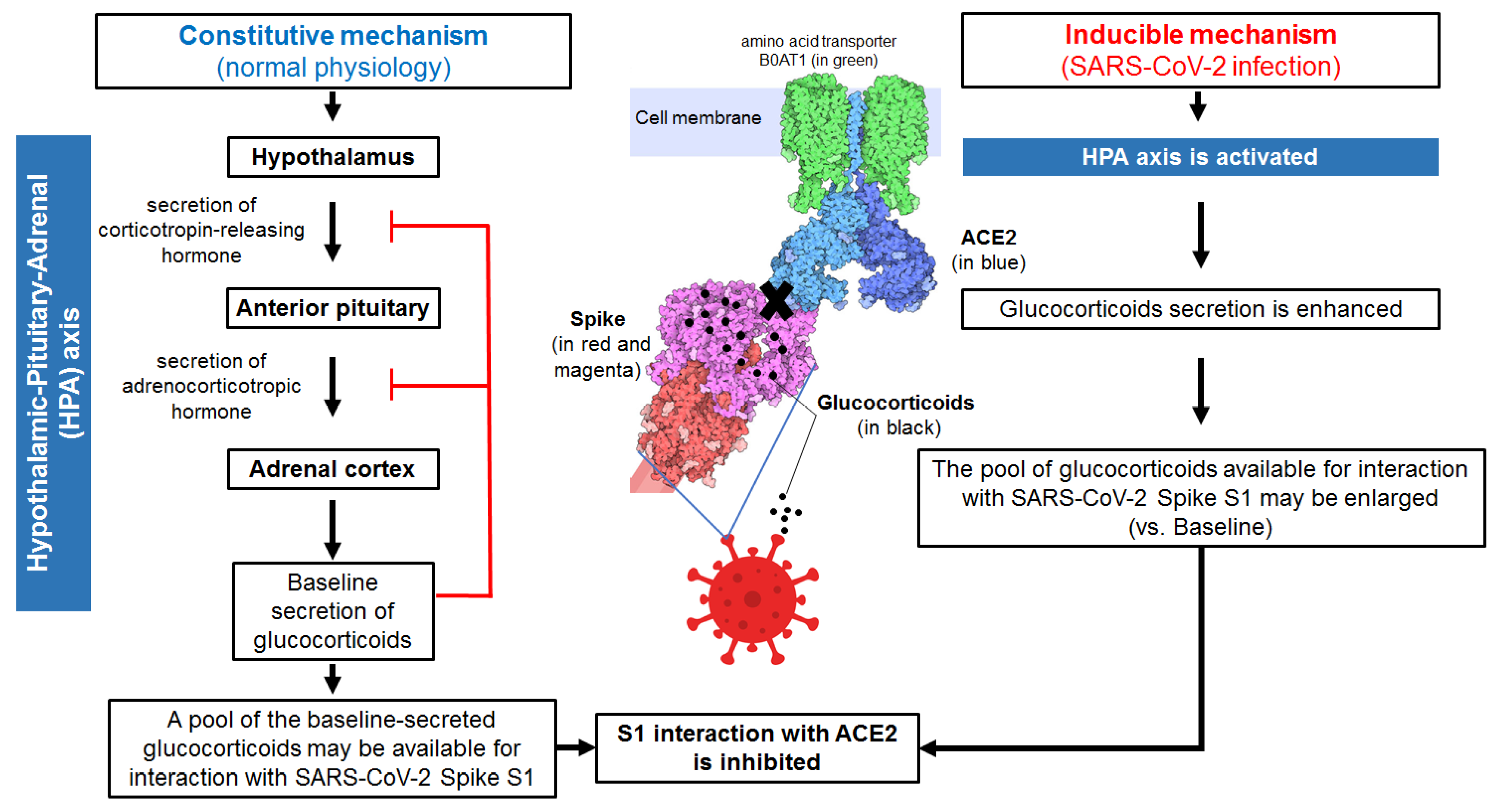
3. Baseline Levels of Endogenous Glucocorticoids and SARS-CoV-2-Induced Glucocorticoid Overproduction May Influence SARS-CoV-2 Interaction with ACE2
3.1. Glucocorticoids Constitutively Secreted by Adrenal Glands May Be Available for a Direct Interaction with SARS-CoV-2 Spike Immediately after Infection of the Host
3.2. Glucocorticoids Inhibition of SARS-CoV-2 S1 Interaction with ACE2 May Be a Constitutive/Inducible Innate Immunity Mechanism
- (i)
- S1 conformational changes may be induced which increase the rigidity of Spike protein reducing its affinity for ACE2.
- (ii)
- S1 may adopt ACE2-inaccessible conformational states (in contrast to ACE2-accessible conformational states, such structures have been proposed to not involve canyons between RBDs [22]), which would make SARS-CoV-2 less infectious.
- (iii)
- The affinity for ACE2 may be reduced for S1 structures having pockets occupied by glucocorticoids.
- (iv)
- SARS-CoV-2 infectivity may be significantly reduced (Figure 1).
4. Conclusions
5. Outlook
- (a)
- Could the proposed constitutive innate defence mechanism involving endogenous glucocorticoids contribute to asymptomatic COVID-19?
- (b)
- Could glucocorticoids have influenced the infectivity of some SARS-CoV-2 variants of concern?
- (c)
- Could blood factors such as plasma proteins acting as glucocorticoid transporters (e.g., corticosteroid-binding globulin, albumin, sex hormone-binding globulin) affect the binding of glucocorticoids to S1?
- (d)
- Do glucocorticoids act in concert with other ligands potentially capable of binding to S1, such as dietary polyunsaturated fatty acid, immunoreactive antibodies or even non-antibodies (proteins, peptides) in the blood, to shift the equilibrium towards stable, locked SARS-CoV-2 S1structures that prevent virus infectivity?
- (e)
- Do endogenous glucocorticoids serve a new innate immune function that protects against a broad spectrum of coronaviruses and their variants that utilize Spike for infection of the host?These notions may be useful for the design of new antivirals for coronavirus diseases.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stahn, C.; Buttgereit, F. Genomic and nongenomic effects of glucocorticoids. Nat. Clin. Pract. Rheumatol. 2008, 4, 525–533. [Google Scholar] [CrossRef]
- Taves, M.D.; Gomez-Sanchez, C.E.; Soma, K.K. Extra-adrenal glucocorticoids and mineralocorticoids: Evidence for local synthesis, regulation, and function. Am. J. Physiol. Endocrinol. Metab. 2011, 301, E11–E24. [Google Scholar] [CrossRef]
- Shimba, A.; Ikuta, K. Control of immunity by glucocorticoids in health and disease. Semin. Immunopathol. 2020, 42, 669–680. [Google Scholar] [CrossRef]
- Shimba, A.; Ikuta, K. Immune-enhancing effects of glucocorticoids in response to day-night cycles and stress. Int. Immunol. 2020, 32, 703–708. [Google Scholar] [CrossRef]
- Coutinho, A.E.; Chapman, K.E. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol. Cell. Endocrinol. 2011, 335, 2–13. [Google Scholar] [CrossRef]
- Okoye, I.S.; Xu, L.; Walker, J.; Elahi, S. The glucocorticoids prednisone and dexamethasone differentially modulate T cell function in response to anti-PD-1 and anti-CTLA-4 immune checkpoint blockade. Cancer Immunol. Immunother. 2020, 69, 1423–1436. [Google Scholar] [CrossRef]
- Prescott, H.C.; Rice, T.W. Corticosteroids in COVID-19 ARDS: Evidence and Hope During the Pandemic. JAMA 2020, 324, 1292–1295. [Google Scholar] [CrossRef]
- Lee, K.H.; Yoon, S.; Jeong, G.H.; Kim, J.Y.; Han, Y.J.; Hong, S.H.; Ryu, S.; Kim, J.S.; Lee, J.Y.; Yang, J.W.; et al. Efficacy of Corticosteroids in Patients with SARS, MERS and COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2392. [Google Scholar] [CrossRef]
- Arabi, Y.M.; Mandourah, Y.; Al-Hameed, F.; Sindi, A.A.; Almekhlafi, G.A.; Hussein, M.A.; Jose, J.; Pinto, R.; Al-Omari, A.; Kharaba, A.; et al. Corticosteroid Therapy for Critically Ill Patients with Middle East Respiratory Syndrome. Am. J. Respir. Crit. Care Med. 2018, 197, 757–767. [Google Scholar] [CrossRef]
- Pastores, S.M.; Annane, D.; Rochwerg, B. Guidelines for the Diagnosis and Management of Critical Illness-Related Corticosteroid Insufficiency (CIRCI) in Critically Ill Patients (Part II): Society of Critical Care Medicine (SCCM) and European Society of Intensive Care Medicine (ESICM) 2017. Crit. Care Med. 2018, 46, 146–148. [Google Scholar] [CrossRef]
- Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; Elmahi, E.; et al. Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Cain, D.W.; Cidlowski, J.A. After 62 years of regulating immunity, dexamethasone meets COVID-19. Nat. Rev. Immunol. 2020, 20, 587–588. [Google Scholar] [CrossRef] [PubMed]
- Sarker, H.; Panigrahi, R.; Hardy, E.; Glover, J.N.M.; Elahi, S.; Fernandez-Patron, C. Glucocorticoids Bind to SARS-CoV-2 S1 at Multiple Sites Causing Cooperative Inhibition of SARS-CoV-2 S1 Interaction With ACE2. Front. Immunol. 2022, 13, 906687. [Google Scholar] [CrossRef] [PubMed]
- Shahbaz, S.; Xu, L.; Osman, M.; Sligl, W.; Shields, J.; Joyce, M.; Tyrrell, D.L.; Oyegbami, O.; Elahi, S. Erythroid precursors and progenitors suppress adaptive immunity and get invaded by SARS-CoV-2. Stem Cell Rep. 2021, 16, 1165–1181. [Google Scholar] [CrossRef] [PubMed]
- Fadaka, A.O.; Sibuyi, N.R.S.; Madiehe, A.M.; Meyer, M. Computational insight of dexamethasone against potential targets of SARS-CoV-2. J. Biomol. Struct. Dyn. 2022, 40, 875–885. [Google Scholar] [CrossRef]
- Ghosh, R.; Chakraborty, A.; Biswas, A.; Chowdhuri, S. Potential therapeutic use of corticosteroids as SARS CoV-2 main protease inhibitors: A computational study. J. Biomol. Struct. Dyn. 2022, 40, 2053–2066. [Google Scholar] [CrossRef]
- Elmaaty, A.A.; Alnajjar, R.; Hamed, M.I.A.; Khattab, M.; Khalifa, M.M.; Al-Karmalawy, A.A. Revisiting activity of some glucocorticoids as a potential inhibitor of SARS-CoV-2 main protease: Theoretical study. RSC Adv. 2021, 11, 10027–10042. [Google Scholar] [CrossRef]
- Junaid, M.; Akter, Y.; Siddika, A.; Nayeem, S.M.A.; Nahrin, A.; Afrose, S.S.; Ezaj, M.M.A.; Alam, M.S. Nature-Derived Hit, Lead, and Drug-Like Small Molecules: Current Status and Future Aspects Against Key Target Proteins of Coronaviruses. Mini Rev. Med. Chem. 2022, 22, 498–549. [Google Scholar] [CrossRef]
- Martin, V.; Sanz-Novo, M.; Leon, I.; Redondo, P.; Largo, A.; Barrientos, C. Computational study on the affinity of potential drugs to SARS-CoV-2 main protease. J. Phys. Condens. Matter 2022, 34, 294005. [Google Scholar] [CrossRef]
- Ghosh, R.; Chakraborty, A.; Biswas, A.; Chowdhuri, S. Computer aided identification of potential SARS CoV-2 main protease inhibitors from diterpenoids and biflavonoids of Torreya nucifera leaves. J. Biomol. Struct. Dyn. 2022, 40, 2647–2662. [Google Scholar] [CrossRef]
- Shoemark, D.K.; Colenso, C.K.; Toelzer, C.; Gupta, K.; Sessions, R.B.; Davidson, A.D.; Berger, I.; Schaffitzel, C.; Spencer, J.; Mulholland, A.J. Molecular Simulations suggest Vitamins, Retinoids and Steroids as Ligands of the Free Fatty Acid Pocket of the SARS-CoV-2 Spike Protein. Angew. Chem. Int. Ed. Engl. 2021, 60, 7098–7110. [Google Scholar] [CrossRef]
- Toelzer, C.; Gupta, K.; Yadav, S.K.N.; Borucu, U.; Davidson, A.D.; Kavanagh Williamson, M.; Shoemark, D.K.; Garzoni, F.; Staufer, O.; Milligan, R.; et al. Free fatty acid binding pocket in the locked structure of SARS-CoV-2 spike protein. Science 2020, 370, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hu, S.; Wang, J.; Xue, Z.; Wang, C.; Wang, N. Dexamethasone inhibits SARS-CoV-2 spike pseudotyped virus viropexis by binding to ACE2. Virology 2021, 554, 83–88. [Google Scholar] [CrossRef]
- Nie, J.; Li, Q.; Wu, J.; Zhao, C.; Hao, H.; Liu, H.; Zhang, L.; Nie, L.; Qin, H.; Wang, M.; et al. Establishment and validation of a pseudovirus neutralization assay for SARS-CoV-2. Emerg. Microbes. Infect. 2020, 9, 680–686. [Google Scholar] [CrossRef]
- Diamond, M.S.; Kanneganti, T.D. Innate immunity: The first line of defense against SARS-CoV-2. Nat. Immunol. 2022, 23, 165–176. [Google Scholar] [CrossRef]
- Tomalka, J.A.; Suthar, M.S.; Diamond, M.S.; Sekaly, R.P. Innate antiviral immunity: How prior exposures can guide future responses. Trends Immunol. 2022, 43, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Paludan, S.R.; Pradeu, T.; Masters, S.L.; Mogensen, T.H. Constitutive immune mechanisms: Mediators of host defence and immune regulation. Nat. Rev. Immunol. 2021, 21, 137–150. [Google Scholar] [CrossRef]
- Iwasaki, A.; Medzhitov, R. Control of adaptive immunity by the innate immune system. Nat. Immunol. 2015, 16, 343–353. [Google Scholar] [CrossRef]
- Walls, A.C.; Park, Y.J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 183, 1735. [Google Scholar] [CrossRef]
- Yan, R.; Zhang, Y.; Li, Y.; Xia, L.; Guo, Y.; Zhou, Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science 2020, 367, 1444–1448. [Google Scholar] [CrossRef]
- Wrapp, D.; Wang, N.; Corbett, K.S.; Goldsmith, J.A.; Hsieh, C.L.; Abiona, O.; Graham, B.S.; McLellan, J.S. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science 2020, 367, 1260–1263. [Google Scholar] [CrossRef]
- Paludan, S.R.; Mogensen, T.H. Constitutive and latent immune mechanisms exert ‘silent’ control of virus infections in the central nervous system. Curr. Opin. Immunol. 2021, 72, 158–166. [Google Scholar] [CrossRef]
- Silverman, M.N.; Pearce, B.D.; Biron, C.A.; Miller, A.H. Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol. 2005, 18, 41–78. [Google Scholar] [CrossRef]
- Tan, T.; Khoo, B.; Mills, E.G.; Phylactou, M.; Patel, B.; Eng, P.C.; Thurston, L.; Muzi, B.; Meeran, K.; Prevost, A.T.; et al. Association between high serum total cortisol concentrations and mortality from COVID-19. Lancet Diabetes Endocrinol. 2020, 8, 659–660. [Google Scholar] [CrossRef]
- Yavropoulou, M.P.; Filippa, M.G.; Mantzou, A.; Ntziora, F.; Mylona, M.; Tektonidou, M.G.; Vlachogiannis, N.I.; Paraskevis, D.; Kaltsas, G.A.; Chrousos, G.P.; et al. Alterations in cortisol and interleukin-6 secretion in patients with COVID-19 suggestive of neuroendocrine-immune adaptations. Endocrine 2022, 75, 317–327. [Google Scholar] [CrossRef]
| Row | Method(s) | Authors’ Main Results and Conclusions |
|---|---|---|
| 1 | Fpocket algorithm; Molecular docking using AutoDockVina and AutoDockTools; Molecular dynamics using GPU-accelerated AMBER, PyRED server, SHAKE algorithm, VMD, Ligplot, and PyMOL; Binding energy calculations, based on MM/GBSA | (i) In silico identification of 52 unique pockets, with high affinity for cortisol and dexamethasone, which are located and distributed on the RBD, NTD, RBD-RBD interface and NTD-RBD interface. (ii) The pockets interact with dexamethasone and cortisol with different affinity. (iii) The specificity of the pocket for dexamethasone or for cortisol depends on the unique glucocorticoid side chain-pocket interactions and the resultant binding affinity. |
| 2 | Limited proteolysis-coupled LC-MS (and methods in Row 1) | (i) Confirmation of several cortisol-binding pockets (e.g., HCY_8, HCY_29, HCY35, HCY 59, HCY_88, HCY_112, HCY_153, HCY_161), and identification of their amino acid sequences. (ii) Suggestion that some mutations in Delta S1 variant (E156-, F157-, R158G) are likely to affect dexamethasone and cortisol binding to S1. (iii) Suggestion that some mutations in Omicron S1 variant (H69-, T95I, G142-, Y144-, N211-, L212I, S371L, S373P, S375F, S477N, T478K, E484A, T547K) are likely to affect glucocorticoid binding to S1. (iv) Suggestion that some mutations (K417N, E484K, and N501Y) in Beta S1 variant are unlikely to affect dexamethasone and cortisol binding to S1. |
| 3 | Cortisol-Acetylcholinesterase conjugate assay, using Cortisol Express ELISA kit (Cayman Chemicals, Ann Arbor, MI, USA); Protein thermal stability assays; GloMelt™ Thermal Shift Protein Stability Kit (Biotium, Fremont, CA, USA); Thermal stability of SARS-CoV-2 S1 assisted by detection with SDS-PAGE; ACE2 Activity Assay Kit (Fluorometric) (Abcam, Cambridge, UK) | (i) Biochemical confirmation that cortisol directly binds to S1. (ii) Dexamethasone and cortisol promote heat-induced unfolding of S1. (iii) Neither cortisol nor dexamethasone compromises ACE2 enzymatic function. |
| 4 | SARS-CoV-2 S1 Protein-ACE2 Binding Inhibitor Screening Kit (BioVision, Milpitas, CA, USA) | (i) Combined dexamethasone and cortisol can inhibit the S1-ACE2 interaction more than each individual glucocorticoid alone. For instance, at 1 nM, cortisol and dexamethasone cooperatively reduce S1 binding to ACE2, to levels comparable to 100 nM cortisol or 100 nM S1 polyclonal antibodies. Ten nM dexamethasone + 1 nM cortisol reduces S1/ACE2 binding from 100% to 33% (~77% reduction). At concentrations above 100 nM, the combination of dexamethasone and cortisol does not produce any difference in inhibition compared to dexamethasone or cortisol alone at the same concentrations. (ii) Cocktails of glucocorticoids and a human chimeric monoclonal anti-SARS-CoV-2 S1 antibody cooperatively increase the inhibition of SARS-CoV-2 S1-ACE2 interaction. For example, the mixture of 10 nM cortisol and 100 nM human chimeric antibody inhibits S1/ACE2 binding from 100% to 27% (~73% reduction), well below the levels of 100 nM S1 chimeric antibody alone. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hardy, E.; Fernandez-Patron, C. Could Endogenous Glucocorticoids Influence SARS-CoV-2 Infectivity? Cells 2022, 11, 2955. https://doi.org/10.3390/cells11192955
Hardy E, Fernandez-Patron C. Could Endogenous Glucocorticoids Influence SARS-CoV-2 Infectivity? Cells. 2022; 11(19):2955. https://doi.org/10.3390/cells11192955
Chicago/Turabian StyleHardy, Eugenio, and Carlos Fernandez-Patron. 2022. "Could Endogenous Glucocorticoids Influence SARS-CoV-2 Infectivity?" Cells 11, no. 19: 2955. https://doi.org/10.3390/cells11192955
APA StyleHardy, E., & Fernandez-Patron, C. (2022). Could Endogenous Glucocorticoids Influence SARS-CoV-2 Infectivity? Cells, 11(19), 2955. https://doi.org/10.3390/cells11192955





