Meta-Analysis of Adipose Tissue Derived Cell-Based Therapy for the Treatment of Knee Osteoarthritis
Abstract
1. Introduction
1.1. The Burden of Osteoarthritis
1.2. Mesenchymal Stem Cells
1.3. Adipose Tissue Derived MSCs
2. Materials and Methods
2.1. Database and Inclusion Criteria
- Any studies which investigated use of AMSCs on humans for the treatment of knee joint osteoarthritis
- Any study that included the use of stromal vascular fraction (SVF) or microfragmented adipose tissue
- Any study which was clinical in nature
- Any study not conducted on human
- Studies which investigated use of MSCs which were not of adipose origin
- Any case studies and reviews
- Studies in which the data sets were either incomplete or inaccessible such as conference abstracts and ongoing randomised controlled trials (RCTs)
2.2. Quality Assessment
2.3. Statistical Analysis
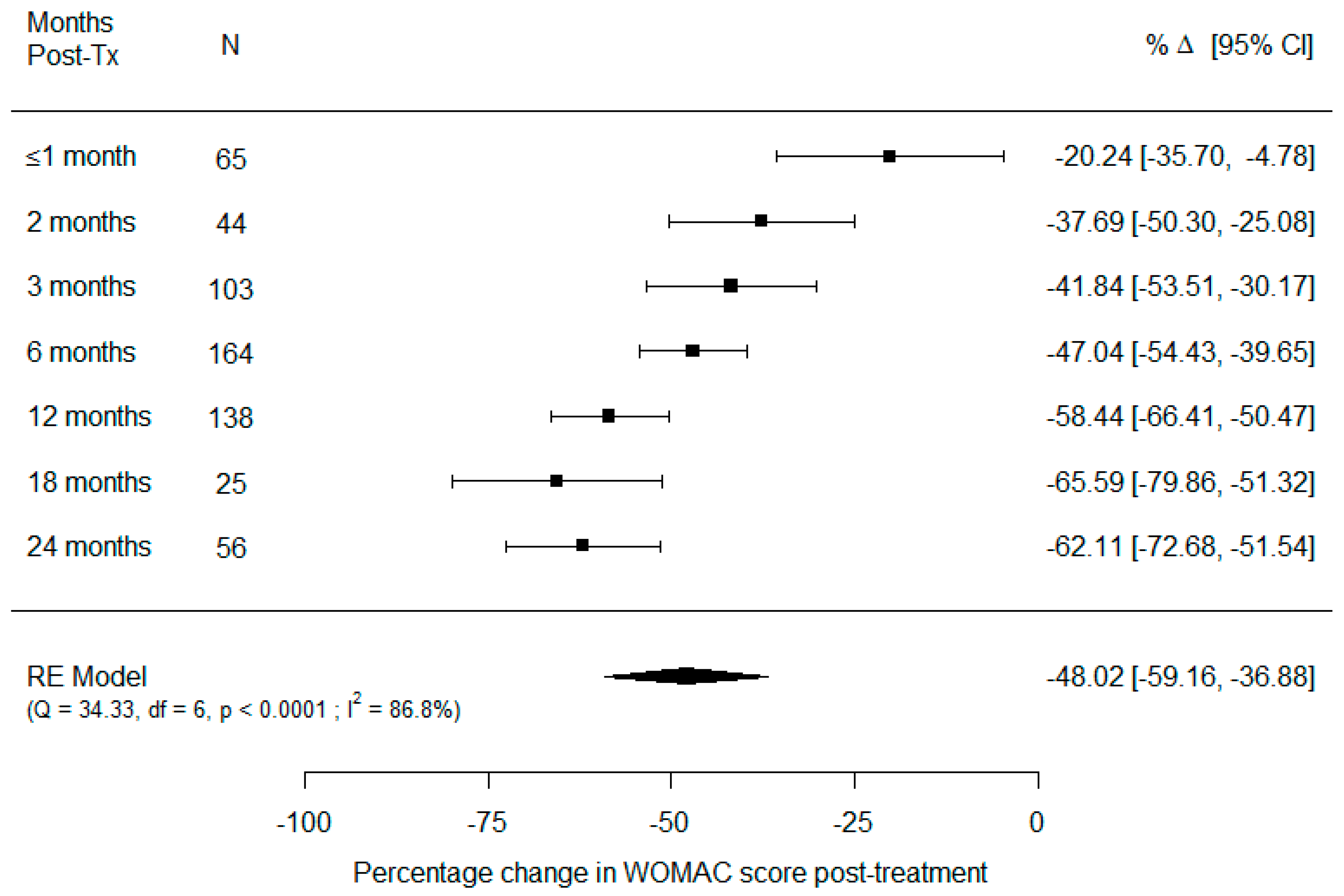
3. Results
3.1. Classification of Osteoarthritis
3.2. Follow-Up
3.3. Adverse Events
3.4. Outcome Measures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- exp cartilage/ or exp “bone and bones”/
- exp Injections, Intra-Articular/
- exp Osteoarthritis, Hip/ or exp Osteoarthritis/ or exp Osteoarthritis, Spine/ or exp Osteoarthritis, Knee/
- exp Mesenchymal Stem Cells/ or exp Mesenchymal Stem Cell Transplantation/
- exp Transplantation, Homologous/ or exp Stem Cell Transplantation/ or exp Transplantation, Autologous/ or exp Mesenchymal Stem Cell Transplantation/
- exp Adipose Tissue/ or adipose.mp.
- adipo*.tw.
- exp Autografts/
- exp Heterografts/
- 4 or 5 or 8 or 9
- 1 or 2 or 10
- 6 or 7
- 11 and 12
- 3 and 13
- Limit 14 to (English language and humans)
- exp cartilage/
- exp intraarticular drug administration/
- exp knee osteoarthritis/
- exp mesenchymal stem cell transplantation/ or exp mesenchymal stem cell/
- exp autograft/
- exp adipose tissue/
- adipo*.tw.
- 4 or 5
- 1 or 2 or 8
- 6 or 7
- 9 and 10
- 3 and 11
- Limit 12 to (human and English language)
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- WHO. Chronic Rheumatic Conditions; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Veronese, N.; Stubbs, B.; Solmi, M.; Smith, T.O.; Noale, M.; Cooper, C.; Maggi, S. Association between lower limb osteoarthritis and incidence of depressive symptoms: Data from the osteoarthritis initiative. Age Ageing 2017, 46, 470–476. [Google Scholar] [CrossRef]
- Kye, S.-Y.; Park, K. Suicidal ideation and suicidal attempts among adults with chronic diseases: A cross-sectional study. Compr. Psychiatry 2017, 73, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Schieir, O.; Tosevski, C.; Glazier, R.H.; Hogg-Johnson, S.; Badley, E.M. Incident myocardial infarction associated with major types of arthritis in the general population: A systematic review and meta-analysis. Ann. Rheum. Dis. 2017, 76, 1396–1404. [Google Scholar] [CrossRef]
- Hubertsson, J.; Turkiewicz, A.; Petersson, I.F.; Englund, M. Understanding Occupation, Sick Leave, and Disability Pension Due to Knee and Hip Osteoarthritis from a Sex Perspective. Arthritis Rheum. 2017, 69, 226–233. [Google Scholar] [CrossRef]
- Zhao, X.; Shah, D.; Gandhi, K.; Wei, W.; Dwibedi, N.; Webster, L.; Sambamoorthi, U. Clinical, humanistic, and economic burden of osteoarthritis among noninstitutionalized adults in the United States. Osteoarthr. Cartil. 2019, 27, 1618–1626. [Google Scholar] [CrossRef]
- Salmon, J.; Rat, A.; Achit, H.; Ngueyon-Sime, W.; Gard, C.; Guillemin, F.; Jolly, D.; Fautrel, B. Health resource use and costs of symptomatic knee and/or hip osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1011–1017. [Google Scholar] [CrossRef]
- Loza, E.; Abásolo, L.; Maese, J.; Carmona, L.; Artrocad Study Group; Lopez-Gomez, J.M.; Batlle-Gualda, E. Economic burden of knee and hip osteoarthritis in spain. Arthritis Rheum. 2009, 61, 158–165. [Google Scholar] [CrossRef]
- United Nations. Ageing|United Nations. Available online: https://www.un.org/en/global-issues/ageing (accessed on 5 May 2021).
- Ackerman, I.N.; Pratt, C.; Gorelik, A.; Liew, D. Projected Burden of Osteoarthritis and Rheumatoid Arthritis in Australia: A Population-Level Analysis. Arthritis Rheum. 2018, 70, 877–883. [Google Scholar] [CrossRef]
- Turkiewicz, A.; Petersson, I.; Björk, J.; Hawker, G.; Dahlberg, L.; Lohmander, L.; Englund, M. Current and future impact of osteoarthritis on health care: A population-based study with projections to year 2032. Osteoarthr. Cartil. 2014, 22, 1826–1832. [Google Scholar] [CrossRef]
- Hootman, J.M.; Helmick, C.G. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2005, 54, 226–229. [Google Scholar] [CrossRef] [PubMed]
- Sen, R.; Hurley, J.A. Osteoarthritis; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Evans, J.T.; Walker, R.W.; Blom, A.W.; Sayers, A.; Whitehouse, M.R. How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 2019, 393, 655–663. [Google Scholar] [CrossRef]
- Kapoor, M.; Martel-Pelletier, J.; Lajeunesse, D.; Pelletier, J.-P.; Fahmi, H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat. Rev. Rheumatol. 2010, 7, 33–42. [Google Scholar] [CrossRef]
- Kobayashi, M.; Squires, G.R.; Mousa, A.; Tanzer, M.; Zukor, D.J.; Antoniou, J.; Feige, U.; Poole, A.R. Role of interleukin-1 and tumor necrosis factor α in matrix degradation of human osteoarthritic cartilage. Arthritis Rheum. 2005, 52, 128–135. [Google Scholar] [CrossRef]
- Martel-Pelletier, J.; Lajeunesse, D.; Pelletier, J.-P. Arthritis and Allied Conditions: A Textbook of Rheumatology, 15th ed.; Williams & Wilkins: Philadelphia, PA, USA, 2005. [Google Scholar]
- Jacques, C.; Gosset, M.; Berenbaum, F.; Gabay, C. The Role of IL-1 and IL-1Ra in Joint Inflammation and Cartilage Degradation. Vitam. Horm. 2006, 74, 371–403. [Google Scholar] [CrossRef]
- Li, H.; Shen, S.; Fu, H.; Wang, Z.; Li, X.; Sui, X.; Yuan, M.; Liu, S.; Wang, G.; Guo, Q. Immunomodulatory Functions of Mesenchymal Stem Cells in Tissue Engineering. Stem Cells Int. 2019, 2019, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Hui, W.; Young, A.D.; Rowan, A.; Xu, X.; Cawston, E.T.; Proctor, C.J. Oxidative changes and signalling pathways are pivotal in initiating age-related changes in articular cartilage. Ann. Rheum. Dis. 2014, 75, 449–458. [Google Scholar] [CrossRef]
- Loeser, R.F. Aging and osteoarthritis: The role of chondrocyte senescence and aging changes in the cartilage matrix. Osteoarthr. Cartil. 2009, 17, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Vincent, T.L. IL-1 in osteoarthritis: Time for a critical review of the literature. F1000Research 2019, 8, 934. [Google Scholar] [CrossRef] [PubMed]
- Philp, A.; Davis, E.T.; Jones, S. Developing anti-inflammatory therapeutics for patients with osteoarthritis. Rheumatology 2016, 56, 869–881. [Google Scholar] [CrossRef]
- Pittenger, M.F.; Mackay, A.M.; Beck, S.C.; Jaiswal, R.K.; Douglas, R.; Mosca, J.D.; Moorman, M.A.; Simonetti, D.W.; Craig, S.; Marshak, D.R. Multilineage Potential of Adult Human Mesenchymal Stem Cells. Science 1999, 284, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Cho, D.-I.; Kim, M.R.; Jeong, H.-Y.; Jeong, H.C.; Jeong, M.H.; Yoon, S.H.; Kim, Y.S.; Ahn, Y. Mesenchymal stem cells reciprocally regulate the M1/M2 balance in mouse bone marrow-derived macrophages. Exp. Mol. Med. 2014, 46, e70. [Google Scholar] [CrossRef] [PubMed]
- Abumaree, M.H.; Al Jumah, M.A.; Kalionis, B.; Jawdat, D.; Al Khaldi, A.; Abomaray, F.M.; Fatani, A.S.; Chamley, L.W.; Knawy, B.A. Human Placental Mesenchymal Stem Cells (pMSCs) Play a Role as Immune Suppressive Cells by Shifting Macrophage Differentiation from Inflammatory M1 to Anti-inflammatory M2 Macrophages. Stem Cell Rev. Rep. 2013, 9, 620–641. [Google Scholar] [CrossRef] [PubMed]
- Saldaña, L.; Bensiamar, F.; Vallés, G.; Mancebo, F.J.; García-Rey, E.; Vilaboa, N. Immunoregulatory potential of mesenchymal stem cells following activation by macrophage-derived soluble factors. Stem Cell Res. Ther. 2019, 10, 58. [Google Scholar] [CrossRef] [PubMed]
- Tse, W.T.; Pendleton, J.D.; Beyer, W.M.; Egalka, M.C.; Guinan, E.C. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: Implications in transplantation. Transplantation 2003, 75, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Le Blanc, K.; Tammik, L.; Sundberg, B.; Haynesworth, S.E.; Ringden, O. Mesenchymal Stem Cells Inhibit and Stimulate Mixed Lymphocyte Cultures and Mitogenic Responses Independently of the Major Histocompatibility Complex. Scand. J. Immunol. 2003, 57, 11–20. [Google Scholar] [CrossRef]
- Najar, M.; Rouas, R.; Raicevic, G.; Boufker, H.I.; Lewalle, P.; Meuleman, N.; Bron, D.; Toungouz, M.; Martiat, P.; Lagneaux, L. Mesenchymal stromal cells promote or suppress the proliferation of T lymphocytes from cord blood and peripheral blood: The importance of low cell ratio and role of interleukin-6. Cytotherapy 2009, 11, 570–583. [Google Scholar] [CrossRef] [PubMed]
- Castro-Oropeza, R.; Vazquez-Santillan, K.; Díaz-Gastelum, C.; Melendez-Zajgla, J.; Zampedri, C.; Ferat-Osorio, E.; Rodríguez-González, A.; Arriaga-Pizano, L.; Maldonado, V. Adipose-derived mesenchymal stem cells promote the malignant phenotype of cervical cancer. Sci. Rep. 2020, 10, 14205. [Google Scholar] [CrossRef]
- Zhao, M.; Sachs, P.C.; Wang, X.; Dumur, C.I.; Idowu, M.O.; Robila, V.; Francis, M.P.; Ware, J.; Beckman, M.; Rizki, A.; et al. Mesenchymal stem cells in mammary adipose tissue stimulate progression of breast cancer resembling the basal-type. Cancer Biol. Ther. 2012, 13, 782–792. [Google Scholar] [CrossRef] [PubMed]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Krause, D.S.; Deans, R.J.; Keating, A.; Prockop, D.J.; Horwitz, E.M. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Fan, J.; Varshney, R.R.; Ren, L.; Cai, D.; Wang, D.-A. Synovium-Derived Mesenchymal Stem Cells: A New Cell Source for Musculoskeletal Regeneration. Tissue Eng. Part B Rev. 2009, 15, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Vandenabeele, F.; De Bari, C.; Moreels, M.; Lambrichts, I.; Dell’Accio, F.; Lippens, P.L.; Luyten, F.P. Morphological and immunocytochemical characterization of cultured fibroblast-like cells derived from adult human synovial membrane. Arch. Histol. Cytol. 2003, 66, 145–153. [Google Scholar] [CrossRef]
- Choi, Y.-S.; Noh, S.-E.; Lim, S.-M.; Lee, C.-W.; Kim, C.-S.; Im, M.-W.; Lee, M.-H.; Kim, D.-I. Multipotency and growth characteristic of periosteum-derived progenitor cells for chondrogenic, osteogenic, and adipogenic differentiation. Biotechnol. Lett. 2007, 30, 593–601. [Google Scholar] [CrossRef]
- Nakahara, H. In vitro differentiation of bone and hypertrophic cartilage from periosteal-derived cells. Exp. Cell Res. 1991, 195, 492–503. [Google Scholar] [CrossRef]
- Vega, A.; Martín-Ferrero, M.A.; Del Canto, F.; Alberca, M.; García, V.; Munar, A.; Orozco, L.; Soler, R.; Fuertes, J.J.; Huguet, M.; et al. Treatment of Knee Osteoarthritis with Allogeneic Bone Marrow Mesenchymal Stem Cells. Transplantation 2015, 99, 1681–1690. [Google Scholar] [CrossRef]
- Charbord, P. Bone Marrow Mesenchymal Stem Cells: Historical Overview and Concepts. Hum. Gene Ther. 2010, 21, 1045–1056. [Google Scholar] [CrossRef] [PubMed]
- Pontikoglou, C.; Deschaseaux, F.; Sensebé, L.; Papadaki, H.A. Bone Marrow Mesenchymal Stem Cells: Biological Properties and Their Role in Hematopoiesis and Hematopoietic Stem Cell Transplantation. Stem Cell Rev. Rep. 2011, 7, 569–589. [Google Scholar] [CrossRef]
- Lin, H.; Sohn, J.; Shen, H.; Langhans, M.T.; Tuan, R.S. Bone marrow mesenchymal stem cells: Aging and tissue engineering applications to enhance bone healing. Biomaterials 2019, 203, 96–110. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Du, H.; Dai, C.; Zhang, L.; Li, S.; Hunter, D.J.; Lu, L.; Bao, C. Human adipose-derived mesenchymal stem cells for osteoarthritis: A pilot study with long-term follow-up and repeated injections. Regen. Med. 2018, 13, 295–307. [Google Scholar] [CrossRef]
- Freitag, J.; Wickham, J.; Shah, K.; Tenen, A. Effect of autologous adipose-derived mesenchymal stem cell therapy in the treatment of an osteochondral lesion of the ankle. BMJ Case Rep. 2020, 13, e234595. [Google Scholar] [CrossRef]
- Laffey, J.; Hayes, M.; Friedenstein, A.J.; Gorskaja, J.F.; Kulagina, N.N. Faculty of 1000 evaluation for Fibroblast precursors in normal and irradiated mouse hematopoietic organs. F1000—Post. Publ. Peer Rev. Biomed. Lit. 2011, 4, 267–274. [Google Scholar] [CrossRef]
- Prockop, D.J. Marrow stromal cells as stem cells for continual renewal of nonhematopoietic tissues and as potential vectors for gene therapy. J. Cell. Biochem. Suppl. 1998, 30–31, 284–285. [Google Scholar] [CrossRef]
- Harrell, C.R.; Markovic, B.S.; Fellabaum, C.; Arsenijevic, A.; Volarevic, V. Mesenchymal stem cell-based therapy of osteoarthritis: Current knowledge and future perspectives. Biomed. Pharmacother. 2019, 109, 2318–2326. [Google Scholar] [CrossRef]
- Si, Z.; Wang, X.; Sun, C.; Kang, Y.; Xu, J.; Wang, X.; Hui, Y. Adipose-derived stem cells: Sources, potency, and implications for regenerative therapies. Biomed. Pharmacother. 2019, 114, 108765. [Google Scholar] [CrossRef] [PubMed]
- Freitag, J.; Bates, D.; Wickham, J.; Shah, K.; Huguenin, L.; Tenen, A.; Paterson, K.; Boyd, R. Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: A randomized controlled trial. Regen. Med. 2019, 14, 213–230. [Google Scholar] [CrossRef] [PubMed]
- Freitag, J.; Shah, K.; Wickham, J.; Boyd, R.; Tenen, A. The effect of autologous adipose derived mesenchymal stem cell therapy in the treatment of a large osteochondral defect of the knee following unsuccessful surgical intervention of osteochondritis dissecans—A case study. BMC Musculoskelet. Disord. 2017, 18, 298. [Google Scholar] [CrossRef]
- Mazini, L.; Rochette, L.; Amine, M.; Malka, G. Regenerative Capacity of Adipose Derived Stem Cells (ADSCs), Comparison with Mesenchymal Stem Cells (MSCs). Int. J. Mol. Sci. 2019, 20, 2523. [Google Scholar] [CrossRef] [PubMed]
- El-Badawy, A.; Amer, M.; Abdelbaset, R.; Sherif, S.N.; Abo-Elela, M.; Ghallab, Y.H.; Elhamid, H.A.; Ismail, Y.; El-Badri, N. Adipose Stem Cells Display Higher Regenerative Capacities and More Adaptable Electro-Kinetic Properties Compared to Bone Marrow-Derived Mesenchymal Stromal Cells. Sci. Rep. 2016, 6, 37801. [Google Scholar] [CrossRef]
- Shi, Y.-Y.; Nacamuli, R.P.; Salim, A.; Longaker, M.T. The Osteogenic Potential of Adipose-Derived Mesenchymal Cells Is Maintained with Aging. Plast. Reconstr. Surg. 2005, 116, 1686–1696. [Google Scholar] [CrossRef] [PubMed]
- Beane, O.S.; Fonseca, V.C.; Cooper, L.L.; Koren, G.; Darling, E.M. Impact of Aging on the Regenerative Properties of Bone Marrow-, Muscle-, and Adipose-Derived Mesenchymal Stem/Stromal Cells. PLoS ONE 2014, 9, e115963. [Google Scholar] [CrossRef]
- Song, W.-J.; Li, Q.; Ryu, M.-O.; Ahn, J.-O.; Bhang, D.H.; Jung, Y.C.; Youn, H.-Y. TSG-6 Secreted by Human Adipose Tissue-derived Mesenchymal Stem Cells Ameliorates DSS-induced colitis by Inducing M2 Macrophage Polarization in Mice. Sci. Rep. 2017, 7, 5187. [Google Scholar] [CrossRef]
- Manferdini, C.; Maumus, M.; Gabusi, E.; Piacentini, A.; Filardo, G.; Peyrafitte, J.-A.; Jorgensen, C.; Bourin, P.; Fleury-Cappellesso, S.; Facchini, A.; et al. Adipose-Derived Mesenchymal Stem Cells Exert Antiinflammatory Effects on Chondrocytes and Synoviocytes From Osteoarthritis Patients Through Prostaglandin E2. Arthritis Rheum. 2013, 65, 1271–1281. [Google Scholar] [CrossRef]
- Ortiz-Virumbrales, M.; Menta, R.; Pérez, L.M.; Lucchesi, O.; Mancheño-Corvo, P.; Avivar-Valderas, Á.; Palacios, I.; Herrero-Mendez, A.; Dalemans, W.; De La Rosa, O.; et al. Human adipose mesenchymal stem cells modulate myeloid cells toward an anti-inflammatory and reparative phenotype: Role of IL-6 and PGE2. Stem Cell Res. Ther. 2020, 11, 462. [Google Scholar] [CrossRef]
- Bourin, P.; Bunnell, B.A.; Casteilla, L.; Dominici, M.; Katz, A.J.; March, K.L.; Redl, H.; Rubin, J.P.; Yoshimura, K.; Gimble, J.M. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: A joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International Society for Cellular Therapy (ISCT). Cytotherapy 2013, 15, 641–648. [Google Scholar] [CrossRef]
- Lin, K.; Matsubara, Y.; Masuda, Y.; Togashi, K.; Ohno, T.; Tamura, T.; Toyoshima, Y.; Sugimachi, K.; Toyoda, M.; Marc, H.; et al. Characterization of adipose tissue-derived cells isolated with the Celution™ system. Cytotherapy 2008, 10, 417–426. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Moher, D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Clement, N.D.; Bardgett, M.; Weir, D.; Holland, J.; Gerrand, C.; Deehan, D.J. What is the Minimum Clinically Important Difference for the WOMAC Index After TKA? Clin. Orthop. Relat. Res. 2018, 476, 2005–2014. [Google Scholar] [CrossRef] [PubMed]
- Jo, C.H.; Chai, J.W.; Jeong, E.C.; Oh, S.; Shin, J.S.; Shim, H.; Yoon, K.S. Intra-articular Injection of Mesenchymal Stem Cells for the Treatment of Osteoarthritis of the Knee: A 2-Year Follow-up Study. Am. J. Sports Med. 2017, 45, 2774–2783. [Google Scholar] [CrossRef]
- Jo, C.H.; Gil Lee, Y.; Shin, W.H.; Kim, H.; Chai, J.W.; Jeong, E.C.; Kim, J.E.; Shim, H.; Shin, J.S.; Shin, I.S.; et al. Intra-Articular Injection of Mesenchymal Stem Cells for the Treatment of Osteoarthritis of the Knee: A Proof-of-Concept Clinical Trial. Stem Cells 2014, 32, 1254–1266. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Kim, H.J.; Kim, K.; Kim, G.B.; Jin, W. Intra-Articular Injection of Autologous Adipose Tissue-Derived Mesenchymal Stem Cells for the Treatment of Knee Osteoarthritis: A Phase IIb, Randomized, Placebo-Controlled Clinical Trial. Stem Cells Transl. Med. 2019, 8, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Spasovski, D.; Spasovski, V.; Baščarević, Z.; Stojiljković, M.; Vreća, M.; Andjelković, M.; Pavlović, S. Intra-articular injection of autologous adipose-derived mesenchymal stem cells in the treatment of knee osteoarthritis. J. Gene Med. 2018, 20, e3002. [Google Scholar] [CrossRef]
- Koh, Y.-G.; Jo, S.-B.; Kwon, O.-R.; Suh, D.-S.; Lee, S.-W.; Park, S.-H.; Choi, Y.-J. Mesenchymal Stem Cell Injections Improve Symptoms of Knee Osteoarthritis. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 748–755. [Google Scholar] [CrossRef]
- Nguyen, P.D.; Tran, T.D.-X.; Nguyen, H.T.-N.; Vu, H.T.; Le, P.T.-B.; Phan, N.L.-C.; Vu, N.B.; Phan, N.K.; Van Pham, P. Comparative Clinical Observation of Arthroscopic Microfracture in the Presence and Absence of a Stromal Vascular Fraction Injection for Osteoarthritis. Stem Cells Transl. Med. 2016, 6, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Yokota, N.; Yamakawa, M.; Shirata, T.; Kimura, T.; Kaneshima, H. Clinical results following intra-articular injection of adipose-derived stromal vascular fraction cells in patients with osteoarthritis of the knee. Regen. Ther. 2017, 6, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Garza, J.R.; Campbell, R.E.; Tjoumakaris, F.P.; Freedman, K.B.; Miller, L.S.; Maria, D.S.; Tucker, B.S. Clinical Efficacy of Intra-articular Mesenchymal Stromal Cells for the Treatment of Knee Osteoarthritis: A Double-Blinded Prospective Randomized Controlled Clinical Trial. Am. J. Sports Med. 2020, 48, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Hong, Z.; Chen, J.; Zhang, S.; Zhao, C.; Bi, M.; Chen, X.; Bi, Q. Intra-articular injection of autologous adipose-derived stromal vascular fractions for knee osteoarthritis: A double-blind randomized self-controlled trial. Int. Orthop. 2018, 43, 1123–1134. [Google Scholar] [CrossRef] [PubMed]
- Hudetz, D.; Borić, I.; Rod, E.; Jeleč, Ž.; Kunovac, B.; Polašek, O.; Vrdoljak, T.; Plečko, M.; Skelin, A.; Polančec, D.; et al. Early results of intra-articular micro-fragmented lipoaspirate treatment in patients with late stages knee osteoarthritis: A prospective study. Croat. Med. J. 2019, 60, 227–236. [Google Scholar] [CrossRef]
- Pers, Y.-M.; Rackwitz, L.; Ferreira, R.; Pullig, O.; Delfour, C.; Barry, F.; Sensebe, L.; Casteilla, L.; Fleury, S.; Bourin, P.; et al. Adipose Mesenchymal Stromal Cell-Based Therapy for Severe Osteoarthritis of the Knee: A Phase I Dose-Escalation Trial. Stem Cells Transl. Med. 2016, 5, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Roato, I.; Belisario, D.C.; Compagno, M.; Lena, A.; Bistolfi, A.; Maccari, L.; Mussano, F.; Genova, T.; Godio, L.; Perale, G.; et al. Concentrated adipose tissue infusion for the treatment of knee osteoarthritis: Clinical and histological observations. Int. Orthop. 2019, 43, 15–23. [Google Scholar] [CrossRef]
- Panni, A.S.; Vasso, M.; Braile, A.; Toro, G.; De Cicco, A.; Viggiano, D.; Lepore, F. Preliminary results of autologous adipose-derived stem cells in early knee osteoarthritis: Identification of a subpopulation with greater response. Int. Orthop. 2019, 43, 7–13. [Google Scholar] [CrossRef]
- Nakamura, N.; Yokota, N.; Hattori, M.; Ohtsuru, T.; Otsuji, M.; Lyman, S.; Shimomura, K. Comparative Clinical Outcomes After Intra-articular Injection with Adipose-Derived Cultured Stem Cells or Noncultured Stromal Vascular Fraction for the Treatment of Knee Osteoarthritis: Response. Am. J. Sports Med. 2020, 48, NP19–NP20. [Google Scholar] [CrossRef]
- Freitag, J.; Bates, D.; Wickham, J.; Shah, K.; Huguenin, L.; Tenen, A.; Paterson, K.; Boyd, R. Evaulation of intra-articular adipose derived mesenchymal stem cell therapy in the treatment of symptomatic knee osteoarthritis—A randomised controlled trial. Cytotherapy 2019, 21, S69. [Google Scholar] [CrossRef]
- Bansal, H.; Comella, K.; Leon, J.; Verma, P.; Agrawal, D.; Koka, P.; Ichim, T. Retracted Article: Intra-articular injection in the knee of adipose derived stromal cells (stromal vascular fraction) and platelet rich plasma for osteoarthritis. J. Transl. Med. 2017, 15, 141. [Google Scholar] [CrossRef] [PubMed]
- Tran, T.D.X.; Wu, C.-M.; Dubey, N.K.; Deng, Y.-H.; Su, C.-W.; Pham, T.T.; Le, P.B.T.; Sestili, P.; Deng, W.-P. Time- and Kellgren–Lawrence Grade-Dependent Changes in Intra-Articularly Transplanted Stromal Vascular Fraction in Osteoarthritic Patients. Cells 2019, 8, 308. [Google Scholar] [CrossRef] [PubMed]
- Zamborsky, R.; Danisovic, L. Surgical Techniques for Knee Cartilage Repair: An Updated Large-Scale Systematic Review and Network Meta-analysis of Randomized Controlled Trials. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 845–858. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Mai, X.; Wang, J.; Feng, E.; Huang, Y. Unicompartmental Knee Arthroplasty vs High Tibial Osteotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J. Arthroplast. 2018, 33, 952–959. [Google Scholar] [CrossRef]
- Damia, E.; Chicharro, D.; Lopez, S.; Cuervo, B.; Rubio, M.; Sopena, J.J.; Vilar, J.M.; Carrillo, J.M. Adipose-Derived Mesenchymal Stem Cells: Are They a Good Therapeutic Strategy for Osteoarthritis? Int. J. Mol. Sci. 2018, 19, 1926. [Google Scholar] [CrossRef]
- Murphy, J.M.; Dixon, K.; Beck, S.; Fabian, D.; Feldman, A.; Barry, F. Reduced chondrogenic and adipogenic activity of mesenchymal stem cells from patients with advanced osteoarthritis. Arthritis Rheum. 2002, 46, 704–713. [Google Scholar] [CrossRef]
- Qu, H.; Sun, S. Efficacy of mesenchymal stromal cells for the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2021, 16, 11. [Google Scholar] [CrossRef]
- Wang, J.; Zhou, L.; Zhang, Y.; Huang, L.; Shi, Q. Mesenchymal stem cells—A promising strategy for treating knee osteoarthritis. Bone Jt. Res. 2020, 9, 719–728. [Google Scholar] [CrossRef]
- Mishra, A.; Tummala, P.; King, A.; Lee, B.; Kraus, M.; Tse, V.; Jacobs, C.R. Buffered Platelet-Rich Plasma Enhances Mesenchymal Stem Cell Proliferation and Chondrogenic Differentiation. Tissue Eng. Part C Methods 2009, 15, 431–435. [Google Scholar] [CrossRef]
- Krüger, J.P.; Hondke, S.; Endres, M.; Pruss, A.; Siclari, A.; Kaps, C. Human platelet-rich plasma stimulates migration and chondrogenic differentiation of human subchondral progenitor cells. J. Orthop. Res. 2011, 30, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Fossett, E.; Khan, W.S.; Pastides, P.; Adesida, A.B. The Effects of Ageing on Proliferation Potential, Differentiation Potential and Cell Surface Characterisation of Human Mesenchymal Stem Cells. Curr. Stem Cell Res. Ther. 2012, 7, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Marędziak, M.; Marycz, K.; Tomaszewski, K.A.; Kornicka, K.; Henry, B.M. The Influence of Aging on the Regenerative Potential of Human Adipose Derived Mesenchymal Stem Cells. Stem Cells Int. 2016, 2016, 2152435. [Google Scholar] [CrossRef] [PubMed]
- Urban, H.; Little, C.B. The role of fat and inflammation in the pathogenesis and management of osteoarthritis. Rheumatology 2018, 57, iv10–iv21. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Brownlee, S.A.; Jones, M.H. The role of arthroscopy in the management of knee osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2014, 28, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Grieshober, J.A.; Stanton, M.; Gambardella, R. Debridement of Articular Cartilage: The Natural Course. Sports Med. Arthrosc. Rev. 2016, 24, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Aronowitz, J.A.; Ellenhorn, J.D.I. Adipose Stromal Vascular Fraction Isolation. Plast. Reconstr. Surg. 2013, 132, 932e–939e. [Google Scholar] [CrossRef]
- Comella, K.; Parlo, M.; Daly, R.; Depasquale, V.; Edgerton, E.; Mallory, P.; Schmidt, R.; Drake, W.P. Safety Analysis of Autologous Stem Cell Therapy in a Variety of Degenerative Diseases and Injuries Using the Stromal Vascular Fraction. J. Clin. Med. Res. 2017, 9, 935–942. [Google Scholar] [CrossRef] [PubMed]


| Authors | Type of Study | Treatment vs. Control | No. of Patients in Control Group (Gender) | No. of Patients in Treatment Group (Gender) | Age, Mean | Location of Defect | Grade of OA (Grading Classification) |
|---|---|---|---|---|---|---|---|
| Lee et al. (2019) [64] | Prospective double blinded RCT | AMSC at 1 dose, control | 12 (3M, 9F) | 12 (3M, 9F) | 62.7 | Knee | II–IV (K-L) |
| Freitag et al. (2019) [76] | Prospective non blinded RCT | AMSC at 2 doses, control | 10 (5M, 5F) | 10 (7M, 3F) for 1 injection. 10 (4M, 6F) for 2 injections | 53.6 | Knee | II–III (K-L) |
| Song et al. (2018) [48] | Prospective double blinded RCT | AMSC at 3 doses, no control | N/A | 18 (4M, 14F) | 54.8 | Knee | II–III (K-L) |
| Roato et al. (2019) [73] | Prospective single arm study | AMSC at 1 dose, no control | N/A | 20 (9M, 11F) | 59.6 | Knee | I–III (K-L) |
| Hudetz et al. (2019) [63] | Prospective non-randomised trial | AMSC injection, no control | N/A | 20 (15M, 5F) | Not specified | Knee | III–IV (K-L) |
| Spasovski et al. (2018) [65] | Prospective single arm study | AMSC at 1 dose, no control | N/A | 9 (3M, 6F) | 63 | Knee | B-D (IKDC) |
| Jo et al. (2017) [62] | Prospective cohort study | AMSC at 3 doses, no control | N/A | 18 (3M, 15F) | 61.8 | Knee | III–IV (K-L) |
| Bansal et al. (2017) [77] | Prospective interventional | AMSC injection, no control | N/A | 10 (6M, 4F) | 58.4 | Knee | I–II (BS) |
| Pers et al. (2016) [72] | Prospective single arm study | AMSC at 3 doses, no control | N/A | 18 (8M, 10F) | 64.6 | Knee | III–IV (K-L) |
| Jo et al. (2014) [63] | Prospective cohort study | AMSC at 3 doses, no control | N/A | 18 (3M, 15F) | 61.8 | Knee | III–IV (K-L) |
| Yokota et al. (2019) [75] | Retrospective cohort study | AMSC vs SVF, no control | N/A | 80 (16M, 64F) | 71.4 | Knee | II–IV (K-L) |
| Authors | Type of Study | Treatment vs. Control | No. of Patients in Control Group (Gender) | No. of Patients in Treatment Group (Gender) | Age, Mean | Location of Defect | Grade of OA (Grading Classification) |
|---|---|---|---|---|---|---|---|
| Garza et al. (2020) [69] | Prospective double blinded RCT | High dose SVF vs low dose SVF vs placebo | 13 (6M, 7F) | 13 (4M, 9F) for low dose SVF. 13 (7M, 6F) for high dose SVF. | 59.0 | Knee | II–III (K-L) |
| Hong et al. (2019) [70] | Prospective RCT | One knee with SVF and the other with hyaluronic acid placebo | 16 (3M, 13F) | 16 (3M, 13F) | Not specified | Knee | II-III (K-L) |
| Tran et al. (2019) [78] | Prospective non-randomised trial | Arthroscopic microfracture vs arthroscopic microfracture and injection of SVF | 15 (3M, 12F) | 18 (5M, 13F) | 58.64 | Knee | II–III (K-L) |
| Yokota et al. (2017) [68] | Prospective uncontrolled | Injection of SVF, no control | N/A | 13 (2M, 11F) | 74.5 | Knee | III–IV (K-L) |
| Nguyen et al. (2016) [67] | Prospective unblinded, non-randomised trial | Arthroscopic fracture vs arthroscopic fracture and injection of SVF and PRP. | 15 (3M, 12F) | 15 (3M, 12F) | 58.4 | Knee | II–III (K-L) |
| Koh et al. (2013) [66] | Prospective cohort study | SVF at 1 dose with PRP, no control | N/A | 18 (6M, 12F) | 54.6 | Knee | III–IV (K-L) |
| Panni et al. (2019) [74] | Retrospective single arm study | SVF at 1 dose following arthroscopy (for chondral shaving/abrasion and/or meniscal regularization), no control | N/A | 52 (22M, 30F) | 57.3 | Knee | 0–II (K-L) |
| Authors | Number of Cells Used/Multiple Injections | Method of Delivery of Cells | MSC Pre-Treatment | Follow-Up Period (Weeks) | Harvest Site | Method of Harvest | MSC Surface Marker Validation Via Flow Cytometry |
|---|---|---|---|---|---|---|---|
| Lee et al. (2019) [64] | 1 × 108 cells | Intra articular injection under USS guidance into unspecified joint space | Adipose tissues were treated with collagenase I and were centrifuged to obtain a pellet which was resuspended in culture media. The cells were cultured for up to 5 days in media until confluent and were then harvested at passage 3 | 26 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90. AMSCs were negative for CD31, CD34, CD45 |
| Freitag et al. (2019) [49] | 100 × 106 cells, single and double injection | Intra articular injection under USS guidance into unspecified location in joint space | Lipoaspirate was digestion followed by centrifugation. MSCs were cultured under hypoxic conditions with standard growth media until 80% confluency and was expanded to passage 2. | 52 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90, CD105, AMSCs were negative for CD14, CD19, CD34, CD45 |
| Song et al. (2018) [48] | 1 × 107, 2 × 107 and 5 × 107 cells, three injections | Intra articular injection under USS guidance into unspecified location in joint space | Lipoaspirated suspensions were digested and centrifuged, then cells were culture-expanded to passage 4. | 96 | Not specified | Liposuction | AMSCs were positive for CD29, CD49d, CD70, CD90 and were negative for actin, CD13, CD34, CD45, HLA-DR |
| Roato et al. (2019) [73] | Not specified | Intra articular injection under arthroscopic guidance into chondral defect site | Lipoaspirate was treated with Collagenase. The resulting cell pellet was then resuspended into culture media and counted. | 78 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90, CD105, IgG1, IgG2a AMSCs were negative for CD44, CD45 |
| Hudetz et al. (2019) [71] | Unspecified | Intra articular injection into unspecified location in joint space | Samples were digested with collagenase and samples were filtered through a 100 μm cell strainer and centrifuged. The cell pellet was resuspended in DMEM. | 48 | Abdomen | Liposuction | AMSCs were positive for CD70, CD90, CD105, CD146. AMSCs were negative for CD31, CD34, CD45. |
| Spasovski et al. (2018) [65] | 0.5–1 × 107 cells | Intra articular injection into unspecified location in joint space | MSCs were digested using collagenase, expanded in standard culture media and harvested between passage 2 and 4. | 78 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90, CD105. AMSCs were negative for CD34, CD45 |
| Jo et al. (2017) [62] | 1 × 107, 5 × 107 and 1 × 108 cells | Intra articular injection under arthroscopic guidance into unspecified location in joint space | Aspirated tissues were digested with collagenase I. Cells were cultured for 4-5 days until confluent. All AMSCs used in this study were collected at passage 3. | 104 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90. AMSCs were negative for CD14, CD34, CD45 |
| Bansal et al. (2017) [77] | 1 × 106 cells | Intra articular injection into unspecified location in joint space | The adipose tissues was filtered and centrifuged. The cell pellet was re-suspended in culture medium and the media was changed every 3-4 days until the cells achieved 90% confluency. | 96 | Abdomen | Liposuction | AMSCs were positive for CD70, CD90, CD105. AMSCs were negative for CD34, CD45, HLA-DR |
| Pers et al. (2016) [72] | 2 × 106, 10 × 106 and 50 × 106 cells | Intra articular injection under USS guidance into unspecified location in joint space | Adipose tissue was digested with collagenase solution and plated in culture medium. Cells were passaged and then cultured in CCM for 14 days with media changes every 3–4 days until confluence. | 26 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90, CD105, IgG1 AMSCs were negative for CD31, CD34, CD45 |
| Jo et al. (2014) [63] | 1 × 107, 5 × 107 and 1 × 108 cells | Intra articular injection under arthroscopic guidance into unspecified location in joint space | Aspirated tissues were digested with collagenase and cells were resuspended in media until confluent. AMSCs used were collected at passage 3. | 26 | Abdomen | Liposuction | AMSCs were positive for CD73, CD90. AMSCs were negative for CD31, CD34, CD45 |
| Nakamura et al. (2019) [75] | 12.75 × 106 cells, unknown for SVF | Intra articular injection into unspecified location in joint space | The collected aspirate was digested with collagenase. Cells were cultured in medium that was replaced every 3 days thereafter. When cells reached 80% confluency they were passaged up to four times. SVF cells were produced without culture in a sterile single-use functionally-closed system, requiring approximately 2–2.5 h from lipoaspirate. | 26 | Abdomen | Liposuction | Not specified |
| Authors | Number of Cells Used/Multiple Injections | Method of Delivery of Cells | SVF Pre-Treatment | Follow-Up Period (Weeks) | Harvest Site | Method of Harvest | MSC Surface Marker Validation Via Flow Cytometry |
|---|---|---|---|---|---|---|---|
| Garza et al. (2020) [69] | 3.0 × 107, 1.5 × 107, 0 cells | Intra articular injection under USS guidance into unspecified joint space | SVF from dissociated tissue was centrifuged and the SVF cell pellet was extracted, resuspended for injection. | 48 | Abdomen | Liposuction | Not specified |
| Hong et al. (2019) [70] | 7.45 × 106 cells | Intra articular injection under arthroscopic guidance into unspecified location in joint space | The SVF from the lipoaspirate was isolated by means of collagenase digestion. The SVF was then washed twice with PBS to remove collagenase. | 48 | Abdomen | Liposuction | Not specified |
| Tran et al. (2019) [78] | 9–12 × 107 cells | Intra articular injection under arthroscopic guidance into chondral defect site | The SVF from the lipoaspirate was isolated through collagenase treatment. The SVF was then diluted with normal saline 0.9% to obtain 6 mL of solution containing 90–120 million cells to administer via injection. | 96 | Abdomen | Liposuction | Not specified |
| Yokota et al. (2017) [68] | Unknown, however estimated to be 3 × 107 cells | Intra articular injection into unspecified location in joint space | Autologous SVF cells were collected in a sterile single-use functionally-closed system, requiring approximately 2–2.5 h. | 4 | Abdomen | Liposuction | Not specified |
| Nguyen et al. (2016) [67] | 1 × 107 cells | Intra articular injection under arthroscopic guidance into chondral defect site | The adipose tissue was digested using collagenase and centrifuged, the pellet was suspended in PBS for cell counting before injection. | 72 | Abdomen | Liposuction | Not specified |
| Koh et al. (2013) [66] | 1.18 × 106 cells | Intra articular injection into unspecified location in joint space | SVF was derived from fat pad tissue and mixed with 3.0 mL of platelet-rich plasma for injection. | 97.2 | Infrapatellar fat pad | Surgical excision of infrapatellar fat pad | Not specified |
| Panni et al. (2019) [74] | Not specified | Intra articular injection under arthroscopic guidance into unspecified location in joint space | The harvested fat was processed with the Lipogems® ortho kit. The final product was transferred directly to syringes for injection. | 61.2 | Abdomen | Liposuction | Not specified |
| Authors | Outcome Measures | Pre-Treatment WOMAC Scores | Post Treatment WOMAC Scores | Conclusions Based on Outcomes | Adverse Events | Nature of Complications |
|---|---|---|---|---|---|---|
| Lee et al. (2019) [64] | WOMAC, VAS, KOOS, ROM, K-L, Joint space width of medial and lateral compartment and HKA angle | Baseline WOMAC score was 60.0 (±17.0 SD) | At 6 months post procedure WOMAC scores were 26.7 (±13.3 SD) | Single injection of AD-MSCs led to a 55% reduction in the WOMAC total score, 59% in the pain score, 54% in the stiffness score, and 54% in the physical function score at 6 months. Significant improvements in the VAS, KOOS, ROM scores were also seen. K-L grade, joint space width of medial and lateral compartment, and HKA angle did not change significantly over 6 months in either groups. No evidence of significant cartilage regeneration in MRI at 6 months after the injection. | 8AEs | 6 cases of arthralgia and 2 cases of joint swelling after the procedure. |
| Freitag et al. (2019) [49] | NPRS-11, WOMAC, KOOS, MOAKS | WOMAC scores were 59.6 (±17.9 SD) for the one injection group and 54.4 (±18.2 SD) for the two-injection group | WOMAC scores were 84 (±9.4 SD) for the one injection group and 87.3 (±8 SD) for the two-injection group at 12 months. | NPRS-11 scores were greater when compared with baseline (< 0.05) throughout all time points in all treatment groups. There was no difference however between treatment groups. KOOS and WOMAC improved in all subscales during follow-up to 12 months. Two-thirds of the control group showed cartilage loss. 30% of the one-injection group had further cartilage loss, 50% had progression of osteophyte formation at 12 months. 89% in the two-injection group had either no progression or improvement in cartilage loss. | 7 AEs and 1 SAE in the one injection group. 8AEs and 1 SAE in the first injection of the two-injection group. 10 AEs in the second injection in the two-injection group. | Mild AEs: minor discomfort, bruising and/or swelling after the injection. SAEs were classified as pain and sweeling for 4 weeks after injection which impacted the daily activities of life for the patient. |
| Song et al. (2018) [48] | WOMAC, NPRS-11, SF-36, | WOMAC scores were 34.75 (±17.05 SD) at baseline | WOMAC scores were 25.94 (±16.09 SD), 20.38 (±19.89 SD), 22.77 (±22.72 SD), 15.00 (±11.36 SD) and 12.44 (±8.99 SD) in the 12th, 24th, 48th, 72nd and 96th week. | WOMAC scores improved with time leading up to follow-up in all groups. Significant improvements in the NPRS-11 scores in the low- and high-dose groups were first observed at three months following treatment. A statistically significant reduction in SF-36 scores were only found in the 12th and 96th week of follow-up The volume of knee cartilage increased over the course of follow-up. This was more apparent in the high-dose group | 8 AEs in the low dose group (66.67%). 7 AEs in the middle dose group (58.33%). 6 AEs in the high dose group (50%). | No SAEs or deaths. All complications were AEs. These were most commonly transient pain and swelling of joints, which were mild to moderate and were spontaneously relieved within 7 days without special treatment. One patient experienced mild oedema and cramps of bilateral lower extremities, which were relieved in 21 days without treatment and not related to the MSC treatment. |
| Roato et al. (2019) [73] | WOMAC, VAS, K-L | WOMAC score was 45.91 (±2.8) pre procedure. (NO SE OR SD GIVEN) | WOMAC scores were 27.47 (±3.02), 15.84 (±2.5) and 12.97 (±2.3) at 3 months, 6 months and 18 months post procedure. (NO SE OR SD GIVEN) | Significant improvement of VAS and WOMAC scores, with a significant pain reduction and increased mobility at 3, 6, and 12 months follow-up. No increase in the thickness of cartilage at 18 months. | 1 SAE | Swelling persisted two months after surgery |
| Hudetz et al. (2019) [71] | KOOS, WOMAC, VAS | WOMAC baseline score was 55.38 (±18.8 SD) | WOMAC scores after 12 months was 32.25 (±14.6 SD) | All scores significantly improved after treatment. | 0 AEs or SAEs | N/A |
| Spasovski et al. (2018) [65] | KSS, HSS, Lysholm score, VAS, MOCART | N/A | N/A | All outcomes significantly improved at 3 and 6 months. However, there was no further improvement beyond 12 or 18 months after treatment. | N/A | N/A |
| Jo et al. (2017) [62] | WOMAC, VAS, KSS, KOOS, K-L, Joint space width of the medial compartment, mechanical axis with weight bearing line, and anatomical axis | WOMAC scores were 43.3 (±12.7 SE) for the low dose group, 69.0 (±5.9 SE) for the mid dose group and 54.2 (±5.2 SE) for the high dose group. | WOMAC scores were 25.3 (±19.5 SE), 14.7 ± (12.7 SE) and 17.0 (±9.8 SE) at 6 months, 1 year and 2 years respectively for the low dose group. WOMAC scores were 48.5 (±9.5 SE), 13.1 (±10.0 SE) and 25.1 (±11.0 SE) at 6 months, 1 year and 2 years respectively for the middle dose group. WOMAC scores were 32.8 (±6.3 SE), 16.0 (±4.4 SE) and 19.0 (±5.5 SE) at 6 months, 1 year and 2 years respectively for the high dose group. | The WOMAC, VAS and KSS scores improved in the high-dose group at 6 months and 1 year. Non-significant trends in the low and middle dose groups. Significant improvement in KSS scores in the low dose groups up to one year. The sports subscore of the KOOS improved until 2 years for the high-dose group. No statistically significant improvements were found in the quality-of-life subscore of the KOOS for any of the dose groups. | None | None |
| Bansal et al. (2017) [77] | WOMAC, 6MWD, cartilage thickness | WOMAC score was 64 at baseline (NO SE OR SD GIVEN) | WOMAC scores were 52, 46, 42, 38 and 41 at 3 months, 6 months, 12 months, 18 months and 24 months respectively. (NO SE OR SD GIVEN) | Significant changes in the WOMAC and 6MWD scores were noted in both the subsets and the total after 2 years as compared to the baseline. MRI evaluation demonstrated that cartilage thickness improved. | 1 AE | Pain and swelling which resolved. |
| Pers et al. (2016) [72] | WOMAC, VAS, PGA, SAS, KOOS, OARSI, SF-36 | WOMAC scores were 63.2 (±4.1 SD) for the low dose group, 65.5 (±8.1 SD) for the mid dose group and 65.2 (±2.3 SD) for the high dose group. | WOMAC scores were 24.6 (±8.6 SD), 22.0 (±8.5 SD) and 30.1 (±8.9 SD) at 1 week, 3 months and 6 months respectively for the low dose group. WOMAC scores were 45.8 (±9.1 SD), 52.8 (±9.6 SD) and 42.6 (±9.1 SD) at 1 week, 3 months and 6 months respectively for the middle dose group. WOMAC scores were 61.1 (±15.3 SD), 38.4 (±16.0 SD) and 42.6 (±16.0 SD) at 1 week, 3 months and 6 months respectively for the high dose group. | Statistically significant improvements in WOMAC, VAS, KOOS and SAS scores were only found in the low dose group at 1 week, 3 months and 6 months. No improvements in the SF-36 in any groups. | 1 SAE and 5 AEs. | The SAE was unstable angina pectoris without increased cardiac markers, which was reported in 1 patient 3 months after ASC injection. The patient’s risk factors included hypertension and hyperlipidemia. Five AEs reported by four patients. There was slight knee pain/joint effusion occurred during the first week after ASC injection that resolved with nonsteroidal anti-inflammatory drugs in three patients and spontaneously in one patient. |
| Jo et al. (2014) [63] | WOMAC, VAS, KSS, K-L, Joint space width of the medial compartment, mechanical axis with weight bearing line, and anatomical axis, ICRS | WOMAC scores were 43.3 (±12.7 SE) for the low dose group, 69.0 (±5.9 SE) for the mid dose group and 54.2 (±5.2 SE) for the high dose group. | WOMAC scores were 44.0 (±4.4 SE), 30.0 (±12.0 SE), 38.7 (±24.7 SE) and 25.3 (±19.5 SE) at 1, 2, 3 and 6 months respectively for the low dose group. WOMAC scores were 72.3 (±4.3 SE), 51.3 (±6.5 SE), 51.3 (±6.7 SE) and 48.5 (±11.0 SE) at 1, 2, 3 and 6 months respectively for the mid dose group. WOMAC scores were 45.5 (±4.5 SE), 40.1 (±6.0 SE), 37.0 (±6.8 SE) and 32.8 (±6.3 SE) at 1, 2, 3 and 6 months respectively for the high dose group. | Significant improvement of the WOMAC and VAS at 6 months compared with baseline in the high-dose groups. This was not seen in the other treatment groups. Knee subsection of KSS significantly increased in the low-dose and the high-dose groups, but improvements in the function subsection of seen in the low-dose group only. Other parameters did not change significantly at 6 months in any groups. The ICRS grade of the cartilage defect significantly improved in the medial femoral and tibial condyle in the high-dose group at second-look arthroscopy. No significant change was found in the lateral parts of the joint. | 1 AE and 1 SAE in the low dose group (66.6%). 2 AEs in the mid dose group (66.6%). 5 AEs in the high dose group (41.66%). | In the low dose group, the AE was an individual case of nasopharyngitis, and the SAE was a urinary calculus. In the mid dose group AEs were individual cases of nasopharyngitis, arthralgia and chest pain. In the high dose group AEs were individual cases of nasopharyngitis, arthralgia, back pain, cough and hypertriglyceridemia. |
| Yokota et al. (2019) [75] | KOOS, VAS, OARSI, K-L | N/A | N/A | Change in KOOS symptoms occurred earlier in the AMSC group than the SVF group, with significant improvement detected at 3 months follow-up. The extent of VAS improvement after injection was greatest in patients with mildest. Patients in the AMSC group had a greater improvement in VAS than patients in the SVF group, regardless of the extent of OA at baseline. The proportion of patients who responded to treatment as determined by the OMERACT-OARSI responder criteria was greater in the AMSC group than the SVF. | 3AEs in the ASC group and 26 AEs in the SVF group. | In the ASC group, there was 1 case of joint swelling after the injection and 2 cases of abdominal induration after harvest. These were all self-limiting. In the SVF group, there were 3 cases of joint swelling after the injection. There were 6 cases of abdominal pain, 5 cases of abdominal swelling and 12 cases of abdominal induration after harvest. These were all self-limiting. |
| Garza et al. (2020) [69] | WOMAC, OS | Baseline WOMAC scores were 49.3 for the placebo group, 56.2 for the low dose group and 47.1 for the high dose group (THIS WAS THE MEAN. NO SE OR SD WAS GIVEN) Median was 49.8 (37.4–57.0), 51.6 (46.3–62.3) and 49.8 (35.6–55.2) for the placebo, low dose and high dose groups. | WOMAC scores for the placebo was 26.0, 22.9, 37.2 and 41.9 at 6 weeks, 3 months, 6 months and 1 year respectively. Median values were 23.0(14.2–37.4), 20.0 (16.0–32.0), 30.2 (21.4–55.2), 41.0 (19.5–55.2). WOMAC scores for the low dose group was 24.8, 19.7, 23.7 and 21.8 at 6 weeks, 3 months, 6 months and 1 year respectively. Median values were 20.0 (10.7–37.4), 14.0 (5.3–35.6), 26.7 (8.9–32.0), 12.5 (7.1–35.6) WOMAC scores for the high dose group was 25.7, 26.5, 20.0 and 13.2 at 6 weeks, 3 months, 6 months and 1 year respectively. Median values were 27.0 (14.2–36.0), 27.0 (10.7–34.7), 8.9 (3.6–32.0), 3.6 (0.0–26.7) | All groups displayed a reduction in total WOMAC score from baseline at 6 month follow-up. All treated groups continued to demonstrate lower total WOMAC scores 1 year after injection as compared with baseline scores and sixth month scores. There was no change in cartilage thickness detected at six month follow-up. | 0 AEs or SAEs | N/A |
| Hong et al. (2019) [70] | VAS, WOMAC, ROM, WORMS, MOCART | Baseline WOMAC pain score was 9.50 (±3.92 SD) for the control group and was 9.44 (±3.90 SD) for the treatment group. Baseline WOMAC stiffness score was 3.00 (±1.55 SD) for the control group and was 3.31 (±1.82 SD) for the treatment group. | WOMAC pain scores were 8.94 (±4.98 SD), 11.56 (±6.84 SD), 12.88 (±5.73 SD) and 15.19 (±4.29 SD) at 1 month, 3 months, 6 months and 12 months respectively for the control group. WOMAC stiffness scores were 4.38 (±2.22 SD), 4.94 (±2.49 SD), 5.44 (±2.56 SD) and 5.69 (±2.57 SD) at 1 month, 3 months, 6 months and 12 months respectively for the control group. WOMAC pain scores were 6.25 (±3.02 SD), 2.13 (±3.52 SD), 1.5 (±3.84 SD) and 1.44 (±4.77 SD) at 1 month, 3 months, 6 months and 12 months respectively for the treatment group. WOMAC stiffness scores were 1.75 (±1.59 SD), 1.12 (±1.80 SD), 0.81 (±1.59 SD) and 1.06 (±2.11 SD) at 1 month, 3 months, 6 months and 12 months respectively for the treatment group. | In the treated group, all scores including VAS, WOMAC pain, WOMAC stiffness, and knee ROM was founded to be significantly improved at one, three, six, and 12-months follow-up as compared with baseline scores within the treated groups and against control groups. Both WORMS and MOCART MRI scores showed a statistically significant improvement in the treatment group, while a deterioration in the control group. | 10 AEs | 4 AEs relating to abdominal pain after harvest which resolved after 1 week. 6 cases of pain and swelling in both knees after surgery. These all resolved after 2 weeks with analgesia. |
| Tran et al. (2019) [78] | VAS, WOMAC, OS, BME, K-L | WOMAC scores were 52.0 (±18.26 SD) and 42.64 (±12.51 SD) at baseline for patients with KL OA grade 2 and 3 respectively. | For KL OA grade 2 patients, WOMAC scores were 24.25 (±19.77 SD) and 18.25 (±20.07 SD) at 12 and 24 months respectively. For KL OA grade 3 patients, WOMAC scores were 18.21 (±8.20 SD) and 9.00 (±8.46 SD) at 12 and 24 months respectively. | No significant difference was found between the VAS scores of the treatment and placebo groups at 12 months.A decreasing trend in the VAS and WOMAC scores of the treatment group was observed up to 24 months compared to controls. Between 12 and 24 months, the VAS scores increased in the placebo group. MRI results showed that after 24 months of treatment, bone marrow oedema was decreased in both the placebo and the SVF treatment groups, the latter demonstrated a greater effect. The Outbridge score also decreased in the SVF-treated group. | N/A | N/A |
| Yokota et al. (2017) [68] | JKOM, WOMAC, VAS | Baseline WOMAC scores were 49.6 (±20.4 SD) | WOMAC scores were 43.0 (±17.4 SD) and 36.5 (±21.9 SD) at 1 month and 6 months after treatment respectively | JKOM, WOMAC, and VAS scores were significantly improved compared to baseline one month following treatment. This effect was also observed at the six-month visit. JKOM scores improved by an average of 35% over baseline compared to a 32% improvement in WOMAC, and 40% for VAS. | 26 AEs | All patients experienced pain and swelling at the fat harvest and injection sites. These however resolved after a few days with analgesia. |
| Nguyen et al. (2016) [67] | WOMAC, Lysholm score, VAS, OS, BME, JMA, | WOMAC scores for the placebo group was 47.27 (±17.13 SD). WOMAC scores for the treatment group was 42.87 (±16.29 SD) | WOMAC scores for the placebo group was 23.27 (±15.61 SD) and 25.60 (±19.69 SD) at 6 and 12 months respectively. WOMAC scores for the treatment group were 19.27 (±14.87 SD) and 17.33 (±14.91 SD) at 6 and 12 months respectively. | WOMAC scores significantly decreased compared with baseline scores at 6 and 12 months.WOMAC scores between the treatment and placebo groups were not significantly different at 12 months, but a significant difference was seen at 18 months. VAS and Lysholm scores improved in the treatment group compared to pre treatment scores at all follow-up timepoints. | 0 AEs or SAEs | N/A |
| Koh et al. (2013) [66] | WOMAC, lysholm score, VAS, WORMS | Baseline WOMAC score was 49.9 (±12.6 SD) | After final follow-up post procedure WOMAC scores were 30.3 (±9.2 SD) | WOMAC scores decreased in the treatment group over the follow-up period. Greater changes in WOMAC score were seen in subjects injected with greater cell numbers. Lysholm and VAS scores also significantly improved over the follow-up period. Significant reduction was observed in the WORMS cartilage subscore. | 1 AE | Notable pain and swelling after injection for 2 weeks. This was self-limiting. |
| Panni et al. (2019) [74] | IKS, VAS, | N/A | N/A | 96.2% of treated subjects reported improvements in knee function and/or pain. A subset (62%) achieved complete or near-complete function recovery and/or pain relief. Two (3.9%) patients reported slight reduction of the pain. | 3AEs | Transient haematoma after harvest |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agarwal, N.; Mak, C.; Bojanic, C.; To, K.; Khan, W. Meta-Analysis of Adipose Tissue Derived Cell-Based Therapy for the Treatment of Knee Osteoarthritis. Cells 2021, 10, 1365. https://doi.org/10.3390/cells10061365
Agarwal N, Mak C, Bojanic C, To K, Khan W. Meta-Analysis of Adipose Tissue Derived Cell-Based Therapy for the Treatment of Knee Osteoarthritis. Cells. 2021; 10(6):1365. https://doi.org/10.3390/cells10061365
Chicago/Turabian StyleAgarwal, Nikhil, Christopher Mak, Christine Bojanic, Kendrick To, and Wasim Khan. 2021. "Meta-Analysis of Adipose Tissue Derived Cell-Based Therapy for the Treatment of Knee Osteoarthritis" Cells 10, no. 6: 1365. https://doi.org/10.3390/cells10061365
APA StyleAgarwal, N., Mak, C., Bojanic, C., To, K., & Khan, W. (2021). Meta-Analysis of Adipose Tissue Derived Cell-Based Therapy for the Treatment of Knee Osteoarthritis. Cells, 10(6), 1365. https://doi.org/10.3390/cells10061365







