Immunomodulatory Factors in Primary Endometrial Cell Cultures Isolated from Cancer and Noncancerous Human Tissue–Focus on RAGE and IDO1
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Characteristic
2.2. Immunohistochemistry
2.3. Isolation and Culture of Cells from Human Endometrium
2.4. Determination of Population Doubling Time (PDT)
2.5. Karyotyping
2.6. Immunofluorescent Staining
2.7. Western Blotting
2.8. Quantification of l-Kyn Generated by Endometrial Cells Cultured In Vitro
2.9. Statistical Analysis
3. Results
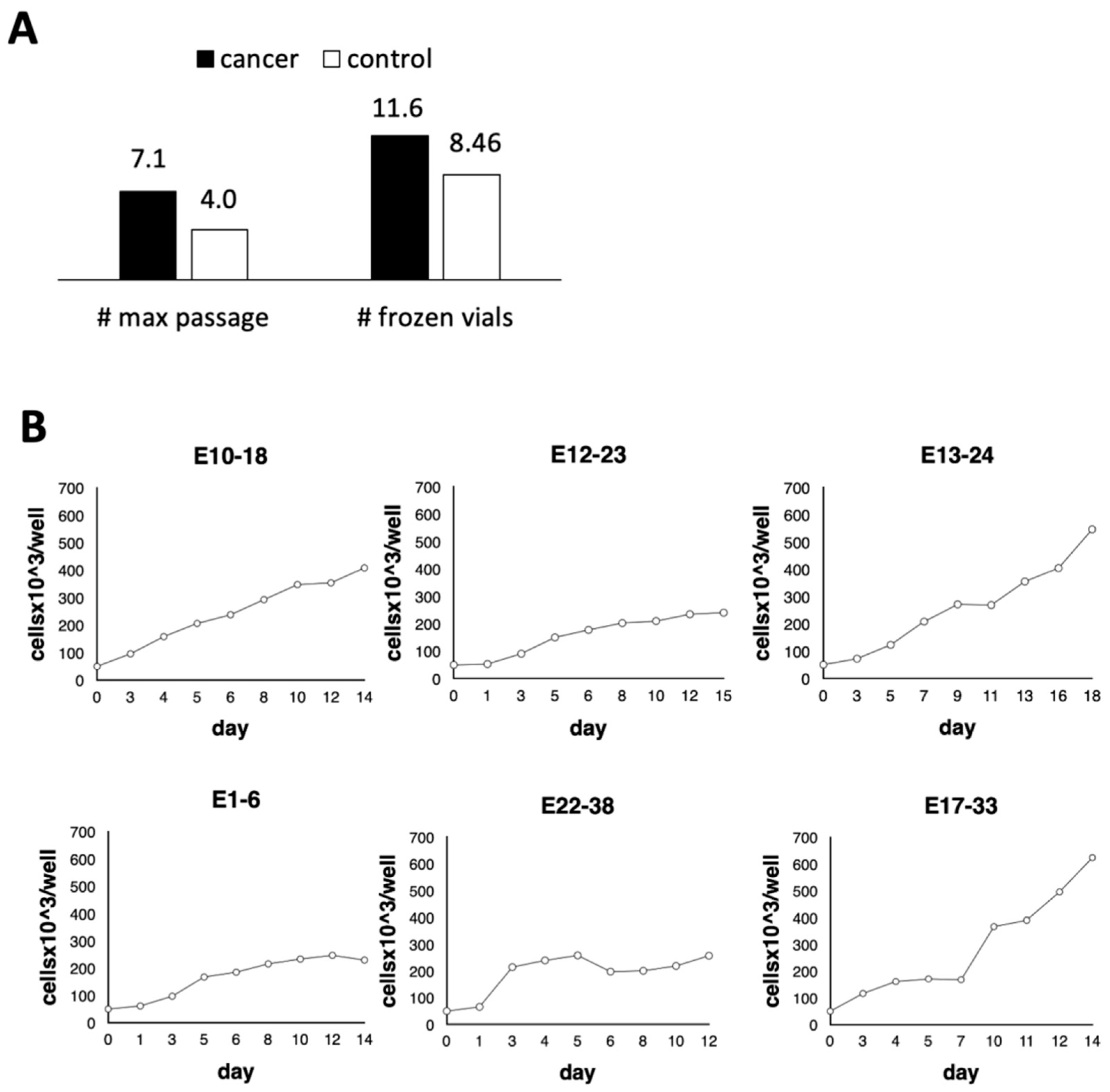
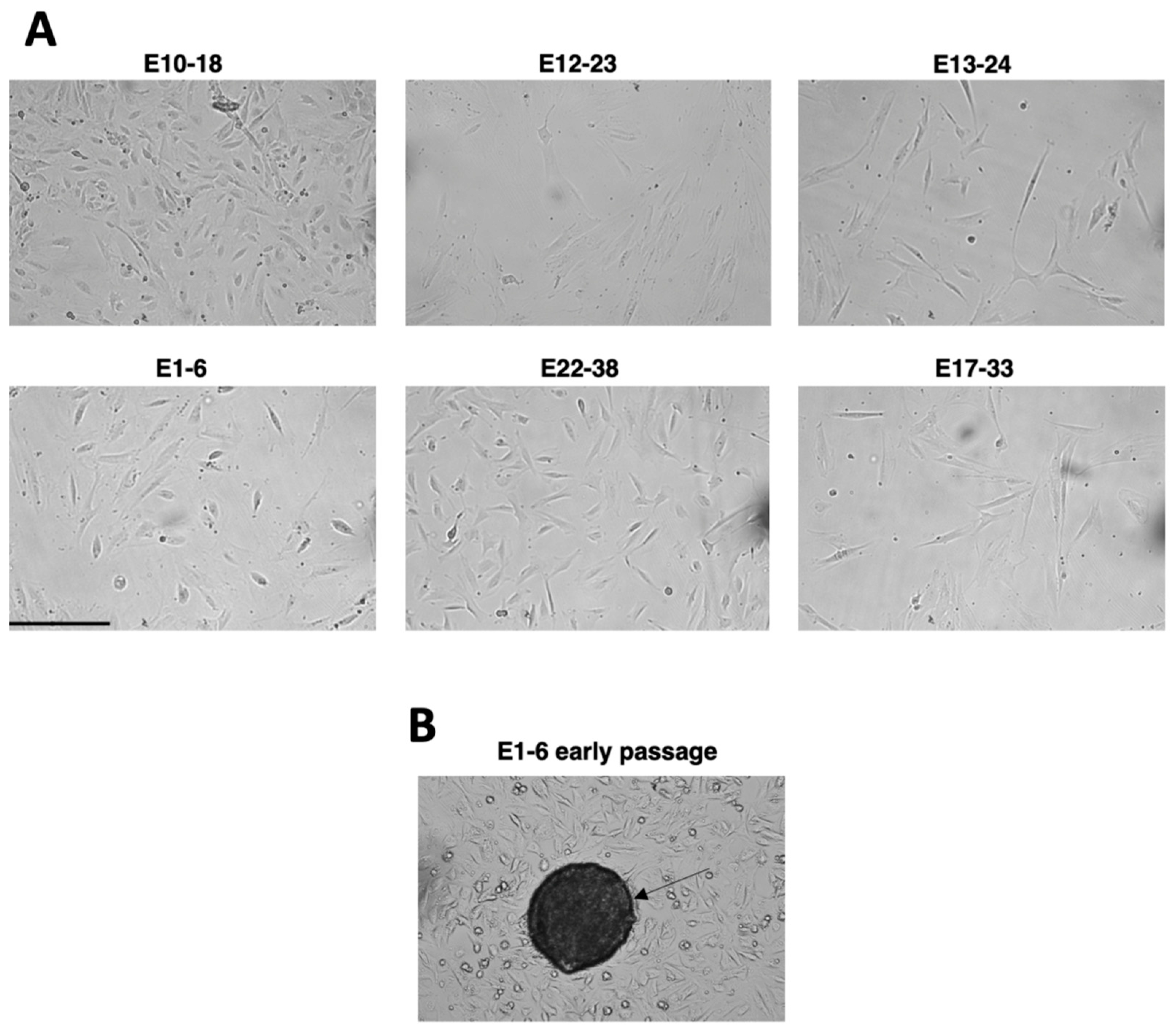
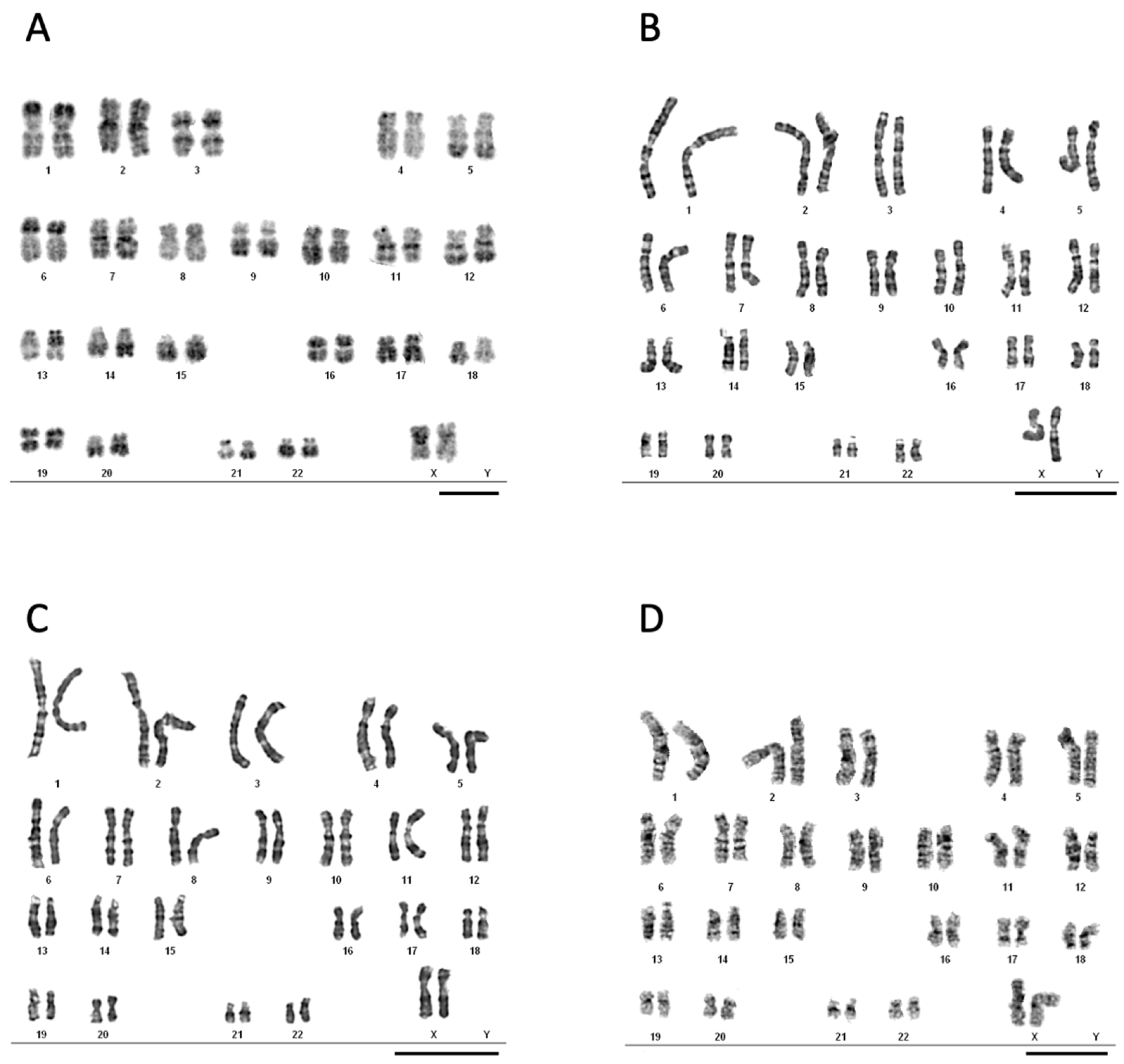
3.1. Development of the Experimental In Vitro Model
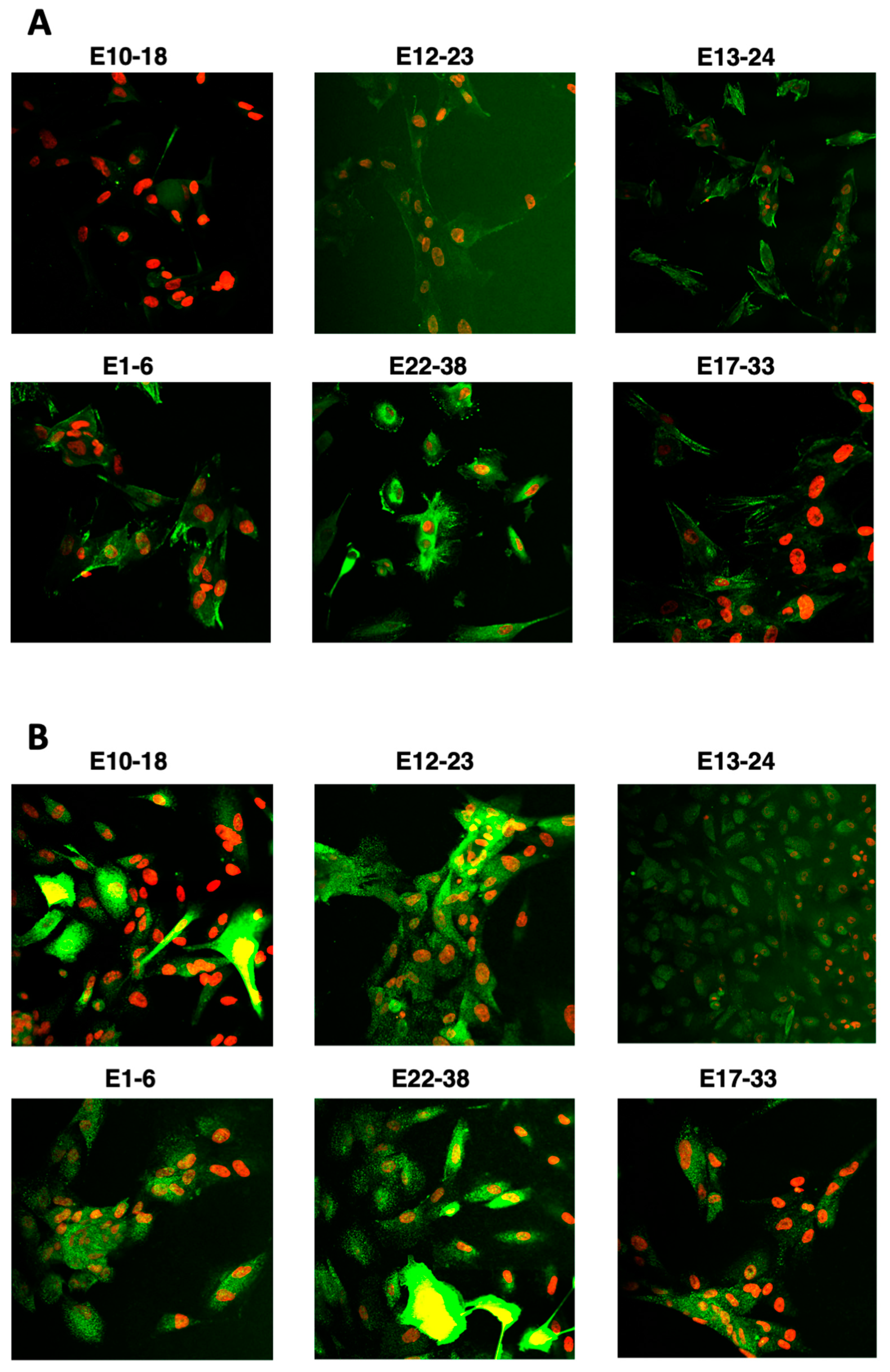
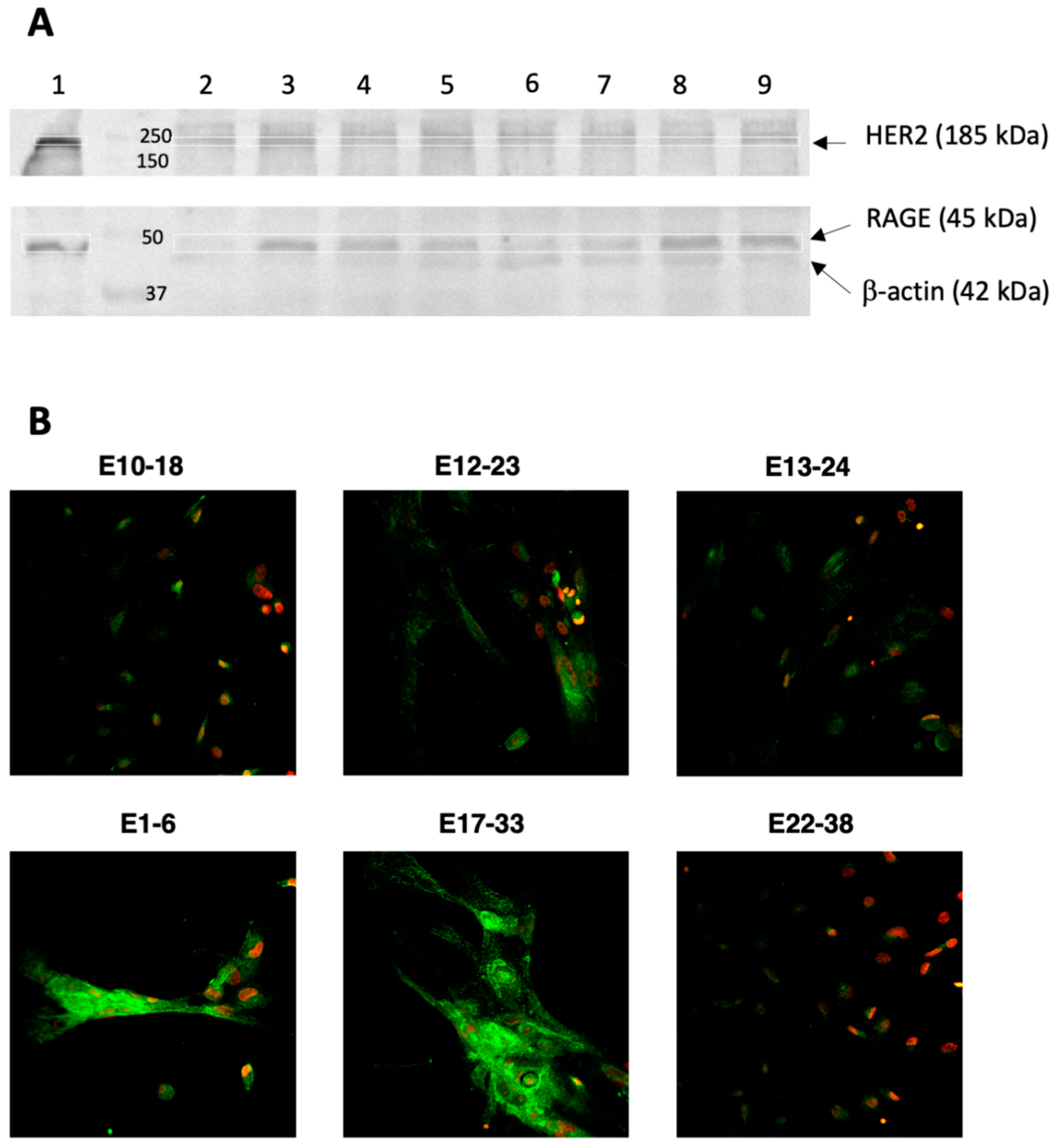
3.2. HER2 and RAGE Status of the Endometrial Cells Cultured In Vitro
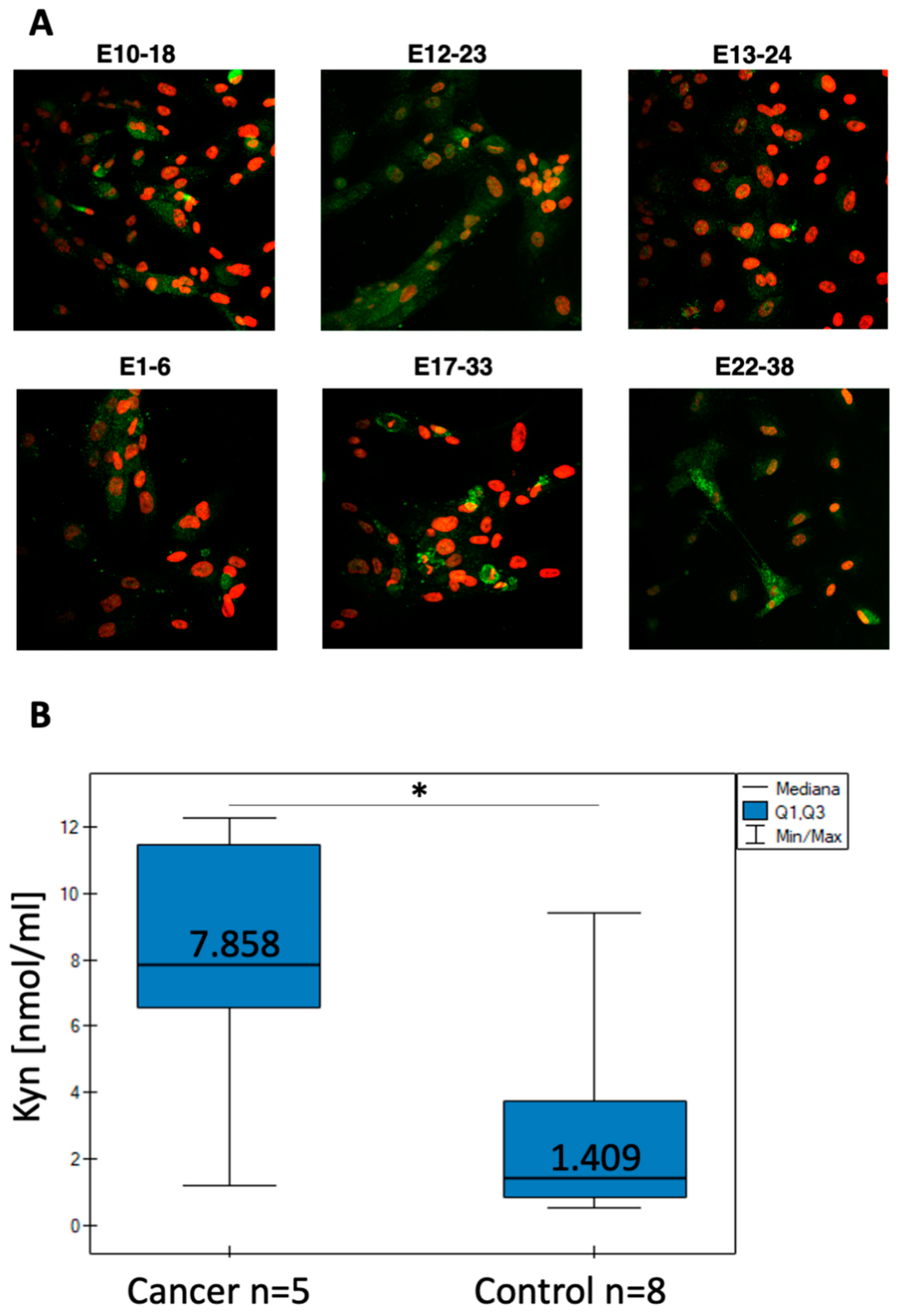
3.3. IDO1 Expression and l-Kynurenine Generation by the Primary Endometrial Cell Cultures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kofod, L.; Lindhard, A.; Hviid, T.V.F. Implications of uterine NK cells and regulatory T cells in the endometrium of infertile women. Hum. Immunol. 2018, 79, 693–701. [Google Scholar] [CrossRef]
- Okada, H.; Tsuzuki, T.; Murata, H. Decidualization of the human endometrium. Reprod. Med. Biol. 2018, 17, 220–227. [Google Scholar] [CrossRef]
- Wu, S.-P.; Li, R.; DeMayo, F.J. Progesterone Receptor Regulation of Uterine Adaptation for Pregnancy. Trends Endocrinol. Metab. 2018, 29, 481–491. [Google Scholar] [CrossRef]
- Ligam, P.; Manuelpillai, U.; Wallace, E.; Walker, D. Localisation of Indoleamine 2,3-dioxygenase and Kynurenine Hydroxylase in the Human Placenta and Decidua: Implications for Role of the Kynurenine Pathway in Pregnancy. Placenta 2005, 26, 498–504. [Google Scholar] [CrossRef]
- Baker, J.M.; Chase, D.M.; Herbst-Kralovetz, M.M. Uterine Microbiota: Residents, Tourists, or Invaders? Front. Immunol. 2018, 9, 208. [Google Scholar] [CrossRef]
- Koscinski, I.; Viville, S.; Porchet, N.; Bernigaud, A.; Escande, F.; Defossez, A.; Buisine, M.P. MUC4 gene polymorphism and expression in women with implantation failure. Hum. Reprod. 2006, 21, 2238–2245. [Google Scholar] [CrossRef][Green Version]
- Margarit, L.; Taylor, A.; Roberts, M.H.; Hopkins, L.; Davies, C.; Brenton, A.G.; Conlan, S.; Bunkheila, A.; Joels, L.; White, J.O.; et al. MUC1 as a Discriminator between Endometrium from Fertile and Infertile Patients with PCOS and Endometriosis. J. Clin. Endocrinol. Metab. 2010, 95, 5320–5329. [Google Scholar] [CrossRef] [PubMed]
- Dharmaraj, N.; Chapela, P.J.; Morgado, M.; Hawkins, S.; Lessey, B.A.; Young, S.L.; Carson, D.D. Expression of the transmembrane mucins, MUC1, MUC4 and MUC16, in normal endometrium and in endometriosis. Hum. Reprod. 2014, 29, 1730–1738. [Google Scholar] [CrossRef] [PubMed]
- Engel, B.J.; Bowser, J.L.; Broaddus, R.R.; Carson, D.D. MUC1 stimulates EGFR expression and function in endometrial cancer. Oncotarget 2016, 7, 32796–32809. [Google Scholar] [CrossRef] [PubMed]
- Paszkiewicz-Gadek, A.; Porowska, H.; Anchim, T.; Wołczyński, S.; Gindzieński, A. Biosynthesis of MUC1 mucin in human endometrial adenocarcinoma is modulated by estradiol and tamoxifen. Gynecol. Endocrinol. 2003, 17, 37–44. [Google Scholar] [CrossRef] [PubMed]
- English, D.P.; Roque, D.M.; Santin, A.D. HER2 Expression Beyond Breast Cancer: Therapeutic Implications for Gynecologic Malignancies. Mol. Diagn. Ther. 2013, 17, 85–99. [Google Scholar] [CrossRef]
- Iqbal, N.; Iqbal, N. Human Epidermal Growth Factor Receptor 2 (HER2) in Cancers: Overexpression and Therapeutic Implications. Mol. Biol. Int. 2014, 2014, 1–9. [Google Scholar] [CrossRef]
- Santin, A.D.; Bellone, S.; Van Stedum, S.; Bushen, W.; Palmieri, M.; Siegel, E.R.; Casas, L.E.D.L.; Roman, J.J.; Burnett, A.; Pecorelli, S. Amplification of c-erbB2 oncogene. Cancer 2005, 104, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Charo, L.M.; Plaxe, S.C. Recent advances in endometrial cancer: A review of key clinical trials from 2015 to 2019. F1000Research 2019, 8, 849. [Google Scholar] [CrossRef]
- Teplinsky, E.; Muggia, F. Targeting HER2 in ovarian and uterine cancers: Challenges and future directions. Gynecol. Oncol. 2014, 135, 364–370. [Google Scholar] [CrossRef]
- Yan, M.; Parker, B.A.; Schwab, R.; Kurzrock, R. HER2 aberrations in cancer: Implications for therapy. Cancer Treat. Rev. 2014, 40, 770–780. [Google Scholar] [CrossRef] [PubMed]
- Healey, G.D.; Pan-Castillo, B.; Garcia-Parra, J.; Davies, J.; Roberts, S.; Jones, E.; Dhar, K.; Nandanan, S.; Tofazzal, N.; Piggott, L.; et al. Antibody drug conjugates against the receptor for advanced glycation end products (RAGE), a novel therapeutic target in endometrial cancer. J. Immunother. Cancer 2019, 7, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Mills, A.; Zadeh, S.; Sloan, E.; Chinn, Z.; Modesitt, S.C.; Ring, K.L. Indoleamine 2,3-dioxygenase in endometrial cancer: A targetable mechanism of immune resistance in mismatch repair-deficient and intact endometrial carcinomas. Mod. Pathol. 2018, 31, 1282–1290. [Google Scholar] [CrossRef] [PubMed]
- Badawy, A.A.-B. Kynurenine Pathway of Tryptophan Metabolism: Regulatory and Functional Aspects. Int. J. Tryptophan Res. 2017, 10. [Google Scholar] [CrossRef]
- Liu, S.; Diao, L.; Huang, C.; Li, Y.; Zeng, Y.; Kwak-Kim, J.Y. The role of decidual immune cells on human pregnancy. J. Reprod. Immunol. 2017, 124, 44–53. [Google Scholar] [CrossRef]
- Vacca, P.; Cantoni, C.; Vitale, M.; Prato, C.; Canegallo, F.; Fenoglio, D.; Ragni, N.; Moretta, L.; Mingari, M.C. Crosstalk between decidual NK and CD14+ myelomonocytic cells results in induction of Tregs and immunosuppression. Proc. Natl. Acad. Sci. USA 2010, 107, 11918–11923. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.-T.; Sun, H.-T.; Zhang, Z.-F.; Shi, R.-X.; Liu, L.-B.; Yu, J.-J.; Zhou, W.-J.; Gu, C.-J.; Yang, S.-L.; Liu, Y.-K.; et al. Indoleamine 2,3-dioxygenase suppresses the cytotoxicity of 1 NK cells in response to ectopic endometrial stromal cells in endometriosis. Reproduction 2018, 156, 397–404. [Google Scholar] [CrossRef]
- Altadill, T.; Dowdy, T.M.; Gill, K.; Reques, A.; Menon, S.S.; Moiola, C.P.; Lopez-Gil, C.; Coll, E.; Matias-Guiu, X.; Cabrera, S.; et al. Metabolomic and Lipidomic Profiling Identifies the Role of the RNA Editing Pathway in Endometrial Carcinogenesis. Sci. Rep. 2017, 7, 8803. [Google Scholar] [CrossRef] [PubMed]
- Ino, K.; Yoshida, N.; Kajiyama, H.; Shibata, K.; Yamamoto, E.; Kidokoro, K.; Takahashi, N.; Terauchi, M.; Nawa, A.; Nomura, S.; et al. Indoleamine 2,3-dioxygenase is a novel prognostic indicator for endometrial cancer. Br. J. Cancer 2006, 95, 1555–1561. [Google Scholar] [CrossRef] [PubMed]
- González, I.; Romero, J.; Rodríguez, B.L.; Pérez-Castro, R.; Rojas, A. The immunobiology of the receptor of advanced glycation end-products: Trends and challenges. Immunobiology 2013, 218, 790–797. [Google Scholar] [CrossRef]
- Zhu, X.; Jin, L.; Zou, S.; Shen, Q.; Jiang, W.; Lin, W.; Zhu, X. Immunohistochemical Expression of RAGE and Its Ligand (S100A9) in Cervical Lesions. Cell Biophys. 2013, 66, 843–850. [Google Scholar] [CrossRef]
- Zheng, L.; Li, D.; Zhou, Y.-M.; Yang, H.; Cheng, D.; Ma, X.-X. Effects of receptor for advanced glycation endproducts on microvessel formation in endometrial cancer. BMC Cancer 2016, 16, 93. [Google Scholar] [CrossRef]
- Xiong, F.; Leonov, S.; Howard, A.C.; Xiong, S.; Zhang, B.; Mei, L.; McNeil, P.; Simon, S.; Xiong, W.-C. Receptor for Advanced Glycation End Products (RAGE) Prevents Endothelial Cell Membrane Resealing and Regulates F-actin Remodeling in a β-Catenin-dependent Manner. J. Biol. Chem. 2011, 286, 35061–35070. [Google Scholar] [CrossRef]
- Al-Swailem, S.; Xu, Z.; Wu, L.; Hartsock, M.J.; Yiu, S.C.; Duh, E.J. Induction of endothelial RAGE ex-pression in pterygium. Mol. Vis. 2014, 20, 1740. [Google Scholar]
- Takahashi, H.K.; Mori, S.; Wake, H.; Liu, K.; Yoshino, T.; Ohashi, K.; Tanaka, N.; Shikata, K.; Makino, H.; Nishibori, M. Advanced Glycation End Products Subspecies-Selectively Induce Adhesion Molecule Expression and Cytokine Production in Human Peripheral Blood Mononuclear Cells. J. Pharmacol. Exp. Ther. 2009, 330, 89–98. [Google Scholar] [CrossRef]
- Sade-Feldman, M.; Kanterman, J.; Ish-Shalom, E.; Elnekave, M.; Horwitz, E.; Baniyash, M. Tumor Necrosis Factor-α Blocks Differentiation and Enhances Suppressive Activity of Immature Myeloid Cells during Chronic Inflammation. Immunology 2013, 38, 541–554. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Khan, H.; Siddiqui, Z.; Khan, M.Y.; Rehman, S.; Shahab, U.; Godovikova, T.; Silnikov, V. Moinuddin AGEs, RAGEs and s-RAGE; friend or foe for cancer. Semin. Cancer Biol. 2018, 49, 44–55. [Google Scholar] [CrossRef]
- Nasser, M.W.; Wani, N.A.; Ahirwar, D.K.; Powell, C.A.; Ravi, J.; Elbaz, M.; Zhao, H.; Padilla, L.; Zhang, X.; Shilo, K.; et al. RAGE Mediates S100A7-Induced Breast Cancer Growth and Metastasis by Modulating the Tumor Microenvironment. Cancer Res. 2015, 75, 974–985. [Google Scholar] [CrossRef] [PubMed]
- Sims, G.P.; Rowe, D.C.; Rietdijk, S.T.; Herbst, R.; Coyle, A.J. HMGB1 and RAGE in Inflammation and Cancer. Annu. Rev. Immunol. 2010, 28, 367–388. [Google Scholar] [CrossRef] [PubMed]
- Merhi, Z.; Kandaraki, E.A.; Diamanti-Kandarakis, E. Implications and Future Perspectives of AGEs in PCOS Pathophysiology. Trends Endocrinol. Metab. 2019, 30, 150–162. [Google Scholar] [CrossRef] [PubMed]
- Kuokkanen, S.; Zhu, L.; Pollard, J.W. Xenografted tissue models for the study of human endometrial biology. Differentiation 2017, 98, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Qu, W.; Zhao, Y.; Wang, X.; Qi, Y.; Zhou, C.; Hua, Y.; Hou, J.; Jiang, S.-W. Culture characters, genetic background, estrogen/progesterone receptor expression, and tumorigenic activities of frequently used sixteen endometrial cancer cell lines. Clin. Chim. Acta 2019, 489, 225–232. [Google Scholar] [CrossRef]
- Flammini, L.; Mantelli, L.; Volpe, A.; Domenichini, G.; Di Lecce, R.; Dondi, M.; Cantoni, A.M.; Barocelli, E.; Quintavalla, F. Rifaximin anti-inflammatory activity on bovine endometrium primary cell cultures: A preliminary study. Veter. Med. Sci. 2018, 4, 326–332. [Google Scholar] [CrossRef]
- Fitzgerald, H.C.; Dhakal, P.; Behura, S.K.; Schust, D.J.; Spencer, T.E. Self-renewing endometrial epithelial organoids of the human uterus. Proc. Natl. Acad. Sci. USA 2019, 116, 23132–23142. [Google Scholar] [CrossRef]
- Girda, E.; Huang, E.C.; Leiserowitz, G.S.; Smith, L.H. The Use of Endometrial Cancer Patient–Derived Organoid Culture for Drug Sensitivity Testing Is Feasible. Int. J. Gynecol. Cancer 2017, 27, 1701–1707. [Google Scholar] [CrossRef]
- Sadok, I.; Tyszczuk-Rotko, K.; Mroczka, R.; Staniszewska, M. Simultaneous voltammetric analysis of tryptophan and kynurenine in culture medium from human cancer cells. Talanta 2020, 209, 120574. [Google Scholar] [CrossRef]
- Sehested, J. A simple method for R banding of human chromosomes, showing a pH-dependent connection between R and G bands. Qual. Life Res. 1974, 21, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.D.; Dabbs, D.J.; Lee, A.V.; McGuire, K.P.; Ahrendt, G.M.; Bhargava, R.; Davidson, N.E.; Brufsky, A.M.; Johnson, R.R.; Oesterreich, S.; et al. Developing in vitro models of human ductal carcinoma in situ from primary tissue explants. Breast Cancer Res. Treat. 2015, 153, 311–321. [Google Scholar] [CrossRef]
- Ricciuti, B.; Leonardi, G.C.; Puccetti, P.; Fallarino, F.; Bianconi, V.; Sahebkar, A.; Baglivo, S.; Chiari, R.; Pirro, M. Targeting indoleamine-2,3-dioxygenase in cancer: Scientific rationale and clinical evidence. Pharmacol. Ther. 2018, 196, 105–116. [Google Scholar] [CrossRef]
- Vanderstraeten, A.; Luyten, C.; Verbist, G.; Tuyaerts, S.; Amant, F. Mapping the immunosuppressive environment in uterine tumors: Implications for immunotherapy. Cancer Immunol. Immunother. 2014, 63, 545–557. [Google Scholar] [CrossRef]
- Mei, J.; Li, M.-Q.; Ding, D.; Li, D.-J.; Jin, L.-P.; Hu, W.-G.; Zhu, X.-Y. Indoleamine 2,3-dioxygenase-1 (IDO1) enhances survival and invasiveness of endometrial stromal cells via the activation of JNK signaling pathway. Int. J. Clin. Exp. Pathol. 2013, 6, 431–444. [Google Scholar] [PubMed]
- Burney, R.O.; Talbi, S.; Hamilton, A.E.; Vo, K.C.; Nyegaard, M.; Nezhat, C.R.; Lessey, B.A.; Giudice, L.C. Gene Expression Analysis of Endometrium Reveals Progesterone Resistance and Candidate Susceptibility Genes in Women with Endometriosis. Endocrinology 2007, 148, 3814–3826. [Google Scholar] [CrossRef] [PubMed]
- Sharma, I.; Dhawan, V.; Saha, S.C.; Rashmi, B.; Dhaliwal, L.K. Implication of the RAGE-EN-RAGE axis in endometriosis. Int. J. Gynecol. Obstet. 2010, 110, 199–202. [Google Scholar] [CrossRef]
- Korwar, A.M.; Bhonsle, H.S.; Chougale, A.D.; Kote, S.S.; Gawai, K.R.; Ghole, V.S.; Koppikar, C.B.; Kulkarni, M.J. Analysis of AGE modified proteins and RAGE expression in HER2/neu negative invasive ductal carcinoma. Biochem. Biophys. Res. Commun. 2012, 419, 490–494. [Google Scholar] [CrossRef]
- Yao, D.; Brownlee, M. Hyperglycemia-Induced Reactive Oxygen Species Increase Expression of the Receptor for Advanced Glycation End Products (RAGE) and RAGE Ligands. Diabetes 2009, 59, 249–255. [Google Scholar] [CrossRef]
- Schutte, S.C.; Taylor, R.N. A tissue-engineered human endometrial stroma that responds to cues for secretory differentiation, decidualization, and menstruation. Fertil. Steril. 2012, 97, 997–1003. [Google Scholar] [CrossRef]
- Lamouille, S.; Xu, J.; Derynck, R. Molecular mechanisms of epithelial–mesenchymal transition. Nat. Rev. Mol. Cell Biol. 2014, 15, 178–196. [Google Scholar] [CrossRef]
- Kyo, S.; Nakamura, M.; Kiyono, T.; Maida, Y.; Kanaya, T.; Tanaka, M.; Yatabe, N.; Inoue, M. Successful Immortalization of Endometrial Glandular Cells with Normal Structural and Functional Characteristics. Am. J. Pathol. 2003, 163, 2259–2269. [Google Scholar] [CrossRef]
- Zhang, H.; Tsao, S.W.; Jin, C.; Strömbeck, B.; Yuen, P.W.; Kwong, Y.-L.; Jin, Y. Sequential cytogenetic and molecular cytogenetic characterization of an SV40T-immortalized nasopharyngeal cell line transformed by Epstein-Barr virus latent membrane protein-1 gene. Cancer Genet. Cytogenet. 2004, 150, 144–152. [Google Scholar] [CrossRef]
- Wu, F.; Chen, X.; Liu, Y.; Liang, B.; Xu, H.; Li, T.C.; Wang, C.C. Decreased MUC1 in endometrium is an independent receptivity marker in recurrent implantation failure during implantation window. Reprod. Biol. Endocrinol. 2018, 16, 60. [Google Scholar] [CrossRef]
- Patterson, A.L.; Zhang, L.; Arango, N.A.; Teixeira, J.; Pru, J.K. Mesenchymal-to-Epithelial Transition Contributes to Endometrial Regeneration Following Natural and Artificial Decidualization. Stem Cells Dev. 2013, 22, 964–974. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Hu, R.; Sullivan, C.; Swanson, R.J.; Oehninger, S.; Sun, Y.-P.; Bocca, S. MFGE8 regulates TGF-β-induced epithelial mesenchymal transition in endometrial epithelial cells in vitro. Reproduction 2016, 152, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Arenda, R.; Jones, B.; Martinez, A.; Goodfellow, P. Endometrial cancer: Molecular markers and management of advancedstage disease. Gynecol. Oncol. 2018, 150, 569–580. [Google Scholar] [CrossRef] [PubMed]
- Halle, M.K.; Tangen, I.L.; Berg, H.F.; Hoivik, E.A.; Mauland, K.K.; Kusonmano, K.; Berg, A.; Hurtado, A.; Kalland, K.H.; Øyan, A.M.; et al. HER2 expression patterns in paired primary and metastatic endometrial cancer lesions. Br. J. Cancer 2018, 118, 378–387. [Google Scholar] [CrossRef] [PubMed]
| No. | Biopsy | Group | Age | Diagnosis |
|---|---|---|---|---|
| 1 | E2-7 | Cancer | 72 | Undifferentiated carcinoma G2, Type II; hyperglycemia |
| 2 | E4-11 | Cancer | 59 | Adenocarcinoma, Type I, G-1, endometrial polyp, dysplasia; hyperglycemia |
| 3 | E9-17 | Cancer | 48 | Type II, G-2, metaplasia in cervix; hyperglycemia |
| 4 | E10-18 | Cancer | 41 | Adenocarcinoma, G-1 and hyperplasia without atypia; hyperglycemia |
| 5 | E12-23 | Cancer | 86 | Type II, G-3 (Carcinoma papillare serosum, HER2+); hyperglycemia |
| 6 | E13-24 | Cancer | 44 | Adenocarcinoma, Type I, G-2 with hyperplasia complex atypica; hyperglycemia |
| 7 | E24-41 | Cancer | 65 | Adenocarcinoma, Type I, G-1; hyperglycemia |
| 8 | E21-37 | Cancer | 66 | Adenocarcinoma, Type I, G-2; hyperglycemia |
| 9 | E16-30 | Cancer | 49 | Adenocarcinoma, Type I, G-2; hyperglycemia |
| 10 | E20-35 | Cancer | 70 | Adenocarcinoma, Type I, G-1; hyperglycemia |
| 11 | E1-6 | Noncancerous | 76 | Endometrial polyp, chronic inflammation of the endometrium; postmenopausal diabetes |
| 12 | E3-8 | Noncancerous | 48 | Chronic inflammation of the endometrium |
| 13 | E5-12 | Noncancerous | 30 | Endometrial polyp, chronic inflammation of the endometrium |
| 14 | E6-14 | Noncancerous | 47 | Endometrial polyp, Endometrial hyperplasia without atypia with chronic inflammation |
| 15 | E7-15 | Noncancerous | 39 | Endometrial necrosis |
| 16 | E11-21 | Noncancerous | 58 | Endometrial polyp; hyperglycemia |
| 17 | E14-25 | Noncancerous | 63 | Endometrial hyperplasia without atypia |
| 18 | E17-33 | Noncancerous | 48 | Endometrial hyperplasia without atypia |
| 19 | E18-34 | Noncancerous | 44 | Endometrial hyperplasia without atypia |
| 20 | E19-36 | Noncancerous | 66 | Endometrial polyp |
| 21 | E22-38 | Noncancerous | 43 | Endometrial hyperplasia without atypia, chronic inflammation of the endometrium |
| 22 | E23-40 | Noncancerous | 39 | Endometrial hyperplasia without atypia |
| No. | Biopsy | Group | IHC Staining | l-Kyn [nmol/mL] | |||
|---|---|---|---|---|---|---|---|
| CK8/18 | HER2 | RAGE | IDO1 | ||||
| 1 | E2-7 | Cancer | na | na | na | na | 1.22 |
| 2 | E4-11 | Cancer | na | na | na | na | 7.86 |
| 3 | E9-17 | Cancer | + | − | + | + | 12.26 |
| 4 | E10-18 | Cancer | + | − | − | − | na |
| 5 | E12-23 | Cancer | na | na | na | na | 11.44 |
| 6 | E13-24 | Cancer | + | − | + | − | 6.55 |
| 7 | E24-41 | Cancer | + | − | + | + | na |
| 8 | E21-37 | Cancer | + | − | + | − | <LOQ |
| 9 | E16-30 | Cancer | + | − | + | + | na |
| 10 | E20-35 | Cancer | na | na | na | na | na |
| 11 | E1-6 | Noncancerous | na | na | na | na | 1.03 |
| 12 | E3-8 | Noncancerous | na | na | na | na | 0.54 |
| 13 | E5-12 | Noncancerous | na | na | na | na | 0.87 |
| 14 | E6-14 | Noncancerous | na | na | na | na | 3.43 |
| 15 | E7-15 | Noncancerous | + | − | − | + | na |
| 16 | E11-21 | Noncancerous | + | − | − | − | 9.39 |
| 17 | E14-25 | Noncancerous | na | na | na | na | <LOQ |
| 18 | E17-33 | Noncancerous | na | na | na | na | 4.78 |
| 19 | E18-34 | Noncancerous | na | na | na | na | 0.77 |
| 20 | E19-36 | Noncancerous | + | − | + | + | na |
| 21 | E22-38 | Noncancerous | + | − | − | − | 1.78 |
| 22 | E23-40 | Noncancerous | na | na | na | na | na |
| Cell Culture | % CK8 | % Vimentin |
|---|---|---|
| E10-18 | 99.3 ± 1.0 | 18.2 ± 7.4 |
| E12-23 | 98.2 ± 3.4 | 5.3 ± 3.1 |
| E13-24 | 98.3 ± 3.4 | 32.9 ± 7.3 |
| E1-6 | 99.4 ± 1.0 | 11.1 ± 4.4 |
| E17-33 | 93.8 ± 6.2 | 23.1 ± 20.7 |
| E22-38 | 96.2 ± 3.2 | 47.3 ± 30.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tkaczuk-Włach, J.; Kędzierski, W.; Jonik, I.; Sadok, I.; Filip, A.; Kankofer, M.; Polkowski, W.; Ziółkowski, P.; Gamian, A.; Staniszewska, M. Immunomodulatory Factors in Primary Endometrial Cell Cultures Isolated from Cancer and Noncancerous Human Tissue–Focus on RAGE and IDO1. Cells 2021, 10, 1013. https://doi.org/10.3390/cells10051013
Tkaczuk-Włach J, Kędzierski W, Jonik I, Sadok I, Filip A, Kankofer M, Polkowski W, Ziółkowski P, Gamian A, Staniszewska M. Immunomodulatory Factors in Primary Endometrial Cell Cultures Isolated from Cancer and Noncancerous Human Tissue–Focus on RAGE and IDO1. Cells. 2021; 10(5):1013. https://doi.org/10.3390/cells10051013
Chicago/Turabian StyleTkaczuk-Włach, Joanna, Witold Kędzierski, Ilona Jonik, Ilona Sadok, Agata Filip, Marta Kankofer, Wojciech Polkowski, Piotr Ziółkowski, Andrzej Gamian, and Magdalena Staniszewska. 2021. "Immunomodulatory Factors in Primary Endometrial Cell Cultures Isolated from Cancer and Noncancerous Human Tissue–Focus on RAGE and IDO1" Cells 10, no. 5: 1013. https://doi.org/10.3390/cells10051013
APA StyleTkaczuk-Włach, J., Kędzierski, W., Jonik, I., Sadok, I., Filip, A., Kankofer, M., Polkowski, W., Ziółkowski, P., Gamian, A., & Staniszewska, M. (2021). Immunomodulatory Factors in Primary Endometrial Cell Cultures Isolated from Cancer and Noncancerous Human Tissue–Focus on RAGE and IDO1. Cells, 10(5), 1013. https://doi.org/10.3390/cells10051013









