New Insights into the Significance of PARP-1 Activation: Flow Cytometric Detection of Poly(ADP-Ribose) as a Marker of Bovine Intramammary Infection
Abstract
1. Introduction
2. Materials and Methods
2.1. Samples Collection
2.2. PAR Detection in LPS Stimulated Bovine Peripheral Blood Mononuclear Cells (PBMC)
2.3. Flow Cytometric Assessment of PAR in Milk Leukocytes
2.4. Preparation of Whole Cell Extracts and Western Blot Analysis
2.5. Statistical Analysis
3. Results
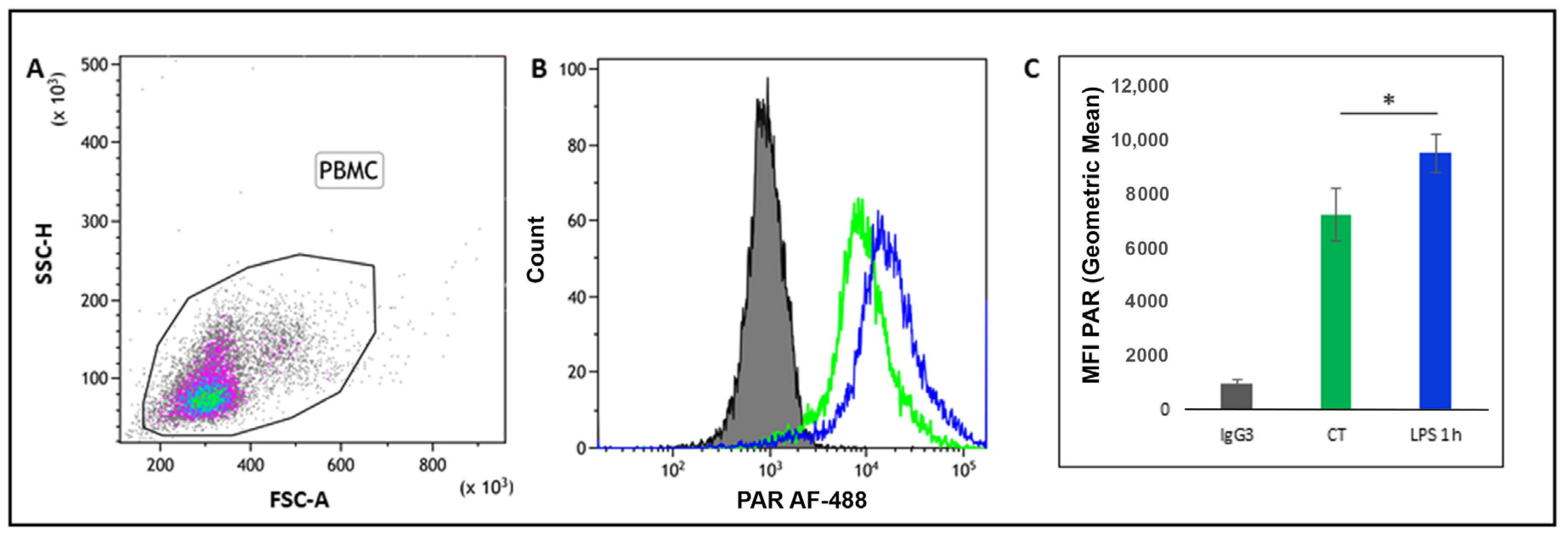
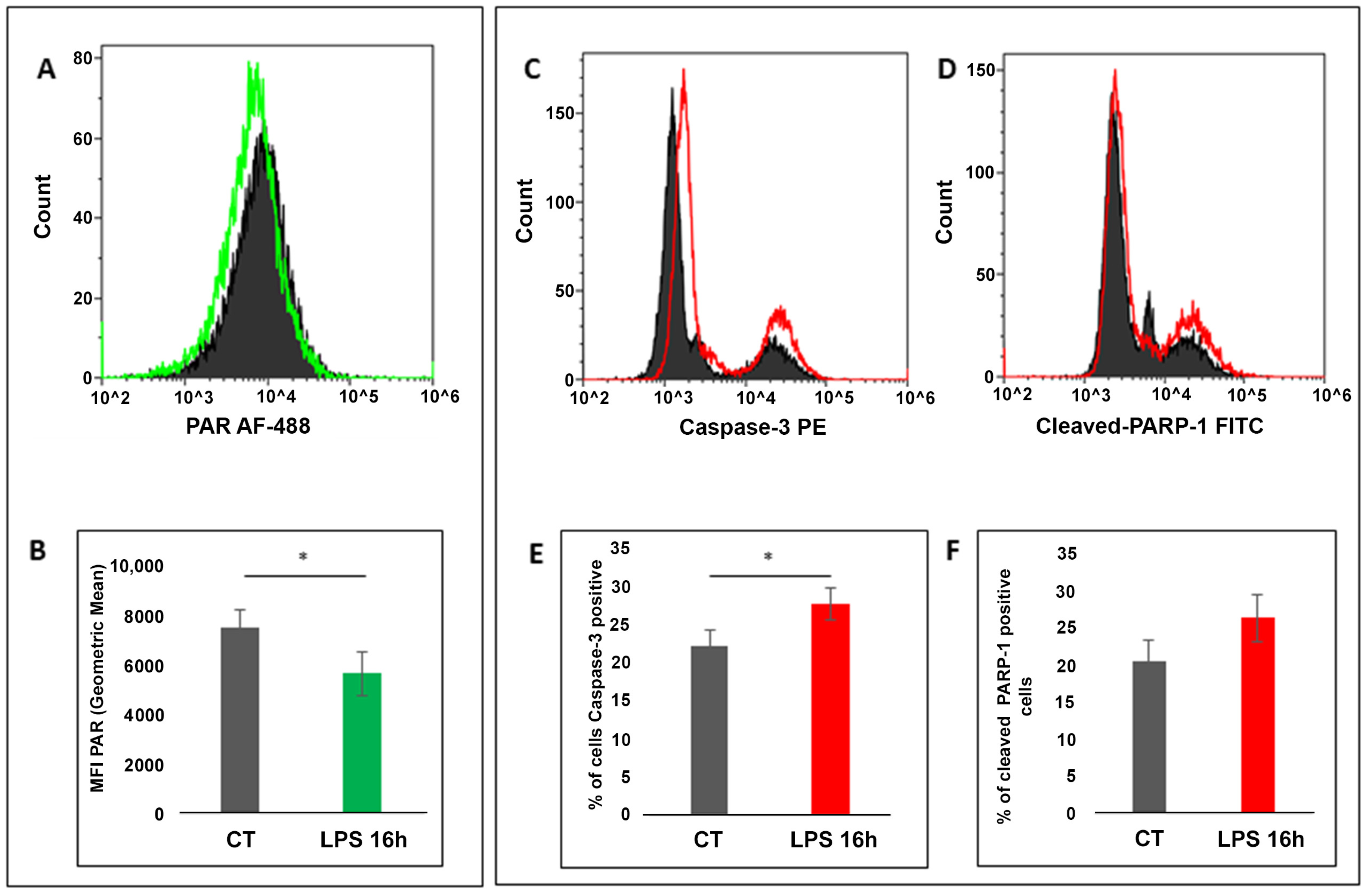
3.1. Flow Cytometry Detection of PAR in “In Vitro” LPS-Stimulated PBMC
3.2. Bacteriological Milk Analysis
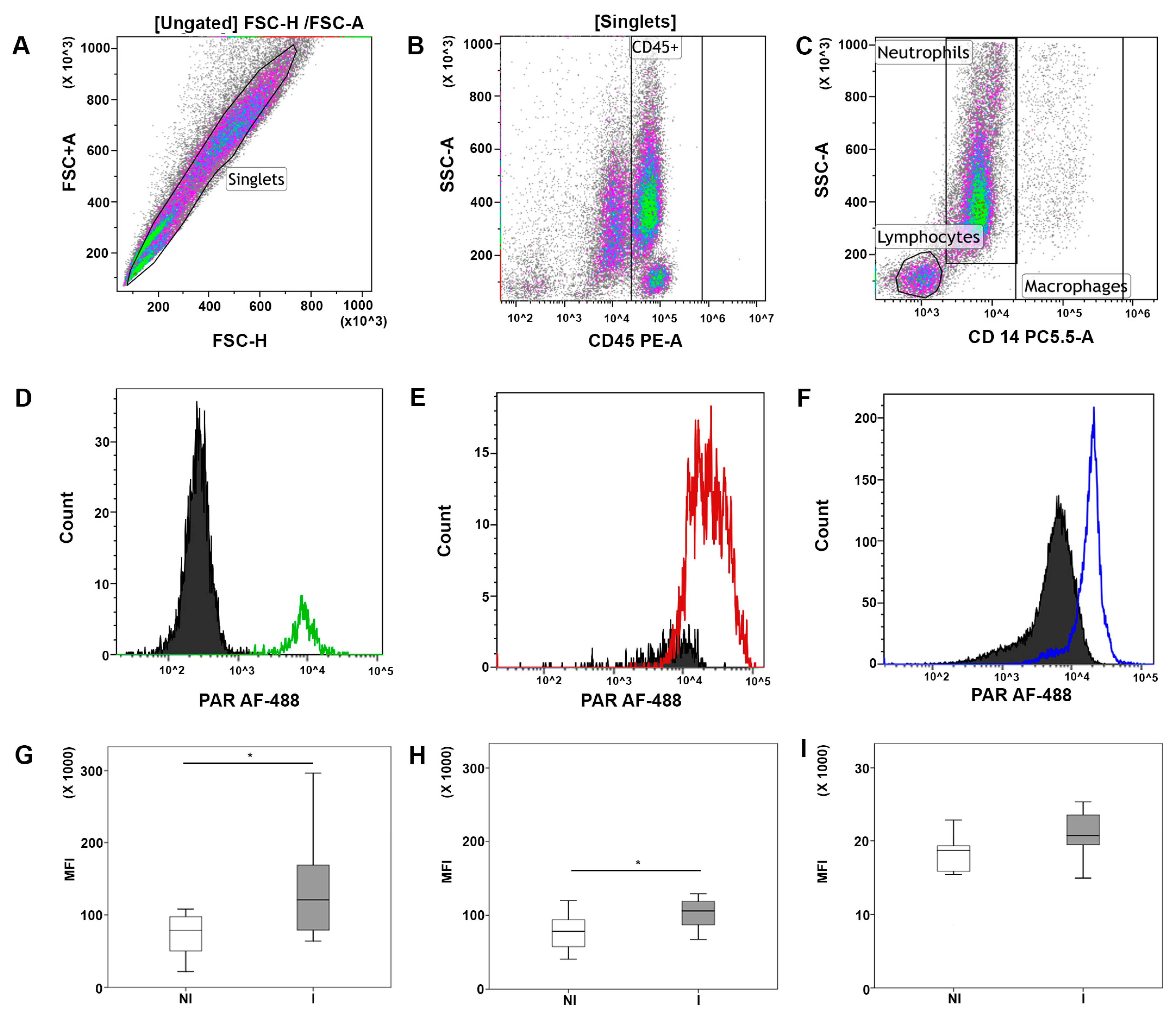
3.3. Flow Cytometry Detection of PAR Levels in Milk Leukocyte Subsets of Healthy and Infected Cows
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015; Available online: http://apps.who.int/iris/bitstream/10665/193736/1/9789241509763_eng.pdf?ua=1 (accessed on 25 February 2021).
- Rainard, P.; Riollet, C. Innate immunity of the bovine mammary gland. Vet. Res. 2006, 37, 369–400. [Google Scholar] [CrossRef] [PubMed]
- Damm, M.; Holm, C.; Blaabjerg, M.; Bro, M.N.; Schwarz, D. Differential somatic cell count-A novel method for routine mastitis screening in the frame of Dairy Herd Improvement testing programs. J. Dairy Sci. 2017, 100, 4926–4940. [Google Scholar] [CrossRef]
- Lugrin, J.; Rosenblatt-Velin, N.; Parapanov, R.; Liaudet, L. The role of oxidative stress during inflammatory processes. Biol. Chem. 2014, 395, 203–230. [Google Scholar] [CrossRef]
- Hassa, P.O.; Hottiger, M.O. The diverse biological roles of mammalian PARPS, a small but powerful family of poly-ADP-ribose polymerases. Front. Biosci. 2008, 13, 3046–3082. [Google Scholar] [CrossRef]
- Altmeyer, M.; Messner, S.; Hassa, P.O.; Fey, M.; Hottiger, M.O. Molecular mechanism of poly(ADP-ribosyl)ation by PARP1 and identification of lysine residues as ADP-ribose acceptor sites. Nucleic Acids Res. 2009, 37, 3723–3738. [Google Scholar] [CrossRef]
- Bai, P.; Virág, L. Role of poly(ADP-ribose) polymerases in the regulation of inflammatory processes. FEBS Lett. 2012, 586, 3771–3777. [Google Scholar] [CrossRef]
- Pazzaglia, S.; Pioli, C. Multifaceted Role of PARP-1 in DNA Repair and Inflammation: Pathological and Therapeutic Implications in Cancer and Non-Cancer Diseases. Cells 2019, 22, 41. [Google Scholar] [CrossRef]
- De Matteis, G.; Reale, A.; Grandoni, F.; Meyer-Ficca, M.L.; Scatà, M.C.; Meyer, R.G.; Buttazzoni, L.; Moioli, B. Assessment of Poly(ADP-ribose) Polymerase1 (PARP1) expression and activity in cells purified from blood and milk of dairy cattle. Vet. Immunol. Immunopathol. 2018, 202, 102–108. [Google Scholar] [CrossRef]
- De Matteis, G.; Grandoni, F.; Scatà, M.C.; Catillo, G.; Moioli, B.; Buttazzoni, L. Flow Cytometry-Detected Immunological Markers and on Farm Recorded Parameters in Composite Cow Milk as Related to Udder Health Status. Vet. Sci. 2020, 7, 114. [Google Scholar] [CrossRef] [PubMed]
- Mabley, J.G.; Horváth, E.M.; Murthy, K.G.; Zsengellér, Z.; Vaslin, A.; Benko, R.; Kollai, M.; Szabó, C. Gender differences in the endotoxin-induced inflammatory and vascular responses: Potential role of poly(ADP-ribose) polymerase activation. J. Pharmacol. Exp. Ther. 2005, 315, 812–820. [Google Scholar] [CrossRef]
- Bacalini, M.G.; Di Lonardo, D.; Catizone, A.; Ciccarone, F.; Bruno, T.; Zampieri, M.; Guastafierro, T.; Calabrese, R.; Fanciulli, M.; Passananti, C.; et al. (Poly(ADP-ribosyl)ation affects stabilization of Che-1 protein in response to DNA damage. DNA Repair 2011, 10, 380–389. [Google Scholar] [CrossRef][Green Version]
- Miettinen, M.; Vedantham, M.; Pulliainen, A.T. Host poly(ADP-ribose) polymerases (PARPs) in acute and chronic bacterial infections. Microb. Infect. 2019, 10, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Widdison, S.; Watson, M.; Coffey, T.J. Early response of bovine alveolar macrophages to infection with live and heat-killed Mycobacterium bovis. Dev. Comp. Immunol. 2011, 35, 580–591. [Google Scholar] [CrossRef]
- Boulanger, D.; Bureau, F.; Mélotte, D.; Mainil, J.; Lekeux, P. Increased nuclear factor κB activity in milk cells of mastitis-affected cows. J. Dairy Sci. 2003, 86, 1259–1267. [Google Scholar] [CrossRef]
- Notebaert, S.; Carlsen, H.; Janssen, D.; Vandenabeele, P.; Blomhoff, R.; Meyer, E. In vivo imaging of NF-κB activity during Escherichia coli-induced mammary gland infection. Cell. Microbiol. 2008, 10, 1249–1258. [Google Scholar] [CrossRef]
- Schwarz, D.; Diesterbeck, U.S.; König, S.; Brügemann, K.; Schlez, K.; Zschöck, M.; Wolter, W.; Czerny, C.P. Flow cytometric differential cell counts in milk for the evaluation of inflammatory reactions in clinically healthy and subclinically infected bovine mammary glands. J. Dairy Sci. 2011, 94, 5033–5044. [Google Scholar] [CrossRef]
- Ogata, S.; Okumura, K.; Taghuci, H. A Simple and Rapid Method for the Detection of Poly(ADP-ribose) by Flow Cytometry. Biosci. Biotechnol. Biochem. 2000, 64, 510–515. [Google Scholar] [CrossRef]
- Kunzmann, A.; Liu, D.; Annett, K.; Malaisé, M.; Thaa, B.; Hyland, P.; Barnett, Y.; Bürkle, A. Flow-cytometric assessment of cellular poly(ADP-ribosyl)ation capacity in peripheral blood lymphocytes. Immun. Ageing 2006, 3, 8. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Horváth, E.M.; Benko, R.; Gero, D.; Kiss, L.; Szabó, C. Treatment with insulin inhibits poly(ADP-ribose)polymerase activation in a rat model of endotoxemia. Life Sci. 2008, 82, 205–209. [Google Scholar] [CrossRef][Green Version]
- Weidele, K.; Kunzmann, A.; Schmitz, M.; Beneke, S.; Bürkle, A. Ex vivo supplementation with nicotinic acid enhances cellular poly(ADP-ribosyl)ation and improves cell viability in human peripheral blood mononuclear cells. Biochem. Pharmacol. 2010, 80, 1103–1112. [Google Scholar] [CrossRef]
- Bohio, A.A.; Sattout, A.; Wang, R.; Wang, K.; Sah, R.K.; Guo, X.; Zeng, X.; Ke, Y.; Boldogh, I.; Ba, X. c-Abl-Mediated Tyrosine Phosphorylation of PARP1 Is Crucial for Expression of Proinflammatory Genes. J. Immunol. 2019, 203, 1521–1531. [Google Scholar] [CrossRef]
- Soldani, C.; Scovassi, A.I. Poly(ADP-ribose) polymerase-1 cleavage during apoptosis: An update. Apoptosis 2002, 7, 321–328. [Google Scholar] [CrossRef]
- Lazebnik, Y.A.; Kaufmann, S.H.; Desnoyers, S.; Poirier, G.G.; Earnshaw, W.C. Cleavage of poly(ADP-ribose) polymerase by a proteinase with properties like ICE. Nature 1994, 371, 346–347. [Google Scholar] [CrossRef]
- Kaufmann, S.H.; Desnoyers, S.; Ottaviano, Y.; Davidson, N.E.; Poirier, G.G. Specific proteolytic cleavage of poly(ADP-ribose) polymerase: An early marker of chemotherapy induced apoptosis. Cancer Res. 1993, 53, 3976–3985. [Google Scholar]
- Crowley, L.C.; Waterhouse, N.J. Detecting Cleaved Caspase-3 in Apoptotic Cells by Flow Cytometry. Cold Spring Harb. Protoc. 2016. [Google Scholar] [CrossRef] [PubMed]
- Giansanti, V.; Donà, F.; Tillhon, M.; Scovassi, A.I. PARP inhibitors: New tools to protect from inflammation. Biochem. Pharmacol. 2010, 80, 1869–1877. [Google Scholar] [CrossRef]
- Palazzo, L.; Mikolčević, P.; Mikoč, A.; Ahel, I. ADP-ribosylation signalling and human disease. Open Biol. 2019, 9, 190041. [Google Scholar] [CrossRef]
| Status | N | SCC (Cells/mL) | p-Value | |
|---|---|---|---|---|
| Mean | SE | |||
| Not Infected | 9 | 109,000 | 66,672 | 0.009 * |
| Infected | 10 | 254,000 | 153,323 | |
| SCC Cells/mL | Lymphocytes (PAR MFI) | Macrophages (PAR MFI) | Neutrophils (PAR MFI) | ||
|---|---|---|---|---|---|
| SCC (cells/mL) | r | 1 | 0.426 | 0.464 | −0.033 |
| p-value | 0.069 | 0.045 | 0.894 | ||
| Lymphocytes (PAR MFI) | r | 1 | 0.523 | 0.227 | |
| p-value | 0.022 | 0.351 | |||
| Macrophages (PAR MFI) | r | 1 | 0.448 | ||
| p-value | 0.054 | ||||
| Neutrophils (PAR MFI) | r | 1 | |||
| p-value |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Matteis, G.; Grandoni, F.; Zampieri, M.; Reale, A.; Scatà, M.C. New Insights into the Significance of PARP-1 Activation: Flow Cytometric Detection of Poly(ADP-Ribose) as a Marker of Bovine Intramammary Infection. Cells 2021, 10, 599. https://doi.org/10.3390/cells10030599
De Matteis G, Grandoni F, Zampieri M, Reale A, Scatà MC. New Insights into the Significance of PARP-1 Activation: Flow Cytometric Detection of Poly(ADP-Ribose) as a Marker of Bovine Intramammary Infection. Cells. 2021; 10(3):599. https://doi.org/10.3390/cells10030599
Chicago/Turabian StyleDe Matteis, Giovanna, Francesco Grandoni, Michele Zampieri, Anna Reale, and Maria Carmela Scatà. 2021. "New Insights into the Significance of PARP-1 Activation: Flow Cytometric Detection of Poly(ADP-Ribose) as a Marker of Bovine Intramammary Infection" Cells 10, no. 3: 599. https://doi.org/10.3390/cells10030599
APA StyleDe Matteis, G., Grandoni, F., Zampieri, M., Reale, A., & Scatà, M. C. (2021). New Insights into the Significance of PARP-1 Activation: Flow Cytometric Detection of Poly(ADP-Ribose) as a Marker of Bovine Intramammary Infection. Cells, 10(3), 599. https://doi.org/10.3390/cells10030599







