GLUT1, GLUT3 Expression and 18FDG-PET/CT in Human Malignant Melanoma: What Relationship Exists? New Insights and Perspectives
Abstract
1. Introduction
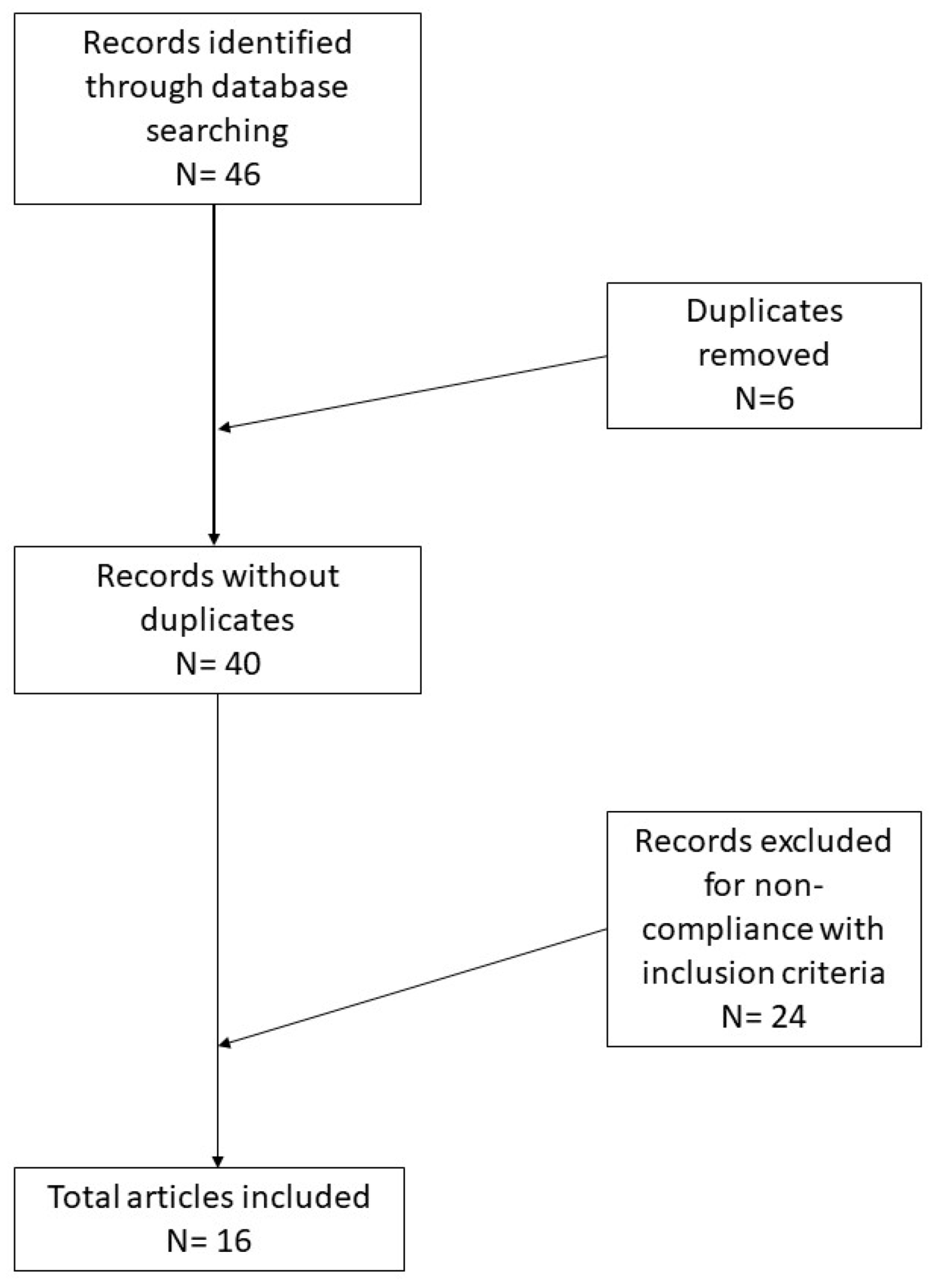
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ali, Z.; Yousaf, N.; Larkin, J. Melanoma epidemiology, biology and prognosis. EJC Suppl. 2013, 11, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.E.; Shalin, S.C.; Tackett, A.J. Current state of melanoma diagnosis and treatment. Cancer Biol. Ther. 2019, 20, 1366–1379. [Google Scholar] [CrossRef] [PubMed]
- Abbas, O.; Miller, D.D.; Bhawan, J. Cutaneous malignant melanoma: Update on diagnostic and prognostic biomarkers. Am. J. Dermatopathol. 2014, 36, 363–379. [Google Scholar] [CrossRef] [PubMed]
- Macapinlac, H.A. FDG PET and PET/CT imaging in lymphoma and melanoma. Cancer J. 2004, 10, 262–270. [Google Scholar] [CrossRef]
- Ždralević, M.; Brand, A.; Di Ianni, L.; Dettmer, K.; Reinders, J.; Singer, K.; Peter, K.; Schnell, A.; Bruss, C.; Decking, S.M.; et al. Double genetic disruption of lactate dehydrogenases A and B is required to ablate the “Warburg effect” restricting tumor growth to oxidative metabolism. J. Biol. Chem. 2018, 293, 15947–15961. [Google Scholar] [CrossRef] [PubMed]
- Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence. Available online: http://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf (accessed on 27 September 2021).
- Cazzato, G.; Arezzo, F.; Colagrande, A.; Cimmino, A.; Lettini, T.; Sablone, S.; Resta, L.; Ingravallo, G. “Animal-Type Melanoma/Pigmented Epithelioid Melanocytoma”: History and Features of a Controversial Entity. Dermatopathology 2021, 8, 271–276. [Google Scholar] [CrossRef]
- Cazzato, G.; Colagrande, A.; Cimmino, A.; Caporusso, C.; Candance, P.M.V.; Trabucco, S.M.R.; Zingarelli, M.; Lorusso, A.; Marrone, M.; Stellacci, A.; et al. Urological Melanoma: A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches. Cancers 2021, 13, 4424. [Google Scholar] [CrossRef]
- Ito, S.; Fukusato, T.; Nemoto, T.; Sekihara, H.; Seyama, Y.; Kubota, S. Coexpression of glucose transporter 1 and matrix metal-loproteinase-2 in human cancers. J. Natl. Cancer Inst. 2002, 94, 1080–1091. [Google Scholar] [CrossRef]
- Chang, S.; Lee, S.; Lee, C.; Kim, J.I.; Kim, Y. Expression of the human erythrocyte glucose transporter in transitional cell carcinoma of the bladder. Urology 2000, 55, 448–452. [Google Scholar] [CrossRef]
- Grover-McKay, M.; Walsh, S.A.; Seftor, E.A.; Thomas, P.A.; Hendrix, M.J. Role for glucose transporter 1 protein in human breast cancer. Pathol. Oncol. Res. 1998, 4, 115–120. [Google Scholar] [CrossRef]
- Kunkel, M.; Moergel, M.; Stockinger, M.; Jeong, J.H.; Fritz, G.; Lehr, H.A.; Whiteside, T.L. Overexpression of GLUT-1 is associated with resistance to radiotherapy and adverse prognosis in squamous cell carcinoma of the oral cavity. Oral Oncol. 2007, 43, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Noguchi, Y.; Satoh, S.; Hayashi, H.; Inayama, Y.; Kitamura, H. Expression of facilitative glucose transporter isoforms in lung carcinomas: Its relation to histologic type, differentiation grade, and tumor stage. Mod. Pathol. 1998, 11, 437–443. [Google Scholar]
- Wachsberger, P.R.; Gressen, E.L.; Bhala, A.; Bobyock, S.B.; Storck, C.; Coss, R.A.; Berd, D.; Leeper, D.B. Variability in glucose transporter-1 levels and hexokinase activity in human melanoma. Melanoma Res. 2002, 12, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Brink, I.; Bissé, E.; Epting, T.; Engelhardt, R. Factors influencing [F-18] 2-fluoro-2-deoxy-D-glucose (F-18 FDG) uptake in melanoma cells: The role of proliferation rate, viability, glucose transporter expression and hexokinase activity. J. Dermatol. 2005, 32, 316–334. [Google Scholar] [CrossRef]
- Parente, P.; Coli, A.; Massi, G.; Mangoni, A.; Fabrizi, M.M.; Bigotti, G. Immunohistochemical expression of the glucose transporters Glut-1 and Glut-3 in human malignant melanomas and benign melanocytic lesions. J. Exp. Clin. Cancer Res. 2008, 27, 34. [Google Scholar] [CrossRef]
- Strobel, K.; Bode, B.; Dummer, R.; Veit-Haibach, P.; Fischer, D.R.; Imhof, L.; Goldinger, S.; Steinert, H.C.; von Schulthess, G.K. Limited value of 18F-FDG PET/CT and S-100B tumour marker in the detection of liver metastases from uveal melanoma compared to liver metastases from cutaneous melanoma. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 1774–1782. [Google Scholar] [CrossRef] [PubMed]
- Park, S.G.; Lee, J.H.; Lee, W.A.; Han, K.M. Biologic correlation between glucose transporters, hexokinase-II, Ki-67 and FDG uptake in malignant melanoma. Nucl. Med. Biol. 2012, 39, 1167–1172. [Google Scholar] [CrossRef] [PubMed]
- Airley, R.; Evans, A.; Mobasheri, A.; Hewitt, S.M. Glucose transporter Glut-1 is detectable in peri-necrotic regions in many human tumor types but not normal tissues: Study using tissue microarrays. Ann. Anat. 2010, 192, 133–138. [Google Scholar] [CrossRef]
- Singer, K.; Kastenberger, M.; Gottfried, E.; Hammerschmied, C.G.; Büttner, M.; Aigner, M.; Seliger, B.; Walter, B.; Schlösser, H.; Hartmann, A.; et al. Warburg phenotype in renal cell carcinoma: High expression of glucose-transporter 1 (GLUT-1) correlates with low CD8+ T-cell infiltration in the tumor. Int. J. Cancer 2011, 128, 2085–2095. [Google Scholar] [CrossRef]
- Slominski, A.; Kim, T.K.; Brożyna, A.A.; Janjetovic, Z.; Brooks, D.L.; Schwab, L.P.; Skobowiat, C.; Jóźwicki, W.; Seagroves, T.N. The role of melanogenesis in regulation of melanoma behavior: Melanogenesis leads to stimulation of HIF-1α expression and HIF-dependent attendant pathways. Arch. Biochem. Biophys. 2014, 563, 79–93. [Google Scholar] [CrossRef]
- Su, J.; Gao, T.; Jiang, M.; Wu, L.; Zeng, W.; Zhao, S.; Peng, C.; Chen, X. CD147 silencing inhibits tumor growth by suppressing glucose transport in melanoma. Oncotarget 2016, 7, 64778–64784. [Google Scholar] [CrossRef] [PubMed]
- Matthews, N.H.; Li, W.Q.; Qureshi, A.A.; Weinstock, M.A.; Cho, E. Epidemiology of Melanoma. In Cutaneous Melanoma: Etiology and Therapy [Internet]; Ward, W.H., Farma, J.M., Eds.; Codon Publications: Brisbane, Australia, 2017; Chapter 1. Available online: https://www.ncbi.nlm.nih.gov/books/NBK481862/ (accessed on 11 October 2021).
- Seleit, I.; Bakry, O.A.; Al-Sharaky, D.R.; Ragab, R.A.A.; Al-Shiemy, S.A. Evaluation of Hypoxia Inducible Factor-1α and Glucose Transporter-1 Expression in Non Melanoma Skin Cancer: An Immunohistochemical Study. J. Clin. Diagn. Res. 2017, 11, EC09–EC16. [Google Scholar] [CrossRef] [PubMed]
- Důra, M.; Němejcová, K.; Jakša, R.; Bártů, M.; Kodet, O.; Tichá, I.; Michálková, R.; Dundr, P. Expression of Glut-1 in Malignant Melanoma and Melanocytic Nevi: An Immunohistochemical Study of 400 Cases. Pathol. Oncol. Res. 2019, 25, 361–368. [Google Scholar] [CrossRef]
- Ruby, K.N.; Liu, C.L.; Li, Z.; Felty, C.C.; Wells, W.A.; Yan, S. Diagnostic and prognostic value of glucose transporters in mela-nocytic lesions. Melanoma Res. 2019, 29, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Na, K.J.; Choi, H.; Oh, H.R.; Kim, Y.H.; Lee, S.B.; Jung, Y.J.; Koh, J.; Park, S.; Lee, H.J.; Jeon, Y.K.; et al. Reciprocal change in Glucose metabolism of Cancer and Immune Cells mediated by different Glucose Transporters predicts Immunotherapy response. Theranostics 2020, 10, 9579–9590. [Google Scholar] [CrossRef] [PubMed]
- Meyer, H.J.; Wienke, A.; Surov, A. Associations between GLUT expression and SUV values derived from FDG-PET in different tumors-A systematic review and meta analysis. PLoS ONE 2019, 14, e0217781. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Lu, P.; Zhou, S.; Zhang, L.; Zhao, J.H.; Tang, J.H. Predictive value of glucose transporter-1 and glucose transporter-3 for survival of cancer patients: A meta-analysis. Oncotarget 2017, 8, 13206–13213. [Google Scholar] [CrossRef][Green Version]
- Reckzeh, E.S.; Karageorgis, G.; Schwalfenberg, M.; Ceballos, J.; Nowacki, J.; Stroet, M.C.M.; Binici, A.; Knauer, L.; Brand, S.; Choidas, A.; et al. Inhibition of Glucose Transporters and Glutaminase Synergistically Impairs Tumor Cell Growth. Cell Chem. Biol. 2019, 26, 1214–1228.e25. [Google Scholar] [CrossRef]
- Asano, T.; Katagiri, H.; Takata, K.; Lin, J.L.; Ishihara, H.; Inukai, K.; Tsukuda, K.; Kikuchi, M.; Hirano, H.; Yazaki, Y.; et al. The role of N-glycosylation of GLUT1 for glucose transport activity. J. Biol. Chem. 1991, 266, 24632–24636. [Google Scholar] [CrossRef]
- Maaßen, T.; Vardanyan, S.; Brosig, A.; Merz, H.; Ranjbar, M.; Kakkassery, V.; Grisanti, S.; Tura, A. Monosomy-3 Alters the Expression Profile of the Glucose Transporters GLUT1-3 in Uveal Melanoma. Int. J. Mol. Sci. 2020, 21, 9345. [Google Scholar] [CrossRef]
| Author(s) | Type of Paper | Neoplasm | Procedure | Results |
|---|---|---|---|---|
| Park et al. [7] | Research article | 19 cases of malignant melanoma | FDG-PET/CT and immunohistochemistry for GLUT1/3 | GLUT1/3 mediate glucose uptake in FDG-PET/CT HK-2 and Ki-67 play no role |
| Dura et al. [8] | Original article | 225 cases of MM/175 benign nevus | Immunohistochemistry for GLUT1 | GLUT1 was expressed in 69/225 MM GLUT1 was negative in benign nevus |
| Strobel et al. [9] | Research article | 27 liver metastases of 13 patients with uveal melanoma 43 liver metastases of 14 patients with CMM | FDG-PET/CT S100B serum marker Cytology Histology Immunohistochemistry for GLUT1 and S-100 | 46% of liver metastases by UM were negative in FDG- PET/CT All liver metastases by CMM were positive S-100B values were significantly higher in the CM patient group compared with the UM patients No obvious difference for GLUT1 and S-100 protein |
| Ruby et al. [10] | Research article | 91 MM 18 metastases of MM 56 benign nevus | Immunohistochemistry for GLUT2/3 | GLUT2 was negative in all melanomas and benign nevi 85.3% expressed either GLUT1 or GLUT3 or both, 39.4% of melanoma cases coexpressed GLUT1 and GLUT3, 17.4% of melanoma cases only expressed GLUT1, 28.4% of melanoma cases only expressed GLUT3 and 14.7% of melanoma cases were negative for both markers |
| Seleit et al. [11] | Case–control and retrospective study | 20BCC 20 SCC | Immunohistochemistry for HIF-1-alpha and GLUT1 | HIF-1-alpha has a role in NMSC pathogenesis, GLUT1 is downregulated |
| Wachsberger et al. [12] | Original article | 31 MM | Western immunoblot analysis for GLUT1 and HK-2 | 30 MM exhibited a 22-fold variation in levels of GLUT1 and 29 exhibited a nine-fold variation in total cellular Hexokinase-II activity |
| Slominski et al. [13] | Original article | 2 cellular lines of MM: amelanotic/melanotic | Cultured cells | Melanogenesis upregulates HIF-1-alpha expression in MM |
| Na et al. [14] | Original article | 63 pulmonary squamous cell carcinoma | FDG-PET/CT RNA-seq Immunohistochemistry | GLUT1/3 may be responsible for a different response to immunotherapy |
| Yamada et al. [15] | Comparative study | 4 cellular lines of human MM: SK-MEL 23, SK-MEL 24 and G361 and 1 murine: B16 | FDG-PET/CT Immunohistochemistry for HK-2 and GLUT1 | Proliferation rate, cell viability and HK expression were important to mediate FDG uptake |
| Parente et al. [16] | Original article | Malignant melanoma/benign nevus | Immunohistochemistry for GLUT1-3 | GLUT1: positive in >90% benign nevus GLUT1: absent in 55% MM GLUT3: present in both (MM and benign nevus) |
| Singer et al. [17] | Research article | 249 RCC | Tissue microarray analysis | In RCC an increased expression of GLUT1 correlates with a decreased presence of CD8 + T lymphocytes |
| Airley et al. [18] | Research article | Different and various tumors | Tissue microarray analysis and immunohistochemistry for GLUT1 | Glut-1 expression in peri- necrotic regions |
| Meyer et al. [19] | Meta-analysis | Different and various tumors | FDG-PET/TC | Overall, only a moderate association was found between GLUT 1/3 expression and SUV values derived from FDG-PET |
| Chen et al. [20] | Review | 12 studies about GLUT1 2 studies about GLUT3 | Review with meta-analysis | A combination of GLUTs 1 and 3 might help predict malignancy of cancers and direct effective cancer therapy |
| Reckzeh et al. [21] | Original article | Various cellular lines | Various procedures | Glutor, very potent glucose uptake inhibitor |
| Su et al. [22] | Research article | Cellular line of MM: A375 | Immunoprecipitation and siRNA | CD147 could downregulate GLUT1 expression by reducing the proliferative rate of MM cells |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cazzato, G.; Colagrande, A.; Cimmino, A.; Abbatepaolo, C.; Bellitti, E.; Romita, P.; Lospalluti, L.; Foti, C.; Arezzo, F.; Loizzi, V.; et al. GLUT1, GLUT3 Expression and 18FDG-PET/CT in Human Malignant Melanoma: What Relationship Exists? New Insights and Perspectives. Cells 2021, 10, 3090. https://doi.org/10.3390/cells10113090
Cazzato G, Colagrande A, Cimmino A, Abbatepaolo C, Bellitti E, Romita P, Lospalluti L, Foti C, Arezzo F, Loizzi V, et al. GLUT1, GLUT3 Expression and 18FDG-PET/CT in Human Malignant Melanoma: What Relationship Exists? New Insights and Perspectives. Cells. 2021; 10(11):3090. https://doi.org/10.3390/cells10113090
Chicago/Turabian StyleCazzato, Gerardo, Anna Colagrande, Antonietta Cimmino, Caterina Abbatepaolo, Emilio Bellitti, Paolo Romita, Lucia Lospalluti, Caterina Foti, Francesca Arezzo, Vera Loizzi, and et al. 2021. "GLUT1, GLUT3 Expression and 18FDG-PET/CT in Human Malignant Melanoma: What Relationship Exists? New Insights and Perspectives" Cells 10, no. 11: 3090. https://doi.org/10.3390/cells10113090
APA StyleCazzato, G., Colagrande, A., Cimmino, A., Abbatepaolo, C., Bellitti, E., Romita, P., Lospalluti, L., Foti, C., Arezzo, F., Loizzi, V., Lettini, T., Sablone, S., Resta, L., Cormio, G., Ingravallo, G., & Rossi, R. (2021). GLUT1, GLUT3 Expression and 18FDG-PET/CT in Human Malignant Melanoma: What Relationship Exists? New Insights and Perspectives. Cells, 10(11), 3090. https://doi.org/10.3390/cells10113090













