The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies
Abstract
1. Introduction
2. HA Synthesis, Properties, and Degradation
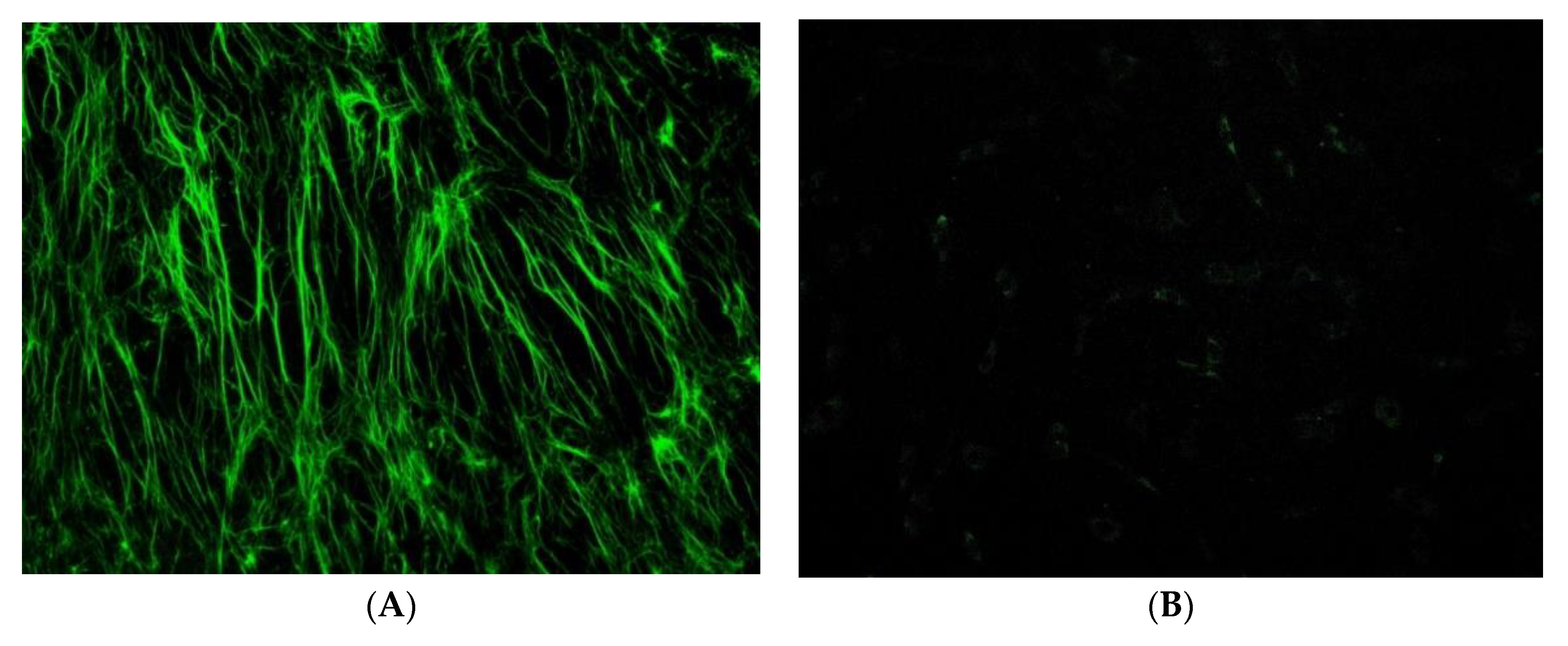
3. Effects on Tendons
4. Tissue Engineering and Tendon Healing
5. Tendinopathies and HA Clinical Applications
6. Rotator Cuff Tendinopathy and HA
7. Patellar Tendinopathy and HA
8. Achilles Tendinopathy and HA
9. Epicondylitis and HA
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Balazs, E.A.; Laurent, T.C.; Jeanloz, R.W. Nomenclature of hyaluronic acid. Biochem. J. 1986, 235, 903. [Google Scholar] [CrossRef]
- Turley, E.A.; Noble, P.W.; Bourguignon, L.Y. Signaling properties of hyaluronan receptors. J. Biol. Chem. 2002, 277, 4589–4592. [Google Scholar] [CrossRef] [PubMed]
- Toole, B.P.; Wight, T.N.; Tammi, M.I. Hyaluronan-cell interactions in cancer and vascular disease. J. Biol. Chem. 2002, 277, 4593–4596. [Google Scholar] [CrossRef] [PubMed]
- Hascall, V.C.; Majors, A.K.; De La Motte, C.A.; Evanko, S.P.; Wang, A.; Drazba, J.A.; Strong, S.A.; Wight, T.N. Intracellular hyaluronan: A new frontier for inflammation? Biochim. Biophys. Acta 2004, 1673, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Kogan, G.; Soltes, L.; Stern, R.; Gemeiner, P. Hyaluronic acid: A natural biopolymer with a broad range of biomedical and industrial applications. Biotechnol. Lett. 2007, 29, 17–25. [Google Scholar] [CrossRef]
- Sawaguchi, N.; Majima, T.; Iwasaki, N.; Funakoshi, T.; Shimode, K.; Onodera, T.; Minami, A. Extracellular matrix modulates expression of cell-surface proteoglycan genes in fibroblasts. Connect Tissue Res. 2006, 47, 141–148. [Google Scholar] [CrossRef]
- Sikes, K.J.; Renner, K.; Li, J.; Grande-Allen, K.J.; Connell, J.P.; Cali, V.; Midura, R.J.; Sandy, J.D.; Plaas, A.; Wang, V.M. Knockout of hyaluronan synthase 1, but not 3, impairs formation of the retrocalcaneal bursa. J. Orthop. Res. 2018, 36, 2622–2632. [Google Scholar] [CrossRef]
- Hess, G.P.; Cappiello, W.L.; Poole, R.M.; Hunter, S.C. Prevention and Treatment of Overuse Tendon Injuries. Sports Med. 1989, 8, 371–384. [Google Scholar] [CrossRef]
- Bolon, B. Mini-Review: Toxic Tendinopathy. Toxicol. Pathol. 2017, 45, 834–837. [Google Scholar] [CrossRef]
- Frizziero, A.; Oliva, F.; Vittadini, F.; Vetrano, M.; Bernetti, A.; Giordan, N.; Vulpiani, M.; Santilli, V.; Masiero, S.; Maffulli, N.; et al. Efficacy of ultrasound-guided hyaluronic acid injections in achilles and patellar tendinopathies:a prospective multicentric clinical trial. Muscles Ligaments Tendon J. 2019, 09, 305. [Google Scholar] [CrossRef]
- Kaux, J.F.; Samson, A.; Crielaard, J.M. Hyaluronic acid and tendon lesions. Muscles Ligaments Tendons J. 2015, 5, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Merolla, G.; Bianchi, P.; Porcellini, G. Ultrasound-guided subacromial injections of sodium hyaluronate for the management of rotator cuff tendinopathy: A prospective comparative study with rehabilitation therapy. Musculoskelet. Surg. 2013, 97 (Suppl. S1), 49–56. [Google Scholar] [CrossRef] [PubMed]
- Kumai, T.; Muneta, T.; Tsuchiya, A.; Shiraishi, M.; Ishizaki, Y.; Sugimoto, K.; Samoto, N.; Isomoto, S.; Tanaka, Y.; Takakura, Y. The short-term effect after a single injection of high-molecular-weight hyaluronic acid in patients with enthesopathies (lateral epicondylitis, patellar tendinopathy, insertional Achilles tendinopathy, and plantar fasciitis): A preliminary study. J. Orthop. Sci. 2014, 19, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Lynen, N.; De Vroey, T.; Spiegel, I.; Van Ongeval, F.; Hendrickx, N.J.; Stassijns, G. Comparison of Peritendinous Hyaluronan Injections Versus Extracorporeal Shock Wave Therapy in the Treatment of Painful Achilles’ Tendinopathy: A Randomized Clinical Efficacy and Safety Study. Arch. Phys. Med. Rehabil. 2017, 98, 64–71. [Google Scholar] [CrossRef]
- Schulz, T.; Schumacher, U.; Prehm, P. Hyaluronan export by the ABC transporter MRP5 and its modulation by intracellular cGMP. J. Biol. Chem. 2007, 282, 20999–21004. [Google Scholar] [CrossRef] [PubMed]
- Vasvani, S.; Kulkarni, P.; Rawtani, D. Hyaluronic acid: A review on its biology, aspects of drug delivery, route of administrations and a special emphasis on its approved marketed products and recent clinical studies. Int. J. Biol. Macromol. 2020, 151, 1012–1029. [Google Scholar] [CrossRef]
- Han, F.; Ishiguro, N.; Ito, T.; Sakai, T.; Iwata, H. Effects of sodium hyaluronate on experimental osteoarthritis in rabbit knee joints. Nagoya J. Med. Sci. 1999, 62, 115–126. [Google Scholar]
- Takahashi, K.; Goomer, R.S.; Harwood, F.; Kubo, T.; Hirasawa, Y.; Amiel, D. The effects of hyaluronan on matrix metalloproteinase-3 (MMP-3), interleukin-1beta(IL-1beta), and tissue inhibitor of metalloproteinase-1 (TIMP-1) gene expression during the development of osteoarthritis. Osteoarthr. Cartil. 1999, 7, 182–190. [Google Scholar] [CrossRef]
- Kang, Y.; Eger, W.; Koepp, H.; Williams, J.M.; Kuettner, K.E.; Homandberg, G.A. Hyaluronan suppresses fibronectin fragment-mediated damage to human cartilage explant cultures by enhancing proteoglycan synthesis. J. Orthop. Res. 1999, 17, 858–869. [Google Scholar] [CrossRef]
- Osti, L.; Berardocco, M.; di Giacomo, V.; Di Bernardo, G.; Oliva, F.; Berardi, A.C. Hyaluronic acid increases tendon derived cell viability and collagen type I expression in vitro: Comparative study of four different Hyaluronic acid preparations by molecular weight. BMC Musculoskelet. Disord 2015, 16, 284. [Google Scholar] [CrossRef] [PubMed]
- Grumet, M.; Friedlander, D.R.; Sakurai, T. Functions of brain chondroitin sulfate proteoglycans during developments: Interactions with adhesion molecules. Perspect. Dev. Neurobiol. 1996, 3, 319–330. [Google Scholar] [PubMed]
- Wight, T.N. Provisional matrix: A role for versican and hyaluronan. Matrix Biol. J. Int. Soc. Matrix Biol. 2017, 60-61, 38–56. [Google Scholar] [CrossRef] [PubMed]
- Roughley, P.J.; Mort, J.S. The role of aggrecan in normal and osteoarthritic cartilage. J. Exp. Orthop. 2014, 1, 8. [Google Scholar] [CrossRef]
- Papadas, A.; Asimakopoulos, F. Versican in the Tumor Microenvironment. Adv. Exp. Med. Biol. 2020, 1272, 55–72. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.H.; Halper, J. Tendon proteoglycans: Biochemistry and function. J. Musculoskelet. Neuronal Interact. 2005, 5, 22–34. [Google Scholar] [PubMed]
- Maxwell, C.A.; McCarthy, J.; Turley, E. Cell-surface and mitotic-spindle RHAMM: Moonlighting or dual oncogenic functions? J. Cell Sci. 2008, 121, 925–932. [Google Scholar] [CrossRef]
- Tolg, C.; McCarthy, J.B.; Yazdani, A.; Turley, E.A. Hyaluronan and RHAMM in wound repair and the “cancerization” of stromal tissues. BioMed Res. Int. 2014, 2014, 103923. [Google Scholar] [CrossRef]
- Assmann, V.; Jenkinson, D.; Marshall, J.F.; Hart, I.R. The intracellular hyaluronan receptor RHAMM/IHABP interacts with microtubules and actin filaments. J. Cell Sci. 1999, 112 Pt 22, 3943–3954. [Google Scholar] [CrossRef]
- Silverman-Gavrila, R.; Silverman-Gavrila, L.; Hou, G.; Zhang, M.; Charlton, M.; Bendeck, M.P. Rear polarization of the microtubule-organizing center in neointimal smooth muscle cells depends on PKCα, ARPC5, and RHAMM. Am. J. Pathol. 2011, 178, 895–910. [Google Scholar] [CrossRef]
- Du, Y.C.; Chou, C.K.; Klimstra, D.S.; Varmus, H. Receptor for hyaluronan-mediated motility isoform B promotes liver metastasis in a mouse model of multistep tumorigenesis and a tail vein assay for metastasis. Proc. Natl. Acad. Sci. USA 2011, 108, 16753–16758. [Google Scholar] [CrossRef]
- Wang, D.; Narula, N.; Azzopardi, S.; Smith, R.S.; Nasar, A.; Altorki, N.K.; Mittal, V.; Somwar, R.; Stiles, B.M.; Du, Y.N. Expression of the receptor for hyaluronic acid mediated motility (RHAMM) is associated with poor prognosis and metastasis in non-small cell lung carcinoma. Oncotarget 2016, 7, 39957–39969. [Google Scholar] [CrossRef]
- Augustin, F.; Fiegl, M.; Schmid, T.; Pomme, G.; Sterlacci, W.; Tzankov, A. Receptor for hyaluronic acid-mediated motility (RHAMM, CD168) expression is prognostically important in both nodal negative and nodal positive large cell lung cancer. J. Clin. Pathol. 2015, 68, 368–373. [Google Scholar] [CrossRef]
- Ishigami, S.; Ueno, S.; Nishizono, Y.; Matsumoto, M.; Kurahara, H.; Arigami, T.; Uchikado, Y.; Setoyama, T.; Arima, H.; Yoshiaki, K.; et al. Prognostic impact of CD168 expression in gastric cancer. BMC cancer 2011, 11, 106. [Google Scholar] [CrossRef]
- Koelzer, V.H.; Huber, B.; Mele, V.; Iezzi, G.; Trippel, M.; Karamitopoulou, E.; Zlobec, I.; Lugli, A. Expression of the hyaluronan-mediated motility receptor RHAMM in tumor budding cells identifies aggressive colorectal cancers. Hum. Pathol. 2015, 46, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.T.; Chen, Z.; Du, Y.N. Immunohistochemical analysis of RHAMM expression in normal and neoplastic human tissues: A cell cycle protein with distinctive expression in mitotic cells and testicular germ cells. Oncotarget 2018, 9, 20941–20952. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.G. Leucocyte Trafficking via the Lymphatic Vasculature- Mechanisms and Consequences. Front. Immunol. 2019, 10, 471. [Google Scholar] [CrossRef] [PubMed]
- de Mos, M.; Joosten, L.A.; Oppers-Walgreen, B.; van Schie, J.T.; Jahr, H.; van Osch, G.J.; Verhaar, J.A. Tendon degeneration is not mediated by regulation of Toll-like receptors 2 and 4 in human tenocytes. J. Orthop. Res. 2009, 27, 1043–1047. [Google Scholar] [CrossRef]
- Su, S.L.; Tsai, C.D.; Lee, C.H.; Salter, D.M.; Lee, H.S. Expression and regulation of Toll-like receptor 2 by IL-1beta and fibronectin fragments in human articular chondrocytes. Osteoarthr. Cartil. 2005, 13, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.A.; Cho, M.L.; Choi, H.Y.; Yoon, C.S.; Jhun, J.Y.; Oh, H.J.; Kim, H.Y. The catabolic pathway mediated by Toll-like receptors in human osteoarthritic chondrocytes. Arthritis Rheum. 2006, 54, 2152–2163. [Google Scholar] [CrossRef]
- Campo, G.M.; Avenoso, A.; D’Ascola, A.; Prestipino, V.; Scuruchi, M.; Nastasi, G.; Calatroni, A.; Campo, S. Hyaluronan differently modulates TLR-4 and the inflammatory response in mouse chondrocytes. BioFactors 2012, 38, 69–76. [Google Scholar] [CrossRef]
- Day, A.J.; Milner, C.M. TSG-6: A multifunctional protein with anti-inflammatory and tissue-protective properties. Matrix Biol. J. Int. Soc. Matrix Biol. 2019, 78-79, 60–83. [Google Scholar] [CrossRef]
- Bignami, A.; Hosley, M.; Dahl, D. Hyaluronic acid and hyaluronic acid-binding proteins in brain extracellular matrix. Anat. Embryol. 1993, 188, 419–433. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.J.; Kim, H.J.; Ha, J.; Kim, H.J.; Ryu, J.; Park, K.H.; Kim, U.H.; Lee, Z.H.; Kim, H.M.; Fisher, D.E.; et al. Hyaluronan inhibits osteoclast differentiation via Toll-like receptor 4. J. Cell Sci. 2007, 120, 166–176. [Google Scholar] [CrossRef]
- Schwartz, A.J.; Sarver, D.C.; Sugg, K.B.; Dzierzawski, J.T.; Gumucio, J.P.; Mendias, C.L. p38 MAPK signaling in postnatal tendon growth and remodeling. PLoS ONE 2015, 10, e0120044. [Google Scholar] [CrossRef]
- Mitsui, Y.; Gotoh, M.; Nakama, K.; Yamada, T.; Higuchi, F.; Nagata, K. Hyaluronic acid inhibits mRNA expression of proinflammatory cytokines and cyclooxygenase-2/prostaglandin E(2) production via CD44 in interleukin-1-stimulated subacromial synovial fibroblasts from patients with rotator cuff disease. J. Orthop. Res. 2008, 26, 1032–1037. [Google Scholar] [CrossRef]
- Holmes, M.W.; Bayliss, M.T.; Muir, H. Hyaluronic acid in human articular cartilage. Age-related changes in content and size. Biochem. J. 1988, 250, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Stecco, C.; Stern, R.; Porzionato, A.; Macchi, V.; Masiero, S.; Stecco, A.; De Caro, R. Hyaluronan within fascia in the etiology of myofascial pain. Surg. Radiol. Anat. 2011, 33, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Huskisson, E.C.; Donnelly, S. Hyaluronic acid in the treatment of osteoarthritis of the knee. Rheumatology 1999, 38, 602–607. [Google Scholar] [CrossRef]
- McKee, C.M.; Penno, M.B.; Cowman, M.; Burdick, M.D.; Strieter, R.M.; Bao, C.; Noble, P.W. Hyaluronan (HA) fragments induce chemokine gene expression in alveolar macrophages. The role of HA size and CD44. J. Clin. Investig. 1996, 98, 2403–2413. [Google Scholar] [CrossRef]
- Tesar, B.M.; Jiang, D.; Liang, J.; Palmer, S.M.; Noble, P.W.; Goldstein, D.R. The role of hyaluronan degradation products as innate alloimmune agonists. Am. J. Transpl. 2006, 6, 2622–2635. [Google Scholar] [CrossRef]
- Stern, R.; Kogan, G.; Jedrzejas, M.; Soltés, L. The many ways to cleave hyaluronan. Biotechnol. Adv. 2007, 25, 537–557. [Google Scholar] [CrossRef]
- Aruffo, A.; Stamenkovic, I.; Melnick, M.; Underhill, C.B.; Seed, B. CD44 is the principal cell surface receptor for hyaluronate. Cell 1990, 61, 1303–1313. [Google Scholar] [CrossRef]
- Stern, R.; Maibach, H.I. Hyaluronan in skin: Aspects of aging and its pharmacologic modulation. Clin. Derm. 2008, 26, 106–122. [Google Scholar] [CrossRef]
- Hubbard, A.K.; Rothlein, R. Intercellular adhesion molecule-1 (ICAM-1) expression and cell signaling cascades. Free Radic Biol. Med. 2000, 28, 1379–1386. [Google Scholar] [CrossRef]
- Edsfeldt, S.; Holm, B.; Mahlapuu, M.; Reno, C.; Hart, D.A.; Wiig, M. PXL01 in sodium hyaluronate results in increased PRG4 expression: A potential mechanism for anti-adhesion. Ups J. Med. Sci. 2017, 122, 28–34. [Google Scholar] [CrossRef]
- Halici, M.; Karaoglu, S.; Canoz, O.; Kabak, S.; Baktir, A. Sodium hyaluronate regulating angiogenesis during Achilles tendon healing. Knee Surg. Sports Traumatol. Arthrosc. 2004, 12, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Slack, C.; Bradley, G.; Beaumont, B.; Poole, A.; Flint, M. Changes in the morphology and synthetic activity of cultured rat tail tendon. Cell Tissue Res. 1986, 245, 359–368. [Google Scholar] [CrossRef] [PubMed]
- St Onge, R.; Weiss, C.; Denlinger, J.L.; Balazs, E.A. A preliminary assessment of Na-hyaluronate injection into “no man’s land” for primary flexor tendon repair. Clin. Orthop. Relat. Res. 1980, 146, 269–275. [Google Scholar]
- Gopinath, C.; Nathar, T.J.; Ghosh, A.; Hickstein, D.D.; Nelson, E.J.R. Contemporary Animal Models For Human Gene Therapy Applications. Curr. Gene Ther. 2015, 15, 531–540. [Google Scholar] [CrossRef]
- Amiel, D.; Ishizue, K.; Billings, E., Jr.; Wiig, M.; Vande Berg, J.; Akeson, W.H.; Gelberman, R. Hyaluronan in flexor tendon repair. J. Hand Surg. Am. 1989, 14, 837–843. [Google Scholar] [CrossRef]
- Sakata, T.; Scudamore, R.A.; Cooke, T.D. Antigen-induced tenosynovitis in hypersensitized rabbits: A model for rheumatoid tenosynovitis. Rheumatol. Int. 1988, 8, 47–53. [Google Scholar] [CrossRef]
- Yuzawa, K. Experimental studies on the healing and restoration of gliding function of the injured digital flexor tendon. Part 9: The use of drugs to prevent adhesion formation of the injured tendon. Nihon Seikeigeka Gakkai Zasshi 1985, 59, 1107–1118. [Google Scholar]
- Tallon, C.; Maffulli, N.; Ewen, S.W. Ruptured Achilles tendons are significantly more degenerated than tendinopathic tendons. Med. Sci. Sports Exerc. 2001, 33, 1983–1990. [Google Scholar] [CrossRef] [PubMed]
- Maganaris, C.N.; Narici, M.V.; Almekinders, L.C.; Maffulli, N. Biomechanics and pathophysiology of overuse tendon injuries: Ideas on insertional tendinopathy. Sports Med. 2004, 34, 1005–1017. [Google Scholar] [CrossRef] [PubMed]
- Chisari, E.; Rehak, L.; Khan, W.S.; Maffulli, N. Tendon healing in presence of chronic low-level inflammation: A systematic review. Br. Med. Bull. 2019, 132, 97–116. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Gotoh, M.; Kanazawa, T.; Ohta, K.; Nakamura, K.; Honda, H.; Ohzono, H.; Shimokobe, H.; Mitsui, Y.; Shirachi, I.; et al. Effects of corticosteroids and hyaluronic acid on torn rotator cuff tendons in vitro and in rats. J. Orthop. Res. 2015, 33, 1523–1530. [Google Scholar] [CrossRef] [PubMed]
- Frizziero, A.; Vittadini, F.; Barazzuol, M.; Gasparre, G.; Finotti, P.; Meneghini, A.; Maffulli, N.; Masiero, S. Extracorporeal shockwaves therapy versus hyaluronic acid injection for the treatment of painful non-calcific rotator cuff tendinopathies: Preliminary results. J. Sports Med. Phys. Fit. 2017, 57, 1162–1168. [Google Scholar] [CrossRef]
- Wiig, M.; Abrahamsson, S.O.; Lundborg, G. Effects of hyaluronan on cell proliferation and collagen synthesis: A study of rabbit flexor tendons in vitro. J. Hand Surg. Am. 1996, 21, 599–604. [Google Scholar] [CrossRef]
- Dean, B.J.; Franklin, S.L.; Carr, A.J. A systematic review of the histological and molecular changes in rotator cuff disease. Bone Jt. Res. 2012, 1, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Neumann, A.; Schinzel, R.; Palm, D.; Riederer, P.; Munch, G. High molecular weight hyaluronic acid inhibits advanced glycation endproduct-induced NF-kappaB activation and cytokine expression. FEBS Lett. 1999, 453, 283–287. [Google Scholar] [CrossRef]
- Ozgenel, G.Y.; Etoz, A. Effects of repetitive injections of hyaluronic acid on peritendinous adhesions after flexor tendon repair: A preliminary randomized, placebo-controlled clinical trial. Ulus Travma Acil. Cerrahi Derg. 2012, 18, 11–17. [Google Scholar] [CrossRef]
- Hsiao, M.Y.; Lin, A.C.; Liao, W.H.; Wang, T.G.; Hsu, C.H.; Chen, W.S.; Lin, F.H. Drug-loaded hyaluronic acid hydrogel as a sustained-release regimen with dual effects in early intervention of tendinopathy. Sci. Rep. 2019, 9, 4784. [Google Scholar] [CrossRef]
- Doroski, D.M.; Levenston, M.E.; Temenoff, J.S. Cyclic tensile culture promotes fibroblastic differentiation of marrow stromal cells encapsulated in poly(ethylene glycol)-based hydrogels. Tissue Eng. Part A 2010, 16, 3457–3466. [Google Scholar] [CrossRef]
- Pereira, H.; Sousa, D.A.; Cunha, A.; Andrade, R.; Espregueira-Mendes, J.; Oliveira, J.M.; Reis, R.L. Hyaluronic Acid. Adv. Exp. Med. Biol. 2018, 1059, 137–153. [Google Scholar] [CrossRef]
- Baier Leach, J.; Bivens, K.A.; Patrick, C.W., Jr.; Schmidt, C.E. Photocrosslinked hyaluronic acid hydrogels: Natural, biodegradable tissue engineering scaffolds. Biotechnol. Bioeng. 2003, 82, 578–589. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, S.; Bahadur, P. Modified hyaluronic acid based materials for biomedical applications. Int. J. Biol. Macromol. 2019, 121, 556–571. [Google Scholar] [CrossRef] [PubMed]
- Kozusko, S.D.; Hassouba, M.; Hill, D.M.; Liu, X.; Dadireddy, K.; Velamuri, S.R. Esterified Hyaluronic Acid Matrix in Lower Extremity Reconstruction With Exposed Tendon and Bone: A Retrospective Review. J. Burn. Care Res. 2020, 41, 828–834. [Google Scholar] [CrossRef] [PubMed]
- Cipollaro, L.; Ciardulli, M.C.; Della Porta, G.; Peretti, G.M.; Maffulli, N. Biomechanical issues of tissue-engineered constructs for articular cartilage regeneration: In vitro and in vivo approaches. Br. Med. Bull. 2019, 132, 53–80. [Google Scholar] [CrossRef]
- d’Angelo, M.; Benedetti, E.; Tupone, M.G.; Catanesi, M.; Castelli, V.; Antonosante, A.; Cimini, A. The Role of Stiffness in Cell Reprogramming: A Potential Role for Biomaterials in Inducing Tissue Regeneration. Cells 2019, 8, 1036. [Google Scholar] [CrossRef]
- Ciardulli, M.C.; Marino, L.; Lovecchio, J.; Giordano, E.; Forsyth, N.R.; Selleri, C.; Maffulli, N.; Porta, G.D. Tendon and Cytokine Marker Expression by Human Bone Marrow Mesenchymal Stem Cells in a Hyaluronate/Poly-Lactic-Co-Glycolic Acid (PLGA)/Fibrin Three-Dimensional (3D) Scaffold. Cells 2020, 9, 1268. [Google Scholar] [CrossRef]
- Esenyel, C.Z.; Tekin, C.; Cakar, M.; Bayraktar, K.; Saygili, S.; Esenyel, M.; Tekin, Z.N. Surgical treatment of the neglected achilles tendon rupture with Hyalonect. J. Am. Podiatr. Med. Assoc. 2014, 104, 434–443. [Google Scholar] [CrossRef]
- Maffulli, N.; Longo, U.G.; Loppini, M.; Denaro, V. Current treatment options for tendinopathy. Expert Opin. Pharm. 2010, 11, 2177–2186. [Google Scholar] [CrossRef]
- Del Buono, A.; Battery, L.; Denaro, V.; Maccauro, G.; Maffulli, N. Tendinopathy and inflammation: Some truths. Int. J. Immunopathol. Pharm. 2011, 24, 45–50. [Google Scholar] [CrossRef]
- Frizziero, A.; Salamanna, F.; Della Bella, E.; Vittadini, F.; Gasparre, G.; Nicoli Aldini, N.; Masiero, S.; Fini, M. The Role of Detraining in Tendon Mechanobiology. Front. Aging Neurosci. 2016, 8, 43. [Google Scholar] [CrossRef] [PubMed]
- Oliva, F.; Piccirilli, E.; Berardi, A.C.; Frizziero, A.; Tarantino, U.; Maffulli, N. Hormones and tendinopathies: The current evidence. Br. Med. Bull. 2016, 117, 39–58. [Google Scholar] [CrossRef]
- Ackermann, P.W.; Renstrom, P. Tendinopathy in sport. Sports Health 2012, 4, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Abate, M.; Silbernagel, K.G.; Siljeholm, C.; Di Iorio, A.; De Amicis, D.; Salini, V.; Werner, S.; Paganelli, R. Pathogenesis of tendinopathies: Inflammation or degeneration? Arthritis Res. Ther. 2009, 11, 235. [Google Scholar] [CrossRef]
- Yamamoto, A.; Takagishi, K.; Osawa, T.; Yanagawa, T.; Nakajima, D.; Shitara, H.; Kobayashi, T. Prevalence and risk factors of a rotator cuff tear in the general population. J. Shoulder. Elb. Surg. 2010, 19, 116–120. [Google Scholar] [CrossRef]
- Meloni, F.; Milia, F.; Cavazzuti, M.; Doria, C.; Lisai, P.; Profili, S.; Meloni, G.B. Clinical evaluation of sodium hyaluronate in the treatment of patients with sopraspinatus tendinosis under echographic guide: Experimental study of periarticular injections. Eur. J. Radiol. 2008, 68, 170–173. [Google Scholar] [CrossRef] [PubMed]
- Flores, C.; Balius, R.; Alvarez, G.; Buil, M.A.; Varela, L.; Cano, C.; Casariego, J. Efficacy and Tolerability of Peritendinous Hyaluronic Acid in Patients with Supraspinatus Tendinopathy: A Multicenter, Randomized, Controlled Trial. Sports Med. Open 2017, 3, 22. [Google Scholar] [CrossRef][Green Version]
- Kaux, J.F.; Forthomme, B.; Goff, C.L.; Crielaard, J.M.; Croisier, J.L. Current opinions on tendinopathy. J. Sports Sci. Med. 2011, 10, 238–253. [Google Scholar]
- Muneta, T.; Koga, H.; Ju, Y.J.; Mochizuki, T.; Sekiya, I. Hyaluronan injection therapy for athletic patients with patellar tendinopathy. J. Orthop. Sci. 2012, 17, 425–431. [Google Scholar] [CrossRef]
- Fogli, M.; Giordan, N.; Mazzoni, G. Efficacy and safety of hyaluronic acid (500–730 kDa) Ultrasound-guided injections on painful tendinopathies: A prospective, open label, clinical study. Muscles Ligaments Tendons J. 2017, 7, 388–395. [Google Scholar] [CrossRef]
- Kaux, J.; Bornheim, S.; Dardenne, N.; Deroisy, R.; Samson, A.J.; Roberjot, M.; Croisier, J.L. Comparison between platelet-rich plasma injections and hyaluronic acid injections in the treatment of patellar tendinopathies: A randomized trial. Muscles Ligaments Tendons J. 2019, 09, 156. [Google Scholar] [CrossRef]
- Vora, A.M.; Myerson, M.S.; Oliva, F.; Maffulli, N. Tendinopathy of the main body of the Achilles tendon. Foot Ankle Clin. 2005, 10, 293–308. [Google Scholar] [CrossRef] [PubMed]
- Gervasi, M.; Barbieri, E.; Capparucci, I.; Annibalini, G.; Sisti, D.; Amatori, S.; Carrabs, V.; Valli, G.; Donati Zeppa, S.; Rocchi, M.B.L.; et al. Treatment of Achilles Tendinopathy in Recreational Runners with Peritendinous Hyaluronic Acid Injections: A Viscoelastometric, Functional, and Biochemical Pilot Study. J. Clin. Med. 2021, 10, 1397. [Google Scholar] [CrossRef] [PubMed]
- Coari, G.P.F.; Tajana, G. Fisiopatologia tendinea & Acido Ialuronico. Med. Sport. 2001, 1, 79. [Google Scholar]
- Verhaar, J.A. Tennis elbow. Anatomical, epidemiological and therapeutic aspects. Int. Orthop. 1994, 18, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Petrella, R.J.; Cogliano, A.; Decaria, J.; Mohamed, N.; Lee, R. Management of Tennis Elbow with sodium hyaluronate periarticular injections. Sports Med. Arthrosc. Rehabil. Ther. Technol. 2010, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.U.; Awan, A.S.; Khan, A.S.; Marwat, I.; Meraj, M. Efficacy Of A Single-Injection Sodium Hyaluronate Treatment In Lateral Epicondylitis. J. Ayub Med. Coll. Abbottabad 2018, 30, 85–89. [Google Scholar] [PubMed]
- Tosun, H.B.; Gumustas, S.; Agir, I.; Uludag, A.; Serbest, S.; Pepele, D.; Ertem, K. Comparison of the effects of sodium hyaluronate-chondroitin sulphate and corticosteroid in the treatment of lateral epicondylitis: A prospective randomized trial. J. Orthop. Sci. 2015, 20, 837–843. [Google Scholar] [CrossRef] [PubMed]


| ECM Components | % |
|---|---|
| Collagen | 86% (type I: 98%) |
| Proteoglycan | 1–5% |
| Elastin | 2% |
| Decorin | <1% |
| Aggrecan | <1% |
| Other proteins | <1% |
| HA SYNTHASES | |
|---|---|
| HMW-HA and LMW-HA | HAS1 |
| HAS2 | |
| LMW-HA | HAS3 |
| HA and ECM Receptors Interactions | |
|---|---|
| Function | |
| CD44 Receptor for hyaluronan-mediated motility (RHAMM) | Binding HA: anti-inflammatory, wound healing, antiangiogenic, immunosuppressive |
| Lymphatic vessel endothelial hyaluronan receptor 1 (LYVE-1) | Lymphatic transport of leukocytes |
| Toll-like receptor 4 (TLR-4) | Binding LMW-HA: pro-inflammatory |
| TNF-stimulated gene 6 (TSG-6) | Tissue protective and anti-inflammatory |
| Glial hyaluronate-binding protein (GHAP) | Reduces the spread of inflammatory cells in nerve tissue |
| Neurocan Versican Aggrecan | Development, cell migration, maturation and differentiation, cell survival, and tissue homeostasis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliva, F.; Marsilio, E.; Asparago, G.; Frizziero, A.; Berardi, A.C.; Maffulli, N. The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies. Cells 2021, 10, 3081. https://doi.org/10.3390/cells10113081
Oliva F, Marsilio E, Asparago G, Frizziero A, Berardi AC, Maffulli N. The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies. Cells. 2021; 10(11):3081. https://doi.org/10.3390/cells10113081
Chicago/Turabian StyleOliva, Francesco, Emanuela Marsilio, Giovanni Asparago, Antonio Frizziero, Anna Concetta Berardi, and Nicola Maffulli. 2021. "The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies" Cells 10, no. 11: 3081. https://doi.org/10.3390/cells10113081
APA StyleOliva, F., Marsilio, E., Asparago, G., Frizziero, A., Berardi, A. C., & Maffulli, N. (2021). The Impact of Hyaluronic Acid on Tendon Physiology and Its Clinical Application in Tendinopathies. Cells, 10(11), 3081. https://doi.org/10.3390/cells10113081









