Molecular Mechanisms of Multi-Organ Failure in COVID-19 and Potential of Stem Cell Therapy
Abstract
:1. Introduction
2. Current Knowledge
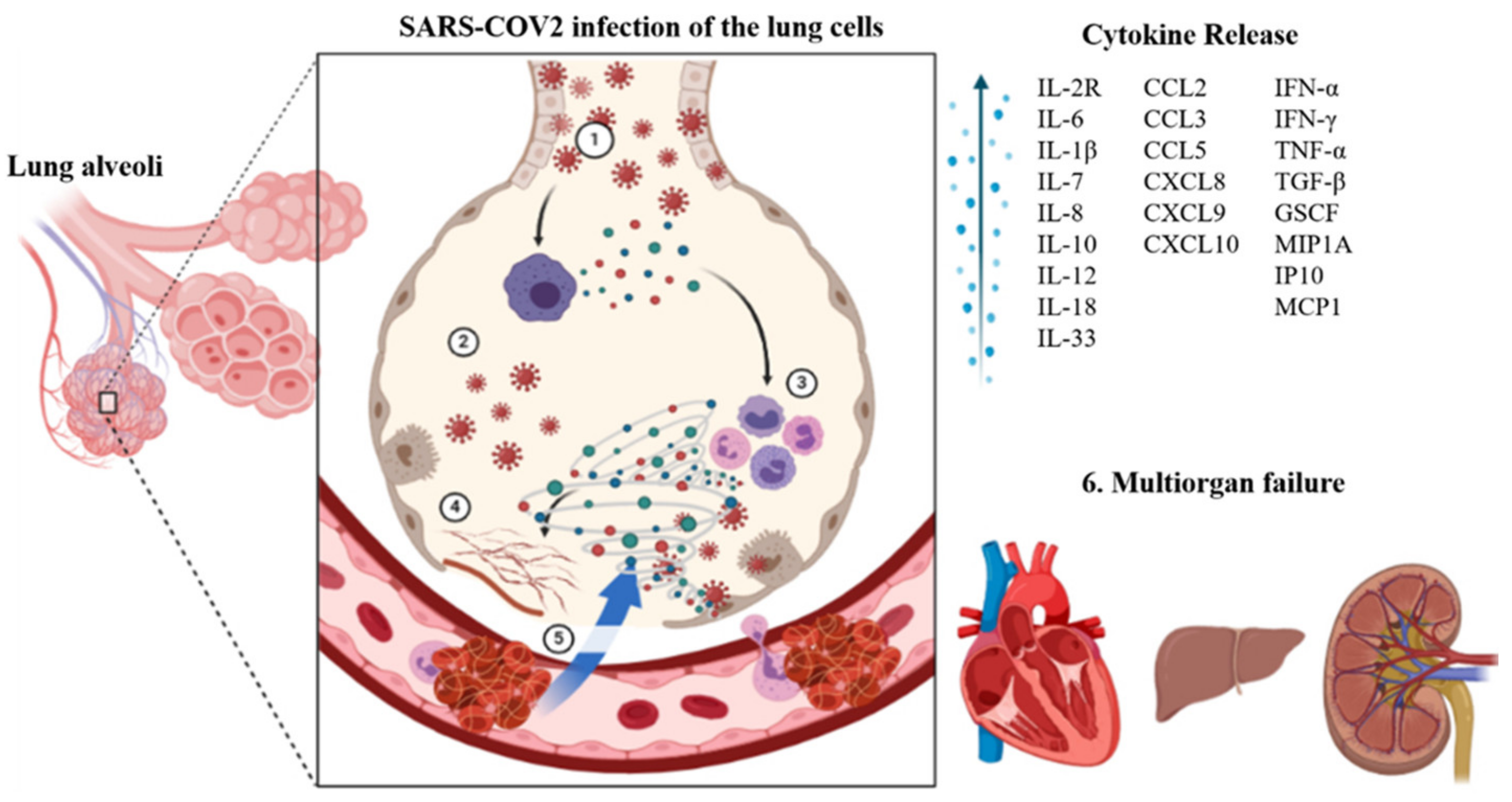
2.1. Immunological Complications
2.2. Hematological Complications
2.3. Respiratory Complications
2.4. Cardiac Complications
2.5. Renal Complications
2.6. Hepatic Complications
2.7. Neurological Complications
3. Stem Cell Therapy
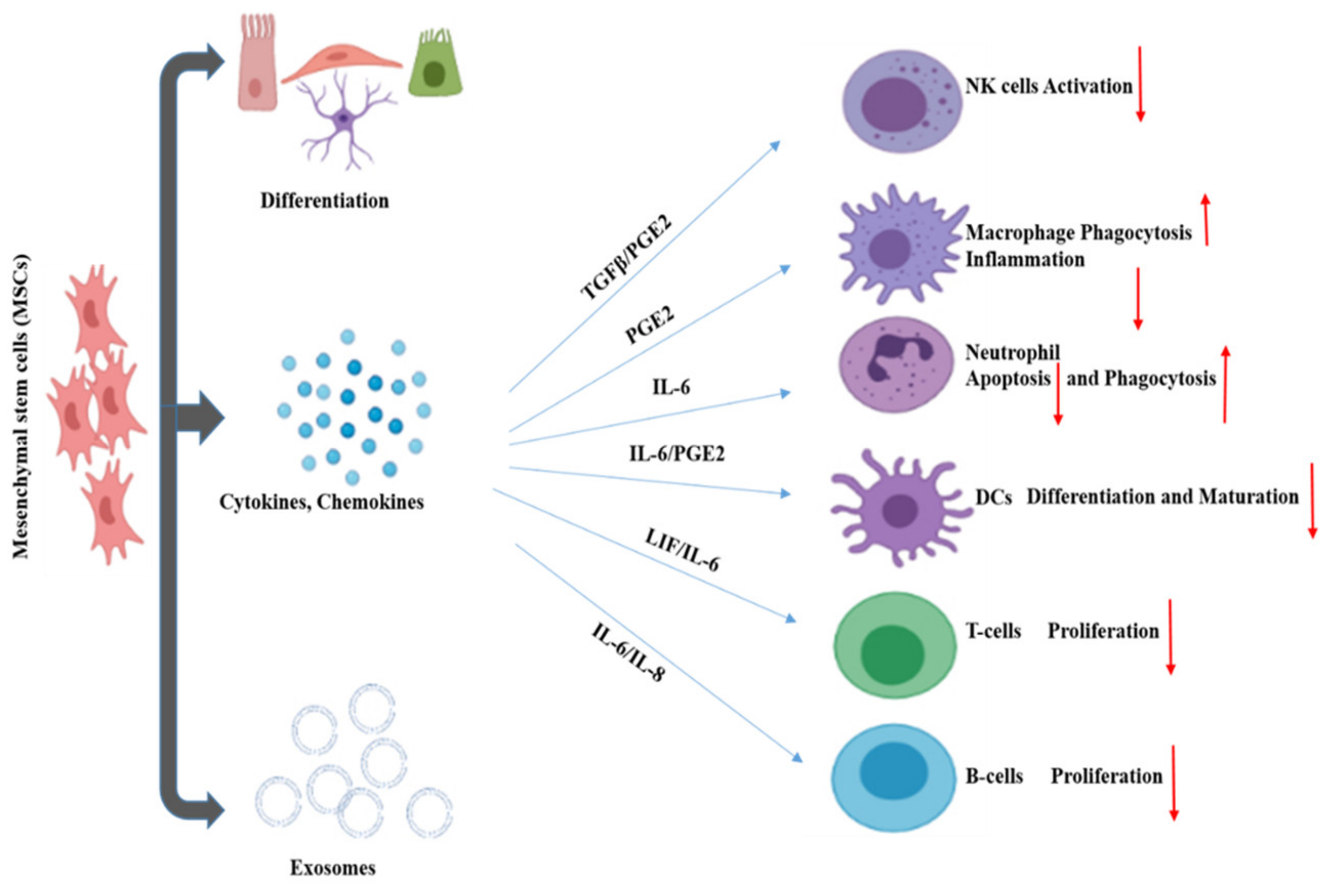
3.1. Immunomodulatory and Regenerative Effects of MSCs
3.2. Clinical Trials
4. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACE2 | Angiotensin-Converting Enzyme 2 |
| ACovCS | Acute COVID-19 Cardiovascular Syndrome |
| AKI | Acute Kidney Injury |
| ALT | Alanine Aminotransferase |
| ARDS | Acute Respiratory Distress Syndrome |
| AST | Aspartate Aminotransferase |
| BBB | Blood–brain barrier |
| BUN | Blood Urea Nitrogen |
| CD4 | Cluster of Differentiation 4 |
| CD8 | Cluster of Differentiation 8 |
| CKD | Chronic Kidney Disease |
| CNS | Central Nervous System |
| COVID-19 | Coronavirus Disease 2019 |
| DIC | Disseminated Intravascular Coagulation |
| FDA | Food and Drug Administration |
| FiO2 | Percentage of inspired oxygen |
| IFN-γ | Interferon Gamma |
| IL-1 | Interleukin 1 |
| IL-1RA | Interleukin Receptor type 1 |
| IL-6 | Interleukin 6 |
| IP-10 | Interferon Inducible Cytokine IP10 |
| MCP-1 | Monocyte Chemoattractant Protein 1 |
| MIP-1 | Macrophage Inflammatory Protein 1-α |
| MSCs | Mesenchymal Stem Cells |
| NK | Natural Killer |
| NRF2 | Nuclear factor erythroid 2-Related Factor 2 |
| PaO2 | Partial Pressure of arterial oxygen |
| PNS | Peripheral Nervous System |
| ROS | Reactive oxygen species |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome CoronaVirus 2 |
| TNF-α | Tumor Necrosis Factor-alpha |
References
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Bio Med. Atenei Parm. 2020, 91, 157. [Google Scholar]
- Roser, M.; Ritchie, H.; Ortiz-Ospina, E.; Hasell, J. Coronavirus Disease (COVID-19)–Statistics and Research. Our World Data. 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 24 October 2021).
- Mahase, E. Coronavirus: COVID-19 has killed more people than SARS and MERS combined, despite lower case fatality rate. BMJ 2020, 368, m641. [Google Scholar] [CrossRef] [Green Version]
- Tindale, L.C.; Stockdale, J.E.; Coombe, M.; Garlock, E.S.; Lau, W.Y.V.; Saraswat, M.; Zhang, L.; Chen, D.; Wallinga, J.; Colijn, C. Evidence for transmission of COVID-19 prior to symptom onset. eLife 2020, 9, e57149. [Google Scholar] [CrossRef]
- Li, G.; Li, W.; He, X.; Cao, Y. Asymptomatic and Presymptomatic Infectors: Hidden Sources of Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2018. [Google Scholar] [CrossRef]
- Weiss, P.; Murdoch, D.R. Clinical course and mortality risk of severe COVID-19. Lancet 2020, 395, 1014–1015. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Yang, L.; Liu, S.; Liu, J.; Zhang, Z.; Wan, X.; Huang, B.; Chen, Y.; Zhang, Y. COVID-19: Immunopathogenesis and Immunotherapeutics. Signal Transduct. Target. Ther. 2020, 5, 1–8. [Google Scholar] [CrossRef]
- Marshall, M. The lasting misery of coronavirus long-haulers. Nature 2020, 585, 339–341. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. Coronavirus Treatment Acceleration Program (CTAP). 2020. Available online: https://www.fda.gov/drugs/coronavirus (accessed on 15 October 2021).
- Golchin, A.; Seyedjafari, E.; Ardeshirylajimi, A. Mesenchymal stem cell therapy for COVID-19: Present or future. Stem Cell Rev. Rep. 2020, 16, 427–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, F.; Xu, R.; Wang, S.; Xu, Z.; Zhang, C.; Li, Y.; Yang, T.; Shi, L.; Fu, J.; Jiang, T.; et al. Human umbilical cord-derived mesenchymal stem cell therapy in patients with COVID-19: A phase 1 clinical trial. Signal Transduct. Target. Ther. 2020, 5, 172. [Google Scholar] [CrossRef] [PubMed]
- Zaim, S.; Chong, J.H.; Sankaranarayanan, V.; Harky, A. COVID-19 and multi-organ response. Curr. Probl. Cardiol. 2020. [Google Scholar] [CrossRef]
- Ge, X.Y.; Li, J.L.; Yang, X.L.; Chmura, A.A.; Zhu, G.; Epstein, J.H.; Mazet, J.K.; Hu, B.; Zhang, W.; Peng, C.; et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature 2013, 503, 535–538. [Google Scholar] [CrossRef]
- Zhang, H.; Penninger, J.M.; Li, Y.; Zhong, N.; Slutsky, A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020, 46, 586–590. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Zhao, Z.; Wang, Y.; Zhou, Y.; Ma, Y.; Zuo, W. Single-cell RNA expression profiling of ACE2, thereceptor of SARS-CoV-2. Biorxiv 2020. [Google Scholar] [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, M.L.; Lely, A.T.; Navis, G.V.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. A J. Pathol. Soc. Great Br. Irel. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.H. Hypothesis: Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may increase the risk of severe COVID-19. J. Travel Med. 2020, 27. [Google Scholar] [CrossRef] [Green Version]
- Perlman, S.; Netland, J. Coronaviruses post-SARS: Update on replication and pathogenesis. Nat. Rev. Microbiol. 2009, 7, 439–450. [Google Scholar] [CrossRef] [Green Version]
- Bernstein, K.E.; Khan, Z.; Giani, J.F.; Cao, D.Y.; Bernstein, E.A.; Shen, X.Z. Angiotensin-converting enzyme in innate and adaptive immunity. Nat. Rev. Nephrol. 2018, 14, 325. [Google Scholar] [CrossRef]
- Xu, J.; Zhong, S.; Liu, J.; Li, L.; Li, Y.; Wu, X.; Li, Z.; Deng, P.; Zhang, J.; Zhong, N.; et al. Detection of severe acute respiratory syndrome coronavirus in the brain: Potential role of the chemokine mig in pathogenesis. Clin. Infect. Dis. 2005, 41, 1089–1096. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.-T.; Shao, S.-C.; Hsu, C.-K.; Wu, I.-W.; Hung, M.-J.; Chen, Y.-C. Incidence of acute kidney injury in COVID-19 infection: A systematic review and meta-analysis. Crit. Care 2020, 24, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Chua, R.L.; Lukassen, S.; Trump, S.; Hennig, B.P.; Wendisch, D.; Pott, F.; Debnath, O.; Thürmann, L.; Kurth, F.; Völker, M.T.; et al. COVID-19 severity correlates with airway epithelium–immune cell interactions identified by single-cell analysis. Nat. Biotechnol. 2020, 38, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet (Lond. Engl.) 2020, 395, 1033. [Google Scholar] [CrossRef]
- Meduri, G.U.; Kohler, G.; Headley, S.; Tolley, E.; Stentz, F.; Postlethwaite, A. Inflammatory cytokines in the BAL of patients with ARDS: Persistent elevation over time predicts poor outcome. Chest 1995, 108, 1303–1314. [Google Scholar] [CrossRef]
- Yang, L.; Xie, X.; Tu, Z.; Fu, J.; Xu, D.; Zhou, Y. The signal pathways and treatment of cytokine storm in COVID-19. Signal Transduct. Target. Ther. 2021, 6, 255. [Google Scholar] [CrossRef]
- José, R.J.; Williams, A.E.; Chambers, R.C. Proteinase-activated receptors in fibroproliferative lung disease. Thorax 2014, 69, 190–192. [Google Scholar] [CrossRef] [Green Version]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef] [Green Version]
- Lippi, G.; Favaloro, E.J. D-dimer is associated with severity of coronavirus disease 2019: A pooled analysis. Thromb. Haemost. 2020, 120, 876. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Yan, X.; Fan, Q.; Liu, H.; Liu, X.; Liu, Z.; Zhang, Z. D-dimer levels on admission to predict in-hospital mortality in patients with COVID-19. J. Thromb. Haemost. 2020, 18, 1324–1329. [Google Scholar] [CrossRef] [PubMed]
- Antoniak, S.; Owens, A.P.; Baunacke, M.; Williams, J.C.; Lee, R.D.; Weithäuser, A.; Sheridan, P.A.; Malz, R.; Luyendyk, J.P.; Esserman, D.A.; et al. PAR-1 contributes to the innate immune response during viral infection. J. Clin. Investig. 2013, 123, 1310–1322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Maat, S.; De Mast, Q.; Jan Danser, A.H.; Van De Veerdonk, F.L.; Maas, C. Impaired Breakdown of Bradykinin and Its Metabolites as a Possible Cause for Pulmonary Edema in COVID-19 Infection. In Seminars in Thrombosis and Hemostasis; Thieme Medical Publishers: New York, NY, USA, 2020. [Google Scholar]
- Mercer, P.F.; Williams, A.E.; Scotton, C.J.; José, R.J.; Sulikowski, M.; Moffatt, J.D.; Murray, L.A.; Chambers, R.C. Proteinase-activated receptor-1, CCL2, and CCL7 regulate acute neutrophilic lung inflammation. Am. J. Respir. Cell Mol. Biol. 2014, 50, 144–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatia, M.; Zemans, R.L.; Jeyaseelan, S. Role of chemokines in the pathogenesis of acute lung injury. Am. J. Respir. Cell Mol. Biol. 2012, 46, 566–572. [Google Scholar] [CrossRef] [Green Version]
- Gao, T.; Hu, M.; Zhang, X.; Li, H.; Zhu, L.; Liu, H.; Dong, Q.; Zhang, Z.; Wang, Z.; Hu, Y.; et al. Highly pathogenic coronavirus N protein aggravates lung injury by MASP-2-mediated complement over-activation. MedRxiv 2020. [Google Scholar] [CrossRef]
- Chen, J.; Wang, X.; Zhang, S.; Liu, B.; Wu, X.; Wang, Y.; Wang, X.; Yang, M.; Sun, J.; Xie, Y. Characteristics of Acute Pulmonary Embolism in Patients with COVID-19 Associated Pneumonia from the City of Wuhan. Clin. Appl. Thromb./Hemost. 2020. [Google Scholar] [CrossRef] [PubMed]
- Hendren, N.S.; Drazner, M.H.; Bozkurt, B.; Cooper, L.T., Jr. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 2020, 141, 1903–1914. [Google Scholar] [CrossRef]
- Turner, A.J.; Hiscox, J.A.; Hooper, N.M. ACE2: From vasopeptidase to SARS virus receptor. Trends Pharmacol. Sci. 2004, 25, 291–294. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.-Y.; Ma, Y.-T.; Zhang, J.-Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [Green Version]
- Fremont-Smith, M.; Gherlone, N.; Smith, N.; Tisdall, P.; Ricke, D.O. Models for COVID-19 Early Cardiac Pathology Following SARS-CoV-2 Infection. Int. J. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Bradley, B.T.; Maioli, H.; Johnston, R.; Chaudhry, I.; Fink, S.L.; Xu, H.; Najafian, B.; Deutsch, G.; Lacy, J.M.; Williams, T.; et al. Histopathology and ultrastructural findings of fatal COVID-19 infections. Lancet 2020, 396, 320–332. [Google Scholar] [CrossRef]
- Abbas, A.M.; Fathy, S.K.; Fawzy, A.T.; Salem, A.S.; Shawky, M.S. The mutual effects of COVID-19 and obesity. Obes. Med. 2020, 19, 100250. [Google Scholar] [CrossRef]
- Nasi, M.; Patrizi, G.; Pizzi, C.; Landolfo, M.; Boriani, G.; Dei Cas, A.; Cicero, A.F.; Fogacci, F.; Rapezzi, C.; Sisca, G.; et al. The role of physical activity in individuals with cardiovascular risk factors: An opinion paper from Italian Society of Cardiology-Emilia Romagna-Marche and SIC-Sport. J. Cardiovasc. Med. (Hagerstown) 2019, 20, 631–639. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef]
- Li, Z.; Wu, M.; Yao, J.; Guo, J.; Liao, X.; Song, S.; Li, J.; Duan, G.; Zhou, Y.; Wu, X.; et al. Caution on kidney dysfunctions of 2019-nCoV patients. MedRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Naicker, S.; Yang, C.-W.; Hwang, S.-J.; Liu, B.-C.; Chen, J.-H.; Jha, V. The Novel Coronavirus 2019 epidemic and kidneys. Kidney Int. 2020, 97, 824–828. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Yang, M.; Wan, C.; Yi, L.X.; Tang, F.; Zhu, H.Y.; Yi, F.; Yang, H.C.; Fogo, A.B.; Nie, X.; et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020, 98, 219–227. [Google Scholar] [CrossRef]
- Zhang, Y.; Zheng, L.; Liu, L.; Zhao, M.; Xiao, J.; Zhao, Q. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int. 2020, 40, 2095–2103. [Google Scholar] [CrossRef] [Green Version]
- Bangash, M.N.; Patel, J.; Parekh, D. COVID-19 and the liver: Little cause for concern. Lancet Gastroenterol. Hepatol. 2020, 5, 529. [Google Scholar] [CrossRef] [Green Version]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.; et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Shi, L.; Wang, F.-S. Liver injury in COVID-19: Management and challenges. Lancet Gastroenterol. Hepatol. 2020, 5, 428–430. [Google Scholar] [CrossRef]
- Dorche, M.S.; Huot, P.; Osherov, M.; Wen, D.; Saveriano, A.; Giacomini, P.; Antel, J.P.; Mowla, A. Neurological complications of coronavirus infection; a comparative review and lessons learned during the COVID-19 pandemic. J. Neurol. Sci. 2020, 417, 117085. [Google Scholar] [CrossRef]
- Paterson, R.W.; Brown, R.L.; Benjamin, L.; Nortley, R.; Wiethoff, S.; Bharucha, T.; Jayaseelan, D.L.; Kumar, G.; Raftopoulos, R.E.; Zambreanu, L.; et al. The emerging spectrum of COVID-19 neurology: Clinical, radiological and laboratory findings. Brain 2020, 143, 3104–3120. [Google Scholar] [CrossRef]
- Varatharaj, A.; Thomas, N.; Ellul, M.; Davies, N.W.; Pollak, T.; Tenorio, E.L.; Sultan, M.; Easton, A.; Breen, G.; Zandi, M.; et al. UK-wide surveillance of neurological and neuropsychiatric complications of COVID-19: The first 153 patients. Lancet Psychiatry 2020, 7, 875–882. [Google Scholar] [CrossRef]
- Abdel-Mannan, O.; Eyre, M.; Löbel, U.; Bamford, A.; Eltze, C.; Hameed, B.; Hemingway, C.; Hacohen, Y. Neurologic and radiographic findings associated with COVID-19 infection in children. JAMA Neurol. 2020, 77, 1440–1445. [Google Scholar] [CrossRef] [PubMed]
- Virhammar, J.; Kumlien, E.; Fällmar, D.; Frithiof, R.; Jackmann, S.; Sköld, M.K.; Kadir, M.; Frick, J.; Lindeberg, J.; Olivero-Reinius, H.; et al. Acute necrotizing encephalopathy with SARS-CoV-2 RNA confirmed in cerebrospinal fluid. Neurology 2020, 95, 445–449. [Google Scholar] [CrossRef]
- Berger, J.R. COVID-19 and the nervous system. J. Neurovirology 2020, 26, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Blau, H.; Brazelton, T.; Weimann, J. The evolving concept of a stem cell: Entity or function? Cell 2001, 105, 829–841. [Google Scholar] [CrossRef] [Green Version]
- Lagasse, E.; Connors, H.; Al-Dhalimy, M.; Reitsma, M.; Dohse, M.; Osborne, L.; Wang, X.; Finegold, M.; Weissman, I.L.; Grompe, M. Purified hematopoietic stem cells can differentiate into hepatocytes in vivo. Nat. Med. 2000, 6, 1229–1234. [Google Scholar] [CrossRef]
- Tuan, R.S.; Boland, G.; Tuli, R. Adult mesenchymal stem cells and cell-based tissue engineering. Arthritis Res. Ther. 2002, 5, 1–14. [Google Scholar]
- Okita, K.; Ichisaka, T.; Yamanaka, S. Generation of germline-competent induced pluripotent stem cells. Nature 2007, 448, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; OuYang, Q.; Zhou, X.; Gu, Y.; Yuan, D.; Li, W.; Liu, G.; Liu, T.; Lu, G. A highly homozygous and parthenogenetic human embryonic stem cell line derived from a one-pronuclear oocyte following in vitro fertilization procedure. Cell Res. 2007, 17, 999–1007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, Q.; Ren, H.; Han, Z. Mesenchymal stem cells: Immunomodulatory capability and clinical potential in immune diseases. J. Cell. Immunother. 2016, 2, 3–20. [Google Scholar] [CrossRef] [Green Version]
- Leng, Z.; Zhu, R.; Hou, W.; Feng, Y.; Yang, Y.; Han, Q.; Shan, G.; Meng, F.; Du, D.; Wang, S.; et al. Transplantation of ACE2-mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020, 11, 216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ratajczak, M.Z.; Kucia, M.; Jadczyk, T.; Greco, N.J.; Wojakowski, W.; Tendera, M.; Ratajczak, J. Pivotal role of paracrine effects in stem cell therapies in regenerative medicine: Can we translate stem cell-secreted paracrine factors and microvesicles into better therapeutic strategies? Leukemia 2012, 26, 1166–1173. [Google Scholar] [CrossRef]
- Wagner, W.; Wein, F.; Seckinger, A.; Frankhauser, M.; Wirkner, U.; Krause, U.; Blake, J.; Schwager, C.; Eckstein, V.; Ansorge, W.; et al. Comparative characteristics of mesenchymal stem cells from human bone marrow, adipose tissue, and umbilical cord blood. Exp. Hematol. 2005, 33, 1402–1416. [Google Scholar] [CrossRef]
- Schmuck, E.G.; Koch, J.M.; Centanni, J.M.; Hacker, T.A.; Braun, R.K.; Eldridge, M.; Hei, D.J.; Hematti, P.; Raval, A.N. Biodistribution and clearance of human mesenchymal stem cells by quantitative three-dimensional cryo-imaging after intravenous infusion in a rat lung injury model. Stem Cells Transl. Med. 2016, 5, 1668–1675. [Google Scholar] [CrossRef] [Green Version]
- Prockop, D.J.; Oh, J.Y. Mesenchymal stem/stromal cells (MSCs): Role as guardians of inflammation. Mol. Ther. 2012, 20, 14–20. [Google Scholar] [CrossRef] [Green Version]
- Uccelli, A.; Pistoia, V.; Moretta, L. Mesenchymal stem cells: A new strategy for immunosuppression? Trends Immunol. 2007, 28, 219–226. [Google Scholar] [CrossRef]
- Cho, D.I.; Kim, M.R.; Jeong, H.Y.; Jeong, H.C.; Jeong, M.H.; Yoon, S.H.; Kim, Y.S.; Ahn, Y. Mesenchymal stem cells reciprocally regulate the M1/M2 balance in mouse bone marrow-derived macrophages. Exp. Mol. Med. 2014, 46, e70. [Google Scholar] [CrossRef]
- Salami, F.; Tavassoli, A.; Mehrzad, J.; Parham, A. Immunomodulatory effects of mesenchymal stem cells on leukocytes with emphasis on neutrophils. Immunobiology 2018, 223, 786–791. [Google Scholar] [CrossRef]
- Rasmusson, I. Immune modulation by mesenchymal stem cells. Exp. Cell Res. 2006, 312, 2169–2179. [Google Scholar] [CrossRef] [Green Version]
- Yi, T.; Song, S.U. Immunomodulatory properties of mesenchymal stem cells and their therapeutic applications. Arch. Pharmacal Res. 2012, 35, 213–221. [Google Scholar] [CrossRef]
- Blazquez, R.; Sanchez-Margallo, F.M.; de la Rosa, O.; Dalemans, W.; Álvarez, V.; Tarazona, R.; Casado, J.G. Immunomodulatory potential of human adipose mesenchymal stem cells derived exosomes on in vitro stimulated T cells. Front. Immunol. 2014, 5, 556. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pittenger, M.F.; Mackay, A.M.; Beck, S.C.; Jaiswal, R.K.; Douglas, R.; Mosca, J.D.; Moorman, M.A.; Simonetti, D.W.; Craig, S.; Marshak, D.R. Multilineage potential of adult human mesenchymal stem cells. Science 1999, 284, 143–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, L.; Huang, H.; Lu, X.; Yan, X.; Jiang, X.; Xu, R.; Wang, S.; Zhang, C.; Yuan, X.; Xu, Z.; et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: A randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct Target Ther. 2021, 6, 58. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Jia, Z. Cell-based therapy in lung regenerative medicine. Regen Med. Res. 2014, 2, 7. [Google Scholar] [CrossRef] [Green Version]
- Brasile, L.; Henry, N.; Orlando, G.; Stubenitsky, B. Potentiating Renal Regeneration Using Mesenchymal Stem Cells. Transplantation 2019, 103, 307–313. [Google Scholar] [CrossRef]
- Apostolou, K.G.; Papanikolaou, I.G.; Katselis, C.; Feretis, T.; Kletsas, D.; Konstadoulakis, M.M.; Lymperi, M.; Saetta, A.A.; Tsikalakis, S.; Agrogiannis, G.; et al. Undifferentiated Adipose Tissue Stem Cell Transplantation Promotes Hepatic Regeneration, Ameliorates Histopathologic Damage of the Liver, and Upregulates the Expression of Liver Regeneration- and Liver-Specific Genes in a Rat Model of Partial Hepatectomy. Stem Cells Int. 2018, 2018, 1393607. [Google Scholar] [CrossRef]
- Liu, S.; Xie, Y.Y.; Wang, L.D.; Tai, C.X.; Chen, D.; Mu, D.; Cui, Y.Y.; Wang, B. A multi-channel collagen scaffold loaded with neural stem cells for the repair of spinal cord injury. Neural Regen Res. 2021, 16, 2284–2292. [Google Scholar]
- A Phase I/II Safety and Tolerability Dose Escalation Study of Autologous Stem Cells to Patients with Liver Insufficiency. 2008. Available online: https://clinicaltrials.gov/ct2/show/results/NCT00655707 (accessed on 1 August 2021).
- Pietrosi, G.; Vizzini, G.; Gerlach, J.; Chinnici, C.; Luca, A.; Amico, G.; D’amato, M.; Conaldi, P.G.; Petri, S.L.; Spada, M.; et al. Phases I-II matched case-control study of human fetal liver cell transplantation for treatment of chronic liver disease. Cell Transplant. 2015, 24, 1627–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, F.; Ichim, T.E.; Pingle, S.; Jones, L.D.; Kesari, S.; Ashili, S. Mesenchymal stem cells as living anti-inflammatory therapy for COVID-19 related acute respiratory distress syndrome. World J. Stem Cells 2020, 12, 1067. [Google Scholar] [CrossRef] [PubMed]
- Mesenchymal Stem Cells Therapy in Patients with COVID-19 Pneumonia. NCT04713878. Available online: https://ClinicalTrials.gov/show/NCT04713878 (accessed on 15 October 2021).
- A Proof of Concept Study for the DNA Repair Driven by the Mesenchymal Stem Cells in Critical COVID-19 Patients. NCT04898088. Available online: https://ClinicalTrials.gov/show/NCT04898088 (accessed on 15 October 2021).
- A Clinical Trial to Determine the Safety and Efficacy of Hope Biosciences Autologous Mesenchymal Stem Cell Therapy (HB-adMSCs) to Provide Protection against COVID-19. NCT04349631. Available online: https://ClinicalTrials.gov/show/NCT04349631 (accessed on 15 October 2021).
- A Randomized, Double-Blind, Placebo-Controlled Clinical Trial to Determine the Safety and Efficacy of Hope Biosciences Allogeneic Mesenchymal Stem Cell Therapy (HB-adMSCs) to Provide Protection Against COVID-19. NCT04348435. Available online: https://ClinicalTrials.gov/show/NCT04348435 (accessed on 15 October 2021).
- Mesenchymal Stem Cells for the Treatment of COVID-19. NCT04573270. Available online: https://ClinicalTrials.gov/show/NCT04573270 (accessed on 15 October 2021).
- Treatment of COVID-19 Associated Pneumonia with Allogenic Pooled Olfactory Mucosa-Derived Mesenchymal Stem Cells. NCT04382547. Available online: https://ClinicalTrials.gov/show/NCT04382547 (accessed on 15 October 2021).
- Use of UC-MSCs for COVID-19 Patients. NCT04355728. Available online: https://ClinicalTrials.gov/show/NCT04355728 (accessed on 15 October 2021).
- An Exploratory Study of ADR-001 in Patients with Severe Pneumonia Caused by SARS-CoV-2 Infection. NCT04522986. Available online: https://ClinicalTrials.gov/show/NCT04522986 (accessed on 15 October 2021).
- Therapeutic Study to Evaluate the Safety and Efficacy of DW-MSC in COVID-19 Patients. NCT04535856. Available online: https://ClinicalTrials.gov/show/NCT04535856 (accessed on 15 October 2021).
- Extracellular Vesicle Infusion Treatment for COVID-19 Associated ARDS. NCT04493242. Available online: https://ClinicalTrials.gov/show/NCT04493242 (accessed on 15 October 2021).
- Raghav, A.; Khan, Z.A.; Upadhayay, V.K.; Tripathi, P.; Gautam, K.A.; Mishra, B.K.; Ahmad, J.; Jeong, G.B. Mesenchymal Stem Cell-Derived Exosomes Exhibit Promising Potential for Treating SARS-CoV-2-Infected Patients. Cells 2021, 10, 587. [Google Scholar] [CrossRef] [PubMed]
- Investigational Treatments for COVID-19 in Tertiary Care Hospital of Pakistan. NCT04492501. Available online: https://ClinicalTrials.gov/show/NCT04492501 (accessed on 15 October 2021).
- Clinical Use of Stem Cells for the Treatment of COVID-19. NCT04392778. Available online: https://ClinicalTrials.gov/show/NCT04392778 (accessed on 15 October 2021).
- Evaluation of Safety and Efficiency of Method of Exosome Inhalation in SARS-CoV-2 Associated Pneumonia. NCT04491240. Available online: https://ClinicalTrials.gov/show/NCT04491240 (accessed on 15 October 2021).
- Menstrual Blood Stem Cells in Severe COVID-19. NCT05019287. Available online: https://ClinicalTrials.gov/show/NCT05019287 (accessed on 15 October 2021).
- Cellular Immuno-Therapy for COVID-19 Acute Respiratory Distress Syndrome. NCT04400032. Available online: https://ClinicalTrials.gov/show/NCT04400032 (accessed on 15 October 2021).
- Shi, L.; Huang, H.; Lu, X.; Yan, X.; Jiang, X.; Xu, R.; Wang, S.; Zhang, C.; Yuan, X.; Xu, Z.; et al. Treatment with human umbilical cord-derived mesenchymal stem cells for COVID-19 patients with lung damage: A randomised, double-blind, placebo-controlled phase 2 trial. CellR4 Repair Replace Regen Reprogram 2020, 8, e2839. [Google Scholar]
- Safety and Efficacy of Mesenchy-Mal Stem Cells in the Manage-Ment of Severe COVID-19 Pneu-Monia; NCT04429763. NCT04429763. Available online: https://ClinicalTrials.gov/show/NCT04429763 (accessed on 15 October 2021).
- Novel Coronavirus Induced Severe Pneumonia Treated by Dental Pulp Mesenchymal Stem Cells. NCT04302519. Available online: https://ClinicalTrials.gov/show/NCT04302519 (accessed on 15 October 2021).
- NestaCell® Mesenchymal Stem Cell to Treat Patients with Severe COVID-19 Pneumonia. NCT04315987. Available online: https://ClinicalTrials.gov/show/NCT04315987 (accessed on 15 October 2021).
- Safety and Effectiveness of Mes-Enchymal Stem Cells in the Treatment of Pneumonia of Coro-Navirus Disease 2019. NCT04371601. Available online: https://ClinicalTrials.gov/show/NCT04371601 (accessed on 15 October 2021).
- Bone Marrow-Derived Mesen-Chymal Stem Cell Treatment for Severe Patients with Coronavirus Disease 2019 (COVID-19). NCT04346368. Available online: https://ClinicalTrials.gov/show/NCT04346368 (accessed on 15 October 2021).
- Use of Mesenchymal Stem Cells in Acute Respiratory Distress Syn-Drome Caused by COVID-19. NCT04456361. Available online: https://ClinicalTrials.gov/show/NCT04456361 (accessed on 15 October 2021).
- Study of Allogeneic Adi-Pose-Derived Mesenchymal Stem Cells for Treatment of COVID-19 Acute Respiratory Distress. NCT04905836. Available online: https://ClinicalTrials.gov/show/NCT04905836 (accessed on 15 October 2021).
- Efficacy of Infusions of MSC From Wharton Jelly in the SARS-CoV-2 (COVID-19) Related Acute Respir-Atory Distress Syndrome. NCT04625738. Available online: https://ClinicalTrials.gov/show/NCT04625738 (accessed on 15 October 2021).
- Study of Allogeneic Adi-Pose-Derived Mesenchymal Stem Cells to Treat Post COVID-19 “Long Haul” Pulmonary Com-Promise. NCT04992247. Available online: https://ClinicalTrials.gov/show/NCT04992247 (accessed on 15 October 2021).
- Study of Human Umbilical Cord Mesenchymal Stem Cells in the Treatment of Severe COVID-19. NCT04273646. Available online: https://ClinicalTrials.gov/show/NCT04273646 (accessed on 15 October 2021).
- Clinical Study for Subjects with COVID-19 Using Allogeneic Adi-Pose Tissue-Derived Mesenchy-Mal Stem Cells. NCT05017298. Available online: https://ClinicalTrials.gov/show/NCT05017298 (accessed on 15 October 2021).
- Expanded Access Protocol on Bone Marrow Mesenchymal Stem Cell Derived Extracellular Vesicle Infusion Treatment for Patients with COVID-19 Associated ARDS. NCT04657458. Available online: https://ClinicalTrials.gov/show/NCT04657458 (accessed on 15 October 2021).
- Clinical Trial to Assess the Safety and Efficacy of Intravenous Ad-ministration of Allogeneic Adult Mesenchymal Stem Cells of Ex-Panded Adipose Tissue in Pa-Tients with Severe Pneumonia Due to COVID-19. NCT04366323. Available online: https://ClinicalTrials.gov/show/NCT04366323 (accessed on 15 October 2021).
- Study to Evaluate the Efficacy and Safety of AstroStem-V in Treat-Ment of COVID-19 Pneumonia. NCT04527224. Available online: https://ClinicalTrials.gov/show/NCT04527224 (accessed on 15 October 2021).
- Autologous Adipose-Derived Stem Cells (AdMSCs) for COVID-19. NCT04428801. Available online: https://ClinicalTrials.gov/show/NCT04428801 (accessed on 15 October 2021).
- Adipose Mesenchymal Cells for Abatement of SARS-CoV-2 Res-piratory Compromise in COVID-19 Disease. NCT04352803. Available online: https://ClinicalTrials.gov/show/NCT04352803 (accessed on 15 October 2021).
- Umbilical Cord Tissue (UC) De-Rived Mesenchymal Stem Cells (MSCs) Versus Placebo to Treat Acute Pulmonary Inflammation Due to COVID-19. NCT04490486. Available online: https://ClinicalTrials.gov/show/NCT04490486 (accessed on 15 October 2021).
- Efficacy and Safety Study of Al-logeneic HB-adMSCs for the Treatment of COVID-19. NCT04362189. Available online: https://ClinicalTrials.gov/show/NCT04362189 (accessed on 15 October 2021).
- Study of Intravenous COVI-MSC for Treatment of COVID-19-Induced Acute Respir-atory Distress. NCT04903327. Available online: https://ClinicalTrials.gov/show/NCT04903327 (accessed on 15 October 2021).
- Mesenchymal Stem Cells (MSCs) in Inflammation-Resolution Pro-Grams of Coronavirus Disease 2019 (COVID-19) Induced Acute Respiratory Distress Syndrome (ARDS). NCT04377334. Available online: https://ClinicalTrials.gov/show/NCT04377334 (accessed on 15 October 2021).
- Study of the Safety of Therapeutic Tx with Immunomodulatory MSC in Adults with COVID-19 Infection Requiring Mechanical Venti-lation. NCT04397796. Available online: https://ClinicalTrials.gov/show/NCT04397796 (accessed on 15 October 2021).
- Use of hUC-MSC Product (BX-U001) for the Treatment of COVID-19 with ARDS. NCT04452097. Available online: https://ClinicalTrials.gov/show/NCT04452097 (accessed on 15 October 2021).
- The Use of Exosomes for the Treatment of Acute Respiratory Distress Syndrome or Novel Coronavirus Pneumonia Caused by COVID-19. NCT04798716. Available online: https://ClinicalTrials.gov/show/NCT04798716 (accessed on 15 October 2021).
- Safety and Feasibility of Allogenic MSC in the Treatment of COVID-19. NCT04467047. Available online: https://ClinicalTrials.gov/show/NCT04467047 (accessed on 15 October 2021).
- ACT-20 in Patients with Severe COVID-19 Pneumonia. NCT04398303. Available online: https://ClinicalTrials.gov/show/NCT04398303 (accessed on 15 October 2021).
- Gorman, E.; Shankar-Hari, M.; Hopkins, P.; Tunnicliffe, W.S.; Perkins, G.D.; Silversides, J.; McGuigan, P.; Jackson, C.; Boyle, R.; McFerran, J.; et al. Repair of Acute Respiratory Distress Syndrome by Stromal Cell Administration in COVID-19 (REALIST-COVID-19): A structured summary of a study protocol for a randomised, controlled trial. Trials 2020, 21, 462. [Google Scholar] [CrossRef]
- Safety and Efficiency of Method of Exosome Inhalation in COVID-19 Associated Pneumonia. NCT04602442. Available online: https://ClinicalTrials.gov/show/NCT04602442 (accessed on 15 October 2021).
- Mesenchymal Stromal Cell Ther-apy for The Treatment of Acute Respiratory Distress Syndrome. NCT04447833. Available online: https://ClinicalTrials.gov/show/NCT04447833 (accessed on 15 October 2021).
- MSCs in COVID-19 ARDS. NCT04371393. Available online: https://ClinicalTrials.gov/show/NCT04371393 (accessed on 15 October 2021).
- Cell Therapy Using Umbilical Cord-Derived Mesenchymal Stro-mal Cells in SARS-CoV-2-Related ARDS. NCT04333368. Available online: https://ClinicalTrials.gov/show/NCT04333368 (accessed on 15 October 2021).
- Stem Cell Educator Therapy Treat the Viral Inflammation in COVID-19. NCT04299152. Available online: https://ClinicalTrials.gov/show/NCT04299152 (accessed on 15 October 2021).
- Multiple Dosing of Mesenchymal Stromal Cells in Patients with ARDS (COVID-19). NCT04466098. Available online: https://ClinicalTrials.gov/show/NCT04466098 (accessed on 15 October 2021).
- Lanzoni, G.; Linetsky, E.; Correa, D.; Cayetano, S.M.; Marttos, A.C.; Alvarez, R.A.; Gil, A.A.; Poggioli, R.; Ruiz, P.; Hirani, K.; et al. Umbilical Cord Mesenchymal Stem Cells for COVID-19 ARDS: A Double Blind, Phase 1/2a, Randomized Controlled Trial. Stem Cells Transl. Med. 2021, 10, 660–673. [Google Scholar] [CrossRef]
- Sengupta, V.; Sengupta, S.; Lazo, A.; Woods, P.; Nolan, A.; Bremer, N. Exosomes Derived from Bone Marrow Mesenchymal Stem Cells as Treatment for Severe COVID-19. Stem Cells Dev. 2020, 29, 747–754. [Google Scholar] [CrossRef]
- Laforge, M.; Elbim, C.; Frère, C.; Hémadi, M.; Massaad, C.; Nuss, P.; Benoliel, J.J.; Becker, C. Tissue damage from neutrophil-induced oxidative stress in COVID-19. Nat. Rev. Immunol. 2020, 20, 515–516. [Google Scholar] [CrossRef]
- Qin, M.; Cao, Z.; Wen, J.; Yu, Q.; Liu, C.; Wang, F.; Zhang, J.; Yang, F.; Li, Y.; Fishbein, G.; et al. An Antioxidant Enzyme Therapeutic for COVID-19. Adv. Mater. 2020, 32, 2004901. [Google Scholar] [CrossRef]
- Jiang, W.; Tan, Y.; Cai, M.; Zhao, T.; Mao, F.; Zhang, X.; Xu, W.; Yan, Z.; Qian, H.; Yan, Y. Human umbilical cord MSC-derived exosomes suppress the development of CCl4-induced liver injury through antioxidant effect. Stem Cells Int. 2018, 2018, 6079642. [Google Scholar] [CrossRef] [Green Version]
- Stavely, R.; Nurgali, K. The emerging antioxidant paradigm of mesenchymal stem cell therapy. Stem Cells Transl. Med. 2020, 9, 985–1006. [Google Scholar] [CrossRef] [PubMed]
- Sivandzade, F.; Prasad, S.; Bhalerao, A.; Cucullo, L. NRF2 and NF-κB interplay in cerebrovascular and neurodegenerative disorders: Molecular mechanisms and possible therapeutic approaches. Redox Biol. 2019, 21, 101059. [Google Scholar] [CrossRef] [PubMed]
- Olagnier, D.; Farahani, E.; Thyrsted, J.; Blay-Cadanet, J.; Herengt, A.; Idorn, M.; Hait, A.; Hernaez, B.; Knudsen, A.; Iversen, M.B.; et al. SARS-CoV2-mediated suppression of NRF2-signaling reveals potent antiviral and anti-inflammatory activity of 4-octyl-itaconate and dimethyl fumarate. Nat. Commun. 2020, 11, 4938. [Google Scholar] [CrossRef] [PubMed]
| Title | Interventions | Location | URL (accessed on 15 October 2021) | |
|---|---|---|---|---|
| 1 | Mesenchymal Stem Cells Therapy in Patients With COVID-19 Pneumonia [88] | Other: Mesenchymal stem cells | Turkey | https://ClinicalTrials.gov/show/NCT04713878 |
| 2 | A Proof of Concept Study for the DNA Repair Driven by the Mesenchymal Stem Cells in Critical COVID-19 Patients [89] | Biological: Mesenchymal Stem Cells Transplantation | Turkey | https://ClinicalTrials.gov/show/NCT04898088 |
| 3 | Treatment With Human Umbilical Cord-derived Mesenchymal Stem Cells for Severe Corona Virus Disease 2019 (COVID-19) [80] | Biological: UC-MSCs|Biological: Saline containing 1% Human serum albuminï¼ solution without UC-MSCsï | China | https://ClinicalTrials.gov/show/NCT04288102 |
| 4 | A Clinical Trial to Determine the Safety and Efficacy of Hope Biosciences Autologous Mesenchymal Stem Cell Therapy (HB-adMSCs) to Provide Protection Against COVID-19 [90] | Biological: HB-adMSCs | United States | https://ClinicalTrials.gov/show/NCT04349631 |
| 5 | A Randomized, Double-Blind, Placebo-Controlled Clinical Trial to Determine the Safety and Efficacy of Hope Biosciences Allogeneic Mesenchymal Stem Cell Therapy (HB-adMSCs) to Provide Protection Against COVID-19 [91] | Biological: HB-adMSCs|Other: Placebos | United States | https://ClinicalTrials.gov/show/NCT04348435 |
| 6 | Mesenchymal Stem Cells for the Treatment of COVID-19 [92] | Biological: PrimePro|Other: Placebo | United States | https://ClinicalTrials.gov/show/NCT04573270 |
| 7 | Treatment of COVID-19 Associated Pneumonia With Allogenic Pooled Olfactory Mucosa-derived Mesenchymal Stem Cells [93] | Biological: Allogenic pooled olfactory mucosa-derived mesenchymal stem cells|Other: Standard treatment according to the Clinical protocols | Belarus | https://ClinicalTrials.gov/show/NCT04382547 |
| 8 | Use of UC-MSCs for COVID-19 Patients [94] | Biological: Umbilical Cord Mesenchymal Stem Cells + Heparin along with best supportive care.|Other: Vehicle + Heparin along with best supportive care | United States | https://ClinicalTrials.gov/show/NCT04355728 |
| 9 | An Exploratory Study of ADR-001 in Patients With Severe Pneumonia Caused by SARS-CoV-2 Infection [95] | Biological: Mesenchymal stem cell | Japan | https://ClinicalTrials.gov/show/NCT04522986 |
| 10 | Therapeutic Study to Evaluate the Safety and Efficacy of DW-MSC in COVID-19 Patients [96] | Drug: allogeneic mesenchymal stem cell|Other: Placebo | Indonesia | https://ClinicalTrials.gov/show/NCT04535856 |
| 11 | Extracellular Vesicle Infusion Treatment for COVID-19 Associated ARDS [97] | Biological: DB-001|Other: Intravenous normal saline | United States | https://ClinicalTrials.gov/show/NCT04493242 |
| 12 | A Pilot Clinical Study on Inhalation of Mesenchymal Stem Cells Exosomes Treating Severe Novel Coronavirus Pneumonia [98] | Biological: MSCs-derived exosomes | China | https://ClinicalTrials.gov/show/NCT04276987 |
| 13 | Investigational Treatments for COVID-19 in Tertiary Care Hospital of Pakistan [99] | Procedure: Therapeutic Plasma exchange|Biological: Convalescent Plasma|Drug: Tocilizumab|Drug: Remdesivir|Biological: Mesenchymal stem cell therapy | Pakistan | https://ClinicalTrials.gov/show/NCT04492501 |
| 14 | Clinical Use of Stem Cells for the Treatment of COVID-19 [100] | Biological: MSC Treatment|Biological: Saline Control | Turkey | https://ClinicalTrials.gov/show/NCT04392778 |
| 15 | Evaluation of Safety and Efficiency of Method of Exosome Inhalation in SARS-CoV-2 Associated Pneumonia [101] | Drug: EXO 1 inhalation|Drug: EXO 2 inhalation|Drug: Placebo inhalation | Russian Federation | https://ClinicalTrials.gov/show/NCT04491240 |
| 16 | Menstrual Blood Stem Cells in Severe COVID-19 [102] | Biological: Allogeneic human menstrual blood stem cells secretome|Other: Intravenous saline injection | Islamic Republic of Iran | https://ClinicalTrials.gov/show/NCT05019287 |
| 17 | Cellular Immuno-Therapy for COVID-19 Acute Respiratory Distress Syndrome [103] | Biological: Mesenchymal Stromal Cells | Canada | https://ClinicalTrials.gov/show/NCT04400032 |
| Title | Interventions | Locations | URL (accessed on 15 October 2021) | |
|---|---|---|---|---|
| 1 | Safety and Efficacy of Mesenchymal Stem Cells in the Management of Severe COVID-19 Pneumonia [105] | Biological: Umbilical cord-derived mesenchymal stem cells|Biological: Placebo | https://ClinicalTrials.gov/show/NCT04429763 | |
| 2 | Novel Coronavirus Induced Severe Pneumonia Treated by Dental Pulp Mesenchymal Stem Cells [106] | Biological: Dental pulp mesenchymal stem cells | https://ClinicalTrials.gov/show/NCT04302519 | |
| 3 | NestaCell® Mesenchymal Stem Cell to Treat Patients with Severe COVID-19 Pneumonia [107] | Biological: NestaCell®|Biological: Placebo | Brazil | https://ClinicalTrials.gov/show/NCT04315987 |
| 4 | Safety and Effectiveness of Mesenchymal Stem Cells in the Treatment of Pneumonia of Coronavirus Disease 2019 [108] | Drug: Oseltamivir|Drug: hormones|Device: oxygen therapy|Procedure: mesenchymal stem cells | China | https://ClinicalTrials.gov/show/NCT04371601 |
| 5 | Bone Marrow-Derived Mesenchymal Stem Cell Treatment for Severe Patients with Coronavirus Disease 2019 (COVID-19) [109] | Biological: BM-MSCs|Biological: Placebo | China | https://ClinicalTrials.gov/show/NCT04346368 |
| 6 | Use of Mesenchymal Stem Cells in Acute Respiratory Distress Syndrome Caused by COVID-19 [110] | Biological: Mesenchymal Stem Cells derived from Wharton Jelly of Umbilical cords | Mexico | https://ClinicalTrials.gov/show/NCT04456361 |
| 7 | Study of Allogeneic Adipose-Derived Mesenchymal Stem Cells for Treatment of COVID-19 Acute Respiratory Distress [111] | Biological: COVI-MSC|Drug: Placebo | https://ClinicalTrials.gov/show/NCT04905836 | |
| 8 | Efficacy of Infusions of MSC From Wharton Jelly in the SARS-CoV-2 (COVID-19) Related Acute Respiratory Distress Syndrome [112] | Biological: Ex vivo expanded Wharton’s Jelly Mesenchymal Stem Cells|Biological: Placebo | https://ClinicalTrials.gov/show/NCT04625738 | |
| 9 | Study of Allogeneic Adipose-Derived Mesenchymal Stem Cells to Treat Post COVID-19 “Long Haul” Pulmonary Compromise [113] | Biological: COVI-MSC|Biological: Placebo | https://ClinicalTrials.gov/show/NCT04992247 | |
| 10 | Study of Human Umbilical Cord Mesenchymal Stem Cells in the Treatment of Severe COVID-19 [114] | Biological: UC-MSCs|Drug: Placebo | China | https://ClinicalTrials.gov/show/NCT04273646 |
| 11 | Clinical Study for Subjects With COVID-19 Using Allogeneic Adipose Tissue-Derived Mesenchymal Stem Cells [115] | Biological: Autologous adipose-derived stem cells | https://ClinicalTrials.gov/show/NCT05017298 | |
| 12 | Expanded Access Protocol on Bone Marrow Mesenchymal Stem Cell Derived Extracellular Vesicle Infusion Treatment for Patients With COVID-19 Associated ARDS [116] | Biological: Bone Marrow Mesenchymal Stem Cell Derived Extracellular Vesicles Infusion Treatment | https://ClinicalTrials.gov/show/NCT04657458 | |
| 13 | Clinical Trial to Assess the Safety and Efficacy of Intravenous Administration of Allogeneic Adult Mesenchymal Stem Cells of Expanded Adipose Tissue in Patients with Severe Pneumonia Due to COVID-19 [117] | Drug: Allogeneic and Expanded Adipose Tissue-Derived Mesenchymal Stem Cells | Spain | https://ClinicalTrials.gov/show/NCT04366323 |
| 14 | Study to Evaluate the Efficacy and Safety of AstroStem-V in Treatment of COVID-19 Pneumonia [118] | Drug: AstroStem-V | https://ClinicalTrials.gov/show/NCT04527224 | |
| 15 | Autologous Adipose-derived Stem Cells (AdMSCs) for COVID-19 [119] | Biological: autologous adipose-derived stem cells | https://ClinicalTrials.gov/show/NCT04428801 | |
| 16 | Adipose Mesenchymal Cells for Abatement of SARS-CoV-2 Respiratory Compromise in COVID-19 Disease [120] | Biological: Autologous Adipose MSC’s | https://ClinicalTrials.gov/show/NCT04352803 | |
| 17 | Umbilical Cord Tissue (UC) Derived Mesenchymal Stem Cells (MSCs) Versus Placebo to Treat Acute Pulmonary Inflammation Due to COVID-19 [121] | Biological: UCMSCs|Other: Placebo | United States | https://ClinicalTrials.gov/show/NCT04490486 |
| 18 | Efficacy and Safety Study of Allogeneic HB-adMSCs for the Treatment of COVID-19 [122] | Biological: HB-adMSC|Other: Placebo | United States | https://ClinicalTrials.gov/show/NCT04362189 |
| 19 | Study of Intravenous COVI-MSC for Treatment of COVID-19-Induced Acute Respiratory Distress [123] | Biological: COVI-MSC|Drug: Placebo | https://ClinicalTrials.gov/show/NCT04903327 | |
| 20 | Mesenchymal Stem Cells (MSCs) in Inflammation-Resolution Programs of Coronavirus Disease 2019 (COVID-19) Induced Acute Respiratory Distress Syndrome (ARDS) [124] | Biological: MSC | Germany | https://ClinicalTrials.gov/show/NCT04377334 |
| 21 | Study of the Safety of Therapeutic Tx with Immunomodulatory MSC in Adults With COVID-19 Infection Requiring Mechanical Ventilation [125] | Biological: BM-Allo. MSC|Biological: Placebo | United States | https://ClinicalTrials.gov/show/NCT04397796 |
| 22 | Use of hUC-MSC Product (BX-U001) for the Treatment of COVID-19 With ARDS [126] | Biological: Human umbilical cord mesenchymal stem cells + best supportive care|Other: Placebo control + best supportive care | https://ClinicalTrials.gov/show/NCT04452097 | |
| 23 | The Use of Exosomes for the Treatment of Acute Respiratory Distress Syndrome or Novel Coronavirus Pneumonia Caused by COVID-19 [127] | Drug: MSC-exosomes delivered intravenously every other day on an escalating dose: (2:4:8)|Drug: MSC-exosomes delivered intravenously every other day on an escalating dose (8:4:8)|Drug: MSC-exosomes delivered intravenously every other day (8:8:8) | United States | https://ClinicalTrials.gov/show/NCT04798716 |
| 24 | Safety and Feasibility of Allogenic MSC in the Treatment of COVID-19 [128] | Biological: Mesenchymal Stromal Cells infusion | https://ClinicalTrials.gov/show/NCT04467047 | |
| 25 | ACT-20 in Patients with Severe COVID-19 Pneumonia [129] | Biological: ACT-20-MSC|Biological: ACT-20-CM|Biological: Placebo | https://ClinicalTrials.gov/show/NCT04398303 | |
| 26 | Repair of Acute Respiratory Distress Syndrome by Stromal Cell Administration (REALIST) (COVID-19) [130] | Biological: Human umbilical cord derived CD362 enriched MSCs|Biological: Placebo (Plasma-Lyte 148) | United Kingdom | https://ClinicalTrials.gov/show/NCT03042143 |
| 27 | Safety and Efficiency of Method of Exosome Inhalation in COVID-19 Associated Pneumonia [131] | Drug: EXO 1 inhalation|Drug: EXO 2 inhalation|Drug: Placebo inhalation | Russian Federation | https://ClinicalTrials.gov/show/NCT04602442 |
| 28 | Mesenchymal Stromal Cell Therapy for The Treatment of Acute Respiratory Distress Syndrome [132] | Drug: Mesenchymal Stromal Stem Cells-KI-MSC-PL-205 | Sweden | https://ClinicalTrials.gov/show/NCT04447833 |
| 29 | MSCs in COVID-19 ARDS [133] | Biological: Remestemcel-L|Drug: Placebo | United States | https://ClinicalTrials.gov/show/NCT04371393 |
| 30 | Cell Therapy Using Umbilical Cord-derived Mesenchymal Stromal Cells in SARS-CoV-2-related ARDS [134] | Biological: Umbilical cord Wharton’s jelly derived human|Other: NaCl 0.9% | France | https://ClinicalTrials.gov/show/NCT04333368 |
| 31 | Stem Cell Educator Therapy Treat the Viral Inflammation in COVID-19 [135] | Combination Product: Stem Cell Educator-Treated Mononuclear Cells Apheresis | https://ClinicalTrials.gov/show/NCT04299152 | |
| 32 | Multiple Dosing of Mesenchymal Stromal Cells in Patients with ARDS (COVID-19) [136] | Biological: Mesenchymal stromal cells|Other: Placebo | United States | https://ClinicalTrials.gov/show/NCT04466098 |
| Therapy | Side effects of therapy | Results | No. of Patients |
|---|---|---|---|
| Exosomes (ExoFlo)-allogeneic-bone marrow-derived-mesenchymal stem cells [138] | Hypoxic respiratory failure, pulmonary embolism, acute renal failure, and expiration. | Improved PaO2/FiO2 ratio. Substantial reduction in levels of the CRP, ferritin, acute phase reactants, and D-dimer. Reductions in neutrophil count. Increase in lymphocyte count, including subsets staining positive for CD3+, CD4+, CD8+. | 24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhalerao, A.; Raut, S.; Noorani, B.; Mancuso, S.; Cucullo, L. Molecular Mechanisms of Multi-Organ Failure in COVID-19 and Potential of Stem Cell Therapy. Cells 2021, 10, 2878. https://doi.org/10.3390/cells10112878
Bhalerao A, Raut S, Noorani B, Mancuso S, Cucullo L. Molecular Mechanisms of Multi-Organ Failure in COVID-19 and Potential of Stem Cell Therapy. Cells. 2021; 10(11):2878. https://doi.org/10.3390/cells10112878
Chicago/Turabian StyleBhalerao, Aditya, Snehal Raut, Behnam Noorani, Salvatore Mancuso, and Luca Cucullo. 2021. "Molecular Mechanisms of Multi-Organ Failure in COVID-19 and Potential of Stem Cell Therapy" Cells 10, no. 11: 2878. https://doi.org/10.3390/cells10112878
APA StyleBhalerao, A., Raut, S., Noorani, B., Mancuso, S., & Cucullo, L. (2021). Molecular Mechanisms of Multi-Organ Failure in COVID-19 and Potential of Stem Cell Therapy. Cells, 10(11), 2878. https://doi.org/10.3390/cells10112878







