Polymer Prosthetic Hand with Finger Copies for Persons with Congenital Defects or After Amputation Using 3D Printing Technology
Abstract
1. Introduction
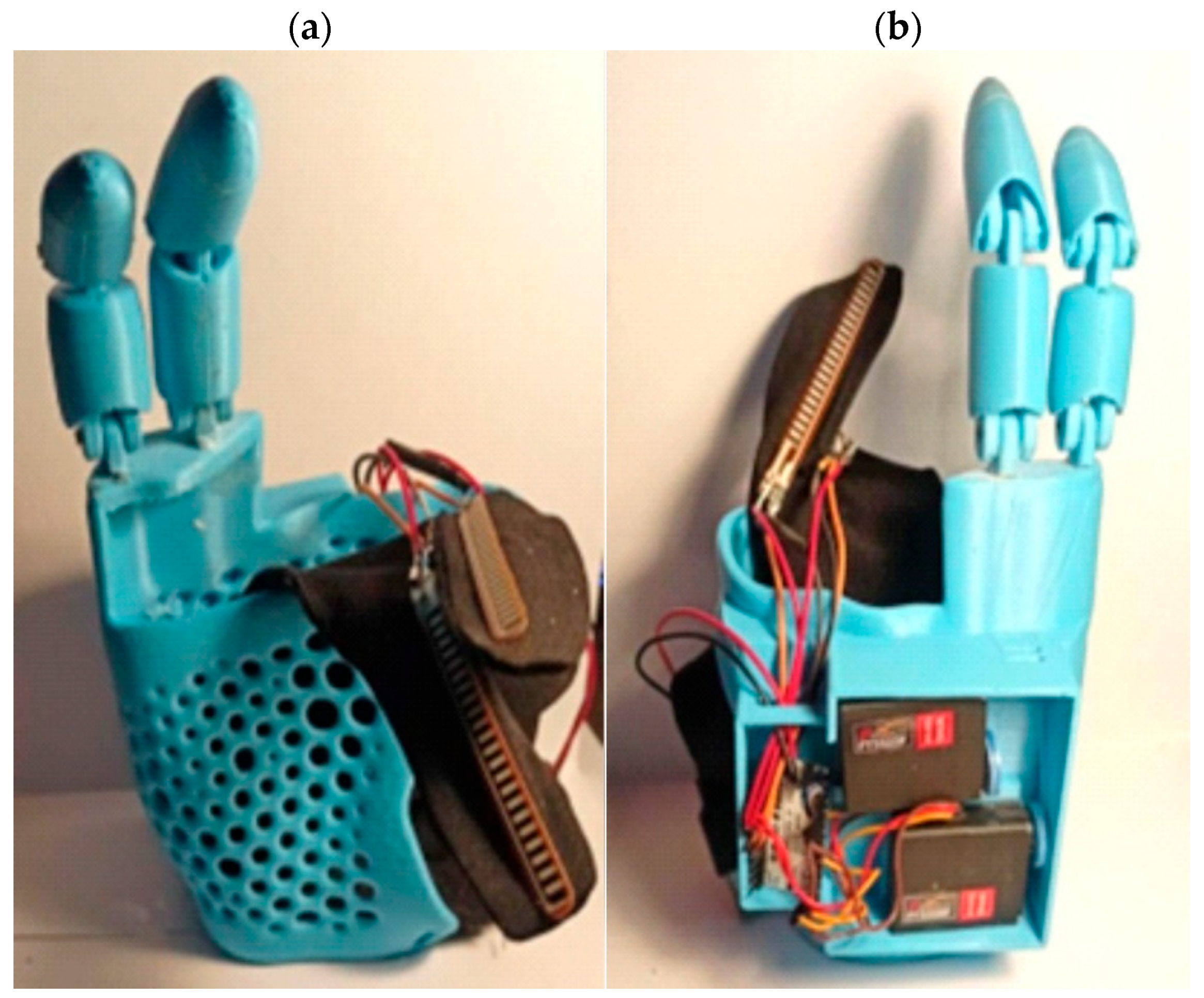
2. Materials and Methods
3. Results and Discussion
3.1. Conceptual Phase—Assessment of Potential Solutions
3.2. Three-Dimensional Scanning
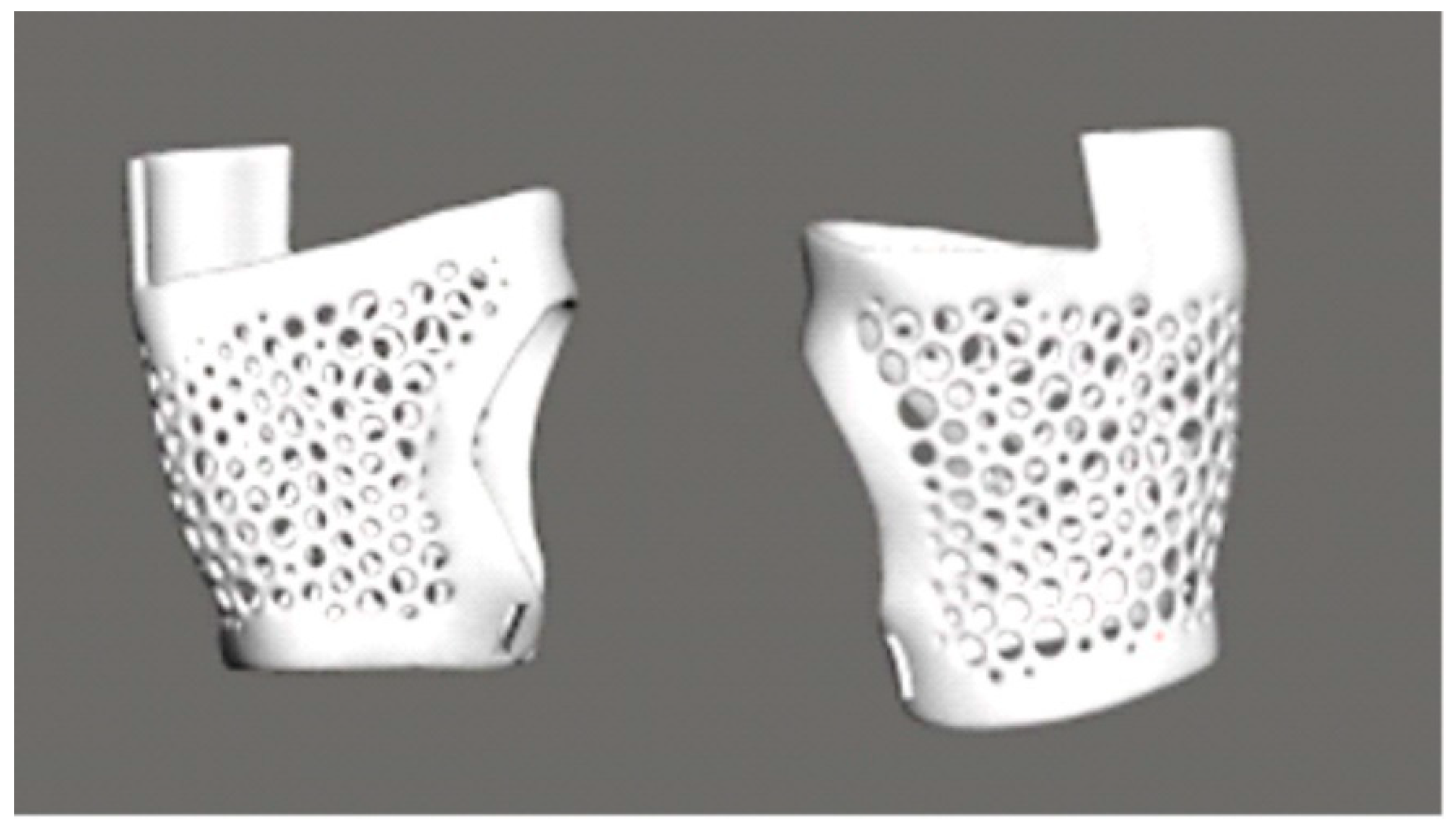
3.3. Design Using CAD Software
- –
- The creation of a base solid in the form of a cuboid with rounded edges is essential for the representation of the general cross-section and shape of the finger.
- –
- The initial step in the procedure is the division of the solid into segments corresponding to individual phalanges. This approach facilitates the subsequent planning of the bending mechanism.
- –
- The initial solid shape is modified through a series of processes involving cutting, rounding, and forming. These modifications are executed in a manner that emulates the technique of modelling from plasticine. The objective of this approach is to achieve a shape that is more natural and ergonomically designed.
- –
- The utilization of the symmetry function was instrumental in ensuring the uniformity of parameters on both sides of the finger. This approach led to a substantial augmentation in the design’s velocity and precision.
- –
- The process of cutting involves the creation of recesses, holes, and additional construction details.
- –
- The following text is intended to provide a comprehensive overview of the subject matter.
3.4. Selection of Material
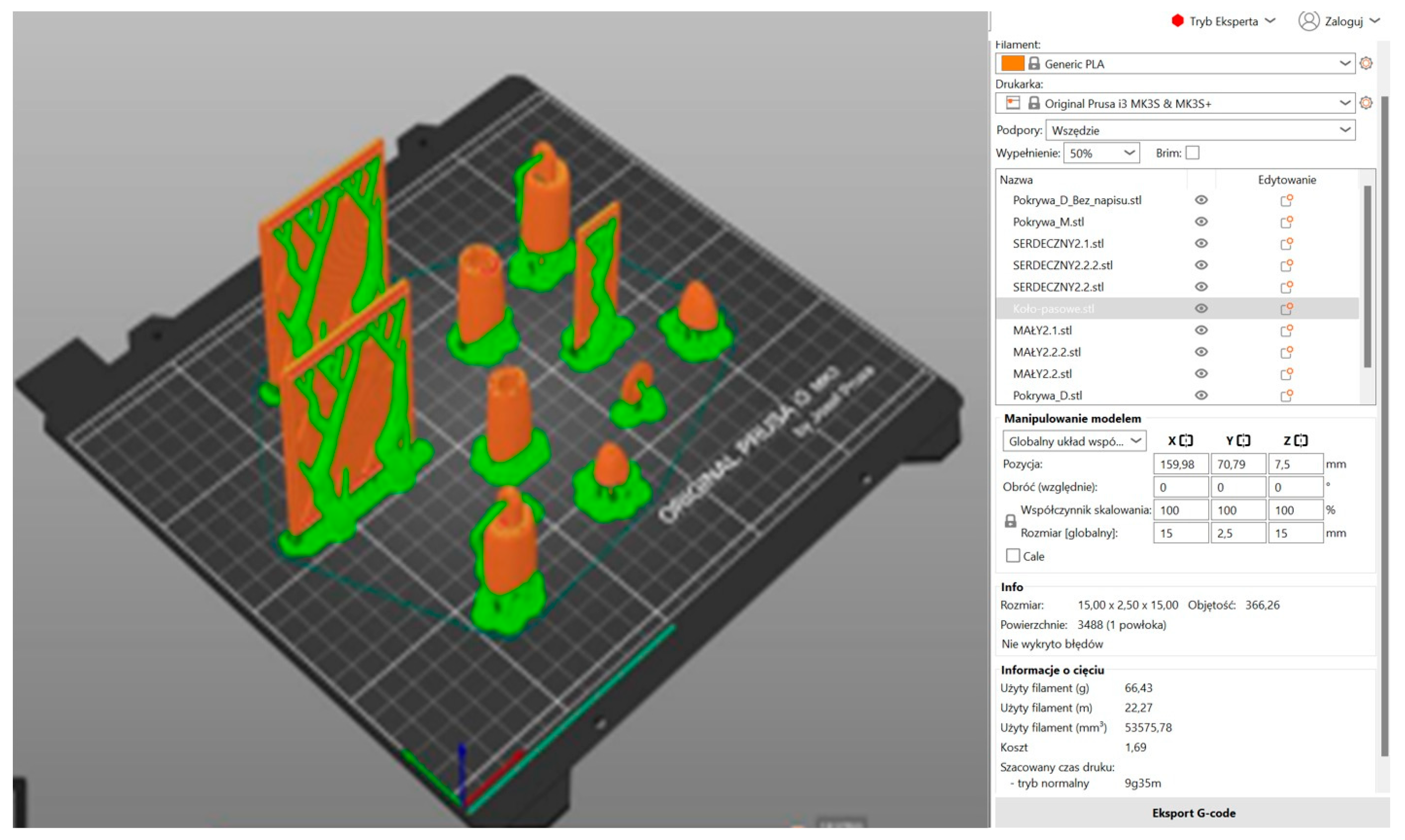
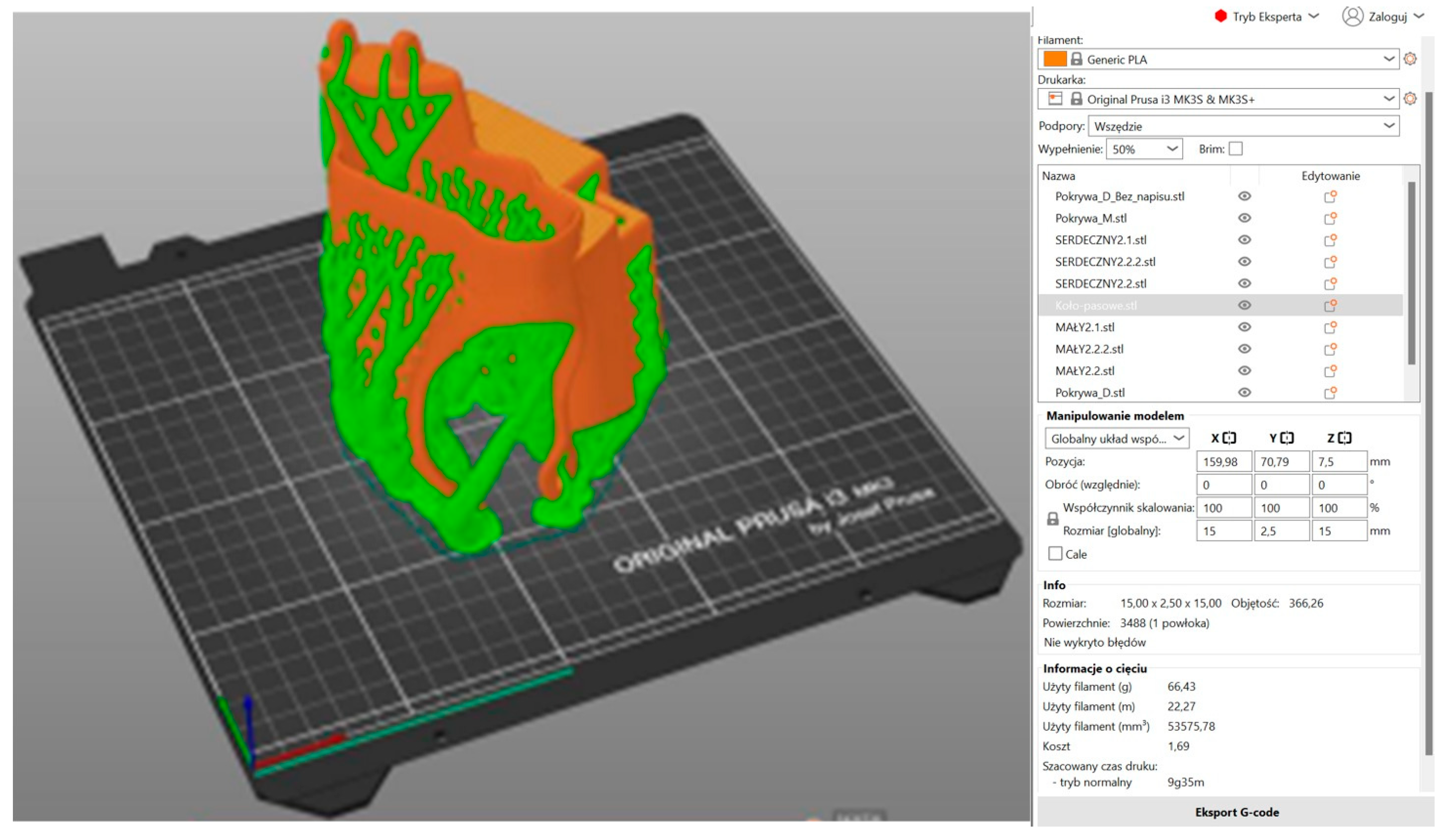
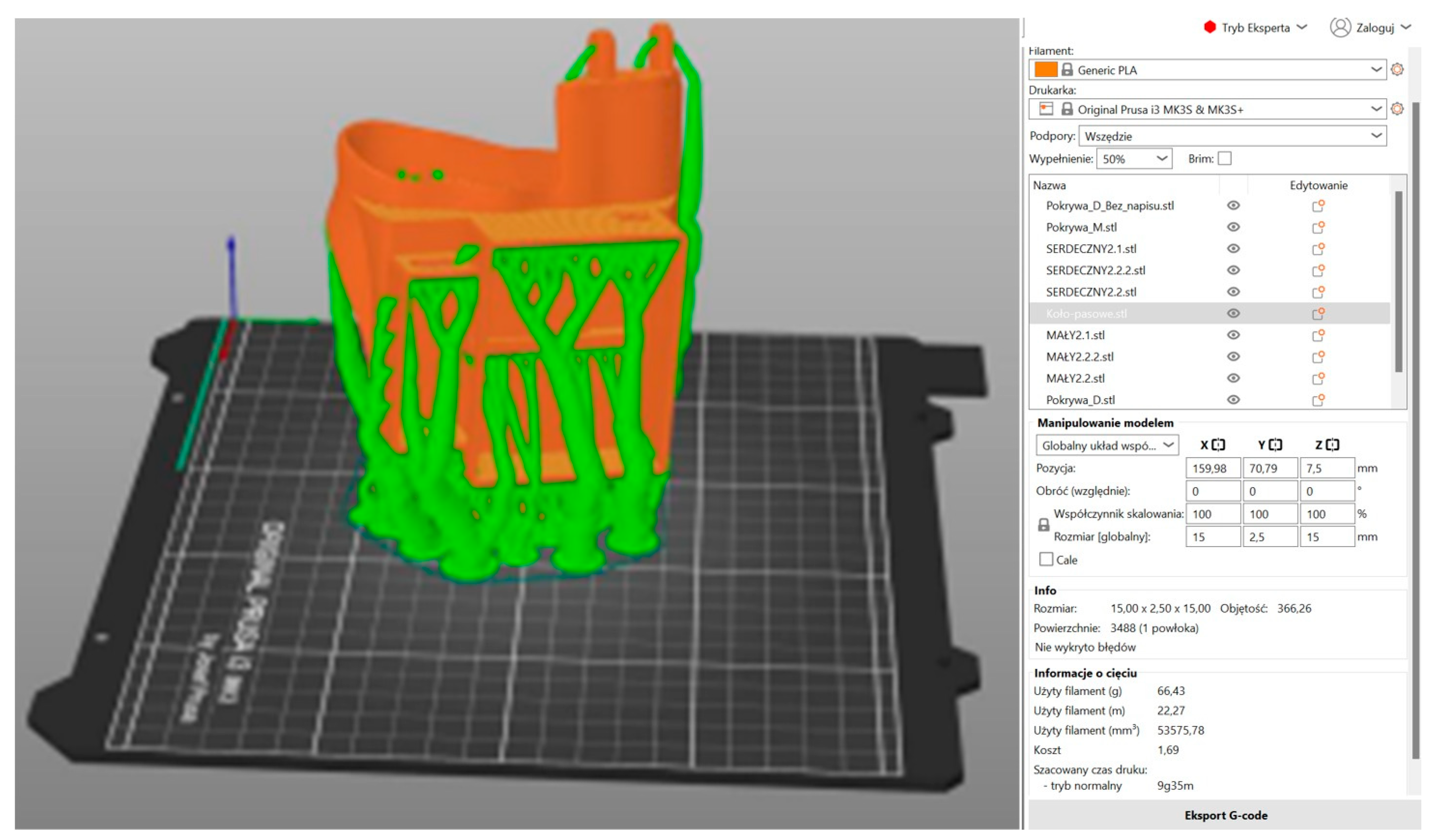
3.5. Three-Dimensional Printing
3.6. Design and Simulation of an Electronic Circuit
3.7. Assembly and Integration of the Electronic System into the Prosthesis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Jakubik, S.; Marianek, M.; Micuła, M.; Ociepka, A.; Osuch, J.; Painta, J.; Ryś, J.; Wieczorek, J.; Włodarczyk-Fligier, A.; Polok-Rubiniec, M.; et al. Comparison of selected materials used in the manufacture of upper limb prostheses. In Proceedings of the TalentDetector2025_Winter: International Students Scientific Conference, Gliwice, Poland, 31 January 2025; pp. 166–170. Available online: https://pimib.polsl.pl/pdf/Talent-Detector-2025-winter1.pdf (accessed on 28 April 2025).
- Berselli, G.; Vassura, G. Grasping the Future: Advances in Powered Upper Limb Prosthetics—Chapter 6. In Design Solutions and Methods for Robotic Hands that Can Help Prosthesis Hands Development; University of Bologna: Bologna, Italy, 2012; pp. 78–91. [Google Scholar] [CrossRef]
- Prostheses of Upper Limb. Available online: https://www.ortotomas.pl/produkty/protezy-konczyn-gornych (accessed on 28 April 2025).
- Young, K.J.; Pierce, J.E.; Zuniga, J.M. Assessment of body-powered 3D printed partial finger prostheses: A case study. 3D Print Med. 2019, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Salazar, M.; Portero, P.; Zambrano, M.; Rosero, R. Review of Robotic Prostheses Manufactured with 3D Printing: Advances, Challenges, and Future Perspectives. Appl. Sci. 2025, 15, 1350. [Google Scholar] [CrossRef]
- Rajczyk, P.; Bednarczyk, K. 3D Printing Technology for the Prototyping of Prosthesis Construction and Exoskeletons. In Research Reviews of Czestochowa University of Technology; Czestochowa University of Technology: Czestochowa, Poland, 2020; pp. 162–167. [Google Scholar] [CrossRef]
- Rismalia, M.; Hidajat, S.C.; Permana, I.G.R.; Hadisujoto, B.; Muslimin, M.; Triawan, F. Infill pattern and density effects on the tensile properties of 3D printed PLA material. J. Phys. Conf. 2019, 1402, 044041. [Google Scholar] [CrossRef]
- Abbady, H.E.M.A.; Klinkenberg, E.T.M.; de Moel, L.; Nicolai, N.; van der Stelt, M.; Verhulst, A.C.; Maal, T.J.J.; Brouwers, L. 3D-printed prostheses in developing countries: A systematic review. Int. Soc. Prosthet. Orthot. 2021, 46, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Dana, H.R.; Ebrahimi, F. Synthesis, properties, and applications of polylactic acid-based polymers. Polym. Eng. Sci. 2023, 63, 22–43. [Google Scholar] [CrossRef]
- Nagarajan, Y.R.; Farukh, F.; Kandan, K.; Singh, A.K.; Mukul, P. Assessing PET composite prosthetic solutions: A step towards inclusive healthcare. Heliyon 2024, 10, e38849. [Google Scholar] [CrossRef] [PubMed]
- Baharuddin, M.H.; Rashid, A.M.A.; Abdullah, N.N.A.A.; Ramlee, M.H. Patient-Specific Design of Prosthesis for Below Knee Amputee: Analysis Between Different Gait. Int. J. Integr. Eng. 2024, 16, 214–223. [Google Scholar] [CrossRef]
- Ghazali, N.; Romli, A.Z.; Ariff, T.F.T.M. Application of Silicone Elastomers in Extraoral Prosthesis: A Narrative Review. Compend. Oral Sci. 2025, 12, 20–39. [Google Scholar] [CrossRef]
- Ventimiglia, P.M. Design of a Human Hand Prosthesis. Bachelor Thesis, Worcester Polytechnic Institute, Worcester, MA, USA, 2012. Available online: https://www.academia.edu/65261008/Design_of_a_Human_Hand_Prosthesis (accessed on 28 April 2025).
- Carey, S.L.; Lura, D.J.; Highsmith, M.J. Differences in myoelectric and body-powered upper-limb prostheses: Systematic literature review. J. Prosthet. Orthot. (JPO) 2015, 52, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Simon, M. Programming Arduino: Getting Started with Sketches, 3rd ed.; McGraw-Hill: Columbus, OH, USA, 2022. [Google Scholar]
- Borowski, G.; Jankowska, A.; Paśnikowska, M. Using parameterization of objects in autodesk inventor in designing structural connectors. Adv. Sci. Technol. Res. J. 2015, 9, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Borthakur, P.P. The Role and Future Directions of 3D Printing in Custom Prosthetic Design. Eng. Proc. 2024, 81, 10. [Google Scholar] [CrossRef]
- Kopar, M.; Yildiz, A.R. Experimentral investigation of mechanical properties of PLA, ABS and PETG 3D printing materials using fused deposition modeling technique. Mater. Test. 2023, 65, 1795–1804. [Google Scholar] [CrossRef]
- Mehmood, A.; Raina, N.; Phakeenuya, V.; Wonganu, B.; Cheenkachorn, K. The current status and market trend of polylactic acid as biopolymer: Awareness and needs for sustainable development. Mater. Today Proc. 2023, 72, 3049–3055. [Google Scholar] [CrossRef]
- Smith, M.; Love, D.C.; Rochman, C.M.; Neff, R.A. Microplastics in Seafood and the Implications for Human Health. Curr. Environ. Health Rep. 2018, 5, 375–386. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Kan, S.M.; Shafiq, M.; Abbas, M. A review on PLA-based biodegradable materials for biomedical applications. Giant 2024, 18, 100261. [Google Scholar] [CrossRef]
- Ruśkowski, P.; Gadomska-Gajadhur, A. Polylactide in medical applications. Polym. Mater. 2017, 2, 32–35. [Google Scholar]
- Farah, S.; Anderson, D.G.; Langer, R. Physical and mechanical properties of PLA, and their functions in widespread applications—A comprehensive review. Adv. Drug Deliv. Rev. 2016, 107, 367–392. [Google Scholar] [CrossRef] [PubMed]
- Parida, P.K.; Biswal, B.B. Desing and Analysis of a Multifingered Robot Hand. Int. J. Robot. Autom. 2012, 1, 69–77. [Google Scholar] [CrossRef]
- Siegel, J.R.; Harwood, J.K.; Lau, A.C.; Brenneis, D.J.A.; Dawson, M.R.; Pilarski, P.M.; Schofield, J.S. A performance evaluation of commercially available and 3D-printable prosthetic hands: A comparison using the anthropomorphic hand assessment protocol. BMC Biomed. Eng. 2024, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Liu, H.; Wang, K.; Qian, Z.; Ren, L.; Ren, L. Comparative Study of Robotic Artificial Actuators and Biological Muscle. Adv. Mech. Eng. 2020, 12, 1687814020933409. [Google Scholar] [CrossRef]
- da Silva, A.B.S.; Mendes, G.E.P.; Bragato, E.S.; Novelli, G.L.; Monjardim, M.; Andrade, R.M. Finger Prosthesis Driven by DEA Pairs as Agonist–Antagonist Artificial Muscles. Biomimetics 2024, 9, 110. [Google Scholar] [CrossRef] [PubMed]






Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Włodarczyk-Fligier, A.; Polok-Rubiniec, M.; Kania, A.; Jakubik, S.; Painta, J.; Ryś, J.; Wieczorek, J.; Marianek, M.; Ociepka, A.; Micuła, M.; et al. Polymer Prosthetic Hand with Finger Copies for Persons with Congenital Defects or After Amputation Using 3D Printing Technology. Polymers 2025, 17, 1983. https://doi.org/10.3390/polym17141983
Włodarczyk-Fligier A, Polok-Rubiniec M, Kania A, Jakubik S, Painta J, Ryś J, Wieczorek J, Marianek M, Ociepka A, Micuła M, et al. Polymer Prosthetic Hand with Finger Copies for Persons with Congenital Defects or After Amputation Using 3D Printing Technology. Polymers. 2025; 17(14):1983. https://doi.org/10.3390/polym17141983
Chicago/Turabian StyleWłodarczyk-Fligier, Anna, Magdalena Polok-Rubiniec, Aneta Kania, Sebastian Jakubik, Jakub Painta, Justyna Ryś, Jakub Wieczorek, Marta Marianek, Agata Ociepka, Mikołaj Micuła, and et al. 2025. "Polymer Prosthetic Hand with Finger Copies for Persons with Congenital Defects or After Amputation Using 3D Printing Technology" Polymers 17, no. 14: 1983. https://doi.org/10.3390/polym17141983
APA StyleWłodarczyk-Fligier, A., Polok-Rubiniec, M., Kania, A., Jakubik, S., Painta, J., Ryś, J., Wieczorek, J., Marianek, M., Ociepka, A., Micuła, M., & Osuch, J. (2025). Polymer Prosthetic Hand with Finger Copies for Persons with Congenital Defects or After Amputation Using 3D Printing Technology. Polymers, 17(14), 1983. https://doi.org/10.3390/polym17141983





