Sol-Gel Derived Gelatin–Bioactive Glass Nanocomposite Biomaterials Incorporating Calcium Chloride and Calcium Ethoxide
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Sol-Gel Derived Gelatin-BG-MWCNT Nanocomposites Using Calcium Chloride and Calcium Ethoxide
2.3. Characterization of Nanocomposites
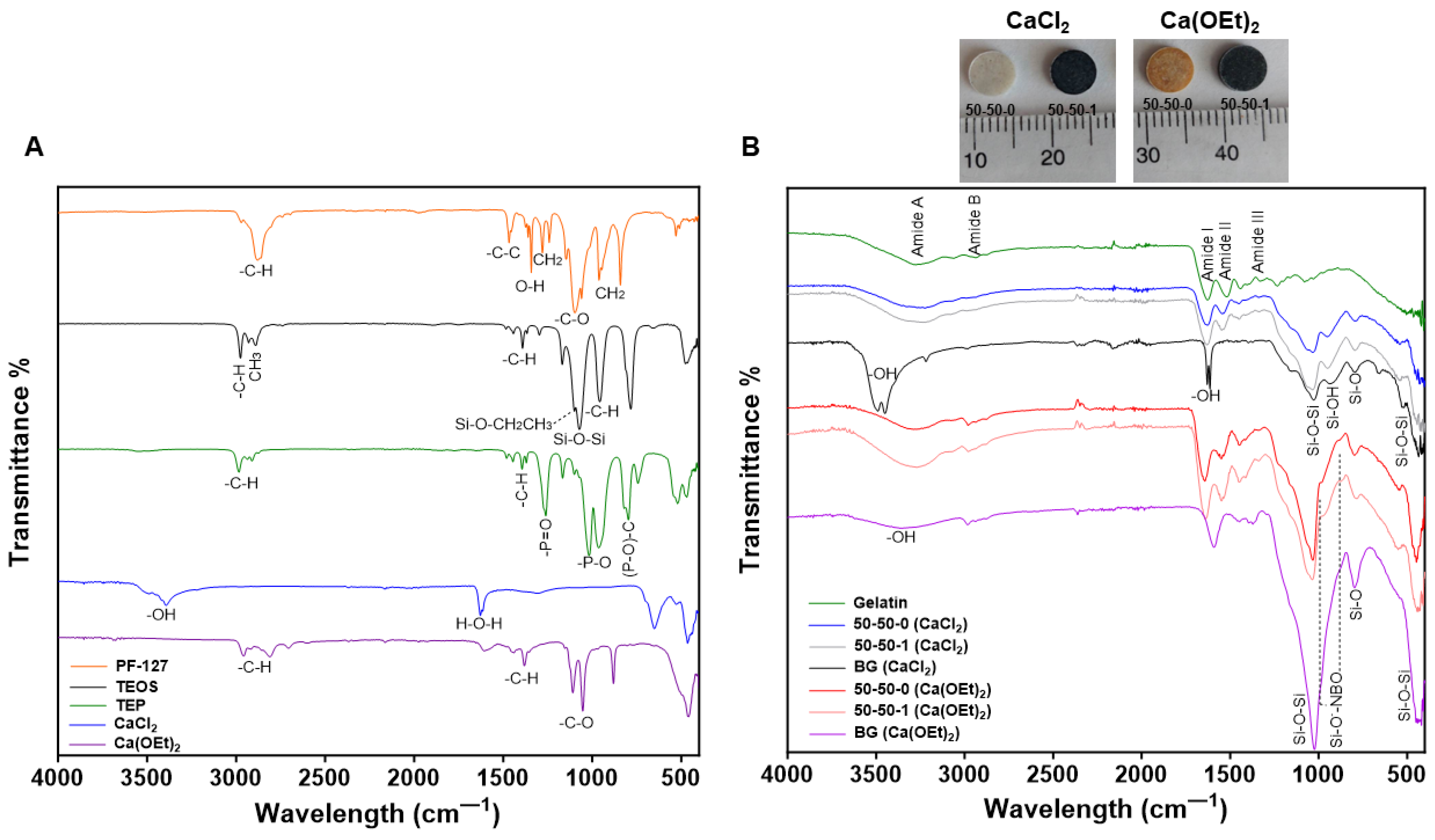
2.3.1. Attenuated Total Reflectance Fourier Transform Infrared Spectroscopy (ATR-FTIR)
2.3.2. Scanning Electron Microscopy (SEM) and Energy Dispersive X-ray Spectroscopy (EDX) Analysis
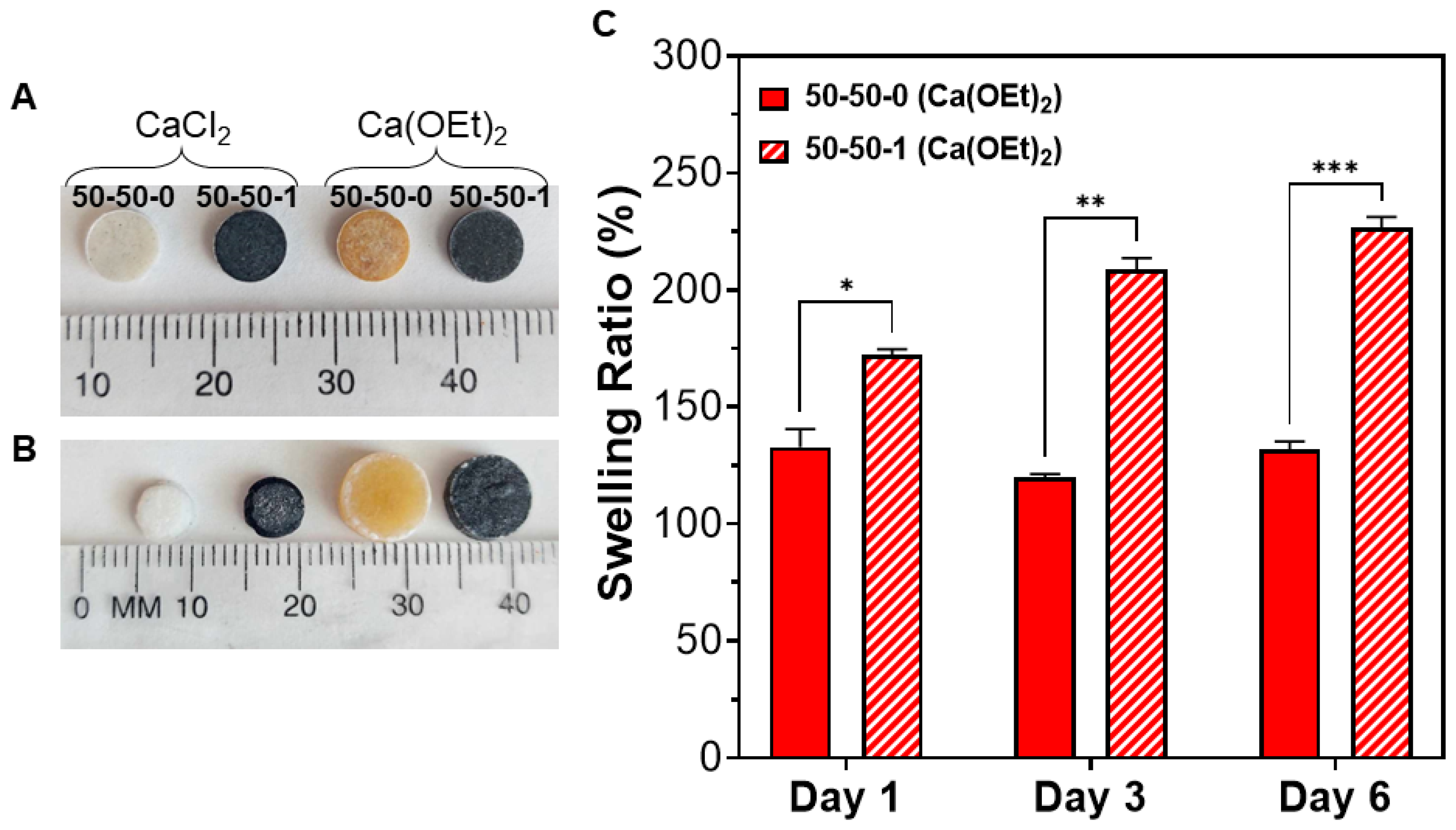
2.3.3. Swelling Behavior of CaCl2- and Ca(OEt)2-Based Nanocomposites
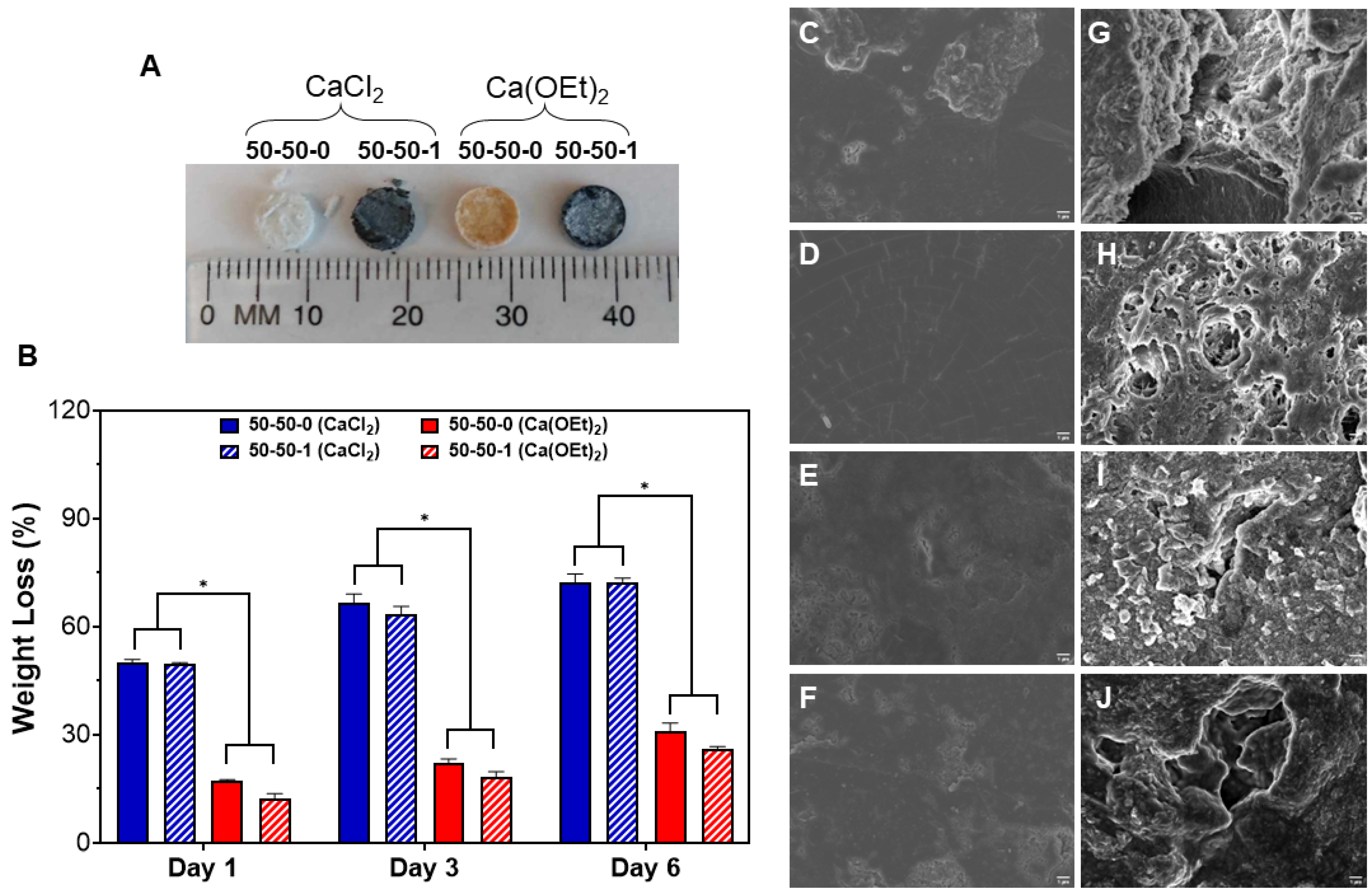
2.3.4. In Vitro Biodegradability of CaCl2- and Ca(OEt)2-Based Nanocomposites
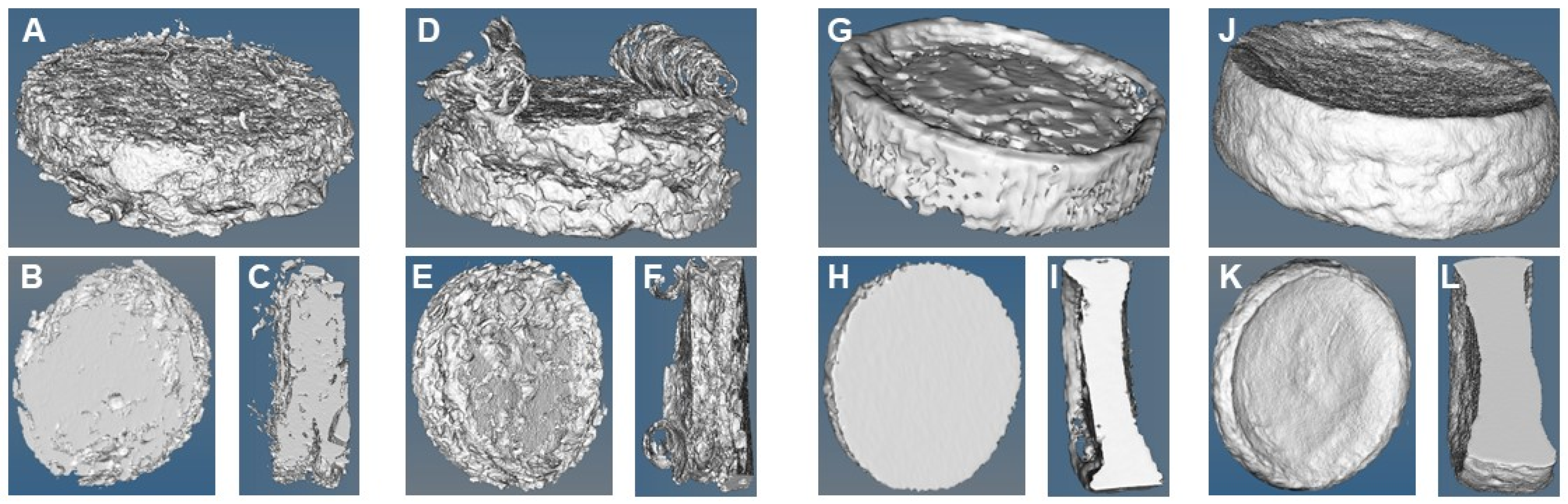
2.3.5. Micro-CT imaging of CaCl2- and Ca(OEt)2-Based Nanocomposites Post-Degradation
2.3.6. In Vitro Bioactivity of CaCl2- and Ca(OEt)2-Based Nanocomposites
2.3.7. Cell Adhesion and Viability of CaCl2- and Ca(OEt)2-Based Nanocomposites
2.3.8. Statistical Analysis
3. Results and Discussion
3.1. Preparation of Gelatin-BG-MWCNT Nanocomposites from CaCl2- and Ca(OEt)2 Calcium Sources
3.2. Surface Morphological and Elemental Distribution of 50-50-1 Nanocomposites Prepared from CaCl2- and Ca(OEt)2 Sources
3.3. Swelling Behavior of Nanocomposites Composed of CaCl2- and Ca(OEt)2 Calcium Sources
3.4. In Vitro Biodegradation Study of CaCl2- and Ca(OEt)2-Based Nanocomposites
3.5. Microstructure, Pore Size and Porosity of CaCl2- and Ca(OEt)2-Based Nanocomposites
3.6. In Vitro Bioactivity of CaCl2- and Ca(OEt)2-Based 50-50-0 and 50-50-1 Nanocomposites
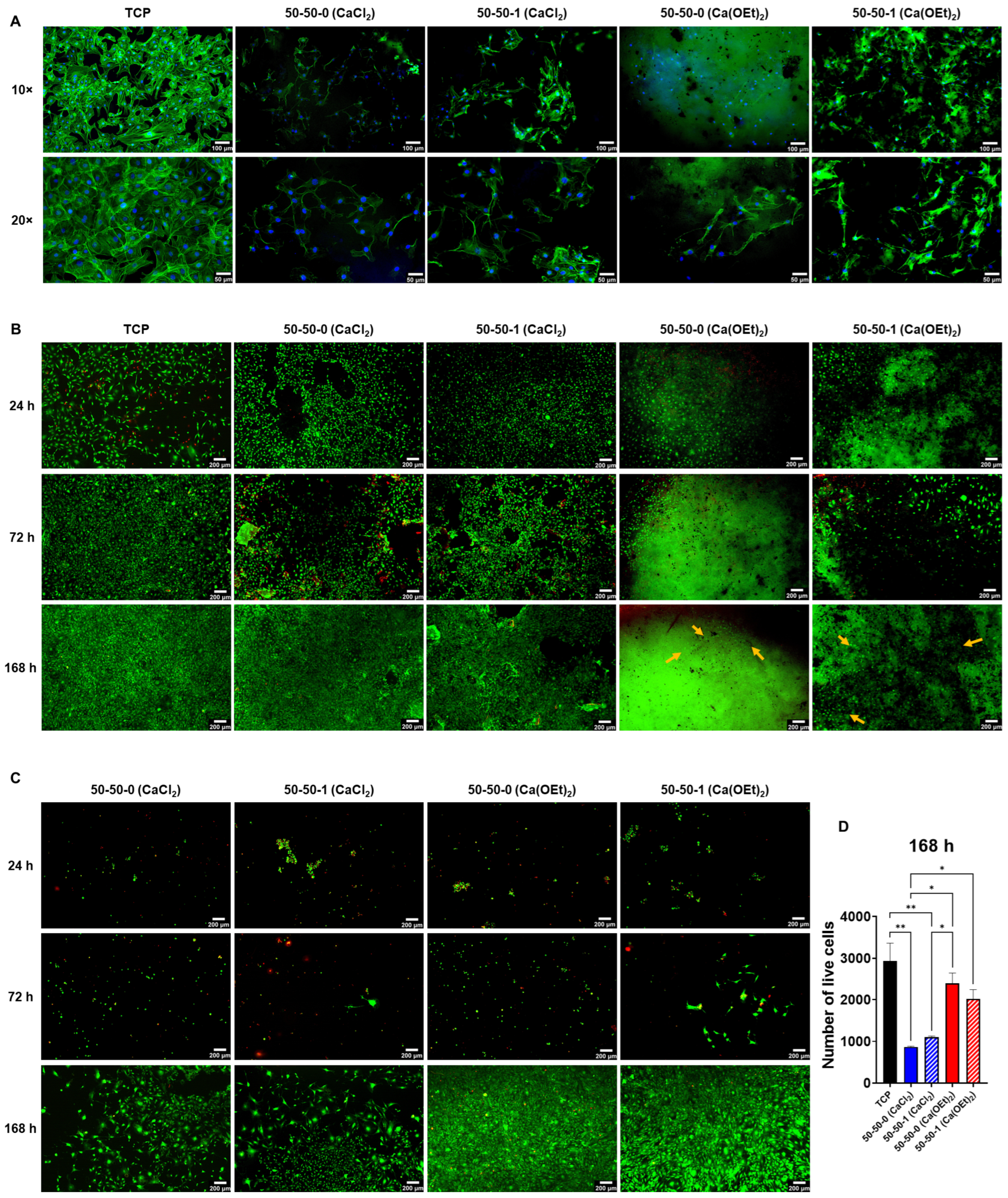
3.7. Mouse Embryo Multipotent Mesenchymal Progenitor 10T1/2 Cell Adhesion, Spreading and Viability on CaCl2- and Ca(OEt)2-Based Nanocomposites
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Aslankoohi, N.; Mequanint, K. Poly(ester amide)–Bioactive Glass Hybrid Biomaterials for Bone Regeneration and Biomolecule Delivery. ACS Appl. Bio Mater. 2020, 3, 3621–3630. [Google Scholar] [CrossRef] [PubMed]
- Mondal, D.; Lin, S.; Rizkalla, A.S.; Mequanint, K. Porous and biodegradable polycaprolactone-borophosphosilicate hybrid scaffolds for osteoblast infiltration and stem cell differentiation. J. Mech. Behav. Biomed. Mater. 2019, 92, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Tallia, F.; Ting, H.-K.; Page, S.J.; Clark, J.P.; Li, S.; Sang, T.; Russo, L.; Stevens, M.M.; Hanna, J.V.; Jones, J.R. Bioactive, Degradable and Tough Hybrids Through Calcium and Phosphate Incorporation. Front. Mater. 2022, 9, 901196. [Google Scholar] [CrossRef]
- Hench, L.L. Bioceramics. J. Am. Ceram. Soc. 2005, 81, 1705–1728. [Google Scholar] [CrossRef]
- Aslankoohi, N.; Lin, S.; Mequanint, K. Bioactive fluorescent hybrid microparticles as a stand-alone osteogenic differentiation inducer. Mater. Today Bio 2022, 13, 100187. [Google Scholar] [CrossRef]
- Jones, J.R.; Lin, S.; Yue, S.; Lee, P.D.; Hanna, J.V.; Smith, M.E.; Newport, R.J. Bioactive glass scaffolds for bone regeneration and their hierarchical characterisation. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2010, 224, 1373–1387. [Google Scholar] [CrossRef] [PubMed]
- Hench, L.L.; Splinter, R.J.; Allen, W.C.; Greenlee, T.K. Bonding mechanisms at the interface of ceramic prosthetic materials. J. Biomed. Mater. Res. 1971, 5, 117–141. [Google Scholar] [CrossRef]
- Jones, J.R.; Gentleman, E.; Polak, J. Bioactive Glass Scaffolds for Bone Regeneration. Elements 2007, 3, 393–399. [Google Scholar] [CrossRef]
- Hench, L.L.; West, J.K. The sol-gel process. Chem. Rev. 1990, 90, 33–72. [Google Scholar] [CrossRef]
- Aslankoohi, N.; Mondal, D.; Rizkalla, A.S.; Mequanint, K. Bone Repair and Regenerative Biomaterials: Towards Recapitulating the Microenvironment. Polymers 2019, 11, 1437. [Google Scholar] [CrossRef]
- Sakuma, W.; Yamasaki, S.; Fujisawa, S.; Kodama, T.; Shiomi, J.; Kanamori, K.; Saito, T. Mechanically Strong, Scalable, Mesoporous Xerogels of Nanocellulose Featuring Light Permeability, Thermal Insulation, and Flame Self-Extinction. ACS Nano 2021, 15, 1436–1444. [Google Scholar] [CrossRef] [PubMed]
- Ksouri, D.; Khireddine, H.; Aksas, A.; Valente, T.; Bir, F.; Slimani, N.; Cabal, B.; Torrecillas, R.; Santos, J.D. Synthesis of ternary bioactive glass derived aerogel and xerogel: Study of their structure and bioactivity. Nova Biotechnol. Chim. 2018, 17, 150–159. [Google Scholar] [CrossRef]
- Pérez-Moreno, A.; Piñero, M.; Fernández-Montesinos, R.; Pinaglia-Tobaruela, G.; Reyes-Peces, M.V.; Mesa-Díaz, M.D.M.; Vilches-Pérez, J.I.; Esquivias, L.; De La Rosa-Fox, N.; Salido, M. Chitosan-Silica Hybrid Biomaterials for Bone Tissue Engineering: A Comparative Study of Xerogels and Aerogels. Gels 2023, 9, 383. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Clark, A.E.; Hench, L.L. An investigation of bioactive glass powders by sol-gel processing. J. Appl. Biomater. 1991, 2, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Sepulveda, P.; Jones, J.R.; Hench, L.L. Characterization of melt-derived 45S5 and sol-gel-derived 58S bioactive glasses. J. Biomed. Mater. Res. 2001, 58, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Sepulveda, P.; Jones, J.R.; Hench, L.L. In vitro dissolution of melt-derived 45S5 and sol-gel derived 58S bioactive glasses. J. Biomed. Mater. Res. 2002, 61, 301–311. [Google Scholar] [CrossRef] [PubMed]
- Aslankoohi, N.; Mequanint, K. Intrinsically fluorescent bioactive glass-poly(ester amide) hybrid microparticles for dual drug delivery and bone repair. Mater. Sci. Eng. C 2021, 128, 112288. [Google Scholar] [CrossRef]
- Allo, B.A.; Rizkalla, A.S.; Mequanint, K. Hydroxyapatite Formation on Sol–Gel Derived Poly(ε-Caprolactone)/Bioactive Glass Hybrid Biomaterials. ACS Appl. Mater. Interfaces 2012, 4, 3148–3156. [Google Scholar] [CrossRef]
- Ryu, J.-H.; Kwon, J.-S.; Kim, K.-M.; Hong, H.J.; Koh, W.-G.; Lee, J.; Lee, H.-J.; Choi, H.-J.; Yi, S.; Shin, H.; et al. Synergistic Effect of Porous Hydroxyapatite Scaffolds Combined with Bioactive Glass/Poly(lactic-co-glycolic acid) Composite Fibers Promotes Osteogenic Activity and Bioactivity. ACS Omega 2019, 4, 2302–2310. [Google Scholar] [CrossRef]
- Prokopowicz, M.; Szewczyk, A.; Sawicki, W. Bioactive monolithic composites of silica/polydimethylsiloxane/calcium phosphate obtained at room temperature in sol–gel micromolding technique. Mater. Lett. 2016, 184, 239–242. [Google Scholar] [CrossRef]
- Ghassemi, T.; Shahroodi, A.; Ebrahimzadeh, M.H.; Mousavian, A.; Movaffagh, J.; Moradi, A. Current Concepts in Scaffolding for Bone Tissue Engineering. Arch. Bone Jt. Surg. 2018, 6, 10. [Google Scholar]
- Pires, P.C.; Mascarenhas-Melo, F.; Pedrosa, K.; Lopes, D.; Lopes, J.; Macário-Soares, A.; Peixoto, D.; Giram, P.S.; Veiga, F.; Paiva-Santos, A.C. Polymer-based biomaterials for pharmaceutical and biomedical applications: A focus on topical drug administration. Eur. Polym. J. 2023, 187, 111868. [Google Scholar] [CrossRef]
- Pérez-Moreno, A.; Reyes-Peces, M.V.; Vilches-Pérez, J.I.; Fernández-Montesinos, R.; Pinaglia-Tobaruela, G.; Salido, M.; De La Rosa-Fox, N.; Piñero, M. Effect of Washing Treatment on the Textural Properties and Bioactivity of Silica/Chitosan/TCP Xerogels for Bone Regeneration. Int. J. Mol. Sci. 2021, 22, 8321. [Google Scholar] [CrossRef] [PubMed]
- Gorgieva, S.; Kokol, V. Collagen- vs. Gelatine-Based Biomaterials and Their Biocompatibility: Review and Perspectives. In Biomaterials Applications for Nanomedicine; Pignatello, R., Ed.; InTechOpen: Rijeka, Croatia, 2011; ISBN 978-953-307-661-4. [Google Scholar]
- Gao, C.; Gao, Q.; Li, Y.; Rahaman, M.N.; Teramoto, A.; Abe, K. In vitro evaluation of electrospun gelatin-bioactive glass hybrid scaffolds for bone regeneration. J. Appl. Polym. Sci. 2013, 127, 2588–2599. [Google Scholar] [CrossRef]
- Thomas, A.; Bera, J. Preparation and characterization of gelatin-bioactive glass ceramic scaffolds for bone tissue engineering. J. Biomater. Sci. Polym. Ed. 2019, 30, 561–579. [Google Scholar] [CrossRef] [PubMed]
- Echave, M.C.; Sánchez, P.; Pedraz, J.L.; Orive, G. Progress of gelatin-based 3D approaches for bone regeneration. J. Drug Deliv. Sci. Technol. 2017, 42, 63–74. [Google Scholar] [CrossRef]
- Arambula-Maldonado, R.; Liu, Y.; Xing, M.; Mequanint, K. Bioactive and electrically conductive GelMA-BG-MWCNT nanocomposite hydrogel bone biomaterials. Biomater. Adv. 2023, 154, 213616. [Google Scholar] [CrossRef] [PubMed]
- Dieudonné, X.; Montouillout, V.; Jallot, É.; Fayon, F.; Lao, J. Bioactive glass hybrids: A simple route towards the gelatin–SiO 2 –CaO system. Chem. Commun. 2014, 50, 8701. [Google Scholar] [CrossRef]
- Yu, B.; Turdean-Ionescu, C.A.; Martin, R.A.; Newport, R.J.; Hanna, J.V.; Smith, M.E.; Jones, J.R. Effect of Calcium Source on Structure and Properties of Sol–Gel Derived Bioactive Glasses. Langmuir 2012, 28, 17465–17476. [Google Scholar] [CrossRef]
- Bossard, C.; Granel, H.; Jallot, É.; Montouillout, V.; Fayon, F.; Soulié, J.; Drouet, C.; Wittrant, Y.; Lao, J. Mechanism of Calcium Incorporation Inside Sol–Gel Silicate Bioactive Glass and the Advantage of Using Ca(OH) 2 over Other Calcium Sources. ACS Biomater. Sci. Eng. 2019, 5, 5906–5915. [Google Scholar] [CrossRef]
- Yu, B.; Poologasundarampillai, G.; Turdean-Ionescu, C.; Smith, M.E.; Jones, J.R. A New Calcium Source for Bioactive Sol-Gel Hybrids. Bioceram. Dev. Appl. 2011, 1, 1–3. [Google Scholar] [CrossRef]
- Ben-Arfa, B.A.E.; Palamá, I.E.; Miranda Salvado, I.M.; Ferreira, J.M.F.; Pullar, R.C. The role of calcium (source & content) on the in vitro behaviour of sol–gel quaternary glass series. Ceram. Int. 2020, 46, 1065–1075. [Google Scholar] [CrossRef]
- Lin, S.; Ionescu, C.; Baker, S.; Smith, M.E.; Jones, J.R. Characterisation of the inhomogeneity of sol–gel-derived SiO2–CaO bioactive glass and a strategy for its improvement. J. Sol-Gel Sci. Technol. 2010, 53, 255–262. [Google Scholar] [CrossRef]
- Rámila, A.; Balas, F.; Vallet-Regí, M. Synthesis Routes for Bioactive Sol−Gel Glasses: Alkoxides versus Nitrates. Chem. Mater. 2002, 14, 542–548. [Google Scholar] [CrossRef]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Clavijo, A.; Hurt, A.; Kotha, A.; Coleman, N. Effect of Calcium Precursor on the Bioactivity and Biocompatibility of Sol-Gel-Derived Glasses. J. Funct. Biomater. 2019, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Shokri, S.; Movahedi, B.; Rafieinia, M.; Salehi, H. A new approach to fabrication of Cs/BG/CNT nanocomposite scaffold towards bone tissue engineering and evaluation of its properties. Appl. Surf. Sci. 2015, 357, 1758–1764. [Google Scholar] [CrossRef]
- Fukada, E.; Yasuda, I. On the Piezoelectric Effect of Bone. J. Phys. Soc. Jpn. 1957, 12, 1158–1162. [Google Scholar] [CrossRef]
- Yasuda, I. The classic: Fundamental aspects of fracture treatment. J. Kyoto Med. Soc. 1953, 4, 395–406, reprinted in Clin. Orthop. Relat. Res. 1977, 124, 5–8. [Google Scholar] [CrossRef]
- Balmer, T.W.; Vesztergom, S.; Broekmann, P.; Stahel, A.; Büchler, P. Characterization of the electrical conductivity of bone and its correlation to osseous structure. Sci. Rep. 2018, 8, 8601. [Google Scholar] [CrossRef]
- Arambula-Maldonado, R.; Mequanint, K. Carbon-based electrically conductive materials for bone repair and regeneration. Mater. Adv. 2022, 3, 5186–5206. [Google Scholar] [CrossRef]
- E Silva, E.P.; Huang, B.; Helaehil, J.V.; Nalesso, P.R.L.; Bagne, L.; de Oliveira, M.A.; Albiazetti, G.C.C.; Aldalbahi, A.; El-Newehy, M.; Santamaria, M., Jr.; et al. In vivo study of conductive 3D printed PCL/MWCNTs scaffolds with electrical stimulation for bone tissue engineering. Bio-Des. Manuf. 2021, 4, 190–202. [Google Scholar] [CrossRef]
- Liu, X.; George, M.N.; Li, L.; Gamble, D.; Miller II, A.L.; Gaihre, B.; Waletzki, B.E.; Lu, L. Injectable Electrical Conductive and Phosphate Releasing Gel with Two-Dimensional Black Phosphorus and Carbon Nanotubes for Bone Tissue Engineering. ACS Biomater. Sci. Eng. 2020, 6, 4653–4665. [Google Scholar] [CrossRef]
- Allo, B.A.; Rizkalla, A.S.; Mequanint, K. Synthesis and Electrospinning of ε-Polycaprolactone-Bioactive Glass Hybrid Biomaterials via a Sol−Gel Process. Langmuir 2010, 26, 18340–18348. [Google Scholar] [CrossRef] [PubMed]
- Costa, K.M.N.; Barros, R.M.; Jorge, E.O.; Sato, M.R.; Chorilli, M.; De Lima Damasceno, B.P.G.; Nicholas, D.; Callan, J.F.; Oshiro Junior, J.A. Doxorubicin-loaded nanostructured lipid carriers functionalized with folic acid against MCF-7 breast cancer cell line. J. Nanopart Res. 2023, 25, 56. [Google Scholar] [CrossRef]
- Acharya, D.; Pandey, P.; Nasiri, F.; Singha, K.M.; Mohanta, B. Synthesis, Characterization and Antibacterial Effects of Ag@SiO2 Core–Shell Nanoparticles. J. Bionanosci. 2017, 11, 391–396. [Google Scholar] [CrossRef]
- Hadela, A.; Lakić, M.; Potočnik, M.; Košak, A.; Gutmaher, A.; Lobnik, A. Novel reusable functionalized magnetic cobalt ferrite nanoparticles as oil adsorbents. Adsorpt. Sci. Technol. 2020, 38, 168–190. [Google Scholar] [CrossRef]
- Tan, P.; Li, Y.-H.; Liu, X.-Q.; Jiang, Y.; Sun, L.-B. Core–Shell AgCl@SiO 2 Nanoparticles: Ag(I)-Based Antibacterial Materials with Enhanced Stability. ACS Sustain. Chem. Eng. 2016, 4, 3268–3275. [Google Scholar] [CrossRef]
- Militzer, C.; Buchsbaum, J.; Dzhagan, V.; Zahn, D.R.T.; Wulff, H.; Helm, C.A.; Goedel, W.A. Atomic Layer Deposition of Titanium Phosphate from Titanium Tetrachloride and Triethyl Phosphate onto Carbon Fibers. Adv. Mater. Inter. 2018, 5, 1800423. [Google Scholar] [CrossRef]
- Araujo, J.A.; Cortese, Y.J.; Mojicevic, M.; Brennan Fournet, M.; Chen, Y. Composite Films of Thermoplastic Starch and CaCl2 Extracted from Eggshells for Extending Food Shelf-Life. Polysaccharides 2021, 2, 677–690. [Google Scholar] [CrossRef]
- Pereira, M.M.; Jones, J.R.; Hench, L.L. Bioactive glass and hybrid scaffolds prepared by sol–gel method for bone tissue engineering. Adv. Appl. Ceram. 2005, 104, 35–42. [Google Scholar] [CrossRef]
- Jurić, S.; Đermić, E.; Topolovec-Pintarić, S.; Bedek, M.; Vinceković, M. Physicochemical properties and release characteristics of calcium alginate microspheres loaded with Trichoderma viride spores. J. Integr. Agric. 2019, 18, 2534–2548. [Google Scholar] [CrossRef]
- Liu, X.; Piao, X.; Wang, Y.; Zhu, S. Calcium Ethoxide as a Solid Base Catalyst for the Transesterification of Soybean Oil to Biodiesel. Energy Fuels 2008, 22, 1313–1317. [Google Scholar] [CrossRef]
- Branda, F. Bioactivity of 1.25CaO · SiO2 glass: An FTIR and X-ray study on powdered samples. Biomaterials 1996, 17, 2247–2251. [Google Scholar] [CrossRef] [PubMed]
- Serra, J.; González, P.; Liste, S.; Serra, C.; Chiussi, S.; León, B.; Pérez-Amor, M.; Ylänen, H.O.; Hupa, M. FTIR and XPS studies of bioactive silica based glasses. J. Non-Cryst. Solids 2003, 332, 20–27. [Google Scholar] [CrossRef]
- Lao, J.; Dieudonné, X.; Benbakkar, M.; Jallot, É. Bioactive glass coating on gelatin scaffolds at ambient temperature: Easy route to make polymer scaffolds become bioactive. J. Mater. Sci. 2017, 52, 9129–9139. [Google Scholar] [CrossRef]
- Yang, X.-R.; Zhao, Y.-Q.; Qiu, Y.-T.; Chi, C.-F.; Wang, B. Preparation and Characterization of Gelatin and Antioxidant Peptides from Gelatin Hydrolysate of Skipjack Tuna (Katsuwonus pelamis) Bone Stimulated by in vitro Gastrointestinal Digestion. Mar. Drugs 2019, 17, 78. [Google Scholar] [CrossRef]
- Jackson, M.; Choo, L.-P.; Watson, P.H.; Halliday, W.C.; Mantsch, H.H. Beware of connective tissue proteins: Assignment and implications of collagen absorptions in infrared spectra of human tissues. Biochim. Biophys. Acta Mol. Basis Dis. 1995, 1270, 1–6. [Google Scholar] [CrossRef]
- Sisson, K.; Zhang, C.; Farach-Carson, M.C.; Chase, D.B.; Rabolt, J.F. Evaluation of Cross-Linking Methods for Electrospun Gelatin on Cell Growth and Viability. Biomacromolecules 2009, 10, 1675–1680. [Google Scholar] [CrossRef]
- Lei, B.; Shin, K.-H.; Noh, D.-Y.; Jo, I.-H.; Koh, Y.-H.; Choi, W.-Y.; Kim, H.-E. Nanofibrous gelatin–silica hybrid scaffolds mimicking the native extracellular matrix (ECM) using thermally induced phase separation. J. Mater. Chem. 2012, 22, 14133. [Google Scholar] [CrossRef]
- Tamahkar Irmak, E. Carbon nanotube based polyvinylalcohol-polyvinylpyrolidone nanocomposite hydrogels for controlled drug delivery applications. Anadolu Univ. J. Sci. Technol. A—Appl. Sci. Eng. 2017, 18, 543–553. [Google Scholar] [CrossRef][Green Version]
- Ravanbakhsh, H.; Bao, G.; Latifi, N.; Mongeau, L.G. Carbon nanotube composite hydrogels for vocal fold tissue engineering: Biocompatibility, rheology, and porosity. Mater. Sci. Eng. C 2019, 103, 109861. [Google Scholar] [CrossRef] [PubMed]
- Xing, Q.; Yates, K.; Vogt, C.; Qian, Z.; Frost, M.C.; Zhao, F. Increasing Mechanical Strength of Gelatin Hydrogels by Divalent Metal Ion Removal. Sci. Rep. 2015, 4, 4706. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Zhao, F.; Zhang, W.; Mo, Y.; Zeng, L.; Li, X.; Chen, X. Sequentially-crosslinked biomimetic bioactive glass/gelatin methacryloyl composites hydrogels for bone regeneration. Mater. Sci. Eng. C 2018, 89, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Vichery, C.; Nedelec, J.-M. Bioactive Glass Nanoparticles: From Synthesis to Materials Design for Biomedical Applications. Materials 2016, 9, 288. [Google Scholar] [CrossRef] [PubMed]
- Suvarnapathaki, S.; Nguyen, M.A.; Wu, X.; Nukavarapu, S.P.; Camci-Unal, G. Synthesis and characterization of photocrosslinkable hydrogels from bovine skin gelatin. RSC Adv. 2019, 9, 13016–13025. [Google Scholar] [CrossRef]
- Tang, Z.; Li, X.; Tan, Y.; Fan, H.; Zhang, X. The material and biological characteristics of osteoinductive calcium phosphate ceramics. Regen. Biomater. 2018, 5, 43–59. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Rodriguez, P.; Sánchez, M.; Landin, M. Drug-Loaded Biomimetic Ceramics for Tissue Engineering. Pharmaceutics 2018, 10, 272. [Google Scholar] [CrossRef]
- Morejón, L.; Delgado, J.A.; Antunes Ribeiro, A.; Varella De Oliveira, M.; Mendizábal, E.; García, I.; Alfonso, A.; Poh, P.; Van Griensven, M.; Balmayor, E.R. Development, Characterization and In Vitro Biological Properties of Scaffolds Fabricated from Calcium Phosphate Nanoparticles. Int. J. Mol. Sci. 2019, 20, 1790. [Google Scholar] [CrossRef]
- Wang, S.; Kowal, T.J.; Marei, M.K.; Falk, M.M.; Jain, H. Nanoporosity Significantly Enhances the Biological Performance of Engineered Glass Tissue Scaffolds. Tissue Eng. Part. A 2013, 19, 1632–1640. [Google Scholar] [CrossRef]
- Mondal, D.; Rizkalla, A.S.; Mequanint, K. Bioactive borophosphosilicate-polycaprolactone hybrid biomaterials via a non-aqueous sol gel process. RSC Adv. 2016, 6, 92824–92832. [Google Scholar] [CrossRef]
- Deguchi, K.; Nomura, S.; Tsuchiya, A.; Takahashi, I.; Ishikawa, K. Effects of the carbonate content in carbonate apatite on bone replacement. J. Tissue Eng. Regen. Med. 2022, 16, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Russo, L.; Taraballi, F.; Lupo, C.; Poveda, A.; Jiménez-Barbero, J.; Sandri, M.; Tampieri, A.; Nicotra, F.; Cipolla, L. Carbonate hydroxyapatite functionalization: A comparative study towards (bio)molecules fixation. Interface Focus 2014, 4, 20130040. [Google Scholar] [CrossRef] [PubMed]
- Maçon, A.L.B.; Kim, T.B.; Valliant, E.M.; Goetschius, K.; Brow, R.K.; Day, D.E.; Hoppe, A.; Boccaccini, A.R.; Kim, I.Y.; Ohtsuki, C.; et al. A unified in vitro evaluation for apatite-forming ability of bioactive glasses and their variants. J. Mater. Sci. Mater. Med. 2015, 26, 115. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Yang, Y.; Wan, R.; Shen, Y.; Zhang, W. Hydrothermal Preparation and Characterization of Ultralong Strontium-Substituted Hydroxyapatite Whiskers Using Acetamide as Homogeneous Precipitation Reagent. Sci. World J. 2014, 2014, 863137. [Google Scholar] [CrossRef] [PubMed]
- Murugan, R.; Ramakrishna, S.; Panduranga Rao, K. Nanoporous hydroxy-carbonate apatite scaffold made of natural bone. Mater. Lett. 2006, 60, 2844–2847. [Google Scholar] [CrossRef]
- Kirsch, M.; Birnstein, L.; Pepelanova, I.; Handke, W.; Rach, J.; Seltsam, A.; Scheper, T.; Lavrentieva, A. Gelatin-Methacryloyl (GelMA) Formulated with Human Platelet Lysate Supports Mesenchymal Stem Cell Proliferation and Differentiation and Enhances the Hydrogel’s Mechanical Properties. Bioengineering 2019, 6, 76. [Google Scholar] [CrossRef]
- Maeno, S.; Niki, Y.; Matsumoto, H.; Morioka, H.; Yatabe, T.; Funayama, A.; Toyama, Y.; Taguchi, T.; Tanaka, J. The effect of calcium ion concentration on osteoblast viability, proliferation and differentiation in monolayer and 3D culture. Biomaterials 2005, 26, 4847–4855. [Google Scholar] [CrossRef]


| Gelatin-BG-MWCNT Nomenclature | Gelatin (wt.%) | BG (wt.%) | MWCNT (wt.%) |
|---|---|---|---|
| 50-50-0 | 50 | 50 | 0 |
| 50-50-1 | 50 | 50 | 1 |
| Sample | Porosity (%) | Pore Wall Thickness (µm) | Pore Size (µm) | Surface Area to Volume Ratio (mm−1) |
|---|---|---|---|---|
| 50-50-0 (CaCl2) | 24.48 | 0.49 | 0.16 | 4.08 |
| 50-50-1 (CaCl2) | 29.59 | 0.41 | 0.16 | 4.90 |
| 50-50-0 Ca(OEt)2 | 5.03 | 1.64 | 0.06 | 1.22 |
| 50-50-1 Ca(OEt)2 | 5.84 | 1.92 | 0.10 | 1.04 |
| Sample | Atomic % Ca before SBF | Atomic % P before SBF | Atomic % Ca after SBF | Atomic % P after SBF | Ca/P Ratio after SBF |
|---|---|---|---|---|---|
| 50-50-0 CaCl2 | 6.40 | 0.03 | 16.93 | 8.76 | 1.93 |
| 50-50-1 CaCl2 | 5.49 | 0.03 | 17.93 | 9.62 | 1.86 |
| 50-50-0 Ca(OEt)2 | 5.83 | 0.04 | 20.40 | 10.34 | 1.97 |
| 50-50-1 Ca(OEt)2 | 4.85 | 0.04 | 20.20 | 10.53 | 1.91 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arambula-Maldonado, R.; Mequanint, K. Sol-Gel Derived Gelatin–Bioactive Glass Nanocomposite Biomaterials Incorporating Calcium Chloride and Calcium Ethoxide. Polymers 2024, 16, 747. https://doi.org/10.3390/polym16060747
Arambula-Maldonado R, Mequanint K. Sol-Gel Derived Gelatin–Bioactive Glass Nanocomposite Biomaterials Incorporating Calcium Chloride and Calcium Ethoxide. Polymers. 2024; 16(6):747. https://doi.org/10.3390/polym16060747
Chicago/Turabian StyleArambula-Maldonado, Rebeca, and Kibret Mequanint. 2024. "Sol-Gel Derived Gelatin–Bioactive Glass Nanocomposite Biomaterials Incorporating Calcium Chloride and Calcium Ethoxide" Polymers 16, no. 6: 747. https://doi.org/10.3390/polym16060747
APA StyleArambula-Maldonado, R., & Mequanint, K. (2024). Sol-Gel Derived Gelatin–Bioactive Glass Nanocomposite Biomaterials Incorporating Calcium Chloride and Calcium Ethoxide. Polymers, 16(6), 747. https://doi.org/10.3390/polym16060747






