Polymer-Based Hydroxyapatite–Silver Composite Resin with Enhanced Antibacterial Activity for Dental Applications
Abstract
1. Introduction
2. Materials and Methods
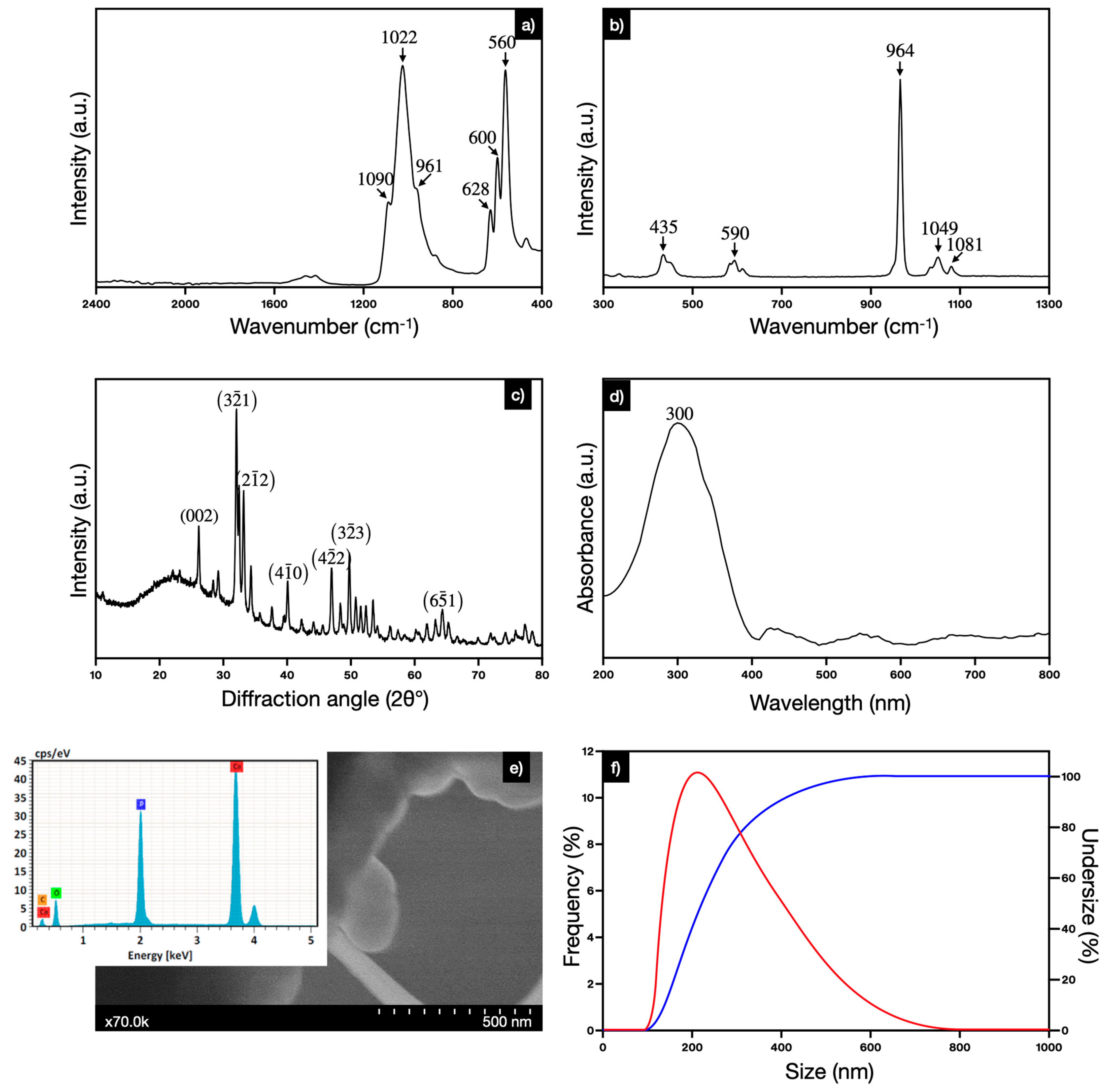
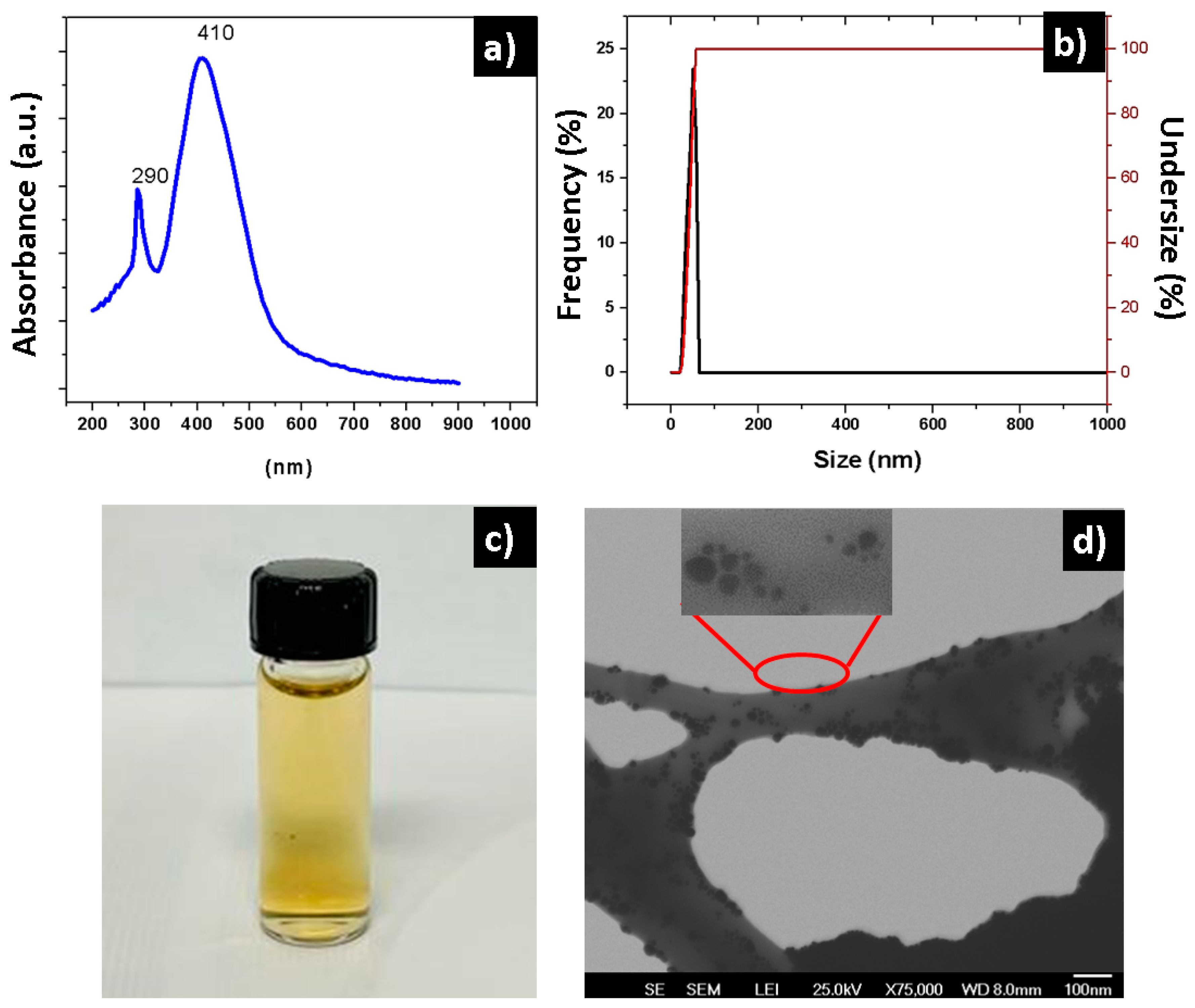
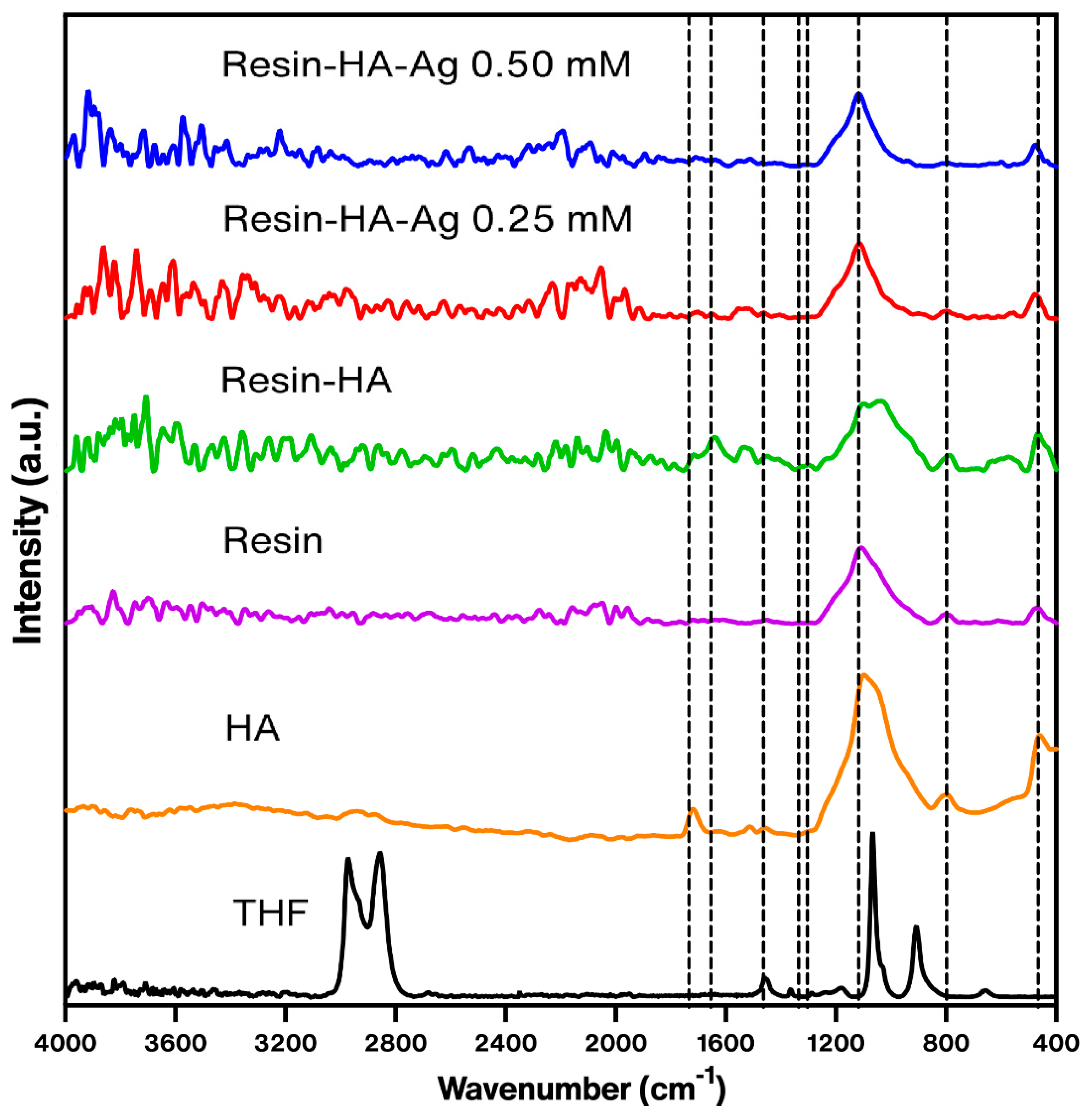
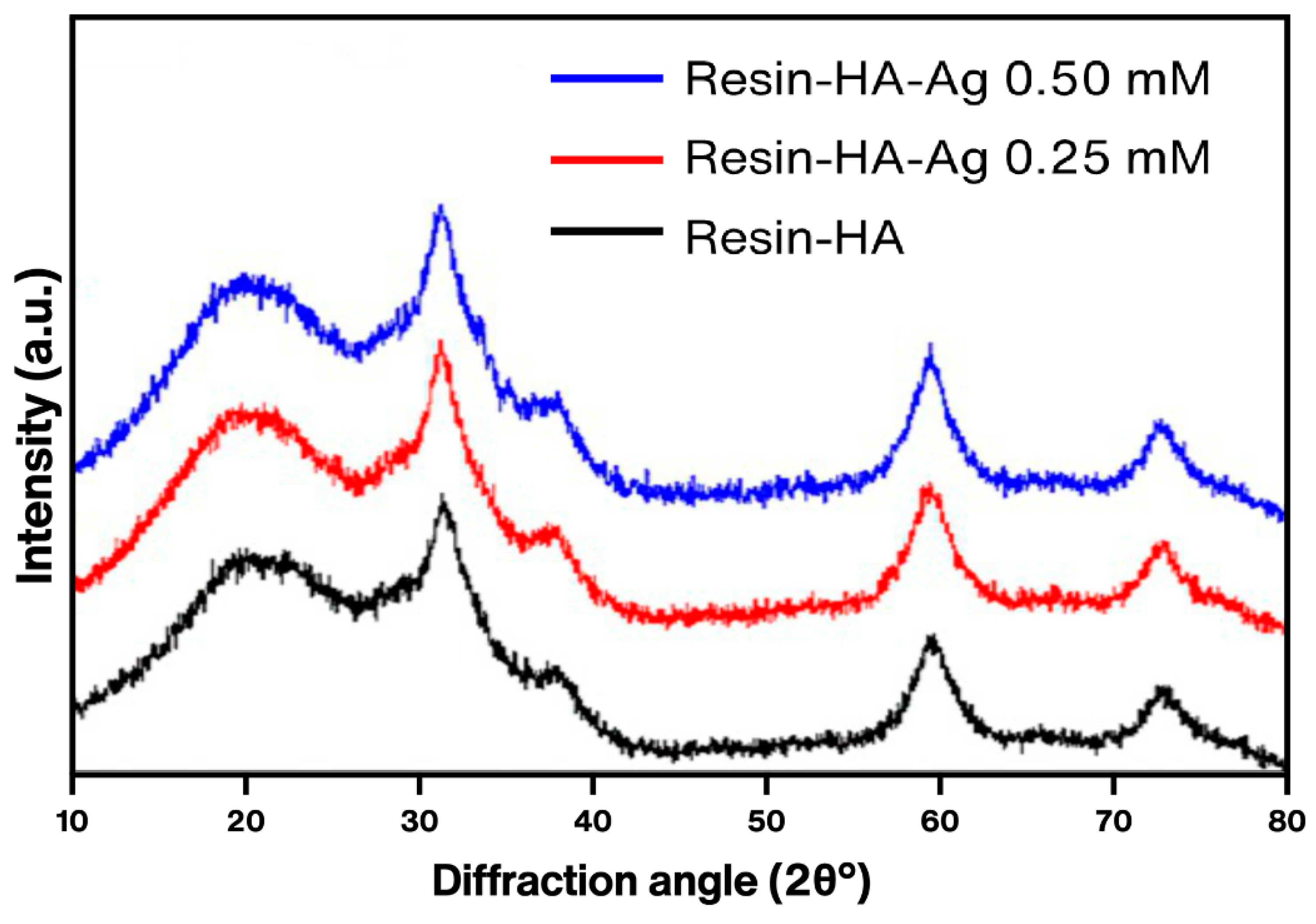
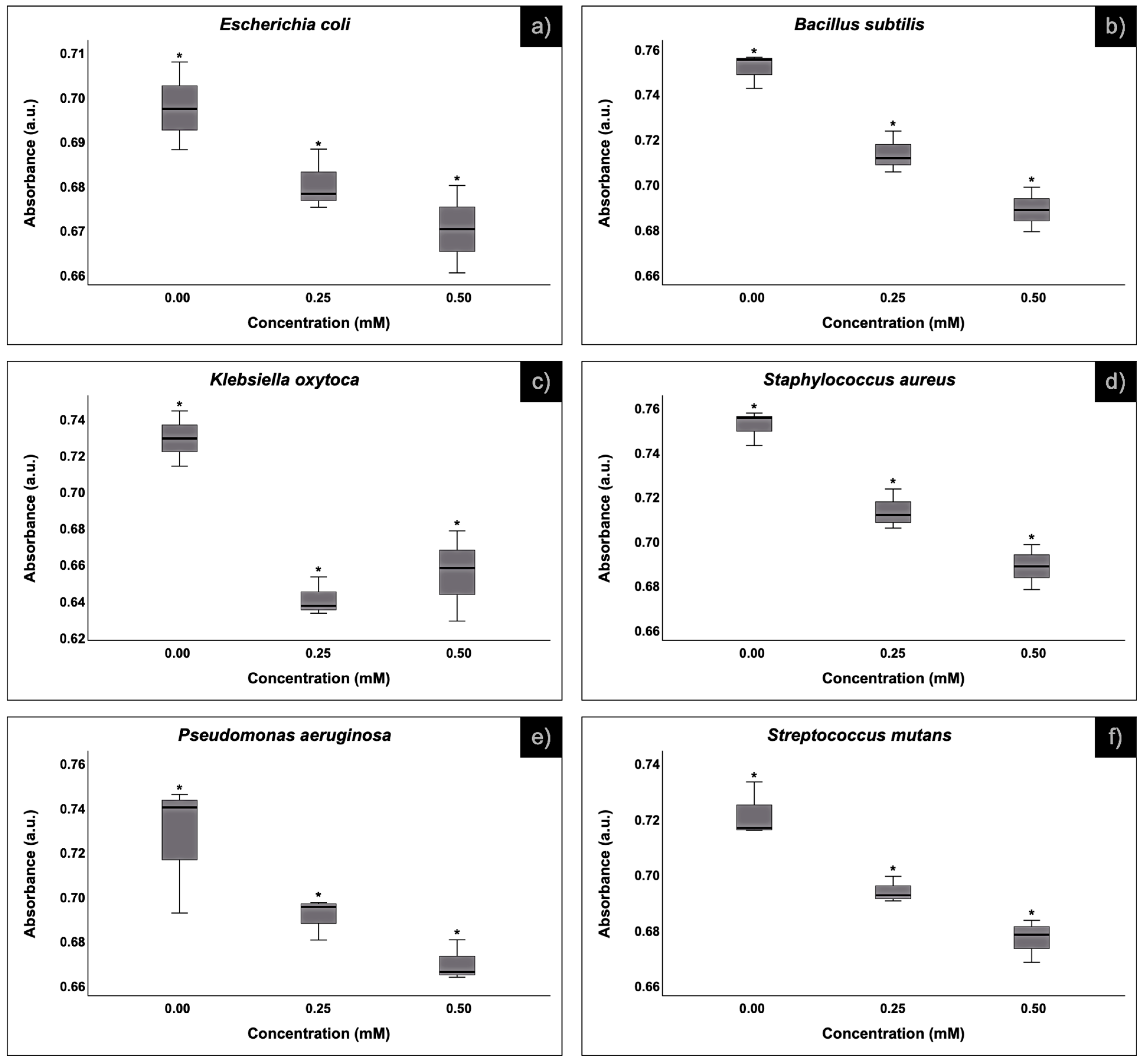
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mathur, V.P.; Dhillon, J.K. Dental Caries: A Disease Which Needs Attention. Indian J. Pediatr. 2017, 85, 202–206. [Google Scholar] [CrossRef]
- Pitts, N.B.; Zero, D.T.; Marsh, P.D.; Ekstr, K.; Weintraub, J.A.; Ramos-Gomez, F.; Tagami, J.; Twetman, S.; Tsakos, G.; Ismail, A. Dental caries. Nat. Rev. Dis. Primers 2017, 3, 17030. [Google Scholar] [CrossRef]
- Pratap, B.; Gupta, R.K.; Bhardwaj, B.; Nag, M. Resin based restorative dental materials: Characteristics and future perspectives. Jpn. Dent. Sci. Rev. 2019, 55, 126–138. [Google Scholar] [CrossRef]
- He, J.; Söderling, E.; Lassila, L.V.J.; Vallittu, P.K. Preparation of antibacterial and radio-opaque dental resin with new polymerizable quaternary ammonium monomer. Dent. Mater. 2015, 31, 575–582. [Google Scholar] [CrossRef]
- Boaro, L.C.C.; Campos, L.M.; Varca, G.H.C.; Dos Santos, T.M.R.; Marques, P.A.; Sugii, M.M.; Saldanha, N.R.; Cogo-Müller, K.; Brandt, W.C.; Braga, R.R.; et al. Antibacterial resin-based composite containing chlorhexidine for dental applications. Dent. Mater. 2019, 35, 909–918. [Google Scholar] [CrossRef]
- Garcia, I.M.; Leitune, V.C.B.; Visioli, F.; Samuel, S.M.W.; Collares, F.M. Influence of zinc oxide quantum dots in the antibacterial activity and cytotoxicity of an experimental adhesive resin. J. Dent. 2018, 73, 57–60. [Google Scholar] [CrossRef]
- Lee, S.J.; Heo, M.; Lee, D.; Han, S.; Moon, J.-H.; Lim, H.-N.; Kwon, I.K. Preparation and characterization of antibacterial orthodontic resin containing silver nanoparticles. Appl. Surf. Sci. 2018, 432, 317–323. [Google Scholar] [CrossRef]
- Khalil, E.; Elkhader, I.A.; Elsahn, N.A.; Ahmed, A.S.; Raj, S.S. Antibacterial activity of novel selenium and zinc nanoparticles toward oral Candida albicans: An In vitro study. Drug Invent. Today 2020, 14, 36–38. [Google Scholar]
- Fernández-Arias, M.; Boutinguiza, M.; del Val, J.; Medina, E.; Rodríguez, D.; Riveiro, A.; Comesaña, R.; Lusquiños, F.; Gil, F.J.; Pou, J. RE-irradiation of silver nanoparticles obtained by laser ablation in water and assessment of their antibacterial effect. Appl. Surf. Sci. 2019, 473, 548–554. [Google Scholar] [CrossRef]
- Dong, Y.; Zhu, H.; Shen, Y.; Zhang, W.; Zhang, L. Antibacterial activity of silver nanoparticles of different particle size against Vibrio Natriegens. PLoS ONE 2019, 14, e0222322. [Google Scholar] [CrossRef]
- Tang, S.; Zheng, J. Antibacterial Activity of Silver Nanoparticles: Structural Effects. Adv. Healthc. Mater. 2018, 7, 1701503. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Bulut, O.; Some, S.; Mandal, A.K.; Yilmaz, M.D. Green synthesis of silver nanoparticles: Biomolecule-nanoparticle organizations targeting antimicrobial activity. RSC Adv. 2019, 9, 2673–2702. [Google Scholar] [CrossRef] [PubMed]
- Blinov, A.V.; Nagdalian, A.A.; Povetkin, S.N.; Gvozdenko, A.A.; Verevkina, M.N.; Rzhepakovsky, I.V.; Lopteva, M.S.; Maglakelidze, D.G.; Kataeva, T.S.; Blinova, A.A.; et al. Surface-Oxidized Polymer-Stabilized Silver Nanoparticles as a Covering Component of Suture Materials. Micromachines 2022, 13, 1105. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Gawad, R.; Osman, R.; Awad, G.A.S.; Mortada, N. Wound healing potential of silver nanoparticles embedded in optimized bio-inspired hybridized chitosan soft and dry hydrogel. Carbohydr. Polym. 2024, 324, 121526. [Google Scholar] [CrossRef]
- Nešporová, K.; Pavlík, V.; Šafránková, B.; Vágnerová, H.; Odráška, P.; Žídek, O.; Císařová, N.; Skoroplyas, S.; Kubala, L.; Velebný, V. Effects of wound dressings containing silver on skin and immune cells. Sci. Rep. 2020, 10, 15216. [Google Scholar] [CrossRef] [PubMed]
- Tschoppe, P.; Zandim, D.L.; Martus, P.; Kielbassa, A.M. Enamel and dentine remineralization by nano-hydroxyapatite toothpastes. J. Dent. 2011, 39, 430–437. [Google Scholar] [CrossRef]
- Huang, S.B.; Gao, S.S.; Yu, H.Y. Effect of nano-hydroxyapatite concentration on remineralization of initial enamel lesion in vitro. Biomed. Mater. 2009, 4, 034104. [Google Scholar] [CrossRef]
- Juntavee, N.; Juntavee, A.; Plongniras, P. Remineralization potential of nano-hydroxyapatite on enamel and cementum surrounding margin of computer-aided design and computer-aided manufacturing ceramic restoration. Int. J. Nanomed. 2018, 13, 2755–2765. [Google Scholar] [CrossRef]
- Najibfard, K.; Ramalingam, K.; Chedjieu, I.; Amaechi, B.T. Remineralization of early caries by a nano-hydroxyapatite dentifrice. J. Clin. Dent. 2011, 22, 139. [Google Scholar]
- Tschoppe, P.; Meyer-Lueckel, H. Mineral distribution of artificial dentinal caries lesions after treatment with fluoride agents in combination with saliva substitutes. Arch. Oral Biol. 2011, 56, 775–784. [Google Scholar] [CrossRef]
- Gilani, M.A.H.; Ameli, N.; Ghorbani, R.; Akhavan, A.; Rabiei, A.; Zeinabadi, M.S.; Kameli, S. Effect of Adding Nano Silver-Hydroxyapatite to the Orthodontic Primer on Bracket-Enamel Shear Bond Strength. J. Evol. Med. Dent. Sci. 2020, 9, 3457–3462. [Google Scholar] [CrossRef]
- Sodagar, A.; Akhavan, A.; Hashemi, E.; Arab, S.; Pourhajibagher, M.; Sodagar, K.; Kharrazifard, M.J.; Bahador, A. Evaluation of the antibacterial activity of a conventional orthodontic composite containing silver/hydroxyapatite nanoparticles. Prog. Orthod. 2016, 17, 40. [Google Scholar] [CrossRef] [PubMed]
- Melo, M.A.; Guedes, S.F.; Xu, H.H.; Rodrigues, L.K. Nanotechnology-based restorative materials for dental caries management. Trends Biotechnol. 2013, 31, 459–467. [Google Scholar] [CrossRef]
- Ai, M.; Du, Z.; Zhu, S.; Geng, H.; Zhang, X.; Cai, Q.; Yang, X. Composite resin reinforced with silver nanoparticles–laden hydroxyapatite nanowires for dental application. Dent. Mater. 2017, 33, 12–22. [Google Scholar] [CrossRef]
- Gradinaru, I.; Ignat, L.; Dascalu, C.G.; Soroaga, L.V.; Antohe, M.E. Studies Regarding the Architectural Design of Various Composites and Nanofibres Used in Dental Medicine. Rev. Chim. 2018, 69, 328–331. [Google Scholar] [CrossRef]
- Garibay-Alvarado, J.A.; Herrera-Ríos, E.B.; Vargas-Requena, C.L.; de Jesús Ruíz-Baltazar, Á.; Reyes-López, S.Y. Cell behavior on silica-hydroxyapatite coaxial composite. PLoS ONE 2021, 16, e0246256. [Google Scholar] [CrossRef] [PubMed]
- Silva-Holguín, P.N.; Reyes-López, S.Y. Synthesis of Hydroxyapatite-Ag Composite as Antimicrobial Agent. Dose-Response 2020, 18, 155932582095134. [Google Scholar] [CrossRef] [PubMed]
- Silva-Holguín, P.N.; Garibay-Alvarado, J.A.; Reyes-López, S.Y. Silver Nanoparticles: Multifunctional Tool in Environmental Water Remediation. Materials 2024, 17, 1939. [Google Scholar] [CrossRef]
- Döbelin, N.; Kleeberg, R. Profex: A graphical user interface for the Rietveld refinement program BGMN. J. Appl. Crystallogr. 2015, 48, 1573–1580. [Google Scholar] [CrossRef]
- Vanlancker, E.; Vanhoecke, B.; Smet, R.; Props, R.; Van de Wiele, T. 5-Fluorouracil sensitivity varies among oral micro-organisms. J. Med. Microbiol. 2016, 65, 775–783. [Google Scholar] [CrossRef]
- Ruíz-Baltazar, Á.d.J.; Reyes-López, S.Y.; Silva-Holguin, P.N.; Larrañaga, D.; Estévez, M.; Pérez, R. Novel biosynthesis of Ag-hydroxyapatite: Structural and spectroscopic characterization. Results Phys. 2018, 9, 593–597. [Google Scholar] [CrossRef]
- Ider, M.; Abderrafi, K.; Eddahbi, A.; Ouaskit, S.; Kassiba, A. Silver Metallic Nanoparticles with Surface Plasmon Resonance: Synthesis and Characterizations. J. Clust. Sci. 2016, 28, 1051–1069. [Google Scholar] [CrossRef]
- Carter, M.K. Correlation of electronic transitions and redox potentials measured for pyrocatechol, resorcinol, hydroquinone, pyrogallol, and gallic acid with results of semi-empirical molecular orbital computations—A useful interpretation tool. J. Mol. Struct. 2007, 831, 26–36. [Google Scholar] [CrossRef]
- Agnihotri, S.; Mukherji, S.; Mukherji, S. Size-controlled silver nanoparticles synthesized over the range 5–100 nm using the same protocol and their antibacterial efficacy. RSC Adv. 2014, 4, 3974–3983. [Google Scholar] [CrossRef]
- Mulfinger, L.; Solomon, S.D.; Bahadory, M.; Jeyarajasingam, A.V.; Rutkowsky, S.A.; Boritz, C. Synthesis and Study of Silver Nanoparticles. J. Chem. Educ. 2007, 84, 322. [Google Scholar] [CrossRef]
- Sökmen, M.; Alomar, S.Y.; Albay, C.; Serdar, G. Microwave assisted production of silver nanoparticles using green tea extracts. J. Alloys Compd. 2017, 725, 190–198. [Google Scholar] [CrossRef]
- Mendes, L.C.; Ribeiro, G.L.; Marques, R.C. In Situ Hydroxyapatite Synthesis: Influence of Collagen on Its Structural and Morphological Characteristic. Mater. Sci. Appl. 2012, 3, 580–586. [Google Scholar] [CrossRef][Green Version]
- Meejoo, S.; Maneeprakorn, W.; Winotai, P. Phase and thermal stability of nanocrystalline hydroxyapatite prepared via microwave heating. Thermochim. Acta 2006, 447, 115–120. [Google Scholar] [CrossRef]
- Azarshin, S.; Moghadasi, J.; A Aboosadi, Z. Surface functionalization of silica nanoparticles to improve the performance of water flooding in oil wet reservoirs. Energy Explor. Exploit. 2017, 35, 685–697. [Google Scholar] [CrossRef]
- Shi, F.; Li, Y.; Wang, H.; Zhang, Q. Fabrication of well-dispersive yttrium-stabilized cubic zirconia nanoparticles via vapor phase hydrolysis. Prog. Nat. Sci. Mater. Int. 2012, 22, 15–20. [Google Scholar] [CrossRef]
- Dwivedi, A.; Baboo, V.; Bajpai, A. Fukui Function Analysis and Optical, Electronic, and Vibrational Properties of Tetrahydrofuran and Its Derivatives: A Complete Quantum Chemical Study. J. Theor. Chem. 2015, 2015, 345234. [Google Scholar] [CrossRef]
- Available online: https://www.acs.org/molecule-of-the-week/archive/t/tetrahydrofuran.html (accessed on 5 June 2024).
- Khedkar, M.V.; Somvanshi, S.B.; Humbe, A.V.; Jadhav, K.M. Surface modified sodium silicate based superhydrophobic silica aerogels prepared via ambient pressure drying process. J. Non-Cryst. Solids 2019, 511, 140–146. [Google Scholar] [CrossRef]
- Khan, A.S.; Khalid, H.; Sarfraz, Z.; Khan, M.; Iqbal, J.; Muhammad, N.; Fareed, M.A.; Rehman, I.U. Vibrational spectroscopy of selective dental restorative materials. Appl. Spectrosc. Rev. 2016, 52, 507–540. [Google Scholar] [CrossRef]
- Said, M.M.; Rehan, M.; El-Sheikh, S.M.; Zahran, M.K.; Abdel-Aziz, M.S.; Bechelany, M.; Barhoum, A. Multifunctional Hydroxyapatite/Silver Nanoparticles/Cotton Gauze for Antimicrobial and Biomedical Applications. Nanomaterials 2021, 11, 429. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, T.; Iryo, K.; Watanabe, N.; Tsuji, M. Preparation of silver nanoparticles by laser ablation in solution: Influence of laser wavelength on particle size. Appl. Surf. Sci. 2002, 202, 80–85. [Google Scholar] [CrossRef]
- Murphy, C.; Jana, N. Controlling the Aspect Ratio of Inorganic Nanorods and Nanowires. Adv. Mater. 2002, 14, 80–82. [Google Scholar] [CrossRef]
- Roque-Ruiz, J.H.; Garibay-Alvarado, J.A.; Medellín-Castillo, N.A.; Reyes-López, S.Y. Preparation of Electrospun Hydroxyapatite-Glass Fibers for Removal of Cadmium (Cd+2) and Lead (Pb+2) from Aqueous Media. Water Air Soil Pollut. 2020, 231, 497. [Google Scholar] [CrossRef]
- Pattabi, R.M.; Thilipan, G.A.K.; Bhat, V.; Sridhar, K.R.; Pattabi, M. Antibacterial efficacy of silver nanoparticles against Escherichia coli. AIP Conf. Proc. 2013, 1512, 372–373. [Google Scholar] [CrossRef]
- Nirmala, R.; Sheikh, F.A.; Kanjwal, M.A.; Lee, J.H.; Park, S.-J.; Navamathavan, R.; Kim, H.Y. Synthesis and characterization of bovine femur bone hydroxyapatite containing silver nanoparticles for the biomedical applications. J. Nanoparticle Res. 2010, 13, 1917–1927. [Google Scholar] [CrossRef]
- Mocanu, A.; Furtos, G.; Rapuntean, S.; Horovitz, O.; Flore, C.; Garbo, C.; Danisteanu, A.; Rapuntean, G.; Prejmerean, C.; Tomoaia-Cotisel, M. Synthesis; characterization and antimicrobial effects of composites based on multi-substituted hydroxyapatite and silver nanoparticles. Appl. Surf. Sci. 2014, 298, 225–235. [Google Scholar] [CrossRef]
- Pazos-Ortiz, E.; Roque-Ruiz, J.H.; Hinojos-Márquez, E.A.; López-Esparza, J.; Donohué-Cornejo, A.; Cuevas-González, J.C.; Espinosa-Cristóbal, L.F.; Reyes-López, S.Y. Dose-Dependent Antimicrobial Activity of Silver Nanoparticles on Polycaprolactone Fibers against Gram-Positive and Gram-Negative Bacteria. J. Nanomater. 2017, 2017, 4752314. [Google Scholar] [CrossRef]
- Riaz, M.; Zia, R.; Ijaz, A.; Hussain, T.; Mohsin, M.; Malik, A. Synthesis of monophasic Ag doped hydroxyapatite and evaluation of antibacterial activity. Mater. Sci. Eng. C 2018, 90, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Wang, T.; Wang, C.; Wang, Z.; Yang, Y.; Li, P.; Cai, R.; Sun, M.; Yuan, H.; Nie, L. Synthesis and characterization of silver nanoparticles-doped hydroxyapatite/alginate microparticles with promising cytocompatibility and antibacterial properties. Colloids Surf. A Physicochem. Eng. Asp. 2020, 585, 124081. [Google Scholar] [CrossRef]
- Gwon, B.; Bae, E.-B.; Lee, J.-J.; Cho, W.-T.; Bae, H.-Y.; Choi, J.-W.; Huh, J.-B. Wear Characteristics of Dental Ceramic CAD/CAM Materials Opposing Various Dental Composite Resins. Materials 2019, 12, 1839. [Google Scholar] [CrossRef] [PubMed]


| Bacteria | Silver Nanoparticles Concentration | ||
|---|---|---|---|
| Resin with HA | 0.25 mM | 0.50 mM | |
| Inhibition diameter (mm) | |||
| Bacillus subtilis | —±0.00 | —±0.00 | —±0.00 |
| Escherichia coli | —±0.00 | —±0.00 | —±0.00 |
| Klebsiella oxytoca | —±0.00 | —±0.00 | 5.73 ± 0.50 |
| Pseudomonas aeruginosa | —±0.00 | —±0.00 | —±0.00 |
| Staphylococcus aureus | —±0.00 | —±0.00 | 12.18 ± 0.97 |
| Streptococcus mutans | —±0.00 | 5.35 ± 0.17 | 12.18 ± 1.32 |
| Material | Inoculum (CFU/mL) | Particle Size (nm) | Concentration AgNPs | Bacterium/(MIC) | Reference |
|---|---|---|---|---|---|
| HA-AgNPs | 1.3 × 106 | 2.65 ± 0.5 | 0.5 mM (0.027 mg/g), 0.25 mM (0.0135 mg/g) | E. coli/>0.5 mM S. mutans/>0.5 mM E. aureus/>0.5 mM K. oxytoca/>0 5 mM P. aeruginosa/>0.5 mM B. subtilis/>0.5 mM | Present work |
| Silver nanoparticles | 1.0 × 104 | 16 | 0, 20, 40, 60, 80 and 100 µg/mL | E: coli/20 µg/mL Inhibit colony-forming unit at 60 µg/mL | [49] |
| Bovine femur bone hydroxyapatite–silver nanoparticles | 1.5 × 106–8 | 8–20 | 0, 1, 3, and 5% | E. coli/3% MRSA/1% | [50] |
| Nano hydroxyapatite doped with silver | 1.0 × 106 | 12.0 ± 5.0 | 2, 2.5, 3, 3.6, 4.5 and 5.4% | E. coli/2% of 10 mm of inhibition S. aureus/2% 11 mm of inhibition | [51] |
| PCL-AgNPs | 1.3 × 106 | 5.6 ± 2.9 | 12.5 mM (0.012 mg/g), 25.0 mM (0.024 mg/g), 50.0 mM (0.046 mg/g) 100.0 mM (0.097 mg/g) | E. coli/>12.5 mM E. aureus/>12.5 mM K. oxytoca./>12.5 mM P. aeruginosa/>12.5 mM | [52] |
| Silver doped hydroxyapatite | 1.0 × 105 | - | 0, 0.1, 0.3, 0.5, 0.7 M of AgNO3 | S. aureus/0.1 M | [53] |
| HA-AgNPs | 1.0 × 105 | - | 0.01 M, 0.05 M, and 0.1 M of AgNO3 | E. coli/0.01 M S. aureus/0.01 M | [54] |
| HA, AgNPs, Cotton | 0.1 × 105–106 | 14 | 2.5 and 5% | S. aureus/99% of inhibition E. coli/96% of inhibition C. albicans/-A. niger/- | [55] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garibay-Alvarado, J.A.; Garcia-Zamarron, D.J.; Silva-Holguín, P.N.; Donohue-Cornejo, A.; Cuevas-González, J.C.; Espinosa-Cristóbal, L.F.; Ruíz-Baltazar, Á.d.J.; Reyes-López, S.Y. Polymer-Based Hydroxyapatite–Silver Composite Resin with Enhanced Antibacterial Activity for Dental Applications. Polymers 2024, 16, 2017. https://doi.org/10.3390/polym16142017
Garibay-Alvarado JA, Garcia-Zamarron DJ, Silva-Holguín PN, Donohue-Cornejo A, Cuevas-González JC, Espinosa-Cristóbal LF, Ruíz-Baltazar ÁdJ, Reyes-López SY. Polymer-Based Hydroxyapatite–Silver Composite Resin with Enhanced Antibacterial Activity for Dental Applications. Polymers. 2024; 16(14):2017. https://doi.org/10.3390/polym16142017
Chicago/Turabian StyleGaribay-Alvarado, Jesús Alberto, Diana Juana Garcia-Zamarron, Pamela Nair Silva-Holguín, Alejandro Donohue-Cornejo, Juan Carlos Cuevas-González, León Francisco Espinosa-Cristóbal, Álvaro de Jesús Ruíz-Baltazar, and Simón Yobanny Reyes-López. 2024. "Polymer-Based Hydroxyapatite–Silver Composite Resin with Enhanced Antibacterial Activity for Dental Applications" Polymers 16, no. 14: 2017. https://doi.org/10.3390/polym16142017
APA StyleGaribay-Alvarado, J. A., Garcia-Zamarron, D. J., Silva-Holguín, P. N., Donohue-Cornejo, A., Cuevas-González, J. C., Espinosa-Cristóbal, L. F., Ruíz-Baltazar, Á. d. J., & Reyes-López, S. Y. (2024). Polymer-Based Hydroxyapatite–Silver Composite Resin with Enhanced Antibacterial Activity for Dental Applications. Polymers, 16(14), 2017. https://doi.org/10.3390/polym16142017








