Plasma Surface Treatment and Application of Polyvinyl Alcohol/Polylactic Acid Electrospun Fibrous Hemostatic Membrane
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of PVA, PLA, and PVA/PLA Fibrous Membranes by Electrospun
2.3. Plasma Treatment of Fibrous Membranes
2.4. Characterization of Fibrous Membranes
2.5. Mechanical Property Test
2.6. Interlayer Bonding
2.7. Water Absorption
2.8. Whole Blood Coagulation Index
2.9. Clotting Time
2.10. Hemolysis Assay
2.11. Cytotoxicity
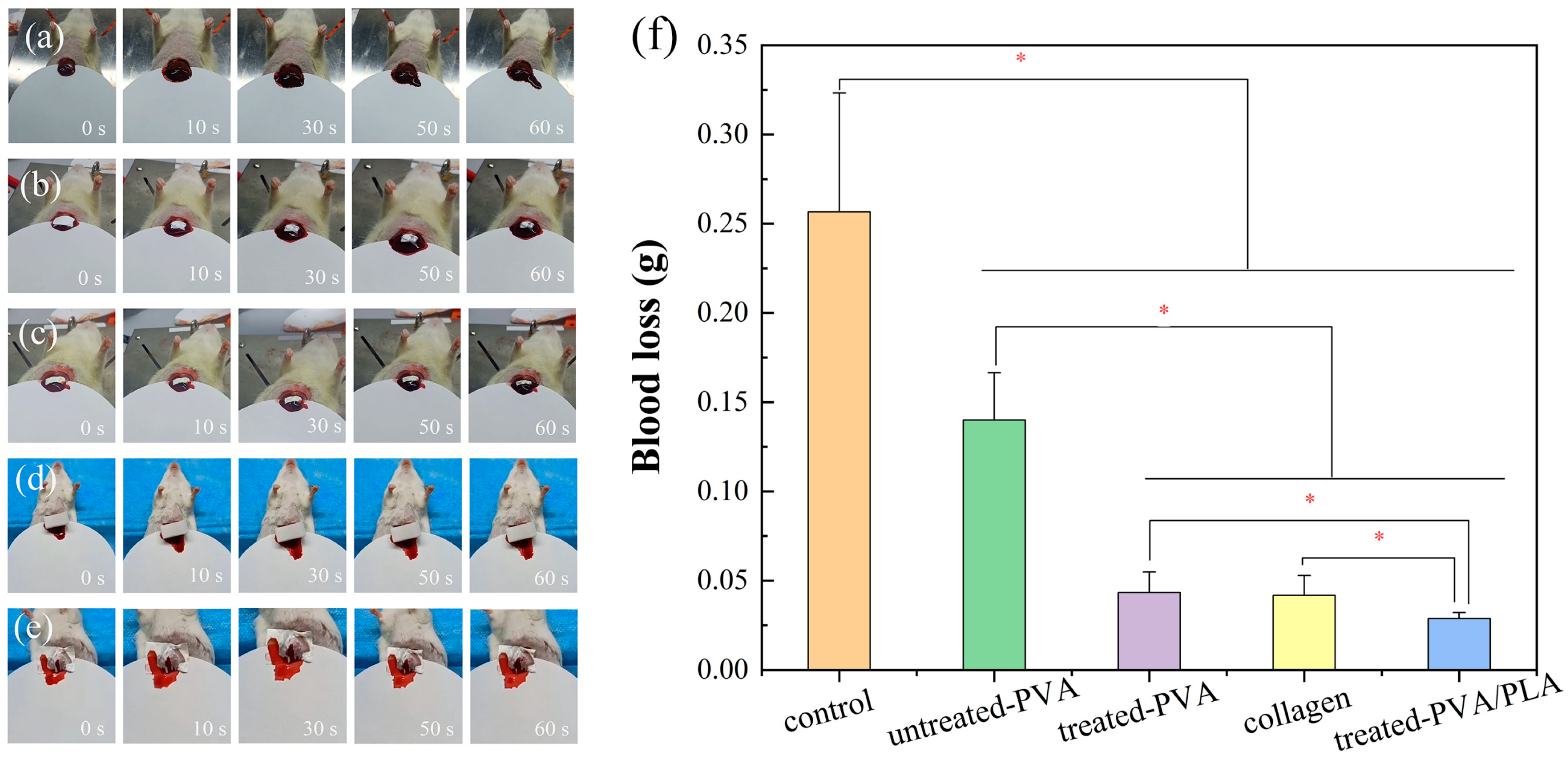
2.12. Liver Hemostasis Experiment
2.13. Statistical Analysis
3. Results and Discussion
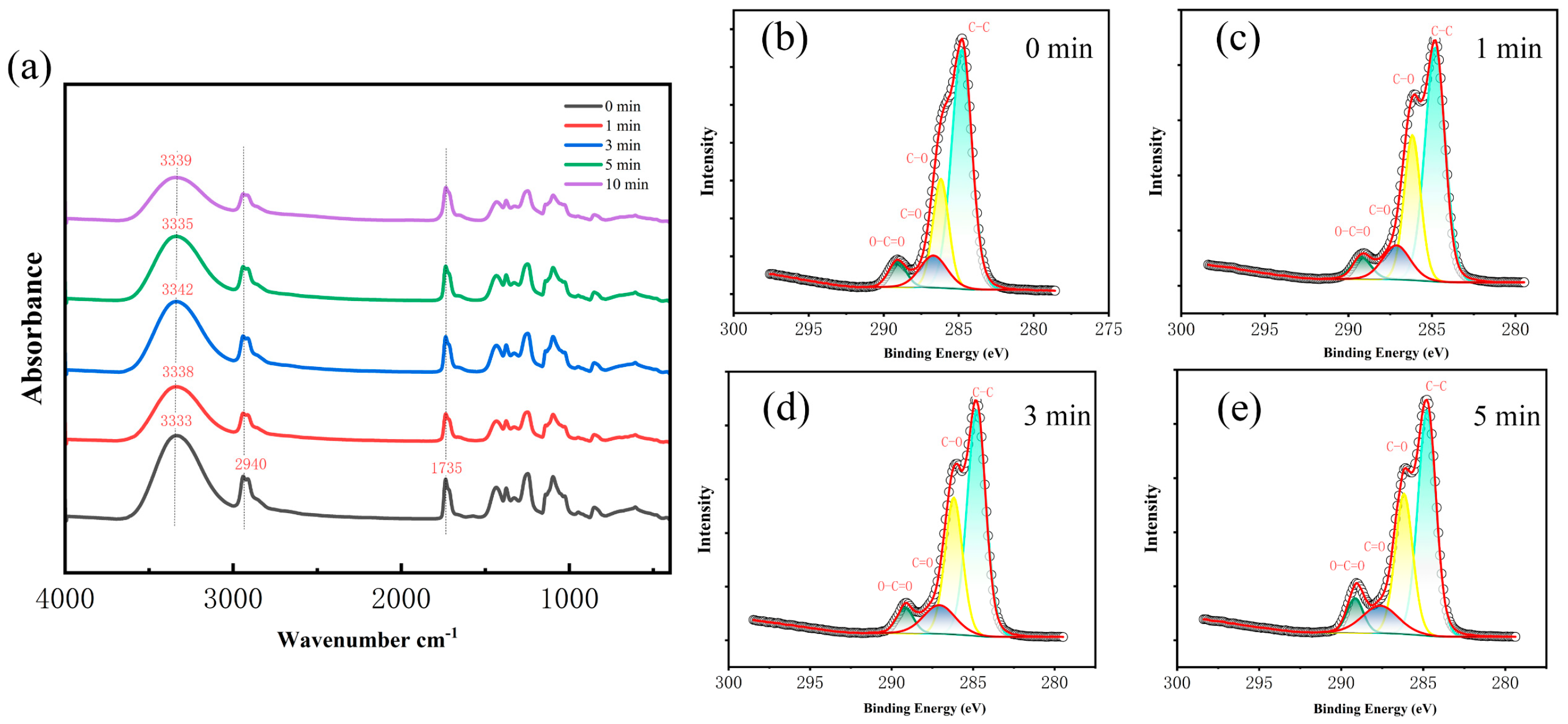
3.1. Characterizations of Plasma-Treated PLA
3.2. Characterizations of Plasma-Treated PVA
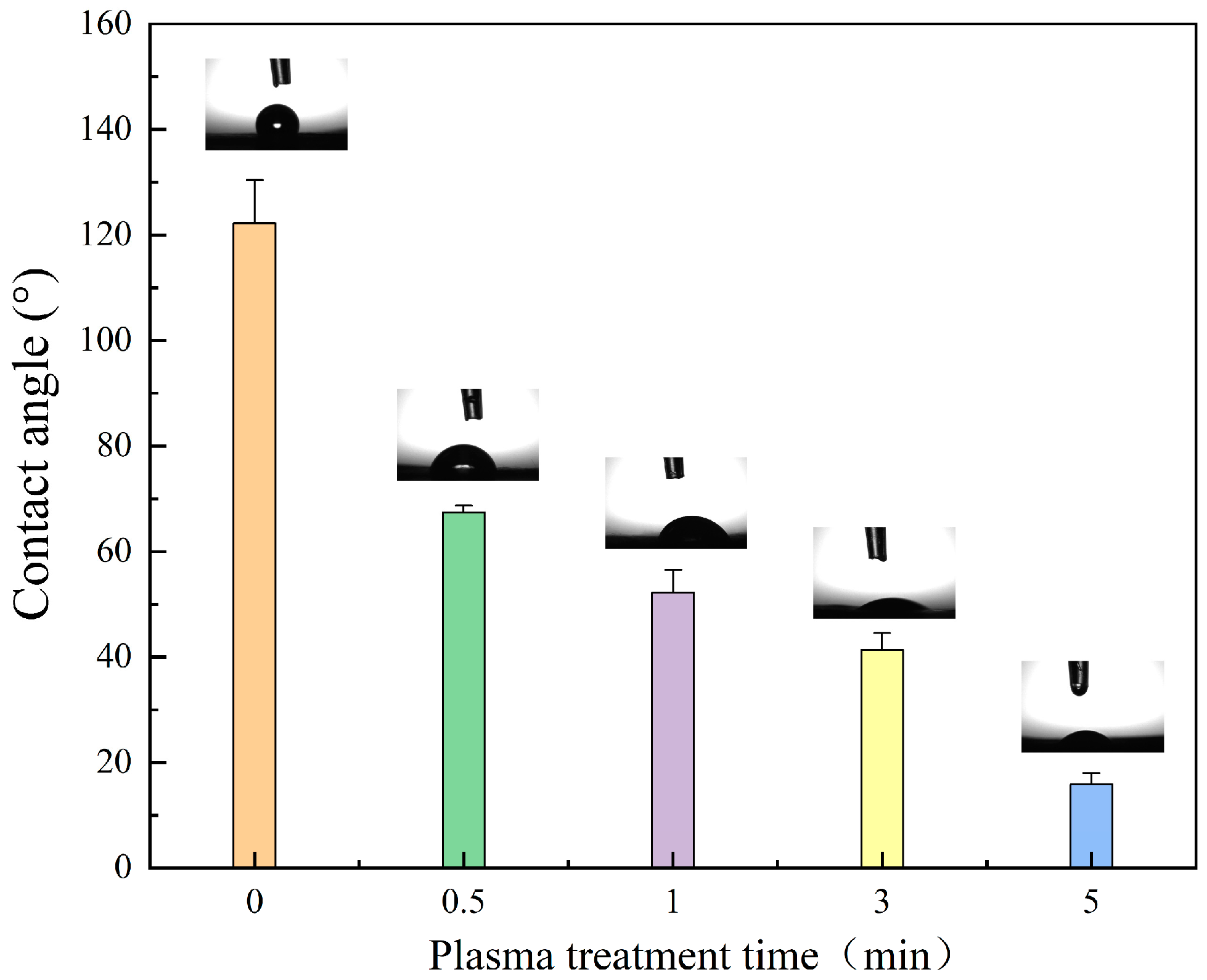
3.3. Wettability
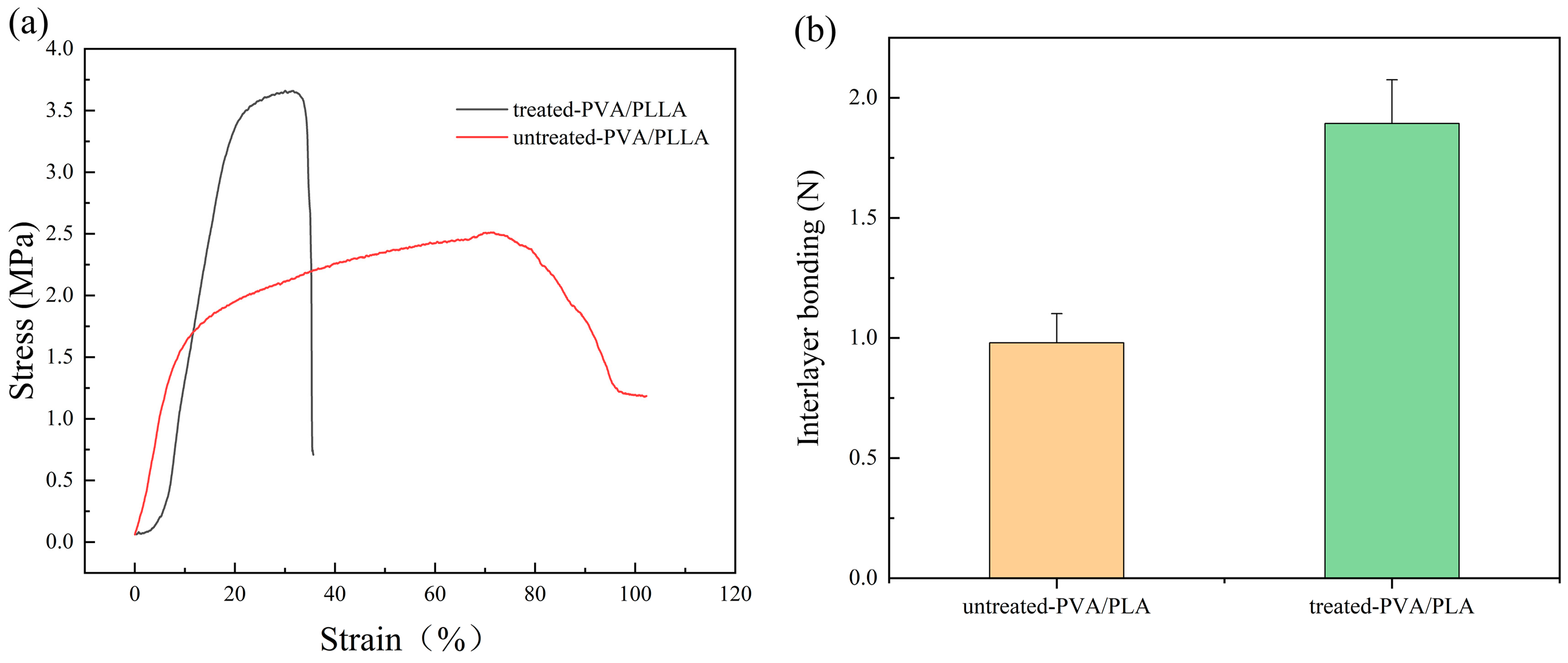
3.4. PVA/PLA Tensile Modulus
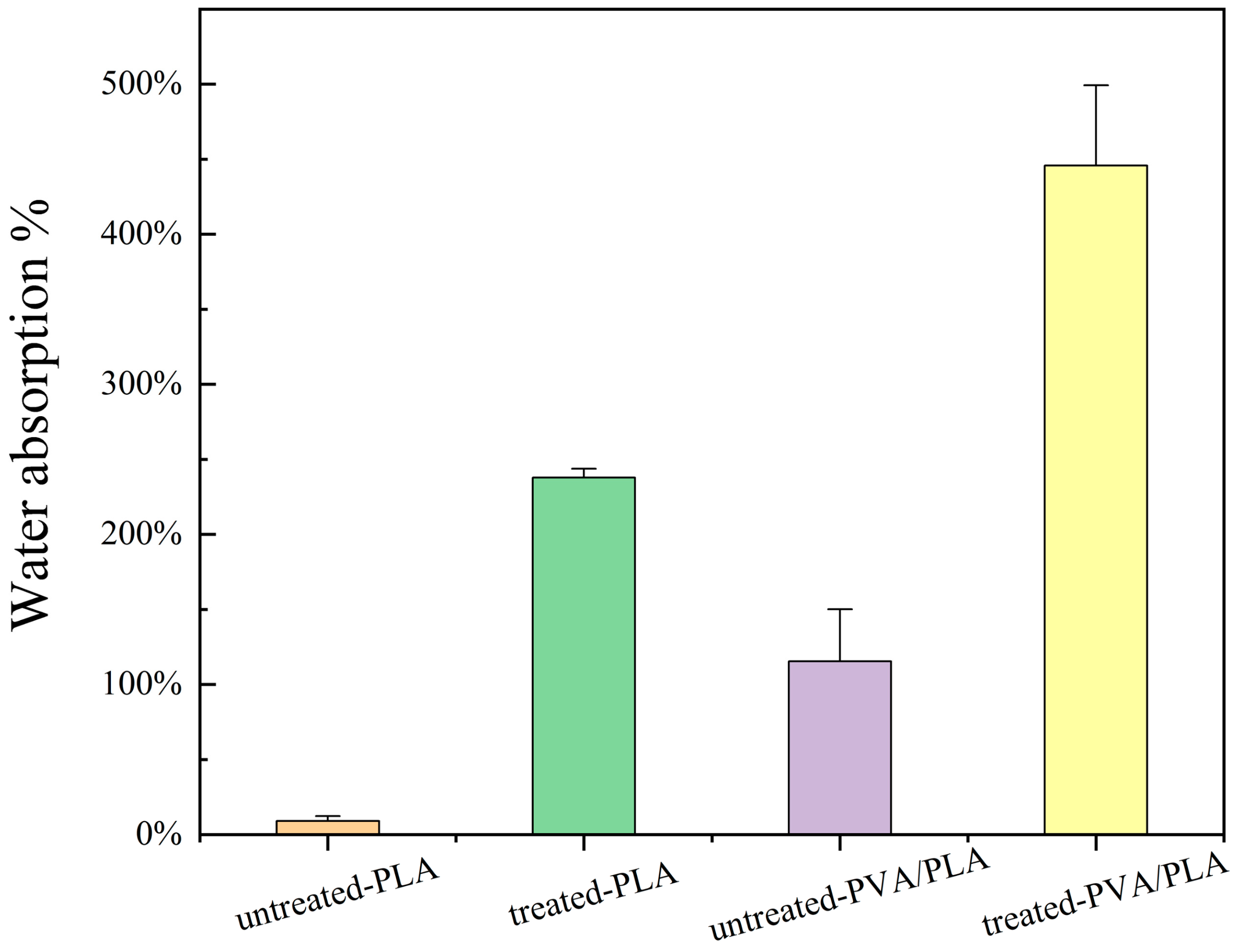
3.5. Water Absorption
3.6. Hemostatic Performance Test
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Han, W.; Wang, S. Advances in Hemostatic Hydrogels That Can Adhere to Wet Surfaces. Gels 2023, 9, 2. [Google Scholar] [CrossRef]
- Guo, B.; Dong, R.; Liang, Y.; Li, M. Hemostatic materials for wound healing applications. Nat. Rev. Chem. 2021, 5, 773–791. [Google Scholar] [CrossRef]
- Zheng, Y.; Shariati, K.; Ghovvati, M.; Vo, S.; Origer, N.; Imahori, T.; Kaneko, N.; Annabi, N. Hemostatic patch with ultra-strengthened mechanical properties for efficient adhesion to wet surfaces. Biomaterials 2023, 301, 122240. [Google Scholar] [CrossRef]
- Sedlár, M.; Kacvinská, K.; Fohlerová, Z.; Izsák, D.; Chalupová, M.; Suchy, P.; Dohnalová, M.; Sopuch, T.; Vojtová, L. A synergistic effect of fibrous carboxymethyl cellulose with equine collagen improved the hemostatic properties of freeze-dried wound dressings. Cellulose 2023, 30, 11113–11131. [Google Scholar] [CrossRef]
- Al-Mofty, S.E.; Karaly, A.H.; Sarhan, W.A.; Azzazy, H.M.E. Multifunctional Hemostatic PVA/Chitosan Sponges Loaded with Hydroxyapatite and Ciprofloxacin. ACS Omega 2022, 7, 13210–13220. [Google Scholar] [CrossRef]
- Mao, G.Z.; Wang, Z.; Tian, S.Y.; Li, H.Y.; Yang, W.Z. A novel chitosan-hyaluronic acid-pullulan composite film wound dressing for effectively inhibiting bacteria and accelerating wound healing. Mater. Today Commun. 2022, 33, 104801. [Google Scholar] [CrossRef]
- Hossain, S.; Mohanty, S.; Verma, D. Polyelectrolyte complex based nanofibrous aggregates for fast hemostasis. Mater. Today Commun. 2021, 27, 102364. [Google Scholar] [CrossRef]
- Ko, Y.G.; Kim, B.N.; Kim, E.J.; Chung, H.Y.; Park, S.Y.; Kim, Y.J.; Kwon, O.H. Bioabsorbable Carboxymethyl Starch-Calcium Ionic Assembly Powder as a Hemostatic Agent. Polymers 2022, 14, 3909. [Google Scholar] [CrossRef]
- Lee, M.H.; Lee, D.R.; Chon, J.W.; Chung, D.J. Hemostatic Patches Based on Crosslinked Chitosan Films Applied in Interventional Procedures. Polymers 2021, 13, 2402. [Google Scholar] [CrossRef]
- Pourshahrestani, S.; Zeimaran, E.; Djordjevic, I.; Kadri, N.A.; Towler, M.R. Inorganic hemostats: The state-of-the-art and recent advances. Mater. Sci. Eng. C-Mater. Biol. Appl. 2016, 58, 1255–1268. [Google Scholar] [CrossRef]
- Lv, H.Y.; Zhao, M.; Li, Y.R.; Li, K.; Chen, S.J.; Zhao, W.W.; Wu, S.H.; Han, Y.T. Electrospun Chitosan-Polyvinyl Alcohol Nanofiber Dressings Loaded with Bioactive Ursolic Acid Promoting Diabetic Wound Healing. Nanomaterials 2022, 12, 2933. [Google Scholar] [CrossRef]
- Yang, X.X.; Shi, N.; Liu, J.; Cheng, Q.Q.; Li, G.Y.; Lyu, J.; Ma, F.G.; Zhang, X.T. 3D Printed Hybrid Aerogel Gauzes Enable Highly Efficient Hemostasis. Adv. Healthc. Mater. 2023, 12, 2201591. [Google Scholar] [CrossRef]
- Kumar, A.; Han, S.S. PVA-based hydrogels for tissue engineering: A review. Int. J. Polym. Mater. Polym. Biomater. 2017, 66, 159–182. [Google Scholar] [CrossRef]
- Ilyas, R.A.; Sapuan, S.M.; Harussani, M.M.; Hakimi, M.; Haziq, M.Z.M.; Atikah, M.S.N.; Asyraf, M.R.M.; Ishak, M.R.; Razman, M.R.; Nurazzi, N.M.; et al. Polylactic Acid (PLA) Biocomposite: Processing, Additive Manufacturing and Advanced Applications. Polymers 2021, 13, 1326. [Google Scholar] [CrossRef]
- Agarwal, Y.; Rajinikanth, P.S.; Ranjan, S.; Tiwari, U.; Balasubramnaiam, J.; Pandey, P.; Arya, D.K.; Anand, S.; Deepak, P. Curcumin loaded polycaprolactone-/polyvinyl alcohol-silk fibroin based electrospun nanofibrous mat for rapid healing of diabetic wound: An in-vitro and in-vivo studies. Int. J. Biol. Macromol. 2021, 176, 376–386. [Google Scholar] [CrossRef]
- Lin, M.G.; Shen, J.L.; Qian, Q.A.; Li, T.; Zhang, C.Y.; Qi, H. Fabrication of Poly(Lactic Acid)@TiO2 Electrospun Membrane Decorated with Metal–Organic Frameworks for Efficient Air Filtration and Bacteriostasis. Polymers 2024, 16, 889. [Google Scholar] [CrossRef]
- Bi, H.Y.; Feng, T.Y.; Li, B.B.; Han, Y.C. In Vitro and In Vivo Comparison Study of Electrospun PLA and PLA/PVA/SA Fiber Membranes for Wound Healing. Polymers 2020, 12, 839. [Google Scholar] [CrossRef]
- Kamoun, E.A.; Loutfy, S.A.; Hussein, Y.; Kenawy, E.S. Recent advances in PVA-polysaccharide based hydrogels and electrospun nanofibers in biomedical applications: A review. Int. J. Biol. Macromol. 2021, 187, 755–768. [Google Scholar] [CrossRef]
- Ji, Y.; Song, W.; Xu, L.; Yu, D.-G.; Bligh, S.W.A. A Review on Electrospun Poly(amino acid) Nanofibers and Their Applications of Hemostasis and Wound Healing. Biomolecules 2022, 12, 794. [Google Scholar] [CrossRef]
- Yang, Y.; Du, Y.; Zhang, J.; Zhang, H.; Guo, B. Structural and Functional Design of Electrospun Nanofibers for Hemostasis and Wound Healing. Adv. Fiber Mater. 2022, 4, 1027–1057. [Google Scholar] [CrossRef]
- Rangel, E.C.; Bento, W.C.A.; Kayama, M.E.; Schreiner, W.H.; Cruz, N.C. Enhancement of polymer hydrophobicity by SF6 plasma treatment and argon plasma immersion ion implantation. Surf. Interface Anal. 2003, 35, 179–183. [Google Scholar] [CrossRef]
- Vesel, A.; Mozetic, M. New developments in surface functionalization of polymers using controlled plasma treatments. J. Phys. D-Appl. Phys. 2017, 50, 293001. [Google Scholar] [CrossRef]
- Firoozi, M.; Entezam, M.; Masaeli, E.; Ejeian, F.; Nasr-Esfahani, M.H. Physical modification approaches to enhance cell supporting potential of poly (vinyl alcohol)-based hydrogels. J. Appl. Polym. Sci. 2022, 139, 51485. [Google Scholar] [CrossRef]
- Li, J.; Niu, J.; Kim, Y.; Chae, H. Surface wettability control and fluorination modeling of amorphous carbon films fluorinated with CF4 plasma. Appl. Surf. Sci. 2023, 635, 157668. [Google Scholar] [CrossRef]
- Mai, Z.R.; Liu, Q.L.; Bian, Y.S.; Wang, P.; Fu, X.W.; Lin, D.S.; Kong, N.Z.; Huang, Y.Q.; Zeng, Z.J.; Li, D.F.; et al. PCL/Collagen/UA Composite Biomedical Dressing with Ordered Microfiberous Structure Fabricated by a 3D Near-Field Electrospinning Process. Polymers 2023, 15, 223. [Google Scholar] [CrossRef]
- Guo, J.Y.; Liu, Q.; Cheng, J.; Fu, X.; Zhang, Y.C.; Yang, H. Hemostatic cotton based on biocompatible poly(vinyl alcohol)/soluble starch-fish skin collagen composites. Mater. Today Commun. 2022, 32, 103812. [Google Scholar] [CrossRef]
- Laput, O.A.; Vasenina, I.V.; Korzhova, A.G.; Bryuzgina, A.A.; Khomutova, U.V.; Tuyakova, S.G.; Akhmadeev, Y.H.; Shugurov, V.V.; Bolbasov, E.N.; Tverdokhlebov, S.I.; et al. Effect of Nitrogen Arc Discharge Plasma Treatment on Physicochemical Properties and Biocompatibility of PLA-Based Scaffolds. Polymers 2023, 15, 3381. [Google Scholar] [CrossRef]
- Laput, O.A.; Vasenina, I.V.; Shapovalova, Y.G.; Ochered’ko, A.N.; Chernyavskii, A.V.; Kudryashov, S.V.; Kurzina, I.A. Low-Temperature Barrier Discharge Plasma Modification of Scaffolds Based on Polylactic Acid. ACS Appl. Mater. Interfaces 2022, 14, 41742–41750. [Google Scholar] [CrossRef]
- Can-Herrera, L.A.; Oliva, A.I.; Cervantes-Uc, J.M. Enhancement of chemical, physical, and surface properties of electrospun PCL/PLA blends by means of air plasma treatment. Polym. Eng. Sci. 2022, 62, 1608–1618. [Google Scholar] [CrossRef]
- Thongsomboon, W.; Srihanam, P.; Baimark, Y. Preparation of flexible poly(L-lactide)-b-poly(ethylene glycol)-b-poly (L-lactide)/talcum/thermoplastic starch ternary composites for use as heat-resistant and single-use bioplastics. Int. J. Biol. Macromol. 2023, 230, 123172. [Google Scholar] [CrossRef]
- Savoji, H.; Lerouge, S.; Ajji, A.; Wertheimer, M.R. Plasma-Etching for Controlled Modification of Structural and Mechanical Properties of Electrospun PET Scaffolds. Plasma Process. Polym. 2015, 12, 314–327. [Google Scholar] [CrossRef]
- Cai, Z.S.; Qiu, Y.P. The mechanism of air/oxygen/helium atmospheric plasma action on PVA. J. Appl. Polym. Sci. 2006, 99, 2233–2237. [Google Scholar] [CrossRef]
- Ghobeira, R.; Tabaei, P.S.E.; Morent, R.; De Geyter, N. Chemical characterization of plasma-activated polymeric surfaces via XPS analyses: A review. Surf. Interfaces 2022, 31, 102087. [Google Scholar] [CrossRef]
- Paneru, R.; Ki, S.H.; Lamichhane, P.; Nguyen, L.N.; Adhikari, B.C.; Jeong, I.J.; Mumtaz, S.; Choi, J.; Kwon, J.S.; Choi, E.H. Enhancement of antibacterial and wettability performances of polyvinyl alcohol/chitosan film using non-thermal atmospheric pressure plasma. Appl. Surf. Sci. 2020, 532, 147339. [Google Scholar] [CrossRef]
- Rao, X.; Zhou, Q.; Wen, Q.; Ou, Z.; Fu, L.; Gong, Y.; Du, X.; Huo, C. High-Performance and Water Resistant PVA-Based Films Modified by Air Plasma Treatment. Membranes 2022, 12, 249. [Google Scholar] [CrossRef]
- Tifui, G.; Dobromir, M.; Sirghi, L. Stiffening of polydimethylsiloxane surface as result of exposure to low-pressure argon discharge plasma. Plasma Process. Polym. 2023, 20, 2300014. [Google Scholar] [CrossRef]
- Rufato, K.B.; Veregue, F.R.; Medeiro, R.d.P.; Francisco, C.B.; Souza, P.R.; Popat, K.C.; Kipper, M.J.; Martins, A.F. Electrospinning of poly(vinyl alcohol) and poly(vinyl alcohol)/tannin solutions: A critical viewpoint about crosslinking. Mater. Today Commun. 2023, 35, 106271. [Google Scholar] [CrossRef]
- Rogojanu, A.; Rusu, E.; Dorohoi, D.O. Characterization of Structural Modifications Induced on Poly(Vinyl Alcohol) Surface by Atmospheric Pressure Plasma. Int. J. Polym. Anal. Charact. 2010, 15, 210–221. [Google Scholar] [CrossRef]
- Szewczyk, P.K.; Ura, D.P.; Metwally, S.; Knapczyk-Korczak, J.; Gajek, M.; Marzec, M.M.; Bernasik, A.; Stachewicz, U. Roughness and Fiber Fraction Dominated Wetting of Electrospun Fiber-Based Porous Meshes. Polymers 2019, 11, 34. [Google Scholar] [CrossRef]
- Ojah, N.; Saikia, D.; Gogoi, D.; Baishya, P.; Ahmed, G.A.; Ramteke, A.; Choudhury, A.J. Surface modification of core-shell silk/PVA nanofibers by oxygen dielectric barrier discharge plasma: Studies of physico-chemical properties and drug release behavior. Appl. Surf. Sci. 2019, 475, 219–229. [Google Scholar] [CrossRef]
- Das, P.; Ojah, N.; Kandimalla, R.; Mohan, K.; Gogoi, D.; Dolui, S.K.; Choudhury, A.J. Surface modification of electrospun PVA/chitosan nanofibers by dielectric barrier discharge plasma at atmospheric pressure and studies of their mechanical properties and biocompatibility. Int. J. Biol. Macromol. 2018, 114, 1026–1032. [Google Scholar] [CrossRef]
- Ojah, N.; Borah, R.; Ahmed, G.A.; Mandal, M.; Choudhury, A.J. Surface modification of electrospun silk/AMOX/PVA nanofibers by dielectric barrier discharge plasma: Physiochemical properties, drug delivery and in-vitro biocompatibility. Prog. Biomater. 2020, 9, 219–237. [Google Scholar] [CrossRef]
- Paneru, R.; Lamichhane, P.; Adhikari, B.C.; Ki, S.H.; Choi, J.; Kwon, J.S.; Choi, E.H. Surface modification of PVA thin film by nonthermal atmospheric pressure plasma for antifogging property. AIP Adv. 2019, 9, 075008. [Google Scholar] [CrossRef]
- Watson, S.; Pattyn, C.; Garakani, M.M.; Ajji, A.; Reuter, S.; Wertheimer, M.R. Wetting and aging behaviors for several O2 and NH3 plasma treated nanofibrous and flat film polymer materials: A comparison. Plasma Process. Polym. 2023, 20, e2200224. [Google Scholar] [CrossRef]
- Fu, Q.; Jin, Y.; Song, X.F.; Gao, J.Y.; Han, X.B.; Jiang, X.Y.; Zhao, Q.; Yu, D.P. Size-dependent mechanical properties of PVA nanofibers reduced via air plasma treatment. Nanotechnology 2010, 21, 095703. [Google Scholar] [CrossRef]
- Zhao, C.; Zhang, X.; Jiang, A.; Pan, Z. Adhesion and protective properties of polyvinyl alcohol nanofibrous composite fabrics. J. Text. Inst. 2018, 109, 1263–1269. [Google Scholar] [CrossRef]
- Ye, T.; Yang, Z.Y.; Hao, R.L.; Guo, J.N.; Dou, G.F.; Meng, Z.Y.; Liu, S.C.; Gu, R.L.; Wu, Z.N.; Sun, Y.B.; et al. Highly Efficient Hemostatic Cross-Linked Polyacrylate Polymer Dressings for Immediate Hemostasis. Polymers 2024, 16, 863. [Google Scholar] [CrossRef]
- Wang, Y.; Zhai, W.; Cheng, S.; Li, J.; Zhang, H. Surface-functionalized design of blood-contacting biomaterials for preventing coagulation and promoting hemostasis. Friction 2023, 11, 1371–1394. [Google Scholar] [CrossRef]
- Cheng, C.; Peng, X.; Xi, L.; Wan, C.; Shi, S.; Wang, Y.; Yu, X. An agar-polyvinyl alcohol hydrogel loaded with tannic acid with efficient hemostatic and antibacterial capacity for wound dressing. Food Funct. 2022, 13, 9622–9634. [Google Scholar] [CrossRef]
- John, J.V.; McCarthy, A.; Karan, A.; Xie, J.W. Electrospun Nanofibers for Wound Management. Chemnanomat 2022, 8, e202100349. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ge, X.; Zhang, L.; Wei, X.; Long, X.; Han, Y. Plasma Surface Treatment and Application of Polyvinyl Alcohol/Polylactic Acid Electrospun Fibrous Hemostatic Membrane. Polymers 2024, 16, 1635. https://doi.org/10.3390/polym16121635
Ge X, Zhang L, Wei X, Long X, Han Y. Plasma Surface Treatment and Application of Polyvinyl Alcohol/Polylactic Acid Electrospun Fibrous Hemostatic Membrane. Polymers. 2024; 16(12):1635. https://doi.org/10.3390/polym16121635
Chicago/Turabian StyleGe, Xiaotian, Li Zhang, Xuanhe Wei, Xi Long, and Yingchao Han. 2024. "Plasma Surface Treatment and Application of Polyvinyl Alcohol/Polylactic Acid Electrospun Fibrous Hemostatic Membrane" Polymers 16, no. 12: 1635. https://doi.org/10.3390/polym16121635
APA StyleGe, X., Zhang, L., Wei, X., Long, X., & Han, Y. (2024). Plasma Surface Treatment and Application of Polyvinyl Alcohol/Polylactic Acid Electrospun Fibrous Hemostatic Membrane. Polymers, 16(12), 1635. https://doi.org/10.3390/polym16121635






