Coating Methods of Carbon Nonwovens with Cross-Linked Hyaluronic Acid and Its Conjugates with BMP Fragments
Abstract
1. Introduction
2. Materials and Methods
2.1. Cross-Linking Process Choosing an Optimal Procedure
2.1.1. Cross-Linking of HA with 1,4-diaminobutane
2.1.2. Cross-Linking of HA with Citric Acid Procedure I
2.1.3. Cross-Linking of HA with Citric Acid Procedure II
2.1.4. Cross-Linking of HA with BDDE
2.2. Cross-Linking of HA on the Carbon Nonwoven Fabric
2.2.1. Cross-Linking of HA on the Carbon Nonwoven Fabric Procedure with BDDE
2.2.2. Cross-Linking of HA on the Carbon Nonwoven Fabric Procedure with CA
2.3. Synthesis of the Polysaccharide–Peptide Conjugate
2.3.1. Synthesis of BMP2 (241-250) Peptide Fragment H-KRMVRISRSL-OH
2.3.2. Synthesis of BMP9 (361-370) Peptide Fragment H-FFPLADDVTP-OH
2.3.3. Chemical Modification of HA with BMP2 (241-250) Peptide Fragment H-KRMVRISRSL-OH by Using EDC and NHS
2.3.4. Chemical Modification of HA with BMP9 (361-370) Peptide Fragment H-FFPLADDVTP-OH by Using Triazine Based Coupling Reagent
2.4. Synthesis of the Hybrid Material—Carbon Nonwoven Fabric Coated by the Conjugates of HA and BMP Fragments
2.4.1. Layer-by-Layer Method—Physical Binding of the Peptide
2.4.2. Using Polysaccharide–Peptide Conjugate Chemical Bond between PEPTIDE and HA
2.5. Analytical Techniques
2.5.1. MALDI-TOF MS
2.5.2. 1H NMR
2.5.3. FT-IR
3. Results and Discussion
3.1. Choosing the Most Effective HA Cross-Linking Method
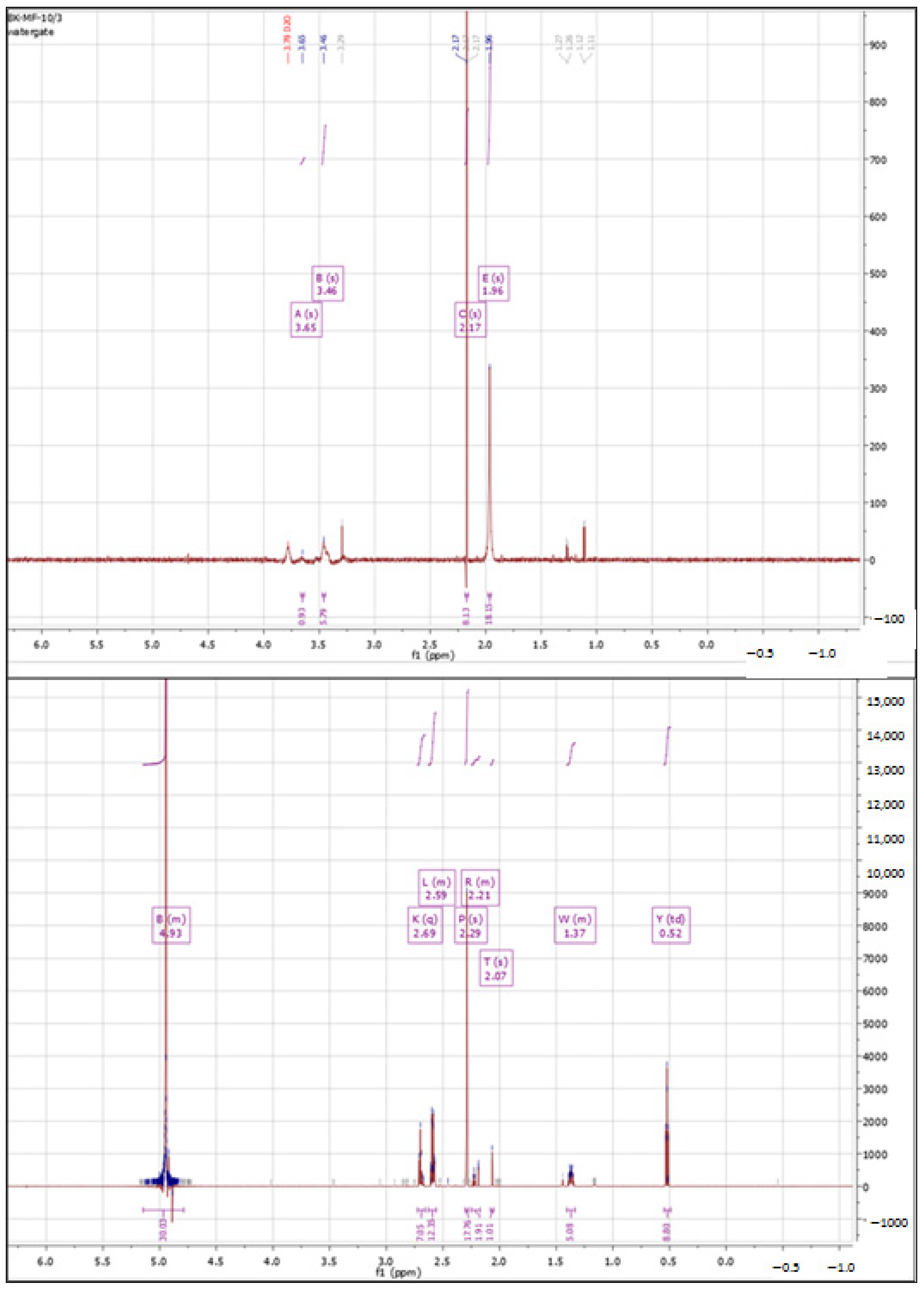
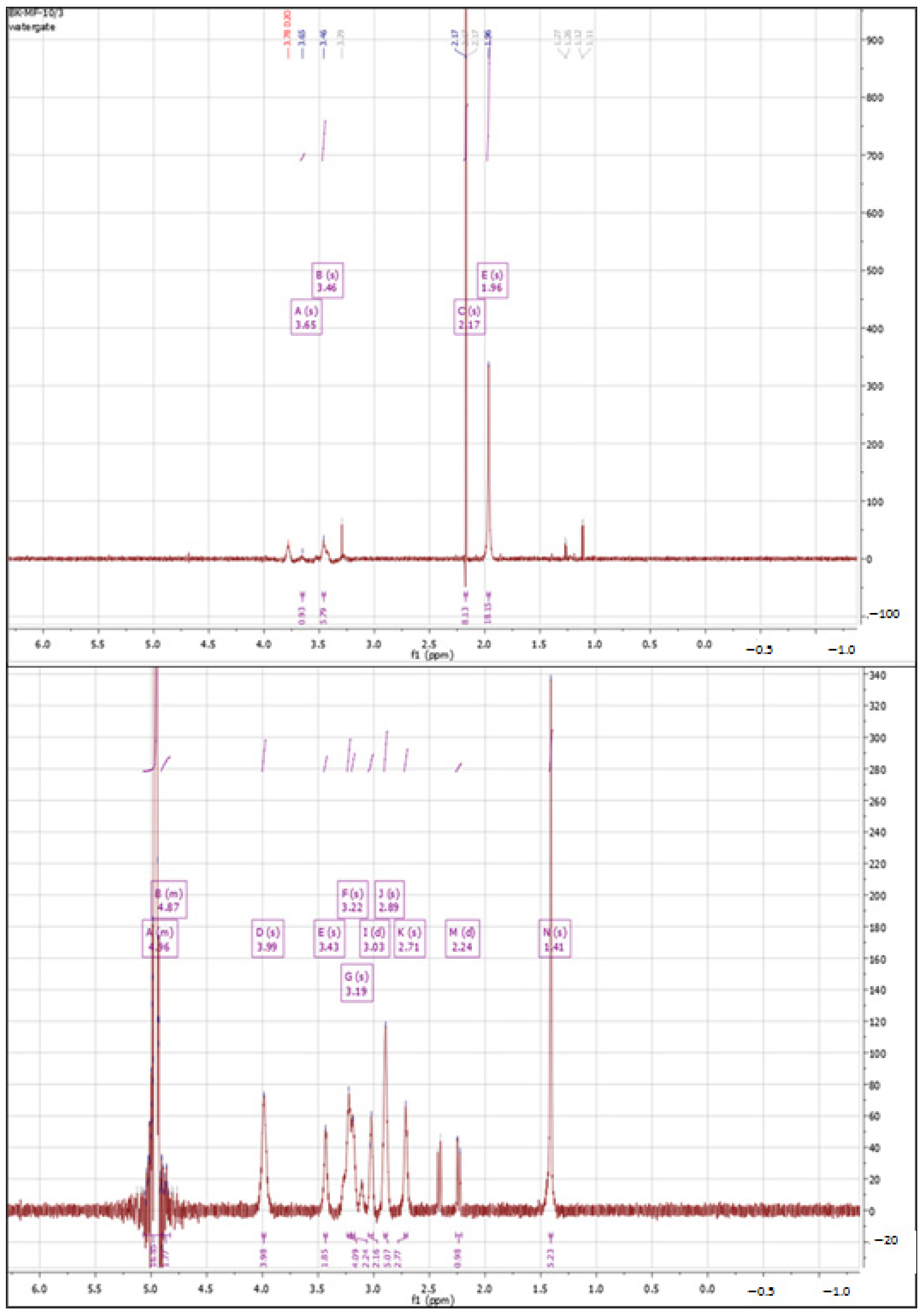
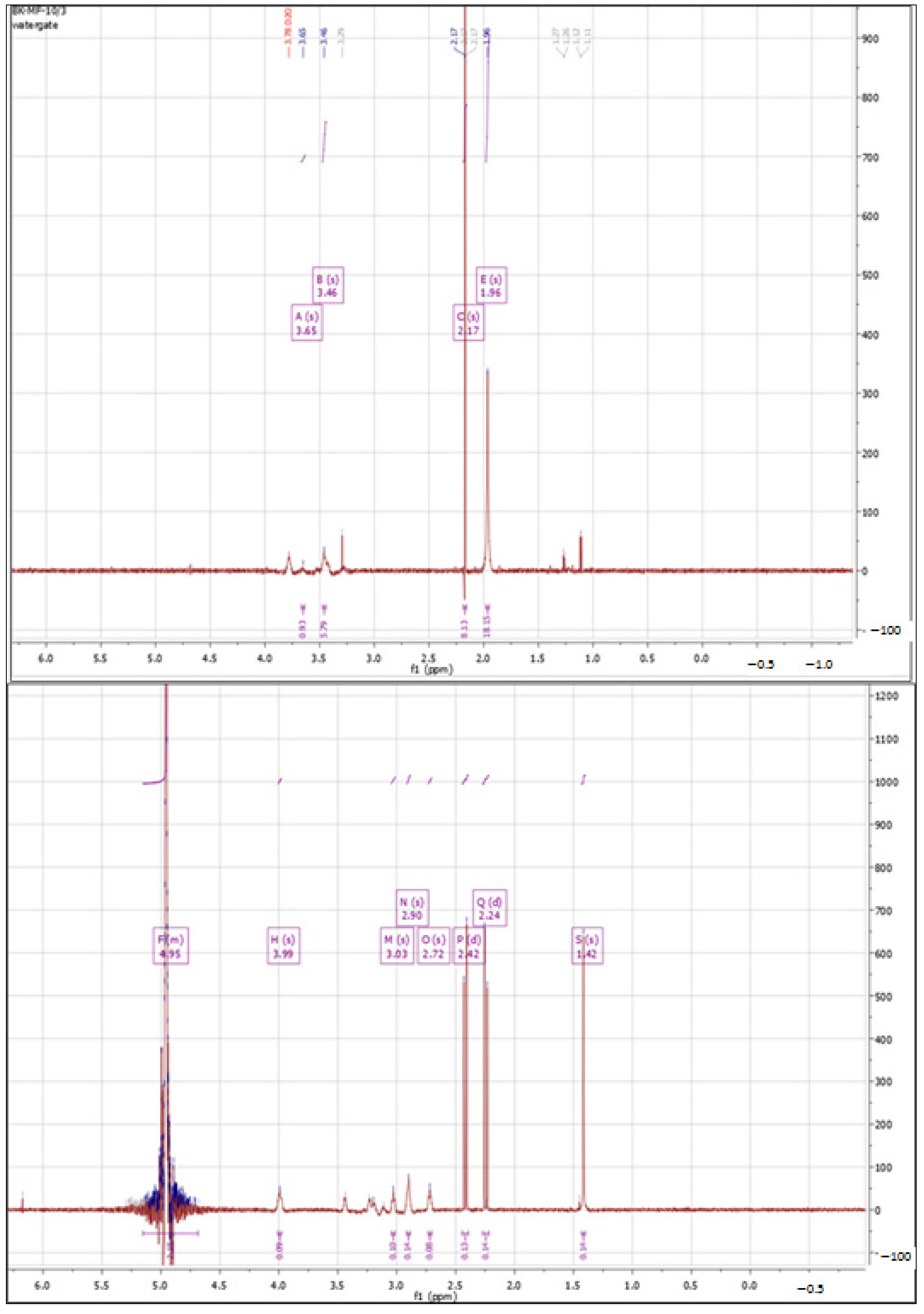
3.1.1. 1H NMR Spectra Analysis
Cross-Linking with 1,4-diaminobutane
Cross-Linking with Citric Acid
Cross-Linking with BDDE
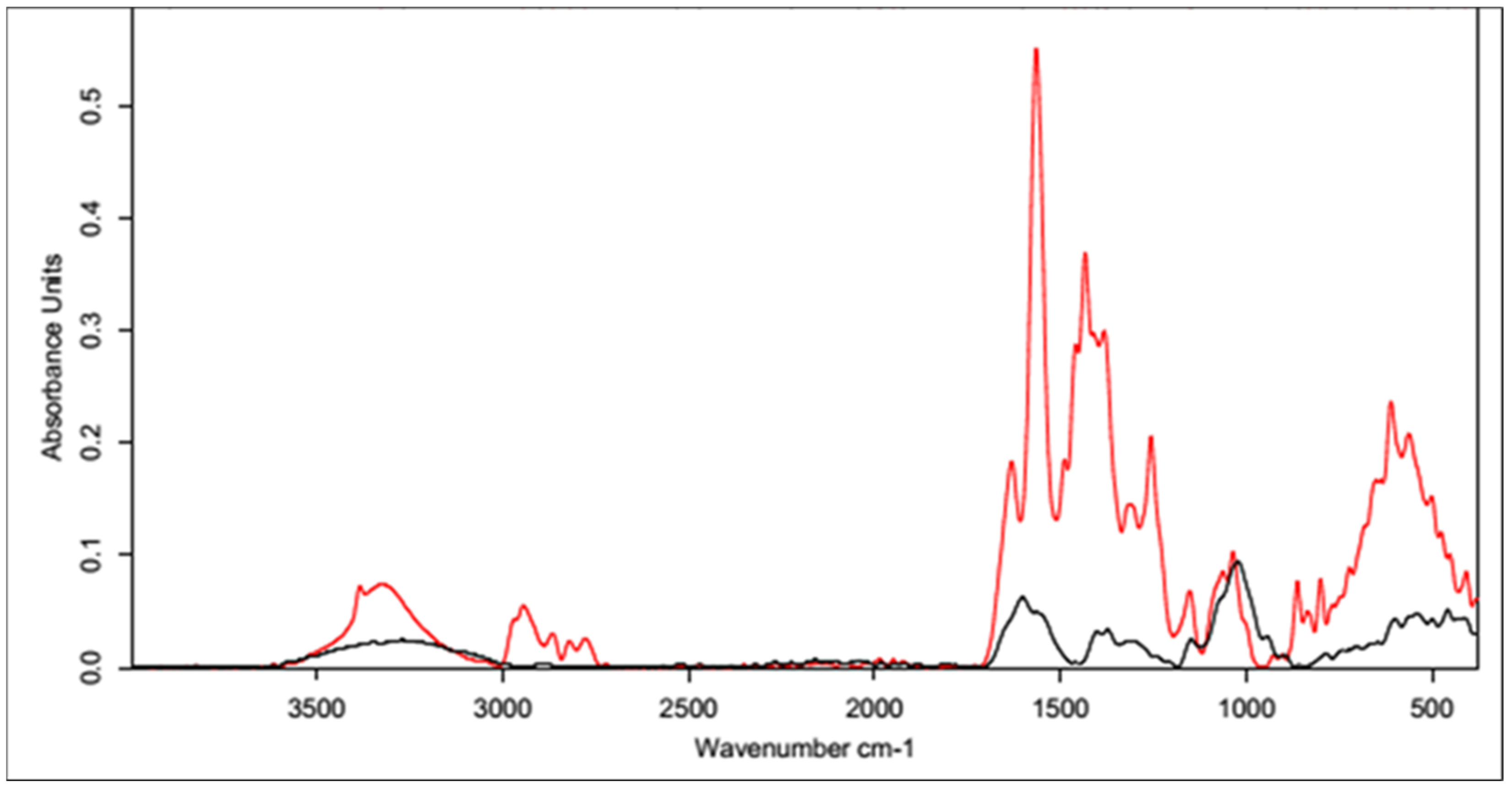
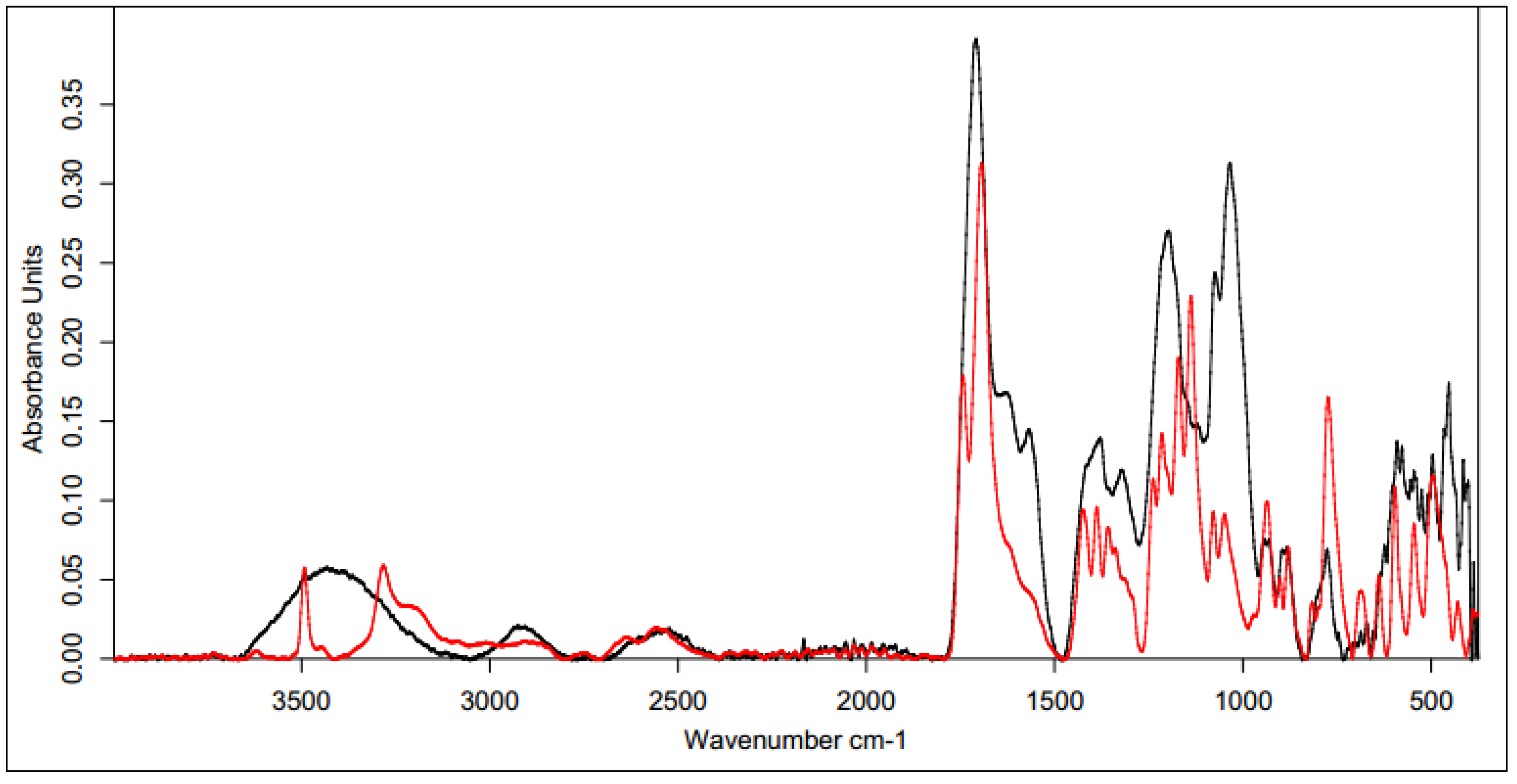
3.1.2. IR Spectra Analysis
Cross-Linking with 1,4-diaminobutane
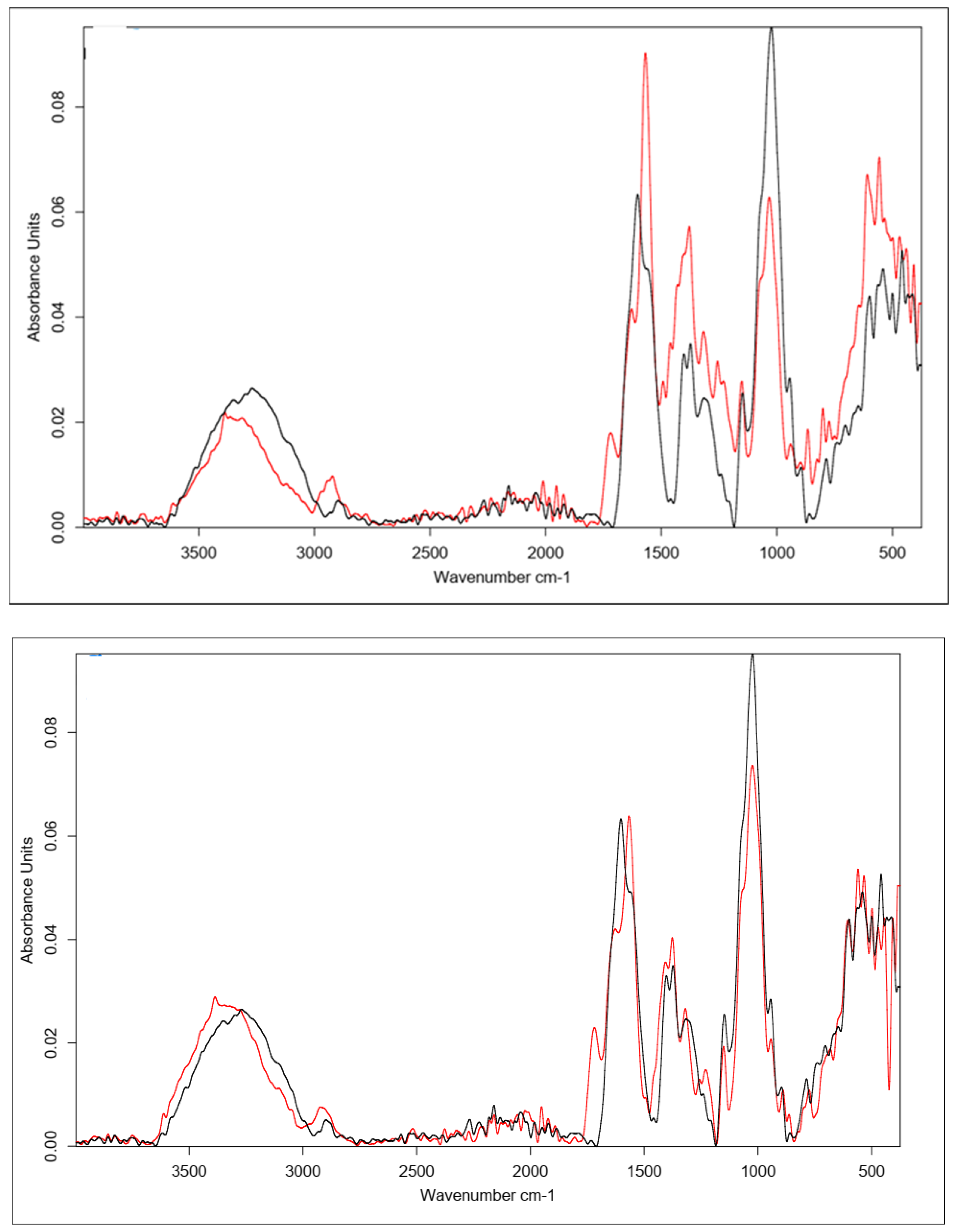
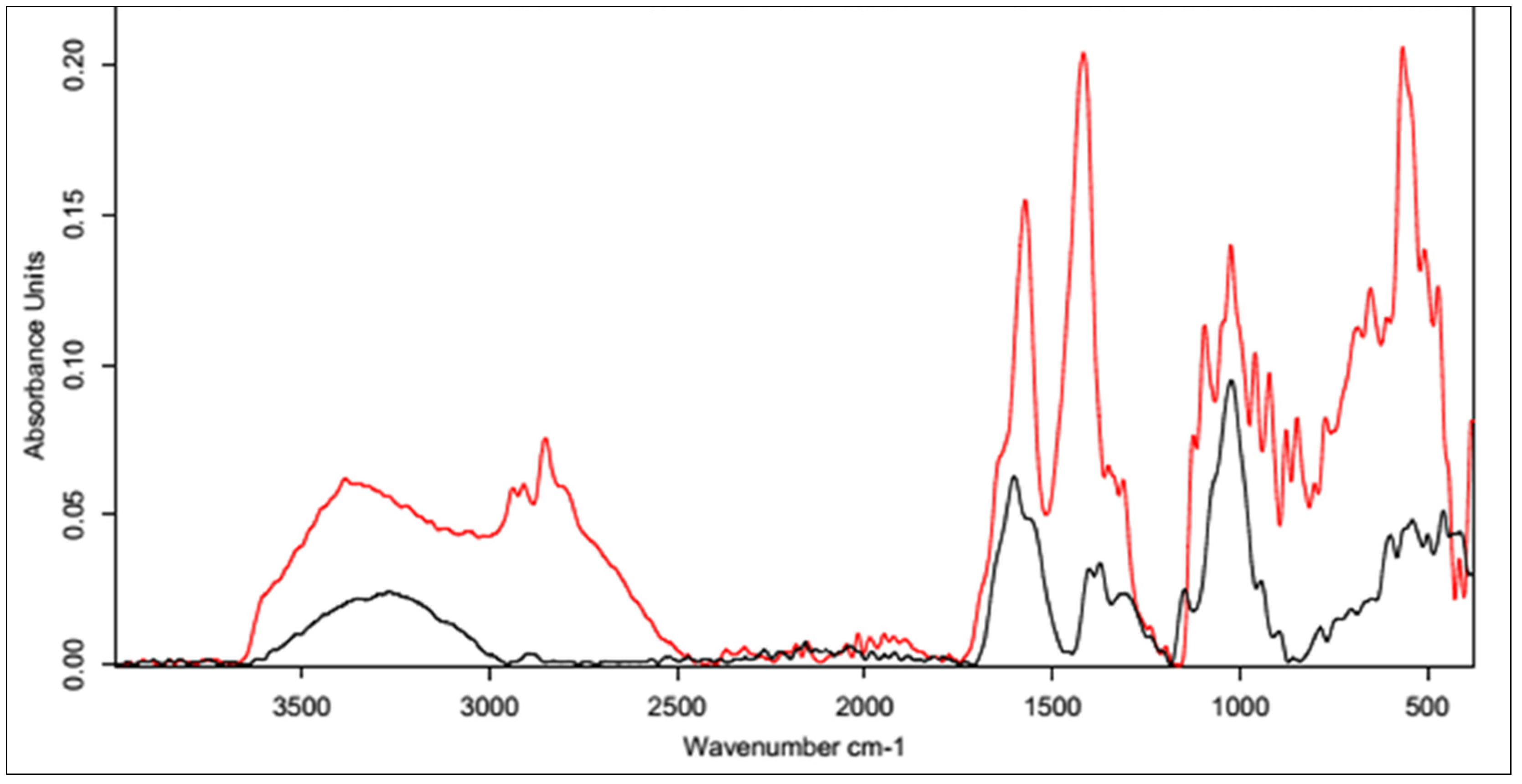
Cross-Linking with Citric Acid
Cross-Linking with BDDE
3.2. Transfer Optimal Method for Cross-Linking into the Procedure of the Surface Functionalization of Carbon Nonwoven Fabric
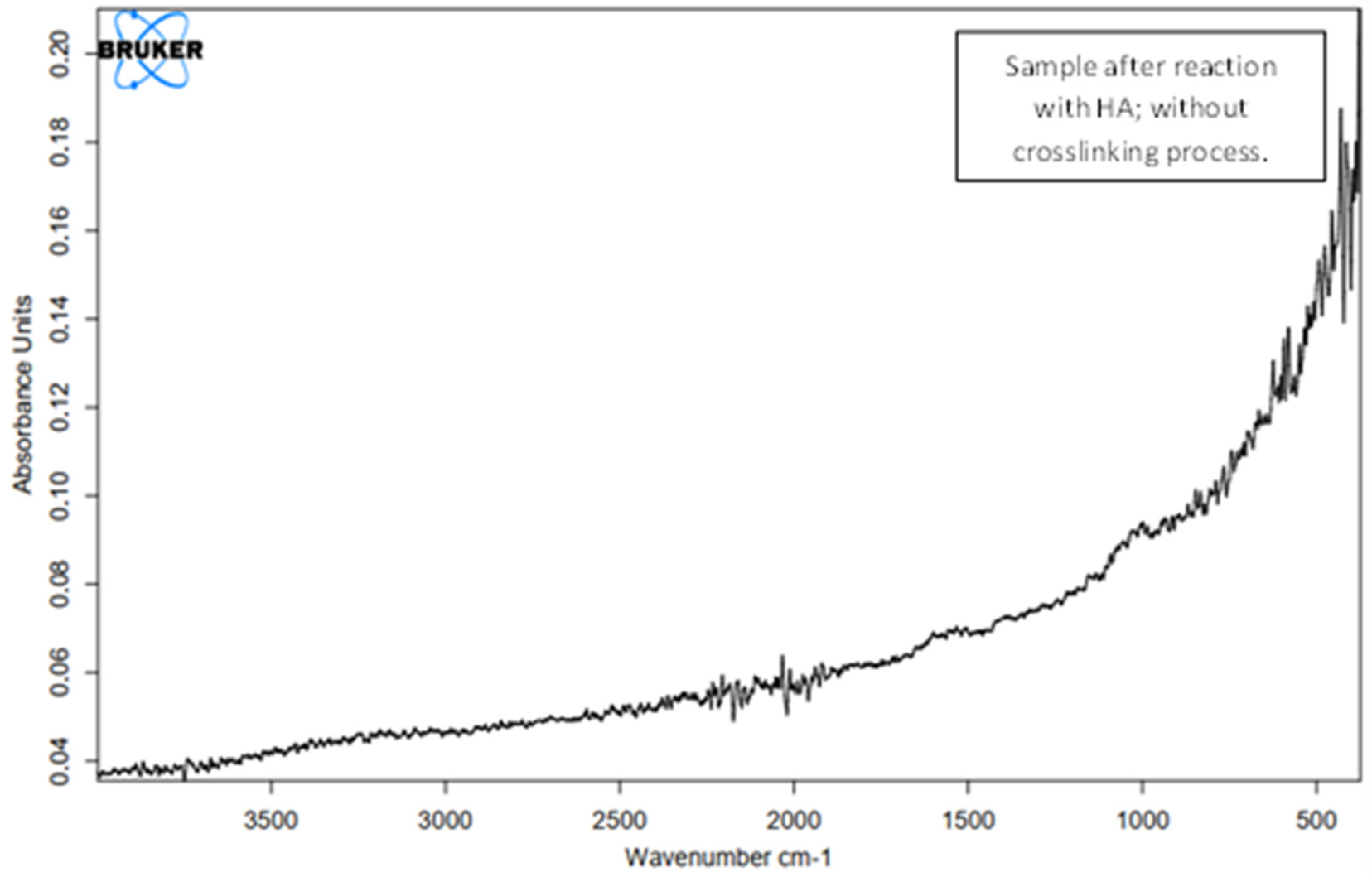
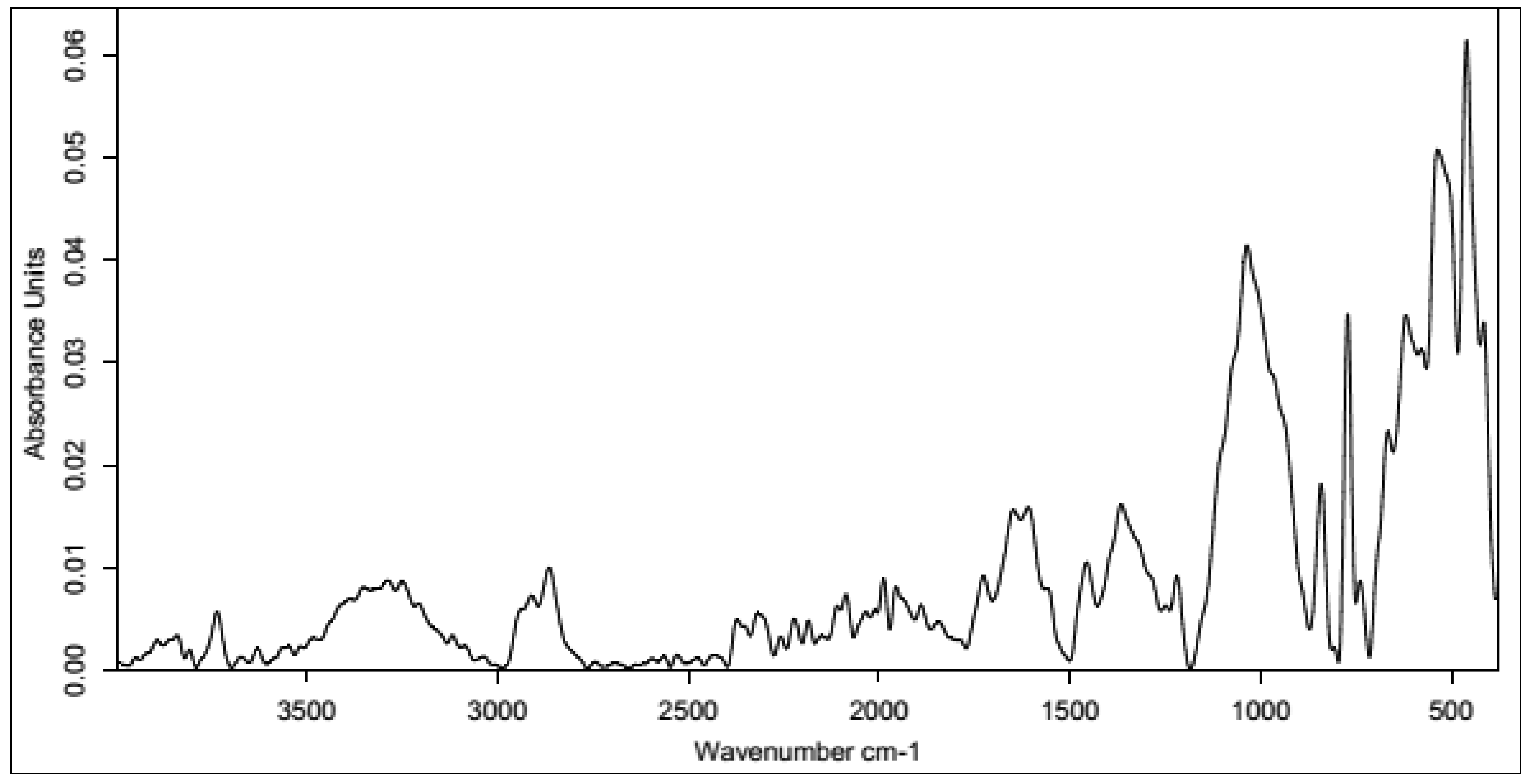
3.2.1. Unmodified HA
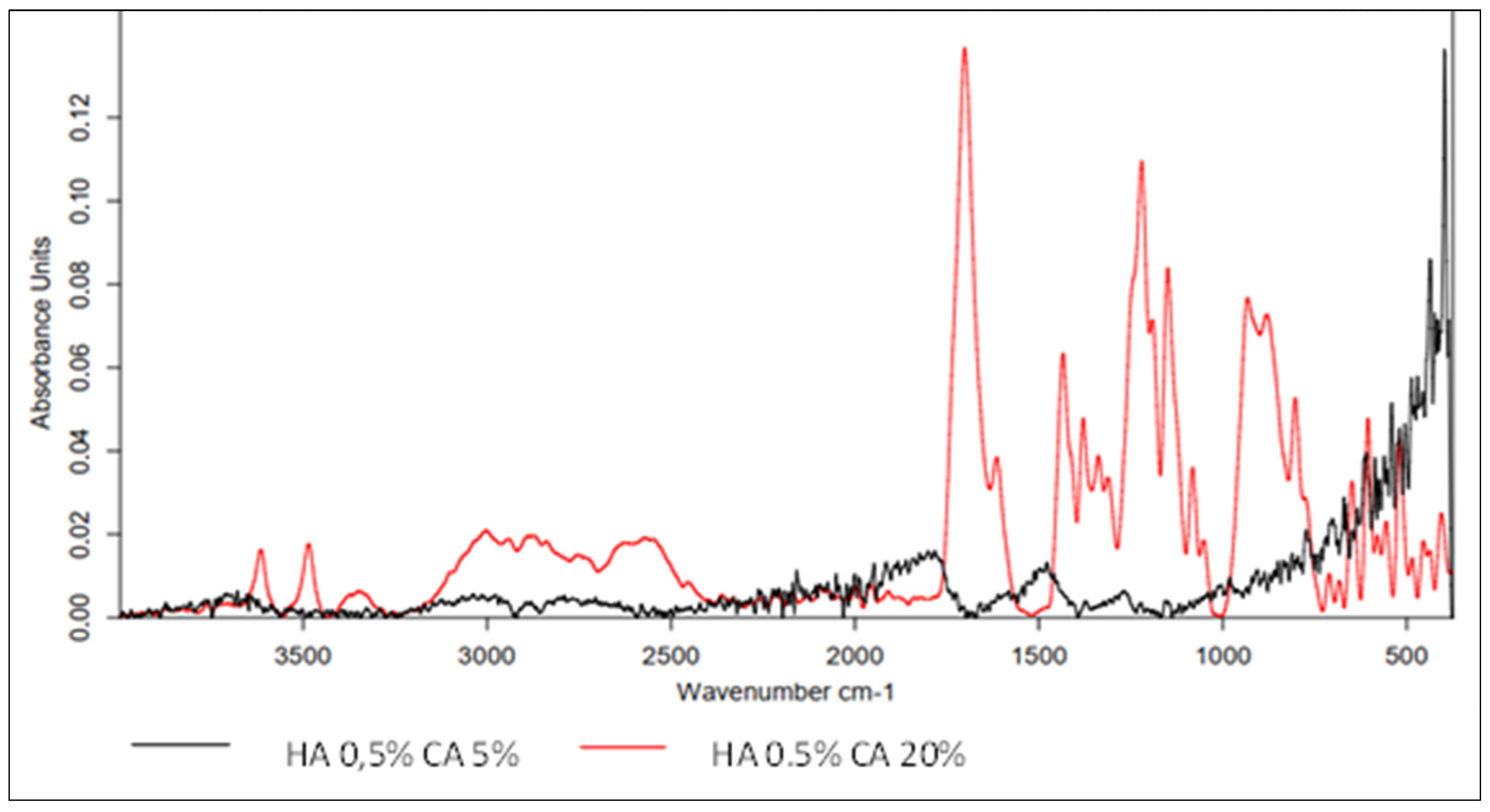
3.2.2. CA-Cross-Linked Hyaluronic Acid
- Band at 1701 cm−1 corresponding to C=O stretching vibrations from the carboxyl group;
- Characteristic peaks of 1434 cm−1 and 1379 cm−1 originating from -OH and C-O-C, respectively;
- Peak at 1311 cm−1 originating from C-O bonds, confirming the cross-linking of HA;
- Low-intensity peaks in the 3600–3000 cm−1 range, indicating the use of oxygen groups during the cross-linking process.
3.2.3. Cross-Linked HA with BDDE
3.3. Attempts to Synthesize Covalent Conjugates of BMP Fragments with HA
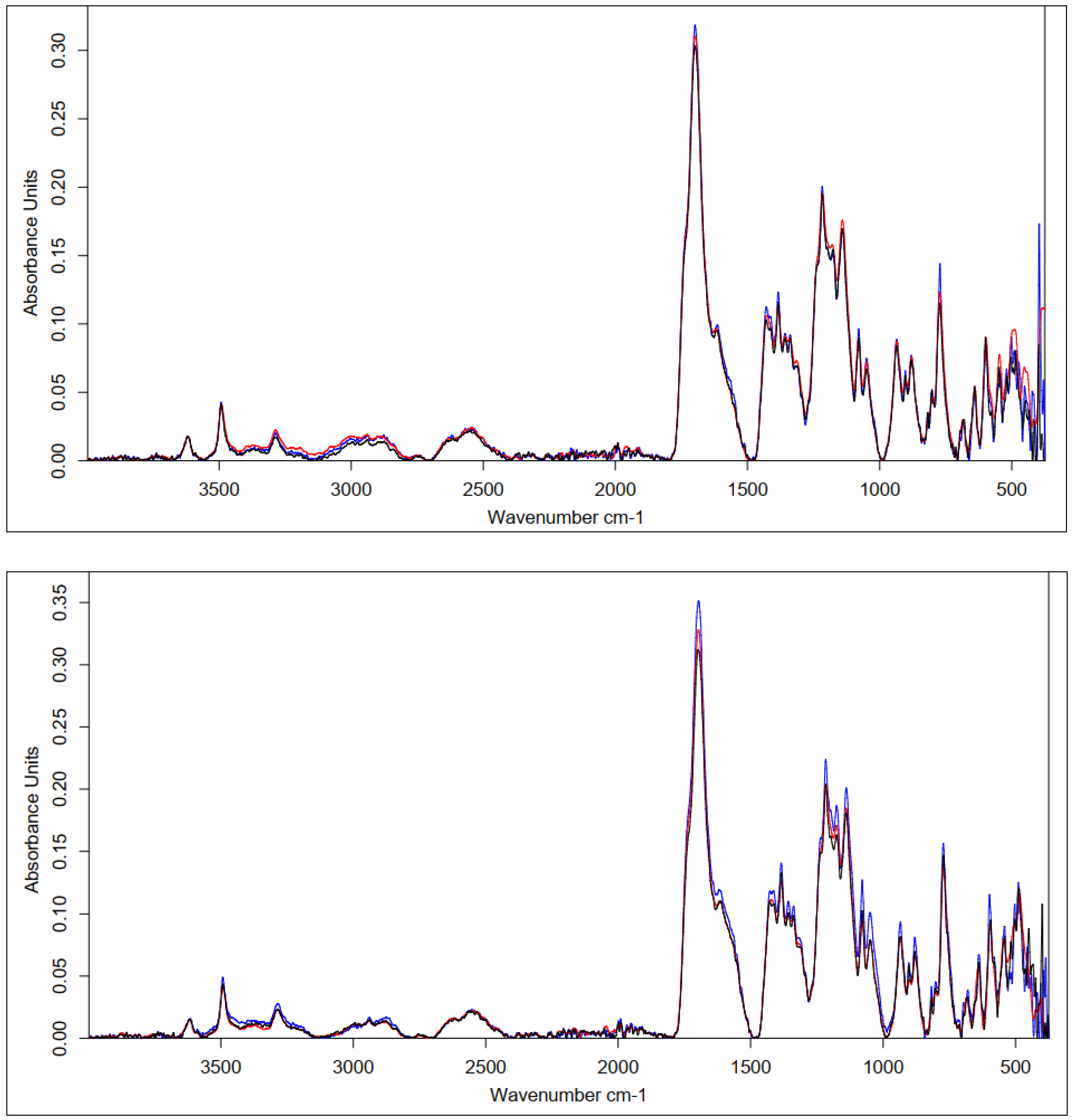
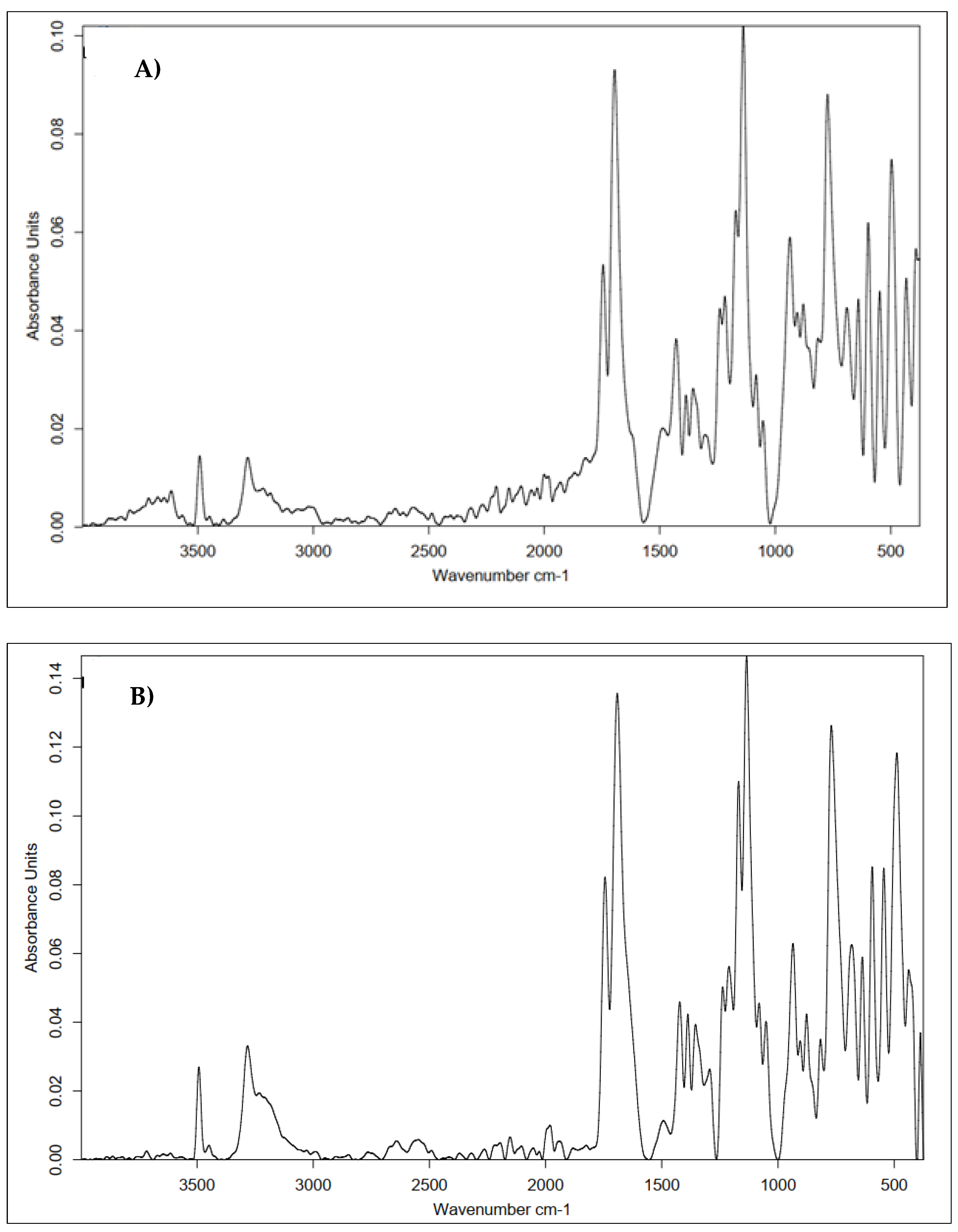
3.3.1. BMP2 (241-250) Peptide Fragment H-KRMVRISRSL-OH
- The shape of the spectrum obtained for the used peptide was characterized by the highest intensities of the individual bands. A decrease in the absorbance values of the conjugate bands in the region of 1700 cm−1 (C=O carbonyl vibrations) and about 1300 cm−1 (C-O vibrations) indicated the formation of a bond with hyaluronic acid.
- There was a decrease in the absorbance value of the characteristic 3500–3000 cm−1 band derived from native hyaluronan, indicating that the carboxyl groups of the acid were used to form an amide bond with the peptide.
- There was an increase in the intensity of the bands at 1700 cm−1 when comparing pure HA to the conjugate. This was due to the incorporation into the structure of the acid, the polypeptide chain, and the formation of an amide bond between them.
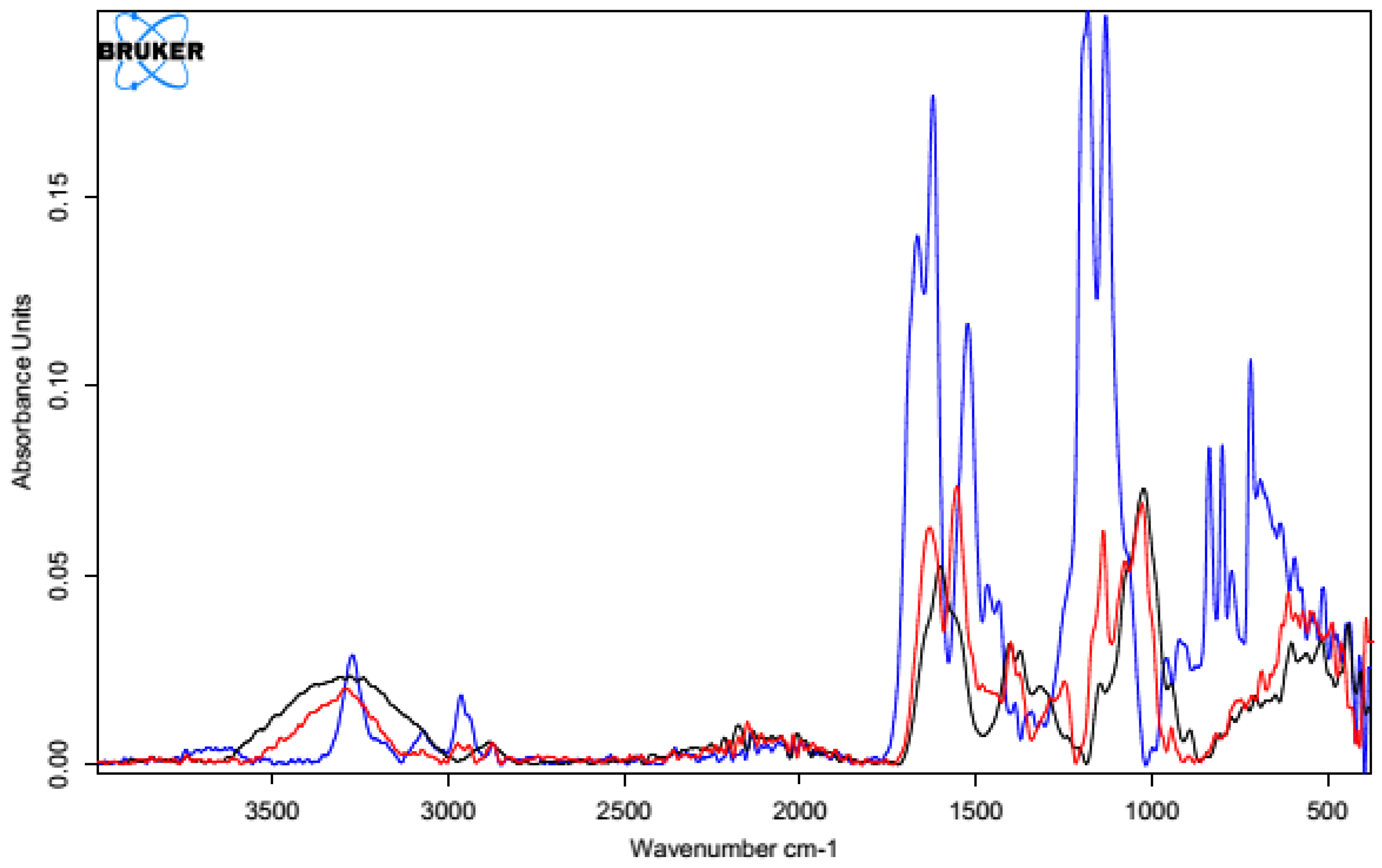
3.3.2. BMP9 (361-370) Peptide Fragment H-FFPLADDVTP-OH
- The shape of the spectrum obtained for the pure peptide was similar to the shape of the spectrum of the polysaccharide–peptide conjugate. The reductions in the absorbance values of the bands in the regions of 1700–1600 cm−1 (C=O carbonyl vibrations) and about 1300 cm−1 (C-O vibrations) indicated the formation of an ester bond with hyaluronic acid.
- There was a shift in the characteristic signal of 3500–3000 cm−1 from native hyaluronan towards lower values (about 3100–2900 cm−1), which indicated the use of carboxyl groups of the acid to form an ester bond with the peptide.
- There was a significant increase in band intensity at 1700 cm−1 compared with pure HA. This was due to the facts that the polypeptide chain was incorporated into the acid structure and an amide bond was formed between them.
3.4. Attempts to Synthesize Hybrid Materials Based on HA-Coated Carbon Nonwoven and a Biologically Active Fragment of BMP
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, W.; Liu, Y.; Xie, Z. Gecko-Like Dry Adhesive surfaces and their applications: A review. J. Bionic Eng. 2021, 18, 1011–1044. [Google Scholar] [CrossRef]
- Kim, B.S.; Kim, M.K.; Cho, Y.; Hamed, E.E.; Gillette, M.U.; Cha, H.; Miljkovic, N.; Aakalu, V.K.; Kang, K.; Son, K.-N.; et al. Electrothermal soft manipulator enabling safe transport and handling of thin cell/tissue sheets and bioelectronic devices. Sci. Adv. 2020, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Jurewicz, I.; King, A.A.K.; Shanker, R.; Large, M.J.; Smith, R.J.; Maspero, R.; Ogilvie, S.P.; Scheerder, J.; Han, J.; Backes, C.; et al. Mechanochromic and thermochromic sensors based on graphene infused polymer opals. Adv. Funct. Mater. 2020, 30, 2002473. [Google Scholar] [CrossRef]
- Weissmann, B.; Meyer, K. The structure of hyaluronic acid and of hyaluronic acid from umbilical cord. J. Am. Chem. Soc. 1954, 76, 1753–1757. [Google Scholar] [CrossRef]
- Lim, S.T.; Forbes, B.; Berry, D.J.; Martin, G.P.; Brown, M.B. In vivo evaluation of novel hyaluronan/chitosan microparticulate delivery systems for the nasal delivery of gentamicin in rabbits. Int. J. Pharm. 2002, 231, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Kim, H.; Park, Y.; Kong, W.H.; Lee, S.W.; Kwok, S.J.J.; Hahn, S.K.; Yun, S.H. Noninvasive transdermal vaccination using hyaluronan nanocarriers and laser adjuvant. Adv. Funct. Mater. 2016, 26, 2512–2522. [Google Scholar] [CrossRef]
- Yang, H.; Song, L.; Zou, Y.; Sun, D.; Wang, L.; Yu, Z.; Guo, J. Role of hyaluronic acids and potential as regenerative biomaterials in wound healing. ACS Appl. Bio Mater. 2020, 4, 311–324. [Google Scholar] [CrossRef]
- Tolg, C.; Telmer, P.; Turley, E. Specific sizes of hyaluronan oligosaccharides stimulate fibroblast migration and excisional wound repair. PLoS ONE 2014, 9, 88479. [Google Scholar] [CrossRef]
- Gariboldi, S.; Palazzo, M.; Zanobbio, L.; Selleri, S.; Sommariva, M.; Sfondrini, L.; Cavicchini, S.; Balsari, A.; Rumio, C. Low molecular weight hyaluronic acid increases the self-defense of skin epithelium by induction of β-Defensin 2 via TLR2 and TLR4. J. Immunol. 2008, 181, 2103–2110. [Google Scholar] [CrossRef]
- Bettenhausen, C. Hyaluronic acid, the everywhere biopolymer. Chem. Eng. News 2021, 99, 26–31. [Google Scholar]
- Cyphert, J.M.; Trempus, C.S.; Garantziotis, S. Size matters: Molecular weight specificity of hyaluronan effects in cell biology. Int. J. Cell Biol. 2015, 2015, 563818. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Jeong, H.; Han, S.; Beack, S.; Hwang, B.W.; Shin, M.; Oh, S.S.; Hahn, S.K. Hyaluronate and its derivatives for customized biomedical applications. Biomaterials 2017, 123, 155–171. [Google Scholar] [CrossRef] [PubMed]
- Weber, G.C.; Buhren, B.A.; Schrumpf, H.; Wohlrab, J.; Gerber, P.A. Clinical applications of hyaluronidase. Adv. Exp. Med. Biol. 2019, 1148, 255–277. [Google Scholar] [PubMed]
- Toole, B.P. Hyaluronan and its binding proteins, the hyaladherins. Curr. Opin. Cell Biol. 1990, 2, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Farwick, M.; Gauglitz, G.; Pavicic, T.; Koehler, T.; Wehmann, M.; Schwach-Abdellaoui, K.; Malle, B.; Tarabin, V.; Schmitz, G.; Korting, H.C. Fifty-kDa hyaluronic acid upregulates some epidermal genes without changing TNF-α expression in reconstituted epidermis. Ski. Pharmacol. Physiol. 2011, 24, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Essendoubi, M.; Gobinet, C.; Reynaud, R.; Angiboust, J.F.; Manafait, M.; Piot, O. Human skin penetration of hyaluronic acid of different molecular weights as probed by Raman spectroscopy. Ski. Res. Technol. 2016, 22, 55–62. [Google Scholar] [CrossRef]
- Tu, C.X.; Zhang, R.X.; Zhang, X.J.; Huang, T. Exogenous N-acetylglucosamine increases hyaluronan production in cultured human dermal fibroblasts. Arch. Dermatol. Res. 2009, 301, 549–551. [Google Scholar] [CrossRef]
- Bhattacharya, D.S.; Svechkarev, D.; Souchek, J.J.; Hill, T.K.; Taylor, M.A.; Natarajan, A.; Mohs, A.M. Impact of structurally modifying hyaluronic acid on CD44 interaction. J. Mater. Chem. B 2017, 5, 8183–8192. [Google Scholar] [CrossRef]
- Lee, W.H.; Rho, J.G.; Yang, Y.; Lee, S.; Kweon, S.; Souhi, K.; Hyung-Mo, Y.; Juhwan, C.; Hongseo, L.; Eunyoung, K.; et al. Hyaluronic acid nanoparticles as a topical agent for treating psoriasis. ACS Nano 2022, 16, 20057–20074. [Google Scholar] [CrossRef]
- Cui, M.; Wiraja, C.; Chew, S.W.T.; Xu, C. Nanodelivery systems for topical management of skin disorders. Mol. Pharm. 2021, 18, 491–505. [Google Scholar] [CrossRef]
- Du, H.; Liu, P.; Zhu, J.; Lan, J.; Li, Y.; Zhang, L.; Zhu, J.; Tao, J. Hyaluronic acid-based dissolving microneedle patch loaded with methotrexate for improved treatment of psoriasis. ACS Appl. Mater. Interfaces 2019, 11, 43588–43598. [Google Scholar] [CrossRef] [PubMed]
- Witting, M.; Boreham, A.; Brodwolf, R.; Vavarova, K.; Alexiev, U.; Friess, W.; Hedtrich, S. Interactions of hyaluronic acid with the skin and implications for the dermal delivery of biomacromolecules. Mol. Pharm. 2015, 12, 1391–1401. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; Huang, W.; Wu, L.; An, Y.; Xuan, T.; He, H.; Ye, M.; Qi, L.; Wu, J. Bioactive ECM mimic hyaluronic acid dressing via sustained releasing of bFGF for enhancing skin wound healing. ACS Appl. Bio Mater. 2020, 3, 3039–3048. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.L.; Eckhart, K.E.; Wolf, M.E.; Sydlik, S.A. Hyaluronic acid-based antibacterial hydrogels for use as wound dressings. ACS Appl. Bio Mater. 2022, 12, 5608–5616. [Google Scholar] [CrossRef]
- Wang, X.; Fan, G.; Guan, Q.; Zhao, L.; Sun, F.; Yang, H.; Zhao, J.; Zhang, J.; Wang, H.; Zhang, W.; et al. Hyaluronic acid-modified zif-8 nano-vehicle for self-adaption release of curcumin for the treatment of burns. ACS Appl. Nano Mater. 2022, 11, 16094–16107. [Google Scholar] [CrossRef]
- Luan, S.; Zhu, Y.; Wu, X.; Wang, Y.; Liang, F.; Song, S. Hyaluronic-acid-based ph-sensitive nanogels for tumor-targeted drug delivery. ACS Biomater. Sci. Eng. 2017, 3, 2410–2419. [Google Scholar] [CrossRef]
- Song, E.; Han, W.; Li, C.; Cheng, D.; Li, L.; Liu, L.; Zhu, G.; Song, Y.; Tan, W. Hyaluronic acid-decorated graphene oxide nanohybrids as nanocarriers for targeted and pH-responsive anticancer drug delivery. ACS Appl. Mater. Interfaces 2014, 6, 11882–11890. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Wang, X.; Tao, F.; Hu, K.; Zhang, J.; Wu, J.; You, L.; Zhao, W. Fluorinated hyaluronic acid encapsulated perfluorocarbon nanoparticles as tumor-targeted oxygen carriers to enhance radiotherapy. Mol. Pharm. 2022, 19, 3948–3958. [Google Scholar] [CrossRef]
- Hu, J.J.; Wang, M.; Lei, X.X.; Jiang, Y.L.; Yuan, L.; Pan, Z.J.; Lu, D.; Luo, F.; Li, J.H.; Tan, H. Scarless healing of injured vocal folds using an injectable hyaluronic acid-waterborne polyurethane hybrid hydrogel to tune inflammation and collagen deposition. ACS Appl. Mater. Interfaces 2022, 14, 42827–42840. [Google Scholar] [CrossRef]
- Migliore, A.; Procopio, S. Effectiveness and utility of hyaluronic acid in osteoarthritis. Clin. Cases Miner. Bone Metab. 2015, 12, 31–33. [Google Scholar] [CrossRef]
- Testa, G.; Giardina, S.M.C.; Culmone, A.; Vescio, A.; Turchetta, M.; Cannavo, S.; Pavone, V. Intra-articular injections in knee osteoarthritis: A review of literature. J. Funct. Morphol. Kinesiol. 2021, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- Chantre, C.O.; Gonzalez, G.M.; Ahn, S.; Cera, L.; Campbell, P.H.; Hoerstrup, S.P.; Parker, K.K. Porous biomimetic hyaluronic acid and extracellular matrix protein nanofiber scaffolds for accelerated cutaneous tissue repair. ACS Appl. Mater. Interfaces 2019, 11, 45498–45510. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, Y.; Zheng, J.; Liu, L.; Zhang, Q. Three-dimensional printing self-healing dynamic/photocrosslinking gelatin-hyaluronic acid double-network hydrogel for tissue engineering. ACS Omega 2022, 7, 12076–12088. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Gao, Z.; Wang, Y.; Guo, L.; Yin, C.; Zhang, X.; Hao, J.; Zhang, G.; Chen, L. Eco-friendly, self-healing hydrogels for adhesive and elastic strain sensors, circuit repairing, and flexible electronic devices. ACS Macromol. 2019, 52, 2531–2541. [Google Scholar] [CrossRef]
- Zhou, D.; Li, S.; Pei, M.; Yang, H.; Gu, S.; Tao, Y.; Ye, D.; Zhou, Y.; Xu, W.; Xiao, P. Dopamine-modified hyaluronic acid hydrogel adhesives with fast-forming and high tissue adhesion. ACS Appl. Mater. Interfaces 2020, 12, 18225–18234. [Google Scholar] [CrossRef]
- Balazs, E.A.; Denlinger, J.L. Clinical uses of hyaluronan. Ciba Found. Symp. 1989, 143, 265–285. [Google Scholar] [PubMed]
- Milas, M.; Rinaudo, M.; Roure, I.; Al-Assaf, S.; Phillips, G.O.; Williams, P.A. Comparative rheological behavior of hyaluronan from bacterial and animal sources with cross-linked hyaluronan (hylan) in aqueous solution. Biopolymers 2001, 59, 191–204. [Google Scholar] [CrossRef] [PubMed]
- Bothner, H.; Wik, O. Rheology of hyaluronate. Acta Otolaryngol. 1987, 104, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Balazs, E.A. Analgesic effect of elastoviscous hyaluronan solutions and the treatment of arthritic pain. Cells Tissues Organs 2003, 174, 49–62. [Google Scholar] [CrossRef]
- Micheels, P. Human anti-hyaluronic acid antibodies: Is it possible? Dermatol. Surg. 2001, 27, 185–191. [Google Scholar] [CrossRef]
- Narins, R.S.; Brandt, F.; Leyden, J.; Lorenc, Z.P.; Rubin, M.; Smith, S. A randomized, double-blind, multicenter comparison of the efficacy and tolerability of restylane versus zyplast for the correction of nasolabial folds. Dermatol. Surg. 2003, 29, 588–595. [Google Scholar] [PubMed]
- Amorim, S.; Pashkuleva, I.; Reis, C.A.; Reis, R.L.; Pires, R.A. Tunable layer-by-layer films containing hyaluronic acid and their interactions with CD44. J. Mater. Chem. B 2020, 8, 3880–3885. [Google Scholar] [CrossRef]
- Ibrahim, S.; Ramamurthi, A. Hyaluronic acid cues for functional endothelialization of vascular constructs. J. Tissue Eng. Regen. Med. 2008, 2, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Riffault, M.; Hoey, D.; Duffy, B.; Curtin, J.; Jaiswal, S. Biomimetic hyaluronic acid-lysozyme composite coating on AZ31 Mg alloy with combined antibacterial and osteoinductive activities. ACS Biomater. Sci. Eng. 2017, 3, 3244–3253. [Google Scholar] [CrossRef] [PubMed]
- Devine, D.M.; Hahn, J.; Richards, R.G.; Gruner, H.; Wieling, R.; Pearce, S.G. Coating of carbon fiber-reinforced polyetheretherketone implants with titanium to improve bone apposition. J. Biomed. Mater. Res.-Part B Appl. Biomater. 2013, 101, 591–598. [Google Scholar] [CrossRef]
- Li, C.S.; Vannabouathong, C.; Sprague, S.; Bhandari, M. The use of carbon-fiber-reinforced (CFR) peek material in orthopedic implants: A systematic review. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2014, 8, 33–45. [Google Scholar] [CrossRef]
- Pienczewska, E.; Rogowska, A.; Samoraj-Dereszkiewicz, A.; Serafin, J.; Skrobot, W. Initial outcomes of anatomical anterior cruciate ligament reconstruction with PEEK CF interference screws in people practising extreme forms of physical activity–Mental aspects. Arch. Budo 2017, 12, 315–327. [Google Scholar]
- Tseng, Y.-T.; Grace, N.F.; Aguib, H.; Sarathchandra, P.; McCormack, A.; Ebeid, A.; Shehata, N.; Nagy, M.; El-Nashar, H.; Yacoub, M.H.; et al. Biocompatibility and application of carbon fibers in heart valve tissue engineering. Front. Cardiovasc. Med. 2021, 8, 1–12. [Google Scholar] [CrossRef]
- Meng, J.; Xiao, B.; Wu, F.; Sun, L.; Li, B.; Guo, W.; Hu, X.; Xu, X.; Wen, T.; Liu, J.; et al. Bio Co-axial fi brous scaffolds integrating with carbon fi ber promote cardiac tissue regeneration post myocardial infarction. Mater. Today Bio 2022, 16, 100415. [Google Scholar] [CrossRef]
- Hosford, P.S.; Wells, J.A.; Christie, I.N.; Lythgoe, M.F.; Millar, J.; Gourine, A.V. Electrochemical carbon fiber-based technique for simultaneous recordings of brain tissue PO2, pH, and extracellular field potentials. Biosens. Bioelectron. X 2020, 3, 100034. [Google Scholar] [CrossRef]
- Fu, X.; Li, G.; Niu, Y.; Xu, J.; Wang, P.; Zhou, Z. Carbon-based fiber materials as implantable depth neural electrodes. Front. Neurosci. 2021, 15, 1748. [Google Scholar] [CrossRef] [PubMed]
- Rajzer, I.; Menaszek, E.; Bacakova, L.; Rom, M.; Blazewicz, M. In vitro and in vivo studies on biocompatibility of carbon fibres. J. Mat. Sci. 2010, 21, 2611–2622. [Google Scholar] [CrossRef] [PubMed]
- Fraczek-Szczypta, A.; Rabiej, S.; Szparaga, G.; Pabjanczyk-Wlazlo, E.; Krol, P.; Brzezinska, M. The structure and properties of the carbon non-wovens modi fi ed with bioactive nanoceramics for medical applications. Mater. Sci. Eng. C 2015, 51, 336–345. [Google Scholar] [CrossRef]
- Czarnecki, J.S.; Jolivet, S.; Blackmore, M.E.; Lafdi, K.; Tsonis, P.A. Cellular automata simulation of osteoblast growth on microfibrous-carbon-based scaffolds. Tissue Eng. Part A 2014, 20, 3176–3188. [Google Scholar] [CrossRef] [PubMed]
- Frączyk, J.; Magdziarz, S.; Stodolak-Zych, E.; Dzierzkowska, E.; Puchowicz, D.; Kamińska, I.; Giełdowska, M.; Boguń, M. Chemical modification as a method of improving biocompatibility of carbon nonwovens. Materials 2021, 14, 3198. [Google Scholar] [CrossRef]
- Lee, B.M.; Park, S.J.; Noh, I.; Kim, C.H. The effects of the molecular weights of hyaluronic acid on the immune responses. Biomater. Res. 2021, 25, 27. [Google Scholar] [CrossRef]
- SpectraBase Putrescine (1,4-diaminobutane)-1H NMR-Spectrum. Available online: https://spectrabase.com/spectrum/Fb14GyCTY3e (accessed on 12 December 2022).
- Chemical Book-Citric acid(77-92-9) 1H NMR. Available online: https://www.chemicalbook.com/SpectrumEN_77-92-9_1HNMR.htm (accessed on 11 December 2022).
- Spectra Base Citric acid-1H NMR-Spectrum. Available online: https://spectrabase.com/spectrum/LbA1PVJxGHk (accessed on 11 December 2022).
- Gatta, A.L.; Schiraldi, C.; Papa, A.; Agostino, A.D.; Cammarota, M.; Rosa, A.D.; Rosa, M.D. Hyaluronan scaffolds via diglycidyl ether crosslinking: Toward improvements in composition and performance. Carbohydr. Polym. 2013, 96, 536–544. [Google Scholar] [CrossRef]
- Al-Sibani, M.; Al-Harrasi, A. Characterization of linear and chemically cross-linked hyaluronic acid using various analytical techniques including FTIR, ESI-MS, H1 NMR, and SEM. J. Biochem. Analyt. Stud. 2018, 3, 1. [Google Scholar]
- Pan, N.C.; Pereira, H.C.B.; da Silva, M.L.C.; Vasconcelos, A.F.D.; Celligoi, M.A.P.C. Improvement production of hyaluronic acid by streptococcus zooepidemicus in sugarcane molasses. Appl. Biochem. Biotechnol. 2017, 182, 276–293. [Google Scholar] [CrossRef]
- Tornihata, K.; Ikada, Y. Preparation of cross-linked hyaluronic acid films of low water content. Biomaterials 1997, 18, 189–195. [Google Scholar]
- Schanté, C.E.; Zuber, G.; Herlin, C.; Vandamme, T.F. Chemical modifications of hyaluronic acid for the synthesis of derivatives for a broad range of biomedical applications. Carbohyd. Polym. 2011, 85, 469–489. [Google Scholar] [CrossRef]
- Mlc, P.; Steiner, B.; Machova, E.; Koo, M.; Krc, M. Synthesis and characterization of new biodegradable hyaluronan alkyl derivatives. Biopolymers 2006, 82, 74–79. [Google Scholar]
- Yamaguchi, A. Historical background and recent advance in BMP research. Clin. Calcium 2006, 16, 732–737. [Google Scholar] [PubMed]
- Wozney, J.M.; Rosen, V.; Celeste, A.J.; Mitsock, L.M.; Whitters, M.J.; Kriz, R.W.; Hewick, R.M.; Wang, E.A. Novel regulators of bone formation: Molecular clones and activities. Science 1988, 242, 1528–1534. [Google Scholar] [CrossRef]
- Simpson, A.H.R.W.; Mills, L.; Noble, B. The role of growth factors and related agents in accelerating fracture healing. J. Bone Jt. Surg. 2006, 88, 701–705. [Google Scholar] [CrossRef]
- Even, J.; Eskander, M.; Kang, J. Bone morphogenetic protein in spine surgery: Current and future uses. J. Am. Acad. Orthop. Surg. 2012, 20, 547–552. [Google Scholar] [CrossRef]
- Wang, C.; Yan, Q.; Liu, H.B.; Zhou, X.H.; Xiao, S.J. Different EDC/NHS activation mechanisms between PAA and PMAA brushes and the following amidation reactions. Langmuir 2011, 27, 12058–12068. [Google Scholar] [CrossRef]
- Mohan, T.; Kleinschek, K.S.; Kargl, R. Polysaccharide peptide conjugates: Chemistry, properties and applications. Carbohydr. Polym. 2022, 280, 118875. [Google Scholar] [CrossRef]
- Pugliese, R.; Gelain, F. Cross-linked self-assembling peptides and their post-assembly functionalization via one-pot and in situ gelation system. Int. J. Mol. Sci. 2020, 21, 4261. [Google Scholar] [CrossRef]
- Kamiński, Z.J.; Kolesińska, B.; Kolesińska, J.; Sabatino, G.; Chelli, M.; Rovero, P.; Błaszczyk, M.; Główka, M.L.; Papini, A.M. N-triazinylammonium tetrafluoroborates. A new generation of efficient coupling reagents useful for peptide synthesis. J. Am. Chem. Soc. 2005, 127, 16912–16920. [Google Scholar] [CrossRef]
- Jastrząbek, K.; Kolesińska, B.; Sabatino, G.; Rizzolo, F.; Papini, A.M.; Kamiński, Z.J. Benzyloxy derivatives of triazine-based coupling reagents designed for an efficient solid phase peptide synthesis on polystyrene resin. Int. J. Pept. Res. Ther. 2007, 13, 229–236. [Google Scholar] [CrossRef]
- Kolesinska, B.; Rozniakowski, K.K.; Fraczyk, J.; Relich, I.; Papini, M.A.; Kaminski, Z.J. The effect of counterion and tertiary amine on the efficiency of N-triazinylammonium sulfonates in solution and solid-phase peptide synthesis. Eur. J. Org. Chem. 2015, 2, 401–408. [Google Scholar] [CrossRef]
- Fraczyk, J.; Kaminski, Z.J.; Katarzynska, J.; Kolesinska, B. 4-(4,6-Dimethoxy-1,3,5-triazin-2-yl)-4-methylmorpholinium Toluene-4-sulfonate (DMT/NMM/TsO−) universal coupling reagent for synthesis in solution. Helv. Chim. Acta 2018, 101, 1700187. [Google Scholar] [CrossRef]






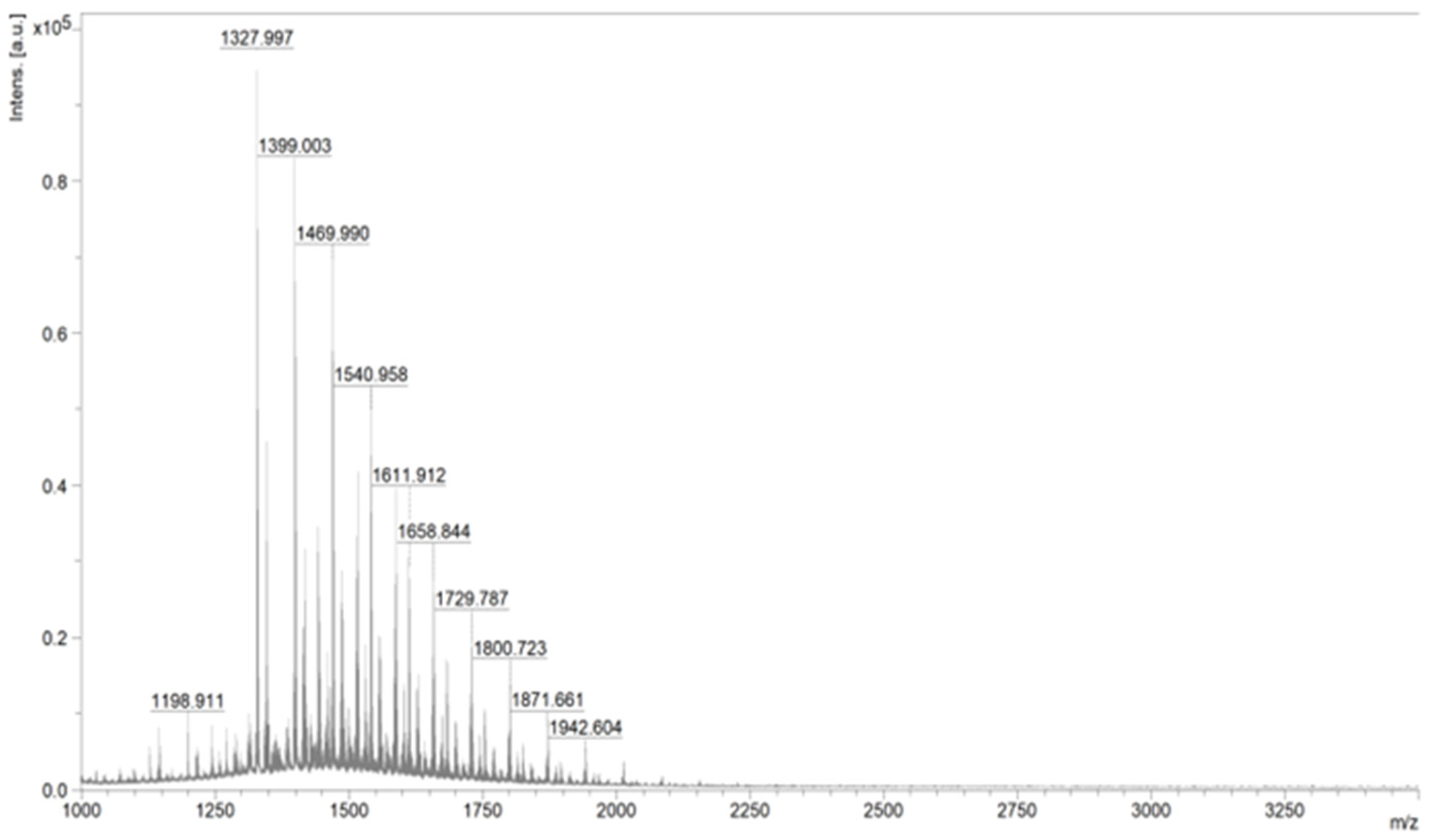







| m/z | Intensity | Interpretation |
|---|---|---|
| 1611.912 | 29,253 | Mass of the expected product |
| 1658.844 | 27,497 | |
| 1540.958 | 49,859 | |
| 1198.911 | 9925 | Mass differing by one mer |
| 1327.997 | 97,107 | Peptide mass |
| 1399.003 | 82,979 |
| m/z | Intensity | Interpretation |
|---|---|---|
| 353.288 | 4895 | Mass of the expected product |
| 375.029 | 5694 | |
| 391.015 | 255 |
| m/z | Intensity | Interpretation |
|---|---|---|
| 1107.554 | 23,195 | Mass of the expected product differing by one mer |
| 1246.593 | 1261 | |
| 1264.605 | 920 | |
| 1194.623 | 1562 | Peptide mass |
| Cross-Linking Agent | Suitability Assessment/Explanations |
|---|---|
| 1,4-butanediamine | Mediocre results. Amine was attached to the polysaccharide chain, but results were below expectations—only a slight modification took place. |
| Citric Acid | Reagent with a simple structure that is able to cross-link HA either chemically or physically with good results. Considered a “green” cross-linking agent. It is non-toxic, biodegradable, and biocompatible. |
| BDDE | Simple method that effectively cross-links HA at a sufficient level. Judging by the obtained structure of the final material, it provides superior mechanical properties relative to CA-using methods, so the acid clumps into larger agglomerates and has a longer duration. If completely cross-linked, it is considered harmless to the human body. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magdziarz, S.; Boguń, M.; Frączyk, J. Coating Methods of Carbon Nonwovens with Cross-Linked Hyaluronic Acid and Its Conjugates with BMP Fragments. Polymers 2023, 15, 1551. https://doi.org/10.3390/polym15061551
Magdziarz S, Boguń M, Frączyk J. Coating Methods of Carbon Nonwovens with Cross-Linked Hyaluronic Acid and Its Conjugates with BMP Fragments. Polymers. 2023; 15(6):1551. https://doi.org/10.3390/polym15061551
Chicago/Turabian StyleMagdziarz, Sylwia, Maciej Boguń, and Justyna Frączyk. 2023. "Coating Methods of Carbon Nonwovens with Cross-Linked Hyaluronic Acid and Its Conjugates with BMP Fragments" Polymers 15, no. 6: 1551. https://doi.org/10.3390/polym15061551
APA StyleMagdziarz, S., Boguń, M., & Frączyk, J. (2023). Coating Methods of Carbon Nonwovens with Cross-Linked Hyaluronic Acid and Its Conjugates with BMP Fragments. Polymers, 15(6), 1551. https://doi.org/10.3390/polym15061551






