CeO2 Nanoparticle-Containing Polymers for Biomedical Applications: A Review
Abstract
1. Introduction
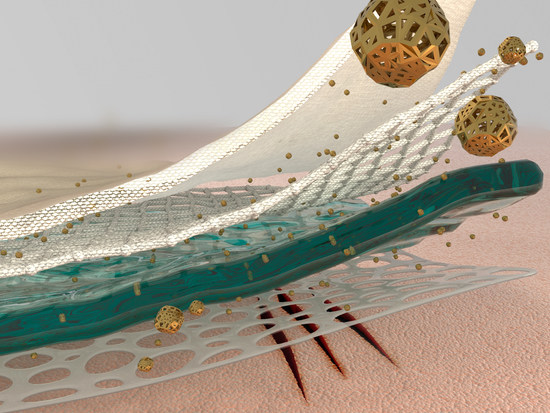
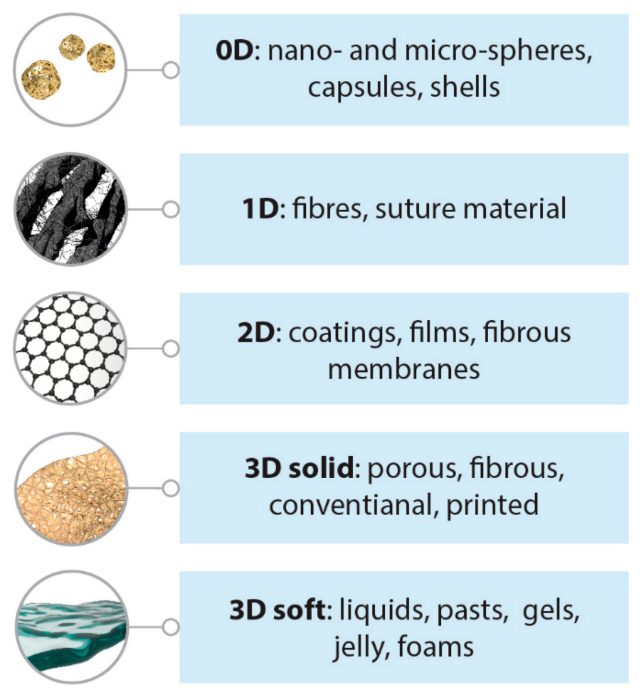
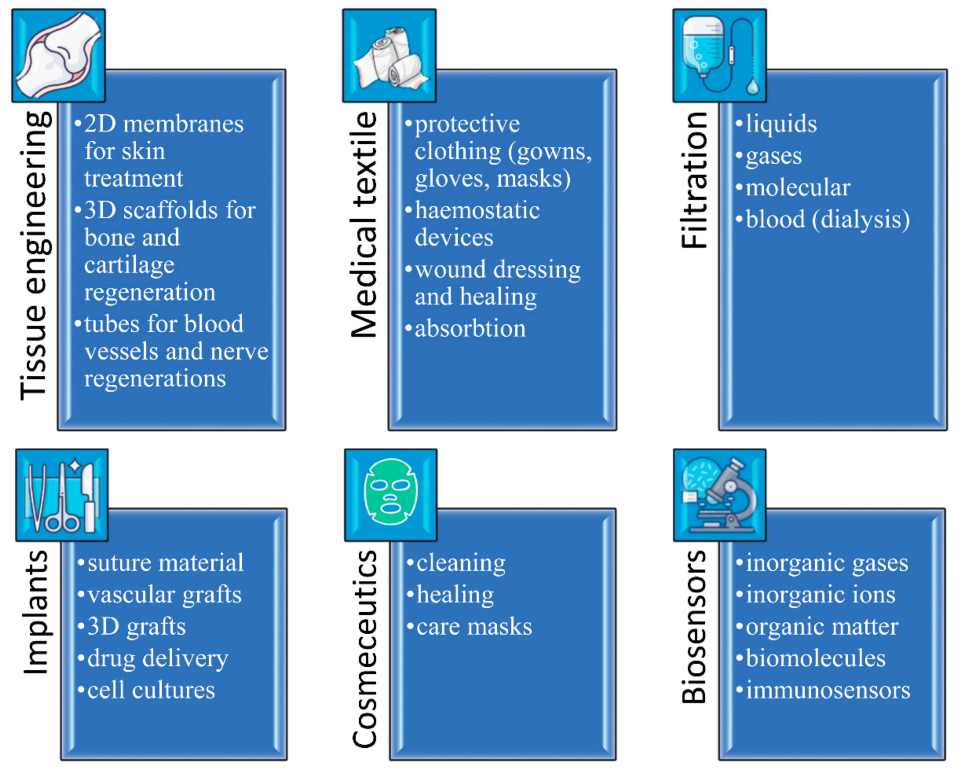
1.1. Polymeric Materials for Biomedical Applications: Advantages and Limitations
1.2. Oxide Fillers for the Modification of the Properties of Polymers
1.3. Multifaceted Biomedical Applications of Cerium Oxide Nanoparticles
1.4. Cerium Oxide Nanoparticles as a Modifier of Polymer Properties
2. Ceria-Containing Tissue Engineering Scaffolds
2.1. Porous Scaffolds
2.2. Electrospun Fibers
2.3. Composite 2D Films and 3D Scaffolds
3. Wound Dressings and Other Topical Applications for Ceria-Containing Polymers
3.1. Electrospun Fibrous Membranes
3.2. 2D Films and Composites
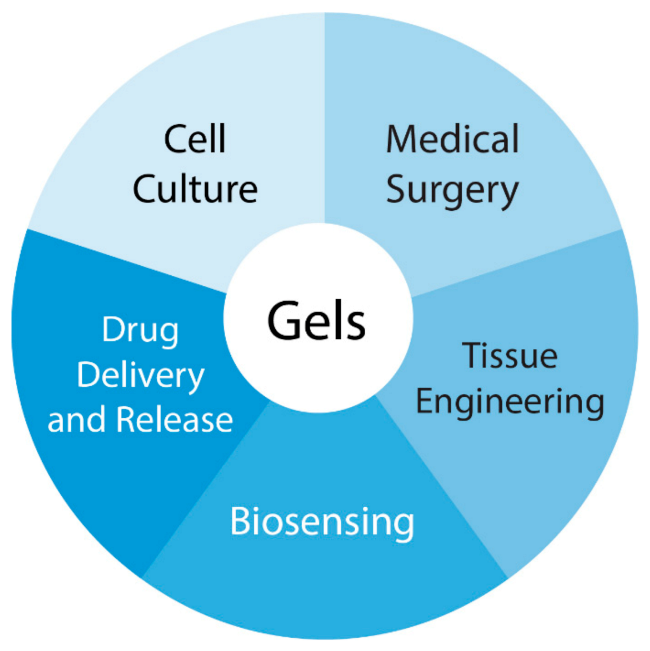
4. Ceria-Containing Gel-Like Polymeric Materials
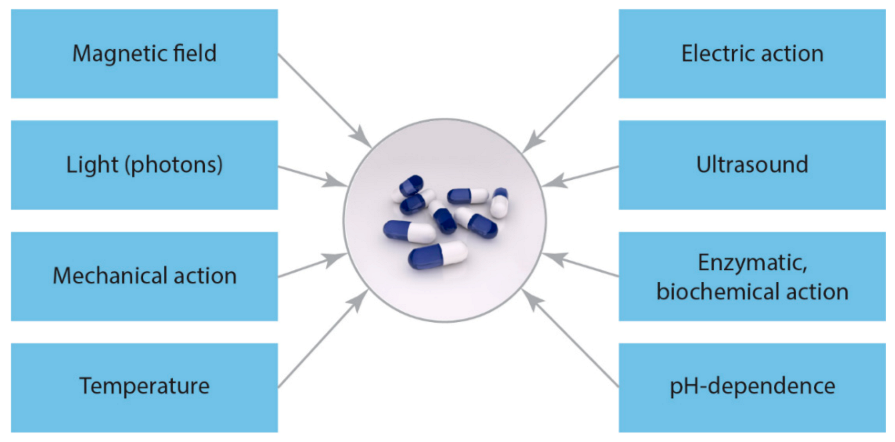
5. Polymeric Composites with Ceria Nanoparticles for Drug Delivery and Gene Therapy
5.1. Polymeric Micro- and Nanoparticles
5.2. Layer-by-Layer Polyelectrolyte Coatings and Capsules
6. Ceria Additives Improving Implants’ Biodegradability
7. Ceria-Containing Antibacterial and Antiviral Multifunctional Materials
7.1. Antibacterial Cerium Compounds in Wound Healing
7.2. Antibacterial CeNPs in Biomedical Polymers
7.3. Antiviral CeNPs in Biomedical Polymers
8. Biosensing with Ceria-Containing Polymer Nanocomposites
9. Other Biomedical Applications and Future Trends of CeNPs-Polymer Composites
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Calori, I.R.; Braga, G.; de Jesus, P.D.C.C.; Bi, H.; Tedesco, A.C. Polymer scaffolds as drug delivery systems. Eur. Polym. J. 2020, 129, 109621. [Google Scholar] [CrossRef]
- Sánchez-Téllez, D.; Téllez-Jurado, L.; Rodríguez-Lorenzo, L. Hydrogels for Cartilage Regeneration, from Polysaccharides to Hybrids. Polymers 2017, 9, 671. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Naqvi, R.A.; Abbas, N.; Khan, S.M.; Nawaz, S.; Hussain, A.; Zahra, N.; Khalid, M.W. Ultra-High-Molecular-Weight-Polyethylene (UHMWPE) as a Promising Polymer Material for Biomedical Applications: A Concise Review. Polymers 2020, 12, 323. [Google Scholar] [CrossRef] [PubMed]
- Patil, N.A.; Njuguna, J.; Kandasubramanian, B. UHMWPE for biomedical applications: Performance and functionalization. Eur. Polym. J. 2020, 125, 109529. [Google Scholar] [CrossRef]
- Abdul Samad, M. Recent Advances in UHMWPE/UHMWPE Nanocomposite/UHMWPE Hybrid Nanocomposite Polymer Coatings for Tribological Applications: A Comprehensive Review. Polymers 2021, 13, 608. [Google Scholar] [CrossRef]
- Maksimkin, A.V.; Senatov, F.S.; Niaza, K.; Dayyoub, T.; Kaloshkin, S.D. Ultra-High Molecular Weight Polyethylene/Titanium-Hybrid Implant for Bone-Defect Replacement. Materials 2020, 13, 3010. [Google Scholar] [CrossRef] [PubMed]
- Šupová, M.; Martynková, G.S.; Barabaszová, K. Effect of Nanofillers Dispersion in Polymer Matrices: A Review. Sci. Adv. Mater. 2011, 3, 1–25. [Google Scholar] [CrossRef]
- Sagadevan, S.; Fareen, A.; Hoque, M.E.; Chowdhury, Z.Z.; Johan, M.R.B.; Rafique, R.F.; Aziz, F.A.; Lett, J.A. Nanostructured Polymer Biocomposites: Pharmaceutical Applications. In Nanostructured Polymer Composites for Biomedical Applications; Elsevier: Amsterdam, The Netherlands, 2019; pp. 227–259. [Google Scholar]
- Murthy, S.; Effiong, P.; Fei, C.C. Metal oxide nanoparticles in biomedical applications. In Metal Oxide Powder Technologies; Elsevier: Amsterdam, The Netherlands, 2020; pp. 233–251. [Google Scholar]
- Prasanna, S.R.V.S.; Balaji, K.; Pandey, S.; Rana, S. Metal Oxide Based Nanomaterials and Their Polymer Nanocomposites. In Nanomaterials and Polymer Nanocomposites; Elsevier: Amsterdam, The Netherlands, 2019; pp. 123–144. [Google Scholar]
- Asar, N.V.; Albayrak, H.; Korkmaz, T.; Turkyilmaz, I. Influence of various metal oxides on mechanical and physical properties of heat-cured polymethyl methacrylate denture base resins. J. Adv. Prosthodont. 2013, 5, 241. [Google Scholar] [CrossRef]
- Cristache, C.M.; Totu, E.E.; Iorgulescu, G.; Pantazi, A.; Dorobantu, D.; Nechifor, A.C.; Isildak, I.; Burlibasa, M.; Nechifor, G.; Enachescu, M. Eighteen Months Follow-Up with Patient-Centered Outcomes Assessment of Complete Dentures Manufactured Using a Hybrid Nanocomposite and Additive CAD/CAM Protocol. J. Clin. Med. 2020, 9, 324. [Google Scholar] [CrossRef]
- Totu, E.E.; Nechifor, A.C.; Nechifor, G.; Aboul-Enein, H.Y.; Cristache, C.M. Poly(methyl methacrylate) with TiO2 nanoparticles inclusion for stereolitographic complete denture manufacturing—The fututre in dental care for elderly edentulous patients? J. Dent. 2017, 59, 68–77. [Google Scholar] [CrossRef]
- Schexnailder, P.; Schmidt, G. Nanocomposite polymer hydrogels. Colloid Polym. Sci. 2009, 287, 1–11. [Google Scholar] [CrossRef]
- Li, H.; Huang, D.; Ren, K.; Ji, J. Inorganic-polymer composite coatings for biomedical devices. Smart Mater. Med. 2021, 2, 1–14. [Google Scholar] [CrossRef]
- Catauro, M.; Bollino, F.; Giovanardi, R.; Veronesi, P. Modification of Ti6Al4V implant surfaces by biocompatible TiO2/PCL hybrid layers prepared via sol-gel dip coating: Structural characterization, mechanical and corrosion behavior. Mater. Sci. Eng. C 2017, 74, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Catauro, M.; Bollino, F.; Papale, F.; Lamanna, G. TiO2/PCL Hybrid Layers Prepared via Sol-Gel Dip Coating for the Surface Modification of Titanium Implants: Characterization and Bioactivity Evaluation. Appl. Mech. Mater. 2015, 760, 353–358. [Google Scholar] [CrossRef]
- Abudula, T.; Qurban, R.O.; Bolarinwa, S.O.; Mirza, A.A.; Pasovic, M.; Memic, A. 3D Printing of Metal/Metal Oxide Incorporated Thermoplastic Nanocomposites With Antimicrobial Properties. Front. Bioeng. Biotechnol. 2020, 8. [Google Scholar] [CrossRef]
- Shcherbakov, A.B.; Zholobak, N.M.; Ivanov, V.K. Biological, biomedical and pharmaceutical applications of cerium oxide. In Cerium Oxide (CeO₂): Synthesis, Properties and Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 279–358. [Google Scholar]
- Popov, A.L.; Popova, N.R.; Selezneva, I.I.; Akkizov, A.Y.; Ivanov, V.K. Cerium oxide nanoparticles stimulate proliferation of primary mouse embryonic fibroblasts in vitro. Mater. Sci. Eng. C 2016, 68, 406–413. [Google Scholar] [CrossRef]
- Das, S.; Chigurupati, S.; Dowding, J.; Munusamy, P.; Baer, D.R.; McGinnis, J.F.; Mattson, M.P.; Self, W.; Seal, S. Therapeutic potential of nanoceria in regenerative medicine. MRS Bull. 2014, 39, 976–983. [Google Scholar] [CrossRef]
- Hosseini, M.; Mozafari, M. Cerium Oxide Nanoparticles: Recent Advances in Tissue Engineering. Materials 2020, 13, 3072. [Google Scholar] [CrossRef]
- Chigurupati, S.; Mughal, M.R.; Okun, E.; Das, S.; Kumar, A.; McCaffery, M.; Seal, S.; Mattson, M.P. Effects of cerium oxide nanoparticles on the growth of keratinocytes, fibroblasts and vascular endothelial cells in cutaneous wound healing. Biomaterials 2013, 34, 2194–2201. [Google Scholar] [CrossRef]
- Genier, F.; Bizanek, M.; Webster, T.; Roy, A. Increased viability of fibroblasts when pretreated with ceria nanoparticles during serum deprivation. Int. J. Nanomed. 2018, 13, 895–901. [Google Scholar] [CrossRef]
- Davan, R.; Prasad, R.G.S.V.; Jakka, V.S.; Aparna, R.S.L.; Phani, A.R.; Jacob, B.; Salins, P.C.; Raju, D.B. Cerium Oxide Nanoparticles Promotes Wound Healing Activity in In-Vivo Animal Model. J. Bionanosci. 2012, 6, 78–83. [Google Scholar] [CrossRef]
- Kalashnikova, I.; Das, S.; Seal, S. Nanomaterials for wound healing: Scope and advancement. Nanomedicine 2015, 10, 2593–2612. [Google Scholar] [CrossRef] [PubMed]
- Korotaeva, A.I.; Legon’kova, O.A.; Savchenkova, I.P.; Belova, M.S.; Ushakova, T.A.; Ivanov, V.K.; Perova, N.V.; Torkova, A.A.; Baranchikov, A.E.; Ivanova, O.S. Experimental Study of the Effects of Nanodispersed Ceria on Wound Repair. Bull. Exp. Biol. Med. 2017, 162, 395–399. [Google Scholar] [CrossRef]
- Ermakov, A.; Popov, A.; Ermakova, O.; Ivanova, O.; Baranchikov, A.; Kamenskikh, K.; Shekunova, T.; Shcherbakov, A.; Popova, N.; Ivanov, V. The first inorganic mitogens: Cerium oxide and cerium fluoride nanoparticles stimulate planarian regeneration via neoblastic activation. Mater. Sci. Eng. C 2019, 104, 109924. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Li, L.-D.; Lyu, G.-M.; Shen, B.-Y.; Han, Y.-F.; Shi, J.-L.; Teng, J.-L.; Feng, L.; Si, S.-Y.; Wu, J.-H.; et al. Chitosan-coated cerium oxide nanocubes accelerate cutaneous wound healing by curtailing persistent inflammation. Inorg. Chem. Front. 2018, 5, 386–393. [Google Scholar] [CrossRef]
- Wu, H.; Li, F.; Wang, S.; Lu, J.; Li, J.; Du, Y.; Sun, X.; Chen, X.; Gao, J.; Ling, D. Ceria nanocrystals decorated mesoporous silica nanoparticle based ROS-scavenging tissue adhesive for highly efficient regenerative wound healing. Biomaterials 2018, 151, 66–77. [Google Scholar] [CrossRef]
- Ma, X.; Cheng, Y.; Jian, H.; Feng, Y.; Chang, Y.; Zheng, R.; Wu, X.; Wang, L.; Li, X.; Zhang, H. Hollow, Rough, and Nitric Oxide-Releasing Cerium Oxide Nanoparticles for Promoting Multiple Stages of Wound Healing. Adv. Healthc. Mater. 2019, 8, 1900256. [Google Scholar] [CrossRef]
- Mohammad, G.; Mishra, V.K.; Pandey, H.P. Antioxidant properties of some nanoparticle may enhance wound healing in T2DM patient. Dig. J. Nanomater. Biostruct. 2008, 3, 159–162. [Google Scholar]
- Amiri, A.; Nikitina, N.; Stepanova, L.; Beregova, T. Potential impact of cerium dioxide nanoparticles (nanoceria) on the concentration of C-reactive protein and middle-mass molecules after wound treatment in rats. Sci. Biol. Sci. 2019, 14–19. [Google Scholar] [CrossRef]
- Kobyliak, N.; Abenavoli, L.; Kononenko, L.; Kyriienko, D.; Spivak, M. Neuropathic diabetic foot ulcers treated with cerium dioxide nanoparticles: A case report. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 228–234. [Google Scholar] [CrossRef]
- Popov, A.L.; Shcherbakov, A.B.; Zholobak, N.M.; Baranchikov, A.E.; Ivanov, V.K. Cerium dioxide nanoparticles as third-generation enzymes (nanozymes). Nanosyst. Phys. Chem. Math. 2017, 760–781. [Google Scholar] [CrossRef]
- Wu, H.; Liao, H.; Li, F.; Lee, J.; Hu, P.; Shao, W.; Li, X.; Ling, D. Bioactive ROS-scavenging nanozymes for regenerative medicine: Reestablishing the antioxidant firewall. Nano Sel. 2020, 1, 285–297. [Google Scholar] [CrossRef]
- Wu, H.; Li, F.; Shao, W.; Gao, J.; Ling, D. Promoting Angiogenesis in Oxidative Diabetic Wound Microenvironment Using a Nanozyme-Reinforced Self-Protecting Hydrogel. ACS Cent. Sci. 2019, 5, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Jansman, M.M.T.; Hosta-Rigau, L. Cerium- and Iron-Oxide-Based Nanozymes in Tissue Engineering and Regenerative Medicine. Catalysts 2019, 9, 691. [Google Scholar] [CrossRef]
- Arya, A.; Sethy, N.K.; Gangwar, A.; Bhargava, N.; Dubey, A.; Roy, M.; Srivastava, G.; Singh, S.K.; Das, M.; Bhargava, K. Cerium oxide nanozyme modulate the ‘exercise’ redox biology of skeletal muscle. Mater. Res. Express 2017, 4, 055401. [Google Scholar] [CrossRef]
- Li, F.; Qiu, Y.; Xia, F.; Sun, H.; Liao, H.; Xie, A.; Lee, J.; Lin, P.; Wei, M.; Shao, Y.; et al. Dual detoxification and inflammatory regulation by ceria nanozymes for drug-induced liver injury therapy. Nano Today 2020, 35, 100925. [Google Scholar] [CrossRef]
- Kalyanaraman, V.; Naveen, S.V.; Mohana, N.; Balaje, R.M.; Navaneethakrishnan, K.R.; Brabu, B.; Murugan, S.S.; Kumaravel, T.S. Biocompatibility studies on cerium oxide nanoparticles—Combined study for local effects, systemic toxicity and genotoxicity via implantation route. Toxicol. Res. 2019, 8, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Rotter, N.; Ung, F.; Roy, A.K.; Vacanti, M.; Eavey, R.D.; Vacanti, C.A.; Bonassar, L.J. Role for Interleukin 1α in the Inhibition of Chondrogenesis in Autologous Implants Using Polyglycolic Acid–Polylactic Acid Scaffolds. Tissue Eng. 2005, 11, 192–200. [Google Scholar] [CrossRef]
- Selvaraj, V.; Manne, N.D.; Arvapalli, R.; Rice, K.M.; Nandyala, G.; Fankenhanel, E.; Blough, E.R. Effect of cerium oxide nanoparticles on sepsis induced mortality and NF-κB signaling in cultured macrophages. Nanomedicine 2015, 10, 1275–1288. [Google Scholar] [CrossRef]
- Selvaraj, V.; Nepal, N.; Rogers, S.; Manne, N.D.P.K.; Arvapalli, R.; Rice, K.M.; Asano, S.; Fankhanel, E.; Ma, J.J.; Shokuhfar, T.; et al. Inhibition of MAP kinase/NF-kB mediated signaling and attenuation of lipopolysaccharide induced severe sepsis by cerium oxide nanoparticles. Biomaterials 2015, 59, 160–171. [Google Scholar] [CrossRef]
- Ponnurangam, S.; O’Connell, G.D.; Chernyshova, I.V.; Wood, K.; Hung, C.T.-H.; Somasundaran, P. Beneficial Effects of Cerium Oxide Nanoparticles in Development of Chondrocyte-Seeded Hydrogel Constructs and Cellular Response to Interleukin Insults. Tissue Eng. Part A 2014, 20, 2908–2919. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Shen, Q.; Xie, Y.; You, M.; Huang, L.; Zheng, X. Incorporation of cerium oxide into hydroxyapatite coating regulates osteogenic activity of mesenchymal stem cell and macrophage polarization. J. Biomater. Appl. 2017, 31, 1062–1076. [Google Scholar] [CrossRef]
- Prefac, G.-A.; Milea, M.-L.; Vadureanu, A.-M.; Muraru, S.; Dobrin, D.-I.; Isopencu, G.-O.; Jinga, S.-I.; Raileanu, M.; Bacalum, M.; Busuioc, C. CeO2 Containing Thin Films as Bioactive Coatings for Orthopaedic Implants. Coatings 2020, 10, 642. [Google Scholar] [CrossRef]
- Davoodbasha, M.A.; Saravanakumar, K.; Abdulkader, A.M.; Lee, S.-Y.; Kim, J.-W. Synthesis of Biocompatible Cellulose-Coated Nanoceria with pH-Dependent Antioxidant Property. ACS Appl. Bio Mater. 2019, 2, 1792–1801. [Google Scholar] [CrossRef]
- Weaver, J.D.; Stabler, C.L. Antioxidant cerium oxide nanoparticle hydrogels for cellular encapsulation. Acta Biomater. 2015, 16, 136–144. [Google Scholar] [CrossRef]
- Bhattacharya, D.; Tiwari, R.; Bhatia, T.; Purohit, M.P.; Pal, A.; Jagdale, P.; Mudiam, M.K.R.; Chaudhari, B.P.; Shukla, Y.; Ansari, K.M.; et al. Accelerated and scarless wound repair by a multicomponent hydrogel through simultaneous activation of multiple pathways. Drug Deliv. Transl. Res. 2019, 9, 1143–1158. [Google Scholar] [CrossRef]
- He, Z.-Y.; Shi, K.; Wei, Y.-Q.; Qian, Z.-Y. Recent Advances of Poly(ether-ether) and Poly(ether-ester) Block Copolymers in Biomedical Applications. Curr. Drug Metab. 2016, 17, 168–186. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Lin, S.; Shang, J.; He, W.; Lan, J. Mechanical, thermal, and ultraviolet resistance properties of poly(ether–ester)/cerium oxide (CeO2) composite fibers. J. Reinf. Plast. Compos. 2014, 33, 1207–1215. [Google Scholar] [CrossRef]
- Jia, R.-P.; Wang, C.-F.; Zheng, K.; He, X.-Y.; Huang, M.-S. Preparation, characterization, and properties of CeO2 /thermoplastic polyurethane nanocomposites. J. Reinf. Plast. Compos. 2015, 34, 1090–1098. [Google Scholar] [CrossRef]
- Inbasekar, C.; Fathima, N.N. Collagen stabilization using ionic liquid functionalised cerium oxide nanoparticle. Int. J. Biol. Macromol. 2020, 147, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Augustine, R.; Dalvi, Y.B.; Dan, P.; George, N.; Helle, D.; Varghese, R.; Thomas, S.; Menu, P.; Sandhyarani, N. Nanoceria Can Act as the Cues for Angiogenesis in Tissue-Engineering Scaffolds: Toward Next-Generation in Situ Tissue Engineering. ACS Biomater. Sci. Eng. 2018, 4, 4338–4353. [Google Scholar] [CrossRef] [PubMed]
- Naganuma, T.; Traversa, E. The effect of cerium valence states at cerium oxide nanoparticle surfaces on cell proliferation. Biomaterials 2014, 35, 4441–4453. [Google Scholar] [CrossRef]
- Xiang, J.; Li, J.; He, J.; Tang, X.; Dou, C.; Cao, Z.; Yu, B.; Zhao, C.; Kang, F.; Yang, L.; et al. Cerium Oxide Nanoparticle Modified Scaffold Interface Enhances Vascularization of Bone Grafts by Activating Calcium Channel of Mesenchymal Stem Cells. ACS Appl. Mater. Interfaces 2016, 8, 4489–4499. [Google Scholar] [CrossRef]
- Marino, A.; Tonda-Turo, C.; De Pasquale, D.; Ruini, F.; Genchi, G.; Nitti, S.; Cappello, V.; Gemmi, M.; Mattoli, V.; Ciardelli, G.; et al. Gelatin/nanoceria nanocomposite fibers as antioxidant scaffolds for neuronal regeneration. Biochim. Biophys. Acta Gen. Subj. 2017, 1861, 386–395. [Google Scholar] [CrossRef]
- Purohit, S.D.; Singh, H.; Bhaskar, R.; Yadav, I.; Chou, C.-F.; Gupta, M.K.; Mishra, N.C. Gelatin—alginate—cerium oxide nanocomposite scaffold for bone regeneration. Mater. Sci. Eng. C 2020, 116, 111111. [Google Scholar] [CrossRef]
- Dulany, K.; Hepburn, K.; Goins, A.; Allen, J.B. In vitro and in vivo biocompatibility assessment of free radical scavenging nanocomposite scaffolds for bone tissue regeneration. J. Biomed. Mater. Res. Part A 2020, 108, 301–315. [Google Scholar] [CrossRef]
- Singh, V.; Singh, S.; Das, S.; Kumar, A.; Self, W.T.; Seal, S. A facile synthesis of PLGA encapsulated cerium oxide nanoparticles: Release kinetics and biological activity. Nanoscale 2012, 4, 2597. [Google Scholar] [CrossRef]
- Kalantari, K.; Mostafavi, E.; Saleh, B.; Soltantabar, P.; Webster, T.J. Chitosan/PVA hydrogels incorporated with green synthesized cerium oxide nanoparticles for wound healing applications. Eur. Polym. J. 2020, 134, 109853. [Google Scholar] [CrossRef]
- Augustine, R.; Hasan, A.; Patan, N.K.; Dalvi, Y.B.; Varghese, R.; Antony, A.; Unni, R.N.; Sandhyarani, N.; Moustafa, A.-E. Al Cerium Oxide Nanoparticle Incorporated Electrospun Poly(3-hydroxybutyrate-co-3-hydroxyvalerate) Membranes for Diabetic Wound Healing Applications. ACS Biomater. Sci. Eng. 2020, 6, 58–70. [Google Scholar] [CrossRef]
- Kalaycıoğlu, Z.; Kahya, N.; Adımcılar, V.; Kaygusuz, H.; Torlak, E.; Akın-Evingür, G.; Erim, F.B. Antibacterial nano cerium oxide/chitosan/cellulose acetate composite films as potential wound dressing. Eur. Polym. J. 2020, 133, 109777. [Google Scholar] [CrossRef]
- Naseri-Nosar, M.; Farzamfar, S.; Sahrapeyma, H.; Ghorbani, S.; Bastami, F.; Vaez, A.; Salehi, M. Cerium oxide nanoparticle-containing poly (ε-caprolactone)/gelatin electrospun film as a potential wound dressing material: In vitro and in vivo evaluation. Mater. Sci. Eng. C 2017, 81, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Rather, H.A.; Thakore, R.; Singh, R.; Jhala, D.; Singh, S.; Vasita, R. Antioxidative study of Cerium Oxide nanoparticle functionalised PCL-Gelatin electrospun fibers for wound healing application. Bioact. Mater. 2018, 3, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Raja, I.S.; Fathima, N.N. Gelatin–Cerium Oxide Nanocomposite for Enhanced Excisional Wound Healing. ACS Appl. Bio Mater. 2018, 1, 487–495. [Google Scholar] [CrossRef]
- Cheng, H.; Shi, Z.; Yue, K.; Huang, X.; Xu, Y.; Gao, C.; Yao, Z.; Zhang, Y.S.; Wang, J. Sprayable hydrogel dressing accelerates wound healing with combined reactive oxygen species-scavenging and antibacterial abilities. Acta Biomater. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hao, D.; Zhang, G.; Gong, Y.; Ma, Z. Development and biological evaluation of cerium oxide loaded polycaprolactone dressing on cutaneous wound healing in nursing care. Mater. Lett. 2020, 265, 127401. [Google Scholar] [CrossRef]
- Sener, G.; Hilton, S.A.; Osmond, M.J.; Zgheib, C.; Newsom, J.P.; Dewberry, L.; Singh, S.; Sakthivel, T.S.; Seal, S.; Liechty, K.W.; et al. Injectable, self-healable zwitterionic cryogels with sustained microRNA—Cerium oxide nanoparticle release promote accelerated wound healing. Acta Biomater. 2020, 101, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Andrabi, S.M.; Majumder, S.; Gupta, K.C.; Kumar, A. Dextran based amphiphilic nano-hybrid hydrogel system incorporated with curcumin and cerium oxide nanoparticles for wound healing. Colloids Surf. B Biointerfaces 2020, 195, 111263. [Google Scholar] [CrossRef]
- Popov, A.L.; Popova, N.; Gould, D.J.; Shcherbakov, A.B.; Sukhorukov, G.B.; Ivanov, V.K. Ceria Nanoparticles-Decorated Microcapsules as a Smart Drug Delivery/Protective System: Protection of Encapsulated P. pyralis Luciferase. ACS Appl. Mater. Interfaces 2018, 10, 14367–14377. [Google Scholar] [CrossRef] [PubMed]
- Sedighi, M.; Rahimi, F.; Rezayan, A.H.; Shahbazi, M.-A.; Witzigmann, D.; Huwyler, J. Combined cerium oxide nanocapping and layer-by-layer coating of porous silicon containers for controlled drug release. J. Mater. Sci. 2018, 53, 14975–14988. [Google Scholar] [CrossRef]
- Popova, N.R.; Popov, A.L.; Ermakov, A.M.; Reukov, V.V.; Ivanov, V.K. Ceria-Containing Hybrid Multilayered Microcapsules for Enhanced Cellular Internalisation with High Radioprotection Efficiency. Molecules 2020, 25, 2957. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Chen, X.; Liu, H. A facile approach for synthesis of nano-CeO2 particles loaded co-polymer matrix and their colossal role for blood-brain barrier permeability in Cerebral Ischemia. J. Photochem. Photobiol. B Biol. 2018, 187, 184–189. [Google Scholar] [CrossRef]
- Mehta, A.; Scammon, B.; Shrake, K.; Bredikhin, M.; Gil, D.; Shekunova, T.; Baranchikov, A.; Ivanov, V.; Reukov, V. Nanoceria: Metabolic interactions and delivery through PLGA-encapsulation. Mater. Sci. Eng. C 2020, 114, 111003. [Google Scholar] [CrossRef]
- More, N.; Ranglani, D.; Kharche, S.; Kapusetti, G. Electrospun mat of thermal-treatment-induced nanocomposite hydrogel of polyvinyl alcohol and cerium oxide for biomedical applications. J. Appl. Polym. Sci. 2020, 137, 49426. [Google Scholar] [CrossRef]
- Mandoli, C.; Pagliari, F.; Pagliari, S.; Forte, G.; Di Nardo, P.; Licoccia, S.; Traversa, E. Stem Cell Aligned Growth Induced by CeO2 Nanoparticles in PLGA Scaffolds with Improved Bioactivity for Regenerative Medicine. Adv. Funct. Mater. 2010, 20, 1617–1624. [Google Scholar] [CrossRef]
- Xu, Z.; Xu, Y.; Basuthakur, P.; Patra, C.R.; Ramakrishna, S.; Liu, Y.; Thomas, V.; Nanda, H.S. Fibro-porous PLLA/gelatin composite membrane doped with cerium oxide nanoparticles as bioactive scaffolds for future angiogenesis. J. Mater. Chem. B 2020, 8, 9110–9120. [Google Scholar] [CrossRef] [PubMed]
- Abuid, N.J.; Gattás-Asfura, K.M.; Schofield, E.A.; Stabler, C.L. Layer-by-Layer Cerium Oxide Nanoparticle Coating for Antioxidant Protection of Encapsulated Beta Cells. Adv. Healthc. Mater. 2019, 8, 1801493. [Google Scholar] [CrossRef] [PubMed]
- Unnithan, A.R.; Ramachandra Kurup Sasikala, A.; Sathishkumar, Y.; Lee, Y.S.; Park, C.H.; Kim, C.S. Nanoceria doped electrospun antibacterial composite mats for potential biomedical applications. Ceram. Int. 2014, 40, 12003–12012. [Google Scholar] [CrossRef]
- Wan, Y.; Hong, L.; Jia, S.; Huang, Y.; Zhu, Y.; Wang, Y.; Jiang, H. Synthesis and characterization of hydroxyapatite–bacterial cellulose nanocomposites. Compos. Sci. Technol. 2006, 66, 1825–1832. [Google Scholar] [CrossRef]
- Karakoti, A.S.; Tsigkou, O.; Yue, S.; Lee, P.D.; Stevens, M.M.; Jones, J.R.; Seal, S. Rare earth oxides as nanoadditives in 3-D nanocomposite scaffolds for bone regeneration. J. Mater. Chem. 2010, 20, 8912. [Google Scholar] [CrossRef]
- Jun, I.; Han, H.-S.; Edwards, J.; Jeon, H. Electrospun Fibrous Scaffolds for Tissue Engineering: Viewpoints on Architecture and Fabrication. Int. J. Mol. Sci. 2018, 19, 745. [Google Scholar] [CrossRef]
- Jain, A.; Behera, M.; Mahapatra, C.; Sundaresan, N.R.; Chatterjee, K. Nanostructured polymer scaffold decorated with cerium oxide nanoparticles toward engineering an antioxidant and anti-hypertrophic cardiac patch. Mater. Sci. Eng. C 2021, 118, 111416. [Google Scholar] [CrossRef] [PubMed]
- Narruddin, W.N.H.B.; Jaganathan, S.K.; Khudzari, A.Z.M.; Ismail, A.F. Effect of solvent on the physicochemical properties of electrospun nanocomposite with gamat oil and cerium oxide for potential medical engineering application. J. Text. Inst. 2020, 1–10. [Google Scholar] [CrossRef]
- You, M.; Li, K.; Xie, Y.; Huang, L.; Zheng, X. The Effects of Cerium Valence States at Cerium Oxide Coatings on the Responses of Bone Mesenchymal Stem Cells and Macrophages. Biol. Trace Elem. Res. 2017, 179, 259–270. [Google Scholar] [CrossRef] [PubMed]
- Zarrintaj, P.; Moghaddam, A.S.; Manouchehri, S.; Atoufi, Z.; Amiri, A.; Amirkhani, M.A.; Nilforoushzadeh, M.A.; Saeb, M.R.; Hamblin, M.R.; Mozafari, M. Can regenerative medicine and nanotechnology combine to heal wounds? The search for the ideal wound dressing. Nanomedicine 2017, 12, 2403–2422. [Google Scholar] [CrossRef]
- Joseph, B.; Augustine, R.; Kalarikkal, N.; Thomas, S.; Seantier, B.; Grohens, Y. Recent advances in electrospun polycaprolactone based scaffolds for wound healing and skin bioengineering applications. Mater. Today Commun. 2019, 19, 319–335. [Google Scholar] [CrossRef]
- Hu, M.; Korschelt, K.; Viel, M.; Wiesmann, N.; Kappl, M.; Brieger, J.; Landfester, K.; Thérien-Aubin, H.; Tremel, W. Nanozymes in Nanofibrous Mats with Haloperoxidase-like Activity To Combat Biofouling. ACS Appl. Mater. Interfaces 2018, 10, 44722–44730. [Google Scholar] [CrossRef]
- Youngblood, R.L.; Truong, N.F.; Segura, T.; Shea, L.D. It’s All in the Delivery: Designing Hydrogels for Cell and Non-viral Gene Therapies. Mol. Ther. 2018, 26, 2087–2106. [Google Scholar] [CrossRef]
- Silina, E.V.; Manturova, N.E.; Vasin, V.I.; Artyushkova, E.B.; Khokhlov, N.V.; Ivanov, A.V.; Stupin, V.A. Efficacy of A Novel Smart Polymeric Nanodrug in the Treatment of Experimental Wounds in Rats. Polymers 2020, 12, 1126. [Google Scholar] [CrossRef]
- Microcapsules and Nanoparticles in Medicine and Pharmacy, 1st ed.; CRC Press LLC: Boca Raton, FL, USA, 1992; ISBN 9780367244057.
- Mott, L.A. Towards the Rational Design and Application of Polymers for Gene Therapy: Internalization and Intracellular Fate. Ph.D. Thesis, University of Kentucky, Lexington, KY, USA, 2019. [Google Scholar]
- Yang, T.; Wu, T.; Lv, L.; Zhang, Z.; Liu, D.; Xu, J.; Chen, D.; Wu, G. Ceria Oxide Nanoparticles an Ideal Carrier Given Little Stress to Cells and Rats. J. Nanosci. Nanotechnol. 2018, 18, 3865–3869. [Google Scholar] [CrossRef]
- Mourya, V.K.; Inamdar, N.N. Trimethyl chitosan and its applications in drug delivery. J. Mater. Sci. Mater. Med. 2009, 20, 1057–1079. [Google Scholar] [CrossRef]
- Mohammad, F.; Arfin, T.; Al-Lohedan, H.A. Enhanced biological activity and biosorption performance of trimethyl chitosan-loaded cerium oxide particles. J. Ind. Eng. Chem. 2017, 45, 33–43. [Google Scholar] [CrossRef]
- Kishor, S.; Harini, K.; Vinoth, K.G.; Suresh, B.K.; Vinayak, S.; Shilpa, S. Folic acid conjugated amine functionalized cerium oxide nanoparticle for cancer targeted gene therapy. Front. Bioeng. Biotechnol. 2016, 4. [Google Scholar] [CrossRef]
- Hasanzadeh, L.; Darroudi, M.; Ramezanian, N.; Zamani, P.; Aghaee-Bakhtiari, S.H.; Nourmohammadi, E.; Kazemi Oskuee, R. Polyethylenimine-associated cerium oxide nanoparticles: A novel promising gene delivery vector. Life Sci. 2019, 232, 116661. [Google Scholar] [CrossRef] [PubMed]
- Zholobak, N.M.; Mironenko, A.P.; Shcherbakov, A.B.; Shydlovska, O.A.; Spivak, M.Y.; Radchenko, L.V.; Marinin, A.I.; Ivanova, O.S.; Baranchikov, A.E.; Ivanov, V.K. Cerium dioxide nanoparticles increase immunogenicity of the influenza vaccine. Antivir. Res. 2016, 127, 1–9. [Google Scholar] [CrossRef]
- Popova, N.R.; Popov, A.L.; Shcherbakov, A.B.; Ivanov, V.K. Layer-by-layer capsules as smart delivery systems of CeO2 nanoparticle-based theranostic agents. Nanosyst. Phys. Chem. Math. 2017, 282–289. [Google Scholar] [CrossRef]
- Popov, A.L.; Popova, N.R.; Tarakina, N.V.; Ivanova, O.S.; Ermakov, A.M.; Ivanov, V.K.; Sukhorukov, G.B. Intracellular Delivery of Antioxidant CeO2 Nanoparticles via Polyelectrolyte Microcapsules. ACS Biomater. Sci. Eng. 2018, 4, 2453–2462. [Google Scholar] [CrossRef]
- Armentano, I.; Dottori, M.; Fortunati, E.; Mattioli, S.; Kenny, J.M. Biodegradable polymer matrix nanocomposites for tissue engineering: A review. Polym. Degrad. Stab. 2010, 95, 2126–2146. [Google Scholar] [CrossRef]
- Mecking, S. Nature or Petrochemistry?—Biologically Degradable Materials. Angew. Chem. Int. Ed. 2004, 43, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Phua, S.K.; Castillo, E.; Anderson, J.M.; Hiltner, A. Biodegradation of a polyurethanein vitro. J. Biomed. Mater. Res. 1987, 21, 231–246. [Google Scholar] [CrossRef]
- Korschelt, K.; Schwidetzky, R.; Pfitzner, F.; Strugatchi, J.; Schilling, C.; von der Au, M.; Kirchhoff, K.; Panthöfer, M.; Lieberwirth, I.; Tahir, M.N.; et al. CeO2−x nanorods with intrinsic urease-like activity. Nanoscale 2018, 10, 13074–13082. [Google Scholar] [CrossRef]
- Zholobak, N.M.; Ivanov, V.K.; Shcherbakov, A.B. Interaction of nanoceria with microorganisms. In Nanobiomaterials in Antimicrobial Therapy; Elsevier: Amsterdam, The Netherlands, 2016; pp. 419–450. [Google Scholar]
- Qi, M.; Li, W.; Zheng, X.; Li, X.; Sun, Y.; Wang, Y.; Li, C.; Wang, L. Cerium and Its Oxidant-Based Nanomaterials for Antibacterial Applications: A State-of-the-Art Review. Front. Mater. 2020, 7. [Google Scholar] [CrossRef]
- Shah, V.; Shah, S.; Shah, H.; Rispoli, F.J.; McDonnell, K.T.; Workeneh, S.; Karakoti, A.; Kumar, A.; Seal, S. Antibacterial Activity of Polymer Coated Cerium Oxide Nanoparticles. PLoS ONE 2012, 7, e47827. [Google Scholar] [CrossRef] [PubMed]
- Qian, L.-W.; Fourcaudot, A.B.; Chen, P.; Brandenburg, K.S.; Weaver, A.J.; Leung, K.P. Cerium nitrate enhances anti-bacterial effects and imparts anti-inflammatory properties to silver dressings in a rat scald burn model. Int. J. Burns Trauma 2020, 10, 91–100. [Google Scholar] [PubMed]
- Thill, A.; Zeyons, O.; Spalla, O.; Chauvat, F.; Rose, J.; Auffan, M.; Flank, A.M. Cytotoxicity of CeO2 Nanoparticles for Escherichia coli. Physico-Chemical Insight of the Cytotoxicity Mechanism. Environ. Sci. Technol. 2006, 40, 6151–6156. [Google Scholar] [CrossRef]
- Pelletier, D.A.; Suresh, A.K.; Holton, G.A.; McKeown, C.K.; Wang, W.; Gu, B.; Mortensen, N.P.; Allison, D.P.; Joy, D.C.; Allison, M.R.; et al. Effects of Engineered Cerium Oxide Nanoparticles on Bacterial Growth and Viability. Appl. Environ. Microbiol. 2010, 76, 7981–7989. [Google Scholar] [CrossRef]
- Fang, X.; Yu, R.; Li, B.; Somasundaran, P.; Chandran, K. Stresses exerted by ZnO, CeO2 and anatase TiO2 nanoparticles on the Nitrosomonas europaea. J. Colloid Interface Sci. 2010, 348, 329–334. [Google Scholar] [CrossRef]
- Shabrandi, A.; Azizi, S.; Hobbenaghi, R.; Ownagh, A.; Keshipour, S. The healing effect of chitosan supported nano-CeO2 on experimental excisional wound infected with pseudomonas aeruginosa in rat. Iran. J. Vet. Surg. 2017, 12, 9–20. [Google Scholar] [CrossRef]
- Fei, Y.; Huang, Q.; Hu, Z.; Yang, X.; Yang, B.; Liu, S. Biomimetic Cerium Oxide Loaded Gelatin PCL Nanosystems for Wound Dressing on Cutaneous Care Management of Multidrug-Resistant Bacterial Wound Healing. J. Clust. Sci. 2020. [Google Scholar] [CrossRef]
- Zholobak, N.M.; Olevinskaia, Z.M.; Spivak, N.I.; Shcherbakov, A.B.; Ivanov, V.K.; Usatenko, A.V. Antiviral effect of cerium dioxide nanoparticles stabilized by low-molecular polyacrylic acid. Mikrobiol. Z. 1993, 72, 42–47. [Google Scholar]
- Shydlovska, O.; Kharchenko, E.; Osenniy, I.; Spivak, M.; Shcherbakov, A.; Zholobak, N. Nanoparticles of cerium dioxide—An effective antiviral agent and adjuvant of biologically active molecules. Sci. Biol. Sci. 2018, 26–30. [Google Scholar] [CrossRef][Green Version]
- Zholobak, N.M.; Shcherbakov, A.B.; Vitukova, E.O.; Yegorova, A.V.; Scripinets, Y.V.; Leonenko, I.I.; Baranchikov, A.Y.; Antonovich, V.P.; Ivanov, V.K. Direct monitoring of the interaction between ROS and cerium dioxide nanoparticles in living cells. RSC Adv. 2014, 4, 51703–51710. [Google Scholar] [CrossRef]
- Mohamed, H.E.A.; Afridi, S.; Khalil, A.T.; Ali, M.; Zohra, T.; Akhtar, R.; Ikram, A.; Shinwari, Z.K.; Maaza, M. Promising antiviral, antimicrobial and therapeutic properties of green nanoceria. Nanomedicine 2020, 15, 467–488. [Google Scholar] [CrossRef] [PubMed]
- Allawadhi, P.; Khurana, A.; Allwadhi, S.; Joshi, K.; Packirisamy, G.; Bharani, K.K. Nanoceria as a possible agent for the management of COVID-19. Nano Today 2020, 35, 100982. [Google Scholar] [CrossRef]
- Shcherbakov, A.B.; Zholobak, N.M.; Spivak, N.Y.; Ivanov, V.K. Advances and prospects of using nanocrystalline ceria in cancer theranostics. Russ. J. Inorg. Chem. 2014, 59, 1556–1575. [Google Scholar] [CrossRef]
- Ibrahim Fouad, G. A proposed insight into the anti-viral potential of metallic nanoparticles against novel coronavirus disease-19 (COVID-19). Bull. Natl. Res. Cent. 2021, 45, 36. [Google Scholar] [CrossRef]
- Nguyet, N.T.; Van Thu, V.; Lan, H.; Trung, T.; Le, A.-T.; Pham, V.-H.; Tam, P.D. Simple Label-Free DNA Sensor Based on CeO2 Nanorods Decorated with Ppy Nanoparticles. J. Electron. Mater. 2019, 48, 6231–6239. [Google Scholar] [CrossRef]
- Sun, X.; Jian, Y.; Wang, H.; Ge, S.; Yan, M.; Yu, J. Ultrasensitive Microfluidic Paper-Based Electrochemical Biosensor Based on Molecularly Imprinted Film and Boronate Affinity Sandwich Assay for Glycoprotein Detection. ACS Appl. Mater. Interfaces 2019, 11, 16198–16206. [Google Scholar] [CrossRef]
- Fu, J. Sensitive Acetylcholinesterase Biosensor Based on Screen- Printed Carbon Electrode Modified with Cerium Oxide- Chitosan/Mesoporous Carbon-Chitosan for Organophosphorus Pesticide Residue Detection. Int. J. Electrochem. Sci. 2018, 9231–9241. [Google Scholar] [CrossRef]
- Zhang, Z.; Zhang, X.; Liu, B.; Liu, J. Molecular Imprinting on Inorganic Nanozymes for Hundred-fold Enzyme Specificity. J. Am. Chem. Soc. 2017, 139, 5412–5419. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.; Lee, J.; Won, B.Y.; Kim, S.; Shin, S.; Kim, M.I.; Park, H.G. Fabrication of conductive oxidase-entrapping nanocomposite of mesoporous ceria–carbon for efficient electrochemical biosensor. RSC Adv. 2015, 5, 78747–78753. [Google Scholar] [CrossRef]
- Ansari, A.A.; Sumana, G.; Khan, R.; Malhotra, B.D. Polyaniline-Cerium Oxide Nanocomposite for Hydrogen Peroxide Sensor. J. Nanosci. Nanotechnol. 2009, 9, 4679–4685. [Google Scholar] [CrossRef]
- De, S.; Mohanty, S.; Nayak, S.K. Nano-CeO2 decorated graphene based chitosan nanocomposites as enzymatic biosensing platform: Fabrication and cellular biocompatibility assessment. Bioprocess Biosyst. Eng. 2015, 38, 1671–1683. [Google Scholar] [CrossRef]
- Pautler, R.; Kelly, E.Y.; Huang, P.-J.J.; Cao, J.; Liu, B.; Liu, J. Attaching DNA to Nanoceria: Regulating Oxidase Activity and Fluorescence Quenching. ACS Appl. Mater. Interfaces 2013, 5, 6820–6825. [Google Scholar] [CrossRef]
- Wang, Q.; Gao, F.; Zhang, X.; Zhang, B.; Li, S.; Hu, Z.; Gao, F. Electrochemical characterization and DNA sensing application of a sphere-like CeO2–ZrO2 and chitosan nanocomposite formed on a gold electrode by one-step electrodeposition. Electrochim. Acta 2012, 62, 250–255. [Google Scholar] [CrossRef]
- Song, Y.; Wei, W.; Qu, X. Colorimetric Biosensing Using Smart Materials. Adv. Mater. 2011, 23, 4215–4236. [Google Scholar] [CrossRef]
- Lang, N.J.; Liu, B.; Liu, J. Characterization of glucose oxidation by gold nanoparticles using nanoceria. J. Colloid Interface Sci. 2014, 428, 78–83. [Google Scholar] [CrossRef]
- Chi, M.; Zhu, Y.; Yang, Z.; Gao, M.; Chen, S.; Song, N.; Wang, C.; Lu, X. Strongly coupled CeO2/Co3O4/poly(3,4-ethylenedioxythiophene) nanofibers with enhanced nanozyme activity for highly sensitive colorimetric detection. Nanotechnology 2017, 28, 295704. [Google Scholar] [CrossRef]
- Zeng, H.-H.; Qiu, W.-B.; Zhang, L.; Liang, R.-P.; Qiu, J.-D. Lanthanide Coordination Polymer Nanoparticles as an Excellent Artificial Peroxidase for Hydrogen Peroxide Detection. Anal. Chem. 2016, 88, 6342–6348. [Google Scholar] [CrossRef]
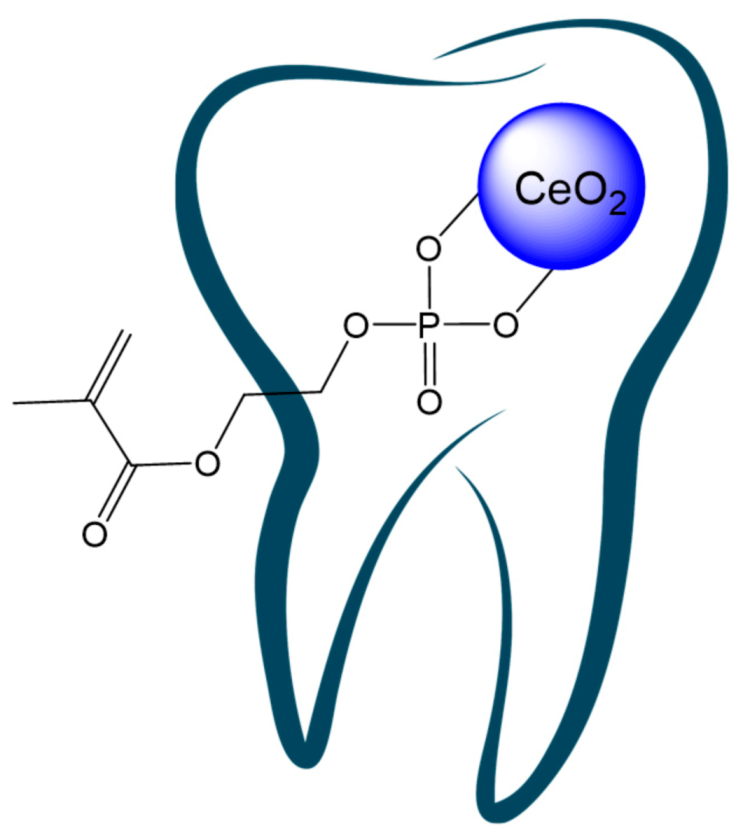
- Mahapatra, C.; Singh, R.K.; Lee, J.-H.; Jung, J.; Hyun, J.K.; Kim, H.-W. Nano-shape varied cerium oxide nanomaterials rescue human dental stem cells from oxidative insult through intracellular or extracellular actions. Acta Biomater. 2017, 50, 142–153. [Google Scholar] [CrossRef]
- Garcia, I.M.; Leitune, V.C.B.; Takimi, A.S.; Bergmann, C.P.; Samuel, S.M.W.; Melo, M.A.; Collares, F.M. Cerium Dioxide Particles to Tune Radiopacity of Dental Adhesives: Microstructural and Physico-Chemical Evaluation. J. Funct. Biomater. 2020, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, C.; Passos Farias, I.; Reis Albuquerque, A.; e Silva, P.; Costa One, G.; Sampaio, F. Antimicrobial activity of nano cerium oxide (IV) (CeO2) against Streptococcus mutans. BMC Proc. 2014, 8, P48. [Google Scholar] [CrossRef]
- Holmes, D.R.; Kereiakes, D.J.; Garg, S.; Serruys, P.W.; Dehmer, G.J.; Ellis, S.G.; Williams, D.O.; Kimura, T.; Moliterno, D.J. Stent Thrombosis. J. Am. Coll. Cardiol. 2010, 56, 1357–1365. [Google Scholar] [CrossRef]
- Jaffer, I.H.; Fredenburgh, J.C.; Hirsh, J.; Weitz, J.I. Medical device-induced thrombosis: What causes it and how can we prevent it? J. Thromb. Haemost. 2015, 13, S72–S81. [Google Scholar] [CrossRef]
- Thies, H. Cerium as an anticoagulant. Ther. Ggw. 1957, 96, 411–412. [Google Scholar]
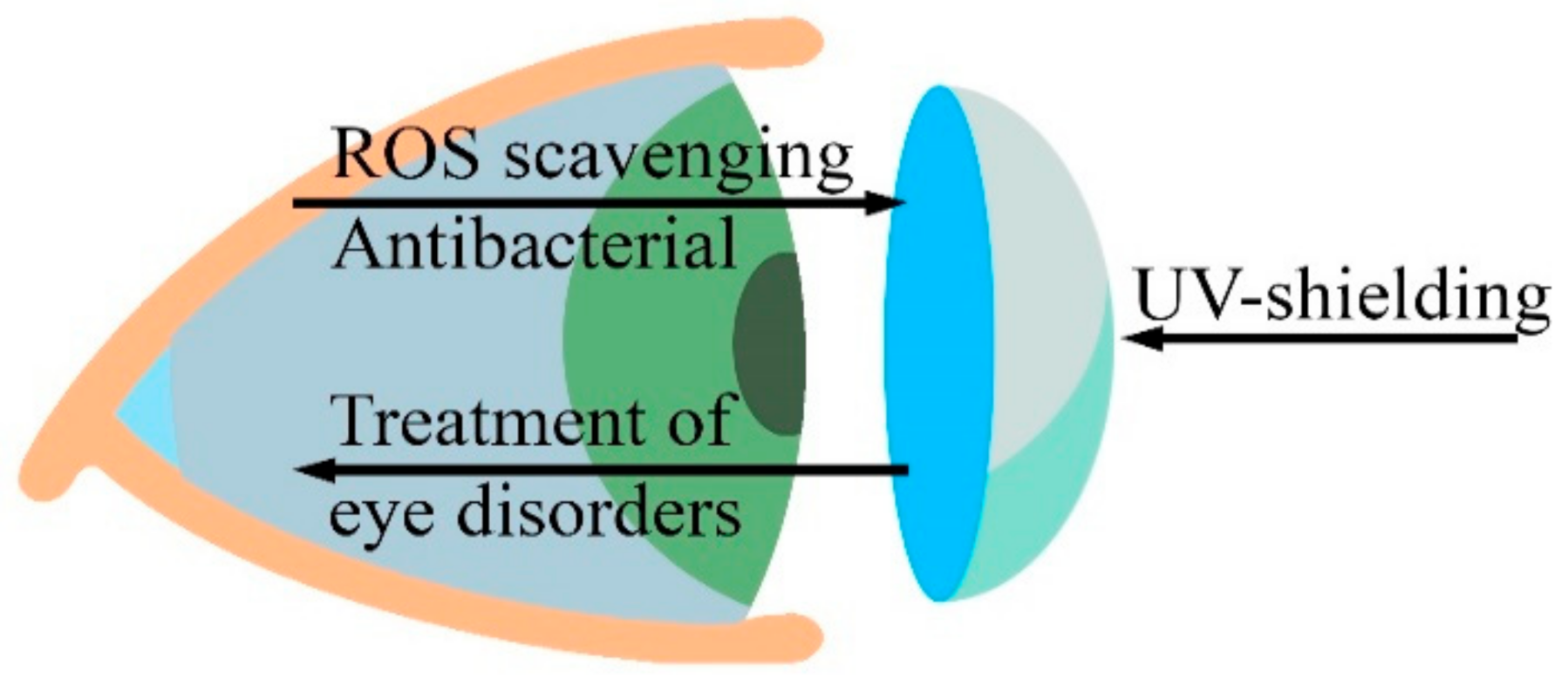
- Maccarone, R.; Tisi, A.; Passacantando, M.; Ciancaglini, M. Ophthalmic Applications of Cerium Oxide Nanoparticles. J. Ocul. Pharmacol. Ther. 2020, 36, 376–383. [Google Scholar] [CrossRef]
- Chen, J.; Patil, S.; Seal, S.; McGinnis, J.F. Rare earth nanoparticles prevent retinal degeneration induced by intracellular peroxides. Nat. Nanotechnol. 2006, 1, 142–150. [Google Scholar] [CrossRef]
- Kyosseva, S. V Cerium oxide nanoparticles as promising ophthalmic therapeutics for the treatment of retinal diseases. World J. Ophthalmol. 2015, 5, 23. [Google Scholar] [CrossRef]
- Matsuda, S.; Ikada, Y. Glues. Concise Encyclopedia of Biomedical Polymers and Polymeric Biomaterials; CRC Press: Boca Raton, FL, USA, 2017; pp. 644–652. [Google Scholar]
- Shahinpoor, M.; Kim, K.J.; Mojarrad, M. Artificial Muscles; CRC Press: Boca Raton, FL, USA, 2007; ISBN 9780429140792. [Google Scholar]
- Junais, P.M.; Govindaraj, G. Conduction and dielectric relaxations in PVA/PVP hydrogel synthesized cerium oxide. Mater. Res. Express 2019, 6, 045914. [Google Scholar] [CrossRef]
- Parvatikar, N.; Ambika Prasad, M.V.N. Frequency-dependent conductivity and dielectric permittivity of polyaniline/CeO2 composites. J. Appl. Polym. Sci. 2006, 100, 1403–1405. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, S.; Yuan, S.; Wang, D.; Hu, P.-H.; Dang, Z.-M. Low dielectric loss and weak frequency dependence of dielectric permittivity of the CeO2/polystyrene nanocomposite films. Appl. Phys. Lett. 2014, 105, 052905. [Google Scholar] [CrossRef]
- Ushakov, N.M.; Yurkov, G.Y.; Gorobinskii, L.V.; Popkov, O.V.; Kosobudskii, I.D. Nanocomposites based on the cerium oxide nanoparticles and polyethylene matrix: Syntheses and properties. Acta Mater. 2008, 56, 2336–2343. [Google Scholar] [CrossRef]
- Park, J.-S.; Choi, J.S. Gene Carriers: Design Elements. Concise Encyclopedia of Biomedical Polymers and Polymeric Biomaterials; CRC Press: Boca Raton, FL, USA, 2017; pp. 623–632. [Google Scholar]
- Tong, R.; Cheng, J. Anticancer Polymeric Nanomedicines. Polym. Rev. 2007, 47, 345–381. [Google Scholar] [CrossRef]
- Zhu, H.; Fang, Y.; Miao, Q.; Qi, X.; Ding, D.; Chen, P.; Pu, K. Regulating Near-Infrared Photodynamic Properties of Semiconducting Polymer Nanotheranostics for Optimized Cancer Therapy. ACS Nano 2017, 11, 8998–9009. [Google Scholar] [CrossRef]
- Russo, T.; De Santis, R.; Gloria, A.; Barbaro, K.; Altigeri, A.; Fadeeva, I.V.; Rau, J.V. Modification of PMMA Cements for Cranioplasty with Bioactive Glass and Copper Doped Tricalcium Phosphate Particles. Polymers 2019, 12, 37. [Google Scholar] [CrossRef]
- Pikis, S.; Goldstein, J.; Spektor, S. Potential neurotoxic effects of polymethylmethacrylate during cranioplasty. J. Clin. Neurosci. 2015, 22, 139–143. [Google Scholar] [CrossRef]
- Najafi, R.; Hosseini, A.; Ghaznavi, H.; Mehrzadi, S.; Sharifi, A.M. Neuroprotective effect of cerium oxide nanoparticles in a rat model of experimental diabetic neuropathy. Brain Res. Bull. 2017, 131, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Rzigalinski, B.A.; Carfagna, C.S.; Ehrich, M. Cerium oxide nanoparticles in neuroprotection and considerations for efficacy and safety. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2017, 9, e1444. [Google Scholar] [CrossRef]
- Estevez, A.Y.; Pritchard, S.; Harper, K.; Aston, J.W.; Lynch, A.; Lucky, J.J.; Ludington, J.S.; Chatani, P.; Mosenthal, W.P.; Leiter, J.C.; et al. Neuroprotective mechanisms of cerium oxide nanoparticles in a mouse hippocampal brain slice model of ischemia. Free Radic. Biol. Med. 2011, 51, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Huang, Q.; Chen, H.; Chen, X.; Long, G. A Fractal Model For Capillary Flow Through A Single Tortuous Capillary With Roughened Surfaces In Fibrous Porous Media. Fractals 2021, 29, 2150017. [Google Scholar] [CrossRef]
- Xiao, B.; Zhang, Y.; Wang, Y.; Jiang, G.; Liang, M.; Chen, X.; Long, G. A Fractal Model For Kozeny–Carman Constant And Dimensionless Permeability Of Fibrous Porous Media With Roughened Surfaces. Fractals 2019, 27, 1950116. [Google Scholar] [CrossRef]
- Xiao, B.; Wang, W.; Zhang, X.; Long, G.; Fan, J.; Chen, H.; Deng, L. A novel fractal solution for permeability and Kozeny-Carman constant of fibrous porous media made up of solid particles and porous fibers. Powder Technol. 2019, 349, 92–98. [Google Scholar] [CrossRef]
- Ouyang, Z.; Mainali, M.K.; Sinha, N.; Strack, G.; Altundal, Y.; Hao, Y.; Winningham, T.A.; Sajo, E.; Celli, J.; Ngwa, W. Potential of using cerium oxide nanoparticles for protecting healthy tissue during accelerated partial breast irradiation (APBI). Phys. Med. 2016, 32, 631–635. [Google Scholar] [CrossRef]
- Chakravarty, R.; Shukla, R.; Ram, R.; Venkatesh, M.; Dash, A.; Tyagi, A.K. Nanoceria-PAN Composite-Based Advanced Sorbent Material: A Major Step Forward in the Field of Clinical-Grade 68Ge/68Ga Generator. ACS Appl. Mater. Interfaces 2010, 2, 2069–2075. [Google Scholar] [CrossRef]

| Polymer | CeNPs Characteristics and Content (w/v%) | Nanocomposite Products | Applications | Results | Ref. |
|---|---|---|---|---|---|
| Tissue engineering | |||||
| Cellulose | Cubic CeNPs, 3.2–32 nm; 300 mL of water containing 1- or 5-mM cerium nitrate and 1% cellulose was used as a precursor. | Three-dimensional scaffolds | Tissue engineering | Nanobiocomposites are not cytotoxic to HeLa cells at a concentration as high as >1 mg·mL−1 and scavenge ROS. | [48] |
| PCL | Size 9–16 nm; 0.5%, 1%, 2% and 3%. | Electrospun fiber scaffolds | Tissue engineering | In vitro (MSC): higher cell adhesion and proliferation were evident relative to bare PCL. In vivo (rats): high cell proliferation rate and blood formation. Angiogenesis was activated by HIF-1α, as shown by the upregulation of VEGF expression in the nanocomposite scaffolds. | [55] |
| PL | CeNPs having different Ce4+ and Ce3+ ratios | Scaffold/artificial-niche | Tissue engineering | Mesenchymal stem (MSCs) and osteoblast-like (MG63) cells were cultured on PL/CNP surfaces with Ce4+- or Ce3+-enriched regions. Despite cell type (MSCs and MG63 cells), different cerium valence state regions promoted or inhibited cell spreading, migration or adhesion behavior, resulting in rapid or slow cell proliferation. | [56] |
| PL | ~5 nm, oleylamine-capped CeNPs, up to 10 wt%: cancellous bone impregnated by PL + CeNPs | Scaffolds | Bone tissue engineering | In vitro: coculture of endothelial progenitor cells and MSC on scaffold supplemented with CeNPs showed the improvement of cell viability and the differentiation process for endothelial progenitor cells. In vivo (mice): higher level of vascularization for scaffold supplemented with CeNPs in comparison with the bare scaffold. | [57] |
| Gelatin | CeNPs by AlfaAesar as a 20% aqueous solution at acidic pH, with nominal size <5 nm. 15% gelatin and 1 mg/mL CeNPs were used as a precursor, GPTMS as a cross-linker | Electrospun fiber scaffolds | Neuronal tissue engineering and regenerative medicine | The scaffolds demonstrate strong antioxidant properties and beneficial multi-cue effects in terms of neurite development and alignment on neuron-like SH-SY5Y cells. | [58] |
| Gelatin/alginate | Mean diameter 35.5 nm, zeta potential −12.35 ± 1.39 mV; 100 μg/mL, 500 μg/mL and 1000 μg/mL | Scaffolds | Bone regeneration | Highest mesenchymal stem cells (MSCs) proliferation rate was observed for 1000 μg/mL CeNPs scaffolds; application of the scaffolds resulted in enhanced osteogenic differentiation of MSCs, as well as free radical scavenging. | [59] |
| POC | <25 nm particle size (Sigma-Aldrich), 10 or 20 wt% relative to POC | Scaffolds | Bone tissue regeneration | Scaffolds are biocompatible and supported cell attachment, proliferation, mineralization and infiltration. They possess protective properties against ROS via the reduction in cytotoxicity, improving mineralization of osteoblast cells in vitro. Cells are able to infiltrate through the scaffolds, the surrounding tissues elicit a minimal immune response. Nanocomposite scaffold system is capable of supporting bone-remodeling processes while providing a protective free radical scavenging effect. | [60] |
| PLGA | CeNPs size ~5 nm; 20 mg of CeNPs in 200 mg of PLGA | Microparticles and scaffolds | CeNPs delivery, tissue engineering including bone remodeling and regeneration | The release kinetics of CNPs from PLGA matrix was investigated under acidic, basic and near-neutral pHs. Superoxide dismutase (SOD) mimetic activity was retained in released CNPs for a long period of time (∼90 days). PLGA encapsulated CeNPs showed excellent biocompatibility. | [61] |
| Wound healing/dressing | |||||
| Chitosan/PVA | zeta potential 50 mV, ∼5 nm in diameter, 0.5% and 1% | Hydrogels | Wound healing | Enhanced cell compatibility and survival, antibacterial activity against MRSA | [62] |
| PHBV | 8.6 ± 3.8 nm in diameter (TEM); 0.5%, 1%, 2% and 4% | Electrospun membranes | Diabetic wound healing | In vitro: For less than 1% w/w of CeNPs content, human mammary epithelial cells adhered parallel to individual fibers; for higher CeNPs content, cells started to flatten and spread over the fibers. In ovo: enhanced blood vessel formation. In vivo (rats): promotes healing of diabetic wounds | [63] |
| Chitosan/cellulose acetate | <25 nm particle size (Sigma-Aldrich), 0.1% and 1% | Films | Wound dressing | Good water vapour transmission rates (WVTR) and water vapour permeability (WVP) values, antibacterial behavior for S. aureus and E. coli. | [64] |
| PCL/gelatin (1:1) | <25 nm particle size, 1.5, 3 and 6% | Electrospun films | Wound dressing | In vitro: 1.5% CeNPs exhibited the highest cell proliferation with L929 cells. In vivo: 1.5% CeNPs accelerated wound healing compared with the sterile gauze. | [65] |
| PCL/gelatin (1:1) | ~42 nm in size, zeta potential 30.8 mV. The nanofibers were fabricated from a polymer solution of 10% w/v PCL, 20% w/v gelatin and 25% v/v 30 mM CeNPs | Electrospun fibers | Wound healing | Enhanced proliferation of 3T3-L1 cells (by ~48%), ROS scavenging ability, three-fold increase in the viability and proliferation of cells. | [66] |
| Gelatin | 2.5–6.5 nm in size. From 50 μg/mL to 500 μg/mL dispersed into gelatin solution (5%, w/v), optimal concentration 250 μg/mL | Composite hydrogels | Wound healing | In vitro: 250 μg/mL provided 86 ± 1.4% cell viability and increased bound water content (swelling ratio was three-fold to that of native gelatin). In vivo (rats): more infiltration of leukocytes and larger deposition of collagen, the wound was healed in 12 days. | [67] |
| GelMA-DOPA | 10–30 nm in size (US Research Nanomaterials), 100.0 μg/mL | Sprayable hydrogel | Wound dressing | Hydrogel provided a multifunctional wound dressing with desired antimicrobial, ROS-scavenging, adhesive, and degradative properties both in vitro and in vivo. | [68] |
| PCL | Mesoporous CeO2 nanorods, 5–25%, optimal 15% | Nanomembranes | Cutaneous wound healing | High antimicrobial activity against E. coli and S. aureus, strong wound healing effect, good biocompatibility. | [69] |
| Zwitterionic cryogel of CBMA or SBMA and HEMA | CeNPs size range of 3–5 nm; 68 μL of aqueous 36.6 μM FITC-labelled CeNPs were added to 250 μL of gel prior to polymerization | Injectable gels | Wound healing | The gels speed up diabetic wound healing and significantly reduce inflammation. | [70] |
| Gelatin/oxidized dextran | Particle size < 50 nm, 430 ug in 1 mL of gel | Hydrogel dressings | Wound healing | Prolonged drug (curcumin) release (∼63% in 108 h), accelerated cell migration, significant antioxidant and anti-inflammatory activity in vivo (∼39%). | [71] |
| PAA/curcumin | 220 by 30–75 nm CeNPs; 0.1 mM, 0.2 mM and 0.4 mM | Hydrogel dressings | Scarless healing of injury | In a full-thickness acute wound healing model of rat, a single application of dressing demonstrated higher wound healing efficacy (78%) and negligible scarring in 7 days. Enhanced cell proliferation, higher collagen content, advanced wound maturity, re-epithelialization and granulation tissue formation were observed. | [50] |
| Drug delivery | |||||
| PArg/DS | Citrate-stabilized CeNPs, 4–7 nm, ζ-potential ~–40 mV | LbL microcapsules | Drug delivery | CeNPs provide “active” protection of loaded content (luciferase enzyme) against hydrogen peroxide and “passive” shielding against small molecules. | [72] |
| Alginate/Chitosan | Citrate-stabilized CeNPs, diameter ~5 nm, ζ-potential −16.99 ± 2.72 mV | LbL-coated silicone containers | Drug delivery | CeNPs functionality prevents burst blowout of model drug (curcumin). | [73] |
| PArg/DS | Citrate-stabilized CeNPs, 2–2.5 nm, negative ζ-potential | LbL microcapsules | Drug delivery, radioprotection | CeNPs microcapsules provide enhanced cellular internalization and good radioprotection. | [74] |
| PEG/PLGA | Mostly uniform spherical CeNPs 5–10 nm in size | ~40 nm nanoparticles | Cerebral ischemic therapy, brain targeted drug delivery | 10 mg/kg concentration resulted in 60–78% lessening of focal ischemia in middle cerebral artery occlusion model of brain stroke. | [75] |
| PLGA | Diameter of 2–3 nm; 1 μM of CeNPs was suspended in 2.5% aqueous PVA solution containing 40 mg of PLGA as a precursor | Microparticles | CeNPs and drugs co-delivery | PLGA is a suitable encapsulating carrier for simultaneous delivery of nanoceria and SOD. This combination effectively reduces oxidative stress in vitro. | [76] |
| Other biomedical applications | |||||
| PVA | 0.5, 1.5 and 3% | Electrospun mats of nanocomposite hydrogels | Various biomedical applications | Better platelet adhesion and accelerated wound healing | [77] |
| TPU | CeNPs size ∼60 nm; 0.1–0.7 wt% | Various biomedical applications | Enhanced blood compatibility, cell viability, chemical resistance, mechanical and thermal properties of TPU. | [53] | |
| Alginate | Dextran-coated CeNPs, 2.7–9 nm radius (23.8% polydispersity); 0.1, 1.0 and 10 mM CeNPs in hydrogel. | Composite hydrogel microcapsules | Cellular transplantation | Cytoprotection of encapsulated insulin-producing MIN6 beta cells from free radical attack. No cytotoxicity up to 10 mM CeNPs. | [49] |
| PLGA | 5 to 8 nm in size; 5, 10 and 20 wt% | Hybrid 2D polymeric-ceramic biosupports | Regenerative medicine | Better murine derived cardiac and mesenchymal stem cells’ proliferative activity is observed for CeO2 polymer composites with respect to either TiO2-filled or unfilled PLGA films. | [78] |
| PL/Gelatin | Polyhedral nanoparticles 5–10 nm in size; 0.25%,0.5% and 1% | Electrospun fibro-porous membranes | Scaffolds for angiogenesis | Good hydrophilicity, water absorption and improved mechanical properties; scaffolds were shown to be biocompatible both in vitro (somatic hybrid endothelial cells) and in vivo (chick embryo angiogenesis assay); pro-angiogenic activities of the scaffolds are comparable to VEGF. | [79] |
| Alginate | Particle size < 5 nm, 20 wt% in H2O, pH~4 (Sigma Aldrich) | LbL-coated alginate microbeads | Biomedical implants, including cellular transplantation | 12 layers of CeNPs/alginate provided complete protection to the entrapped beta cells from exposure to 100 μM H2O2, with no significant changes in metabolic activity, oxidant capacity or insulin secretion dynamics, when compared to untreated control. | [80] |
| PU with CA/Zein | CeO2 nanofibers were composed of nanoparticles ca.10–20 nm in size; 10% | Electrospun fiber mats | Antibacterial smart material | Composite nanofibers demonstrated notable toxicity against Escherichia coli, Klebsiella pneumoniae, Salmonella enterica (Gram-negative), Staphylococcus aureus and Enterococcus faecalis (Gram-positive) strains. | [81] |
| Improvement of Ceria Nanoparticles’ Properties | |
| Physical, chemical | Decreased CeNPs solubility and free Ce-ions leakage; Local concentration control; Surface charge control; Stimuli-related release control; Tunable microenvironment for anti/prooxidant activity control. |
| Biomedical | Decreased toxicity: Decreasing Ce-ions’ toxicity; Reducing phagocytosis; Preventing cell membrane damage. Easy-to-remove materials; Impaired clearance. |
| Improvement of polymer properties | |
| Physical | Tunable mechanical, thermal and electric properties; UV-resistance, UV-protection and shielding; Radiodensity/radiopacity; Roughness and surface energy control; Wettability, swelling and solubility control; Porosity and permeability control (liquids, gases, water vapors). |
| Chemical, biochemical | Enhanced chemical resistance, decreased erosion/corrosion, prolonged durability; Antioxidant properties: Free radicals scavenging; ROS decomposition; Oxygen buffering. Redox balance control; Enhanced biomolecules adhesion; Tunable scaffold mineralization; Mitigation of proinflammatory cytokines level. |
| Biomedical | Enhanced cell adhesion, proliferation, migration and tissue repair; Faster healing rate; Better biocompatibility; Decreased inflammation; Decreased foreign body reactions and rejections; Bactericide/bacteriostatic, fungicide, virucide activity; Enhanced implants visualization (radiocontrast); Biodegradability control. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shcherbakov, A.B.; Reukov, V.V.; Yakimansky, A.V.; Krasnopeeva, E.L.; Ivanova, O.S.; Popov, A.L.; Ivanov, V.K. CeO2 Nanoparticle-Containing Polymers for Biomedical Applications: A Review. Polymers 2021, 13, 924. https://doi.org/10.3390/polym13060924
Shcherbakov AB, Reukov VV, Yakimansky AV, Krasnopeeva EL, Ivanova OS, Popov AL, Ivanov VK. CeO2 Nanoparticle-Containing Polymers for Biomedical Applications: A Review. Polymers. 2021; 13(6):924. https://doi.org/10.3390/polym13060924
Chicago/Turabian StyleShcherbakov, Alexander B., Vladimir V. Reukov, Alexander V. Yakimansky, Elena L. Krasnopeeva, Olga S. Ivanova, Anton L. Popov, and Vladimir K. Ivanov. 2021. "CeO2 Nanoparticle-Containing Polymers for Biomedical Applications: A Review" Polymers 13, no. 6: 924. https://doi.org/10.3390/polym13060924
APA StyleShcherbakov, A. B., Reukov, V. V., Yakimansky, A. V., Krasnopeeva, E. L., Ivanova, O. S., Popov, A. L., & Ivanov, V. K. (2021). CeO2 Nanoparticle-Containing Polymers for Biomedical Applications: A Review. Polymers, 13(6), 924. https://doi.org/10.3390/polym13060924