Abstract
Despite the growing interest in possible applications of computer science and artificial intelligence (AI) in the field of neurocritical care (neuro-ICU), widespread clinical applications are still missing. In neuro-ICU, the collection and analysis in real time of large datasets can play a crucial role in advancing this medical field and improving personalized patient care. For example, AI algorithms can detect subtle changes in brain activity or vital signs, alerting clinicians to potentially life-threatening conditions and facilitating rapid intervention. Consequently, data-driven AI and predictive analytics can greatly enhance medical decision making, diagnosis, and treatment, ultimately leading to better outcomes for patients. Nevertheless, there is a significant disparity between the current capabilities of AI systems and the potential benefits and applications that could be achieved with more advanced AI technologies. This gap is usually indicated as the AI chasm. In this paper, the underlying causes of the AI chasm in neuro-ICU are analyzed, along with proposed recommendations for utilizing AI to attain a competitive edge, foster innovation, and enhance patient outcomes. To bridge the AI divide in neurocritical care, it is crucial to foster collaboration among researchers, clinicians, and policymakers, with a focus on specific use cases. Additionally, strategic investments in AI technology, education and training, and infrastructure are needed to unlock the potential of AI technology. Before implementing a technology in patient care, it is essential to conduct thorough studies and establish clinical validation in real-world environments to ensure its effectiveness and safety. Finally, the development of ethical and regulatory frameworks is mandatory to ensure the secure and efficient deployment of AI technology throughout the process.
1. Introduction
Neurocritical care, also known as neurointensive care, is a specialized medical discipline that focuses on treating severe and life-threatening neurological disorders such as stroke, traumatic brain injury, intracranial hemorrhage, and seizures. The care of critically ill patients with these disorders requires multiple intensive care approaches, including mechanical ventilation, hemodynamics monitoring, and neuroimaging. As a result, neurocritical care often involves complex decision making and requires specialized expertise and skills. Clinicians working in this field must be able to interpret advanced imaging tests, understand the pathophysiology of neurological disorders, and manage the complex medical needs of critically ill patients admitted to the neurocritical intensive care unit (neuro-ICU).
In this complex scenario, automatically interpreting large amounts of data collected through multimodal monitoring has become a critical clinical requirement to improve patient care and reduce resource consumption by facilitating clinical decision making [1]. Remarkably, the use of artificial intelligence (AI) in healthcare is growing rapidly, with an annualized growth rate of 48% [2]. Therefore, due to the improvement in technology and the analysis of vast amounts of patient data through model-based and data-driven methods, AI and machine learning (ML) have the potential to revolutionize neurocritical care [3,4,5,6].
Recently, there has been a surge in the publication of scholarly articles that focus on the applications of big data and AI in neuro-ICU. For example, Savin et al. [7] adopted ML strategies for identifying potential factors linked to the development of healthcare-associated ventriculitis and meningitis. Moreover, researchers from the Florida Institute of Technology and Rutgers University in the United States (US) implemented an interesting artificial neural network architecture for early prediction of an abnormal increase in intracranial pressure (ICP) in traumatic brain injury patients [8]. More recently, Schweingruber et al. [9] utilized a recurrent neural network method with the same aim, and Liu and co-authors [10] investigated the outcome trajectories (hospital mortality) in critically ill patients with embolic stroke. ML strategies have also been adopted for other purposes, such as improving the assessment of consciousness [11], monitoring intracranial hemorrhage [12], as well as electrophysiological analyses [13], and the prediction of both neurological recovery after neuro-ICU stay [14] and delayed cerebral ischemia after subarachnoid hemorrhage [15]. The possible applications are numerous and interesting prospects focus on the elaboration of algorithms for the prediction of ICU admission in myasthenia gravis [16], the early diagnosis of nonconvulsive seizures [17], and the development of closed-loop systems for personalized neuromodulation for individuals with drug-resistant epilepsy [18]. Furthermore, exploring the potential of chatbots to enhance neurological diagnosis and management is a fascinating and promising endeavor [19], although the current technology has significant limitations [20]. Finally, a multimodal strategy that combines biosignals with behavioral features can be used for automatic pain assessment in critically ill patients with communication barriers [21,22].
The growing interest in this area of research emphasizes the potential benefits that big data and AI can bring to the healthcare industry, highlighting the importance of the continued exploration and development of these technologies in clinical practice. AI and ML can be effectively used to develop more accurate predictive models for patient outcomes, improve real-time monitoring of patient data, and assist with treatment decisions. Nevertheless, although various dimensions in this research field have been explored, significant gaps still need to be filled. Undoubtedly, the use of AI and ML in neuro-ICU is in its early stages, and there are many challenges that need to be addressed. These include issues related to data quality and availability, the need for appropriate algorithms and models, and the ethical considerations surrounding the use of these technologies in healthcare.
The term “AI chasm” is typically used to describe the gap between the current capabilities and limitations of AI systems and the potential benefits and applications that could be achieved with more advanced AI technologies [23]. This gap creates a barrier that prevents AI from being fully integrated into many real-world applications, leading to a mismatch between the hype and expectations around AI and its actual capabilities. Notably, according to an analysis conducted in the US, only 14% of research findings are implemented into clinical practice within a span of 17 years [24]. Thus, the AI chasm is seen as a major challenge for the future development of AI, as overcoming this gap will require new breakthroughs in AI research and development [25].
Employing a narrative review of the literature, this paper summarizes the causes of the AI chasm in neurocritical care and proposes suggestions for leveraging AI to gain competitive advantages, drive innovation, and achieve better patient outcomes. A dedicated paragraph is devoted to discussing ethics problems.
2. Crossing the AI Chasm
Despite the disparate use of AI- and ML-derived strategies for improving neuro-ICU management (Table 1), the gap between the development of an algorithm and model and their application is a common problem in medicine. To overcome the problem, several strategies can be implemented. Obviously, data are the true key to AI, and in neuro-ICUs, large datasets can be collected. The vast datasets collected in neuro-ICUs provide valuable information on various aspects of patient care, including vital signs, lab results, medication dosages, neuromonitoring findings, imaging studies, and biomarkers. By analyzing these multimodal data, AI algorithms can help identify patterns and predict potential health risks, useful for improving patient outcomes (Figure 1).

Table 1.
Examples of AI-based strategies for improving neurocritical care management.
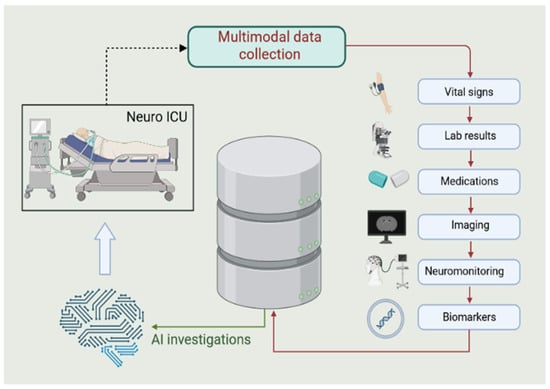
Figure 1.
Data collection in neuro-ICU. Neuro-ICUs usually gather a wealth of information that can be utilized to build extensive multimodal datasets. These repositories encompass crucial aspects of patient care such as vital signs, lab results, medication dosages, imaging studies, neuromonitoring findings, and biomarkers. The analysis of these data with AI algorithms can help identify patterns useful for improving patient outcomes. Created with BioRender.com (accessed on 8 April 2023).
Nevertheless, even if well structured, most datasets cannot fit the needs of the real AI world. Data from continuous electroencephalography (EEG), electrocorticography, cerebral microdialysis, brain tissue oxygenation, and findings from noninvasive monitoring (e.g., neuroimaging) must implement well-designed datasets and continually update the model.
For example, the DENDRITe (Data Exploration and Navigation for Discovery, Retrieval, and Information Transmission) data repository project from Duke University is a multisource neuro-ICU dataset (e.g., genomics, proteomics, imaging, and clinical data) that is updated daily [26]. Thus, the challenge of data management requires ad hoc upstream investments and resource allocation. Investments are also warranted to overcome nonnegligible engineering problems such as stability, updating, restoring, and backup.
The possibility of using public repositories represents a necessary step that the scientific community must consider. This implies the need to release datasets for public access, although it can be challenging to determine whether this goal is achievable. As Azard et al. [27] suggested, the eICU Collaborative Research Database is a commendable example of scientific sharing [28]. The repository comprises de-identified patient multimodal data, including demographics, vital signs, laboratory tests, medications, procedures, diagnoses, and outcomes. These data have been collected from more than 200 hospitals across the US and cover over 200,000 ICU admissions.
It is crucial to acknowledge that gathering an extensive amount of data can be relatively easy and cost-effective in the digital era. However, making sense of these data and extracting meaningful insights requires significant time, effort, and expertise. Furthermore, not all data points hold equal importance or relevance to a particular analysis or decision-making process. Consequently, having more data does not necessarily result in more useful or actionable insights. Quality assurance on collected data is mandatory for model training, as the basic rule of ML is “garbage in, garbage out” [29]. In this context, a good AI system must process and analyze data efficiently while effectively communicating with human operators when potential problems arise and intervention is necessary. The human–AI interface refers to the interaction between human beings and AI systems, where each role is complementary and mutually beneficial. In this way, the AI system should identify abnormal patterns or behaviors that could indicate a problem, such as system failures, security breaches, or deviation from expected outcomes. When the AI system detects an issue, it should generate alerts or notifications that draw human operators’ attention to the problem. A good human–AI interface should allow for two-way communication, enabling administrators to provide feedback to the AI system or modify its behavior when necessary. This feedback can be used to fine-tune the system’s algorithms and improve its accuracy in detecting potential problems in the future.
The importance of clearly defining goals is another commonly underestimated issue, which is related to poor collaboration among scientists from different fields. In the case of ML, close collaboration between scientists is essential to optimizing the most complex stages of the process, including preprocessing and exploratory data analysis [30].
In addition to considering the stage of structuring and analyzing datasets, it is important to consider other key stages of the process. One such stage is the imputation of missing data. Missing data can be categorized into three types, namely missing completely at random (MCAR), missing at random (MAR), and missing not at random (MNAR). Understanding the type of missing data is important because it affects the analysis and interpretation of the results. For example, if the missing data are MCAR, then the analysis can be performed without any special treatment. However, if the missing data are MAR or MNAR, then the analysis needs to account for the missingness in some way, such as multiple imputations or maximum likelihood estimation. Thus, when dealing with missing data, it is important to consider whether it is appropriate to exclude partially coherent data or if there is a possibility for their manipulation. Making informed decisions about missing data imputation can have a significant impact on the accuracy and reliability of the resulting analysis and can help to ensure that the conclusions drawn from the data are sound and trustworthy. Several approaches are available for the imputation of missing data [31]. Therefore, careful consideration should be given to all aspects of the data analysis process, including missing data imputation, to ensure that the results obtained are valid and meaningful.
The industrial development of an AI process and the transition from data-based prototypes to products require several steps. Technical expertise is an end in itself if the potential of discovery is not understood. In this context, clinicians have great employment opportunities. One of the first steps involves hiring staff to monitor and maintain data after implementation. The terms ML-Ops or Data Ops identify experts who do not have explicit knowledge of the AI system’s implementation but can guide infrastructure building and monitor the model’s availability and performance.
3. Ethical Issues
Ethics problems can represent a serious obstacle to AI translation. The use of AI in medicine raises ethical and regulatory concerns related to privacy, security, and bias [32]. Governments have a key role in this regulatory process. They must establish frameworks, set technical standards for AI systems, provide funding and resources, promote international cooperation, and monitor compliance with regulatory frameworks and technical standards. In addition to governments, other involved stakeholders include healthcare providers, industry, patients, ethics experts, and standards organizations such as the International Organization for Standardization (ISO).
Regulatory frameworks for ethical issues of AI in medicine must address several crucial elements. For example, AI algorithms used in healthcare require access to vast amounts of patient data to train and learn, which creates the potential for sensitive data to be exposed or compromised. Unauthorized access or disclosure of these data could result in serious breaches of privacy and confidentiality, leading to harm to patients and legal implications for healthcare providers. Furthermore, AI systems are vulnerable to cybersecurity threats, and malicious actors may attempt not only to exploit these vulnerabilities but also to gain access to sensitive patient data or manipulate the decision-making processes of healthcare providers. Therefore, it is crucial to establish robust security protocols and ensure that the AI technology used in healthcare meets the highest standards of data protection [33]. The DENDRITe repository project is a valuable example. To safeguard sensitive data, the platform has been crafted with a focus on security and privacy, featuring strong authentication and access control mechanisms [26].
The potential for bias is a significant concern when using AI in healthcare. The accuracy and reliability of AI algorithms are heavily dependent on the quality and representativeness of the data used to train them. If the data used to train an AI model are biased in any way, the model will inherit that bias and produce biased results. This can have severe consequences, leading to inaccurate diagnoses and treatment recommendations, especially for underrepresented or historically marginalized patient populations. It could also perpetuate discrimination and exacerbate health disparities [34].
Concerning the reliability of the AI-based developed systems, attaining complete certainty and accuracy of a predictive model is unattainable. This is due to various factors, such as the inherent complexity and unpredictability of certain phenomena, the limited availability and quality of data, and the limitations of the modeling algorithms themselves. As a result, even with the most advanced modeling techniques and vast amounts of data implemented, there will always be a degree of uncertainty and error in any predictive model [35]. Thus, it is essential to understand the strengths and limitations of the tools that clinicians are utilizing. On the other hand, this principle holds true for AI, as it does for all other medical applications of techniques. It is crucial to explain this concept clearly to users.
The ability to establish the predictive error is one of the possible solutions to increase credibility. A full understanding of how AI works is another gap that needs to be bridged to overcome ethical problems. In this context, a great challenge is a need to ensure that AI and ML algorithms are transparent and explainable so that clinicians can understand how they arrived at their recommendations. The term model explainability refers to a series of procedures aimed at making black boxes transparent. More specifically, it refers to the ability of AI and ML models to provide clear and interpretable explanations of their decision-making process. In addition to improving clinical decision making, model explainability can also help build trust in AI and ML models among clinicians and patients. Model explainability can be achieved through a variety of techniques. One effective method is to utilize algorithms that provide transparent and interpretable outputs, such as decision trees or rule-based systems. The processes of Shapley Additive exPlanations (SHAP) and Local Interpretable Model-Agnostic Explanations (LIME) are useful strategies. By a simplifying process, they calculate the contributions of the individual elements to the final result (such as the individual players in a team). Another approach is to use visualization techniques that allow clinicians to see how the model arrived at its decision, such as heat maps or saliency maps [36].
Finally, it should be advised that ethicists will be involved in the planning of AI projects from the beginning [37]. Demonstrating the functionality of the AI system is a crucial step in overcoming skepticism. This initial step is necessary to dispel any misunderstandings about the role of AI in healthcare. While AI can assist and direct decision making, it is not designed to replace clinicians. The real purpose of AI is to augment the capabilities of healthcare professionals and improve patient outcomes. Therefore, it is essential to showcase how AI can help clinicians to achieve better healthcare results.
4. Perspectives and Ongoing Research
Different strategies for addressing the AI chasm in neurocritical care have been suggested [1,3,24,26,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] (Table 2).

Table 2.
Suggested strategies for addressing AI chasm in neurocritical care.
A frequently underestimated aspect is the improvement of multiprofessional partnerships and knowledge dissemination. With regard to scientific publications, surprisingly, many articles that can be of great interest escape clinician’s reading. Computer scientists often tend to publish in conference proceedings and journals that may not be indexed in databases other than the clinical sector. IEEE Xplore, for example, is a digital library provided by the Institute of Electrical and Electronics Engineers (IEEE). It is one of the most comprehensive collections of technical literature in the fields of electrical engineering, computer science, and related technologies [38]. Nevertheless, this important opportunity is not known to all clinicians. Collaboration between clinicians and computer scientists can also serve to overcome this limit and this purpose. It can encourage the development of models conceived only to be disseminated in their theoretical essence, publishing the gathered experiences in journals that are disseminated among interested stakeholders.
Technology acceptance is a significant issue, and in the healthcare industry, the adoption of new technologies can be slow and challenging due to several factors. These include concerns about patient safety, lack of familiarity with the technology, and fear of change. According to an international survey, clinicians consider AI models as the last resort among all the various tools, including guidelines, training programs, second opinions, literature searches, etc. [39]. Therefore, there is a greater need to disseminate knowledge on this topic, rather than simply providing training and education. This can help address the underlying concerns and barriers that clinicians may have about the opportunities presented by the use of AI.
Standardization of data is mandatory to ensure that AI models can be applied across different institutions and datasets. This step can facilitate collaboration and data sharing, which is critical for advancing the field. Apart from the DENDRITe repository and the eICU Collaborative Research Database [28], other datasets include the freely accessible MIMIC-III (Medical Information Mart for Intensive Care III) [40] and the Critical Care Health Informatics Collaborative (CCHIC) databases. In particular, CCHIC was created using electronic health records (EHRs) and contains 70 data points related to admission and discharge, as well as a median of 1030 time-varying measures [41].
Real-world evidence (RWE) and causal inference strategies can be valuable instruments for evaluating the effectiveness and safety of AI applications in clinical practice. RWE includes data that are collected from EHRs, administrative claims databases, data from disease registries, and evidence achieved from other sources. It can provide insights into how AI is being used in real-world settings. Thus, in contrast to clinical trials, which are designed to test the efficacy of a specific intervention under controlled conditions, RWE can help evaluate the effectiveness and safety of AI in more diverse and representative patient populations. This can be especially important for evaluating the impact of AI in routine clinical care, where factors such as patient variability, co-morbidities, and other confounding variables can impact outcomes. Causal inference methods can also be used to analyze RWE and help establish cause-and-effect relationships between the use of AI and clinical outcomes. These methods aim to control for confounding variables and other biases that can arise in clinical studies and can help provide more robust evidence for the effectiveness and safety of AI [42,43].
Although the potential application of AI in neuro-ICU is a hot topic, clinical experiences are still limited, and quality studies are needed. Notably, physician’s lack of awareness and comfort with AI are frequently significant obstacles to utilizing AI-derived technologies in clinical practice [39,44]. Scientific societies must intervene to define detailed programs for acquiring basic knowledge of AI and ML. More importantly, the development of shared multiprofessional programs should be encouraged. In other words, clinical researchers must work closely with data scientists, computer scientists, and professionals who can act as interpreters between the two worlds due to their clinical background and computer science expertise. This approach can be particularly useful in complex areas to bridge disease-specific knowledge gaps [45].
Enhancements are required for the existing models to finally stimulate clinical research. The development of deep learning (DL) architectures has been driven by the availability of massive datasets. Thus, new models can combine multimodal parameters. For example, Vasseneix et al. [46] adopted an effective DL method for integrating medical imaging data to predict ICP. Moreover, the results proposed by Megjhani et al. [47] on delayed cerebral ischemia due to dysfunctional cerebral autoregulation are very encouraging. They reported a balanced accuracy of 67.3% and an F1 score of 0.68 (at 7 days). Mohd Noor et al. [48] proposed a binary EEG-based deep learning approach using long short-term memory (LSTM) to differentiate between improved and unimproved outcomes in patients with moderate traumatic brain injury, in a more recent study. The classification accuracy was 87.50 ± 0.05%. A recent scoping review focused on the performance of AI algorithms in clinical decision support systems for medical specialties found that in the field of neurocritical care, the accuracy range of algorithms was between 61.8% and 100% [49]. These results are highly encouraging, as they demonstrate that the integration of data and the development of complex neural architectures are crucial for the evolutionary process of AI in neurocritical care.
Nonetheless, there is a need to use more complex data, but above all, more elaborate preprocessing and exploratory analyses. These phases require a significant amount of time dedicated to the study, up to 80%. Summarization and visualization techniques can stimulate appropriate manipulation and mining of the dataset to arrive at the expected result. An intermediate step to verify the goodness of the product could be the simulation in different scenarios. For instance, an example scenario would be the model’s behavior when applied to a patient with specific characteristics. In this regard, patient clusterization into phenotypes is an aspect that needs to be addressed carefully. Before considering how to clinically apply the algorithm and the model, researchers could plan AI strategies to identify the phenotypes on which to act [50,51]. However, ensuring and assessing generalizability remains a significant challenge [6]. This latter step is vital for advancing scientific knowledge and making informed decisions in various fields, including medicine, public health, and education. Therefore, researchers must strive to address these challenges and employ rigorous methods to enhance the generalizability of their findings. Additional research, including replication studies and meta-analyses, is usually required to determine the robustness and validity of the findings [52].
The use of AI in neuro-ICU offers great potential to improve patient outcomes and streamline clinical decision making. However, as with any new technology, ethical and regulatory considerations must be considered to ensure that these tools are safe, effective, and have a positive impact on patient care. This requires ongoing monitoring and evaluation of AI tools to assess their performance and address any ethical concerns that may arise, such as issues related to patient privacy and data security [53]. Furthermore, regulatory bodies play a crucial role in the development and implementation of AI tools in neuro-ICU, as they can provide guidance on issues such as device approval and reimbursement.
Addressing disease-specific knowledge gaps is an essential step that requires extensive collaboration involving the structuring and analysis of datasets, as well as tailored research approaches. Identifying specific use cases can help researchers and clinicians focus their efforts and resources on developing and implementing AI solutions that can make a real difference in patient outcomes. For instance, oncology patients are highly susceptible to a range of neurologic adverse events, the severity of which can vary significantly [54]. Unfortunately, in this setting, research is lacking. Moreover, since hydrocephalus is a frequently observed concern in the neonatal ICU, different ML and DL models have been investigated to predict outcomes [55] or the need for shunt placement [56].
Finally, investing in AI technology in healthcare is a critical step in crossing the AI chasm and unlocking its full potential to revolutionize patient care [57]. Consequently, strategic investments in research and development, education, and infrastructure are needed. They can also be useful for addressing regulatory and ethical concerns as well as for education and training. One area of investment is in the development of AI algorithms that are specifically designed for neuro-ICU applications. These algorithms must be trained on large, diverse, and representative datasets to ensure their accuracy and reliability. Investing in data collection, curation, and labeling, as well as creating a regulatory framework that incentivizes the sharing of data across healthcare institutions, can facilitate the creation of high-quality datasets for AI training. More importantly, investing in infrastructure is essential for the successful integration of AI technology in healthcare. This includes upgrading healthcare information systems to ensure compatibility with AI systems, improving network connectivity and bandwidth, and investing in cloud computing technology. These infrastructure investments can enable the efficient sharing and processing of large amounts of patient data, making AI technology more effective and accessible to healthcare providers [58]. For this purpose, dedicated AI models could also be integrated into telehealth platforms and for structuring telemedicine-supported neuro-ICU [59,60]. This process could also be useful for research aims [61,62,63].
Ongoing Research
The use of AI in neuro-ICU has become a topic of significant interest, with several studies currently underway. These ongoing investigations offer promise for the future of AI in neuro-ICU and its potential to revolutionize patient care.
In a study conducted by the Trousseau Hospital in Paris, researchers are gathering digital EEG signals to create a library for designing an effective AI system in implementing hypothermia protocols (ClinicalTrials.gov Identifier NCT05114070). This study exemplifies how AI can be integrated into a given protocol to improve patient outcomes. Another investigation aims to design prognostic models for long-term outcomes after aneurysmal subarachnoid hemorrhage by combining brain imaging, clinical data, biomarkers, and metabolomics data (NCT04696523). Additionally, there are ongoing studies on the development and validation of automated tools for seizure detection (NCT04991779) and coma prognosis (NCT03826407). A fascinating project at the University of Vienna is evaluating the use of multimodal neuromonitoring to prevent delayed cerebral ischemia after acute brain injuries (NCT04737369).
5. Conclusions
The vast potential of data collection makes neuro-ICU an ideal setting for conducting AI-based research and implementing AI-driven applications. Consequently, AI and ML have the capacity to revolutionize neurocritical care by improving patient monitoring, predicting outcomes, and analyzing medical images. However, there are still many challenges that need to be addressed before these technologies can be widely adopted in clinical practice. To overcome the AI chasm in the field of neurocritical care, it is necessary to establish partnerships among researchers, clinicians, and policymakers. This should involve targeting specific use cases and creating ethical and regulatory frameworks that guarantee the secure and efficient implementation of AI technology.
Author Contributions
Conceptualization, M.C. and E.G.B.; methodology, V.B. and A.V.; software, J.M.; validation, M.C.; data curation, J.M.; writing—original draft preparation, M.C., F.D.M. and H.B.; writing—review and editing, E.G.B.; visualization, V.B.; supervision, E.G.B. All authors have read and agreed to the published version of the manuscript.
Funding
This article received no external funding.
Data Availability Statement
The data that support the findings of this narrative review are available from the corresponding author, J.M., upon reasonable request.
Acknowledgments
The authors are grateful to Valeria Vicario from the Istituto Nazionale Tumori IRCCS Fondazione Pascale for providing an excellent bibliographic service and assistance.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chaudhry, F.; Hunt, R.J.; Hariharan, P.; Anand, S.K.; Sanjay, S.; Kjoller, E.E.; Bartlett, C.M.; Johnson, K.W.; Levy, P.D.; Noushmehr, H.; et al. Machine Learning Applications in the Neuro ICU: A Solution to Big Data Mayhem? Front. Neurol. 2020, 11, 554633. [Google Scholar] [CrossRef] [PubMed]
- Use of AI in Healthcare & Medicine is Booming—Here’s How the Medical Field Is Benefiting from AI in 2023 and Beyond. Available online: https://www.insiderintelligence.com/insights/artificial-intelligence-healthcare/ (accessed on 8 April 2023).
- Al-Mufti, F.; Kim, M.; Dodson, V.; Sursal, T.; Bowers, C.; Cole, C.; Scurlock, C.; Becker, C.; Gandhi, C.; Mayer, S.A. Machine Learning and Artificial Intelligence in Neurocritical Care: A Specialty-Wide Disruptive Transformation or a Strategy for Success. Curr. Neurol. Neurosci. Rep. 2019, 19, 89. [Google Scholar] [CrossRef] [PubMed]
- Bellini, V.; Valente, M.; Pelosi, P.; Del Rio, P.; Bignami, E. Big Data and Artificial Intelligence in Intensive Care Unit: From “Bla, Bla, Bla” to the Incredible Five’s. Neurocrit. Care 2022, 37 (Suppl. S2), 170–172. [Google Scholar] [CrossRef] [PubMed]
- United States Government Accountability Office (GAO). Technology Assessment. Artificial Intelligence in Health Care. Benefits and Challenges of Machine Learning. Technologies for Medical Diagnostics. Available online: https://www.gao.gov/assets/gao-22-104629.pdf (accessed on 8 April 2023).
- Gravesteijn, B.Y.; Steyerberg, E.W.; Lingsma, H.F. Modern Learning from Big Data in Critical Care: Primum Non Nocere. Neurocrit. Care 2022, 37 (Suppl. S2), 174–184. [Google Scholar] [CrossRef]
- Savin, I.; Ershova, K.; Kurdyumova, N.; Ershova, O.; Khomenko, O.; Danilov, G.; Shifrin, M.; Zelman, V. Healthcare-associated ventriculitis and meningitis in a neuro-ICU: Incidence and risk factors selected by machine learning approach. J. Crit. Care 2018, 45, 95–104. [Google Scholar] [CrossRef]
- Ye, G.; Balasubramanian, V.; Li, J.K.; Kaya, M. Machine Learning-Based Continuous Intracranial Pressure Prediction for Traumatic Injury Patients. IEEE J. Transl. Eng. Health Med. 2022, 10, 4901008. [Google Scholar] [CrossRef]
- Schweingruber, N.; Mader, M.M.D.; Wiehe, A.; Röder, F.; Göttsche, J.; Kluge, S.; Westphal, M.; Czorlich, P.; Gerloff, C. A recurrent machine learning model predicts intracranial hypertension in neurointensive care patients. Brain 2022, 145, 2910–2919. [Google Scholar] [CrossRef]
- Liu, W.; Ma, W.; Bai, N.; Li, C.; Liu, K.; Yang, J.; Zhang, S.; Zhu, K.; Zhou, Q.; Liu, H.; et al. Identification of key predictors of hospital mortality in critically ill patients with embolic stroke using machine learning. Biosci. Rep. 2022, 42, BSR20220995. [Google Scholar] [CrossRef]
- Claassen, J.; Doyle, K.; Matory, A.; Couch, C.; Burger, K.M.; Velazquez, A.; Okonkwo, J.U.; King, J.R.; Park, S.; Agarwal, S.; et al. Detection of Brain Activation in Unresponsive Patients with Acute Brain Injury. N. Engl. J. Med. 2019, 380, 2497–2505. [Google Scholar] [CrossRef]
- Arbabshirani, M.R.; Fornwalt, B.K.; Mongelluzzo, G.J.; Suever, J.D.; Geise, B.D.; Patel, A.A.; Moore, G.J. Advanced machine learning in action: Identification of intracranial hemorrhage on computed tomography scans of the head with clinical workflow integration. NPJ Digit Med. 2018, 1, 9. [Google Scholar] [CrossRef]
- Koren, J.P.; Herta, J.; Fürbass, F.; Pirker, S.; Reiner-Deitemyer, V.; Riederer, F.; Flechsenhar, J.; Hartmann, M.; Kluge, T.; Baumgartner, C. Automated Long-Term EEG Review: Fast and Precise Analysis in Critical Care Patients. Front. Neurol. 2018, 9, 454. [Google Scholar] [CrossRef]
- Stapleton, C.J.; Acharjee, A.; Irvine, H.J.; Wolcott, Z.C.; Patel, A.B.; Kimberly, W.T. High-throughput metabolite profiling: Identification of plasma taurine as a potential biomarker of functional outcome after aneurysmal subarachnoid hemorrhage. J. Neurosurg. 2019, 133, 1842–1849. [Google Scholar] [CrossRef]
- Tanioka, S.; Ishida, F.; Nakano, F.; Kawakita, F.; Kanamaru, H.; Nakatsuka, Y.; Nishikawa, H.; Suzuki, H.; pSEED Group. Machine Learning Analysis of Matricellular Proteins and Clinical Variables for Early Prediction of Delayed Cerebral Ischemia After Aneurysmal Subarachnoid Hemorrhage. Mol. Neurobiol. 2019, 56, 7128–7135. [Google Scholar] [CrossRef]
- Chang, C.C.; Yeh, J.H.; Chiu, H.C.; Chen, Y.M.; Jhou, M.J.; Liu, T.C.; Lu, C.J. Utilization of Decision Tree Algorithms for Supporting the Prediction of Intensive Care Unit Admission of Myasthenia Gravis: A Machine Learning-Based Approach. J. Pers. Med. 2022, 12, 32. [Google Scholar] [CrossRef]
- Kamousi, B.; Karunakaran, S.; Gururangan, K.; Markert, M.; Decker, B.; Khankhanian, P.; Mainardi, L.; Quinn, J.; Woo, R.; Parvizi, J. Monitoring the Burden of Seizures and Highly Epi-leptiform Patterns in Critical Care with a Novel Machine Learning Method. Neurocrit. Care. 2021, 34, 908–917. [Google Scholar] [CrossRef]
- Ryvlin, P.; Rheims, S.; Hirsch, L.J.; Sokolov, A.; Jehi, L. Neuromodula-tion in epilepsy: State-of-the-art approved therapies. Lancet Neurol. 2021, 20, 1038–1047. [Google Scholar] [CrossRef]
- King, M.R. The Future of AI in Medicine: A Perspective from a Chatbot. Ann. Bio-Med Eng. 2023, 51, 291–295. [Google Scholar] [CrossRef]
- Cascella, M.; Montomoli, J.; Bellini, V.; Bignami, E. Evaluating the Feasibility of ChatGPT in Healthcare: An Analysis of Multiple Clinical and Research Scenarios. J. Med. Syst. 2023, 47, 33. [Google Scholar] [CrossRef]
- Fratino, S.; Garré, A.; Garufi, A.; Hafidi, S.; Migliorino, E.; Stropeni, S.; Bogossian, E.G.; Ndieugnou Djan-gang, N.; Albano, G.; Creteur, J.; et al. Evaluation of nociception in unconscious critically ill patients using a multimodal approach. Anaesth. Crit. Care Pain Med. 2023, 42, 101175. [Google Scholar] [CrossRef]
- Cascella, M.; Montomoli, J.; Bellini, V.; Bignami, E.G. Integrating data science and neural architecture techniques for automatic pain assessment in critically ill patients. Anaesth. Crit. Care Pain Med. 2023, 42, 101220. [Google Scholar] [CrossRef]
- Aristidou, A.; Jena, R.; Topol, E.J. Bridging the chasm between AI and clinical implementation. Lancet 2022, 399, 620. [Google Scholar] [CrossRef] [PubMed]
- Westfall, J.M.; Mold, J.; Fagnan, L. Practice-based research—“Blue Highways” on the NIH roadmap. JAMA 2007, 297, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Car, J.; Sheikh, A.; Wicks, P.; Williams, M.S. Beyond the hype of big data and artificial intelligence: Building foundations for knowledge and wisdom. BMC Med. 2019, 17, 143. [Google Scholar] [CrossRef] [PubMed]
- Duke Neurocritical Care Patient Data Repository. Available online: https://datacatalog.mclibrary.duke.edu/dataset/duke-neurocritical-care-patient-data-repository (accessed on 26 February 2023).
- Azad, T.D.; Shah, P.P.; Kim, H.B.; Stevens, R.D. Endotypes and the Path to Precision in Moderate and Severe Traumatic Brain Injury. Neurocrit. Care. 2022, 37 (Suppl. S2), 259–266. [Google Scholar] [CrossRef]
- Pollard, T.J.; Johnson, A.E.W.; Raffa, J.D.; Celi, L.A.; Mark, R.G.; Badawi, O. The eICU collaborative research database, a freely available multi-center database for critical care research. Sci. Data 2018, 5, 180178. [Google Scholar] [CrossRef]
- Bignami, E.G.; Vittori, A.; Lanza, R.; Compagnone, C.; Cascella, M.; Bellini, V. The Clinical Researcher Journey in the Artificial Intelligence Era: The PAC-MAN’s Challenge. Healthcare 2023, 11, 975. [Google Scholar] [CrossRef]
- Bellini, V.; Cascella, M.; Cutugno, F.; Russo, M.; Lanza, R.; Compagnone, C.; Bignami, E.G. Understanding basic principles of Artificial Intelligence: A practical guide for intensivists. Acta Biomed. 2022, 93, e2022297. [Google Scholar] [CrossRef]
- Yang, S.; Du, P.; Feng, X.; He, D.; Chen, Y.; Zhong, L.L.D.; Yan, X.; Luo, J. Propensity score analysis with missing data using a multi-task neural network. BMC Med. Res. Methodol. 2023, 23, 41. [Google Scholar] [CrossRef]
- Cobianchi, L.; Verde, J.M.; Loftus, T.J.; Piccolo, D.; Dal Mas, F.; Mascagni, P.; Garcia Vazquez, A.; Ansaloni, L.; Marseglia, G.R.; Massaro, M.; et al. Artificial Intelligence and Surgery: Ethical Dilemmas and Open Issues. J. Am. Coll Surg. 2022, 235, 268–275. [Google Scholar] [CrossRef]
- Raimundo, R.; Rosário, A. The Impact of Artificial Intelligence on Data System Security: A Literature Review. Sensors 2021, 21, 7029. [Google Scholar] [CrossRef]
- Panch, T.; Mattie, H.; Atun, R. Artificial intelligence and algorithmic bias: Implications for health systems. J. Glob. Health 2019, 9, 010318. [Google Scholar] [CrossRef]
- Koohy, H. The rise and fall of machine learning methods in biomedical research. F1000Res 2017, 6, 2012. [Google Scholar] [CrossRef]
- Amann, J.; Blasimme, A.; Vayena, E.; Frey, D.; Madai, V.I.; Precise4Q Consortium. Explainability for artificial intelligence in healthcare: A multidisciplinary perspective. BMC Med. Inform. Decis. Mak. 2020, 20, 310. [Google Scholar] [CrossRef]
- Keskinbora, K.H. Medical ethics considerations on artificial intelligence. J. Clin. Neurosci. 2019, 64, 277–282. [Google Scholar] [CrossRef]
- IEEE Xplore. Available online: https://ieeexplore.ieee.org/Xplore/home.jsp (accessed on 25 February 2023).
- Cobianchi, L.; Piccolo, D.; Dal Mas, F.; Agnoletti, V.; Ansaloni, L.; Balch, J.; Biffl, W.; Butturini, G.; Catena, F.; Coccolini, F.; et al. Surgeons’ perspectives on artificial intelligence to support clinical decision-making in trauma and emergency contexts: Results from an international survey. World J. Emerg. Surg. 2023, 18, 1. [Google Scholar] [CrossRef]
- Johnson, A.E.; Pollard, T.J.; Shen, L.; Lehman, L.W.; Feng, M.; Ghassemi, M.; Moody, B.; Szolovits, P.; Celi, L.A.; Mark, R.G. MIMIC-III, a freely accessible critical care database. Sci. Data 2016, 3, 160035. [Google Scholar] [CrossRef]
- Harris, S.; Shi, S.; Brealey, D.; MacCallum, N.S.; Denaxas, S.; Perez-Suarez, D.; Ercole, A.; Watkinson, P.; Jones, A.; Ashworth, S.; et al. Critical Care Health Informatics Collaborative (CCHIC): Data, tools and methods for reproducible research: A multi-centre UK intensive care database. Int. J. Med. Inform. 2018, 112, 82–89. [Google Scholar] [CrossRef]
- Marwaha, J.S.; Kvedar, J.C. Crossing the chasm from model performance to clinical impact: The need to improve implementation and evaluation of AI. NPJ Digit. Med. 2022, 5, 25. [Google Scholar] [CrossRef]
- Levy, J.J.; O’Malley, A.J. Don’t dismiss logistic regression: The case for sensible extraction of interactions in the era of machine learning. BMC Med. Res. Methodol. 2020, 20, 171. [Google Scholar] [CrossRef]
- Russak, A.J.; Chaudhry, F.; De Freitas, J.K.; Baron, G.; Chaudhry, F.F.; Bienstock, S.; Paranjpe, I.; Vaid, A.; Ali, M.; Zhao, S.; et al. Machine Learning in Cardiology-Ensuring Clinical Impact Lives Up to the Hype. J. Cardiovasc. Pharmacol. Ther. 2020, 25, 379–390. [Google Scholar] [CrossRef]
- Simpkins, A.N.; Busl, K.M.; Amorim, E.; Barnett-Tapia, C.; Cervenka, M.C.; Dhakar, M.B.; Etherton, M.R.; Fung, C.; Griggs, R.; Holloway, R.G.; et al. Neurotherapeutics Symposium 2019. Proceedings from the Neurotherapeutics Symposium on Neurological Emergencies: Shaping the Future of Neurocritical Care. Neurocrit. Care 2020, 33, 636–645. [Google Scholar] [CrossRef] [PubMed]
- Vasseneix, C.; Najjar, R.P.; Xu, X.; Tang, Z.; Loo, J.L.; Singhal, S.; Tow, S.; Milea, L.; Ting, D.S.W.; Liu, Y.; et al. Accuracy of a deep learning system for classification of papilledema severity on ocular fundus photographs. Neurology 2021, 97, e369–e377. [Google Scholar] [CrossRef] [PubMed]
- Megjhani, M.; Weiss, M.; Kwon, S.B.; Ford, J.; Nametz, D.; Kastenholz, N.; Fogel, H.; Velazquez, A.; Roh, D.; Agarwal, S.; et al. Vector Angle Analysis of Multimodal Neuromonitoring Data for Continuous Prediction of Delayed Cerebral Ischemia. Neurocrit. Care 2022, 37 (Suppl. S2), 230–236. [Google Scholar] [CrossRef] [PubMed]
- Mohd Noor, N.S.E.; Ibrahim, H.; Lai, C.Q.; Abdullah, J.M. A Long Short-Term Memory Network Using Resting-State Electroencephalogram to Predict Outcomes Following Moderate Traumatic Brain Injury. Computers 2023, 12, 45. [Google Scholar] [CrossRef]
- Narindrarangkura, P.; Kim, M.S.; Boren, S.A. A Scoping Review of Artificial Intelligence Algorithms in Clinical Decision Support Systems for Internal Medicine Subspecialties. ACI Open. 2021, 5, e67–e79. [Google Scholar] [CrossRef]
- Jha, R.M.; Elmer, J.; Zusman, B.E.; Desai, S.; Puccio, A.M.; Okonkwo, D.O.; Park, S.Y.; Shutter, L.A.; Wallisch, J.S.; Conley, Y.P.; et al. Intracranial pressure trajectories: A novel approach to informing severe traumatic brain injury Phenotypes. Crit. Care Med. 2018, 46, 1792–1802. [Google Scholar] [CrossRef]
- Dhar, R.; Meyfroidt, G. Navigating the Ocean of Big Data in Neurocritical Care. Neurocrit. Care 2022, 37 (Suppl. S2), 157–159. [Google Scholar] [CrossRef]
- Carminati, L. Generalizability in Qualitative Research: A Tale of Two Traditions. Qual. Health Res. 2018, 28, 2094–2101. [Google Scholar] [CrossRef]
- Islam, M.S.; Ameedeen, M.A.B.; Rahman, M.A.; Ajra, H.; Ismail, Z.B. Healthcare-Chain: Blockchain-Enabled Decentralized Trustworthy System in Healthcare Management Industry 4.0 with Cyber Safeguard. Computers 2023, 12, 46. [Google Scholar] [CrossRef]
- Lin, A.L.; Avila, E.K. Neurologic emergencies in the patients with cancer. J. Intensive Care Med. 2017, 32, 99–115. [Google Scholar] [CrossRef]
- Tabrizi, P.R.; Obeid, R.; Mansoor, A.; Ensel, S.; Cerrolaza, J.J.; Penn, A.; Linguraru, M.G. Cranial ultrasound-based prediction of post hemorrhagic hydrocephalus outcome in premature neonates with intraventricular hemorrhage. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2017, 2017, 169–172. [Google Scholar] [CrossRef]
- Pisapia, J.M.; Akbari, H.; Rozycki, M.; Goldstein, H.; Bakas, S.; Rathore, S.; Moldenhauer, J.S.; Storm, P.B.; Zarnow, D.M.; Anderson, R.C.E.; et al. Use of Fetal Magnetic Resonance Image Analysis and Machine Learning to Predict the Need for Postnatal Cerebrospinal Fluid Diversion in Fetal Ventriculomegaly. JAMA Pediatr. 2018, 172, 128–135. [Google Scholar] [CrossRef]
- Sheikh, A.; Anderson, M.; Albala, S.; Casadei, B.; Franklin, B.D.; Richards, M.; Taylor, D.; Tibble, H.; Mossialos, E. Health information technology and digital innovation for national learning health and care systems. Lancet Digit. Health 2021, 3, e383–e396. [Google Scholar] [CrossRef]
- Reddy, S.; Allan, S.; Coghlan, S.; Cooper, P. A governance model for the application of AI in health care. J. Am. Med. Inform. Assoc. 2020, 27, 491–497. [Google Scholar] [CrossRef]
- Becker, C.D.; Fusaro, M.V.; Scurlock, C. Telemedicine in the ICU: Clinical outcomes, economic aspects, and trainee education. Curr. Opin. Anaesthesiol. 2019, 32, 129–135. [Google Scholar] [CrossRef]
- Cascella, M.; Coluccia, S.; Monaco, F.; Schiavo, D.; Nocerino, D.; Grizzuti, M.; Romano, M.C.; Cuomo, A. Different Machine Learning Approaches for Implementing Telehealth-Based Cancer Pain Management Strategies. J. Clin. Med. 2022, 11, 5484. [Google Scholar] [CrossRef]
- Klein, K.E.; Rasmussen, P.A.; Winners, S.L.; Frontera, J.A. Teleneurocritical care and telestroke. Crit. Care Clin. 2015, 31, 197–224. [Google Scholar] [CrossRef]
- Freeman, W.D.; Rogers, A.; Rabinstein, A. TeleNeuroICU: Expanding the Reach of Subspecialty Neurocritical Care. Semin. Neurol. 2022, 42, 18–30. [Google Scholar] [CrossRef]
- Cascella, M.; Schiavo, D.; Grizzuti, M.; Romano, M.C.; Coluccia, S.; Bimonte, S.; Cuomo, A. Implementation of a Hybrid Care Model for Telemedicine-based Cancer Pain Management at the Cancer Center of Naples, Italy: A Cohort Study. Vivo 2023, 37, 385–392. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).