Simple Summary
There are no reliable pre-treatment markers that predict tumor response to total neoadjuvant therapy in patients with locally advanced rectal cancer. The aim of this study is to evaluate the usefulness of pre-treatment SEPTIN9 gene methylation ratio as a predictor of tumor response to total neoadjuvant therapy and its correlation with tumor size and tumor stage in patients with locally advanced rectal cancer. Pre-treatment SEPTIN9 gene methylation ratio (p = 0.033) and tumor size (p = 0.026), but not tumor stage, significantly correlated with tumor response to total neoadjuvant therapy. Pre-treatment SEPTIN9 gene methylation ratio also correlated with N stage (p = 0.040) and tumor size (p = 0.001), but not with T stage (p = 0.846). Thus, pre-treatment SEPTIN9 gene methylation ratio correlates with tumor size and N stage and can predict tumor response to total neoadjuvant therapy in patients with locally advanced rectal cancer.
Abstract
Background and objective: Multiple markers have been proposed, but there are no reliable pre-treatment markers that predict tumor response to total neoadjuvant therapy in patients with locally advanced rectal cancer. The objective of this study is to evaluate the usefulness of pre-treatment SEPTIN9 gene methylation ratio as a predictor of tumor response to total neoadjuvant therapy and its correlation with tumor size and tumor stage in patients with locally advanced rectal cancer. Methods: Patients with locally advanced rectal cancer (T3/4 and/or N+ histologically confirmed rectal cancer) undergoing total neoadjuvant therapy were included. Tumor size and tumor stage were determined by magnetic resonance. SEPTIN9 gene methylation in plasmatic cfDNA was analyzed by droplet digital PCR at the time of diagnosis. After completing total neoadjuvant therapy, tumor response was assessed by magnetic resonance and proctoscopy. The correlation between pre-treatment SEPTIN9 gene methylation ratio, tumor size, tumor stage and tumor response was analyzed. Results: 39 patients with locally advanced rectal cancer were included. Pre-treatment SEPTIN9 gene methylation ratio (p = 0.033) and tumor size (p = 0.026), but not tumor stage, significantly correlated with tumor response to total neoadjuvant therapy. Pre-treatment SEPTIN9 gene methylation ratio also correlated with N stage (p = 0.040) and tumor size (p = 0.001), but not with T stage (p = 0.846). Conclusions: Pre-treatment SEPTIN9 gene methylation ratio correlates with tumor size and N stage and can predict tumor response to total neoadjuvant therapy in patients with locally advanced rectal cancer.
1. Introduction
Colorectal cancer (CRC) is the third most common cancer in the world, while rectal cancer (RC) accounts for approximately 732,000 new cases per year, according to data from the American Society of Clinical Oncology [1].
Locally advanced rectal cancer (LARC) is defined as T3/4 and/or N+ rectal cancer. The standard treatment of LARC, which includes neoadjuvant chemoradiation followed by radical surgery with total mesorectal excision and adjuvant chemotherapy, achieves good survival rates and excellent local control of the disease, with low rates of local recurrence but with remaining high rates of distant metastasis [2]. Furthermore, surgical resection involves important morbidity that significantly affects quality of life [3].
Consequently, during the last decades, there has been a growing interest in organ preservation approaches to avoid the morbidity derived from surgery in those patients with a complete clinical response (cCR) to neoadjuvant treatment. Total neoadjuvant therapy (TNT) has demonstrated achievements of better systemic control of the disease and increased rates of cCR, which has led to avoiding surgery in those patients with a cCR in a “watch and wait” (WW) follow-up protocol [2].
Tumor response to neoadjuvant chemoradiation is an important prognostic factor in patients with LARC. Multiple markers have been proposed, but no reliable pre-treatment markers that predict tumor response to TNT in patients with LARC have been developed enough to reach regular clinical use, since all of them have important limitations [4].
SEPTIN9 gene methylation (SEPT9m) is an epigenetic phenomenon that occurs during CRC tumorigenesis and a well-demonstrated biomarker in plasma for screening and early diagnosis of CRC [5]. Moreover, it has also demonstrated its utility as a biomarker of complete surgical resection and tumor recurrence during the follow-up after surgery in patients with CRC [6,7].
To our knowledge, its value as a predictor of tumor response to TNT in patients with LARC has not been explored. Thus, the objective of this study is to evaluate the usefulness of the pre-treatment SEPTIN9 gene methylation ratio (SEPT9mr) as a predictor of tumor response to TNT and its correlation with tumor size and tumor stage in patients with LARC, since we hypothesize that pre-treatment SEPT9mr should be correlated and could predict tumor response to TNT.
2. Materials and Methods
2.1. Patients’ Selection
Patients with histologically confirmed LARC (T3/4 and/or N+ RC) included in a TNT protocol with the goal of organ preservation in Fundación Jiménez Díaz University Hospital were enrolled in this study after discussion in a multidisciplinary committee.
2.2. LARC Diagnosis
Diagnosis of LARC was made by digital rectal examination (DRE), magnetic resonance imaging (MRI), and proctoscopy with a biopsy positive for adenocarcinoma. Tumor size (largest tumor diameter) and tumor stage at diagnosis were determined by MRI. A thoracic-abdominopelvic CT (Siemens, Munich, Germany) scan confirmed the absence of distant metastases at the time of diagnosis in each case.
2.3. Treatment of LARC
After the diagnosis of LARC, patients received one of the following schemes of TNT with the goal of organ preservation:
Chemoradiation with short-or long-course radiotherapy and concomitant sensitizing chemotherapy with capecitabine followed by 6–8 cycles of consolidation systemic chemotherapy with FOLFOX (oxaliplatin, 5-fluorouracil, and folinic acid).
Induction chemotherapy with FOLFOX was followed by chemoradiation with short- or long-course radiotherapy and concomitant sensitizing chemotherapy with capecitabine.
2.4. Evaluation of Tumor Response to TNT
After completing TNT, evaluation of tumor response was performed by DRE, proctoscopy, and MRI. Tumor response was graded following MRI Tumor Regression Grade (mrTRG) as follows [8]:
mrTRG 1: Complete response. No evidence of tumor signal intensity or fibrosis only.
mrTRG 2: Good response. Dense fibrosis or minimal residual tumor.
mrTRG 3: Moderate response. Mixed fibrosis/mucin and intermediate signal representing residual tumor, but fibrosis still predominates.
mrTRG 4: Slight response. Small areas of fibrosis or mucin but mostly tumor.
mrTRG 5: No response. Same appearance as original tumor or tumor growth.
Patients with a grade 1–2 mrTRG and a negative proctoscopy were supposed to have a cCR, were included in a WW protocol, and closely followed by DRE, CT scan, MRI, and proctoscopy. Patients with a grade 3–5 mrTRG and/or a positive proctoscopy, who did not reach a cCR, were indicated for surgery (either abdominoperineal amputation, anterior low resection of the rectum or transanal local resection).
2.5. SEPT9m Analysis
For each patient, pre-treatment SEPT9m in plasmatic cell-free DNA (cfDNA) was analyzed by droplet digital polymerase chain reaction (ddPCR).
At the time of LARC diagnosis, before starting TNT, 20 mL of whole peripheral blood was collected from each patient in 2 EDTA tubes. Plasma was isolated within a maximum of 2 h through two centrifugation steps: first at 1800 G, 4 °C, for 10 min to eliminate cell debris, followed by a second centrifugation at 3000 G, 4 °C, for 10 min. Isolated plasma was then stored frozen at −80 °C for further analysis.
cfDNA isolation from plasma was performed using QIAamp Circulating Nucleic Acid Kit (Qiagen, Hilden, Germany). Isolated cfDNA was afterward treated with an EZ DNA Methylation Kit by spin column (Zymo Research, Irvine, CA, USA).
SEPT9m in cfDNA was analyzed by the ddPCR assay QX200 Droplet Digital PCR System (Bio-Rad Laboratories, Hercules, CA, USA). Samples were prepared by mixing 10 μL of ddPCR Supermix for probes No dUTP (Bio-Rad Laboratories, Hercules, CA, USA), 1 μL of FAM and HEX fluorescent probes (specific for mutant/methylated and wild-type gene, respectively), and 1 to 8.8 μL of template DNA in a final reaction volume of 20 μL. Three replicates were analyzed per sample. Distillated water instead of DNA was used for no template control and served as a control for detecting environmental contamination. DNA from HCT-116 cell line, which has hypermethylation of the SEPTIN9 gene, was used as positive control.
Primers for SEPTIN9 gene (5′-AGAGAATTTTGTTTGGTTGTTGTTTAAATATATAG-3′ and 5′-AAAAAAAAAATTCCTCCCCTTCC-3′) (Bio-Rad Laboratories, Hercules, CA, USA) and fluorescent probes for the methylated and unmethylated sequences (methylated-FAM 5′-TGTAGAAGGATTTTGCGTTCGG-3′ unmethylated-HEX 5′-TTGTAGAAG/ZEN/GATTTTGTGTGTTTGG-3′) were used once the DNA was converted with bisulfite. A total of 40 cycles of ddPCR were employed at 95 °C for 10 min including 94 °C for 30 s and 52 °C for 1 min for amplification, a final cycle at 98 °C for 10 min, and a holding temperature of 4 °C.
Droplets were generated by a QX200 droplet generator (Bio-Rad Laboratories, Hercules, CA, USA), and endpoint PCR was performed on a T100 Thermal Cycler (Bio-Rad Laboratories, Hercules, CA, USA). After thermal cycling, the fluorescent signals of droplets were detected in the FAM and HEX channels of a QX200 droplet reader (Bio-Rad Laboratories, Hercules, CA, USA). Data were analyzed by Quanta Soft v.1.7 Software (Bio-Rad Laboratories, Hercules, CA, USA). Results were reported as the number of copies of genetic alteration per μL of reaction (Figure 1).
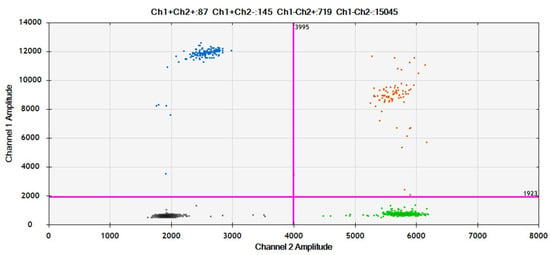
Figure 1.
Example of SEPT9m analysis by ddPCR: Blue: drops with methylated SEPTIN9 gene. Orange: drops with methylated + unmethylated SEPTIN9 gene. Green: drops with unmethylated SEPTIN9 gene. Black: no template control.
We previously observed that analyzing the absolute value of analytes from global plasma samples is highly variable to reach an objectively assessable result. Therefore, we considered the individual ratio of methylated to unmethylated SEPTIN9 gene, which we called “SEPTIN9 gene methylation ratio” (SEPT9mr), to be more consistent and objective. SEPT9mr was therefore calculated as follows:
3. Results
A total of 39 patients (61.5% male, 38.5% female) were included from December 2020 to January 2024. The median age was 63.3 (38–80) years.
The median tumor size was 4.3 cm, ranging from 2 to 8.5 cm. Regarding tumor stage, 2 patients (5.1%) had a T2 stage, 31 patients (79.5%) had a T3 stage, and 6 patients (15.4%) had a T4 stage. A total of 4 patients (10.3%) had an N0 stage, 20 patients (51.3%) had an N1 stage, and 15 patients (28.5%) had an N2 stage. The median SEPT9mr at the time of diagnosis was 0.0317. (Table 1).

Table 1.
Demographic and tumor characteristics.
A total of 23 (59%) patients achieved a cCR and enrolled in a WW protocol. A total of four (10.3%) patients were not supposed to achieve a cCR and underwent surgery, but the histopathological analysis of the surgical specimen revealed the absence of tumor, so they were considered as complete tumor response (cTR) because a complete pathological response (cPR) was demonstrated. Thus, 27 (69.2%) patients in total obtained a cTR. The remaining 12 (30.8%) patients did not achieve a cCR and were indicated either for radical or local resection, which confirmed the absence of cTR (Table 2).

Table 2.
Tumor response to TNT.
Both groups (patients with and without cTR) were comparable in terms of sex and age. A statistically significant lower SEPT9mr was observed in the group of patients who achieved a cTR to TNT, compared with those who did not achieve a cTR (0.023 vs. 0.032, p = 0.033), so higher values of SEPT9mr seem to predict a lower probability of cTR. Significant differences in tumor size (4.0 vs. 4.9 cm, p = 0.026), but not in tumor stage, between patients with and without cTR to TNT were also observed, so greater tumors seem to correlate with a lower likelihood of cTR (Table 3).

Table 3.
Correlation between age, sex, tumor size, tumor stage, SEPT9mr, and tumor response to TNT.
SEPT9mr also shows a statistically significant correlation with the N stage (p = 0.040) but not with the T stage (p = 0.846) in a Kruskal–Wallis test, and there is a moderate correlation with tumor size (Spearman’s correlation coefficient = 0.54, p = 0.001).
The likelihood of cTR depending on SEPT9mr and tumor size was explored in a logistic regression analysis (Figure 2) (Table 4).
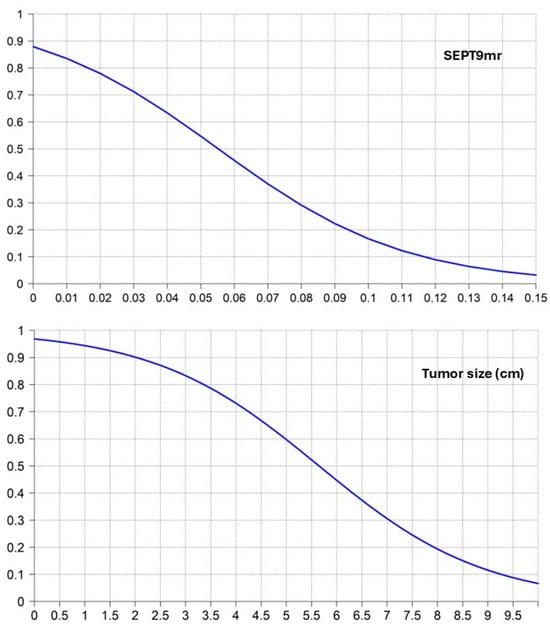
Figure 2.
Logistic regression curves of SEPT9mr and tumor size predicting the likelihood of cTR.

Table 4.
Logistic regression analysis of SEPT9mr and tumor size predicting the likelihood of cTR.
4. Discussion
Human carcinogenesis not only depends on genetic changes but also on epigenetic alterations like DNA methylation. Thus, aberrant DNA hypermethylation in the promoter region of some genes may lead to inappropriate gene silencing and cancer development [9]. SEPTIN9 is a gene located in chromosome 17q25 that codifies filamentous proteins involved in microtubule formation, angiogenesis, cell motility, cell proliferation, and cell cycle control, among others [9,10,11].
SEPTIN9 gene hypermethylation is one of the most studied epigenetic changes, given its implication in CRC carcinogenesis [9,11], and a well-known biomarker for CRC diagnosis and follow-up. High specificity and negative predictive value, and moderate sensitivity have been de-scribed for the early detection of CRC [5]. Given its significant decrease after surgery [12,13], it has demonstrated its utility as a biomarker of complete surgical resection [6], minimal residual disease, and tumor recurrence after surgery in patients with CRC [7,13]. It has also been proposed as a potential biomarker of antitumor therapy effectiveness since SEPT9m levels in plasma decrease by 1.7 times after chemotherapy and 2.3 times after RC resection [14]. Moreover, the plasmatic levels of SEPT9m are quantitatively correlated with tumor burden in patients with stage IV CRC and correlated with prognosis in terms of survival [15].
Tumor response to neoadjuvant chemoradiation is an important prognostic factor in patients with LARC [4], but the prediction of tumor response to TNT is a difficult setting. Multiple markers have been proposed, both pre- and post-neoadjuvant chemoradiation, with varied results: gene expression analysis; patient-derived organoids; single-nucleotide polymorphisms (SNPs); DNA methylation; microRNAs; circulating tumor DNA (ctDNA); carcinoembryonic antigen (CEA); circulating tumor cells; tumor size; T and N stage; tumor distance from the anal verge; circumferential extent; anterior tumor position; intratumoral budding; tumor microenvironment; mucinous histology; poor tumor differentiation; macroscopic ulceration; gut microbiome; lymphovascular invasion, perineural invasion, and absence of necrosis; tumor–stroma ratio; lymphocyte–monocyte ratio; body mass index; hemoglobin levels; PET/CT standardized uptake value (SUV); radiomics; time after chemoradiation; APC, PIK3CA, TP53, SMAD4, KRAS, NRAS, and BRAF mutations; pro-apoptotic factor Bax; the anti-apoptotic X-linked inhibitor of apoptosis protein (XIAP); VEGF; hypoxia-inducible protein factor-1 (HIF-1); osteopontin; myoferlin; fatty acid metabolism; and cytokines like IL-1 and IL-8… [4,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36]. But no reliable pre-treatment markers that predict tumor response to TNT in patients with LARC have been developed enough to reach regular clinical application, since all of them have important limitations [4].
One of the most employed biomarkers for diagnosis and follow-up of CRC is CEA, since its elevation is considered a strong marker of recurrence [37]. Nevertheless, CEA is not a specific marker of CRC, so it can be elevated in other digestive neoplasms and inflammatory diseases [37], and 70% of patients with RC have negative CEA levels [38]. Despite the fact that CEA does not seem to be a reliable marker for these settings, low CEA levels (≤5 ng/mL) have been associated with an increased likelihood of cPR to neoadjuvant chemoradiation in patients with LARC in some studies [35].
Therefore, there is an imperative need for the development of new biomarkers that could solve these limitations and predict tumor response to TNT. According to our results, pre-treatment SEPT9mr in plasmatic cfDNA significantly correlates with tumor size, N stage and tumor response to TNT, so higher values of SEPT9mr seem to predict a lower probability of cTR. Therefore, based on the pre-treatment SEPT9mr that we could select, at the time of diagnosis, those patients who will respond to TNT. Tumor size, but not tumor stage, also correlates with tumor response to TNT, so greater tumors seem to correlate with a lower likelihood of cTR.
It is important that there are no statistically significant differences in age between both groups (patients with and without a cTR), since DNA methylation is a physiological phenomenon that also increases with aging [39,40].
One of the main advantages of SEPT9mr compared with other SEPT9m tests is that it brings a quantitative, continuous, non-dichotomic, and relative value of the degree of methylation of SEPTIN9 gene that can also be monitored during LARC treatment and follow-up.
Nevertheless, these results must be taken with caution due to the relatively small sample size analyzed and validated in forthcoming studies, including larger, independent cohorts.
5. Conclusions
Pre-treatment SEPT9mr significantly correlates with tumor size, N stage, and the likelihood of cTR to TNT in patients with LARC. Therefore, SEPT9mr seems to be a valuable pre-treatment biomarker for predicting tumor response to TNT.
Author Contributions
Conceptualization: V.D.-P., M.G.-A., M.L.-A. and D.G.-O.; formal analysis: V.D.-P., M.G.-A., R.O.-S. and L.V.-C.; funding acquisition: M.G.-A., H.G. and D.G.-O.; investigation: V.D.-P., M.L.-A., R.O.-S., M.G.-A. and D.G.-O.; methodology: V.D.-P., M.G.-A., R.O.-S., M.L.-A. and D.G.-O.; project administration: V.D.-P., M.G.-A., M.L.-A. and D.G.-O.; resources: V.D.-P., M.G.-A., R.O.-S., L.V.-C., C.C., E.R.-H., R.F.-M. and D.R.-R.; supervision: V.D.-P., M.G.-A., M.L.-A., H.G. and D.G.-O.; validation: V.D.-P., M.G.-A. and R.O.-S.; visualization: V.D.-P.; writing—original draft: V.D.-P.; writing—review and editing: M.L.-A., R.O.-S., L.V.-C., C.C., E.R.-H., R.F.-M., D.R.-R., H.G., M.G.-A. and D.G.-O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the “Fondo de Investigaciones Sanitarias–ISCIII–FEDER”, Ministry of Health, Spain (grant number PI20/01052), and co-funded by the European Regional Development Fund.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Fundación Jiménez Díaz Research Ethics Committee (PIC 140-2017_FJD) on 10 February 2021.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Acknowledgments
Authors acknowledge Ignacio Mahillo for his help in the statistical analysis and Celia Urrutia and Miriam Riesco for blood sample collection.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| CRC | Colorectal cancer |
| RC | Rectal cancer |
| LARC | Locally advanced rectal cancer |
| cCR | Complete clinical response |
| TNT | Total neoadjuvant therapy |
| WW | Watch and wait |
| SEPT9m | SEPTIN9 gene methylation |
| SEPT9mr | SEPTIN9 gene methylation ratio |
| DRE | Digital rectal examination |
| MRI | Magnetic resonance imaging |
| mTRG | MRI Tumor Regression Grade |
| cfDNA | Cell-free DNA |
| ddPCR | Droplet digital polymerase chain reaction |
| cTR | Complete tumor response |
| cPR | Complete pathological response |
| CEA | Carcinoembryonic antigen |
References
- Colorectal Cancer: Statistics|Cancer.Net [Internet]. Available online: https://www.cancer.net/cancer-types/colorectal-cancer/statistics (accessed on 4 March 2025).
- Kasi, A.; Abbasi, S.; Handa, S.; Al-Rajabi, R.; Saeed, A.; Baranda, J.; Sun, W. Total Neoadjuvant Therapy vs Standard Therapy in Locally Advanced Rectal Cancer: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e2030097. [Google Scholar] [CrossRef]
- Kang, S.B.; Cho, J.R.; Jeong, S.Y.; Oh, J.H.; Ahn, S.; Choi, S.; Kim, D.W.; Lee, B.H.; Youk, E.G.; Park, S.C.; et al. Quality of life after sphincter preservation surgery or abdominoperineal resection for low rectal cancer (ASPIRE): A long-term prospective, multicentre, cohort study. Lancet Reg. Health West. Pac. 2020, 6, 100087. [Google Scholar] [CrossRef] [PubMed]
- Kokaine, L.; Gardovskis, A.; Gardovskis, J. Evaluation and Predictive Factors of Complete Response in Rectal Cancer after Neoadjuvant Chemoradiation Therapy. Medicina 2021, 57, 1044. [Google Scholar] [CrossRef] [PubMed]
- Hariharan, R.; Jenkins, M. Utility of the methylated SEPT9 test for the early detection of colorectal cancer: A systematic review and meta-analysis of diagnostic test accuracy. BMJ Open Gastroenterol. 2020, 7, e000355. [Google Scholar] [CrossRef] [PubMed]
- Leon Arellano, M.; García-Arranz, M.; Ruiz, R.; Olivera, R.; Magallares, S.; Olmedillas-Lopez, S.; Valdes-Sanchez, T.; Guadalajara, H.; García-Olmo, D. A First Step to a Biomarker of Curative Surgery in Colorectal Cancer by Liquid Biopsy of Methylated Septin 9 Gene. Dis. Markers. 2020, 2020, 9761406. [Google Scholar] [CrossRef]
- Leon Arellano, M.; García-Arranz, M.; Guadalajara, H.; Olivera-Salazar, R.; Valdes-Sanchez, T.; García-Olmo, D. Analysis of Septin 9 Gene Hypermethylation as Follow-Up Biomarker of Colorectal Cancer Patients after Curative Surgery. Diagnostics 2022, 12, 993. [Google Scholar] [CrossRef]
- Patel, U.B.; Taylor, F.; Blomqvist, L.; George, C.; Evans, H.; Tekkis, P.; Quirke, P.; Sebag-Montefiore, D.; Moran, B.; Heald, R.; et al. Magnetic resonance imaging-detected tumor response for locally advanced rectal cancer predicts survival outcomes: MERCURY experience. J. Clin. Oncol. 2011, 29, 3753–3760. [Google Scholar] [CrossRef]
- Fukushige, S.; Horii, A. DNA methylation in cancer: A gene silencing mechanism and the clinical potential of its biomarkers. Tohoku J. Exp. Med. 2013, 229, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Mostowy, S.; Cossart, P. Septins: The fourth component of the cytoskeleton. Nat. Rev. Mol. Cell Biol. 2012, 13, 183–194. [Google Scholar] [CrossRef]
- Peterson, E.A.; Petty, E.M. Conquering the complex world of human septins: Implications for health and disease. Clin. Genet. 2010, 77, 511–524. [Google Scholar] [CrossRef]
- Abd El Kader, L.; Soliman, A.H.; Salem, S.E.; Akel, S.Y.; Ibrahim, N.H. The Clinical Significance of Septin 9 and Colon Cancer Specific Antigen-2 (CCSA-2) in Colorectal Cancer. Asian Pac. J. Cancer Prev. 2023, 24, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.Y.; Chan, C.S.Y.; Lau, K.S.; Ng, L.; Cheng, Y.Y.; Leung, W.K. Application of droplet digital polymerase chain reaction of plasma methylated septin 9 on detection and early monitoring of colorectal cancer. Sci. Rep. 2021, 11, 23446. [Google Scholar] [CrossRef]
- Ponomaryova, A.A.; Rykova, E.Y.; Solovyova, A.I.; Tarasova, A.S.; Kostromitsky, D.N.; Dobrodeev, A.Y.; Afanasiev, S.A.; Cherdyntseva, N.V. Dynamic Changes in Circulating Methylated Markers in Response to Antitumor Therapy of Rectal Cancer. J. Gastrointest. Cancer. 2024, 55, 1190–1198. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Hu, P.; Liu, J.; Chen, L. mSEPT9 Can Monitor the Response and Predict the Prognosis of Stage IV Colorectal Cancer Patients with Liver Metastasis Undergoing Potentially Curative Surgery. J. Surg. Res. 2021, 267, 485–494. [Google Scholar] [CrossRef]
- Empuku, S.; Nakajima, K.; Akagi, T.; Kaneko, K.; Hijiya, N.; Etoh, T.; Shiraishi, N.; Moriyama, M.; Inomata, M. An 80-gene set to predict response to preoperative chemoradiotherapy for rectal cancer by principle component analysis. Mol. Clin. Oncol. 2016, 4, 733–739. [Google Scholar] [CrossRef]
- Yao, Y.; Xu, X.; Yang, L.; Zhu, J.; Wan, J.; Shen, L.; Xia, F.; Fu, G.; Deng, Y.; Pan, M.; et al. Patient-Derived Organoids Predict Chemoradiation Responses of Locally Advanced Rectal Cancer. Cell Stem Cell. 2020, 26, 17–26.e6. [Google Scholar] [CrossRef]
- Timmerman, C.; Taveras, L.R.; Huerta, S. Clinical and molecular diagnosis of pathologic complete response in rectal cancer: An update. Expert. Rev. Mol. Diagn. 2018, 18, 887–896. [Google Scholar] [CrossRef]
- Dayde, D.; Tanaka, I.; Jain, R.; Tai, M.C.; Taguchi, A. Predictive and Prognostic Molecular Biomarkers for Response to Neoadjuvant Chemoradiation in Rectal Cancer. Int. J. Mol. Sci. 2017, 18, 573. [Google Scholar] [CrossRef]
- De Palma, F.D.E.; Luglio, G.; Tropeano, F.P.; Pagano, G.; D’Armiento, M.; Kroemer, G.; Maiuri, M.C.; De Palma, G.D. The Role of Micro-RNAs and Circulating Tumor Markers as Predictors of Response to Neoadjuvant Therapy in Locally Advanced Rectal Cancer. Int. J. Mol. Sci. 2020, 21, 7040. [Google Scholar] [CrossRef]
- Yi, Y.; Shen, L.; Shi, W.; Xia, F.; Zhang, H.; Wang, Y.; Zhang, J.; Wang, Y.; Sun, X.; Zhang, Z.; et al. Gut Microbiome Components Predict Response to Neoadjuvant Chemoradiotherapy in Patients with Locally Advanced Rectal Cancer: A Prospective, Longitudinal Study. Clin. Cancer Res. 2021, 27, 1329–1340. [Google Scholar] [CrossRef]
- Patel, P.M.; Harris, K.; Huerta, S. Clinical and molecular diagnosis of pathologic complete response in rectal cancer. Expert. Rev. Mol. Diagn. 2015, 15, 1505–1516. [Google Scholar] [CrossRef] [PubMed]
- Bedrikovetski, S.; Traeger, L.; Vather, R.; Moore, J.W.; Sammour, T. Clinical and biochemical predictors of tumor response after neoadjuvant therapy in rectal cancer. Asia Pac. J. Clin. Oncol. 2023, 19, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, E.; Bektas, S.; Pelen, Z.; Yanik, I.; Er, A.M.; Cengel, F.; Gumuskaya, P.Ö. Histopathological, Radiological, and Demographic Factors Predicting the Response to Neoadjuvant Therapy for Rectal Cancer. J. Gastrointest. Cancer. 2022, 53, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.K.; Hur, H. New Perspectives on Predictive Biomarkers of Tumor Response and Their Clinical Application in Preoperative Chemoradiation Therapy for Rectal Cancer. Yonsei Med. J. 2015, 56, 1461–1477. [Google Scholar] [CrossRef]
- Fowler, H.; Clifford, R.E.; Bowden, D.; Sutton, P.A.; Govindarajah, N.; Fok, M.; Glenn, M.; Wall, M.; Rubbi, C.; Buczacki, S.J.A.; et al. Myoferlin: A Potential Marker of Response to Radiation Therapy and Survival in Locally Advanced Rectal Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2024, 120, 1111–1123. [Google Scholar] [CrossRef]
- Wen, X.; Zee, S.Y.; Shroyer, K.R.; Bandovic, J. Intratumoral Budding and Tumor Microenvironment in Pretreatment Rectal Cancer Biopsies Predict the Response to Neoadjuvant Chemoradiotherapy. Appl. Immunohistochem. Mol. Morphol. 2022, 30, 1–7. [Google Scholar] [CrossRef]
- Alden, S.L.; Lee, V.; Narang, A.K.; Meyer, J.; Gearhart, S.L.; Christenson, E.S. Circulating Tumor DNA to Predict Radiographic and Pathologic Response to Total Neoadjuvant Therapy in Locally Advanced Rectal Cancer. Oncologist 2024, 29, e414–e418. [Google Scholar] [CrossRef]
- Zhou, H.; Chen, Y.; Xiao, Y.; Wu, Q.; Li, H.; Li, Y.; Su, G.; Ke, L.; Wu, J.; Li, J. Evaluation of the ability of fatty acid metabolism signature to predict response to neoadjuvant chemoradiotherapy and prognosis of patients with locally advanced rectal cancer. Front. Immunol. 2022, 13, 1050721. [Google Scholar] [CrossRef]
- Jeon, S.H.; Song, C.; Chie, E.K.; Kim, B.; Kim, Y.H.; Chang, W.; Lee, Y.J.; Chung, J.H.; Chung, J.B.; Lee, K.W.; et al. Combining Radiomics and Blood Test Biomarkers to Predict the Response of Locally Advanced Rectal Cancer to Chemoradiation. In Vivo 2020, 34, 2955–2965. [Google Scholar] [CrossRef]
- Huang, Y.; Lee, D.; Young, C. Predictors for complete pathological response for stage II and III rectal cancer following neoadjuvant therapy—A systematic review and meta-analysis. Am. J. Surg. 2020, 220, 300–308. [Google Scholar] [CrossRef]
- Strous, M.T.A.; Faes, T.K.E.; Heemskerk, J.; Lohman, B.G.P.M.; Simons, P.C.G.; Janssen Heijnen, M.L.G.; Vogelaar, F.J.; de Bruïne, A.P. Tumour-stroma ratio to predict pathological response to neo-adjuvant treatment in rectal cancer. Surg. Oncol. 2022, 45, 101862. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.; Eglinton, T.W.; Frizelle, F.A. Clinical predictors of response to chemoradiotherapy for rectal cancer as an aid to organ preservation. ANZ J. Surg. 2021, 91, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Chapman, B.C.; Lai, S.H.; Friedrich, T.; Lieu, C.H.; Moskalenko, M.; Olsen, J.R.; Herter, W.; Birnbaum, E.H.; McCarter, M.D.; Vogel, J.D. Rectal Cancer: Clinical and Molecular Predictors of a Complete Response to Total Neoadjuvant Therapy. Dis. Colon. Rectum. 2023, 66, 521–530. [Google Scholar] [CrossRef]
- Xu, Y.J.; Tao, D.; Qin, S.B.; Xu, X.Y.; Yang, K.W.; Xing, Z.X.; Zhou, J.Y.; Jiao, Y.; Wang, L.L. Prediction of pathological complete response and prognosis in locally advanced rectal cancer. World J. Gastrointest. Oncol. 2024, 16, 2520–2530. [Google Scholar] [CrossRef]
- Yilmaz, S.; Liska, D.; Conces, M.L.; Tursun, N.; Elamin, D.; Ozgur, I.; Maspero, M.; Rosen, D.R.; Khorana, A.A.; Balagamwala, E.H.; et al. What Predicts Complete Response to Total Neoadjuvant Therapy in Locally Advanced Rectal Cancer? Dis. Colon. Rectum. 2025, 68, 60–68. [Google Scholar] [CrossRef]
- Lech, G.; Słotwiński, R.; Słodkowski, M.; Krasnodębski, I.W. Colorectal cancer tumour markers and biomarkers: Recent therapeutic advances. World J. Gastroenterol. 2016, 22, 1745–1755. [Google Scholar] [CrossRef]
- Shen, D.; Wang, X.; Wang, H.; Xu, G.; Xie, Y.; Zhuang, Z.; Huang, Z.; Li, J.; Lin, J.; Wang, P.; et al. Current Surveillance After Treatment is Not Sufficient for Patients With Rectal Cancer With Negative Baseline CEA. J. Natl. Compr. Canc Netw. 2022, 20, 653–662.e3. [Google Scholar] [CrossRef]
- Mishra, S.; Raval, M.; Kachhawaha, A.S.; Tiwari, B.S.; Tiwari, A.K. Aging: Epigenetic modifications. Prog. Mol. Biol. Transl. Sci. 2023, 197, 171–209. [Google Scholar] [CrossRef]
- Johnson, A.A.; Akman, K.; Calimport, S.R.; Wuttke, D.; Stolzing, A.; de Magalhães, J.P. The role of DNA methylation in aging, rejuvenation, and age-related disease. Rejuvenation Res. 2012, 15, 483–494. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).