CAR-T Cell Therapies in B-Cell Acute Lymphoblastic Leukemia: Emerging Data and Open Issues
Simple Summary
Abstract
1. Introduction
2. CAR-T: Pivotal Clinical Trials
3. Sequential Use of CAR T and allo-SCT
4. Dual-Targeting CAR T
5. Allogeneic CAR-T
6. Fast CAR-T
7. Incorporation of CAR-T Cell Therapy into Frontline Treatment of B-ALL
8. T-Cell Acute Lymphoblastic Leukemia (T-ALL) and the Role of CAR-T Therapy
9. Toxicities Associated with CAR T
10. Expert Opinion
11. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jabbour, E.J.; Faderl, S.; Kantarjian, H.M. Adult acute lymphoblastic leukemia. Mayo Clin. Proc. 2005, 80, 1517–1527. [Google Scholar] [CrossRef]
- Bassan, R.; Hoelzer, D. Modern therapy of acute lymphoblastic leukemia. J. Clin. Oncol. 2011, 29, 532–543. [Google Scholar] [CrossRef]
- Pui, C.H.; Relling, M.V.; Downing, J.R. Acute lymphoblastic leukemia. N. Engl. J. Med. 2004, 350, 1535–1548. [Google Scholar] [CrossRef] [PubMed]
- Siegel, S.E.; Stock, W.; Johnson, R.H.; Advani, A.; Muffly, L.; Douer, D.; Reed, D.; Lewis, M.; Freyer, D.R.; Shah, B.; et al. Pediatric-Inspired Treatment Regimens for Adolescents and Young Adults with Philadelphia Chromosome-Negative Acute Lymphoblastic Leukemia: A Review. AMA Oncol. 2018, 4, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Pulte, D.; Gondos, A.; Brenner, H. Improvement in survival in younger patients with acute lymphoblastic leukemia from the 1980s to the early 21st century. Blood 2009, 113, 1408–1411. [Google Scholar] [CrossRef]
- Kantarjian, H.; Thomas, D.; O’Brien, S.; Cortes, J.; Giles, F.; Jeha, S.; Bueso-Ramos, C.E.; Pierce, S.; Shan, J.; Koller, C.; et al. Long-term follow-up results of hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (Hyper-CVAD), a dose-intensive regimen, in adult acute lymphocytic leukemia. Cancer 2004, 101, 2788–2801. [Google Scholar] [CrossRef] [PubMed]
- Giebel, S.; Labopin, M.; Socié, G.; Beelen, D.; Browne, P.; Volin, L.; Kyrcz-Krzemien, S.; Yakoub-Agha, I.; Aljurf, M.; Wu, D.; et al. Improving results of allogeneic hematopoietic cell transplantation for adults with acute lymphoblastic leukemia in first complete remission: An analysis from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. Haematologica 2017, 102, 139–149. [Google Scholar] [CrossRef]
- Gökbuget, N.; Boissel, N.; Chiaretti, S.; Dombret, H.; Doubek, M.; Fielding, A.; Foà, R.; Giebel, S.; Hoelzer, D.; Hunault, M.; et al. Management of ALL in adults: 2024 ELN recommendations from a European expert panel. Blood 2024, 143, 1903–1930. [Google Scholar] [CrossRef]
- Gökbuget, N.; Dombret, H.; Ribera, J.M.; Fielding, A.K.; Advani, A.; Bassan, R.; Chia, V.; Doubek, M.; Giebel, S.; Hoelzer, D.; et al. International reference analysis of outcomes in adults with B-precursor Ph-negative relapsed/refractory acute lymphoblastic leukemia. Haematologica 2016, 101, 1524–1533. [Google Scholar] [CrossRef]
- Einsiedel, H.G.; von Stackelberg, A.; Hartmann, R.; Fengler, R.; Schrappe, M.; Janka-Schaub, G.; Mann, G.; Hählen, K.; Göbel, U.; Klingebiel, T.; et al. Long-term outcome in children with relapsed ALL by risk-stratified salvage therapy: Results of trial acute lymphoblastic leukemia-relapse study of the Berlin- Frankfurt-Munster Group 87. J. Clin. Oncol. 2005, 23, 7942–7950. [Google Scholar] [CrossRef]
- Tallen, G.; Ratei, R.; Mann, G.; Kaspers, G.; Niggli, F.; Karachunsky, A.; Ebell, W.; Escherich, G.; Schrappe, M.; Klingebiel, T.; et al. Long-term outcome in children with relapsed acute lymphoblastic leukemia after time-point and site-of- relapse stratification and intensified short-course multidrug chemotherapy: Results of trial ALL-REZ BFM 90. J. Clin. Oncol. 2010, 28, 2339–2347. [Google Scholar] [CrossRef]
- Hahn, T.; Wall, D.; Camitta, B.; Davies, S.; Dillon, H.; Gaynon, P.; Larson, R.A.; Parsons, S.; Seidenfeld, J.; Weisdorf, D.; et al. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute lymphoblastic leukemia in adults: An evidence-based review. Biol. Blood Marrow Transplant. 2006, 12, 1–30. [Google Scholar] [CrossRef]
- Eapen, M.; Raetz, E.; Zhang, M.-J.; Muehlenbein, C.; Devidas, M.; Abshire, T.; Billett, A.; Homans, A.; Camitta, B.; Carroll, W.L.; et al. Outcomes after HLA-matched sibling transplantation or chemotherapy in children with B-precursor acute lymphoblastic leukemia in a second remission: A collaborative study of the Children’s Oncology Group and the Center for International Blood and Marrow Transplant Research. Blood 2006, 107, 4961–4967. [Google Scholar] [PubMed][Green Version]
- Passweg, J.R.; Baldomero, H.; Atlija, M.; Kleovoulou, I.; Witaszek, A.; Alexander, T.; Angelucci, E.; Averbuch, D.; Bazarbachi, A.; Ciceri, F.; et al. The 2023 EBMT report on hematopoietic cell transplantation and cellular therapies. Increased use of allogeneic HCT for myeloid malignancies and of CAR-T at the expense of autologous HCT. Bone Marrow Transplant. 2025, 60, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Spellman, S.R.; Xu, K.; Oloyede, T.; Ahn, K.W.; Akhtar, O.; Bolon, Y.-T.; Broglie, L.; Bloomquist, J.; Bupp, C.; Chen, M.; et al. Current Activity Trends and Outcomes in Hematopoietic Cell Transplantation and Cellular Therapy—A Report from the CIBMTR. Transplant. Cell Ther. 2025, 31, 505–532. [Google Scholar] [CrossRef]
- Malagola, M.; Greco, R.; Peccatori, J.; Isidori, A.; Romee, R.; Mohty, M.; Ciceri, F.; Russo, D. Editorial: Strengths and Challenges of Allo-SCT in the Modern Era. Front. Oncol. 2022, 12, 850403. [Google Scholar] [CrossRef] [PubMed]
- Grupp, S.A.; Kalos, M.; Barrett, D.; Aplenc, R.; Porter, D.L.; Rheingold, S.R.; Teachey, D.T.; Chew, A.; Hauck, B.; Wright, J.F.; et al. Chimeric antigen receptor-modified T cells for acute lymphoid leukemia. N. Engl. J. Med. 2013, 368, 1509–1518. [Google Scholar] [CrossRef]
- Brentjens, R.J.; Davila, M.L.; Riviere, I.; Park, J.; Wang, X.; Cowell, L.G.; Bartido, S.; Stefanski, J.; Taylor, C.; Olszewska, M.; et al. CD19-targeted T cells rapidly induce molecular remissions in adults with chemotherapy-refractory acute lymphoblastic leukemia. Sci. Transl. Med. 2013, 5, 177ra38. [Google Scholar] [CrossRef]
- Kochenderfer, J.N.; Dudley, M.E.; Feldman, S.A.; Wilson, W.H.; Spaner, D.E.; Maric, I.; Stetler-Stevenson, M.; Phan, G.Q.; Hughes, M.S.; Sherry, R.M.; et al. B-cell depletion and remissions of malignancy along with cytokine-associated toxicity in a clinical trial of anti-CD19 chimeric-antigen-receptor-transduced T cells. Blood 2012, 119, 2709–2720. [Google Scholar] [CrossRef]
- Davila, M.L.; Riviere, I.; Wang, X.; Bartido, S.; Park, J.; Curran, K.; Chung, S.S.; Stefanski, J.; Borquez-Ojeda, O.; Olszewska, M.; et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci. Transl. Med. 2014, 6, 224ra25. [Google Scholar] [CrossRef]
- Park, J.H.; Riviere, I.; Gonen, M.; Wang, X.; Sénéchal, B.; Curran, K.J.; Sauter, C.; Wang, Y.; Santomasso, B.; Mead, E.; et al. Long-term follow-up of CD19 CAR therapy in acute lymphoblastic leukemia. N. Engl. J. Med. 2018, 378, 449–459. [Google Scholar] [CrossRef] [PubMed]
- A Grupp, S.; Frey, N.V.; Aplenc, R.; Barrett, D.M.; Chew, A.; Kalos, M.; Levine, B.L.; Litchman, M.; Maude, S.L.; Rheingold, S.R.; et al. T Cells engineered with a chimeric antigen receptor (CAR) targeting CD19 (CTL019) produce significant in vivo proliferation, complete responses and long-term persistence without GVHD in children and adults with relapsed, refractory ALL. Blood 2013, 122, 67. [Google Scholar] [CrossRef]
- Rampotas, A.; Roddie, C. The present and future of CAR T-cell therapy for adult B-cell ALL. Blood 2025, 145, 1485–1497. [Google Scholar] [CrossRef] [PubMed]
- Ershova, A.; Goldaeva, A.; Staliarova, A.; Bulatov, E.; Petukhov, A.; Barlev, N. Future perspectives on novel CAR-T therapeutics beyond CD19 and BCMA in onco-hematology. Front. Immunol. 2025, 16, 1592377. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leahy, A.B.; Elgarten, C.W.; Grupp, S.A.; Maude, S.L.; Teachey, D.T. Tisagenlecleucel for the treatment of B-cell acute lymphoblastic leukemia. Expert. Rev. Anticancer Ther. 2018, 18, 959–971. [Google Scholar] [CrossRef]
- Maude, S.L.; Laetsch, T.W.; Buechner, J.; Rives, S.; Boyer, M.; Bittencourt, H.; Bader, P.; Verneris, M.R.; Stefanski, H.E.; Myers, G.D.; et al. Tisagenlecleucel in Children and Young Adults with B-Cell Lymphoblastic Leukemia. N. Engl. J. Med. 2018, 378, 439–448. [Google Scholar] [CrossRef]
- Laetsch, T.W.; Maude, S.L.; Rives, S.; Hiramatsu, H.; Bittencourt, H.; Bader, P.; Baruchel, A.; Boyer, M.; De Moerloose, B.; Qayed, M.; et al. Three-Year Update of Tisagenlecleucel in Pediatric and Young Adult Patients with Relapsed/Refractory Acute Lymphoblastic Leukemia in the ELIANA Trial. J. Clin. Oncol. 2023, 41, 1664–1669. [Google Scholar] [CrossRef]
- Pasquini, M.C.; Hu, Z.-H.; Curran, K.; Laetsch, T.; Locke, F.; Rouce, R.; Pulsipher, M.A.; Phillips, C.L.; Keating, A.; Frigault, M.J.; et al. Real-world evidence of tisagenlecleucel for pediatric acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Adv. 2020, 4, 5414–5424. [Google Scholar] [CrossRef]
- Shah, B.D.; Ghobadi, A.; Oluwole, O.O.; Logan, A.C.; Boissel, N.; Cassaday, R.D.; Leguay, T.; Bishop, M.R.; Topp, M.S.; Tzachanis, D.; et al. KTE-X19 for relapsed or refractory adult B-cell acute lymphoblastic leukaemia: Phase 2 results of the single-arm, open-label, multicentre ZUMA-3 study. Lancet 2021, 398, 491–502. [Google Scholar] [CrossRef]
- Shah, B.D.; Cassaday, R.D.; Park, J.H.; Houot, R.; Logan, A.C.; Boissel, N.; Leguay, T.; Bishop, M.R.; Topp, M.S.; O’Dwyer, K.M.; et al. Three-year analysis of adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia treated with brexucabtagene autoleucel in ZUMA-3. Leukemia 2025, 39, 1058–1068. [Google Scholar] [CrossRef] [PubMed]
- Bouchkouj, N.; Lin, X.; Wang, X.; Przepiorka, D.; Xu, Z.; Purohit-Sheth, T.; Theoret, M. FDA Approval Summary: Brexucabtagene Autoleucel for Treatment of Adults with Relapsed or Refractory B-Cell Precursor Acute Lymphoblastic Leukemia. Oncologist 2022, 27, 892–899. [Google Scholar] [CrossRef]
- Oluwole, O.; Ghobadi, A.; Cassaday, R.; Park, J.H.; Houot, R.; Logan, A.; Boissel, N.; Leguay, T.; Bishop, M.; Topp, M.; et al. Five-Year Survival Outcomes of Patiens (PTS) with Relapsed or Refractory B-Cell Acute Lymphoblastic Leukemia (R/R B-ALL) Treaded with Brexucabtagene Autoleucel (BREXU-CEL) in ZUMA-3. In Proceedings of the European Hematology Association Congress, Milan, Italy, 12 June–15 October 2025; 2025. [Google Scholar]
- Roloff, G.W.; Aldoss, I.; Kopmar, N.E.; Lin, C.; Dekker, S.E.; Gupta, V.K.; O’Connor, T.E.; Jeyakumar, N.; Muhsen, I.N.; Valtis, Y.; et al. Outcomes After Brexucabtagene Autoleucel Administered as a Standard Therapy for Adults with Relapsed/Refractory B-Cell ALL. J. Clin. Oncol. 2025, 43, 558–566. [Google Scholar] [CrossRef] [PubMed]
- FDA. FDA Approves Obecabtageneautoleucel for Adults with Relapsed or Refractory B-Cell Precursor Acute Lymphoblastic Leukemia. 8 November 2024. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-obecabtagene-autoleucel-adults-relapsed-or-refractory-b-cell-precursor-acute (accessed on 10 July 2025).
- Yared, J.A.; Fromowitz, A.; Kocoglu, M.; Hardy, N.; Atanackovic, D.; Rapoport, A.P. Obecabtageneautoleucel, a novel CD19-directed CAR T-cell therapy for relapsed/refractory B-cell acute lymphoblastic leukemia: The future for reducing toxicity and T-cell exhaustion? Expert Rev. Hematol. 2025, 18, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Roddie, C.; Sandhu, K.S.; Tholouli, E.; Logan, A.C.; Shaughnessy, P.; Barba, P.; Ghobadi, A.; Guerreiro, M.; Yallop, D.; Abedi, M.; et al. Obecabtagene Autoleucel in Adults with B-Cell Acute Lymphoblastic Leukemia. N. Engl. J. Med. 2024, 391, 2219–2230. [Google Scholar] [CrossRef]
- Park, J.H.; Roddie, C.; Tholouli, E.; Sandhu, K.S.; Shaughnessy, P.; Barba, P.; Guerreiro, M.; Yallop, D.; Logan, A.; Abedi, M.; et al. Can CAR T-cell therapy be a definitive treatment for adult r/r B-ALL without transplant? Long-term findings and predictors of sustained remission for obecabtageneautoleucel. In Proceedings of the European Hematology Association Congress, Milan, Italy, 12–15 June 2025. [Google Scholar]
- Shah, B.D.; Yallop, D.; Jabbour, E.; Barba, P.; Tholouli, E.; Topp, M.S.; Sandhu, K.S.; Chaganti, S.; Park, J.H.; Menne, T.; et al. Efficacy and safety outcomes of obecabtageneautoleucel (obe-cel) stratified by age in patients with relapsed/refractory B-cell acute lymphoblastic leukemia (r/r B-ALL). In Proceedings of the European Hematology Association Congress, Milan, Italy, 12–15 June 2025. [Google Scholar]
- Cappell, K.M.; Kochenderfer, J.N. Long-term outcomes following CAR T cell therapy: What we know so far. Nat. Rev. Clin. Oncol. 2023, 20, 359–371. [Google Scholar] [CrossRef]
- Hay, K.A.; Gauthier, J.; Hirayama, A.V.; Voutsinas, J.M.; Wu, Q.; Li, D.; Gooley, T.A.; Cherian, S.; Chen, X.; Pender, B.S.; et al. Factors associated with durable EFS in adult B-cell ALL patients achieving MRD-negative CR after CD19 CAR T-cell therapy. Blood 2019, 133, 1652–1663. [Google Scholar] [CrossRef]
- Jiang, H.; Li, C.; Yin, P.; Guo, T.; Liu, L.; Xia, L.; Wu, Y.; Zhou, F.; Ai, L.; Shi, W.; et al. Anti-CD19 chimeric antigen receptor-modified T-cell therapy bridging to allogeneic hematopoietic stem cell transplantation for relapsed/refractory B-cell acute lymphoblastic leukemia: An open-label pragmatic clinical trial. Am. J. Hematol. 2019, 94, 1113–1122. [Google Scholar] [CrossRef]
- Pan, J.; Yang, J.F.; Deng, B.P.; Zhao, X.J.; Zhang, X.; Lin, Y.H.; Wu, Y.N.; Deng, Z.L.; Zhang, Y.L.; Liu, S.H.; et al. High efficacy and safety of low-dose CD19-directed CAR-T cell therapy in 51 refractory or relapsed B acute lymphoblastic leukemia patients. Leukemia 2017, 31, 2587–2593. [Google Scholar] [CrossRef]
- Shah, B.D.; Cassaday, R.D.; Park, J.H.; Houot, R.; Oluwole, O.O.; Logan, A.C.; Boissel, N.; Leguay, T.; Bishop, M.R.; Topp, M.S.; et al. Impact of prior therapies and subsequent transplantation on outcomes in adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia treated with brexucabtagene autoleucel in ZUMA-3. J. Immunother. Cancer 2023, 11, e007118. [Google Scholar] [CrossRef]
- Aldoss, I.; Shan, H.; Yang, D.; Clark, M.C.; Al Malki, M.; Aribi, A.; Agrawal, V.; Sandhu, K.; Salhotra, A.; Pourhassan, H.; et al. Consolidation with First and Second Allogeneic Transplants in Adults with Relapsed/Refractory B-ALL Following Response to CD19CAR T Cell Therapy. Transplant. Cell Ther. 2024, 30, 788.e1–788.e9. [Google Scholar] [CrossRef]
- Shadman, M.; Gauthier, J.; Hay, K.A.; Voutsinas, J.M.; Milano, F.; Li, A.; Hirayama, A.V.; Sorror, M.L.; Cherian, S.; Chen, X.; et al. Safety of allogeneic hematopoietic transplant in adults after CD19-targeted CAR T-cell therapy. Blood Adv. 2019, 3, 3062–3069. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Dong, Y.; Shi, J.; Zhang, M.; Kong, D.; Feng, J.; Fu, S.; Xiao, P.; Hong, R.; Xu, H.; et al. Sequential allogeneic HSCT after CAR-T therapy for relapsed/refractory acute lymphoblastic leukemia patients: A long-term follow-up result. J. Adv. Res. 2025, in press. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q.; Wei, R.; Wang, Q.; Jiang, S.; Wu, Y.; Min, C.; Guo, S.; Zhang, Y.; Sun, X.; Wu, H.; et al. A bi-specific CAR-T cell therapy targeting CD19 and CD22 in relapsed or refractory B-ALL. Clin. Exp. Med. 2025, 25, 264. [Google Scholar] [CrossRef]
- NCT02443831—CARPALL: Immunotherapy with CD19 CAR T-Cells for CD19+ Haematological Malignancies. Available online: https://www.mycancergenome.org/content/clinical_trials/NCT02443831/ (accessed on 13 November 2020).
- Ghorashian, S.; Kramer, A.M.; Onuoha, S.; Wright, G.; Bartram, J.; Richardson, R.; Albon, S.J.; Casanovas-Company, J.; Castro, F.; Popova, B.; et al. Enhanced CAR T cell expansion and prolonged persistence in pediatric patients with ALL treated with a low-affinity CD19 CAR. Nat. Med. 2019, 25, 1408–1414. [Google Scholar] [CrossRef]
- Ghorashian, S.; Lucchini, G.; Richardson, R.; Nguyen, K.; Terris, C.; Guvenel, A.; Oporto-Espuelas, M.; Yeung, J.; Pinner, D.; Chu, J.; et al. CD19/CD22 targeting with cotransduced CAR T cells to prevent antigen-negative relapse after CAR T-cell therapy for B-cell ALL. Blood 2024, 143, 118–123. [Google Scholar] [CrossRef]
- Biederstädt, A.; Bassermann, F.; Hecker, J.S. Allogeneic CAR-engineered cellular therapy for relapsed and refractory large B cell lymphoma: A systematic review and meta-analysis. Front. Immunol. 2025, 16, 1585556. [Google Scholar] [CrossRef]
- Available online: https://clinicaltrials.gov/study/NCT04150497 (accessed on 4 November 2019).
- Jain, N.; Chevallier, P.; Liu, H.; Schiller, G.J.; Méar, J.-B.; DeAngelo, D.J.; Curran, K.J.; Grupp, S.; Baruchel, A.; Balsat, M.; et al. Updated Results of the Phase I BALLI-01 Trial of UCART22 Process 2 (P2), an Anti-CD22 Allogeneic CAR-T Cell Product Manufactured ByCellectis Biologics, in Patients with Relapsed or Refractory (R/R) CD22+ B-Cell Acute Lymphoblastic Leukemia (B-ALL). Blood 2023, 142 (Suppl. S1), 4847. [Google Scholar] [CrossRef]
- Boissel, N.; Chevallier, P.; Curran, K.; Schiller, G.; Liu, H.; Larson, R.; Deangelo, D.J.; Mear, J.B.; Grupp, S.; Baruchel, A. P1408, updated results of the Phase I BALLI-01 trial of UCART22, an ANTI-CD22 allogeneic CAR-T CELL product, in patients with relapsed or refractory (R/R) CD22+ B-cell acute lymphoblastic leukemia (B-ALL). Hemasphere 2023, 7 (Suppl. S3), e323373f. [Google Scholar] [CrossRef]
- Sun, G.; Mei, H.; Zhou, Y.; Wang, A.; Pan, T.; Lu, H.; Ren, J.; Zhu, X. A phase I study of allogeneic anti-CD19 CAR-T therapy for patients with CD19+ relapsed/refractory acute B-lymphoblastic leukemia. J. Clin. Oncol. 2025, 43, 6525. [Google Scholar] [CrossRef]
- Tan, X.; Wang, J.; Chen, S.; Liu, L.; Li, Y.; Tu, S.; Yi, H.; Zhou, J.; Wang, S.; Liu, L.; et al. Novel CD19 Fast-CAR-T cells vs. CD19 conventional CAR-T cells for the treatment of relapsed/refractory CD19-positive B-cell acute lymphoblastic leukemia. Chin. Med. J. 2025. In press. [Google Scholar]
- Haddad, F.G.; Kantarjian, H.; Short, N.J.; Jain, N.; Senapati, J.; Ravandi, F.; Jabbour, E. Incorporation of Immunotherapy Into Adult B-Cell Acute Lymphoblastic Leukemia Therapy. J. Natl. Compr. Canc. Netw. 2025, 23, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Aldoss, I.; Khaled, S.K.; Wang, X.; Palmer, J.; Wang, Y.; Wagner, J.R.; Clark, M.C.; Simpson, J.; Paul, J.; Vyas, V.; et al. Favorable activity and safety profile of memory-enriched CD19-targeted chimeric antigen receptor T-cell therapy in adults with high-risk relapsed/refractory ALL. Clin. Cancer Res. 2023, 29, 742–753. [Google Scholar] [CrossRef] [PubMed]
- Aldoss, I.; Wang, X.; Zhang, J.; Guan, M.; Espinosa, R.; Agrawal, V.; Artz, A.; Sanani, N.; Goldberg, L.; Kim, T.; et al. CD19-CAR T cells as definitive consolidation for older adults with B-cell acute lymphoblastic leukemia in first complete remission: A pilot study. Blood 2024, 144 (Suppl. S1), 966. [Google Scholar] [CrossRef]
- Feng, Y.; Leveille, E.; Park, J.H.; Müschen, M. Moving cellular therapies to the front line for Ph+ B cell acute lymphoblastic leukemia. Cell Rep. Med. 2025, 6, 102184. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gökbuget, N.; Boissel, N.; Chiaretti, S.; Dombret, H.; Doubek, M.; Fielding, A.K.; Foà, R.; Giebel, S.; Hoelzer, D.; Hunault, M.; et al. Diagnosis, prognostic factors, and assessment of ALL in adults: 2024 ELN recommendations from a European expert panel. Blood 2024, 143, 1891–1902. [Google Scholar] [CrossRef]
- Raetz, E.A.; Teachey, D.T. T-cell acute lymphoblastic leukemia. Hematol. Am. Soc. Hematol. Educ. Program 2016, 2016, 580–588. [Google Scholar] [CrossRef]
- Teachey, D.T.; O’Connor, D. How I treat newly diagnosed T-cell acute lymphoblastic leukemia and T-cell lymphoblastic lymphoma in children. Blood 2020, 135, 159–166. [Google Scholar] [CrossRef]
- Litzow, M.R.; Ferrando, A.A. How I treat T-cell acute lymphoblastic leukemia in adults. Blood 2015, 126, 833–841. [Google Scholar] [CrossRef]
- Shen, Y.; Lu, H.; Lin, J.; Liu, M.; Chu, M.; Shen, D.; Zhang, X.; Fan, Y.; Chen, J.; Hu, S.; et al. Haploidentical hematopoietic cell transplantation combined with umbilical cord blood vs. haploidentical hematopoietic cell transplantation in T-cell acute lymphoblastic leukemia patients: A multicenter real-world study. Transplant. Cell Ther. 2025, in press. [Google Scholar] [CrossRef]
- Xiao, J.; Liu, Y.; Shen, Y.; Li, J.; Wang, Y.; Chen, S.; Tang, X.; Yang, L.; Zhou, B.; Xu, Y.; et al. Clinical Outcomes of CD7 CAR-T Cell Therapy in Relapsed or Refractory T-Cell Acute Lymphoblastic Leukemia and Lymphoblastic Lymphoma Patients. Hematol. Oncol. 2025, 43, e70081. [Google Scholar] [CrossRef] [PubMed]
- Dashti, M.; Habibi, M.A.; Nejati, N.; Robat-Jazi, B.; Ahmadpour, M.; Dokhani, N.; Nejad, A.R.; Karami, S.; Alinejad, E.; Malekijoo, A.H.; et al. Clinical Efficacy and Safety of CD7-Targeted CAR T Cell Therapy for T-cell Malignancies: A Systematic Review and Meta-analysis. Anticancer Agents Med. Chem. 2025, 25, 42–51. [Google Scholar] [CrossRef]
- Yang, Y.; Zhang, Y.; Mu, W. Engineering CD5-targeting CAR-NK cells from peripheral blood for the treatment of CD5-positive hematological malignancies. J. Transl. Med. 2025, 23, 409. [Google Scholar]
- Tirado, N.; Fidyt, K.; Mansilla, M.J.; Garcia-Perez, A.; Martínez-Moreno, A.; Vinyoles, M.; Alcain, J.; García-Peydró, M.; Roca-Ho, H.; Fernandez-Fuentes, N.; et al. CAR-T cells targeting CCR9 and CD1a for the treatment of T cell acute lymphoblastic leukemia. J. Hematol. Oncol. 2025, 18, 69. [Google Scholar] [CrossRef]
- Xiao, X.; Huang, S.; Chen, S.; Wang, Y.; Sun, Q.; Xu, X.; Li, Y. Mechanisms of cytokine release syndrome and neurotoxicity of CAR T-cell therapy and associated prevention and management strategies. J. Exp. Clin. Cancer Res. 2021, 40, 367. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fajgenbaum, D.C.; June, C.H. Cytokine Storm. N. Engl. J. Med. 2020, 383, 2255–2273. [Google Scholar] [CrossRef]
- Neelapu, S.S. Managing the toxicities of CAR T-cell therapy. Hematol. Oncol. 2019, 37 (Suppl. S1), 48–52. [Google Scholar] [CrossRef]
- Yoo, J.W. Management of adverse events in young adults and children with acute B-cell lymphoblastic leukemia receiving anti-CD19 chimeric antigen receptor (CAR) T-cell therapy. Blood Res. 2023, 58 (Suppl. S1), S20–S28. [Google Scholar] [CrossRef]
- Graham, C.E.; Velasco, R.; Tomas, A.A.; Stewart, O.P.; Dachy, G.; del Bufalo, F.; Doglio, M.; Henter, J.-I.; Ortí, G.; Peric, Z.; et al. Non-ICANS neurological complications after CAR T-cell therapies: Recommendations from the EBMT Practice Harmonisation and Guidelines Committee. Lancet Oncol. 2025, 26, e203–e213. [Google Scholar] [CrossRef]
- Lee, D.W.; Santomasso, B.D.; Locke, F.L.; Ghobadi, A.; Turtle, C.J.; Brudno, J.N.; Maus, M.V.; Park, J.H.; Mead, E.; Pavletic, S.; et al. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol. Blood Marrow Transplant. 2019, 25, 625–638. [Google Scholar] [CrossRef]
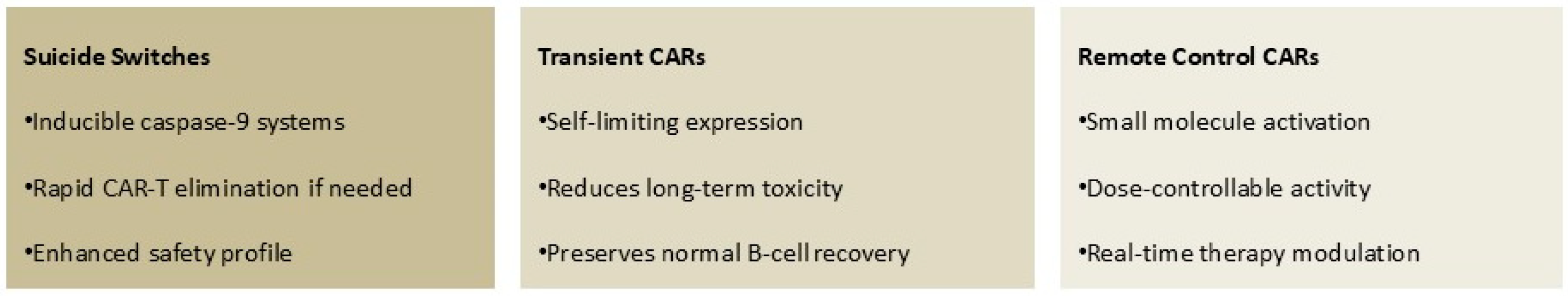
- Zugasti, I.; Espinosa-Aroca, L.; Fidyt, K.; Mulens-Arias, V.; Diaz-Beya, M.; Juan, M.; Urbano-Ispizua, Á.; Esteve, J.; Velasco-Hernandez, T.; Menéndez, P. CAR-T cell therapy for cancer: Current challenges and future directions. Signal Transduct. Target Ther. 2025, 10, 210. [Google Scholar] [CrossRef]
- Khan, S.H.; Choi, Y.; Veena, M.; Lee, J.K.; Shin, D.S. Advances in CAR T cell therapy: Antigen selection, modifications, and current trials for solid tumors. Front. Immunol. 2025, 15, 1489827. [Google Scholar] [CrossRef]
- Gryka-Marton, M.; Grabowska, A.D.; Szukiewicz, D. Breaking the Barrier: The Role of Proinflammatory Cytokines in BBB Dysfunction. Int. J. Mol. Sci. 2025, 26, 3532. [Google Scholar] [CrossRef]
- Stock, S.; Klüver, A.; Fertig, L.; Menkhoff, V.D.; Subklewe, M.; Endres, S.; Kobold, S. Mechanisms and strategies for safe chimeric antigen receptor T-cell activity control. Int. J. Cancer 2023, 153, 1706–1725. [Google Scholar] [CrossRef]
- Aparicio-Pérez, C.; Carmona, M.; Benabdellah, K.; Herrera, C. Failure of ALL recognition by CAR T cells: A review of CD 19-negative relapses after anti-CD 19 CAR-T treatment in B-ALL. Front. Immunol. 2023, 14, 1165870. [Google Scholar] [CrossRef] [PubMed]
- Zebley, C.C.; Brown, C.; Mi, T.; Fan, Y.; Alli, S.; Boi, S.; Galletti, G.; Lugli, E.; Langfitt, D.; Metais, J.-Y.; et al. CD19-CAR T cells undergo exhaustion DNA methylation programming in patients with acute lymphoblastic leukemia. Cell Rep. 2021, 37, 110079. [Google Scholar] [CrossRef] [PubMed]
- Ottaviano, G.; Georgiadis, C.; Gkazi, S.A.; Syed, F.; Zhan, H.; Etuk, A.; Preece, R.; Chu, J.; Kubat, A.; Adams, S.; et al. Phase 1 clinical trial of CRISPR-engineered CAR19 universal T cells for treatment of children with refractory B cell leukemia. Sci. Transl. Med. 2022, 14, eabq3010. [Google Scholar] [CrossRef] [PubMed]
- Siebart, J.C.; Chan, C.S.; Yao, X.; Su, F.-Y.; Kwong, G.A. In vivo gene delivery to immune cells. Curr. Opin. Biotechnol. 2024, 88, 103169. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, Q.; Sun, Z.; Chen, L. Memory T cells: Strategies for optimizing tumor immunotherapy. Protein Cell 2020, 11, 549–564. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baena, J.C.; Victoria, J.S.; Toro-Pedroza, A.; Aragón, C.C. Smart CAR-T Nanosymbionts: Archetypes and proto-models. Front. Immunol. 2025, 16, 1635159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Main Process Steps: |
|---|
|
| Key Molecular Details: |
|
| Clinical Context: |
|
| Agent | Costimulatory Molecule | CD19 Binding Domain | Indication |
|---|---|---|---|
| Tisagenlecleucel | 4-1BB | FMC63 (murine scFv) | Patients aged ≤25 years |
| Brexucabtageneautoleucel | CD28 | FMC63 (murine scFv) | Patients aged ≥25 years |
| Obecabtageneautoleucel | 4-1BB | CAT (fast off-rate scFv) | Patients aged ≥18 years |
| Author (Year) | Construct | Number of Patients | Age, Median, Range | Patients Who Responded and Proceeded to allo-SCT (% of Responders) | Median Time to allo-SCT Post CAR-T Infusion | TRM (%) | Main Results |
|---|---|---|---|---|---|---|---|
| Hay (2019 ) [40] | CD19.41BB | 53 | 39 (20–76) | 18/45 (40%) | 70 (44–138) | 23 | With a median follow-up of 28.4 months after allo-SCT, the 2-year EFS and OS were 61% and 72%, respectively. Allo-SCT was associated with longer EFS compared with no allo-SCT. |
| Park (2018) [41] | 19-28z CAR T | 53 | 44 (23–74) | 17/44 (39%) | 74 (44–312) | 35 | After allo-SCT, median OS is 12.9 months. Among patients with a low disease burden, the median OS was 20.1 months. |
| Jiang (2019) [42] | CD19.41BB | 58 | 28 (10–85) | 21/47 (45%) | 44 (33–89) | 10 | There was no difference in OS between MRD-CR patients who received allo-SCT and those who did not. However, EFS and RFS were significantly prolonged by allo-SCT in the subgroups. |
| Pan (2017) [43] | CD19 41BB | 51 | 27/45 (60%) | 84 (35–293) | 7.5 | Twenty-three of twenty-seven CR/CRi patients bridged to allo-SCT remained in MRD, with a median follow-up time of 206 (45–427) days. | |
| Shah (2023) [44] | CD19.CD28 | 78 | 42.5 (18–84) | 14/57 (25%) | 95 (60–390) | Not reported | Patients with subsequent allo-SCT experienced favorable long-term response durability, with a median DOR of 44.2 months. |
| Aldoss (2024) [45] | CD19.various | 45 | 31 (19–67) | 45/45 26 (58%) and 19 (42%) received their first and second allo-SCT as consolidation post CAR-T therapy | 93 (42–262) | 2.4 | With a median follow-up of 2.47 years (range: 0.13–6.93), 2-year OS, RFS, CIR, and NRM were 57.3%, 56.2%, 23.3%, and 20.4% respectively. Two-year OS, RFS, CIR, and NRM were not significantly different between patients who underwent their first vs. second transplant, respectively. |
| Roloff (2024) [46] | CD19.CD28 | 189 | 46 (18–81) | 30/151 (20%) | 99 (45–234) | 17 | In multivariable analysis, patients receiving consolidative allo-SCT (hazard ratio, 0.34 [95% CI, 0.14 to 0.85]) after CAR-T had superior PFS compared with those who did not receive any consolidation or maintenance therapy. |
| Shadman (2019) [47] | CD19.41BB | 19 | 39 (23–74) | 19/19 (100%) | 72 (28–138) | 21 | At a median follow-up of 36 month, 1-year estimate of OS was 58% (95% CI, 40–85). Longer time from CAR-T therapy to allo-SCT (≥80 vs. <80 days) was associated with higher risk for death (hazard ratio [HR], 4.01; 95% CI, 1.14–14.0; p = 0.03) and higher NRM (HR, 4.4; 95% CI, 0.54–21.1; p = 0.19). |
| Roddie (2024) [36] | CD19.41BB | 127 | 47 (20–81) | 18/99 (18%) | 101 (38–421) | Not reported | In 6 of 18 patients (33%), this procedure was a second allo-SCT. Of 11 patients who had persisting CAR T cells before allo-SCT and who had samples available afterward, none had CAR T cells detected after allo-SCT. No substantial difference in EFS or OS was observed between patients who received allo-SCT and those who did not. |
| Yang (2025) [48] | CD3ζ and 4-1BB | 32.1 (15–67) | 51 after achieving MRD-CR | 2.6 (1.8–4.1) | 6.7 | This study provides the most extensive follow-up of real-world data on sequential allo-SCT after CAR-T therapy. Sequential allo-SCT after CAR-T treatment shows durable remissions in patients achieving MRD-negative CR. With 4 years of follow-up, OS reaches 68.9%, highlighting the long-term benefits. Sequential therapy demonstrates manageable safety, with an acute GVHD incidence of 31.4% and no GVHD-related deaths. Age and high-risk genetic factors are key determinants of long-term outcomes, requiring personalized treatment strategies. |
| Characteristic | Autologous CAR T-Cells | Allogeneic CAR T-Cells |
|---|---|---|
| Donor origin | Patient | Healthy donor |
| Production and manufacturing | Complex logistics | Scaled-up industrialized process |
| Cost | Currently high | Expected to be moderate |
| Main risks | CRS; CAR-related gene modifications; potential long-term adverse effects, such as B-cell aplasia | CRS; CAR and/or gene-editing-related gene modifications; GvHD; allogeneic cell rejection |
| Persistence | Months to years | Weeks to months |
| Redosing | Limited by cell number | Limited by the risk of alloimmunization |
| Mechanism | Advantage | Status |
|---|---|---|
| Bicistronic or tandem CAR designs targeting both CD19 and CD22 | Reduces antigen escape, maintains efficacy against CD19-negative variants | Phase I/II trials showing promising results with improved durability |
| CRISPR/Cas9-engineered allogeneic T-cells with TCR/HLA knockout | Off-the-shelf availability, reduced manufacturing time to hours | Multiple platforms in clinical development (UCART19, CTX110) |
| CAR-T cells engineered to secrete supportive cytokines (IL-15, IL-12) | Enhanced persistence and activity in immunosuppressive environments | Preclinical development with first trials expected in 2026 |
| Boolean logic circuits requiring multiple antigens for activation | Improved specificity, reduced on-target off-tumor effects | Early preclinical development for enhanced safety |
| Current Patient Selection (2025) | Future Patient Selection (2027–2030) | 2030 Treatment Paradigm |
|---|---|---|
|
| First-Line Integration CAR-T therapy integrated into upfront treatment protocols for high-risk B-ALL patients, replacing intensive chemotherapy phases |
| Same-Day Treatment Universal CAR-T cells available immediately upon diagnosis, with personalized modifications made in real time | ||
| Minimal Toxicity Smart safety switches and controlled activation systems eliminate severe CRS and neurotoxicity | ||
| Durable Cures Self-renewing CAR-T cells provide lifelong surveillance and protection against relapse |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alati, C.; Pitea, M.; Molica, M.; Scalise, L.; Porto, G.; Bilardi, E.; Lazzaro, G.; Micò, M.C.; Pugliese, M.; Canale, F.A.; et al. CAR-T Cell Therapies in B-Cell Acute Lymphoblastic Leukemia: Emerging Data and Open Issues. Cancers 2025, 17, 3027. https://doi.org/10.3390/cancers17183027
Alati C, Pitea M, Molica M, Scalise L, Porto G, Bilardi E, Lazzaro G, Micò MC, Pugliese M, Canale FA, et al. CAR-T Cell Therapies in B-Cell Acute Lymphoblastic Leukemia: Emerging Data and Open Issues. Cancers. 2025; 17(18):3027. https://doi.org/10.3390/cancers17183027
Chicago/Turabian StyleAlati, Caterina, Martina Pitea, Matteo Molica, Luca Scalise, Gaetana Porto, Erica Bilardi, Giuseppe Lazzaro, Maria Caterina Micò, Marta Pugliese, Filippo Antonio Canale, and et al. 2025. "CAR-T Cell Therapies in B-Cell Acute Lymphoblastic Leukemia: Emerging Data and Open Issues" Cancers 17, no. 18: 3027. https://doi.org/10.3390/cancers17183027
APA StyleAlati, C., Pitea, M., Molica, M., Scalise, L., Porto, G., Bilardi, E., Lazzaro, G., Micò, M. C., Pugliese, M., Canale, F. A., Loteta, B., Naso, V., Policastro, G., Utano, G., Rizzuto, A., Marafioti, V., Rossi, M., & Martino, M. (2025). CAR-T Cell Therapies in B-Cell Acute Lymphoblastic Leukemia: Emerging Data and Open Issues. Cancers, 17(18), 3027. https://doi.org/10.3390/cancers17183027







