Real-World Effectiveness and Safety of Photoimmunotherapy for Head and Neck Cancer: A Multicenter Retrospective Study
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Outcomes and Assessments
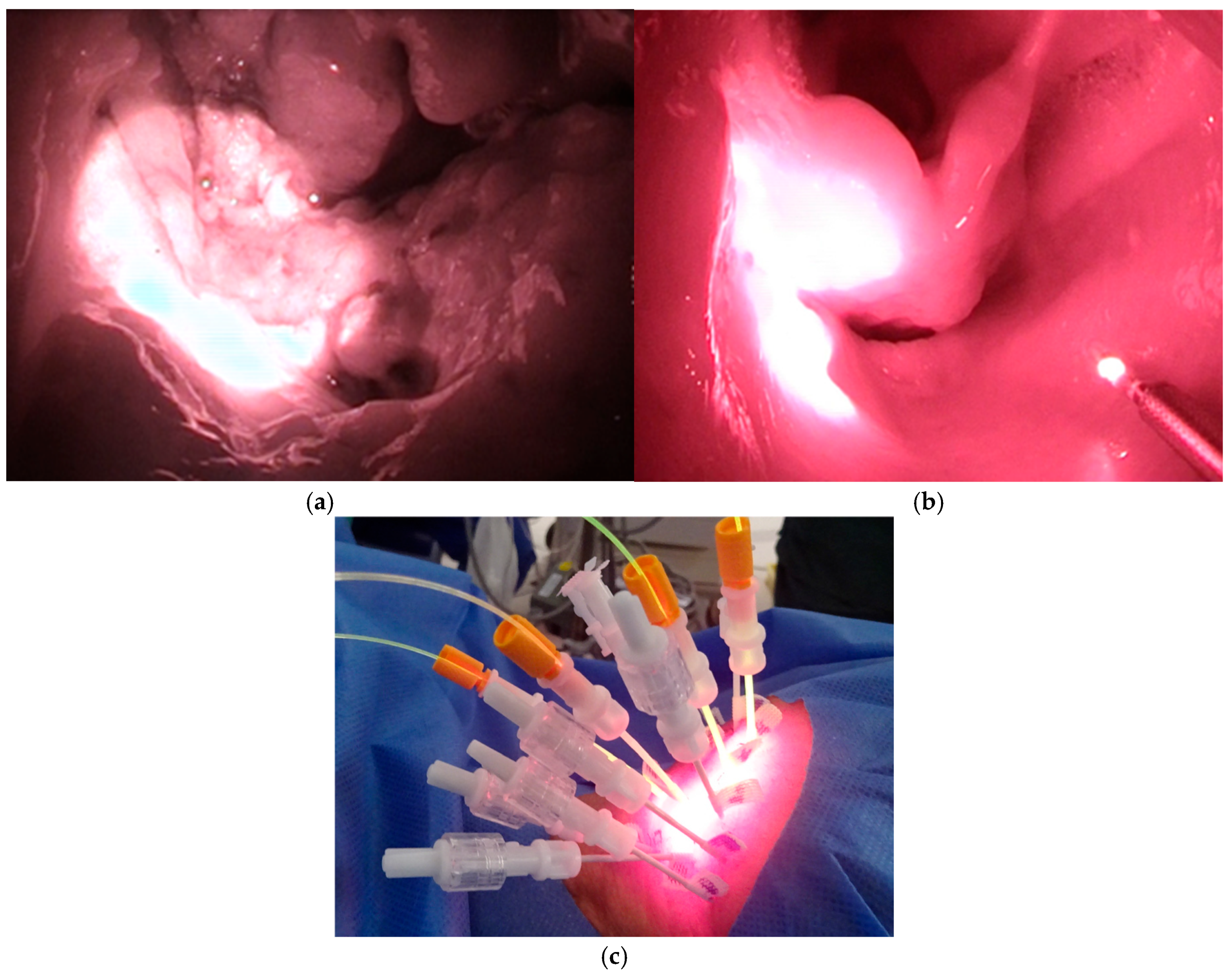
2.4. Photoimmunotherapy for Head and Neck Cancer
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Effectiveness
3.3. Safety
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AE | Adverse event |
| BOR | Best overall response |
| CI | Confidence interval |
| CR | Complete response |
| DCR | Disease control rate |
| EGFR | Epidermal growth factor receptor |
| HN-PIT | Photoimmunotherapy for head and neck cancer |
| ICI | Immune checkpoint inhibitor |
| LA/LR-HNC | Locally advanced or locally recurrent head and neck cancer |
| ORR | Objective response rate |
| OS | Overall survival |
| PD | Progressive disease |
| PD-1 | Programmed cell death protein 1 |
| PFS | Progression-free survival |
| PIT | Photoimmunotherapy |
| PR | Partial response |
| QOL | Quality of life |
| RECIST | Response Evaluation Criteria In Solid Tumors |
| R/M HNSCC | Recurrent or metastatic head and neck squamous cell carcinoma |
| RWD | Real-world data |
| SD | Stable disease |
| TTF | Time to treatment failure |
References
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Pulte, D.; Brenner, H. Changes in survival in head and neck cancers in the late 20th and early 21st century: A period analysis. Oncologist 2010, 15, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, S.; Zimmermann, A.; Wilhelm, T.; Werner, J.A. Survival after distant metastasis in head and neck cancer. Anticancer Res. 2015, 35, 5499–5502. [Google Scholar] [PubMed]
- Mitsunaga, M.; Ogawa, M.; Kosaka, N.; Rosenblum, L.T.; Choyke, P.L.; Kobayashi, H. Cancer cell-selective in vivo near infrared photoimmunotherapy targeting specific membrane molecules. Nat. Med. 2011, 17, 1685–1691. [Google Scholar] [CrossRef]
- Sato, K.; Ando, K.; Okuyama, S.; Moriguchi, S.; Ogura, T.; Totoki, S.; Hanaoka, H.; Nagaya, T.; Kokawa, R.; Takakura, H.; et al. Photoinduced ligand release from a silicon phthalocyanine dye conjugated with monoclonal antibodies: A mechanism of cancer cell cytotoxicity after near-infrared photoimmunotherapy. ACS Cent. Sci. 2018, 4, 1559–1569. [Google Scholar] [CrossRef]
- Hsu, M.A.; Okamura, S.M.; De Magalhaes Filho, C.D.; Bergeron, D.M.; Rodriguez, A.; West, M.; Yadav, D.; Heim, R.; Fong, J.J.; Garcia-Guzman, M. Cancer-targeted photoimmunotherapy induces antitumor immunity and can be augmented by anti-PD-1 therapy for durable anticancer responses in an immunologically active murine tumor model. Cancer Immunol. Immunother. 2023, 72, 151–168. [Google Scholar] [CrossRef]
- Nagaya, T.; Friedman, J.; Maruoka, Y.; Ogata, F.; Okuyama, S.; Clavijo, P.E.; Choyke, P.L.; Allen, C.; Kobayashi, H. Host immunity following near-infrared photoimmunotherapy is enhanced with PD-1 checkpoint blockade to eradicate established antigenic tumors. Cancer Immunol. Res. 2019, 7, 401–413. [Google Scholar] [CrossRef]
- Nakajima, K.; Takakura, H.; Shimizu, Y.; Ogawa, M. Changes in plasma membrane damage inducing cell death after treatment with near-infrared photoimmunotherapy. Cancer Sci. 2018, 109, 2889–2896. [Google Scholar] [CrossRef]
- Cognetti, D.M.; Johnson, J.M.; Curry, J.M.; Kochuparambil, S.T.; McDonald, D.; Mott, F.; Fidler, M.J.; Stenson, K.; Vasan, N.R.; Razaq, M.A.; et al. Phase 1/2a, open-label, multicenter study of RM-1929 photoimmunotherapy in patients with locoregional, recurrent head and neck squamous cell carcinoma. Head Neck 2021, 43, 3875–3887. [Google Scholar] [CrossRef]
- Tahara, M.; Okano, S.; Enokida, T.; Ueda, Y.; Fujisawa, T.; Shinozaki, T.; Tomioka, T.; Okano, W.; Biel, M.A.; Ishida, K.; et al. A phase I, single-center, open-label study of RM-1929 photoimmunotherapy in Japanese patients with recurrent head and neck squamous cell carcinoma. Int. J. Clin. Oncol. 2021, 26, 1812–1821. [Google Scholar] [CrossRef]
- Okamoto, I.; Okada, T.; Tokashiki, K.; Tsukahara, K. Quality-of-life evaluation of patients with unresectable locally advanced or locally recurrent head and neck carcinoma treated with head and neck photoimmunotherapy. Cancers 2022, 14, 4413. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, D.; Suzuki, H.; Beppu, S.; Terada, H.; Sawabe, M.; Hanai, N. Near-infrared photoimmunotherapy for oropharyngeal cancer. Cancers 2022, 14, 5662. [Google Scholar] [CrossRef] [PubMed]
- Hirakawa, H.; Ikegami, T.; Kinjyo, H.; Hayashi, Y.; Agena, S.; Higa, T.; Kondo, S.; Toyama, M.; Maeda, H.; Suzuki, M. Feasibility of near-infrared photoimmunotherapy combined with immune checkpoint inhibitor therapy in unresectable head and neck cancer. Anticancer Res. 2024, 44, 3907–3912. [Google Scholar] [CrossRef] [PubMed]
- Nishikawa, D.; Shimabukuro, T.; Suzuki, H.; Beppu, S.; Terada, H.; Kobayashi, Y.; Hanai, N. Predictive factors for the efficacy of head and neck photoimmunotherapy and optimization of treatment schedules. Cancer Diagn. Progn. 2025, 5, 179–188. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Brierley, J.D.; Gospodarowicz, M.K.; Wittekind, C. TNM Classification of Malignant Tumours, 8th ed.; Wiley-Blackwell: Oxford, UK, 2017. [Google Scholar]
- National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE) Version 5. 2017. Available online: https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50 (accessed on 4 February 2025).
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Omura, G.; Honma, Y.; Matsumoto, Y.; Shinozaki, T.; Itoyama, M.; Eguchi, K.; Sakai, T.; Yokoyama, K.; Watanabe, T.; Ohara, A.; et al. Transnasal photoimmunotherapy with cetuximab sarotalocan sodium: Outcomes on the local recurrence of nasopharyngeal squamous cell carcinoma. Auris Nasus Larynx 2023, 50, 641–645. [Google Scholar] [CrossRef]
- Koyama, S.; Ehara, H.; Donishi, R.; Taira, K.; Fukuhara, T.; Fujiwara, K. Therapeutic host anticancer immune response through photoimmunotherapy for head and neck cancer may overcome resistance to immune checkpoint inhibitors. Case Rep. Oncol. 2024, 17, 913–920. [Google Scholar] [CrossRef]
- Makino, T.; Sato, Y.; Uraguchi, K.; Naoi, Y.; Fukuda, Y.; Ando, M. Near-infrared photoimmunotherapy for salivary duct carcinoma. Auris Nasus Larynx 2024, 51, 323–327. [Google Scholar] [CrossRef]
- Shibutani, Y.; Sato, H.; Suzuki, S.; Shinozaki, T.; Kamata, H.; Sugisaki, K.; Kawanobe, A.; Uozumi, S.; Kawasaki, T.; Hayashi, R. A case series on pain accompanying photoimmunotherapy for head and neck cancer. Healthcare 2023, 11, 924. [Google Scholar] [CrossRef]
- Idogawa, H.; Shinozaki, T.; Okano, W.; Matsuura, K.; Hayashi, R. Nasopharyngeal carcinoma treated with photoimmunotherapy. Cureus 2023, 15, e49315. [Google Scholar] [CrossRef]
- Koyama, S.; Ehara, H.; Donishi, R.; Morisaki, T.; Ogura, T.; Taira, K.; Fukuhara, T.; Fujiwara, K. Photoimmunotherapy with surgical navigation and computed tomography guidance for recurrent maxillary sinus carcinoma. Auris Nasus Larynx 2023, 50, 646–651. [Google Scholar] [CrossRef]
- Kishikawa, T.; Terada, H.; Sawabe, M.; Beppu, S.; Nishikawa, D.; Suzuki, H.; Hanai, N. Utilization of ultrasound in photoimmunotherapy for head and neck cancer: A case report. J. Ultrasound 2025, 28, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Kano, S.; Suzuki, M.; Hamada, S.; Idogawa, H.; Tsushima, N.; Ashikaga, Y.; Wakabayashi, Y.; Soyama, T.; Hida, Y.; et al. SlicerPIT: Software development and implementation for planning and image-guided therapy in photoimmunotherapy. Int. J. Clin. Oncol. 2024, 29, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Okada, R.; Ito, T.; Kawabe, H.; Tsutsumi, T.; Asakage, T. Mixed reality-supported near-infrared photoimmunotherapy for oropharyngeal cancer: A case report. Ann Med. Surg. 2024, 86, 5551–5556. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network (NCCN). Clinical Practice Guidelines in Oncology, Head and Neck Cancers Version 2.2025. Available online: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck_blocks.pdf (accessed on 31 January 2025).
- Ferris, R.L.; Blumenschein, G., Jr.; Fayette, J.; Guigay, J.; Colevas, A.D.; Licitra, L.; Harrington, K.; Kasper, S.; Vokes, E.E.; Even, C.; et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 2016, 375, 1856–1867. [Google Scholar] [CrossRef]
- Burtness, B.; Harrington, K.J.; Greil, R.; Soulières, D.; Tahara, M.; de Castro, G., Jr.; Psyrri, A.; Basté, N.; Neupane, P.; Bratland, Å.; et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): A randomised, open-label, phase 3 study. Lancet 2019, 394, 1915–1928. [Google Scholar] [CrossRef]
- Okamoto, I. Photoimmunotherapy for head and neck cancer: A systematic review. Auris Nasus Larynx 2025, 52, 186–194. [Google Scholar] [CrossRef]
- Shinozaki, T.; Matsuura, K.; Okano, W.; Tomioka, T.; Nishiya, Y.; Machida, M.; Hayashi, R. Eligibility for photoimmunotherapy in patients with unresectable advanced or recurrent head and neck cancer and changes before and after systemic therapy. Cancers 2023, 15, 3795. [Google Scholar] [CrossRef]



| Characteristics | All Patients (n = 40) | |
|---|---|---|
| Number | % | |
| Age, years | ||
| Mean | 67 | |
| Median | 70 | |
| Range | 36–87 | |
| Sex | ||
| Male | 27 | 67.5 |
| Female | 13 | 32.5 |
| ECOG Performance Status | ||
| 0 | 32 | 80.0 |
| 1 | 7 | 17.5 |
| 2 | 1 | 2.5 |
| Primary tumor site | ||
| Oral cavity | 17 | 42.5 |
| Upper gingiva | 5 | 12.5 |
| Tongue | 4 | 10.0 |
| Lower gingiva | 3 | 7.5 |
| Floor of mouth | 2 | 5.0 |
| Buccal mucosa | 2 | 5.0 |
| Hard palate | 1 | 2.5 |
| Oropharynx | 7 | 17.5 |
| p16-positive | 3 | 7.5 |
| p16-negative | 4 | 10.0 |
| Nasopharynx | 5 | 12.5 |
| Hypopharynx | 3 | 7.5 |
| Larynx | 3 | 7.5 |
| Paranasal sinus | 3 | 7.5 |
| External auditory canal | 2 | 5.0 |
| Target lesion (with duplicates) | ||
| Oropharynx | 24 | |
| Anterior wall | 8 | |
| Lateral wall | 7 | |
| Posterior wall | 5 | |
| Superior wall | 4 | |
| Oral cavity | 16 | |
| Tongue | 5 | |
| Buccal mucosa | 3 | |
| Lower gingiva | 3 | |
| Hard palate | 2 | |
| Upper gingiva | 2 | |
| Floor of mouth | 1 | |
| Nasopharynx | 6 | |
| Cervical lymph node | 5 | |
| Maxillary sinus | 5 | |
| Nasal cavity | 2 | |
| External auditory canal | 2 | |
| Histology | ||
| Squamous cell carcinoma | 38 | 95.0 |
| Adenoid cystic carcinoma | 1 | 2.5 |
| Lymphoepithelial carcinoma | 1 | 2.5 |
| T category | ||
| 0 | 4 | 10.0 |
| 1 | 12 | 30.0 |
| 2 | 8 | 20.0 |
| 3 | 8 | 20.0 |
| 4 | 8 | 20.0 |
| N category | ||
| 0 | 35 | 87.5 |
| 1 | 1 | 2.5 |
| 2 | 0 | 0.0 |
| 3 | 4 | 10.0 |
| M category | ||
| 0 | 39 | 97.5 |
| 1 | 1 | 2.5 |
| History of surgery | ||
| Yes | 31 | 77.5 |
| No | 9 | 22.5 |
| History of neck dissection | ||
| Yes | 28 | 70.0 |
| No | 12 | 30.0 |
| History of radiotherapy | ||
| Yes | 38 | 95.0 |
| No | 2 | 5.0 |
| History of systemic therapy | ||
| Yes | 8 | 20.0 |
| No | 32 | 80.0 |
| Clinical Outcomes | Number | % |
|---|---|---|
| Objective response rate | 30 | 75.0 |
| Disease control rate | 38 | 95.0 |
| Complete response | 11 | 27.5 |
| Partial response | 19 | 47.5 |
| Stable disease | 8 | 20.0 |
| Progressive disease | 2 | 5.0 |
| Adverse Events | Patients, n (%) | |||||
|---|---|---|---|---|---|---|
| Grade | Grade | Grade | Grade | Grade | All | |
| I | II | III | IV | V | ||
| Pain | 7 (17.5) | 25 (62.5) | 5 (12.5) | 0 (0.0) | 0 (0.0) | 37 (92.5) |
| Mucositis | 14 (35.0) | 15 (37.5) | 3 (7.5) | 0 (0.0) | 0 (0.0) | 32 (80.0) |
| Hemorrhage | 24 (60.0) | 7 (17.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 31 (77.5) |
| Dysphagia | 8 (20.0) | 5 (12.5) | 6 (15.0) | 0 (0.0) | 0 (0.0) | 19 (47.5) |
| Laryngeal edema | 1 (2.5) | 12 (30.0) | 0 (0.0) | 4 (10.0) | 0 (0.0) | 17 (42.5) |
| Edema of the face | 10 (25.0) | 3 (7.5) | 5 (12.5) | 0 (0.0) | 0 (0.0) | 18 (45.0) |
| Fistula | 5 (12.5) | 4 (10.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 11 (27.5) |
| Sepsis | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) | 1 (2.5) | 2 (5.0) |
| Infusion reaction | 1 (2.5) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (5.0) |
| Facial nerve disorder | 0 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Lemierre’s syndrome | 0 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Pneumonitis | 0 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Liver dysfunction | 0 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Anemia | 0 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Acneiform rash | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Vertigo | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Fever | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Retained needle fragment | 0 (0.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Photosensitivity | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
| Nausea | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (2.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okamoto, I.; Hasegawa, O.; Kushihashi, Y.; Masubuchi, T.; Tokashiki, K.; Tsukahara, K. Real-World Effectiveness and Safety of Photoimmunotherapy for Head and Neck Cancer: A Multicenter Retrospective Study. Cancers 2025, 17, 2671. https://doi.org/10.3390/cancers17162671
Okamoto I, Hasegawa O, Kushihashi Y, Masubuchi T, Tokashiki K, Tsukahara K. Real-World Effectiveness and Safety of Photoimmunotherapy for Head and Neck Cancer: A Multicenter Retrospective Study. Cancers. 2025; 17(16):2671. https://doi.org/10.3390/cancers17162671
Chicago/Turabian StyleOkamoto, Isaku, On Hasegawa, Yukiomi Kushihashi, Tatsuo Masubuchi, Kunihiko Tokashiki, and Kiyoaki Tsukahara. 2025. "Real-World Effectiveness and Safety of Photoimmunotherapy for Head and Neck Cancer: A Multicenter Retrospective Study" Cancers 17, no. 16: 2671. https://doi.org/10.3390/cancers17162671
APA StyleOkamoto, I., Hasegawa, O., Kushihashi, Y., Masubuchi, T., Tokashiki, K., & Tsukahara, K. (2025). Real-World Effectiveness and Safety of Photoimmunotherapy for Head and Neck Cancer: A Multicenter Retrospective Study. Cancers, 17(16), 2671. https://doi.org/10.3390/cancers17162671






