Changes in Cancer Care for Patients Aged 80 and Above: A Cohort Study from Samsung Comprehensive Cancer Center in South Korea
Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Variables and Data Collection
2.3. Statistical Analysis
3. Results
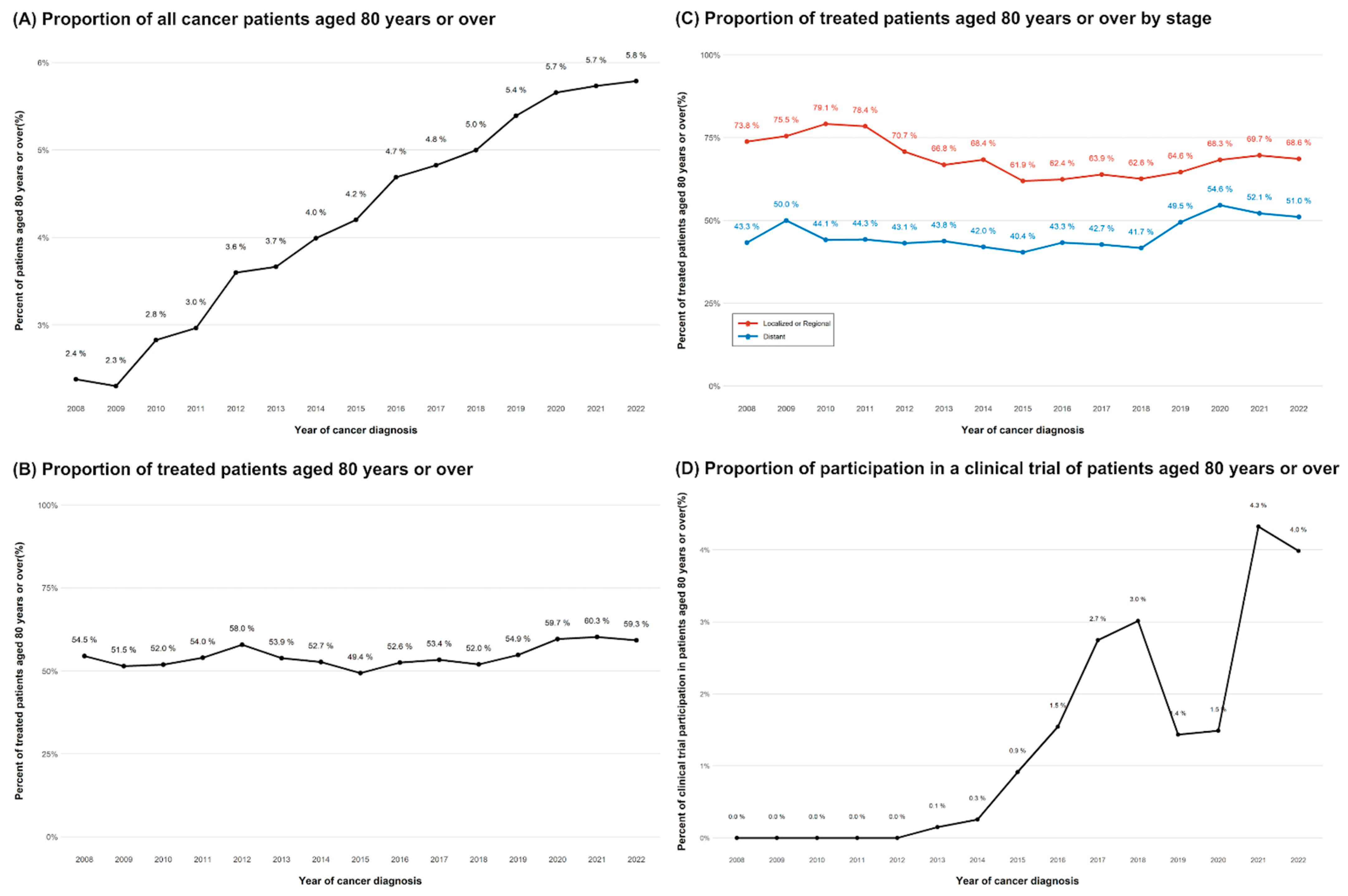
3.1. Trends in Elderly Patients and Characteristics
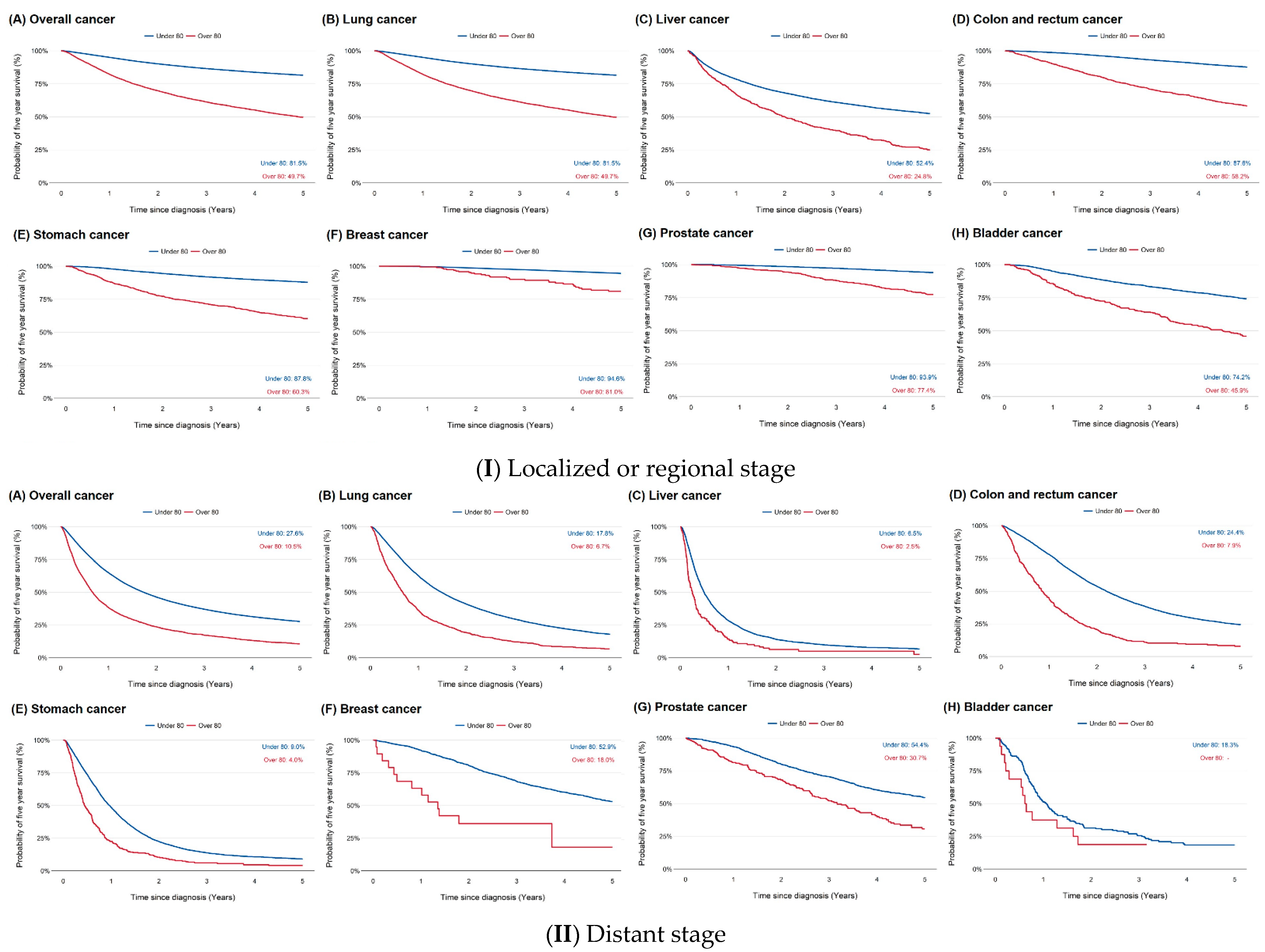
3.2. Survival Outcomes by Age and Stage
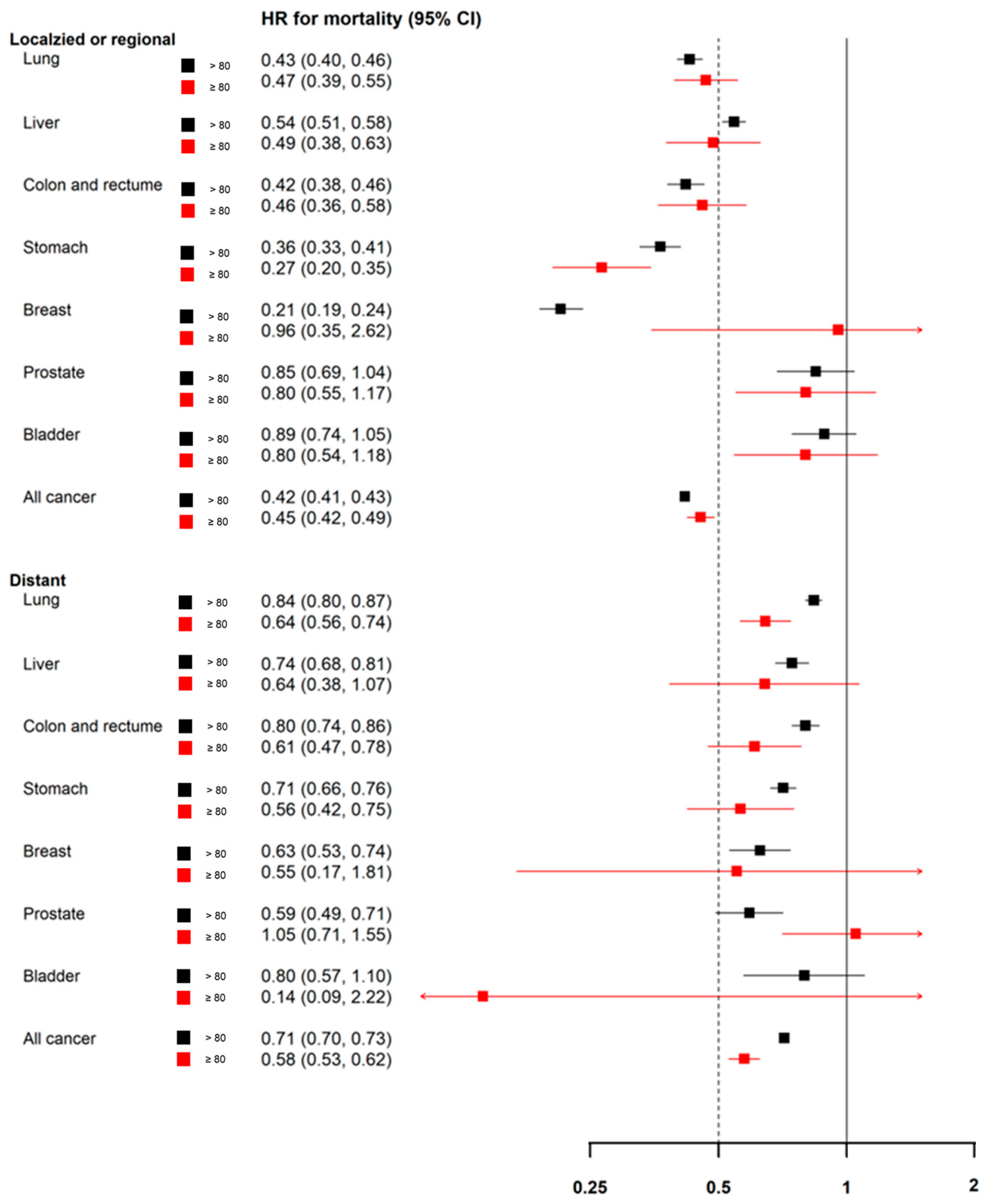
3.3. Effect of Treatment on Survival
4. Discussion
4.1. Perspectives for Clinical Practice
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- DeSantis, C.E.; Miller, K.D.; Dale, W.; Mohile, S.G.; Cohen, H.J.; Leach, C.R.; Goding Sauer, A.; Jemal, A.; Siegel, R.L. Cancer statistics for adults aged 85 years and older, 2019. CA Cancer J. Clin. 2019, 69, 452–467. [Google Scholar] [CrossRef] [PubMed]
- Van Herck, Y.; Feyaerts, A.; Alibhai, S.; Papamichael, D.; Decoster, L.; Lambrechts, Y.; Pinchuk, M.; Bechter, O.; Herrera-Caceres, J.; Bibeau, F.; et al. Is cancer biology different in older patients? Lancet Healthy Longev. 2021, 2, e663–e677. [Google Scholar] [CrossRef] [PubMed]
- Dale, W.; Klepin, H.D.; Williams, G.R.; Alibhai, S.M.H.; Bergerot, C.; Brintzenhofeszoc, K.; Hopkins, J.O.; Jhawer, M.P.; Katheria, V.; Loh, K.P.; et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Systemic Cancer Therapy: ASCO Guideline Update. J. Clin. Oncol. 2023, 41, 4293–4312. [Google Scholar] [CrossRef] [PubMed]
- Craigs, C.L.; Bennett, M.I.; Hurlow, A.; West, R.M.; Ziegler, L.E. Older age is associated with less cancer treatment: A longitudinal study of English cancer patients. Age Ageing 2018, 47, 833–840. [Google Scholar] [CrossRef]
- Smith, D.R.; Formenti, S.C. Treatment deescalation for older women with favorable breast cancers: Patient values and shared decision making. JNCI J. Natl. Cancer Inst. 2025, 117, 1096–1100. [Google Scholar] [CrossRef]
- Marino, P.; Mininni, M.; Deiana, G.; Marino, G.; Divella, R.; Bochicchio, I.; Giuliano, A.; Lapadula, S.; Lettini, A.R.; Sanseverino, F. Healthy Lifestyle and Cancer Risk: Modifiable Risk Factors to Prevent Cancer. Nutrients 2024, 16, 800. [Google Scholar] [CrossRef]
- Lee, S.Y.; Hong, Y.K.; Ji, W.; Lee, J.C.; Choi, C.M. Active Treatment Improves Overall Survival in Extremely Older Non-Small Cell Lung Cancer Patients: A Multicenter Retrospective Cohort Study. Cancer Res. Treat. 2021, 53, 104–111. [Google Scholar] [CrossRef]
- Kim, C.M.; Lee, J.B.; Shin, S.J.; Ahn, J.B.; Lee, M.; Kim, H.S. The efficacy of immune checkpoint inhibitors in elderly patients: A meta-analysis and meta-regression. ESMO Open 2022, 7, 100577. [Google Scholar] [CrossRef]
- Zhou, H.; Cai, L.L.; Lin, Y.F.; Ma, J.J. Toxicity profile of camrelizumab-based immunotherapy in older adults with advanced cancer. Sci. Rep. 2024, 14, 18992. [Google Scholar] [CrossRef]
- Nebhan, C.A.; Cortellini, A.; Ma, W.; Ganta, T.; Song, H.; Ye, F.; Irlmeier, R.; Debnath, N.; Saeed, A.; Radford, M.; et al. Clinical Outcomes and Toxic Effects of Single-Agent Immune Checkpoint Inhibitors Among Patients Aged 80 Years or Older With Cancer: A Multicenter International Cohort Study. JAMA Oncol. 2021, 7, 1856–1861. [Google Scholar] [CrossRef]
- Presley, C.J.; Krok-Schoen, J.L.; Wall, S.A.; Noonan, A.M.; Jones, D.C.; Folefac, E.; Williams, N.; Overcash, J.; Rosko, A.E. Implementing a multidisciplinary approach for older adults with Cancer: Geriatric oncology in practice. BMC Geriatr. 2020, 20, 231. [Google Scholar] [CrossRef]
- Jayawardhana, T.; Anuththara, S.; Nimnadi, T.; Karadanaarachchi, R.; Jayathilaka, R.; Galappaththi, K. Asian ageing: The relationship between the elderly population and economic growth in the Asian context. PLoS ONE 2023, 18, e0284895. [Google Scholar] [CrossRef]
- Jung, K.Y.; Kim, T.; Jung, J.; Lee, J.; Choi, J.S.; Mira, K.; Chang, D.K.; Cha, W.C. The Effectiveness of Near-Field Communication Integrated with a Mobile Electronic Medical Record System: Emergency Department Simulation Study. JMIR Mhealth Uhealth 2018, 6, e11187. [Google Scholar] [CrossRef]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Pineros, M. Global Cancer Observatory: Cancer Today–Data and Methods; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Park, E.H.; Jung, K.W.; Park, N.J.; Kang, M.J.; Yun, E.H.; Kim, H.J.; Kim, J.E.; Kong, H.J.; Im, J.S.; Seo, H.G. Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2021. Cancer Res. Treat. 2024, 56, 357–371. [Google Scholar] [CrossRef]
- Pilleron, S.; Soto-Perez-de-Celis, E.; Vignat, J.; Ferlay, J.; Soerjomataram, I.; Bray, F.; Sarfati, D. Estimated global cancer incidence in the oldest adults in 2018 and projections to 2050. Int. J. Cancer 2021, 148, 601–608. [Google Scholar] [CrossRef]
- Ju, W.; Zheng, R.; Zhang, S.; Zeng, H.; Sun, K.; Wang, S.; Chen, R.; Li, L.; Wei, W.; He, J. Cancer statistics in Chinese older people, 2022: Current burden, time trends, and comparisons with the US, Japan, and the Republic of Korea. Sci. China Life Sci. 2023, 66, 1079–1091. [Google Scholar] [CrossRef]
- Ito, K.; Kimura, T. Complex Epidemiology of Prostate Cancer in Asian Countries. Korean J. Urol. Oncol. 2023, 21, 5–13. [Google Scholar] [CrossRef]
- Cui, J.; Ding, R.; Liu, H.; Ma, M.; Zuo, R.; Liu, X. Trends in the incidence and survival of cancer in individuals aged 55 years and older in the United States, 1975–2019. BMC Public. Health 2024, 24, 72. [Google Scholar] [CrossRef]
- Jones, C.H.; Dolsten, M. Author Correction: Healthcare on the brink: Navigating the challenges of an aging society in the United States. NPJ Aging 2024, 10, 25. [Google Scholar] [CrossRef]
- Dharmarajan, K.V.; Presley, C.J.; Wyld, L. Care Disparities Across the Health Care Continuum for Older Adults: Lessons From Multidisciplinary Perspectives. Am. Soc. Clin. Oncol. Educ. Book 2021, 41, 1–10. [Google Scholar] [CrossRef]
- Panitsas, F.; Kothari, J.; Vallance, G.; Djebbari, F.; Ferguson, L.; Sultanova, M.; Ramasamy, K. Treat or palliate: Outcomes of very elderly myeloma patients. Haematologica 2018, 103, e32–e34. [Google Scholar] [CrossRef]
- Sobhi, S.; Wormald, R.; Hollitt, S.; Flukes, S. Survival and prognosis of surgical head and neck cancer patients aged 80 years and older. Laryngoscope Investig. Otolaryngol. 2023, 8, 659–666. [Google Scholar] [CrossRef]
- Benderra, M.A.; Serrano, A.G.; Paillaud, E.; Tapia, C.M.; Cudennec, T.; Chouaïd, C.; Lorisson, E.; de la Taille, A.; Laurent, M.; Brain, E.; et al. Prognostic value of comorbidities in older patients with cancer: The ELCAPA cohort study. ESMO Open 2023, 8, 101831. [Google Scholar] [CrossRef]
- Hu, J.; Lan, J.; Xu, G. Role of frailty in predicting prognosis of older patients with lung cancer: An updated systematic review and meta-analysis. J. Geriatr. Oncol. 2024, 15, 101804. [Google Scholar] [CrossRef]

| Characteristics | <80 | ≥80 | p Value |
|---|---|---|---|
| N = 287,944 | N = 13,111 | ||
| Age at diagnosis (years), mean (SD) | 56.6 (13.6) | 83.1 (3.1) | <0.01 |
| Gender, male | 151,661 (52.7%) | 7918 (60.4%) | <0.01 |
| Body mass index (kg/m2) | |||
| Underweight (≤18.5 kg/m2) | 11,726 (4%) | 868 (6%) | |
| Normal (18.5–23 kg/m2) | 96,323 (33.5%) | 4297 (32.8%) | |
| Overweight (23–25 kg/m2) | 60,939 (21.2%) | 2541 (19.4%) | |
| Obese (>25 kg/m2) | 82,480 (28.6%) | 2825 (21.5%) | |
| Unknown | 36,476 (12.7) | 2580 (19.7) | |
| Residence area | <0.01 | ||
| Seoul | 56,444 (19.6%) | 3671 (28.0%) | |
| Others | 221,543 (76.9%) | 8926 (68.1%) | |
| Unknown | 9957 (3.5%) | 514 (3.9%) | |
| Marital status at diagnosis, married | <0.01 | ||
| Uncoupled (unmarred, separated, widowed) | 31,171 (10.8%) | 2097 (16.0%) | |
| Coupled | 193,356 (67.2%) | 6865 (52.4%) | |
| Unknown | 63,417 (22.0%) | 4149 (31.6%) | |
| Working status at diagnosis | <0.01 | ||
| No work | 187,078 (65.0) | 11,389 (86.9%) | |
| White color | 60,708 (21.1%) | 590 (4.5%) | |
| Blue color | 22,755 (7.9%) | 831 (6.3%) | |
| Service | 4468 (1.6%) | 34 (0%) | |
| Others | 795 (0%) | 21 (0%) | |
| Unknown | 12,140 (4.2%) | 246 (2%) | |
| Diagnosis path (2013–) | <0.01 | ||
| Detected from Health screening | 102,627 (35.6%) | 4023 (30.7%) | |
| Incidentally diagnosed cancer | 7304 (2.5%) | 619 (4.7%) | |
| Detected due to symptoms | 75,875 (26.4%) | 5152 (39.3%) | |
| Unknown | 19,880 (6.9%) | 950 (7.2%) | |
| Type of cancer | <0.01 | ||
| Lip, oral cavity and pharynx | 5262 (1.8%) | 199 (1.5%) | |
| Esophagus | 5897 (2.0%) | 297 (2.3%) | |
| Stomach | 37,580 (13.1%) | 2011 (15.3%) | |
| Colon and rectum | 29,729 (10.3%) | 1813 (13.8%) | |
| Liver | 22,083 (7.7%) | 798 (6.1%) | |
| Gallbladder, etc. | 5817 (2.0%) | 628 (4.8%) | |
| Pancreas | 7797 (2.7%) | 640 (4.9%) | |
| Larynx | 1093 (0.4%) | 77 (0.6%) | |
| Lung | 38,308 (13.3%) | 2483 (18.9%) | |
| Breast | 32,916 (11.4%) | 244 (1.9%) | |
| Cervix uteri | 4517 (1.6%) | 108 (0.8%) | |
| Corpus uteri | 3713 (1.3%) | 48 (0.4%) | |
| Ovary | 4097 (1.4%) | 66 (0.5%) | |
| Prostate | 14,045 (4.9%) | 1056 (8.1%) | |
| Testis | 414 (0.0%) | 1 (0.0%) | |
| Kidney | 7951 (2.8%) | 217 (1.7%) | |
| Bladder | 3489 (1.2%) | 428 (3.3%) | |
| Brain and central nervous system (CNS) | 4226 (1.5%) | 121 (0.9%) | |
| Thyroid | 28,397 (9.9%) | 131 (1.0%) | |
| Hodgkin lymphoma | 530 (0.2%) | 7 (0.1%) | |
| Non-Hodgkin lymphoma | 7477 (2.6%) | 325 (2.5%) | |
| Multiple myeloma | 1799 (0.6%) | 104 (0.8%) | |
| Leukemia | 2979 (1.0%) | 85 (0.6%) | |
| Other and unspecified | 17,828 (6.2%) | 1224 (9.3%) | |
| SEER stage | <0.01 | ||
| Localized | 113,145 (39.3%) | 4169 (31.8%) | |
| Regional | 94,987 (33%) | 4199 (32.0%) | |
| Distant | 53,587 (18.6%) | 3154 (24.1%) | |
| Unknown | 26,225 (9.1%) | 1589 (12.1%) | |
| Diagnosis and treatment | <0.01 | ||
| SMC diagnosis, first treatment at SMC | 81,571 (28.3%) | 4032 (30.8%) | |
| Diagnosis elsewhere, first treatment at SMC | 115,692 (40.2%) | 3289 (25.1%) | |
| SMC diagnosis, first treatment elsewhere | 397 (0.1%) | 22 (0.2%) | |
| Diagnosis and first treatment elsewhere | 48,591 (16.9%) | 1751 (13.4%) | |
| SMC diagnosis only | 41,693 (14.5%) | 4017 (30.6%) | |
| Treatment within 4 months (N = 203,181) | |||
| Surgery | 141,272 (72.1%) | 4247 (58.6%) | <0.01 |
| Chemotherapy (cytotoxic, targeted, immunotherapy) | 79,746 (40.7%) | 1850 (25.5%) | <0.01 |
| Radiotherapy | 31,895 (16.3%) | 1238 (17.1%) | 0.07 |
| Hormone therapy | 13,421 (6.8%) | 513 (7.1%) | 0.46 |
| Biochemical therapy | 3245 (1.7%) | 164 (2.3%) | <0.01 |
| Others | 12,203 (6.2%) | 553 (7.6%) | <0.01 |
| <80 | ≥80 | <80 vs. ≥80 HR (95% CI) | |
|---|---|---|---|
| Overall | |||
| Any stages | |||
| All cancer | 70.39 (70.22%, 70.57%) | 38.42 (37.53%, 39.53%) | 1.30 (1.26, 1.33) |
| Lung cancer | 47.03 (46.50%, 47.56%) | 24.07 (22.28%, 26.01%) | 1.22 (1.15, 1.29) |
| Liver cancer | 45.36 (44.68%, 46.04%) | 22.20 (19.25%, 25.60%) | 1.63 (1.48, 1.79) |
| Colon and rectum cancer | 73.68 (73.15%, 74.21%) | 45.81 (43.42%, 48.34%) | 2.07 (1.90, 2.26) |
| Stomach cancer | 76.59 (76.15%, 77.03%) | 47.53 (45.26%, 49.91%) | 1.92 (1.77, 2.08) |
| Breast cancer | 92.03 (91.72%, 92.35%) | 73.61 (67.71%, 80.03%) | 3.23 (2.40, 4.36) |
| Prostate cancer | 89.27 (88.71%, 89.84%) | 65.51 (62.28%, 68.91%) | 1.56 (1.32, 1.85) |
| Bladder cancer | 71.33 (69.76%, 72.96%) | 46.32 (41.46%, 51.76%) | 1.35 (1.11, 1.64) |
| Localized or Regional | |||
| All cancer | 81.46 (81.28%, 81.63%) | 49.66 (48.50%, 50.85%) | 1.41 (1.35, 1.46) |
| Lung cancer | 68.55 (67.89%, 69.22%) | 38.65 (35.72%, 41.81%) | 1.31 (1.20, 1.44) |
| Liver cancer | 52.40 (51.61%, 53.20%) | 24.77 (21.11%, 29.07%) | 1.61 (1.44, 1.80) |
| Colon and rectum cancer | 87.64 (87.17%, 88.11%) | 58.22 (55.37%, 61.22%) | 2.10 (1.85, 2.38) |
| Stomach cancer | 87.81 (87.43%, 88.20%) | 60.34 (57.61%, 63.20%) | 1.76 (1.56, 1.98) |
| Breast cancer | 94.58 (94.30%, 94.87%) | 80.98 (74.94%, 87.50%) | 2.90 (1.94, 4.34) |
| Prostate cancer | 93.93 (93.44%, 94.42%) | 77.37 (73.86%, 81.06%) | 1.24 (0.96, 1.60) |
| Bladder cancer | 74.20 (72.55%, 75.90%) | 45.91 (40.65%, 51.86%) | 1.31 (1.06, 1.63) |
| Distant | |||
| All cancer | 27.61 (27.21%, 28.02%) | 10.53 (9.34%, 11.87%) | 1.14 (1.10, 1.19) |
| Lung cancer | 17.82 (17.16%, 18.50%) | 6.66 (5.08%, 8.74%) | 1.17 (1.08, 1.26) |
| Liver cancer | 6.50 (5.59%, 7.57%) | 2.47 (0.49%, 12.49%) | 1.61 (1.31, 1.97) |
| Colon and rectum cancer | 24.41 (23.28%, 25.61%) | 7.90 (5.34%, 11.69%) | 1.83 (1.61, 2.08) |
| Stomach cancer | 9.04 (8.19%, 9.97%) | 4.00 (2.11%, 7.57%) | 1.62 (1.40, 1.87) |
| Breast cancer | 52.94 (50.38%, 55.63%) | 18.05 (3.97%, 81.96%) | 2.94 (1.61, 5.36) |
| Prostate cancer | 54.42 (51.64%, 57.34%) | 30.73 (24.11%, 39.16%) | 1.61 (1.26, 2.07) |
| Bladder cancer | 18.30 (13.07%, 25.64%) | - | 1.36 (0.68, 2.71) |
| Treated | |||
| Any stages | |||
| All cancer | 76.54 (76.34%, 76.73%) | 48.53 (47.27%, 49.81%) | 1.22 (1.17, 1.27) |
| Lung cancer | 54.35 (53.72%, 54.97%) | 32.14 (29.43%, 35.09%) | 1.14 (1.05, 1.24) |
| Liver cancer | 56.09 (55.21%, 56.99%) | 30.99 (26.11%, 36.79%) | 1.61 (1.40, 1.86) |
| Colon and rectum cancer | 79.76 (79.17%, 80.35%) | 58.20 (55.21%, 61.36%) | 2.09 (1.85, 2.35) |
| Stomach cancer | 83.44 (82.99%, 83.88%) | 65.67 (62.71%, 68.78%) | 1.82 (1.60, 2.07) |
| Breast cancer | 94.82 (94.63%, 95.21%) | 78.54 (71.85%, 85.86%) | 2.89 (1.91, 4.38) |
| Prostate cancer | 91.59 (90.96%, 92.22%) | 66.78 (62.31%, 71.56%) | 1.75 (1.37, 2.22) |
| Bladder cancer | 74.20 (72.05%, 76.41%) | 50.67 (43.90%, 58.48%) | 1.19 (0.89, 1.59) |
| Localized or Regional | |||
| All cancer | 85.62 (85.44%, 85.88%) | 57.36 (55.95%, 58.81%) | 1.38 (1.31, 1.46) |
| Lung cancer | 73.89 (73.19%, 74.59%) | 47.20 (43.40%, 51.34%) | 1.27 (1.12, 1.44) |
| Liver cancer | 62.36 (61.43%, 63.30%) | 33.29 (28.05%, 39.52%) | 1.62 (1.38, 1.89) |
| Colon and rectum cancer | 90.60 (90.12%, 91.08%) | 65.57 (62.42%, 68.88%) | 2.03 (1.72, 2.39) |
| Stomach cancer | 90.71 (90.34%, 91.08%) | 71.43 (68.42%, 74.58%) | 1.64 (1.40, 1.92) |
| Breast cancer | 96.58 (96.34%, 96.83%) | 81.79 (75.17%, 88.99%) | 3.32 (2.06, 5.36) |
| Prostate cancer | 94.66 (94.11%, 95.20%) | 77.08 (72.43%, 82.03%) | 1.27 (0.91, 1.78) |
| Bladder cancer | 76.99 (74.84%, 79.20%) | 50.59 (43.69%, 58.58%) | 1.14 (0.84, 1.54) |
| Distant | |||
| All cancer | 31.73 (31.19%, 32.28%) | 14.99 (12.93%, 17.36%) | 1.01 (0.95, 1.08) |
| Lung cancer | 19.92 (19.07%, 20.81%) | 8.71 (6.19%, 12.25%) | 1.08 (0.97, 1.20) |
| Liver cancer | 8.42 (6.99%, 10.14%) | 7.06 (1.39%, 35.84%) | 1.43 (0.98, 2.10) |
| Colon and rectum cancer | 29.06 (27.47%, 30.73%) | 12.82 (8.10%, 20.29%) | 1.65 (1.35, 2.01) |
| Stomach cancer | 10.44 (9.21%, 11.83%) | 7.97 (3.81%, 16.67%) | 1.59 (1.25, 2.00 |
| Breast cancer | 59.00 (59.95%, 62.22%) | - | 2.07 (0.81, 5.31) |
| Prostate cancer | 60.02 (56.27%, 64.02%) | 31.68 (23.05%, 43.55%) | 2.00 (1.42, 2.81) |
| Bladder cancer | 19.38 (12.21%, 30.76%) | - | 1.45 (0.53, 3.99) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.T.; Kang, D.; Kim, S.J.; Lee, J.H.; Kim, H.K.; Cho, Y.B.; Paik, Y.H.; Kim, S.W.; Jeong, B.C.; Seol, H.J.; et al. Changes in Cancer Care for Patients Aged 80 and Above: A Cohort Study from Samsung Comprehensive Cancer Center in South Korea. Cancers 2025, 17, 2017. https://doi.org/10.3390/cancers17122017
Kim ST, Kang D, Kim SJ, Lee JH, Kim HK, Cho YB, Paik YH, Kim SW, Jeong BC, Seol HJ, et al. Changes in Cancer Care for Patients Aged 80 and Above: A Cohort Study from Samsung Comprehensive Cancer Center in South Korea. Cancers. 2025; 17(12):2017. https://doi.org/10.3390/cancers17122017
Chicago/Turabian StyleKim, Seung Tae, Danbee Kang, Seok Jin Kim, Jun Ho Lee, Hong Kwan Kim, Yong Beom Cho, Yong Han Paik, Seok Won Kim, Byong Chang Jeong, Ho Jun Seol, and et al. 2025. "Changes in Cancer Care for Patients Aged 80 and Above: A Cohort Study from Samsung Comprehensive Cancer Center in South Korea" Cancers 17, no. 12: 2017. https://doi.org/10.3390/cancers17122017
APA StyleKim, S. T., Kang, D., Kim, S. J., Lee, J. H., Kim, H. K., Cho, Y. B., Paik, Y. H., Kim, S. W., Jeong, B. C., Seol, H. J., Chung, M. K., Lee, K. T., Kim, K., Seo, S.-w., Lee, J.-W., Park, H. C., Shin, D. W., Cho, J., Kim, W., ... Lee, W. Y. (2025). Changes in Cancer Care for Patients Aged 80 and Above: A Cohort Study from Samsung Comprehensive Cancer Center in South Korea. Cancers, 17(12), 2017. https://doi.org/10.3390/cancers17122017






