Patterns and Incidence of Pneumonitis and Initial Treatment Outcomes with Durvalumab Consolidation Therapy after Radical Chemoradiotherapy for Stage III Non-Small Cell Lung Cancer
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Treatment
2.3. Endpoints
2.4. Statistical Analyses
3. Results
3.1. Patient Characteristics and Treatment
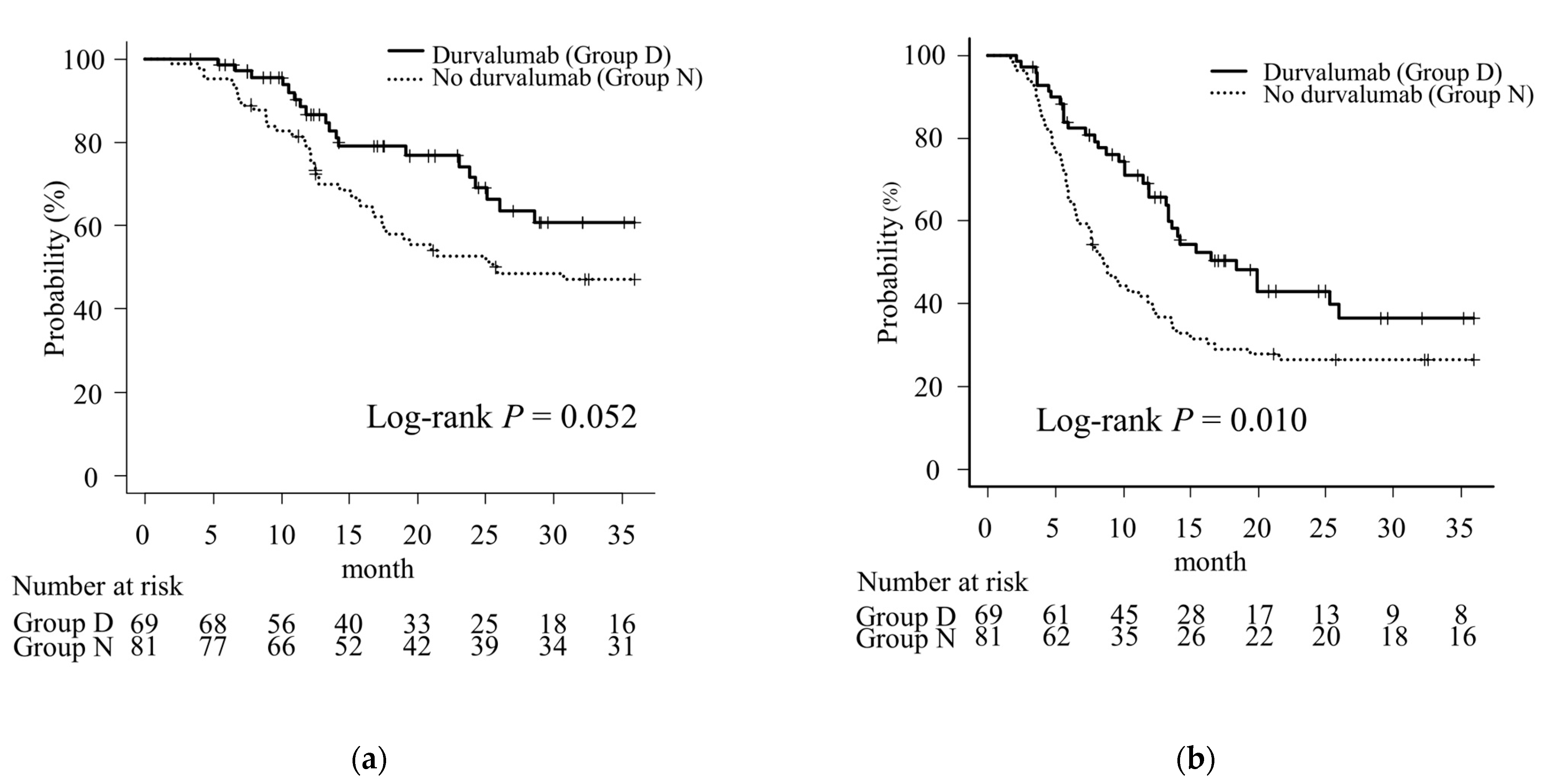
3.2. The OS and PFS
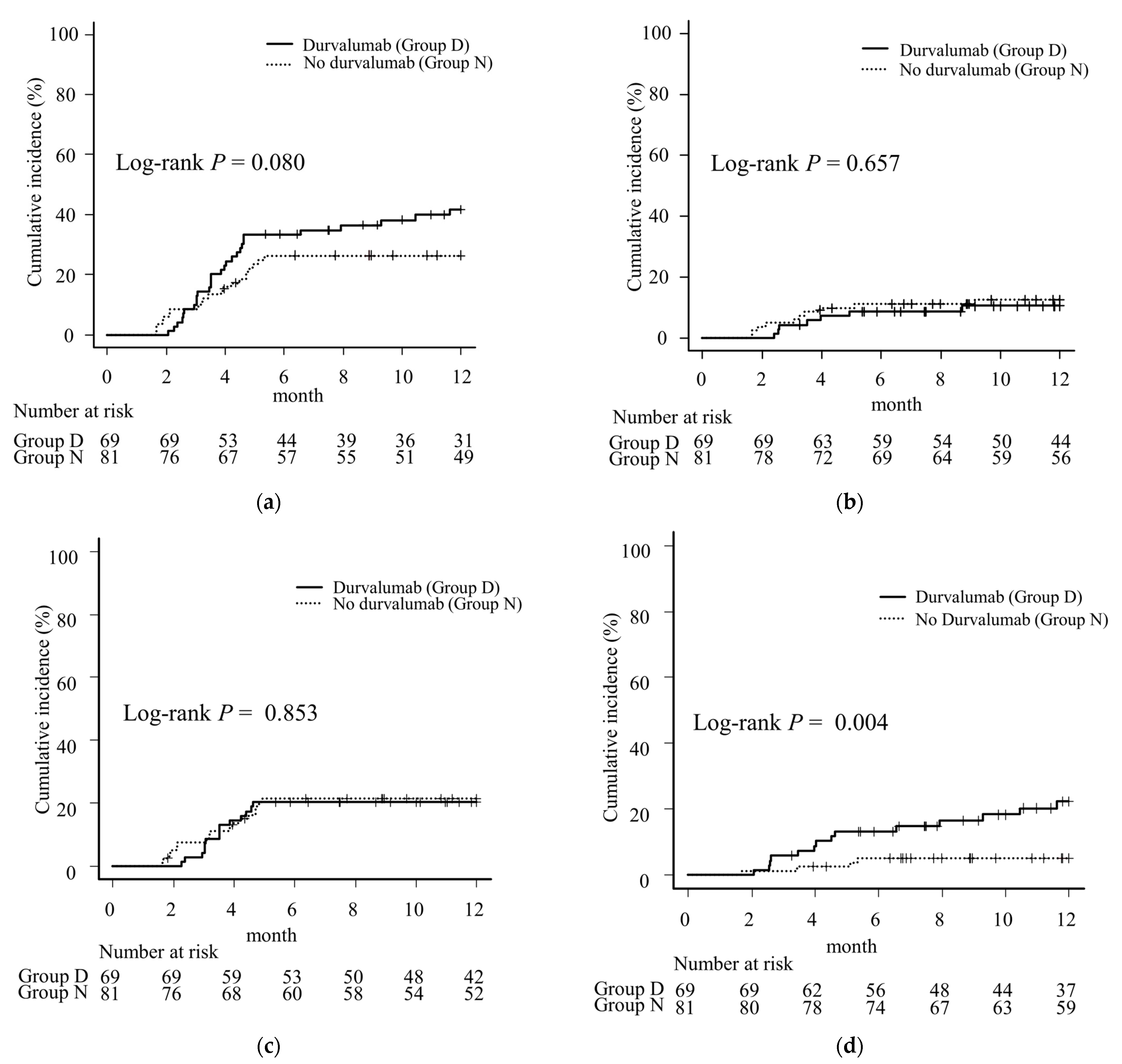
3.3. Incidence of Pneumonitis
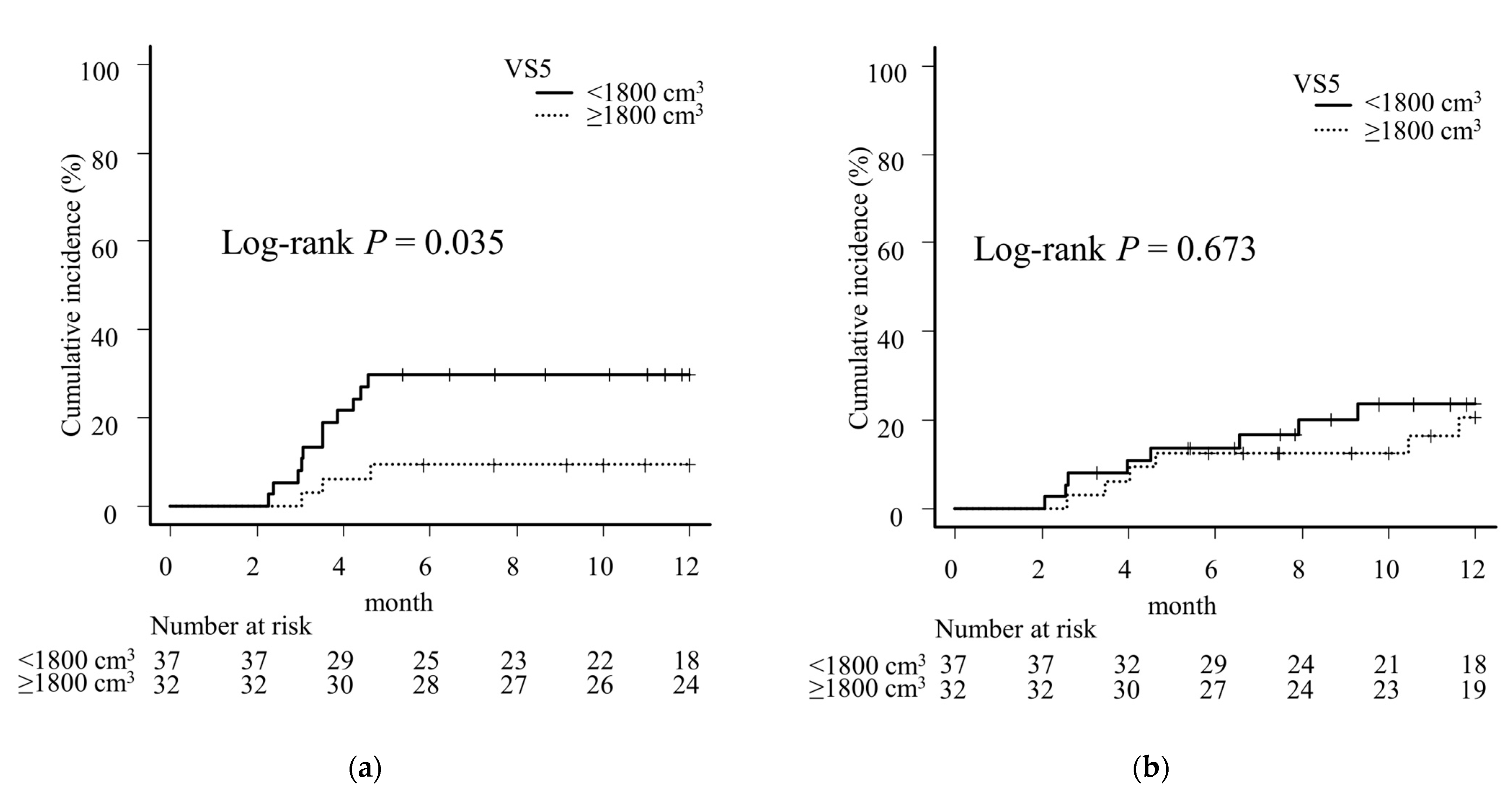
3.4. Univariate and Multivariate Analyses for Pneumonitis ≥ G2
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Curran, W.J., Jr.; Paulus, R.; Langer, C.J.; Komaki, R.; Lee, J.S.; Hauser, S.; Movsas, B.; Wasserman, T.; Rosenthal, S.A.; Gore, E.; et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: Randomized phase III trial RTOG 9410. J. Natl. Cancer Inst. 2011, 103, 1452–1460. [Google Scholar] [CrossRef] [PubMed]
- Bradley, J.D.; Hu, C.; Komaki, R.R.; Masters, G.A.; Blumenschein, G.R.; Schild, S.E.; Bogart, J.A.; Forster, K.M.; Magliocco, A.M.; Kavadi, V.S.; et al. Long-Term Results of NRG Oncology RTOG 0617: Standard- Versus High-Dose Chemoradiotherapy with or Without Cetuximab for Unresectable Stage III Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2019, 38, 706–714. [Google Scholar] [CrossRef]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; de Wit, M.; et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N. Engl. J. Med. 2017, 377, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Kurata, T.; Chiappori, A.; Lee, K.H.; de Wit, M.; et al. Overall survival with Durvalumab after chemoradiotherapy in stage III NSCLC. N. Engl. J. Med. 2018, 379, 2342–2350. [Google Scholar] [CrossRef] [PubMed]
- Spigel, D.R.; Faivre-Finn, C.; Gray, J.E.; Vicente, D.; Planchard, D.; Paz-Ares, L.; Vansteenkiste, J.F.; Garassino, M.C.; Hui, R.; Quantin, X.; et al. Five-year survival outcomes from the PACIFIC trial: Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. J. Clin. Oncol. 2022, 40, 1301–1311. [Google Scholar] [CrossRef]
- Girard, N.; Bar, J.; Garrido, P.; Garassino, M.C.; McDonald, F.; Mornex, F.; Filippi, A.R.; Smit, H.J.M.; Peters, S.; Field, J.K.; et al. Treatment Characteristics and Real-World Progression-Free Survival in Patients with Unresectable Stage III NSCLC Who Received Durvalumab After Chemoradiotherapy: Findings From the PACIFIC-R Study. J. Thorac. Oncol. 2023, 18, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.A.; Noh, J.M.; Sun, J.M.; Lee, S.H.; Ahn, J.S.; Ahn, M.J.; Pyo, H.; Ahn, Y.C.; Park, K. Real world data of durvalumab consolidation after chemoradiotherapy in stage III non-small-cell lung cancer. Lung Cancer 2020, 146, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Wu, L.; Gandhi, S.; Jing, W.; Nguyen, Q.; Chen, A.; Chang, J.Y.; Nurieva, R.; Sheshadri, A.; Altan, M.; et al. Treatment-related pulmonary adverse events induced by chemoradiation and durvalumab affect survival in locally advanced non-small cell lung cancer. Radiother. Oncol. 2022, 176, 149–156. [Google Scholar] [CrossRef]
- Yegya-Raman, N.; Friedes, C.; Lee, S.H.; Iocolano, M.; Duan, L.; Wang, X.; Li, B.; Aggarwal, C.; Cohen, R.B.; Su, W.; et al. Pneumonitis Rates Before and After Adoption of Immunotherapy Consolidation in Patients with Locally Advanced Non-Small Cell Lung Cancer Treated with Concurrent Chemoradiation. Int. J. Radiat. Oncol. Biol. Phys. 2023, 118, 1445–1454. [Google Scholar] [CrossRef]
- Tsujino, K.; Hirota, S.; Endo, M.; Obayashi, K.; Kotani, Y.; Satouchi, M.; Kado, T.; Takada, Y. Predictive value of dose-volume histogram parameters for predicting radiation pneumonitis after concurrent chemoradiation for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 110–115. [Google Scholar] [CrossRef]
- Marks, L.B.; Bentzen, S.M.; Deasy, J.O.; Kong, F.S.; Bradley, J.D.; Vogelius, I.S.; Naqa, I.E.; Hubbs, J.L.; Lebesque, J.V.; Timmerman, R.D.; et al. Radiation dose-volume effects in the lung. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, S70–S76. [Google Scholar] [CrossRef] [PubMed]
- Tatsuno, S.; Doi, H.; Okada, W.; Inoue, E.; Nakamatsu, K.; Tanooka, M.; Tanaka, M.; Nishimura, Y. Risk factors for radiation pneumonitis after rotating gantry intensity-modulated radiation therapy for lung cancer. Sci. Rep. 2022, 12, 590. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Hong, J.; Zou, X.; Lv, W.; Guo, F.; Hong, H.; Zhang, W. Association between absolute volumes of lung spared from low-dose irradiation and radiation-induced lung injury after intensity-modulated radiotherapy in lung cancer: A retrospective analysis. J. Radiat. Res. 2015, 56, 883–888. [Google Scholar] [CrossRef] [PubMed]
- Tsujino, K.; Hashimoto, T.; Shimada, T.; Yoden, E.; Fujii, O.; Ota, Y.; Satouchi, M.; Negoro, S.; Adachi, S.; Soejima, T. Combined analysis of V20, VS5, pulmonary fibrosis score on baseline computed tomography, and patient age improves prediction of severe radiation pneumonitis after concurrent chemoradiotherapy for locally advanced non-small-cell lung cancer. J. Thorac. Oncol. 2014, 9, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Chun, S.G.; Hu, C.; Choy, H.; Komaki, R.U.; Timmerman, R.D.; Schild, S.E.; Bogart, J.A.; Dobelbower, M.C.; Bosch, W.; Galvin, J.M.; et al. Impact of Intensity-Modulated Radiation Therapy Technique for Locally Advanced Non-Small-Cell Lung Cancer: A Secondary Analysis of the NRG Oncology RTOG 0617 Randomized Clinical Trial. J. Clin. Oncol. 2017, 35, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Kashihara, T.; Nakayama, Y.; Ito, K.; Kubo, Y.; Okuma, K.; Shima, S.; Nakamura, S.; Takahashi, K.; Inaba, K.; Murakami, N.; et al. Usefulness of Simple Original Interstitial Lung Abnormality Scores for Predicting Radiation Pneumonitis Requiring Steroidal Treatment After Definitive Radiation Therapy for Patients with Locally Advanced Non-Small Cell Lung Cancer. Adv. Radiat. Oncol. 2020, 6, 100606. [Google Scholar] [CrossRef] [PubMed]
- Mayahara, H.; Uehara, K.; Harada, A.; Kitatani, K.; Yabuuchi, T.; Miyazaki, S.; Ishihara, T.; Kawaguchi, H.; Kubota, H.; Okada, H.; et al. Predicting factors of symptomatic radiation pneumonitis induced by durvalumab following concurrent chemoradiotherapy in locally advanced non-small cell lung cancer. Radiat. Oncol. 2022, 17, 7. [Google Scholar] [CrossRef]
- Shaverdian, N.; Thor, M.; Shepherd, A.F.; Offin, M.D.; Jackson, A.; Wu, A.J.; Gelblum, D.Y.; Yorke, E.D.; Simone, C.B., 2nd; Chaft, J.E.; et al. Radiation pneumonitis in lung cancer patients treated with chemoradiation plus durvalumab. Cancer Med. 2020, 9, 4622–4631. [Google Scholar] [CrossRef]
- Kazerooni, E.A.; Martinez, F.J.; Flint, A.; Jamadar, D.A.; Gross, B.H.; Spizarny, D.L.; Cascade, P.N.; Whyte, R.I.; Lynch, J.P., 3rd; Toews, G. Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: Correlation with pathologic scoring. AJR Am. J. Roentgenol. 1997, 169, 977–983. [Google Scholar] [CrossRef]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Ohri, N.; Halmos, B.; Bodner, W.R.; Cheng, H.; Garg, M.K.; Gucalp, R.; Guha, C. Who benefits the most from adjuvant durvalumab after chemoradiotherapy for non-small cell lung cancer? An exploratory analysis. Pract. Radiat. Oncol. 2021, 11, e172–e179. [Google Scholar] [CrossRef]
- Kishi, N.; Matsuo, Y.; Shintani, T.; Ogura, M.; Mitsuyoshi, T.; Araki, N.; Fujii, K.; Okumura, S.; Nakamatsu, K.; Kishi, T.; et al. Recurrence patterns and progression-free survival after chemoradiotherapy with or without consolidation durvalumab for stage III non-small cell lung cancer. J. Radiat. Res. 2023, 64, 142–153. [Google Scholar] [CrossRef] [PubMed]
- Ghita, M.; Dunne, V.L.; McMahon, S.J.; Osman, S.O.; Small, D.M.; Weldon, S.; Taggart, C.C.; McGarry, C.K.; Hounsell, A.R.; Graves, E.E.; et al. Preclinical evaluation of dose-volume effects and lung toxicity occurring in and out-of-field. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 1231–1240. [Google Scholar] [CrossRef]
- Katayama, N.; Sato, S.; Katsui, K.; Takemoto, M.; Tsuda, T.; Yoshida, A.; Morito, T.; Nakagawa, T.; Mizuta, A.; Waki, T.; et al. Analysis of factors associated with radiation-induced bronchiolitis obliterans organizing pneumonia syndrome after breast-conserving therapy. Int. J. Radiat. Oncol. Biol. Phys. 2009, 73, 1049–1054. [Google Scholar] [CrossRef] [PubMed]
- Murofushi-Nemoto, K.; Oguchi, M.; Gosho, M.; Kozuka, T.; Sakurai, H. Radiation-induced bronchiolitis obliterans organizing pneumonia (BOOP) syndrome in breast cancer patients is associated with age. Radiat. Oncol. 2015, 10, 103. [Google Scholar] [CrossRef]
- Ogo, E.; Komaki, R.; Abe, T.; Uchida, M.; Fujimoto, K.; Suzuki, G.; Tsuji, C.; Suefuji, H.; Etou, H.; Hattori, C.; et al. The clinical characteristics and non-steroidal treatment for radiation-induced bronchiolitis obliterans organizing pneumonia syndrome after breast-conserving therapy. Radiother. Oncol. 2010, 97, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Ebi, J.; Tamaki, T.; Yukawa, A.; Nakajima, M.; Ohtake, T.; Suzuki, Y. Incidence of organizing pneumonia after whole-breast radiotherapy for breast cancer, and risk factor analysis. J. Radiat. Res. 2018, 59, 298–302. [Google Scholar] [CrossRef]
- Murai, T.; Shibamoto, Y.; Nishiyama, T.; Baba, F.; Miyakawa, A.; Ayakawa, S.; Ogino, H.; Otsuka, S.; Iwata, H. Organizing pneumonia after stereotactic ablative radiotherapy of the lung. Radiat. Oncol. 2012, 7, 123. [Google Scholar] [CrossRef]
- Ochiai, S.; Nomoto, Y.; Yamashita, Y.; Murashima, S.; Hasegawa, D.; Kurobe, Y.; Toyomasu, Y.; Kawamura, T.; Takada, A.; Ii, N. Radiation-induced organizing pneumonia after stereotactic body radiotherapy for lung tumor. J. Radiat. Res. 2015, 56, 904–911. [Google Scholar] [CrossRef]
- Shintani, T.; Kishi, N.; Matsuo, Y.; Ogura, M.; Mitsuyoshi, T.; Araki, N.; Fujii, K.; Okumura, S.; Nakamatsu, K.; Kishi, T.; et al. Incidence and Risk Factors of Symptomatic Radiation Pneumonitis in Non-Small-Cell Lung Cancer Patients Treated with Concurrent Chemoradiotherapy and Consolidation Durvalumab. Clin. Lung Cancer 2021, 22, 401–410. [Google Scholar] [CrossRef]
- Saito, G.; Oya, Y.; Taniguchi, Y.; Kawachi, H.; Daichi, F.; Matsumoto, H.; Iwasawa, S.; Suzuki, H.; Niitsu, T.; Miyauchi, E.; et al. Real-world survey of pneumonitis and its impact on durvalumab consolidation therapy in patients with non-small cell lung cancer who received chemoradiotherapy after durvalumab approval (HOPE-005/CRIMSON). Lung Cancer 2021, 161, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Masuo, M.; Shinohara, E.; Kitano, M.; Maruta, R.; Chonabayashi, S.; Endo, S.; Matumoto, S.; Nishiyama, N.; Machitori, Y.; Kobayashi, M. A comparison of the incidence of ≥grade 2 radiation pneumonitis between intensity-modulated radiotherapy and three-dimensional conformal radiotherapy in patients with unresectable non-small cell lung cancer treated with durvalumab after concurrent chemoradiotherapy. Jpn. J. Clin. Oncol. 2023, 54, hyad158. [Google Scholar] [CrossRef]
- Tsukita, Y.; Yamamoto, T.; Mayahara, H.; Hata, A.; Takeda, Y.; Nakayama, H.; Tanaka, S.; Uchida, J.; Usui, K.; Toyoda, T.; et al. Intensity-modulated radiation therapy with concurrent chemotherapy followed by durvalumab for stage III non-small cell lung cancer: A multi-center retrospective study. Radiother. Oncol. 2021, 160, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Inoue, H.; Ono, A.; Kawabata, T.; Mamesaya, N.; Kawamura, T.; Kobayashi, H.; Omori, S.; Wakuda, K.; Kenmotsu, H.; Naito, T.; et al. Clinical and radiation dose-volume factors related to pneumonitis after treatment with radiation and durvalumab in locally advanced non-small cell lung cancer. Investig. New Drugs 2020, 38, 1612–1617. [Google Scholar] [CrossRef]
| Before PSM | After PSM | |||||
|---|---|---|---|---|---|---|
| Durvalumab (Group D, n = 69) | No Durvalumab (Group N, n = 81) | p | Durvalumab (Group D, n = 30) | No Durvalumab (Group N, n = 30) | p | |
| Sex | 1.000 | 0.789 | ||||
| Male | 48 (70) | 57 (70) | 20 (67) | 18 (60) | ||
| Female | 21 (30) | 24 (30) | 10 (33) | 12 (40) | ||
| Age, median (range) | 71 (44–84) | 70 (48–87) | 0.652 | 71 (57–77) | 71 (48–85) | 0.215 |
| ECOG-PS | 0.257 | 0.624 | ||||
| 0 | 33 (48) | 28 (35) | 14 (47) | 10 (33) | ||
| 1 | 32 (46) | 46 (57) | 14 (47) | 17 (57) | ||
| 2 | 4 (6) | 7 (9) | 2 (7) | 3 (10) | ||
| Smoking history | 0.817 | 0.706 | ||||
| Yes | 60 (87) | 69 (85) | 27 (90) | 25 (83) | ||
| No | 9 (13) | 12 (15) | 3 (10) | 5 (17) | ||
| PF score | 0.058 | 0.117 | ||||
| 0 | 60 (87) | 62 (77) | 25 (83) | 23 (77) | ||
| 1 | 6 (9) | 8 (10) | 3 (10) | 1 (3) | ||
| 2 | 2 (3) | 11 (14) | 1 (3) | 6 (20) | ||
| 3 | 1 (1) | 0 (0) | 1 (3) | 0 (0) | ||
| Clinical stage (UICC 8th) | 0.844 | 0.312 | ||||
| IIIA | 37 (54) | 40 (49) | 19 (63) | 13 (43) | ||
| IIIB | 24 (35) | 32 (40) | 8 (27) | 11 (37) | ||
| IIIC | 8 (12) | 9 (11) | 3 (10) | 6 (20) | ||
| Histology | 0.660 | 0.470 | ||||
| Squamous cell carcinoma | 28 (41) | 32 (40) | 15 (50) | 13 (43) | ||
| Adenocarcinoma | 35 (51) | 40 (49) | 14 (47) | 13 (43) | ||
| Others | 6 (9) | 9 (11) | 1 (3) | 4 (13) | ||
| Treatment purpose | 0.132 | 1.000 | ||||
| Definitive | 53 (77) | 69 (85) | 26 (87) | 27 (90) | ||
| Salvage | 16 (23) | 12 (15) | 4 (13) | 3 (10) | ||
| Driver gene mutation | 0.416 | 0.671 | ||||
| Yes | 5 (7) (EGFR 4, ALK 1) | 10 (12) (EGFR 8, ALK 2) | 2 (7) (EGFR 1, ALK 1) | 4 (13) (EGFR 4) | ||
| No | 64 (93) | 71 (88) | 28 (93) | 26 (87) | ||
| PD-L1 TPS | <0.001 | 0.259 | ||||
| <1% | 15 (22) | 9 (11) | 6 (20) | 4 (13) | ||
| 1–50% | 19 (28) | 5 (6) | 9 (30) | 4 (13) | ||
| 50–100% | 13 (19) | 12 (15) | 5 (17) | 10 (33) | ||
| Not available | 22 (32) | 55 (68) | 10 (33) | 12 (40) | ||
| Radiation technique | <0.001 | 1.000 | ||||
| 3D-CRT | 24 (35) | 69 (85) | 19 (63) | 18 (60) | ||
| VMAT | 45 (65) | 12 (15) | 11 (37) | 12 (40) | ||
| Radiation field | <0.001 | 1.000 | ||||
| ENI | 13 (19) | 63 (78) | 13 (43) | 12 (47) | ||
| IFRT | 56 (81) | 18 (22) | 17 (57) | 18 (53) | ||
| Prescription dose | 0.505 | 0.612 | ||||
| <60 Gy | 1 (1) | 0 (0) | 1 (3) | 0 (0) | ||
| =60 Gy | 65 (94) | 79 (98) | 27 (90) | 29 (97) | ||
| >60 Gy | 3 (4) | 2 (2) | 2 (7) | 1 (3) | ||
| PTV (cm3), median (IQR) | 421 (316–583) | 622 (409–903) | <0.001 | 566 (368–804) | 601 (290–833) | 0.929 |
| TLV (cm3), median (IQR) | 3348 (2680–4118) | 3141 (2648–3884) | 0.371 | 3163 (2652–4091) | 2941 (2628–3746) | 0.433 |
| MLD (Gy), median (IQR) | 12.3 (9.9–15.6) | 13.8 (10.6–15.8) | 0.155 | 12.8 (10.7–16.0) | 13.9 (10.5–16.4) | 0.706 |
| V5 (%), median (IQR) | 47.9 (39.7–56.6) | 42.8 (35.7–51.0) | 0.140 | 44.9 (41.5–55.8) | 45.1 (35.5–56.5) | 0.912 |
| V20 (%), median (IQR) | 22.0 (16.6–25.4) | 24.4 (19.0–28.7) | 0.066 | 22.8 (19.3–30.4) | 25.6 (18.7–28.9) | 0.690 |
| VS5 (cm3), median (IQR) | 1692 (1327–2310) | 1708 (1365–2243) | 0.908 | 1655 (1268–2152) | 1591 (1337–1877) | 0.717 |
| Chemotherapy regimen | <0.001 | 0.208 | ||||
| CBDCA + PTX | 30 (43) | 12 (15) | 11 (37) | 6 (20) | ||
| CDDP + TS-1 | 20 (29) | 13 (16) | 8 (27) | 6 (20) | ||
| CDDP + VNR | 8 (12) | 23 (28) | 7 (23) | 7 (23) | ||
| CBDCA | 9 (13) | 18 (22) | 4 (13) | 6 (20) | ||
| CBDCA + TS-1 | 0 (0) | 6 (7) | 0 (0) | 1 (3) | ||
| Others | 2 (3) | 9 (11) | 0 (0) | 4 (13) | ||
| No Durvalumab (Group N) | Durvalumab (Group D) | |||||
|---|---|---|---|---|---|---|
| Out-of-Field Pneumonitis (n = 4) | In-Field Pneumonitis (n = 17) | p | Out-of-Field Pneumonitis (n = 14) | In-Field Pneumonitis (n = 14) | p | |
| MLD (Gy) | 15.66 (12.95–17.33) | 15.41 (12.36–17.45) | 0.965 | 10.46 (9.18–14.02) | 14.96 (12.30–17.48) | 0.005 |
| V5 (%) | 63.69 (46.05–81.52) | 49.11 (43.50–52.61) | 0.275 | 43.57 (32.68–54.31) | 51.07 (44.08–57.18) | 0.074 |
| V20 (%) | 27.23 (23.91–29.34) | 28.50 (21.51–33.29) | 0.654 | 19.20 (14.56–24.56) | 26.41 (20.68–31.17) | 0.008 |
| VS5 (cm3) | 1241 (729–1649) | 1517 (1444–1859) | 0.395 | 1677 (1336–1999) | 1516 (1320–1859) | 0.486 |
| TLV (cm3) | 3120 (2290–3941) | 3201 (2648–3700) | 0.829 | 3025 (2488–3974) | 3155 (2653–3694) | 0.772 |
| Univariate | Multivariate | ||||
|---|---|---|---|---|---|
| Variables | HR (95% CI) | p | HR (95% CI) | p | |
| Sex | Male | 1.38 (0.51–3.77) | 0.530 | ||
| Female | [Reference] | ||||
| Age (years) | ≥70 | 0.97 (0.41–2.29) | 0.948 | ||
| <70 | [Reference] | ||||
| Smoking history | Yes | 1.81 (0.42–7.79) | 0.424 | ||
| No | [Reference] | ||||
| PF score | 0 | [Reference] | [Reference] | ||
| 1–3 | 3.53 (1.50–8.33) | 0.004 | 2.89 (1.21–6.91) | 0.017 | |
| Radiation technique | VMAT | 1.15 (0.34–3.90) | 0.826 | ||
| 3D-CRT | [Reference] | ||||
| Radiation field | IFRT | 1.30 (0.48–3.55) | 0.607 | ||
| ENI | [Reference] | ||||
| PTV (cm3) | per 10 cm3 | 1.01 (1.00–1.02) | 0.136 | ||
| Chemotherapy regimen | CDDP included | 0.68 (0.29–1.61) | 0.384 | ||
| CBDCA included | [Reference] | ||||
| MLD (Gy) | ≥14 | 3.48 (1.35–8.99) | 0.010 | 2.91 (1.11–7.63) | 0.030 |
| <14 | [Reference] | [Reference] | |||
| VS5 (cm3) | <1800 | 2.25 (0.91–5.59) | 0.080 | ||
| ≥1800 | [Reference] | ||||
| Univariate | Multivariate | ||||
|---|---|---|---|---|---|
| Variables | HR (95% CI) | p | HR (95% CI) | p | |
| Sex | Male | 1.23 (0.54–2.79) | 0.626 | ||
| Female | [Reference] | ||||
| Age (years) | ≥70 | 1.11 (0.52–2.38) | 0.784 | ||
| <70 | [Reference] | ||||
| Smoking history | Yes | 1.54 (0.47–5.11) | 0.479 | ||
| No | [Reference] | ||||
| PF score | 0 | [Reference] | [Reference] | ||
| 1–3 | 1.25 (0.43–3.61) | 0.677 | 1.70 (0.57–5.05) | 0.340 | |
| Radiation technique | VMAT | 1.16 (0.52–2.57) | 0.716 | ||
| 3D-CRT | [Reference] | ||||
| Radiation field | IFRT | 2.13 (0.64–7.06) | 0.205 | ||
| ENI | [Reference] | ||||
| PTV (cm3) | per 10 cm3 | 1.00 (0.99–1.02) | 0.917 | ||
| Chemotherapy regimen | CDDP included | 1.53 (0.73–3.21) | 0.262 | ||
| CBDCA included | [Reference] | ||||
| MLD (Gy) | ≥14 | 0.97 (0.44–2.14) | 0.939 | 0.67 (0.29–1.55) | 0.351 |
| <14 | [Reference] | [Reference] | |||
| VS5 (cm3) | <1800 | 2.32 (1.05–5.13) | 0.038 | 2.87 (1.23–6.69) | 0.015 |
| ≥1800 | [Reference] | [Reference] | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sato, M.; Odagiri, K.; Tabuchi, Y.; Okamoto, H.; Shimokawa, T.; Nakamura, Y.; Hata, M. Patterns and Incidence of Pneumonitis and Initial Treatment Outcomes with Durvalumab Consolidation Therapy after Radical Chemoradiotherapy for Stage III Non-Small Cell Lung Cancer. Cancers 2024, 16, 1162. https://doi.org/10.3390/cancers16061162
Sato M, Odagiri K, Tabuchi Y, Okamoto H, Shimokawa T, Nakamura Y, Hata M. Patterns and Incidence of Pneumonitis and Initial Treatment Outcomes with Durvalumab Consolidation Therapy after Radical Chemoradiotherapy for Stage III Non-Small Cell Lung Cancer. Cancers. 2024; 16(6):1162. https://doi.org/10.3390/cancers16061162
Chicago/Turabian StyleSato, Mizuki, Kazumasa Odagiri, Yuya Tabuchi, Hiroaki Okamoto, Tsuneo Shimokawa, Yukiko Nakamura, and Masaharu Hata. 2024. "Patterns and Incidence of Pneumonitis and Initial Treatment Outcomes with Durvalumab Consolidation Therapy after Radical Chemoradiotherapy for Stage III Non-Small Cell Lung Cancer" Cancers 16, no. 6: 1162. https://doi.org/10.3390/cancers16061162
APA StyleSato, M., Odagiri, K., Tabuchi, Y., Okamoto, H., Shimokawa, T., Nakamura, Y., & Hata, M. (2024). Patterns and Incidence of Pneumonitis and Initial Treatment Outcomes with Durvalumab Consolidation Therapy after Radical Chemoradiotherapy for Stage III Non-Small Cell Lung Cancer. Cancers, 16(6), 1162. https://doi.org/10.3390/cancers16061162





