Frontline and Relapsed Rhabdomyosarcoma (FaR-RMS) Clinical Trial: A Report from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG)
Abstract
Simple Summary
Abstract
1. Introduction
- the introduction of novel regimens compared to current standard of care in the most advanced disease states: Very High-Risk (VHR), High Risk (HR), and Relapse;
- the optimal duration of vinorelbine and cyclophosphamide maintenance chemotherapy;
- the use of radiotherapy to improve local control in VHR, HR, and Standard Risk (SR) patients and metastatic control in VHR disease.
- the risk stratification using PAX-FOXO1 fusion gene status instead of histological subtyping;
- the use of [18F]FDG PET-CT and diffusion-weighted MRI imaging (DWI) response assessments as prognostic biomarkers for outcome following induction chemotherapy;
- the impact of local therapy (radiotherapy and surgery) on the health-related quality of life (HRQoL) for specific subgroups of patients.
2. Background
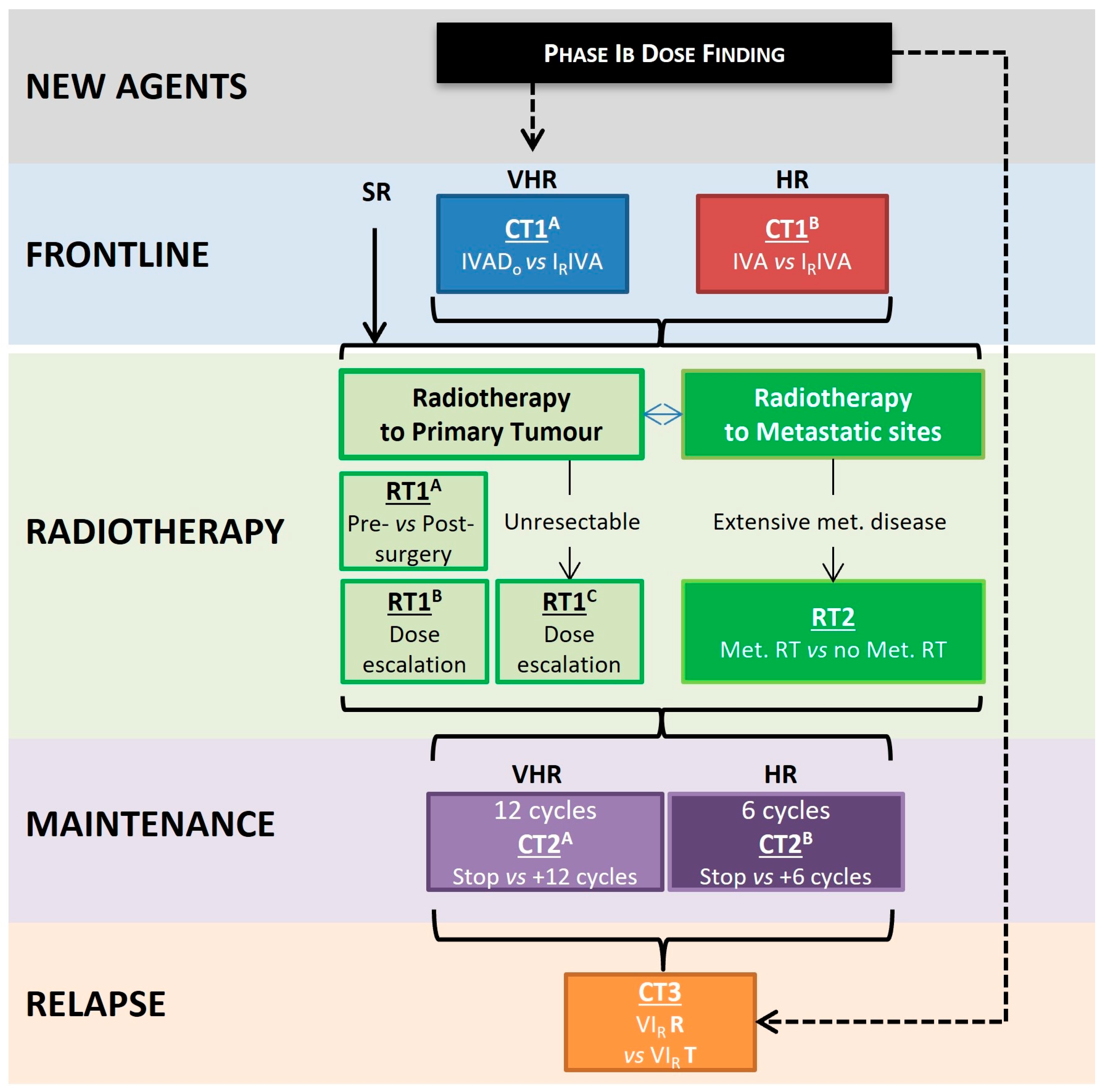
3. The Trial Design
- VHR = Very High-Risk; and HR = High Risk;
- I = Ifosfamide; V = vincristine; A = Actinomycin D; Do = Doxorubicin; IR = Irinotecan; and R = Regorafenib;
- RT1A = Randomisation for pre- or postoperative radiotherapy;
- RT1B = Randomisation for dose escalation for patients with resectable tumours at high risk of local failure;
- RT1C = Randomisation for dose escalation for patients with unresectable tumours at high risk of local failure;
- RT2 = Randomisation for radiotherapy to primary site vs. all metastatic sites for patients with widely metastatic disease (Oberlin score > 3);
- CT1A = Randomisation between induction chemotherapy of IVADo and IRIVA in newly diagnosed patients with VHR disease;
- CT1B = Randomisation between induction chemotherapy of IVA and IRIVA in newly diagnosed patients with HR disease;
- CT2A = Randomisation between 12- and 24-month maintenance chemotherapy for patients with VHR disease;
- CT2B = Randomisation between 6- and 12-month maintenance chemotherapy for patients with VHR disease;
- CT3 = Randomisation between VIRT and VIRR.
4. Eligibility and Risk Stratification
- PAX-FOXO1 fusion status is now used in place of alveolar/non-alveolar histology;
- The former subgroup D has moved from Standard to High-Risk;
- Genitourinary (GU) bladder/prostate and biliary sites are now considered favourable rather than unfavourable sites, based on analysis of RMS 2005 data;
- The newly designated VHR group now includes metastatic RMS in addition to PAX:FOXO1 fusion-positive, node-positive RMS (this differs from the previous EpSSG RMS 2005 study because metastatic patients are eligible for inclusion within FaR-RMS).
4.1. Can Outcomes Be Improved by Utilising New Combinations of Systemic Anti-Cancer Therapies, including the Addition of New Biologically Targeted Drugs
4.1.1. Frontline Treatment for Newly Diagnosed Patients
4.1.2. Patients with Relapsed Disease
4.2. Improving Outcomes for RMS through Optimisation of Radiotherapy Strategy
4.2.1. The Timing of Adjuvant Radiotherapy
4.2.2. Can Dose Escalation of Radiotherapy Improve Local Control in Patients at a Higher Risk of Local Failure?
4.2.3. Can Radiotherapy to All Metastatic Sites in Unfavourable Metastatic Disease Reduce the Risk of Relapse and Improve EFS?
- ○
- Age < 1 y or ≥10 y;
- ○
- ‘Unfavourable’ site: extremity, other, and unidentified;
- ○
- Bone or bone marrow involvement;
- ○
- ≥3 metastatic sites.
4.3. Can Prolongation of Maintenance Therapy Reduce the Risk of Relapse and Improve OS?
4.4. To Assess Whether PAX-FOXO1 Fusion Status in place of Histological Diagnosis Improves Riskt Stratification
5. Statistical Considerations
6. Health-Related Quality of Life and Patient-Reported Outcome Measures
7. Imaging Studies
8. Associated Biological/Biomarker Studies + Opportunity for Biobanking
8.1. Frontline
8.2. Relapse (Collaboration with Bayer)
8.3. VIVO Tissue Bank
9. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- FaR-RMS: An Overarching Study for Children and Adults with Frontline and Relapsed RhabdoMyoSarcoma—Full Text View—ClinicalTrials.gov. Available online: https://classic.clinicaltrials.gov/ct2/show/NCT04625907 (accessed on 21 February 2024).
- Hallpike, E. Creative participation for young cancer survivors: Designing a logo for the European paediatric Soft tissue sarcoma Study Group (EpSSG) Frontline and Relapse-Rhabdomyosarcoma Study (FaR-RMS). In Proceedings of the 4th Global AYA Conference, London, UK, 13–15 July 2020. [Google Scholar]
- Available online: https://www.alicesarc.org/ (accessed on 21 February 2024).
- Ferrari, A.; Dileo, P.; Casanova, M.; Bertulli, R.; Meazza, C.; Gandola, L.; Navarria, P.; Collini, P.; Gronchi, A.; Olmi, P.; et al. Rhabdomyosarcoma in adults. A retrospective analysis of 171 patients treated at a single institution. Cancer 2003, 98, 571–580. [Google Scholar] [CrossRef]
- Sultan, I.; Qaddoumi, I.; Yaser, S.; Rodriguez-Galindo, C.; Ferrari, A. Comparing adult and pediatric rhabdomyosarcoma in the surveillance, epidemiology and end results program, 1973 to 2005: An analysis of 2600 patients. J. Clin. Oncol. 2009, 27, 3391–3397. [Google Scholar] [CrossRef]
- Available online: https://www.childrenwithcancer.org.uk/childhood-cancer-info/cancer-types/rhabdomyosarcoma/ (accessed on 21 February 2024).
- Martin-Giacalone, B.A.; Weinstein, P.A.; Plon, S.E.; Lupo, P.J. Pediatric Rhabdomyosarcoma: Epidemiology and Genetic Susceptibility. J. Clin. Med. 2021, 10, 2028. [Google Scholar] [CrossRef]
- Parham, D.M.; Ellison, D.A. Rhabdomyosarcomas in adults and children: An update. Arch. Pathol. Lab. Med. 2006, 130, 1454–1465. [Google Scholar] [CrossRef]
- Rudzinski, E.R.; Anderson, J.R.; Hawkins, D.S.; Skapek, S.X.; Parham, D.M.; Teot, L.A. The World Health Organization Classification of Skeletal Muscle Tumors in Pediatric Rhabdomyosarcoma: A Report from the Children’s Oncology Group. Arch. Pathol. Lab. Med. 2015, 139, 1281–1287. [Google Scholar] [CrossRef]
- Skapek, S.X.; Anderson, J.; Barr, F.G.; Bridge, J.A.; Gastier-Foster, J.M.; Parham, D.M.; Rudzinski, E.R.; Triche, T.; Hawkins, D.S. PAX-FOXO1 fusion status drives unfavorable outcome for children with rhabdomyosarcoma: A children’s oncology group report. Pediatr. Blood Cancer 2013, 60, 1411–1417. [Google Scholar] [CrossRef]
- Burke, M.; Anderson, J.R.; Kao, S.C.; Rodeberg, D.; Qualman, S.J.; Wolden, S.L.; Meyer, W.H.; Breitfeld, P.P. Assessment of response to induction therapy and its influence on 5-year failure-free survival in group III rhabdomyosarcoma: The Intergroup Rhabdomyosarcoma Study-IV experience—A report from the Soft Tissue Sarcoma Committee of the Children’s Oncology Group. J. Clin. Oncol. 2007, 25, 4909–4913. [Google Scholar] [CrossRef]
- Oberlin, O.; Rey, A.; Sanchez de Toledo, J.; Martelli, H.; Jenney, M.E.; Scopinaro, M.; Bergeron, C.; Merks, J.H.; Bouvet, N.; Ellershaw, C.; et al. Randomized comparison of intensified six-drug versus standard three-drug chemotherapy for high-risk nonmetastatic rhabdomyosarcoma and other chemotherapy-sensitive childhood soft tissue sarcomas: Long-term results from the International Society of Pediatric Oncology MMT95 study. J. Clin. Oncol. 2012, 30, 2457–2465. [Google Scholar] [CrossRef]
- Osenberg, A.R.; Anderson, J.R.; Lyden, E.; Rodeberg, D.A.; Wolden, S.L.; Kao, S.C.; Parham, D.M.; Arndt, C.; Hawkins, D.S. Early response as assessed by anatomic imaging does not predict failure-free survival among patients with Group III rhabdomyosarcoma: A report from the Children’s Oncology Group. Eur. J. Cancer 2014, 50, 816–823. [Google Scholar] [CrossRef]
- Oberlin, O.; Rey, A.; Lyden, E.; Bisogno, G.; Stevens, M.C.; Meyer, W.H.; Carli, M.; Anderson, J.R. Prognostic factors in metastatic rhabdomyosarcomas: Results of a pooled analysis from United States and European cooperative groups. J. Clin. Oncol. 2008, 26, 2384–2389. [Google Scholar] [CrossRef]
- Bisogno, G.; Minard-Colin, V.; Zanetti, I.; Ferrari, A.; Gallego, S.; Dávila Fajardo, R.; Mandeville, H.; Kelsey, A.; Alaggio, R.; Orbach, D.; et al. Nonmetastatic Rhabdomyosarcoma in Children and Adolescents: Overall Results of the European Pediatric Soft Tissue Sarcoma Study Group RMS2005 Study. J. Clin. Oncol. 2023, 41, 2342–2349. [Google Scholar] [CrossRef]
- Crist, W.M.; Anderson, J.R.; Meza, J.L.; Fryer, C.; Raney, R.B.; Ruymann, F.B.; Breneman, J.; Qualman, S.J.; Wiener, E.; Wharam, M.; et al. Intergroup rhabdomyosarcoma study-IV: Results for patients with nonmetastatic disease. J. Clin. Oncol. 2001, 19, 3091–3102. [Google Scholar] [CrossRef]
- Meza, J.L.; Anderson, J.; Pappo, A.S.; Meyer, W.H.; Children’s Oncology Group. Analysis of prognostic factors in patients with nonmetastatic rhabdomyosarcoma treated on intergroup rhabdomyosarcoma studies III and IV: The Children’s Oncology Group. J. Clin. Oncol. 2006, 24, 3844–3851. [Google Scholar] [CrossRef]
- Chisholm, J.C.; Marandet, J.; Rey, A.; Scopinaro, M.; de Toledo, J.S.; Merks, J.H.; O’Meara, A.; Stevens, M.C.; Oberlin, O. Prognostic factors after relapse in nonmetastatic rhabdomyosarcoma: A nomogram to better define patients who can be salvaged with further therapy. J. Clin. Oncol. 2011, 29, 1319–1325. [Google Scholar] [CrossRef]
- Bisogno, G.; Jenney, M.; Bergeron, C.; Gallego Melcón, S.; Ferrari, A.; Oberlin, O.; Carli, M.; Stevens, M.; Kelsey, A.; De Paoli, A.; et al. Addition of dose-intensified doxorubicin to standard chemotherapy for rhabdomyosarcoma (EpSSG RMS 2005): A multicentre, open-label, randomised controlled, phase 3 trial. Lancet Oncol. 2018, 19, 1061–1071. [Google Scholar] [CrossRef]
- Ferrari, A.; Chisholm, J.C.; Jenney, M.; Minard-Colin, V.; Orbach, D.; Casanova, M.; Guillen, G.; Glosli, H.; van Rijn, R.R.; Schoot, R.A.; et al. Adolescents and young adults with rhabdomyosarcoma treated in the European paediatric Soft tissue sarcoma Study Group (EpSSG) protocols: A cohort study. Lancet Child Adolesc. Health 2022, 6, 545–554. [Google Scholar] [CrossRef]
- Di Carlo, D.; Chisholm, J.; Kelsey, A.; Alaggio, R.; Bisogno, G.; Minard-Colin, V.; Jenney, M.; Dávila Fajardo, R.; Merks, J.H.M.; Shipley, J.M.; et al. Biological Role and Clinical Implications of MYOD1L122R Mutation in Rhabdomyosarcoma. Cancers 2023, 15, 1644. [Google Scholar] [CrossRef]
- Schoot, R.A.; Chisholm, J.; Casanova, M.; Minard-Colin, V.; Geoerger, B.; Cameron, A.L.; Coppadoro, B.; Zanetti, I.; Orbach, D.; Kelsey, A.; et al. Metastatic Rhabdomyosarcoma: Results of the European Paediatric Soft Tissue Sarcoma Study Group MTS 2008 Study and Pooled Analysis with the Concurrent BERNIE Study. J. Clin. Oncol. 2022, 40, 3730–3740. [Google Scholar] [CrossRef]
- Pappo, A.S.; Anderson, J.R.; Crist, W.M.; Wharam, M.D.; Breitfeld, P.P.; Hawkins, D.; Raney, R.B.; Womer, R.B.; Parham, D.M.; Qualman, S.J.; et al. Survival after relapse in children and adolescents with rhabdomyosarcoma: A report from the Intergroup Rhabdomyosarcoma Study Group. J. Clin. Oncol. 1999, 17, 3487–3493. [Google Scholar] [CrossRef]
- Oberoi, S.; Qumseya, A.; Xue, W.; Harrison, D.J.; Rudzinski, E.R.; Wolden, S.L.; Dasgupta, R.; Venkatramani, R.; Gupta, A.A. Feasibility of combining temsirolimus to vincristine, dactinomycin, cyclophosphamide, and vincristine and irinotecan chemotherapy for children with intermediate-risk rhabdomyosarcoma: A report from Children’s Oncology Group. Pediatr. Blood Cancer 2023, 70, e30436. [Google Scholar] [CrossRef]
- Defachelles, A.S.; Bogart, E.; Casanova, M.; Merks, J.H.M.; Bisogno, G.; Calareso, G.; Gallego Melcon, S.; Gatz, S.A.; Le Deley, M.C.; McHugh, K.; et al. Randomized Phase II Trial of Vincristine-Irinotecan with or without Temozolomide, in Children and Adults with Relapsed or Refractory Rhabdomyosarcoma: A European Paediatric Soft Tissue Sarcoma Study Group and Innovative Therapies for Children with Cancer Trial. J. Clin. Oncol. 2021, 39, 2979–2990. [Google Scholar] [CrossRef]
- Rogers, T.N.; Seitz, G.; Fuchs, J.; Martelli, H.; Dasgupta, R.; Routh, J.C.; Hawkins, D.S.; Koscielniak, E.; Bisogno, G.; Rodeberg, D.A. Surgical management of paratesticular rhabdomyosarcoma: A consensus opinion from the Children’s Oncology Group, European paediatric Soft tissue sarcoma Study Group, and the Cooperative Weichteilsarkom Studiengruppe. Pediatr. Blood Cancer 2021, 68, e28938. [Google Scholar] [CrossRef]
- Casey, D.L.; Mandeville, H.; Bradley, J.A.; Ter Horst, S.A.J.; Sheyn, A.; Timmermann, B.; Wolden, S.L. Local control of parameningeal rhabdomyosarcoma: An expert consensus guideline from the International Soft Tissue Sarcoma Consortium (INSTRuCT). Pediatr. Blood Cancer 2022, 69, e29751. [Google Scholar] [CrossRef]
- Hawkins, D.S.; Bisogno, G.; Koscielniak, E. Introducing INSTRuCT: An international effort to promote cooperation and data sharing. Pediatr. Blood Cancer 2023, 70, e28701. [Google Scholar] [CrossRef]
- Blagden, S.P.; Billingham, L.; Brown, L.C.; Buckland, S.W.; Cooper, A.M.; Ellis, S.; Fisher, W.; Hughes, H.; Keatley, D.A.; Maignen, F.M.; et al. Effective delivery of Complex Innovative Design (CID) cancer trials-A consensus statement. Br. J. Cancer 2020, 122, 473–482. [Google Scholar] [CrossRef]
- Antonijevic, Z.; Beckman, R.A. (Eds.) Platform Trial Designs in Drug Development; Chapman and Hall/CRC: Boca Raton, FL, USA, 2018. [Google Scholar] [CrossRef]
- Noujaim, J.; Thway, K.; Jones, R.L.; Miah, A.; Khabra, K.; Langer, R.; Kasper, B.; Judson, I.; Benson, C.; Kollàr, A. Adult Pleomorphic Rhabdomyosarcoma: A Multicentre Retrospective Study. Anticancer Res. 2015, 35, 6213–6217. [Google Scholar]
- Arndt, C.A.S.; Bisogno, G.; Koscielniak, E. Fifty years of rhabdomyosarcoma studies on both sides of the pond and lessons learned. Cancer Treat. Rev. 2018, 68, 94–101. [Google Scholar] [CrossRef]
- Haduong, J.H.; Heske, C.M.; Allen-Rhoades, W.; Xue, W.; Teot, L.A.; Rodeberg, D.A.; Donaldson, S.S.; Weiss, A.; Hawkins, D.S.; Venkatramani, R. An update on rhabdomyosarcoma risk stratification and the rationale for current and future Children’s Oncology Group clinical trials. Pediatr. Blood Cancer 2022, 69, e29511. [Google Scholar] [CrossRef]
- Arndt, C.A.; Stoner, J.A.; Hawkins, D.S.; Rodeberg, D.A.; Hayes-Jordan, A.A.; Paidas, C.N.; Parham, D.M.; Teot, L.A.; Wharam, M.D.; Breneman, J.C.; et al. Vincristine, Actinomycin, and Cyclophosphamide Compared with Vincristine, Actinomycin, and Cyclophosphamide Alternating with Vincristine, Topotecan, and Cyclophosphamide for Intermediate-Risk Rhabdomyosarcoma: Children’s Oncology Group Study D9803. J. Clin. Oncol. 2009, 27, 5182–5188. [Google Scholar] [CrossRef]
- Hawkins, D.S.; Chi, Y.Y.; Anderson, J.R.; Tian, J.; Arndt, C.A.S.; Bomgaars, L.; Donaldson, S.S.; Hayes-Jordan, A.; Mascarenhas, L.; McCarville, M.B.; et al. Addition of Vincristine and Irinotecan to Vincristine, Dactinomycin, and Cyclophosphamide Does Not Improve Outcome for Intermediate-Risk Rhabdomyosarcoma: A Report From the Children’s Oncology Group. J. Clin. Oncol. 2018, 36, 2770–2777. [Google Scholar] [CrossRef] [PubMed]
- Gallego, S.; Chi, Y.Y.; De Salvo, G.L.; Li, M.; Merks, J.H.M.; Rodeberg, D.A.; van Scheltinga, S.T.; Mascarenhas, L.; Orbach, D.; Jenney, M.; et al. Alveolar rhabdomyosarcoma with regional nodal involvement: Results of a combined analysis from two cooperative groups. Pediatr. Blood Cancer 2021, 68, e28832. [Google Scholar] [CrossRef]
- Bisogno, G.; De Salvo, G.L.; Bergeron, C.; Gallego Melcón, S.; Merks, J.H.; Kelsey, A.; Martelli, H.; Minard-Colin, V.; Orbach, D.; Glosli, H.; et al. Vinorelbine and continuous low-dose cyclophosphamide as maintenance chemotherapy in patients with high-risk rhabdomyosarcoma (RMS 2005): A multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2019, 20, 1566–1575. [Google Scholar] [CrossRef]
- Gallego, S.; Zanetti, I.; Orbach, D.; Ranchère, D.; Shipley, J.; Zin, A.; Bergeron, C.; de Salvo, G.L.; Chisholm, J.; Ferrari, A.; et al. Fusion status in patients with lymph node-positive (N1) alveolar rhabdomyosarcoma is a powerful predictor of prognosis: Experience of the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG). Cancer 2018, 124, 3201–3209. [Google Scholar] [CrossRef]
- Weigel, B.J.; Lyden, E.; Anderson, J.R.; Meyer, W.H.; Parham, D.M.; Rodeberg, D.A.; Michalski, J.M.; Hawkins, D.S.; Arndt, C.A. Intensive Multiagent Therapy, Including Dose-Compressed Cycles of Ifosfamide/Etoposide and Vincristine/Doxorubicin/Cyclophosphamide, Irinotecan, and Radiation, in Patients with High-Risk Rhabdomyosarcoma: A Report From the Children’s Oncology Group. J. Clin. Oncol. 2016, 34, 117–122. [Google Scholar] [CrossRef]
- Bergeron, C.; Thiesse, P.; Rey, A.; Orbach, D.; Boutard, P.; Thomas, C.; Schmitt, C.; Scopinaro, M.J.; Bernard, F.; Stevens, M.; et al. Revisiting the role of doxorubicin in the treatment of rhabdomyosarcoma: An up-front window study in newly diagnosed children with high-risk metastatic disease. Eur. J. Cancer 2008, 44, 427–431. [Google Scholar] [CrossRef]
- Chisholm, J.C.; Merks, J.H.M.; Casanova, M.; Bisogno, G.; Orbach, D.; Gentet, J.C.; Thomassin-Defachelles, A.S.; Chastagner, P.; Lowis, S.; Ronghe, M.; et al. Open-label, multicentre, randomised, phase II study of the EpSSG and the ITCC evaluating the addition of bevacizumab to chemotherapy in childhood and adolescent patients with metastatic soft tissue sarcoma (the BERNIE study). Eur. J. Cancer 2017, 83, 177–184. [Google Scholar] [CrossRef]
- Pappo, A.S.; Lyden, E.; Breitfeld, P.; Donaldson, S.S.; Wiener, E.; Parham, D.; Crews, K.R.; Houghton, P.; Meyer, W.H. Two Consecutive Phase II Window Trials of Irinotecan Alone or in Combination with Vincristine for the Treatment of Metastatic Rhabdomyosarcoma: The Children’s Oncology Group. J. Clin. Oncol. 2007, 25, 362–369. [Google Scholar] [CrossRef]
- Mascarenhas, L.; Lyden, E.R.; Breitfeld, P.P.; Walterhouse, D.O.; Donaldson, S.S.; Paidas, C.N.; Parham, D.M.; Anderson, J.R.; Meyer, W.H.; Hawkins, D.S. Randomized Phase II Window Trial of Two Schedules of Irinotecan with Vincristine in Patients with First Relapse or Progression of Rhabdomyosarcoma: A Report From the Children’s Oncology Group. J. Clin. Oncol. 2010, 28, 4658–4663. [Google Scholar] [CrossRef]
- Bisogno, G.; Ferrari, A.; Tagarelli, A.; Sorbara, S.; Chiaravalli, S.; Poli, E.; Scarzello, G.; De Corti, F.; Casanova, M.; Affinita, M.C. Integrating irinotecan in standard chemotherapy: A novel dose-density combination for high-risk pediatric sarcomas. Pediatr. Blood Cancer 2021, 68, e28951. [Google Scholar] [CrossRef]
- Skolnik, J.M.; Barrett, J.S.; Jayaraman, B.; Patel, D.; Adamson, P.C. Shortening the Timeline of Pediatric Phase I Trials: The Rolling Six Design. J. Clin. Oncol. 2008, 26, 190–195. [Google Scholar] [CrossRef]
- Heske, C.M.; Mascarenhas, L. Relapsed Rhabdomyosarcoma. J. Clin. Med. 2021, 10, 804. [Google Scholar] [CrossRef]
- Skapek, S.X.; Ferrari, A.; Gupta, A.A.; Lupo, P.J.; Butler, E.; Shipley, J.; Barr, F.G.; Hawkins, D.S. Rhabdomyosarcoma. Nat. Rev. Dis. Primers 2019, 5, 1. [Google Scholar] [CrossRef]
- Daudigeos-Dubus, E.; Le Dret, L.; Lanvers-Kaminsky, C.; Bawa, O.; Opolon, P.; Vievard, A.; Villa, I.; Pagès, M.; Bosq, J.; Vassal, G.; et al. Regorafenib: Antitumor Activity upon Mono and Combination Therapy in Preclinical Pediatric Malignancy Models. PLoS ONE 2015, 10, e0142612. [Google Scholar] [CrossRef]
- Harrison, D.J.; Gill, J.D.; Roth, M.E.; Zhang, W.; Teicher, B.; Erickson, S.; Gatto, G.; Kurmasheva, R.T.; Houghton, P.J.; Smith, M.A.; et al. Initial in vivo testing of a multitarget kinase inhibitor, regorafenib, by the Pediatric Preclinical Testing Consortium. Pediatr. Blood Cancer 2020, 67, e28222. [Google Scholar] [CrossRef]
- Goldstein, M.; Meller, I.; Orr-Urtreger, A. FGFR1 over-expression in primary rhabdomyosarcoma tumors is associated with hypomethylation of a 5′ CpG Island and abnormal expression of theAKT1,NOG, andBMP4 genes. Genes Chromosomes Cancer 2007, 46, 1028–1038. [Google Scholar] [CrossRef]
- Missiaglia, E.; Selfe, J.; Hamdi, M.; Williamson, D.; Schaaf, G.; Fang, C.; Koster, J.; Summersgill, B.; Messahel, B.; Versteeg, R.; et al. Genomic imbalances in rhabdomyosarcoma cell lines affect expression of genes frequently altered in primary tumors: An approach to identify candidate genes involved in tumor development. Genes Chromosomes Cancer 2009, 48, 455–467. [Google Scholar] [CrossRef]
- Geoerger, B.; Morland, B.; Jiménez, I.; Frappaz, D.; Pearson, A.D.J.; Vassal, G.; Maeda, P.; Kincaide, J.; Mueller, U.; Schlief, S.; et al. Phase 1 dose-escalation and pharmacokinetic study of regorafenib in paediatric patients with recurrent or refractory solid malignancies. Eur. J. Cancer 2021, 153, 142–152. [Google Scholar] [CrossRef]
- Casanova, M.; Bautista, F.; Campbell-Hewson, Q.; Makin, G.; Marshall, L.V.; Verschuur, A.C.; Cañete Nieto, A.; Corradini, N.; Ploeger, B.A.; Brennan, B.J.; et al. Regorafenib Plus Vincristine and Irinotecan in Pediatric Patients with Recurrent/Refractory Solid Tumors: An Innovative Therapies for Children with Cancer Study. Clin. Cancer Res. 2023, 29, 4341–4351. [Google Scholar] [CrossRef]
- Barker, H.E.; Paget, J.T.E.; Khan, A.A.; Harrington, K.J. The tumour microenvironment after radiotherapy: Mechanisms of resistance and recurrence. Nat. Rev. Cancer 2015, 15, 409–425. [Google Scholar] [CrossRef]
- O’Sullivan, B.; Davis, A.M.; Turcotte, R.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Kandel, R.; Goddard, K.; Sadura, A.; et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: A randomised trial. Lancet 2002, 359, 2235–2241. [Google Scholar] [CrossRef]
- Seitz, G.; Dantonello, T.M.; Int-Veen, C.; Blumenstock, G.; Godzinski, J.; Klingebiel, T.; Schuck, A.; Leuschner, I.; Koscielniak, E.; Fuchs, J. Treatment efficiency, outcome and surgical treatment problems in patients suffering from localized embryonal bladder/prostate rhabdomyosarcoma: A report from the cooperative soft tissue sarcoma trial CWS-96. Pediatr. Blood Cancer 2011, 56, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Réguerre, Y.; Martelli, H.; Rey, A.; Rogers, T.; Gaze, M.; Ben Arush, M.W.; Devalck, C.; Oberlin, O.; Stevens, M.; Orbach, D. Local therapy is critical in localised pelvic rhabdomyosarcoma: Experience of the International Society of Pediatric Oncology Malignant Mesenchymal Tumor (SIOP-MMT) committee. Eur. J. Cancer 2012, 48, 2020–2027. [Google Scholar] [CrossRef]
- Donaldson, S.S.; Meza, J.; Breneman, J.C.; Crist, W.M.; Laurie, F.; Qualman, S.J.; Wharam, M. Results from the IRS-IV randomized trial of hyperfractionated radiotherapy in children with rhabdomyosarcoma—A report from the IRSG 1 1For a complete list of the members of the Children’s Oncology Group Soft Tissue Sarcoma Committee (formerly Intergroup Rhabdomyosarcoma Group) representing the Children’s Oncology Group and the Quality Assurance Review Center. Int. J. Radiat. Oncol. Biol. Phys. 2001, 51, 718–728. [Google Scholar] [CrossRef]
- Michalski, J.M.; Meza, J.; Breneman, J.C.; Wolden, S.L.; Laurie, F.; Jodoin, M.; Raney, B.; Wharam, M.D.; Donaldson, S.S. Influence of radiation therapy parameters on outcome in children treated with radiation therapy for localized parameningeal rhabdomyosarcoma in Intergroup Rhabdomyosarcoma Study Group trials II through IV. Int. J. Radiat. Oncol. Biol. Phys. 2004, 59, 1027–1038. [Google Scholar] [CrossRef]
- Lin, C.; Donaldson, S.S.; Meza, J.L.; Anderson, J.R.; Lyden, E.R.; Brown, C.K.; Morano, K.; Laurie, F.; Arndt, C.A.; Enke, C.A.; et al. Effect of Radiotherapy Techniques (IMRT vs. 3D-CRT) on Outcome in Patients with Intermediate-Risk Rhabdomyosarcoma Enrolled in COG D9803—A Report From the Children’s Oncology Group. Int. J. Radiat. Oncol. Biol. Phys. 2012, 82, 1764–1770. [Google Scholar] [CrossRef]
- Cameron, A.L.; Elze, M.C.; Casanova, M.; Geoerger, B.; Gaze, M.N.; Minard-Colin, V.; McHugh, K.; van Rijn, R.R.; Kelsey, A.; Martelli, H.; et al. The Impact of Radiation Therapy in Children and Adolescents with Metastatic Rhabdomyosarcoma. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 968–978. [Google Scholar] [CrossRef]
- Liu, A.K.; Stinauer, M.; Albano, E.; Greffe, B.; Tello, T.; Maloney, K. Local control of metastatic sites with radiation therapy in metastatic Ewing sarcoma and rhabdomyosarcoma. Pediatr. Blood Cancer 2011, 57, 169–171. [Google Scholar] [CrossRef]
- Skamene, S.; Abish, S.; Mitchell, D.; Freeman, C. Radiotherapy is Important for Local Control at Primary and Metastatic Sites in Pediatric Rhabdomyosarcoma. Cureus 2015, 7, e388. [Google Scholar] [CrossRef]
- Rodeberg, D.; Arndt, C.; Breneman, J.; Lyden, E.; Donaldson, S.; Paidas, C.; Andrassy, R.; Meyer, W.; Wiener, E. Characteristics and outcomes of rhabdomyosarcoma patients with isolated lung metastases from IRS-IV. J Pediatr. Surg. 2005, 40, 256–262. [Google Scholar] [CrossRef]
- Dantonello, T.M.; Winkler, P.; Boelling, T.; Friedel, G.; Schmid, I.; Mattke, A.C.; Ljungman, G.; Bielack, S.S.; Klingebiel, T.; Koscielniak, E.; et al. Embryonal rhabdomyosarcoma with metastases confined to the lungs: Report from the CWS Study Group. Pediatr. Blood Cancer 2011, 56, 725–732. [Google Scholar] [CrossRef]
- Chisholm, J.C.; Schoot, R.A.; Cameron, A.L.; Casanova, M.; Minard-Collin, V.; Coppadoro, B.; Garrido, M.; Rogers, T.; Orbach, D.; Glosli, H.; et al. Outcomes in lung-only metastatic rhabdomyosarcoma: An analysis of data from the European paediatric Soft tissue sarcoma Study Group MTS 2008 study. EJC Paediatr. Oncol. 2023, 2, 100018. [Google Scholar] [CrossRef]
- Bisogno, G.; Minard-Colin, V.; Jenney, M.; Ferrari, A.; Chisholm, J.; Di Carlo, D.; Hjalgrim, L.L.; Orbach, D.; Merks, J.H.M.; Casanova, M. Maintenance Chemotherapy for Patients with Rhabdomyosarcoma. Cancers 2023, 15, 4012. [Google Scholar] [CrossRef]
- Natale, G.; Bocci, G. Does metronomic chemotherapy induce tumor angiogenic dormancy? A review of available preclinical and clinical data. Cancer Lett. 2018, 432, 28–37. [Google Scholar] [CrossRef]
- Kerbel, R.S.; Kamen, B.A. The anti-angiogenic basis of metronomic chemotherapy. Nat. Rev. Cancer 2004, 4, 423–436. [Google Scholar] [CrossRef]
- Casanova, M.; Ferrari, A.; Bisogno, G.; Merks, J.H.; De Salvo, G.L.; Meazza, C.; Tettoni, K.; Provenzi, M.; Mazzarino, I.; Carli, M. Vinorelbine and low-dose cyclophosphamide in the treatment of pediatric sarcomas. Cancer 2004, 101, 1664–1671. [Google Scholar] [CrossRef]
- Minard-Colin, V.; Ichante, J.L.; Nguyen, L.; Paci, A.; Orbach, D.; Bergeron, C.; Defachelles, A.S.; André, N.; Corradini, N.; Schmitt, C.; et al. Phase II study of vinorelbine and continuous low doses cyclophosphamide in children and young adults with a relapsed or refractory malignant solid tumour: Good tolerance profile and efficacy in rhabdomyosarcoma—A report from the Société Française des Cancers et leucémies de l’Enfant et de l’adolescent (SFCE). Eur. J. Cancer 2012, 48, 2409–2416. [Google Scholar] [CrossRef]
- Marty, M.; Fumoleau, P.; Adenis, A.; Rousseau, Y.; Merrouche, Y.; Robinet, G.; Senac, I.; Puozzo, C. Oral vinorelbine pharmacokinetics and absolute bioavailability study in patients with solid tumors. Ann. Oncol. 2001, 12, 1643–1649. [Google Scholar] [CrossRef]
- Johansen, M.; Kuttesch, J.; Bleyer, W.A.; Krailo, M.; Ames, M.; Madden, T. Phase I Evaluation of Oral and Intravenous Vinorelbine in Pediatric Cancer Patients: A Report from the Children’s Oncology Group. Clin. Cancer Res. 2006, 12, 516–522. [Google Scholar] [CrossRef]
- Williamson, D.; Missiaglia, E.; de Reyniès, A.; Pierron, G.; Thuille, B.; Palenzuela, G.; Thway, K.; Orbach, D.; Laé, M.; Fréneaux, P.; et al. Fusion Gene–Negative Alveolar Rhabdomyosarcoma Is Clinically and Molecularly Indistinguishable From Embryonal Rhabdomyosarcoma. J. Clin. Oncol. 2010, 28, 2151–2158. [Google Scholar] [CrossRef]
- Missiaglia, E.; Williamson, D.; Chisholm, J.; Wirapati, P.; Pierron, G.; Petel, F.; Concordet, J.P.; Thway, K.; Oberlin, O.; Pritchard-Jones, K.; et al. PAX3/FOXO1 Fusion Gene Status Is the Key Prognostic Molecular Marker in Rhabdomyosarcoma and Significantly Improves Current Risk Stratification. J. Clin. Oncol. 2012, 30, 1670–1677. [Google Scholar] [CrossRef]
- Rudzinski, E.R.; Kelsey, A.; Vokuhl, C.; Linardic, C.M.; Shipley, J.; Hettmer, S.; Koscielniak, E.; Hawkins, D.S.; Bisogno, G. Pathology of childhood rhabdomyosarcoma: A consensus opinion document from the Children’s Oncology Group, European Paediatric Soft Tissue Sarcoma Study Group, and the Cooperative Weichteilsarkom Studiengruppe. Pediatr. Blood Cancer 2021, 68, e28798. [Google Scholar] [CrossRef]
- Selfe, J.; Olmos, D.; Al-Saadi, R.; Thway, K.; Chisholm, J.; Kelsey, A.; Shipley, J. Impact of fusion gene status versus histology on risk-stratification for rhabdomyosarcoma: Retrospective analyses of patients on UK trials. Pediatr. Blood Cancer 2017, 64, e26386. [Google Scholar] [CrossRef]
- Davicioni, E.; Anderson, J.R.; Buckley, J.D.; Meyer, W.H.; Triche, T.J. Gene Expression Profiling for Survival Prediction in Pediatric Rhabdomyosarcomas: A Report From the Children’s Oncology Group. J. Clin. Oncol. 2010, 28, 1240–1246. [Google Scholar] [CrossRef]
- Costa, D.S.J.; Mercieca-Bebber, R.; Rutherford, C.; Tait, M.-A.; King, M.T. How is quality of life defined and assessed in published research? Qual. Life Res. 2021, 30, 2109–2121. [Google Scholar] [CrossRef]
- Kluetz, P.G.; Slagle, A.; Papadopoulos, E.J.; Johnson, L.L.; Donoghue, M.; Kwitkowski, V.E.; Chen, W.H.; Sridhara, R.; Farrell, A.T.; Keegan, P.; et al. Focusing on Core Patient-Reported Outcomes in Cancer Clinical Trials: Symptomatic Adverse Events, Physical Function, and Disease-Related Symptoms. Clin. Cancer Res. 2016, 22, 1553–1558. [Google Scholar] [CrossRef]
- Leiser, D.; Calaminus, G.; Malyapa, R.; Bojaxhiu, B.; Albertini, F.; Kliebsch, U.; Mikroutsikos, L.; Morach, P.; Bolsi, A.; Walser, M.; et al. Tumour control and Quality of Life in children with rhabdomyosarcoma treated with pencil beam scanning proton therapy. Radiother. Oncol. 2016, 120, 163–168. [Google Scholar] [CrossRef]
- Martelli, H.; Borrego, P.; Guérin, F.; Boubnova, J.; Minard-Colin, V.; Dumas, I.; Chargari, C.; Haie-Meder, C. Quality of life and functional outcome of male patients with bladder–prostate rhabdomyosarcoma treated with conservative surgery and brachytherapy during childhood. Brachytherapy 2016, 15, 306–311. [Google Scholar] [CrossRef]
- Varni, J.W.; Burwinkle, T.M.; Seid, M.; Skarr, D. The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambul. Pediatr. 2003, 3, 329–341. [Google Scholar] [CrossRef]
- Giesinger, J.M.; Kuijpers, W.; Young, T.; Tomaszewski, K.A.; Friend, E.; Zabernigg, A.; Holzner, B.; Aaronson, N.K. Thresholds for clinical importance for four key domains of the EORTC QLQ-C30: Physical functioning, emotional functioning, fatigue and pain. Health Qual. Life Outcomes 2016, 14, 87. [Google Scholar] [CrossRef]
- van Gorp, M.; Grootenhuis, M.A.; Darlington, A.S.; Wakeling, S.; Jenney, M.; Merks, J.H.M.; Hjalgrim, L.L.; Adams, M. Patient Reported Outcomes and Measures in Children with Rhabdomyosarcoma. Cancers 2023, 15, 420. [Google Scholar] [CrossRef]
- van Ewijk, R.; Vaarwerk, B.; Breunis, W.B.; Schoot, R.A.; Ter Horst, S.A.J.; van Rijn, R.R.; van der Lee, J.H.; Merks, J.H.M. The Value of Early Tumor Size Response to Chemotherapy in Pediatric Rhabdomyosarcoma. Cancers 2021, 13, 510. [Google Scholar] [CrossRef]
- Partridge, S.C.; Zhang, Z.; Newitt, D.C.; Gibbs, J.E.; Chenevert, T.L.; Rosen, M.A.; Bolan, P.J.; Marques, H.S.; Romanoff, J.; Cimino, L.; et al. Diffusion-weighted MRI Findings Predict Pathologic Response in Neoadjuvant Treatment of Breast Cancer: The ACRIN 6698 Multicenter Trial. Radiology 2018, 289, 618–627. [Google Scholar] [CrossRef] [PubMed]
- Vos, J.L.; Zuur, C.L.; Smit, L.A.; de Boer, J.P.; Al-Mamgani, A.; van den Brekel, M.W.M.; Haanen, J.B.A.G.; Vogel, W.V. [18F]FDG-PET accurately identifies pathological response early upon neoadjuvant immune checkpoint blockade in head and neck squamous cell carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2010–2022. [Google Scholar] [CrossRef]
- Norman, G.; Fayter, D.; Lewis-Light, K.; McHugh, K.; Levine, D.; Phillips, B. Mind the gap: Extent of use of diffusion-weighted MRI in children with rhabdomyosarcoma. Pediatr. Radiol. 2015, 45, 778–781. [Google Scholar] [CrossRef]
- Norman, G.; Fayter, D.; Lewis-Light, K.; Chisholm, J.; McHugh, K.; Levine, D.; Jenney, M.; Mandeville, H.; Gatz, S.; Phillips, B. An emerging evidence base for PET-CT in the management of childhood rhabdomyosarcoma: Systematic review. BMJ Open 2015, 5, e006030. [Google Scholar] [CrossRef]
- O, J.H.; Lodge, M.A.; Wahl, R.L. Practical PERCIST: A Simplified Guide to PET Response Criteria in Solid Tumors 1.0. Radiology 2016, 280, 576–584. [Google Scholar] [CrossRef]
- Wahl, R.L.; Jacene, H.; Kasamon, Y.; Lodge, M.A. From RECIST to PERCIST: Evolving Considerations for PET Response Criteria in Solid Tumors. J. Nucl. Med. 2009, 50, 122S–150S. [Google Scholar] [CrossRef]
- Pinker, K.; Riedl, C.; Weber, W.A. Evaluating tumor response with FDG PET: Updates on PERCIST, comparison with EORTC criteria and clues to future developments. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 55–66. [Google Scholar] [CrossRef]
- Barrington, S.F.; Mikhaeel, N.G.; Kostakoglu, L.; Meignan, M.; Hutchings, M.; Müeller, S.P.; Schwartz, L.H.; Zucca, E.; Fisher, R.I.; Trotman, J.; et al. Role of Imaging in the Staging and Response Assessment of Lymphoma: Consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J. Clin. Oncol. 2014, 32, 3048–3058. [Google Scholar] [CrossRef]
- McCague, C.; Ramlee, S.; Reinius, M.; Selby, I.; Hulse, D.; Piyatissa, P.; Bura, V.; Crispin-Ortuzar, M.; Sala, E.; Woitek, R. Introduction to radiomics for a clinical audience. Clin. Radiol. 2023, 78, 83–98. [Google Scholar] [CrossRef]
- van Timmeren, J.E.; Cester, D.; Tanadini-Lang, S.; Alkadhi, H.; Baessler, B. Radiomics in medical imaging—‘how-to’ guide and critical reflection. Insights Imaging 2020, 11, 91. [Google Scholar] [CrossRef]
- Kelly, S.M.; Effeney, R.; Gaze, M.N.; Bernier-Chastagner, V.; Blondeel, A.; Clementel, E.; Corning, C.; Dieckmann, K.; Essiaf, S.; Gandola, L.; et al. QUARTET: A SIOP Europe project for quality and excellence in radiotherapy and imaging for children and adolescents with cancer. Eur. J. Cancer 2022, 172, 209–220. [Google Scholar] [CrossRef] [PubMed]
- van Ewijk, R.; Schoot, R.A.; Sparber-Sauer, M.; Ter Horst, S.A.J.; Jehanno, N.; Borgwardt, L.; de Keizer, B.; Merks, J.H.M.; de Luca, A.; McHugh, K.; et al. European guideline for imaging in paediatric and adolescent rhabdomyosarcoma—Joint statement by the European Paediatric Soft Tissue Sarcoma Study Group, the Cooperative Weichteilsarkom Studiengruppe and the Oncology Task Force of the European Society of Paediatric Radiology. Pediatr. Radiol. 2021, 51, 1940–1951. [Google Scholar] [CrossRef] [PubMed]
- Vali, R.; Alessio, A.; Balza, R.; Borgwardt, L.; Bar-Sever, Z.; Czachowski, M.; Jehanno, N.; Kurch, L.; Pandit-Taskar, N.; Parisi, M.; et al. SNMMI Procedure Standard/EANM Practice Guideline on Pediatric 18F-FDG PET/CT for Oncology 1.0. J. Nucl. Med. 2021, 62, 99–110. [Google Scholar] [CrossRef] [PubMed]

| Risk Group | Subgroup | Fusion Status | IRS Group | Site | Nodal Status | Size or Age |
|---|---|---|---|---|---|---|
| Low-risk | A | Negative | I | Any | N0 | Both favourable |
| Standard risk | B | Negative | I | Any | N0 | One of both favourable |
| C | Negative | II, III | Favourable | N0 | Any | |
| High-risk | D | Negative | II, III | Unfavourable | N0 | Any |
| E | Negative | II, III | Any | N1 | Any | |
| F | Positive | I, II, III | Any | N0 | Any | |
| Very high-risk | G | Positive | II, III | Any | N1 | Any |
| H | Any | IV | Any | Any | Any |
| Question | Description |
|---|---|
| 1 | Can outcomes be improved by utilising new combinations of systemic anti-cancer therapies, including the addition of new biologically targeted drugs in:
|
| 2 | Can outcomes be improved through optimising radiotherapy schedules?
|
| 3 | Can prolongation of maintenance therapy reduce the risk of relapse and improve OS for patients with HR and VHR disease? |
| 4 | Can PAX-FOXO1 fusion status be utilised instead of histological diagnosis to improve treatment stratification? |
| 5 | Can [18F]FDG PET-CT and the apparent diffusion coefficient (ADC) evaluated by the DW-MRI response assessment following induction chemotherapy be used as prognostic biomarkers for local control and/or survival? |
| 6 | Can the DWI-MRI response assessment following induction chemotherapy be used as a prognostic biomarker for local control and/or survival? |
| Randomisation | Minimum Number of Patients in Total | Assumed Baseline Event Free Rate for the Primary Outcome, 3-Year (%) | |
|---|---|---|---|
| Radiotherapy | 1a | 350 | 80 |
| 1b | 315 | 79 | |
| 1c | 350 | 72 | |
| 2 | 210 | 40 | |
| Newly diagnosed chemotherapy | Very high-risk | 370 | 35 |
| High-risk | 470 | 65 | |
| Very high-risk maintenance | 260 | 35 to 45 | |
| High-risk maintenance | 240 | 65 | |
| Relapse | 260 for the regorafenib questions 420 in 7 years with additional arms | 30, 1 year |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chisholm, J.; Mandeville, H.; Adams, M.; Minard-Collin, V.; Rogers, T.; Kelsey, A.; Shipley, J.; van Rijn, R.R.; de Vries, I.; van Ewijk, R.; et al. Frontline and Relapsed Rhabdomyosarcoma (FaR-RMS) Clinical Trial: A Report from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG). Cancers 2024, 16, 998. https://doi.org/10.3390/cancers16050998
Chisholm J, Mandeville H, Adams M, Minard-Collin V, Rogers T, Kelsey A, Shipley J, van Rijn RR, de Vries I, van Ewijk R, et al. Frontline and Relapsed Rhabdomyosarcoma (FaR-RMS) Clinical Trial: A Report from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG). Cancers. 2024; 16(5):998. https://doi.org/10.3390/cancers16050998
Chicago/Turabian StyleChisholm, Julia, Henry Mandeville, Madeleine Adams, Veronique Minard-Collin, Timothy Rogers, Anna Kelsey, Janet Shipley, Rick R. van Rijn, Isabelle de Vries, Roelof van Ewijk, and et al. 2024. "Frontline and Relapsed Rhabdomyosarcoma (FaR-RMS) Clinical Trial: A Report from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG)" Cancers 16, no. 5: 998. https://doi.org/10.3390/cancers16050998
APA StyleChisholm, J., Mandeville, H., Adams, M., Minard-Collin, V., Rogers, T., Kelsey, A., Shipley, J., van Rijn, R. R., de Vries, I., van Ewijk, R., de Keizer, B., Gatz, S. A., Casanova, M., Hjalgrim, L. L., Firth, C., Wheatley, K., Kearns, P., Liu, W., Kirkham, A., ... Jenney, M. (2024). Frontline and Relapsed Rhabdomyosarcoma (FaR-RMS) Clinical Trial: A Report from the European Paediatric Soft Tissue Sarcoma Study Group (EpSSG). Cancers, 16(5), 998. https://doi.org/10.3390/cancers16050998









