Reduced Risk of Hepatocellular Carcinoma in Patients with Chronic Hepatitis B Receiving Long-Term Besifovir Therapy
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Primary and Secondary Endpoints
2.3. Clinical Assessment and Definitions
2.4. Models for the Prediction of HCCs
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Patients
3.2. Antiviral Responses and Changes in Fibrosis Indexes
3.3. Incidence of HCC and Characteristics of the Patients who Developed HCCs
3.4. Identification of Risk Factors on the HCC Development
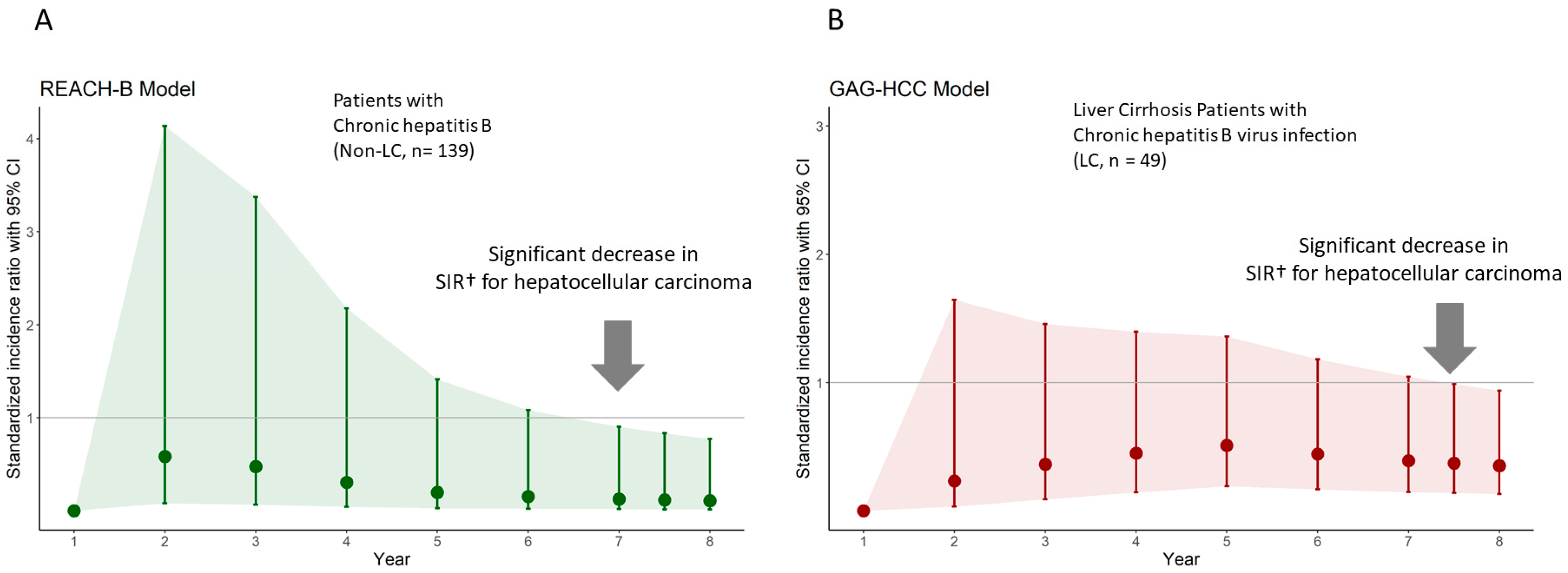
3.5. The Influence of BSV Treatment on the Prediction of HCCs
3.6. Risk Scores on HCC Development and Performance of Prediction Models
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lin, C.L.; Kao, J.H. Development of hepatocellular carcinoma in treated and untreated patients with chronic hepatitis B virus infection. Clin. Mol. Hepatol. 2023, 29, 605–622. [Google Scholar] [CrossRef]
- Yuen, M.F.; Tanaka, Y.; Fong, D.Y.; Fung, J.; Wong, D.K.; Yuen, J.C.; But, D.Y.; Chan, A.O.; Wong, B.C.; Mizokami, M.; et al. Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. J. Hepatol. 2009, 50, 80–88. [Google Scholar] [CrossRef]
- Wong, V.W.; Chan, S.L.; Mo, F.; Chan, T.C.; Loong, H.H.; Wong, G.L.; Lui, Y.Y.; Chan, A.T.; Sung, J.J.; Yeo, W.; et al. Clinical scoring system to predict hepatocellular carcinoma in chronic hepatitis B carriers. J. Clin. Oncol. 2010, 28, 1660–1665. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.I.; Yuen, M.F.; Chan, H.L.; Han, K.H.; Chen, P.J.; Kim, D.Y.; Ahn, S.H.; Chen, C.J.; Wong, V.W.; Seto, W.K.; et al. Risk estimation for hepatocellular carcinoma in chronic hepatitis B (REACH-B): Development and validation of a predictive score. Lancet Oncol. 2011, 12, 568–574. [Google Scholar] [CrossRef]
- Papatheodoridis, G.; Dalekos, G.; Sypsa, V.; Yurdaydin, C.; Buti, M.; Goulis, J.; Calleja, J.L.; Chi, H.; Manolakopoulos, S.; Mangia, G.; et al. PAGE-B predicts the risk of developing hepatocellular carcinoma in Caucasians with chronic hepatitis B on 5-year antiviral therapy. J. Hepatol. 2016, 64, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Sohn, W.; Cho, J.Y.; Kim, J.H.; Lee, J.I.; Kim, H.J.; Woo, M.A.; Jung, S.H.; Paik, Y.H. Risk score model for the development of hepatocellular carcinoma in treatment-naïve patients receiving oral antiviral treatment for chronic hepatitis B. Clin. Mol. Hepatol. 2017, 23, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Fan, R.; Papatheodoridis, G.; Sun, J.; Innes, H.; Toyoda, H.; Xie, Q.; Mo, S.; Sypsa, V.; Guha, I.N.; Kumada, T.; et al. aMAP risk score predicts hepatocellular carcinoma development in patients with chronic hepatitis. J. Hepatol. 2020, 73, 1368–1378. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.R.; Loomba, R.; Berg, T.; Aguilar Schall, R.E.; Yee, L.J.; Dinh, P.V.; Flaherty, J.F.; Martins, E.B.; Therneau, T.M.; Jacobson, I.; et al. Impact of long-term tenofovir disoproxil fumarate on incidence of hepatocellular carcinoma in patients with chronic hepatitis B. Cancer 2015, 121, 3631–3638. [Google Scholar] [CrossRef]
- Hosaka, T.; Suzuki, F.; Kobayashi, M.; Seko, Y.; Kawamura, Y.; Sezaki, H.; Akuta, N.; Suzuki, Y.; Saitoh, S.; Arase, Y.; et al. Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virus infection. Hepatology 2013, 58, 98–107. [Google Scholar] [CrossRef]
- Tan, D.J.H.; Ng, C.H.; Tay, P.W.L.; Syn, N.; Muthiah, M.D.; Lim, W.H.; Tang, A.S.P.; Lim, K.E.; Lim, G.E.H.; Tamaki, N.; et al. Risk of Hepatocellular Carcinoma With Tenofovir vs Entecavir Treatment for Chronic Hepatitis B Virus: A Reconstructed Individual Patient Data Meta-analysis. JAMA Netw. Open 2022, 5, e2219407. [Google Scholar] [CrossRef]
- Choi, J.; Kim, H.J.; Lee, J.; Cho, S.; Ko, M.J.; Lim, Y.S. Risk of Hepatocellular Carcinoma in Patients Treated With Entecavir vs Tenofovir for Chronic Hepatitis B: A Korean Nationwide Cohort Study. JAMA Oncol. 2019, 5, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Song, J.E.; Park, J.Y. Besifovir dipivoxil maleate: A novel antiviral agent with low toxicity and high genetic barriers for chronic hepatitis B. Expert Opin. Pharmacother. 2021, 22, 2427–2433. [Google Scholar] [CrossRef] [PubMed]
- Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for management of chronic hepatitis B. Clin. Mol. Hepatol. 2019, 25, 93–159. [Google Scholar] [CrossRef] [PubMed]
- Yim, H.J.; Kim, W.; Ahn, S.H.; Jung, Y.K.; Um, S.H.; Sohn, J.H.; Jang, J.Y.; Kim, D.J.; Park, E.S.; Jin, S.Y.; et al. Besifovir therapy improves hepatic histology and reduces covalently closed circular DNA in chronic hepatitis B patients. J. Gastroenterol. Hepatol. 2022, 37, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Bianca, C.; Sidhartha, E.; Tiribelli, C.; El-Khobar, K.E.; Sukowati, C.H.C. Role of hepatitis B virus in development of hepatocellular carcinoma: Focus on covalently closed circular DNA. World J. Hepatol. 2022, 14, 866–884. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, Y.D.; Lee, M.; Jun, B.G.; Kim, T.S.; Suk, K.T.; Kang, S.H.; Kim, M.Y.; Cheon, G.J.; Kim, D.J.; et al. Modified PAGE-B score predicts the risk of hepatocellular carcinoma in Asians with chronic hepatitis B on antiviral therapy. J. Hepatol. 2018, 69, 1066–1073. [Google Scholar] [CrossRef]
- Hsu, Y.C.; Yip, T.C.; Ho, H.J.; Wong, V.W.; Huang, Y.T.; El-Serag, H.B.; Lee, T.Y.; Wu, M.S.; Lin, J.T.; Wong, G.L.; et al. Development of a scoring system to predict hepatocellular carcinoma in Asians on antivirals for chronic hepatitis B. J. Hepatol. 2018, 69, 278–285. [Google Scholar] [CrossRef]
- Yang, H.I.; Yeh, M.L.; Wong, G.L.; Peng, C.Y.; Chen, C.H.; Trinh, H.N.; Cheung, K.S.; Xie, Q.; Su, T.H.; Kozuka, R.; et al. Real-World Effectiveness From the Asia Pacific Rim Liver Consortium for HBV Risk Score for the Prediction of Hepatocellular Carcinoma in Chronic Hepatitis B Patients Treated With Oral Antiviral Therapy. J. Infect. Dis. 2020, 221, 389–399. [Google Scholar] [CrossRef]
- Yu, J.H.; Suh, Y.J.; Jin, Y.J.; Heo, N.Y.; Jang, J.W.; You, C.R.; An, H.Y.; Lee, J.W. Prediction model for hepatocellular carcinoma risk in treatment-naive chronic hepatitis B patients receiving entecavir/tenofovir. Eur. J. Gastroenterol. Hepatol. 2019, 31, 865–872. [Google Scholar] [CrossRef]
- Yuen, M.F.; Ahn, S.H.; Lee, K.S.; Um, S.H.; Cho, M.; Yoon, S.K.; Lee, J.W.; Park, N.H.; Kweon, Y.O.; Sohn, J.H.; et al. Two-year treatment outcome of chronic hepatitis B infection treated with besifovir vs. entecavir: Results from a multicentre study. J. Hepatol. 2015, 62, 526–532. [Google Scholar] [CrossRef]
- Triolo, M.; Della Corte, C.; Colombo, M. Impact of HBV therapy on the incidence of hepatocellular carcinoma. Liver Int. 2014, 34 (Suppl. S1), 139–145. [Google Scholar] [CrossRef]
- Rinaldi, L.; Giorgione, C.; Mormone, A.; Esposito, F.; Rinaldi, M.; Berretta, M.; Marfella, R.; Romano, C. Non-Invasive Measurement of Hepatic Fibrosis by Transient Elastography: A Narrative Review. Viruses 2023, 15, 1730. [Google Scholar] [CrossRef]
- Foucher, J.; Chanteloup, E.; Vergniol, J.; Castera, L.; Le Bail, B.; Adhoute, X.; Bertet, J.; Couzigou, P.; de Ledinghen, V. Diagnosis of cirrhosis by transient elastography (FibroScan): A prospective study. Gut 2006, 55, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Ucar, F.; Sezer, S.; Ginis, Z.; Ozturk, G.; Albayrak, A.; Basar, O.; Ekiz, F.; Coban, S.; Yuksel, O.; Armutcu, F.; et al. APRI, the FIB-4 score, and Forn’s index have noninvasive diagnostic value for liver fibrosis in patients with chronic hepatitis B. Eur. J. Gastroenterol. Hepatol. 2013, 25, 1076–1081. [Google Scholar] [CrossRef] [PubMed]
- Wai, C.T.; Greenson, J.K.; Fontana, R.J.; Kalbfleisch, J.D.; Marrero, J.A.; Conjeevaram, H.S.; Lok, A.S. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 2003, 38, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Sterling, R.K.; Lissen, E.; Clumeck, N.; Sola, R.; Correa, M.C.; Montaner, J.; Sulkowski, M.S.; Torriani, F.J.; Dieterich, D.T.; Thomas, D.L.; et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 2006, 43, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Murata, K.; Mizokami, M. Possible biological mechanisms of entecavir versus tenofovir disoproxil fumarate on reducing the risk of hepatocellular carcinoma. J. Gastroenterol. Hepatol. 2023, 38, 683–691. [Google Scholar] [CrossRef]
- Murata, K.; Asano, M.; Matsumoto, A.; Sugiyama, M.; Nishida, N.; Tanaka, E.; Inoue, T.; Sakamoto, M.; Enomoto, N.; Shirasaki, T.; et al. Induction of IFN-lambda3 as an additional effect of nucleotide, not nucleoside, analogues: A new potential target for HBV infection. Gut 2018, 67, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Murata, K.; Tsukuda, S.; Suizu, F.; Kimura, A.; Sugiyama, M.; Watashi, K.; Noguchi, M.; Mizokami, M. Immunomodulatory Mechanism of Acyclic Nucleoside Phosphates in Treatment of Hepatitis B Virus Infection. Hepatology 2020, 71, 1533–1545. [Google Scholar] [CrossRef] [PubMed]

| Variable § | All Patients (n = 188) | Non-Cirrhotic Patients (n = 139) | Liver Cirrhosis (n = 49) | p-Value | |
|---|---|---|---|---|---|
| Male sex, n (%) | 120 (63.83) | 87 (62.59) | 33 (67.35) | 0.551 | |
| Age (years) | 45.2 ± 10.96 | 43.5 ±10.80 | 50.2 ± 9.94 | <0.001 | |
| Positive HBeAg, n (%) | 112 (59.57) | 87 (62.59) | 25 (51.02) | 0.156 | |
| HBV DNA (log IU/mL) | 6.40 ± 1.63 | 6.51 ± 1.63 | 6.08 ± 1.60 | 0.075 | |
| ALT (U/L) | 115.65 ± 120.46 | 117.63 ± 126.80 | 110.04 ± 101.30 | 0.767 | |
| AST (U/L) | 77.91 ± 68.90 | 73.15 ± 64.66 | 91.43 ± 78.89 | 0.386 | |
| DM, n (%) | 35 (18.5) | 18 (13.0) | 17 (34.7) | 0.001 | |
| Platelet (103/μL) | 189.77 ± 67.07 | 202.39 ± 52.39 | 153.98 ± 88.69 | <0.001 | |
| Bilirubin (mg/dL) | 0.67 ± 0.33 | 0.66 ± 0.35 | 0.69 ± 0.29 | 0.375 | |
| Albumin (g/dL) | 4.25 ± 0.31 | 4.28 ± 0.30 | 4.17 ± 0.32 | 0.045 | |
| AFP (ng/mL) | 16.80 ± 59.04 | 9.96 ± 18.83 | 36.19 ± 109.73 | <0.001 | |
| APRI | 1.30 ± 1.47 | 1.05 ± 0.94 | 2.04 ± 2.00 | 0.003 | |
| Fib-4 | 2.06 ± 1.79 | 1.57 ± 0.76 | 3.47 ± 2.83 | <0.001 | |
| Prognostic scores | GAG-HCC | 84.25 ± 20.99 | 74.07 ± 12.41 | 113.15 ± 11.03 | <0.001 |
| REACH-B | 10.88 ± 2.16 | 10.65 ± 2.19 | 11.55 ± 1.94 | 0.012 | |
| PAGE-B | 11.63 ± 4.98 | 10.68 ± 4.99 | 14.39 ± 3.88 | <0.001 | |
| mPAGE-B | 8.97 ± 3.11 | 8.33 ± 3.08 | 10.78 ± 2.41 | <0.001 | |
| CAMD | 7.78 ± 5.08 | 5.50 ± 3.68 | 14.24 ± 1.91 | <0.001 | |
| HCC-RESCUE | 60.79 ± 17.86 | 52.86 ± 12.47 | 83.29 ± 9.81 | <0.001 | |
| REAL-B | 3.90 ± 2.07 | 3.01 ± 1.45 | 6.43 ± 1.35 | <0.001 | |
| AASL | 8.88 ± 5.89 | 5.69 ± 2.52 | 17.92 ± 2.00 | <0.001 |
| Univariable Analysis | Multivariable Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| HR | Lower | Upper | p-Value | HR | Lower | Upper | p-Value | |
| Cirrhosis | 13.629 | 1.523 | 121.957 | 0.020 | 11.125 | 1.232 | 100.447 | 0.032 |
| Age (≥50 years) | 7.368 | 0.824 | 65.913 | 0.074 | 5.579 | 0.618 | 50.366 | 0.126 |
| Male | 2.085 | 0.233 | 18.655 | 0.511 | ||||
| DM | 0.997 | 0.111 | 8.923 | 0.998 | ||||
| HBeAg positive | 5.956 | 0.666 | 53.295 | 0.111 | ||||
| HBV DNA | 0.658 | 0.395 | 1.098 | 0.109 | ||||
| Platelet | 1.000 | 0.986 | 1.014 | 0.984 | ||||
| Albumin | 1.627 | 0.090 | 29.476 | 0.742 | ||||
| AFP | 0.996 | 0.965 | 1.029 | 0.822 | ||||
| AST | 0.999 | 0.984 | 1.013 | 0.856 | ||||
| ALT | 0.990 | 0.968 | 1.011 | 0.339 | ||||
| Year | Observation (Cumulative No. of Cases) | Prediction | SIR (Observation/ Prediction) | 95% CI Lower Limit | 95% CI Upper Limit | p-Value |
|---|---|---|---|---|---|---|
| 1 | 0 | 0.73 | 0 | 0 | - | 1.000 |
| 2 | 1 | 1.72 | 0.583 | 0.082 | 4.135 | 0.589 |
| 3 | 1 | 2.10 | 0.475 | 0.067 | 3.375 | 0.457 |
| 4 | 1 | 3.26 | 0.306 | 0.043 | 2.175 | 0.237 |
| 5 | 1 | 5.01 | 0.199 | 0.028 | 1.416 | 0.107 |
| 6 | 1 | 6.55 | 0.153 | 0.022 | 1.084 | 0.060 |
| 7 | 1 | 7.84 | 0.128 | 0.018 | 0.905 | 0.039 |
| 7.5 | 1 | 8.51 | 0.118 | 0.017 | 0.834 | 0.032 |
| 8 | 1 | 9.18 | 0.109 | 0.015 | 0.773 | 0.027 |
| Year | Observation (Cumulative no. of Cases) | Prediction | SIR (Observation/ Prediction) | 95% CI Lower Limit | 95% CI Upper Limit | p-Value |
|---|---|---|---|---|---|---|
| 1 | 0 | 3.14 | 0 | 0 | . | 1 |
| 2 | 1 | 4.31 | 0.232 | 0.033 | 1.646 | 0.144 |
| 3 | 2 | 5.49 | 0.364 | 0.091 | 1.457 | 0.153 |
| 4 | 3 | 6.66 | 0.450 | 0.145 | 1.396 | 0.167 |
| 5 | 4 | 7.84 | 0.510 | 0.192 | 1.359 | 0.178 |
| 6 | 4 | 9.02 | 0.444 | 0.167 | 1.182 | 0.104 |
| 7 | 4 | 10.19 | 0.392 | 0.147 | 1.046 | 0.061 |
| 7.5 | 4 | 10.78 | 0.371 | 0.139 | 0.989 | 0.047 |
| 8 | 4 | 11.37 | 0.352 | 0.132 | 0.938 | 0.037 |
| Cox’s Proportional Hazard Regression Model | AUROC | ||||||
|---|---|---|---|---|---|---|---|
| HR | Lower | Upper | p-Value | Value | Lower | Upper | |
| PAGE-B | 1.195 | 0.957 | 1.491 | 0.116 | 0.698 | 0.385 | 1.000 |
| mPAGE-B | 1.480 | 1.006 | 2.177 | 0.047 | 0.771 | 0.508 | 1.000 |
| REAL-B | 1.872 | 1.154 | 3.037 | 0.011 | 0.866 | 0.806 | 0.925 |
| HCC-RESCUE | 1.127 | 1.041 | 1.221 | 0.003 | 0.924 | 0.851 | 0.998 |
| CAMD | 1.573 | 1.132 | 2.188 | 0.007 | 0.912 | 0.832 | 0.991 |
| AASL | 1.345 | 1.068 | 1.693 | 0.012 | 0.909 | 0.821 | 0.998 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yim, H.J.; Kang, S.H.; Jung, Y.K.; Ahn, S.H.; Kim, W.; Yang, J.M.; Jang, J.Y.; Kweon, Y.O.; Cho, Y.K.; Kim, Y.J.; et al. Reduced Risk of Hepatocellular Carcinoma in Patients with Chronic Hepatitis B Receiving Long-Term Besifovir Therapy. Cancers 2024, 16, 887. https://doi.org/10.3390/cancers16050887
Yim HJ, Kang SH, Jung YK, Ahn SH, Kim W, Yang JM, Jang JY, Kweon YO, Cho YK, Kim YJ, et al. Reduced Risk of Hepatocellular Carcinoma in Patients with Chronic Hepatitis B Receiving Long-Term Besifovir Therapy. Cancers. 2024; 16(5):887. https://doi.org/10.3390/cancers16050887
Chicago/Turabian StyleYim, Hyung Joon, Seong Hee Kang, Young Kul Jung, Sang Hoon Ahn, Won Kim, Jin Mo Yang, Jae Young Jang, Yong Oh Kweon, Yong Kyun Cho, Yoon Jun Kim, and et al. 2024. "Reduced Risk of Hepatocellular Carcinoma in Patients with Chronic Hepatitis B Receiving Long-Term Besifovir Therapy" Cancers 16, no. 5: 887. https://doi.org/10.3390/cancers16050887
APA StyleYim, H. J., Kang, S. H., Jung, Y. K., Ahn, S. H., Kim, W., Yang, J. M., Jang, J. Y., Kweon, Y. O., Cho, Y. K., Kim, Y. J., Hong, G. Y., Kim, D. J., Sohn, J. H., Lee, J. W., Park, S. J., Yim, S. Y., Park, J. K., & Um, S. H. (2024). Reduced Risk of Hepatocellular Carcinoma in Patients with Chronic Hepatitis B Receiving Long-Term Besifovir Therapy. Cancers, 16(5), 887. https://doi.org/10.3390/cancers16050887









