The Added Value of Controlling Nutritional Status (Conut) Score for Preoperative Counselling on Significant Early Loss of Renal Function After Radical Nephrectomy for Renal Cell Carcinoma
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients Characteristics
2.2. Endpoints
2.3. Statistical Analysis
3. Results
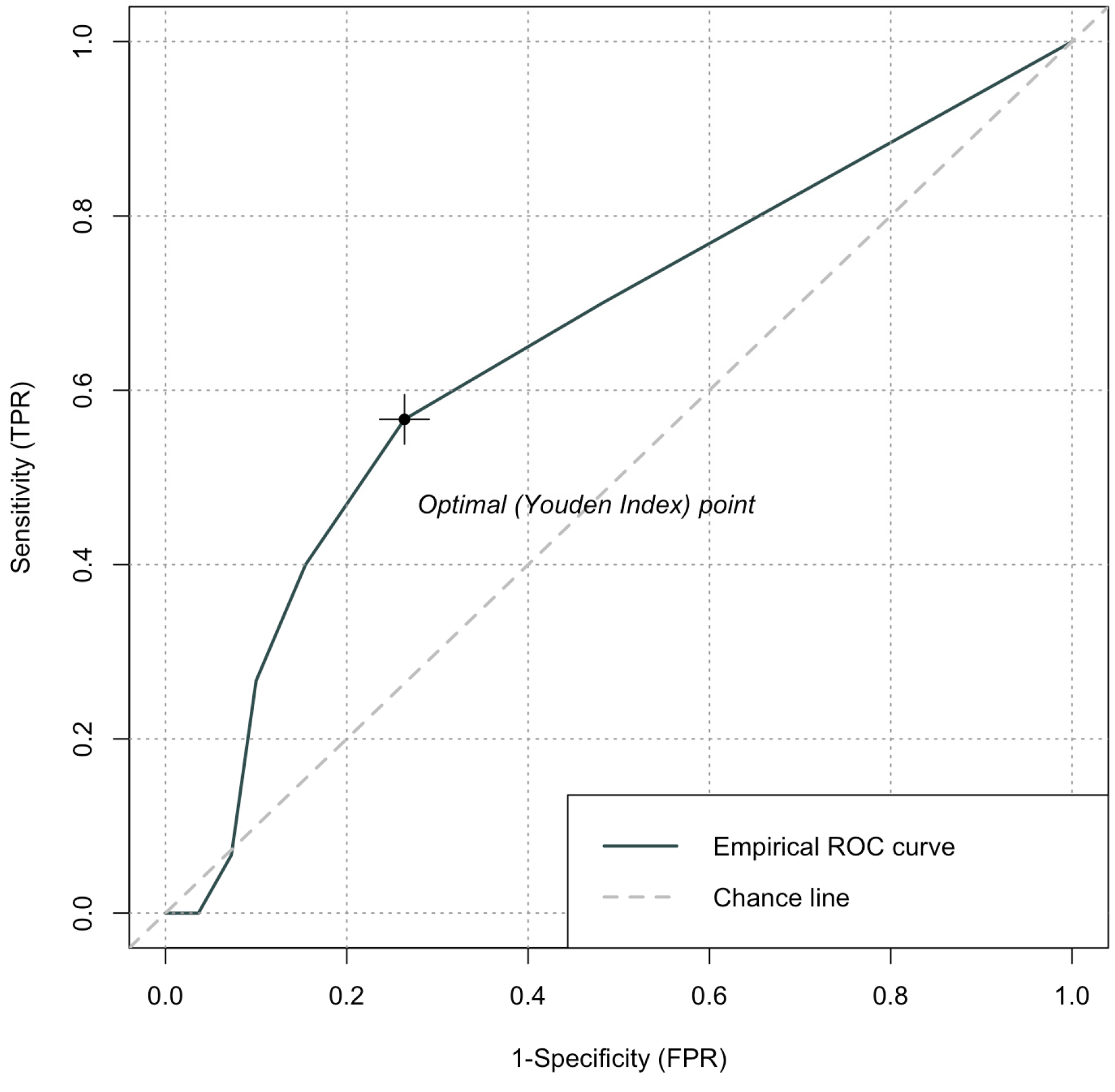
3.1. Determination of CONUT Score and Cut-Off Value
3.2. Clinico-Pathological and Surgical Features of the Study Cohort
3.3. Risk Factors Associated with Clinically Significant eGFR Decline
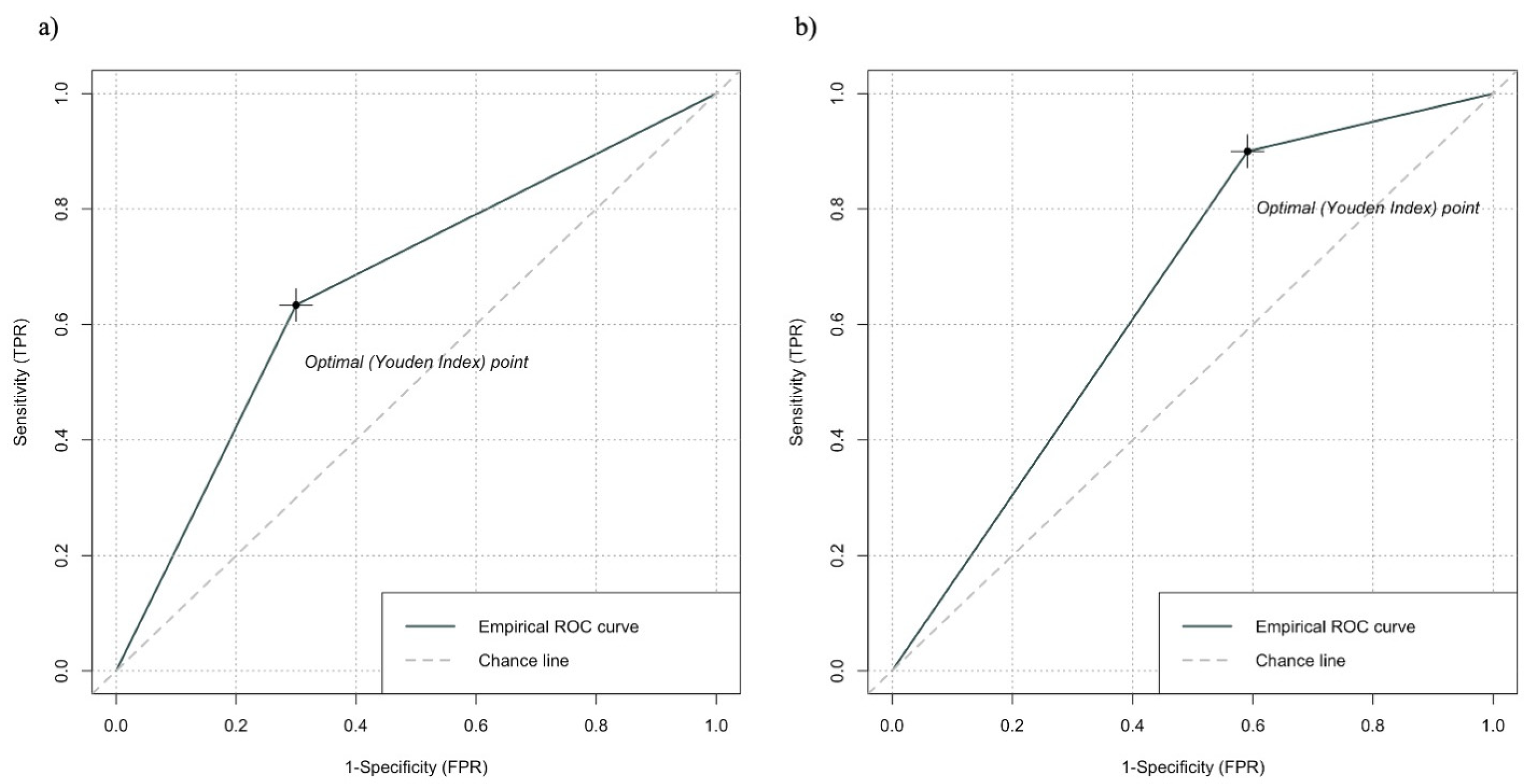
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Traunero, F.; Claps, F.; Silvestri, T.; Mir, M.C.; Ongaro, L.; Rizzo, M.; Piasentin, A.; Liguori, G.; Vedovo, F.; Celia, A.; et al. Reliable Prediction of Post-Operative Complications’ Rate Using the G8 Screening Tool: A Prospective Study on Elderly Patients Undergoing Surgery for Kidney Cancer. J. Clin. Med. 2022, 11, 3785. [Google Scholar] [CrossRef] [PubMed]
- European Association of Urology Guidelines on Renal Cell Carcinoma: The 2022 Update. Available online: https://www.sciencedirect.com/science/article/pii/S0302283822016761 (accessed on 20 September 2024).
- Piasentin, A.; Claps, F.; Silvestri, T.; Rebez, G.; Traunero, F.; Mir, M.C.; Rizzo, M.; Celia, A.; Cicero, C.; Urbani, M.; et al. Assessing Trifecta Achievement after Percutaneous Cryoablation of Small Renal Masses: Results from a Multi-Institutional Collaboration. Medicina 2022, 58, 1041. [Google Scholar] [CrossRef] [PubMed]
- Pecoraro, A.; Campi, R.; Bertolo, R.; Mir, M.C.; Marchioni, M.; Serni, S.; Joniau, S.; Van Poppel, H.; Albersen, M.; Roussel, E. Estimating Postoperative Renal Function After Surgery for Nonmetastatic Renal Masses: A Systematic Review of Available Prediction Models. Eur. Urol. Oncol. 2023, 6, 137–147. [Google Scholar] [CrossRef] [PubMed]
- Bossi, P.; Delrio, P.; Mascheroni, A.; Zanetti, M. The Spectrum of Malnutrition/Cachexia/Sarcopenia in Oncology According to Different Cancer Types and Settings: A Narrative Review. Nutrients 2021, 13, 1980. [Google Scholar] [CrossRef]
- Bullock, A.F.; Greenley, S.L.; McKenzie, G.A.G.; Paton, L.W.; Johnson, M.J. Relationship between Markers of Malnutrition and Clinical Outcomes in Older Adults with Cancer: Systematic Review, Narrative Synthesis and Meta-Analysis. Eur. J. Clin. Nutr. 2020, 74, 1519–1535. [Google Scholar] [CrossRef]
- Pressoir, M.; Desné, S.; Berchery, D.; Rossignol, G.; Poiree, B.; Meslier, M.; Traversier, S.; Vittot, M.; Simon, M.; Gekiere, J.P.; et al. Prevalence, Risk Factors and Clinical Implications of Malnutrition in French Comprehensive Cancer Centres. Br. J. Cancer 2010, 102, 966–971. [Google Scholar] [CrossRef]
- Claps, F.; Pavan, N.; Boltri, M.; Traunero, F.; Liguori, G.; Trombetta, C. The Role of Preoperative Controlling Nutritional Status (CONUT) Score in the Assessment of Survival Outcomes in Patients with Muscle Invasive Bladder Cancer (MIBC) Treated with Radical Cystectomy: A Pilot Study. Eur. Urol. Suppl. 2018, 17, e1029. [Google Scholar] [CrossRef]
- Ishihara, H.; Kondo, T.; Yoshida, K.; Omae, K.; Takagi, T.; Iizuka, J.; Tanabe, K. Preoperative Controlling Nutritional Status (CONUT) Score as a Novel Predictive Biomarker of Survival in Patients with Localized Urothelial Carcinoma of the Upper Urinary Tract Treated with Radical Nephroureterectomy. Urol. Oncol. Semin. Orig. Investig. 2017, 35, 539.e9–539.e16. [Google Scholar] [CrossRef]
- Suzuki, H.; Ito, M.; Takemura, K.; Nakanishi, Y.; Kataoka, M.; Sakamoto, K.; Tobisu, K.; Koga, F. Prognostic Significance of the Controlling Nutritional Status (CONUT) Score in Advanced Urothelial Carcinoma Patients. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 76.e11–76.e17. [Google Scholar] [CrossRef]
- de Ulíbarri, J.I.; González-Madroño, A.; de Villar, N.G.; González, P.; González, B.; Mancha, A.; Rodríguez, F.; Fernández, G. CONUT: A Tool for Controlling Nutritional Status. First Validation in a Hospital Population. Nutr. Hosp. 2005, 20, 38–45. [Google Scholar]
- Elghiaty, A.; Kim, J.; Jang, W.S.; Park, J.S.; Heo, J.E.; Rha, K.H.; Choi, Y.D.; Ham, W.S. Preoperative Controlling Nutritional Status (CONUT) Score as a Novel Immune-Nutritional Predictor of Survival in Non-Metastatic Clear Cell Renal Cell Carcinoma of ≤7 cm on Preoperative Imaging. J. Cancer Res. Clin. Oncol. 2019, 145, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.W.; Seo, S.P.; Kim, W.T.; Yun, S.J.; Lee, S.-C.; Kim, W.-J.; Hwang, E.C.; Kang, S.H.; Hong, S.-H.; Chung, J.; et al. Prognostic Impact of Nutritional Status Assessed by the Controlling Nutritional Status (CONUT) Score in Patients with Surgically Treated Renal Cell Carcinoma. Nutr. Cancer 2018, 70, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Xu, B.; Luo, C.; Zhang, Z.; Ma, B.; Jin, J.; Zhang, Q. The Prognostic Value of Preoperative Controlling Nutritional Status Score in Non-Metastatic Renal Cell Carcinoma Treated with Surgery: A Retrospective Single-Institution Study. Cancer Manag. Res. 2019, 11, 7567–7575. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Bao, L.; Wang, W.; Wang, Q.; Pan, Y.; Gao, X. Prognostic Impact of the Controlling Nutritional Status Score Following Curative Nephrectomy for Patients with Renal Cell Carcinoma. Medicine 2018, 97, e13409. [Google Scholar] [CrossRef]
- Jin, H.; Zhu, K.; Wang, W. The Predictive Values of Pretreatment Controlling Nutritional Status (CONUT) Score in Estimating Short- and Long-term Outcomes for Patients with Gastric Cancer Treated with Neoadjuvant Chemotherapy and Curative Gastrectomy. J. Gastric Cancer 2021, 21, 155–168. [Google Scholar] [CrossRef]
- Harimoto, N.; Yoshizumi, T.; Inokuchi, S.; Itoh, S.; Adachi, E.; Ikeda, Y.; Uchiyama, H.; Utsunomiya, T.; Kajiyama, K.; Kimura, K.; et al. Prognostic Significance of Preoperative Controlling Nutritional Status (CONUT) Score in Patients Undergoing Hepatic Resection for Hepatocellular Carcinoma: A Multi-institutional Study. Ann. Surg. Oncol. 2018, 25, 3316–3323. [Google Scholar] [CrossRef]
- Chung, J.S.; Son, N.H.; Byun, S.-S.; Lee, S.E.; Hong, S.K.; Jeong, C.W.; Lee, S.C.; Chae, D.-W.; Choi, W.S.; Park, Y.H.; et al. Trends in Renal Function after Radical Nephrectomy: A Multicentre Analysis: Renal Function Recovery after Radical Nephrectomy. BJU Int. 2014, 113, 408–415. [Google Scholar] [CrossRef]
- Huang, W.C.; Levey, A.S.; Serio, A.M.; Snyder, M.; Vickers, A.J.; Raj, G.V.; Scardino, P.T.; Russo, P. Chronic Kidney Disease after Nephrectomy in Patients with Renal Cortical Tumours: A Retrospective Cohort Study. Lancet Oncol. 2006, 7, 735–740. [Google Scholar] [CrossRef]
- Peng, L.; Meng, C.; Li, J.; You, C.; Du, Y.; Xiong, W.; Xia, Z.; Cao, D.; Li, Y. The Prognostic Significance of Controlling Nutritional Status (CONUT) Score for Surgically Treated Renal Cell Cancer and Upper Urinary Tract Urothelial Cancer: A Systematic Review and Meta-Analysis. Eur. J. Clin. Nutr. 2022, 76, 801–810. [Google Scholar] [CrossRef]
- Chen, J.; Cao, D.; Peng, Z.; Song, P.; Liu, Z.; Yang, L.; Wang, L.; Zhou, J.; Wei, Q.; Dong, Q. The Prognostic Value of the Controlling Nutritional Status Score on Patients Undergoing Nephrectomy for Upper Tract Urothelial Carcinoma or Renal Cell Carcinoma: A Systematic Review and Meta-Analysis. Br. J. Nutr. 2022, 128, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, Z.A.; Capitanio, U.; Lane, B.R.; Larcher, A.; Yim, K.; Dey, S.; Cotta, B.H.; Meagher, M.F.; Kirmiz, S.; Bezinque, A.; et al. Should Partial Nephrectomy Be Considered “Elective” in Patients with Stage 2 Chronic Kidney Disease? A Comparative Analysis of Functional and Survival Outcomes after Radical and Partial Nephrectomy. World J. Urol. 2019, 37, 2429–2437. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.V.; Walia, A.; Saidian, A.; Puri, D.; Meagher, M.F.; Hakimi, K.; Tanaka, H.; Patil, D.; Yasuda, Y.; Saito, K.; et al. Impact of Worsening Surgically Induced Chronic Kidney Disease (CKD-S) in Preoperative CKD-Naïve Patients on Survival in Renal Cell Carcinoma. BJU Int. 2022, 131, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.S.; Son, N.H.; Lee, S.E.; Hong, S.K.; Lee, S.C.; Kwak, C.; Hong, S.H.; Kim, Y.J.; Kang, S.H.; Byun, S.-S. Overall Survival and Renal Function after Partial and Radical Nephrectomy among Older Patients with Localised Renal Cell Carcinoma: A Propensity-Matched Multicentre Study. Eur. J. Cancer 2015, 51, 489–497. [Google Scholar] [CrossRef] [PubMed]
- Zabor, E.C.; Furberg, H.; Lee, B.; Campbell, S.; Lane, B.R.; Thompson, R.H.; Antonio, E.C.; Noyes, S.L.; Zaid, H.; Jaimes, E.A.; et al. Long-Term Renal Function Recovery Following Radical Nephrectomy for Kidney Cancer: Results from a Multicenter Confirmatory Study. J. Urol. 2018, 199, 921–926. [Google Scholar] [CrossRef]
- Choi, D.K.; Jung, S.B.; Park, B.H.; Jeong, B.C.; Seo, S.I.; Jeon, S.S.; Lee, H.M.; Choi, H.Y.; Jeon, H.G. Compensatory Structural and Functional Adaptation after Radical Nephrectomy for Renal Cell Carcinoma According to Preoperative Stage of Chronic Kidney Diseasee. J. Urol. 2015, 194, 910–915. [Google Scholar] [CrossRef]
- Sorbellini, M.; Kattan, M.W.; Snyder, M.E.; Hakimi, A.A.; Sarasohn, D.M.; Russo, P. Prognostic Nomogram for Renal Insufficiency After Radical or Partial Nephrectomy. J. Urol. 2006, 176, 472–476. [Google Scholar] [CrossRef]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.-M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
| Parameter | Normal | Light | Moderate | Severe |
|---|---|---|---|---|
| Serum albumin (mg/dL) | 3.5–4.5 | 3.0–3.49 | 2.5–2.99 | >2.5 |
| score | 0 | 2 | 4 | 6 |
| Total lymphocytes (/mL) | >1600 | 1200–1599 | 800–1199 | <800 |
| score | 0 | 1 | 2 | 3 |
| Cholesterol (mg/dL) | >180 | 140–180 | 100–139 | <100 |
| Score | 0 | 1 | 2 | 3 |
| Screening total score | 0–1 | 2–4 | 5–8 | 9–12 |
| Variables | Overall | Low CONUT Score | High CONUT Score | p |
|---|---|---|---|---|
| Patients, n (%) | 140 (100.0) | 94 (67.1) | 46 (32.9) | |
| Baseline clinical characteristics | ||||
| Age (years), median (IQR) | 66 (56–74) | 70 (64–78) | 63 (56–73) | 0.0005 |
| Gender, n (%) | 0.37 | |||
| Male | 98 (70.0) | 63 (67.0) | 35 (76.1) | |
| Female | 42 (30.0) | 31 (33.0) | 11 (23.9) | |
| BMI (kg/m2), median (IQR) | 27.0 (25.0–31.5) | 26.0 (24.0–31.0) | 29.0 (25.0–32.0) | 0.12 |
| CCI, n (%) | 0.21 | |||
| 0 | 71 (50.7) | 53 (56.4) | 18 (39.1) | |
| 1 | 38 (27.1) | 24 (25.5) | 14 (30.4) | |
| ≥2 | 31 (22.1) | 17 (18.1) | 14 (30.4) | |
| HTN, n (%) | 63 (45.0) | 38 (40.4) | 25 (54.3) | 0.17 |
| DM, n (%) | 21 (15.0) | 11 (10.6) | 10 (23.9) | 0.19 |
| cT stage, n (%) | 0.14 | |||
| cT1 (a, b) | 85 (61.2) | 64 (68.1) | 21 (45.7) | |
| cT2 (a, b) | 34 (21.4) | 20 (21.3) | 14 (30.4) | |
| cT3 (a, b, c) | 21 (15.0) | 10 (10.6) | 11 (23.9) | |
| Preop. Hb (g/dL), median (IQR) | 13.7 (12.6–14.6) | 13.8 (13.0–14.7) | 13.4 (11.6–14.4) | 0.55 |
| Preop. eGFR (mL/min), median (IQR) | 82.1 (73.1–93.3) | 84.0 (71.9–92.1) | 82.7 (74.2–93.5) | 0.76 |
| Preop. CRP (mg/dL), median (IQR) | 0.5 (0.3–2.2) | 0.3 (0.3–0.8) | 0.74 (0.3–5.83) | 0.04 |
| Fibrinogen (mg/dL), median (IQR) | 341.0 (282.6–429.0) | 325.4 (279.1–390.6) | 401.3 (298.2–524.5) | 0.007 |
| Preoperative CKD stage, n (%) | 0.31 | |||
| I | 48 (34.4) | 31 (33.0) | 17 (37.0) | |
| II | 91 (65.0) | 63 (66.0) | 28 (60.9) | |
| IIIa | 1 (0.7) | 0 (0.0) | 1 (2.2) | |
| Perioperative information | ||||
| Surgical approach, n (%) | 0.52 | |||
| Open | 97 (69.3) | 63 (67.0) | 34 (73.9) | |
| Laparoscopic | 43 (30.7) | 31 (33.0) | 12 (26.1) | |
| Blood loss (mL), median (IQR) | 100 (50–400) | 100 (50–400) | 200 (50–500) | 0.32 |
| Intraoperative complications, n (%) | 13 (9.3) | 5 (5.3) | 8 (17.4) | 0.04 |
| Regional LND, n (%) | 39 (27.9) | 24 (25.5) | 15 (32.6) | 0.5 |
| Perioperative complications, n (%) | 0.003 | |||
| None | 105 (75.0) | 78 (83.0) | 27 (58.7) | |
| Minor | 31 (22.1) | 13 (13.8) | 18 (39.1) | |
| Major | 4 (2.9) | 3 (3.2) | 1 (2.2) | |
| Pathological features | ||||
| pT stage, n (%) | 0.006 | |||
| pT1 (a, b) | 72 (51.4) | 55 (58.5) | 17 (37.0) | |
| pT2 (a, b) | 23 (16.4) | 17 (18.1) | 6 (13.0) | |
| pT3 (a, b, c) | 45 (32.1) | 22 (23.4) | 23 (50.0) | |
| pN stage, n (%) | 0.5 | |||
| pN0 | 39 (27.9) | 24 (25.5) | 15 (32.6) | |
| pNx | 101 (72.1) | 70 (74.5) | 31 (67.4) | |
| Fuhrman grade, n (%) | 0.02 | |||
| G1 | 11 (7.9) | 11 (11.7) | 0 (0.0) | |
| G2 | 67 (47.9) | 49 (52.1) | 18 (39.1) | |
| G3 | 48 (34.3) | 29 (30.9) | 19 (41.3) | |
| G4 | 14 (10.0) | 5 (5.3) | 9 (19.6) | |
| Sarcomatoid features, n (%) | 4 (2.9) | 3 (3.2) | 1 (2.2) | 0.20 |
| Necrosis in the specimen, n (%) | 65 (46.4) | 39 (41.5) | 26 (56.5) | 0.14 |
| Venous thrombosis, n (%) | 19 (13.6) | 8 (8.5) | 11 (23.9) | 0.03 |
| Follow-up information | ||||
| Follow up (months), median (IQR) | 59.5 (40.0–95.2) | 61.0 (39.0–99.0) | 54.0 (43.0–92.0) | 0.29 |
| Recurrence events, n (%) | 22 (15.7) | 11 (11.7) | 11 (23.9) | 0.11 |
| All-cause events, n (%) | 27 (19.3) | 11 (11.7) | 16 (34.8) | 0.001 |
| Cancer-specific events, n (%) | 12 (8.6) | 5 (5.3) | 7 (15.2) | 0.10 |
| 24-month eGFR < 45 (mL/min), n (%) | 30 (21.4) | 13 (13.8) | 17 (37.0) | 0.002 |
| Univariable | Multivariable | |||
|---|---|---|---|---|
| Variable | OR (95%CI) | p | OR (95%CI) | p |
| Age (years) | ||||
| <70 | Ref. (1.0) | - | Ref. (1.0) | - |
| ≥70 | 4.03 (1.75–9.67) | <0.001 | 2.01 (1.17–3.09) | 0.05 |
| Gender | ||||
| Male | Ref. (1.0) | - | - | - |
| Female | 2.14 (0.91–4.94) | 0.07 | - | - |
| BMI (kg/m2) as cont. | 1.03 (0.91–1.18) | 0.6 | - | - |
| DM | ||||
| No | Ref. (1.0) | - | - | - |
| Yes | 1.58 (0.52–4.36) | 0.4 | - | - |
| HTN | ||||
| No | Ref. (1.0) | - | - | - |
| Yes | 1.29 (0.57–2.92) | 0.5 | - | - |
| CCI | ||||
| 0 | Ref. (1.0) | - | - | - |
| 1 | 3.56 (1.41–9.34) | 0.07 | - | - |
| ≥2 | 1.46 (0.46–4.39) | 0.5 | - | - |
| Preoperative CKD stage | ||||
| I | Ref. (1.0) | - | Ref. (1.0) | - |
| II–IIIa | 6.33 (2.07–27.6) | <0.001 | 6.05 (1.79–28.3) | 0.001 |
| cT stage | ||||
| ≤70 mm (cT1) | Ref. (1.0) | - | - | - |
| >70 mm (>cT1) | 1.66 (0.73–3.77) | 0.2 | - | - |
| CONUT | ||||
| Low | Ref. (1.0) | - | Ref. (1.0) | - |
| High | 3.56 (1.59–8.59) | 0.002 | 3.98 (1.58–10.4) | 0.004 |
| AUC of the model (95%CI) | 0.80 (0.71–0.88) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boltri, M.; Traunero, F.; Ongaro, L.; Migliozzi, F.; Vianello, F.; Lenardon, O.; Visalli, F.; Buttazzi, L.; Maruzzi, D.; Trombetta, C.; et al. The Added Value of Controlling Nutritional Status (Conut) Score for Preoperative Counselling on Significant Early Loss of Renal Function After Radical Nephrectomy for Renal Cell Carcinoma. Cancers 2024, 16, 3519. https://doi.org/10.3390/cancers16203519
Boltri M, Traunero F, Ongaro L, Migliozzi F, Vianello F, Lenardon O, Visalli F, Buttazzi L, Maruzzi D, Trombetta C, et al. The Added Value of Controlling Nutritional Status (Conut) Score for Preoperative Counselling on Significant Early Loss of Renal Function After Radical Nephrectomy for Renal Cell Carcinoma. Cancers. 2024; 16(20):3519. https://doi.org/10.3390/cancers16203519
Chicago/Turabian StyleBoltri, Matteo, Fabio Traunero, Luca Ongaro, Francesca Migliozzi, Fabio Vianello, Oliviero Lenardon, Francesco Visalli, Lorenzo Buttazzi, Daniele Maruzzi, Carlo Trombetta, and et al. 2024. "The Added Value of Controlling Nutritional Status (Conut) Score for Preoperative Counselling on Significant Early Loss of Renal Function After Radical Nephrectomy for Renal Cell Carcinoma" Cancers 16, no. 20: 3519. https://doi.org/10.3390/cancers16203519
APA StyleBoltri, M., Traunero, F., Ongaro, L., Migliozzi, F., Vianello, F., Lenardon, O., Visalli, F., Buttazzi, L., Maruzzi, D., Trombetta, C., Simonato, A., Pavan, N., & Claps, F. (2024). The Added Value of Controlling Nutritional Status (Conut) Score for Preoperative Counselling on Significant Early Loss of Renal Function After Radical Nephrectomy for Renal Cell Carcinoma. Cancers, 16(20), 3519. https://doi.org/10.3390/cancers16203519






