PARP Inhibitors in Pancreatic Cancer with Homologous Recombination Repair Gene Mutations: A Single-Institution Experience
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection and Clinical Data Collection
2.2. Treatment Assessment
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
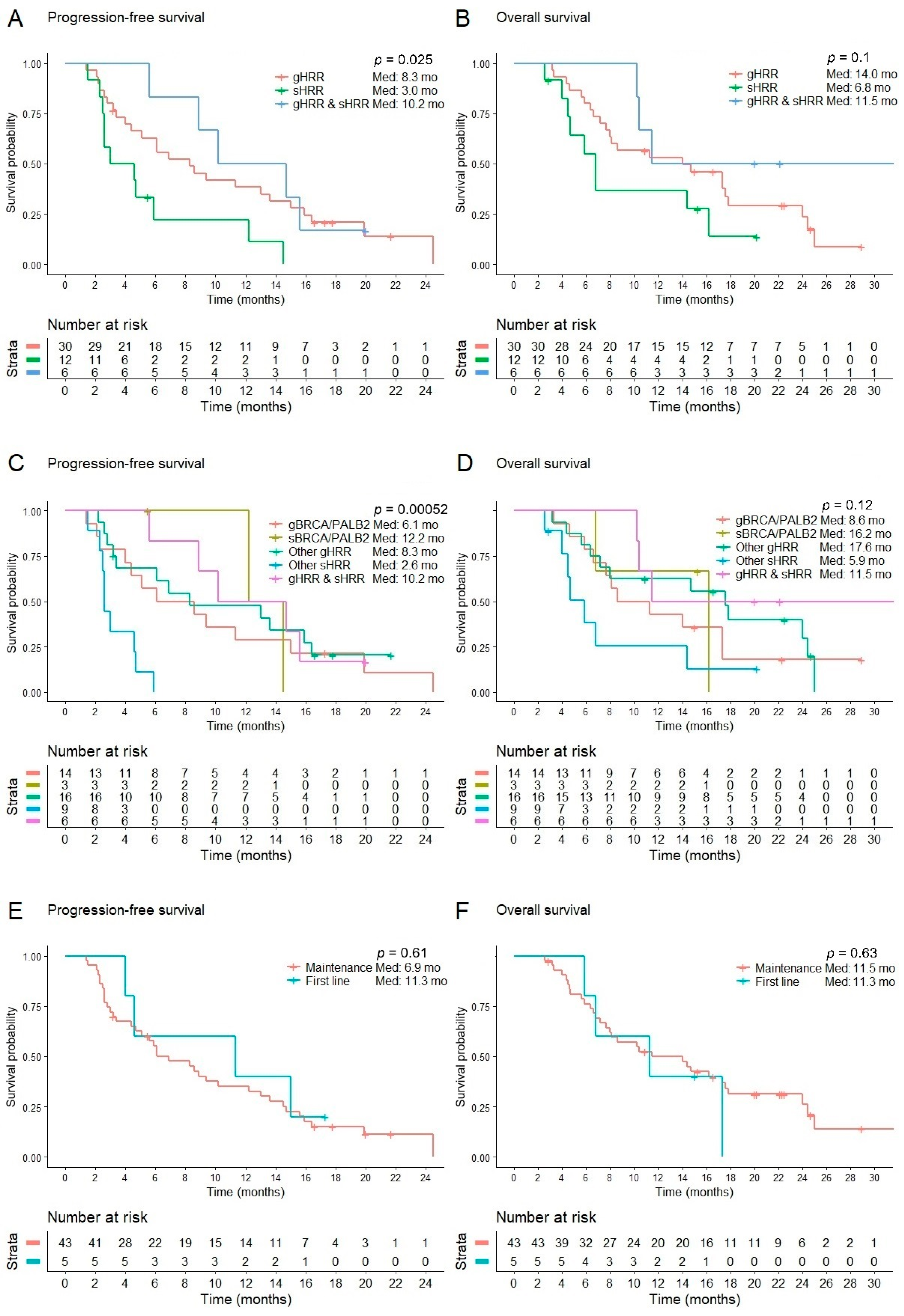
3.2. Efficacy
3.3. Maintenance after Chemotherapy
3.4. First Line for Borderline Performance Status
3.5. Treatment after Refractory to a PARP Inhibitor
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zheng, F.; Zhang, Y.; Chen, S.; Weng, X.; Rao, Y.; Fang, H. Mechanism and current progress of Poly ADP-ribose polymerase (PARP) inhibitors in the treatment of ovarian cancer. Biomed. Pharmacother. 2020, 123, 109661. [Google Scholar] [CrossRef] [PubMed]
- Das, P.K.; Matada, G.S.P.; Pal, R.; Maji, L.; Dhiwar, P.S.; Manjushree, B.V.; Viji, M. Poly (ADP-ribose) polymerase (PARP) inhibitors as anticancer agents: An outlook on clinical progress, synthetic strategies, biological activity, and structure-activity relationship. Eur. J. Med. Chem. 2024, 274, 116535. [Google Scholar] [CrossRef] [PubMed]
- Mateo, J.; Lord, C.J.; Serra, V.; Tutt, A.; Balmaña, J.; Castroviejo-Bermejo, M.; Cruz, C.; Oaknin, A.; Kaye, S.B.; de Bono, J.S. A decade of clinical development of PARP inhibitors in perspective. Ann. Oncol. 2019, 30, 1437–1447. [Google Scholar] [CrossRef]
- Lord, C.J.; Ashworth, A. PARP inhibitors: Synthetic lethality in the clinic. Science 2017, 355, 1152–1158. [Google Scholar] [CrossRef] [PubMed]
- Park, W.; Chen, J.; Chou, J.F.; Varghese, A.M.; Yu, K.H.; Wong, W.; Capanu, M.; Balachandran, V.; McIntyre, C.A.; El Dika, I.; et al. Genomic Methods Identify Homologous Recombination Deficiency in Pancreas Adenocarcinoma and Optimize Treatment Selection. Clin. Cancer Res. 2020, 26, 3239–3247. [Google Scholar] [CrossRef]
- Aguirre, A.J.; Nowak, J.A.; Camarda, N.D.; Moffitt, R.A.; Ghazani, A.A.; Hazar-Rethinam, M.; Raghavan, S.; Kim, J.; Brais, L.K.; Ragon, D.; et al. Real-time Genomic Characterization of Advanced Pancreatic Cancer to Enable Precision Medicine. Cancer Discov. 2018, 8, 1096–1111. [Google Scholar] [CrossRef]
- Casolino, R.; Paiella, S.; Azzolina, D.; Beer, P.A.; Corbo, V.; Lorenzoni, G.; Gregori, D.; Golan, T.; Braconi, C.; Froeling, F.E.M.; et al. Homologous Recombination Deficiency in Pancreatic Cancer: A Systematic Review and Prevalence Meta-Analysis. J. Clin. Oncol. 2021, 39, 2617–2631. [Google Scholar] [CrossRef]
- Heeke, A.L.; Pishvaian, M.J.; Lynce, F.; Xiu, J.; Brody, J.R.; Chen, W.-J.; Baker, T.M.; Marshall, J.L.; Isaacs, C. Prevalence of Homologous Recombination–Related Gene Mutations Across Multiple Cancer Types. JCO Precis. Oncol. 2018, 2, 1–13. [Google Scholar] [CrossRef]
- de Bono, J.; Mateo, J.; Fizazi, K.; Saad, F.; Shore, N.; Sandhu, S.; Chi, K.N.; Sartor, O.; Agarwal, N.; Olmos, D.; et al. Olaparib for Metastatic Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2020, 382, 2091–2102. [Google Scholar] [CrossRef]
- Golan, T.; Hammel, P.; Reni, M.; Van Cutsem, E.; Macarulla, T.; Hall, M.J.; Park, J.-O.; Hochhauser, D.; Arnold, D.; Oh, D.-Y.; et al. Maintenance Olaparib for Germline BRCA-Mutated Metastatic Pancreatic Cancer. N. Engl. J. Med. 2019, 381, 317–327. [Google Scholar] [CrossRef]
- Kindler, H.L.; Hammel, P.; Reni, M.; Van Cutsem, E.; Macarulla, T.; Hall, M.J.; Park, J.O.; Hochhauser, D.; Arnold, D.; Oh, D.-Y.; et al. Overall Survival Results From the POLO Trial: A Phase III Study of Active Maintenance Olaparib Versus Placebo for Germline BRCA-Mutated Metastatic Pancreatic Cancer. J. Clin. Oncol. 2022, 40, 3929–3939. [Google Scholar] [CrossRef] [PubMed]
- Reiss, K.A.; Mick, R.; O’Hara, M.H.; Teitelbaum, U.; Karasic, T.B.; Schneider, C.; Cowden, S.; Southwell, T.; Romeo, J.; Izgur, N.; et al. Phase II Study of Maintenance Rucaparib in Patients With Platinum-Sensitive Advanced Pancreatic Cancer and a Pathogenic Germline or Somatic Variant in BRCA1, BRCA2, or PALB2. J. Clin. Oncol. 2021, 39, 2497–2505. [Google Scholar] [CrossRef]
- Boyle, T.A.; Mondal, A.K.; Saeed-Vafa, D.; Ananth, S.; Ahluwalia, P.; Kothapalli, R.; Chaubey, A.; Roberts, E.; Qin, D.; Magliocco, A.M.; et al. Guideline-Adherent Clinical Validation of a Comprehensive 170-Gene DNA/RNA Panel for Determination of Small Variants, Copy Number Variations, Splice Variants, and Fusions on a Next-Generation Sequencing Platform in the CLIA Setting. Front. Genet. 2021, 12, 503830. [Google Scholar] [CrossRef] [PubMed]
- Tung, N.M.; Robson, M.E.; Ventz, S.; Santa-Maria, C.A.; Nanda, R.; Marcom, P.K.; Shah, P.D.; Ballinger, T.J.; Yang, E.S.; Vinayak, S.; et al. TBCRC 048: Phase II Study of Olaparib for Metastatic Breast Cancer and Mutations in Homologous Recombination-Related Genes. J. Clin. Oncol. 2020, 38, 4274–4282. [Google Scholar] [CrossRef]
- Batalini, F.; Madison, R.W.; Sokol, E.S.; Jin, D.X.; Chen, K.T.; Decker, B.; Pavlick, D.C.; Frampton, G.M.; Wulf, G.M.; Garber, J.E.; et al. Homologous Recombination Deficiency Landscape of Breast Cancers and Real-World Effectiveness of Poly ADP-Ribose Polymerase Inhibitors in Patients With Somatic BRCA1/2, Germline PALB2, or Homologous Recombination Deficiency Signature. JCO Precis. Oncol. 2023, 7, e2300091. [Google Scholar] [CrossRef] [PubMed]
- Mohyuddin, G.R.; Aziz, M.; Britt, A.; Wade, L.; Sun, W.; Baranda, J.; Al-Rajabi, R.; Saeed, A.; Kasi, A. Similar response rates and survival with PARP inhibitors for patients with solid tumors harboring somatic versus Germline BRCA mutations: A Meta-analysis and systematic review. BMC Cancer 2020, 20, 507. [Google Scholar] [CrossRef]
- Fusco, M.J.; Saeed-Vafa, D.; Carballido, E.M.; Boyle, T.A.; Malafa, M.; Blue, K.L.; Teer, J.K.; Walko, C.M.; McLeod, H.L.; Hicks, J.K.; et al. Identification of Targetable Gene Fusions and Structural Rearrangements to Foster Precision Medicine in KRAS Wild-Type Pancreatic Cancer. JCO Precis. Oncol. 2021, 5, 65–74. [Google Scholar] [CrossRef]
- Philip, P.A.; Azar, I.; Xiu, J.; Hall, M.J.; Hendifar, A.E.; Lou, E.; Hwang, J.J.; Gong, J.; Feldman, R.; Ellis, M.; et al. Molecular Characterization of KRAS Wild-type Tumors in Patients with Pancreatic Adenocarcinoma. Clin. Cancer Res. 2022, 28, 2704–2714. [Google Scholar] [CrossRef]
- Elhariri, A.; Patel, J.; Mahadevia, H.; Albelal, D.; Ahmed, A.K.; Jones, J.C.; Borad, M.J.; Babiker, H. Identifying Actionable Alterations in KRAS Wild-Type Pancreatic Cancer. Target. Oncol. 2024, 19, 679–689. [Google Scholar] [CrossRef]
- Javle, M.; Shacham-Shmueli, E.; Xiao, L.; Varadhachary, G.; Halpern, N.; Fogelman, D.; Boursi, B.; Uruba, S.; Margalit, O.; Wolff, R.A.; et al. Olaparib Monotherapy for Previously Treated Pancreatic Cancer With DNA Damage Repair Genetic Alterations Other Than Germline BRCA Variants: Findings From 2 Phase 2 Nonrandomized Clinical Trials. JAMA Oncol. 2021, 7, 693–699. [Google Scholar] [CrossRef]
- Joris, S.; Denys, H.; Collignon, J.; Rasschaert, M.; T’Kint de Roodenbeke, D.; Duhoux, F.P.; Canon, J.-L.; Tejpar, S.; Mebis, J.; Decoster, L.; et al. Efficacy of olaparib in advanced cancers with germline or somatic mutations in BRCA1, BRCA2, CHEK2 and ATM, a Belgian Precision tumor-agnostic phase II study. ESMO Open 2023, 8, 102041. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Hayashi, H.; Kawano, R.; Ishikawa, M.; Aimono, E.; Mizuno, T.; Kuroda, H.; Kojima, Y.; Niikura, N.; Kawanishi, A.; et al. BRCA1/2 reversion mutations in a pan-cancer cohort. Cancer Sci. 2024, 115, 635–647. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.J.; Yablonovitch, A.; Till, J.E.; Yen, J.; Kiedrowski, L.A.; Hood, R.; O’Hara, M.H.; Teitelbaum, U.; Karasic, T.B.; Schneider, C.; et al. The Clinical Implications of Reversions in Patients with Advanced Pancreatic Cancer and Pathogenic Variants in BRCA1, BRCA2, or PALB2 after Progression on Rucaparib. Clin. Cancer Res. 2023, 29, 5207–5216. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.K.; Harrell, M.I.; Oza, A.M.; Oaknin, A.; Ray-Coquard, I.; Tinker, A.V.; Helman, E.; Radke, M.R.; Say, C.; Vo, L.T.; et al. BRCA Reversion Mutations in Circulating Tumor DNA Predict Primary and Acquired Resistance to the PARP Inhibitor Rucaparib in High-Grade Ovarian Carcinoma. Cancer Discov. 2019, 9, 210–219. [Google Scholar] [CrossRef]
- Loehr, A.; Hussain, A.; Patnaik, A.; Bryce, A.H.; Castellano, D.; Font, A.; Shapiro, J.; Zhang, J.; Sautois, B.; Vogelzang, N.J.; et al. Emergence of BRCA Reversion Mutations in Patients with Metastatic Castration-resistant Prostate Cancer After Treatment with Rucaparib. Eur. Urol. 2023, 83, 200–209. [Google Scholar] [CrossRef]
- Mitri, Z.; Goodyear, S.M.; Mills, G. Strategies for the prevention or reversal of PARP inhibitor resistance. Expert Rev. Anticancer. Ther. 2024, 24, 959–975. [Google Scholar] [CrossRef]
- Kawamoto, Y.; Yamai, T.; Ikezawa, K.; Seiki, Y.; Watsuji, K.; Hirao, T.; Urabe, M.; Kai, Y.; Takada, R.; Mukai, K.; et al. Clinical significance of germline breast cancer susceptibility gene (gBRCA) testing and olaparib as maintenance therapy for patients with pancreatic cancer. BMC Cancer 2024, 24, 1000. [Google Scholar] [CrossRef]
- Kindler, H.L.; Yoo, H.K.; Hettle, R.; Cui, K.Y.; Joo, S.; Locker, G.Y.; Golan, T. Patient-centered outcomes in the POLO study of active maintenance olaparib for germline BRCA-mutated metastatic pancreatic cancer. Cancer 2023, 129, 1411–1418. [Google Scholar] [CrossRef]
- Kubo, T.; Muramatsu, J.; Arihara, Y.; Murota, A.; Ishikawa, K.; Yoshida, M.; Nagashima, H.; Tamura, F.; Ikeda, Y.; Usami, M.; et al. Clinical characterization of patients with gBRCA1/2 mutation-positive unresectable pancreatic cancer: A multicenter prospective study. Jpn J. Clin. Oncol. 2024, 54, 47–53. [Google Scholar] [CrossRef]
- Miao, R.; Yu, J.; Blue, K.; Sommerer, K.; Shah, A.; Bottiglieri, S.; Ho, T.; Hicks, K.; Kim, D.W. 354P PARP inhibitors in Pancreatic Cancer with Homologous Recombination Repair Gene Mutations: A Single-Institution Experience. In Proceedings of the ESMO Gastrointestinal Cancers Congress 2024, Munich, Germany, 26–29 June 2024. [Google Scholar]
| Baseline Characteristics | Patients (n = 48) |
|---|---|
| Age, years, median (range) | 71 (42–90) |
| Sex, n (%) Male Female | 26 (54) 22 (46) |
| Race, n (%) | |
| White | 48 (100) |
| ECOG at screening, n (%) | |
| 0 | 7 (15) |
| 1 | 28 (58) |
| 2 | 13 (27) |
| Site of primary tumor, n (%) | |
| Head | 23 (48) |
| Body | 14 (29) |
| Tail | 11 (23) |
| Staging, n (%) | |
| Locally advanced disease | 9 (19) |
| Metastatic disease | 39 (81) |
| Metastatic site, n (%) | n = 39 |
| Liver | 26 (67) |
| Lung | 11 (28) |
| Peritoneum | 8 (21) |
| Retroperitoneal lymph nodes | 5 (13) |
| HRR mutation, n (%) | |
| Germline BRCA or PALB2 | 17 (35) |
| Somatic BRCA or PALB2 | 6 (13) |
| Germline non-BRCA non-PALB2 HRR | 19 (40) |
| Somatic non-BRCA non-PALB2 HRR | 12 (25) |
| RAS status, n (%) | |
| Wild type | 11 (23) |
| KRAS G12D | 6 (13) |
| KRAS G12R | 3 (6) |
| KRAS G12S | 1 (2) |
| KRAS G12V | 9 (19) |
| KRAS Q61H | 3 (6) |
| NRAS G12D | 1 (2) |
| Unknown | 14 (29) |
| Treatment setting, n (%) | |
| First-line monotherapy | 5 (10) |
| First-line maintenance therapy | 32 (74) |
| Subsequent line maintenance therapy | 11 (26) |
| Previous chemotherapy, n (%) | n = 43 |
| FOLFIRINOX | 25 (58) |
| Gemcitabine/nab-paclitaxel | 21 (49) |
| Gemcitabine/cisplatin | 3 (7) |
| 5FU/liposomal irinotecan | 3 (7) |
| FOLFOX | 2 (5) |
| Liposomal irinotecan monotherapy | 1 (2) |
| Gemcitabine monotherapy | 1 (2) |
| Other (trametinib, cobimetinib) | 1 (2) |
| Best Overall Response | Total Evaluable | Germline BRCA or PALB2 * | Somatic BRCA or PALB2 * | Germline Non-BRCA Non-PALB2 HRR * | Somatic Non-BRCA Non-PALB2 HRR * | Germline and Somatic HRR # | p Value |
|---|---|---|---|---|---|---|---|
| n = 46 | n = 14 | n = 3 | n = 14 | n = 9 | n= 6 | ||
| PR, n (%) | 10 (22) | 4 (29) | 1 (33) | 1 (11) | 4 (67) | ||
| SD, n (%) | 26 (57) | 7 (50) | 2 (67) | 12 (86) | 3 (33) | 2 (33) | |
| PD, n (%) | 10 (22) | 3 (21) | 2 (14) | 5 (56) | |||
| ORR (CR + PR), n (%) | 10 (22) | 4 (29) | 1 (33) | 0 (0) | 1 (11) | 4 (67) | 0.016 |
| DCR (CR + PR + SD), n (%) | 36 (78) | 11 (79) | 3 (100) | 12 (86) | 4 (44) | 6 (100) | 0.061 |
| Progression-Free Survival (Months) | Overall Survival (Months) | |||||||
|---|---|---|---|---|---|---|---|---|
| n | Median | 95% CI | Log-Rank p | Median | 95% CI | Log-Rank p | ||
| All | 48 | 6.9 | 3.4–10.4 | 11.5 | 6.0–17.0 | |||
| HRR mutation | ||||||||
| BRCA/PALB2 | 21 | 9.4 | 5.6–13.2 | 0.662 | 11.5 | 5.8–17.2 | 0.665 | |
| Non-BRCA/PALB2 | 27 | 5.9 | 3.5–8.3 | 14.4 | 5.4–23.4 | |||
| Germline mutation * | 30 | 8.3 | 4.0–12.6 | 0.025 | 14.0 | 5.7–22.3 | 0.101 | |
| Somatic mutation * | 12 | 3.0 | 0.0–6.4 | 6.8 | 5.4–8.2 | |||
| Concomitant germline and somatic # | 6 | 10.2 | 3.2–17.2 | 11.5 | 0.0–24.3 | |||
| Germline BRCA/PALB2 * | 14 | 6.1 | 0.0–12.5 | <0.001 | 8.6 | 2.7–14.5 | 0.121 | |
| Somatic BRCA/PALB2 * | 3 | 12.2 | 16.2 | |||||
| Germline non-BRCA/PALB2 * | 16 | 8.3 | 0.0–16.8 | 17.6 | 12.6–22.6 | |||
| Somatic non-BRCA/PALB2 * | 9 | 2.6 | 2.5–2.7 | 5.9 | 4.0–7.8 | |||
| Concomitant germline and somatic # | 6 | 10.2 | 3.2–17.2 | 11.5 | 0.0–24.3 | |||
| Treatment setting | ||||||||
| Maintenance | 43 | 6.9 | 3.6–10.2 | 0.608 | 11.5 | 4.3–18.7 | 0.629 | |
| First line | 5 | 11.3 | 0.0–25.7 | 11.3 | 1.6–21.0 | |||
| Chemotherapy prior to maintenance | ||||||||
| Platinum based | 25 | 5.1 | 0.7–9.5 | 0.154 | 14.0 | 4.2–23.8 | 0.919 | |
| Non-platinum based | 18 | 10.2 | 2.5–17.9 | 11.5 | 3.5–19.5 | |||
| Total | Maintenance after Platinum | Maintenance after Non-Platinum | First Line | |
|---|---|---|---|---|
| ECOG | n = 48 | n = 25 | n = 18 | n = 5 |
| 0, n (%) | 7 (15) | 7 (28) | 0 (0) | 0 (0) |
| 1, n (%) | 28 (58) | 17 (68) | 11 (61) | 0 (0) |
| 2, n (%) | 13 (27) | 1 (4) | 7 (39) | 5 (100) |
| Best overall response | Evaluable n = 46 | n = 24 | n = 17 | n = 5 |
| PR, n (%) | 10 (22) | 3 (13) | 6 (35) | 1 (20) |
| SD, n (%) | 26 (57) | 13 (54) | 9 (53) | 4 (80) |
| PD, n (%) | 10 (22) | 8 (33) | 2 (12) | |
| ORR (CR + PR), n (%) | 10 (22) | 3 (13) | 6 (35) | 1 (20) |
| DCR (CR + PR + SD), n (%) | 36 (78) | 16 (67) | 15 (88) | 5 (100) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miao, R.; Blue, K.; Sommerer, K.; Shah, A.; Bottiglieri, S.; del Cueto, A.; Berry, D.K.; Ho, T.T.; Hicks, J.K.; Kim, D.W. PARP Inhibitors in Pancreatic Cancer with Homologous Recombination Repair Gene Mutations: A Single-Institution Experience. Cancers 2024, 16, 3447. https://doi.org/10.3390/cancers16203447
Miao R, Blue K, Sommerer K, Shah A, Bottiglieri S, del Cueto A, Berry DK, Ho TT, Hicks JK, Kim DW. PARP Inhibitors in Pancreatic Cancer with Homologous Recombination Repair Gene Mutations: A Single-Institution Experience. Cancers. 2024; 16(20):3447. https://doi.org/10.3390/cancers16203447
Chicago/Turabian StyleMiao, Ruoyu, Kirsten Blue, Katelyn Sommerer, Anand Shah, Sal Bottiglieri, Alex del Cueto, Darcy K. Berry, Teresa T. Ho, James Kevin Hicks, and Dae Won Kim. 2024. "PARP Inhibitors in Pancreatic Cancer with Homologous Recombination Repair Gene Mutations: A Single-Institution Experience" Cancers 16, no. 20: 3447. https://doi.org/10.3390/cancers16203447
APA StyleMiao, R., Blue, K., Sommerer, K., Shah, A., Bottiglieri, S., del Cueto, A., Berry, D. K., Ho, T. T., Hicks, J. K., & Kim, D. W. (2024). PARP Inhibitors in Pancreatic Cancer with Homologous Recombination Repair Gene Mutations: A Single-Institution Experience. Cancers, 16(20), 3447. https://doi.org/10.3390/cancers16203447







