The Immune Landscape and Immunotherapeutic Strategies in Platinum-Refractory Testicular Germ Cell Tumors
Abstract
Simple Summary
Abstract
1. Introduction
2. Search Methodology
3. The Immune Landscape of TGCTs
4. Immune Microenvironment Alternations after Chemotherapy Induction
5. Immunotherapy in TGCTs
5.1. PD-1/PD-L1 Inhibitors
5.2. Anti-CD30 Antibody-Drug Conjugate Therapy
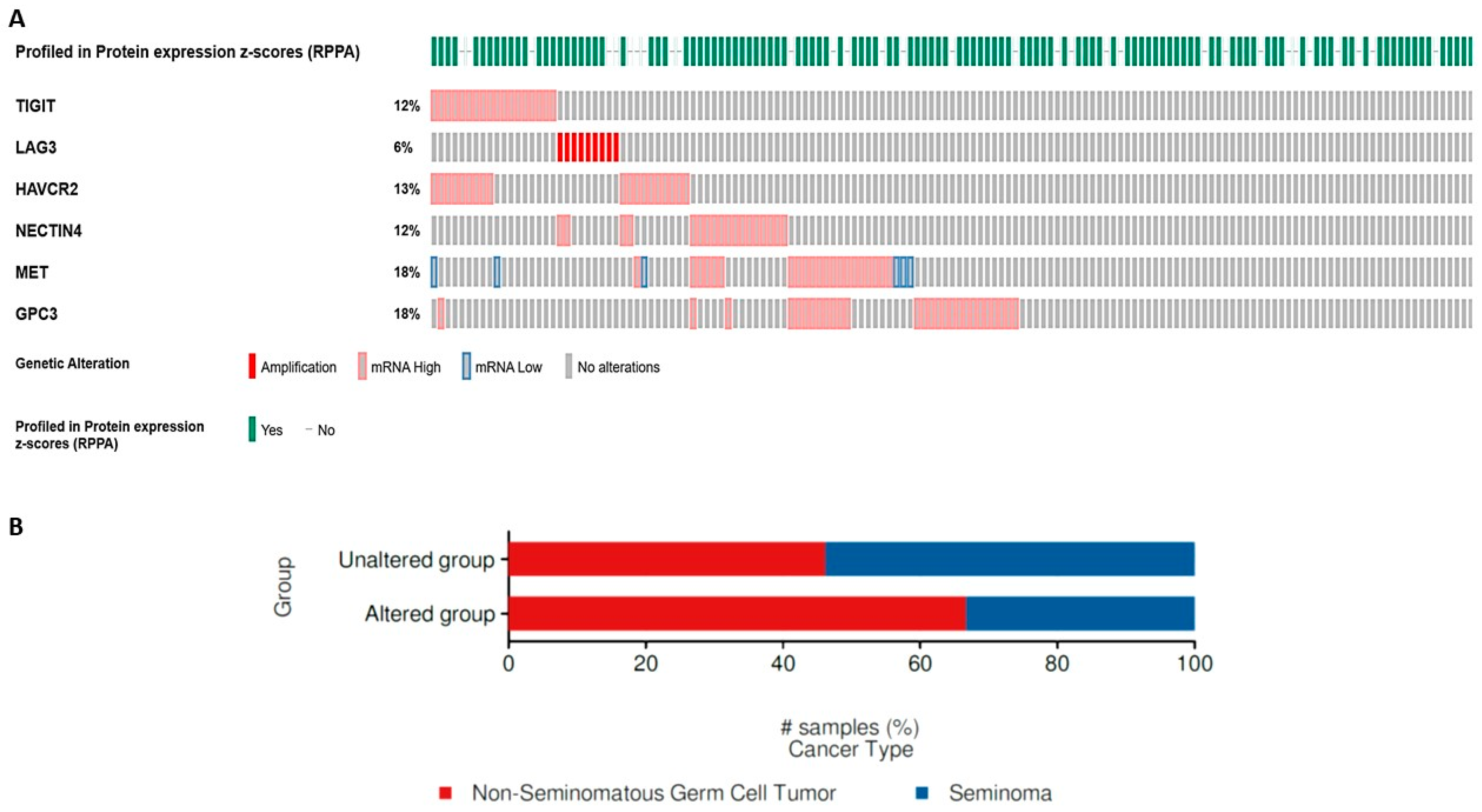
5.3. Emerging Immunotherapeutic Targets
5.4. Prodrug Therapeutics
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gilligan, T.; Lin, D.W.; Aggarwal, R.; Chism, D.; Cost, N.; Derweesh, I.H.; Emamekhoo, H.; Feldman, D.R.; Geynisman, D.M.; Hancock, S.L.; et al. Testicular Cancer, Version 2.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc Netw. 2019, 17, 1529–1554. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, C.T.; Stephenson, A.J. Role of Postchemotherapy Retroperitoneal Lymph Node Dissection in Advanced Germ Cell Tumors. Hematol. Oncol. Clin. N. Am. 2011, 25, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Rajpert-De Meyts, E.; McGlynn, K.A.; Okamoto, K.; Jewett, M.A.S.; Bokemeyer, C. Testicular Germ Cell Tumours. Lancet 2016, 387, 1762–1774. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, U.D.; Demirer, T.; Wandt, H.; Taverna, C.; Siegert, W.; Bornhauser, M.; Kozak, T.; Papiani, G.; Ballardini, M.; Rosti, G. Second-Line High-Dose Chemotherapy in Patients with Mediastinal and Retroperitoneal Primary Non-Seminomatous Germ Cell Tumors: The EBMT Experience. Ann. Oncol. 2005, 16, 146–151. [Google Scholar] [CrossRef]
- De Giorgi, U.; Rosti, G.; Salvioni, R.; Papiani, G.; Ballardini, M.; Pizzocaro, G.; Marangolo, M. Long-Term Outcome of Salvage High-Dose Chemotherapy in Patients with Germ Cell Tumor with Poor Prognostic Features. Urol. Oncol. Semin. Orig. Investig. 2011, 29, 284–290. [Google Scholar] [CrossRef] [PubMed]
- De Giorgi, U.; Rosti, G.; Slavin, S.; Yaniv, I.; Harousseau, J.L.; Ladenstein, R.; Demirer, T.; Dini, G. Salvage High-Dose Chemotherapy for Children with Extragonadal Germ-Cell Tumours. Br. J. Cancer 2005, 93, 412–417. [Google Scholar] [CrossRef]
- Feldman, D.R.; Patil, S.; Trinos, M.J.; Carousso, M.; Ginsberg, M.S.; Sheinfeld, J.; Bajorin, D.F.; Bosl, G.J.; Motzer, R.J. Progression-Free and Overall Survival in Patients with Relapsed/Refractory Germ Cell Tumors Treated with Single-Agent Chemotherapy: Endpoints for Clinical Trial Design. Cancer 2012, 118, 981–986. [Google Scholar] [CrossRef]
- Kollmannsberger, C.; Nichols, C.; Bokemeyer, C. Recent Advances in Management of Patients with Platinum-Refractory Testicular Germ Cell Tumors. Cancer 2006, 106, 1217–1226. [Google Scholar] [CrossRef]
- Ostrowski, K.A.; Walsh, T.J. Infertility with Testicular Cancer. Urol. Clin. N. Am. 2015, 42, 409–420. [Google Scholar] [CrossRef]
- Curreri, S.A.; Fung, C.; Beard, C.J. Secondary Malignant Neoplasms in Testicular Cancer Survivors. Urol. Oncol. Semin. Orig. Investig. 2015, 33, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Conti, M.; Tazzari, V.; Baccini, C.; Pertici, G.; Serino, L.P.; De Giorgi, U. Anticancer Drug Delivery with Nanoparticles. In Vivo 2006, 20, 697–701. [Google Scholar] [PubMed]
- De Giorgi, U.; Rosti, G.; Aieta, M.; Testore, F.; Burattini, L.; Fornarini, G.; Naglieri, E.; Lo Re, G.; Zumaglini, F.; Marangolo, M. Phase II Study of Oxaliplatin and Gemcitabine Salvage Chemotherapy in Patients with Cisplatin-Refractory Nonseminomatous Germ Cell Tumor. Eur. Urol. 2006, 50, 1032–1039. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Fijak, M.; Meinhardt, A. The Testis in Immune Privilege. Immunol. Rev. 2006, 213, 66–81. [Google Scholar] [CrossRef]
- Milia-Argeiti, E.; Mourah, S.; Vallée, B.; Huet, E.; Karamanos, N.K.; Theocharis, A.D.; Menashi, S. EMMPRIN/CD147-Encriched Membrane Vesicles Released from Malignant Human Testicular Germ Cells Increase MMP Production through Tumor–Stroma Interaction. Biochim. Et Biophys. Acta (BBA)-General. Subj. 2014, 1840, 2581–2588. [Google Scholar] [CrossRef]
- Kozlova, N.; Grossman, J.E.; Iwanicki, M.P.; Muranen, T. The Interplay of the Extracellular Matrix and Stromal Cells as a Drug Target in Stroma-Rich Cancers. Trends Pharmacol. Sci. 2020, 41, 183–198. [Google Scholar] [CrossRef]
- Anderson, N.M.; Simon, M.C. The Tumor Microenvironment. Curr. Biol. 2020, 30, R921–R925. [Google Scholar] [CrossRef]
- Müller, M.R.; Skowron, M.A.; Albers, P.; Nettersheim, D. Molecular and Epigenetic Pathogenesis of Germ Cell Tumors. Asian J. Urol. 2021, 8, 144–154. [Google Scholar] [CrossRef]
- Klein, B.; Haggeney, T.; Fietz, D.; Indumathy, S.; Loveland, K.L.; Hedger, M.; Kliesch, S.; Weidner, W.; Bergmann, M.; Schuppe, H.-C. Specific Immune Cell and Cytokine Characteristics of Human Testicular Germ Cell Neoplasia. Human. Reprod. 2016, 31, 2192–2202. [Google Scholar] [CrossRef]
- Skowron, M.A.; Eul, K.; Stephan, A.; Ludwig, G.F.; Wakileh, G.A.; Bister, A.; Söhngen, C.; Raba, K.; Petzsch, P.; Poschmann, G.; et al. Profiling the 3D Interaction between Germ Cell Tumors and Microenvironmental Cells at the Transcriptome and Secretome Level. Mol. Oncol. 2022, 16, 3107–3127. [Google Scholar] [CrossRef] [PubMed]
- Bellmunt, J.; Powles, T.; Vogelzang, N.J. A Review on the Evolution of PD-1/PD-L1 Immunotherapy for Bladder Cancer: The Future Is Now. Cancer Treat. Rev. 2017, 54, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Fankhauser, C.D.; Curioni-Fontecedro, A.; Allmann, V.; Beyer, J.; Tischler, V.; Sulser, T.; Moch, H.; Bode, P.K. Frequent PD-L1 Expression in Testicular Germ Cell Tumors. Br. J. Cancer 2015, 113, 411–413. [Google Scholar] [CrossRef] [PubMed]
- Cierna, Z.; Mego, M.; Miskovska, V.; Machalekova, K.; Chovanec, M.; Svetlovska, D.; Hainova, K.; Rejlekova, K.; Macak, D.; Spanik, S.; et al. Prognostic Value of Programmed-Death-1 Receptor (PD-1) and Its Ligand 1 (PD-L1) in Testicular Germ Cell Tumors. Ann. Oncol. 2016, 27, 300–305. [Google Scholar] [CrossRef]
- Jennewein, L.; Bartsch, G.; Gust, K.; Kvasnicka, H.-M.; Haferkamp, A.; Blaheta, R.; Mittelbronn, M.; Harter, P.N.; Mani, J. Increased Tumor Vascularization Is Associated with the Amount of Immune Competent PD-1 Positive Cells in Testicular Germ Cell Tumors. Oncol. Lett. 2018, 15, 9852–9860. [Google Scholar] [CrossRef] [PubMed]
- Chovanec, M.; Cierna, Z.; Miskovska, V.; Machalekova, K.; Svetlovska, D.; Kalavska, K.; Rejlekova, K.; Spanik, S.; Kajo, K.; Babal, P.; et al. Prognostic Role of Programmed-Death Ligand 1 (PD-L1) Expressing Tumor Infiltrating Lymphocytes in Testicular Germ Cell Tumors. Oncotarget 2017, 8, 21794–21805. [Google Scholar] [CrossRef]
- Siska, P.J.; Johnpulle, R.A.N.; Zhou, A.; Bordeaux, J.; Kim, J.Y.; Dabbas, B.; Dakappagari, N.; Rathmell, J.C.; Rathmell, W.K.; Morgans, A.K.; et al. Deep Exploration of the Immune Infiltrate and Outcome Prediction in Testicular Cancer by Quantitative Multiplexed Immunohistochemistry and Gene Expression Profiling. OncoImmunology 2017, 6, e1305535. [Google Scholar] [CrossRef] [PubMed]
- Pęksa, R.; Kunc, M.; Popęda, M.; Piątek, M.; Bieńkowski, M.; Żok, J.; Starzyńska, A.; Perdyan, A.; Sowa, M.; Duchnowska, R.; et al. Combined Assessment of Immune Checkpoint Regulator VISTA on Tumor-Associated Immune Cells and Platelet-to-Lymphocyte Ratio Identifies Advanced Germ Cell Tumors with Higher Risk of Unfavorable Outcomes. Cancers 2021, 13, 1750. [Google Scholar] [CrossRef]
- Lobo, J.; Rodrigues, Â.; Guimarães, R.; Cantante, M.; Lopes, P.; Maurício, J.; Oliveira, J.; Jerónimo, C.; Henrique, R. Detailed Characterization of Immune Cell Infiltrate and Expression of Immune Checkpoint Molecules PD-L1/CTLA-4 and MMR Proteins in Testicular Germ Cell Tumors Disclose Novel Disease Biomarkers. Cancers 2019, 11, 1535. [Google Scholar] [CrossRef]
- Sadigh, S.; Farahani, S.J.; Shah, A.; Vaughn, D.; Lal, P. Differences in PD-L1–Expressing Macrophages and Immune Microenvironment in Testicular Germ Cell Tumors. Am. J. Clin. Pathol. 2020, 153, 387–395. [Google Scholar] [CrossRef]
- Imamoglu, G.I.; Eren, T.; Baylan, B.; Karacın, C. May High Levels of Systemic Immune-Inflammation Index and Hematologic Inflammation Markers Suggest a Further Stage in Testicular Tumours? Urol. Int. 2019, 103, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Chovanec, M.; Cierna, Z.; Miskovska, V.; Machalekova, K.; Kalavska, K.; Rejlekova, K.; Svetlovska, D.; Macak, D.; Spanik, S.; Kajo, K.; et al. Systemic Immune-Inflammation Index in Germ-Cell Tumours. Br. J. Cancer 2018, 118, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Fankhauser, C.D.; Sander, S.; Roth, L.; Gross, O.; Eberli, D.; Sulser, T.; Seifert, B.; Beyer, J.; Hermanns, T. Systemic Inflammatory Markers Have Independent Prognostic Value in Patients with Metastatic Testicular Germ Cell Tumours Undergoing First-Line Chemotherapy. Br. J. Cancer 2018, 118, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Ribnikar, D.; Stukalin, I.; Bedard, P.L.; Hamilton, R.J.; Jewett, M.; Warde, P.; Chung, P.; Anson-Cartwright, L.; Templeton, A.J.; Amir, E.; et al. The Prognostic Value of Neutrophil-to-Lymphocyte Ratio in Metastatic Testicular Cancer. Curr. Oncol. 2021, 28, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Cursano, M.C.; Kopf, B.; Scarpi, E.; Menna, C.; Casadei, C.; Schepisi, G.; Lolli, C.; Altavilla, A.; Gallà, V.; Santini, D.; et al. Prognostic Role of Systemic Inflammatory Indexes in Germ Cell Tumors Treated with High-Dose Chemotherapy. Front. Oncol. 2020, 10, 1325. [Google Scholar] [CrossRef]
- Chovanec, M.; Mego, M.; Cholujova, D.; Gronesova, P.; Miskovska, V.; Sycova-Mila, Z.; Usakova, V.; Svetlovska, D.; Bujdak, P.; Spanik, S.; et al. A Cytokine and Angiogenic Factor (CAF) Analysis in Plasma in Testicular Germ Cell Tumor Patients (TGCTs). JCO 2015, 33, e15552. [Google Scholar] [CrossRef]
- Chen, G.; Emens, L.A. Chemoimmunotherapy: Reengineering Tumor Immunity. Cancer Immunol. Immunother. 2013, 62, 203–216. [Google Scholar] [CrossRef]
- Chemnitz, J.M.; Parry, R.V.; Nichols, K.E.; June, C.H.; Riley, J.L. SHP-1 and SHP-2 Associate with Immunoreceptor Tyrosine-Based Switch Motif of Programmed Death 1 upon Primary Human T Cell Stimulation, but Only Receptor Ligation Prevents T Cell Activation. J. Immunol. 2004, 173, 945–954. [Google Scholar] [CrossRef]
- Jackaman, C.; Majewski, D.; Fox, S.A.; Nowak, A.K.; Nelson, D.J. Chemotherapy Broadens the Range of Tumor Antigens Seen by Cytotoxic CD8+ T Cells in Vivo. Cancer Immunol. Immunother. 2012, 61, 2343–2356. [Google Scholar] [CrossRef]
- Wan, S.; Pestka, S.; Jubin, R.G.; Lyu, Y.L.; Tsai, Y.-C.; Liu, L.F. Chemotherapeutics and Radiation Stimulate MHC Class I Expression through Elevated Interferon-Beta Signaling in Breast Cancer Cells. PLoS ONE 2012, 7, e32542. [Google Scholar] [CrossRef]
- Tsavaris, N.; Kosmas, C.; Vadiaka, M.; Kanelopoulos, P.; Boulamatsis, D. Immune Changes in Patients with Advanced Breast Cancer Undergoing Chemotherapy with Taxanes. Br. J. Cancer 2002, 87, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Michels, T.; Shurin, G.V.; Naiditch, H.; Sevko, A.; Umansky, V.; Shurin, M.R. Paclitaxel Promotes Differentiation of Myeloid-Derived Suppressor Cells into Dendritic Cells in Vitro in a TLR4-Independent Manner. J. Immunotoxicol. 2012, 9, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Le, D.T.; Jaffee, E.M. Regulatory T-Cell Modulation Using Cyclophosphamide in Vaccine Approaches: A Current Perspective. Cancer Res. 2012, 72, 3439–3444. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.M.; Wilson, N.S.; Waithman, J.; Villadangos, J.A.; Carbone, F.R.; Heath, W.R.; Belz, G.T. Cognate CD4+ T Cell Licensing of Dendritic Cells in CD8+ T Cell Immunity. Nat. Immunol. 2004, 5, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Al-Hogbani, M.; Duguay, J.; Wagner, D.C.; Haferkamp, A.; Joubert, P.; Frees, S.; Rendon, R.; Power, N.; Périgny, M.; Toren, P. Expression of programmed death ligand-1 (PD-L1) in metastatic and postchemotherapy viable testicular germ cell tumors. Urol. Oncol. 2021, 39, 303.e1–303.e8. [Google Scholar] [CrossRef] [PubMed]
- Kourie, H.R.; Awada, G.; Awada, A.H. Learning from the “Tsunami” of Immune Checkpoint Inhibitors in 2015. Crit. Rev. Oncol./Hematol. 2016, 101, 213–220. [Google Scholar] [CrossRef]
- Zschäbitz, S.; Lasitschka, F.; Hadaschik, B.; Hofheinz, R.-D.; Jentsch-Ullrich, K.; Grüner, M.; Jäger, D.; Grüllich, C. Response to Anti-Programmed Cell Death Protein-1 Antibodies in Men Treated for Platinum Refractory Germ Cell Cancer Relapsed after High-Dose Chemotherapy and Stem Cell Transplantation. Eur. J. Cancer 2017, 76, 1–7. [Google Scholar] [CrossRef]
- Chi, E.A.; Schweizer, M.T. Durable Response to Immune Checkpoint Blockade in a Platinum-Refractory Patient With Nonseminomatous Germ Cell Tumor. Clin. Genitourin. Cancer 2017, 15, e855–e857. [Google Scholar] [CrossRef]
- Loh, K.P.; Fung, C. Novel Therapies in Platinum-Refractory Metastatic Germ Cell Tumor: A Case Report with a Focus on a PD-1 Inhibitor. Rare Tumors 2017, 9, 47–49. [Google Scholar] [CrossRef]
- Adra, N.; Einhorn, L.H.; Althouse, S.K.; Ammakkanavar, N.R.; Musapatika, D.; Albany, C.; Vaughn, D.; Hanna, N.H. Phase II Trial of Pembrolizumab in Patients with Platinum Refractory Germ-Cell Tumors: A Hoosier Cancer Research Network Study GU14-206. Ann. Oncol. 2018, 29, 209–214. [Google Scholar] [CrossRef]
- Tsimberidou, A.-M.; Vo, H.H.; Subbiah, V.; Janku, F.; Piha-Paul, S.; Yilmaz, B.; Gong, J.; Naqvi, M.F.; Tu, S.-M.; Campbell, M.; et al. Pembrolizumab in Patients with Advanced Metastatic Germ Cell Tumors. Oncologist 2021, 26, 558–e1098. [Google Scholar] [CrossRef]
- Mego, M.; Svetlovska, D.; Chovanec, M.; Rečkova, M.; Rejlekova, K.; Obertova, J.; Palacka, P.; Sycova-Mila, Z.; De Giorgi, U.; Mardiak, J. Phase II Study of Avelumab in Multiple Relapsed/Refractory Germ Cell Cancer. Investig. New Drugs 2019, 37, 748–754. [Google Scholar] [CrossRef]
- Necchi, A.; Giannatempo, P.; Raggi, D.; Mariani, L.; Colecchia, M.; Farè, E.; Monopoli, F.; Calareso, G.; Ali, S.M.; Ross, J.S.; et al. An Open-Label Randomized Phase 2 Study of Durvalumab Alone or in Combination with Tremelimumab in Patients with Advanced Germ Cell Tumors (APACHE): Results from the First Planned Interim Analysis. Eur. Urol. 2019, 75, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Albany, C.; Einhorn, L.; Garbo, L.; Boyd, T.; Josephson, N.; Feldman, D.R. Treatment of CD30-Expressing Germ Cell Tumors and Sex Cord Stromal Tumors with Brentuximab Vedotin: Identification and Report of Seven Cases. Oncologist 2018, 23, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Necchi, A.; Magazzu, D.; Anichini, A.; Raggi, D.; Giannatempo, P.; Nicolai, N.; Colecchia, M.; Paolini, B.; Coradeschi, E.; Tassi, E.; et al. An Open-Label, Single-Group, Phase 2 Study of Brentuximab Vedotin as Salvage Therapy for Males with Relapsed Germ-Cell Tumors (GCT): Results at the End of First Stage (FM12GCT01). JCO 2016, 34, 480. [Google Scholar] [CrossRef]
- Ashkar, R.; Feldman, D.R.; Adra, N.; Zaid, M.A.; Funt, S.A.; Althouse, S.K.; Perkins, S.M.; Snow, C.I.; Lazzara, K.M.; Sego, L.M.; et al. Phase II Trial of Brentuximab Vedotin in Relapsed/Refractory Germ Cell Tumors. Investig. New Drugs 2021, 39, 1656–1663. [Google Scholar] [CrossRef]
- Hinsch, A.; Blessin, N.C.; Simon, R.; Kluth, M.; Fischer, K.; Hube-Magg, C.; Li, W.; Makrypidi-Fraune, G.; Wellge, B.; Mandelkow, T.; et al. Expression of the Immune Checkpoint Receptor TIGIT in Seminoma. Oncol. Lett. 2019, 18, 1497–1502. [Google Scholar] [CrossRef]
- Das, M.; Zhu, C.; Kuchroo, V.K. Tim-3 and Its Role in Regulating Anti-Tumor Immunity. Immunol. Rev. 2017, 276, 97–111. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Cao, J.; Zhao, C.; Li, X.; Zhou, C.; Hirsch, F.R. TIM-3, a Promising Target for Cancer Immunotherapy. OTT 2018, 11, 7005–7009. [Google Scholar] [CrossRef] [PubMed]
- Long, L.; Zhang, X.; Chen, F.; Pan, Q.; Phiphatwatchara, P.; Zeng, Y.; Chen, H. The Promising Immune Checkpoint LAG-3: From Tumor Microenvironment to Cancer Immunotherapy. Genes Cancer 2018, 9, 176–189. [Google Scholar] [CrossRef]
- Tu, L.; Guan, R.; Yang, H.; Zhou, Y.; Hong, W.; Ma, L.; Zhao, G.; Yu, M. Assessment of the Expression of the Immune Checkpoint Molecules PD-1, CTLA4, TIM-3 and LAG-3 across Different Cancers in Relation to Treatment Response, Tumor-Infiltrating Immune Cells and Survival. Int. J. Cancer 2020, 147, 423–439. [Google Scholar] [CrossRef] [PubMed]
- Nair, R.; Westin, J. CAR T-Cells. Adv. Exp. Med. Biol. 2020, 1244, 215–233. [Google Scholar] [CrossRef] [PubMed]
- Pantuck, M.; Palaskas, N.; Drakaki, A. Next Generation T-Cell Therapy for Genitourinary Malignancies, Part A: Introduction and Current State of the Art. Cancer Treat. Res. Commun. 2018, 17, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, J.A.; Reidy, A.; Mirandola, L.; Trotter, K.; Suvorava, N.; Figueroa, A.; Konala, V.; Aulakh, A.; Littlefield, L.; Grizzi, F.; et al. Chimeric Antigen Receptor Engineering: A Right Step in the Evolution of Adoptive Cellular Immunotherapy. Int. Rev. Immunol. 2015, 34, 154–187. [Google Scholar] [CrossRef]
- Katari, U.L.; Keirnan, J.M.; Worth, A.C.; Hodges, S.E.; Leen, A.M.; Fisher, W.E.; Vera, J.F. Engineered T Cells for Pancreatic Cancer Treatment. HPB 2011, 13, 643–650. [Google Scholar] [CrossRef] [PubMed]
- Martino, M.; Naso, V.; Loteta, B.; Canale, F.A.; Pugliese, M.; Alati, C.; Musuraca, G.; Nappi, D.; Gaimari, A.; Nicolini, F.; et al. Chimeric Antigen Receptor T-Cell Therapy: What We Expect Soon. Int. J. Mol. Sci. 2022, 23, 13332. [Google Scholar] [CrossRef]
- Mackensen, A.; Haanen, J.B.a.G.; Koenecke, C.; Alsdorf, W.; Wagner-Drouet, E.; Heudobler, D.; Borchmann, P.; Bokemeyer, C.; Klobuch, S.; Smit, E.; et al. LBA38 BNT211-01: A Phase I Trial to Evaluate Safety and Efficacy of CLDN6 CAR T Cells and CLDN6-Encoding MRNA Vaccine-Mediated in Vivo Expansion in Patients with CLDN6-Positive Advanced Solid Tumours. Ann. Oncol. 2022, 33, S1404–S1405. [Google Scholar] [CrossRef]
- Söhngen, C.; Thomas, D.J.; Skowron, M.A.; Bremmer, F.; Eckstein, M.; Stefanski, A.; Driessen, M.D.; Wakileh, G.A.; Stühler, K.; Altevogt, P.; et al. CD24 targeting with NK-CAR immunotherapy in testis, prostate, renal and (luminal-type) bladder cancer and identification of direct CD24 interaction partners. FEBS J. 2023, 290, 4864–4876. [Google Scholar] [CrossRef]
- Ganguli, N.; Kumari, P.; Dash, S.; Samanta, D. Molecular and structural basis of TIGIT: Nectin-4 interaction, a recently discovered pathway crucial for cancer immunotherapy. Biochem. Biophys. Res. Commun. 2023, 677, 31–37. [Google Scholar] [CrossRef]
- Lazar, V.; Zhang, B.; Magidi, S.; Le Tourneau, C.; Raymond, E.; Ducreux, M.; Bresson, C.; Raynaud, J.; Wunder, F.; Onn, A.; et al. A transcriptomics approach to expand therapeutic options and optimize clinical trials in oncology. Ther. Adv. Med. Oncol. 2023, 15, 17588359231156382. [Google Scholar] [CrossRef]
- Zhao, J.; Qin, L.; He, G.; Xie, T.; Hu, G.; Wang, F.; Zhong, H.; Zhu, J.; Xu, Y. Administration of a glypican-3 peptide increases the infiltration and cytotoxicity of CD8+ T cells against testicular yolk sac tumor, associated with enhancing the intratumoral cGAS/STING signaling. Cancer Med. 2023, 12, 21293–21307. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, Y.A.G.; Qu, C.; Chen, J. Pan-Cancer Analysis of PARP1 Alterations as Biomarkers in the Prediction of Immunotherapeutic Effects and the Association of Its Expression Levels and Immunotherapy Signatures. Front. Immunol. 2021, 12, 721030. [Google Scholar] [CrossRef]
- Zhou, Z.; Xu, S.; Jiang, L.; Tan, Z.; Wang, J. A Systematic Pan-Cancer Analysis of CASP3 as a Potential Target for Immunotherapy. Front. Mol. Biosci. 2022, 9, 776808. [Google Scholar] [CrossRef]
- Bo, H.; Zhu, F.; Liu, Z.; Deng, Q.; Liu, G.; Li, R.; Zhu, W.; Tan, Y.; Liu, G.; Fan, J.; et al. Integrated analysis of high-throughput sequencing data reveals the key role of LINC00467 in the invasion and metastasis of testicular germ cell tumors. Cell Death Discov. 2021, 7, 206. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Wang, S.; Jiang, Z.; Tang, L.; Liu, Z.; Cao, J.; Hu, Z.; Chen, X.; Luo, Y.; Bo, H. Long Non-Coding RNA RFPL3S Functions as a Biomarker of Prognostic and Immunotherapeutic Prediction in Testicular Germ Cell Tumor. Front. Immunol. 2022, 13, 859730. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Gao, J.; Li, X.; Gao, R.; Lu, X.; Zhou, J.; Yan, F.; Wang, H.; Liu, Y.; Hao, Z.; et al. TIMEAS, a promising method for the stratification of testicular germ cell tumor patients with distinct immune microenvironment, clinical outcome and sensitivity to frontline therapies. Cell Oncol. 2023, 46, 745–759. [Google Scholar] [CrossRef] [PubMed]
- Lobo, J.; Constâncio, V.; Leite-Silva, P.; Guimarães, R.; Cantante, M.; Braga, I.; Maurício, J.; Looijenga, L.H.J.; Henrique, R.; Jerónimo, C. Differential methylation EPIC analysis discloses cisplatin-resistance related hypermethylation and tumor-specific heterogeneity within matched primary and metastatic testicular germ cell tumor patient tissue samples. Clin. Epigenetics 2021, 13, 70. [Google Scholar] [CrossRef]
- Sanborn, R.E.; Hamid, O.; de Vries, E.G.; Ott, P.A.; Garcia-Corbacho, J.; Boni, V.; Bendell, J.; Autio, K.A.; Cho, D.C.; Plummer, R.; et al. CX-072 (pacmilimab), a Probody PD-L1 inhibitor, in combination with ipilimumab in pa-tients with advanced solid tumors (PROCLAIM-CX-072): A first-in-human, dose-finding study. J. Immunother. Cancer 2021, 9, e002446. [Google Scholar] [CrossRef]
- Del Giudice, F.; Kasman, A.M.; De Berardinis, E.; Busetto, G.M.; Belladelli, F.; Eisenberg, M.L. Association between male infertility and male-specific malignancies: Systematic review and meta-analysis of population-based retrospective cohort studies. Fertil. Steril. 2020, 114, 984–996. [Google Scholar] [CrossRef]
| Immune Factor | Function | Clinical Relevance | Ref |
|---|---|---|---|
| Collagen I/IV Fibronectin | extracellular matrix proteins | cisplatin resistance | [21] |
| PD-L1 (cancer cells) (TILs) | immune evasion | non-seminoma (choriocarcinoma), advanced stage, elevated serum markers, metastases, short PFS, short OS, higher CPS in metastases and postchemo seminoma low-risk IGCCCG group, better prognosis | [23,24,45] [26] |
| T-cell and NK-cell signatures | immune activation | early stage | [27] |
| Treg, neutrophil, mast cell, and macrophage signatures | immune evasion | advanced stage | [27] |
| VISTA | immune activation | choriocarcinoma, prolonged PFS, prolonged OS | [28] |
| CTLA-4 (TILs) | immune evasion | LVI (-) and lower pT and N stages | [29] |
| NLR, LMR, SII | systemic inflammation | high-risk IGCCCG, short PFS, short OS | [31,32,33,34,35] |
| Immunotherapy | Study Type | Results | Ref. |
|---|---|---|---|
| Nivolumab, Pembrolizumab | retrospective | 2/7 patients PR | [45] |
| Nivolumab | case report | SD × 14 mos | [46] |
| Pembrolizumab | case report | POD after 1 cycle | [47] |
| Pembrolizumab | phase II | 2/12 patients SD | [48] |
| Pembrolizumab | phase II | 3/12 patients SD | [49] |
| Avelumab | phase II | 8/8 POD, mPFS 0.9 mos, mOS 2.7 mos | [50] |
| Durvalumab + Tremelimumab | phase II | 1/22 patients PR 1/22 patients SD | [51] |
| Brentuximab vedotin | phase II | 2/7 patients PR | [52] |
| Brentuximab vedotin | phase II | 7/9 STM response, ORR 22.2% (1 CR + 1 PR), 3-month PFS 11.1% 6-month OS 85.7% | [53] |
| Brentuximab vedotin | phase II | 6/18 patients SD, 5/18 STM response | [54] |
| CLDN6 CAR-T cells | phase I | DCR 85%, ORR 57% including 1 CR | [65] |
| CX-072 (pacmilimab) | phase I | 1 PR for >12 months | [76] |
| Enfortumab Vedotin +/− Pembrolizumab | phase II | Primary endpoint: ORR (ongoing study) | NCT06041503 |
| Ipilimumab + Nivolumab + Cabozantinib | phase II | Primary endpoint: ORR (ongoing study) | NCT03866382 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Evmorfopoulos, K.; Marsitopoulos, K.; Karachalios, R.; Karathanasis, A.; Dimitropoulos, K.; Tzortzis, V.; Zachos, I.; Vlachostergios, P.J. The Immune Landscape and Immunotherapeutic Strategies in Platinum-Refractory Testicular Germ Cell Tumors. Cancers 2024, 16, 428. https://doi.org/10.3390/cancers16020428
Evmorfopoulos K, Marsitopoulos K, Karachalios R, Karathanasis A, Dimitropoulos K, Tzortzis V, Zachos I, Vlachostergios PJ. The Immune Landscape and Immunotherapeutic Strategies in Platinum-Refractory Testicular Germ Cell Tumors. Cancers. 2024; 16(2):428. https://doi.org/10.3390/cancers16020428
Chicago/Turabian StyleEvmorfopoulos, Konstantinos, Konstantinos Marsitopoulos, Raphael Karachalios, Athanasios Karathanasis, Konstantinos Dimitropoulos, Vassilios Tzortzis, Ioannis Zachos, and Panagiotis J. Vlachostergios. 2024. "The Immune Landscape and Immunotherapeutic Strategies in Platinum-Refractory Testicular Germ Cell Tumors" Cancers 16, no. 2: 428. https://doi.org/10.3390/cancers16020428
APA StyleEvmorfopoulos, K., Marsitopoulos, K., Karachalios, R., Karathanasis, A., Dimitropoulos, K., Tzortzis, V., Zachos, I., & Vlachostergios, P. J. (2024). The Immune Landscape and Immunotherapeutic Strategies in Platinum-Refractory Testicular Germ Cell Tumors. Cancers, 16(2), 428. https://doi.org/10.3390/cancers16020428






