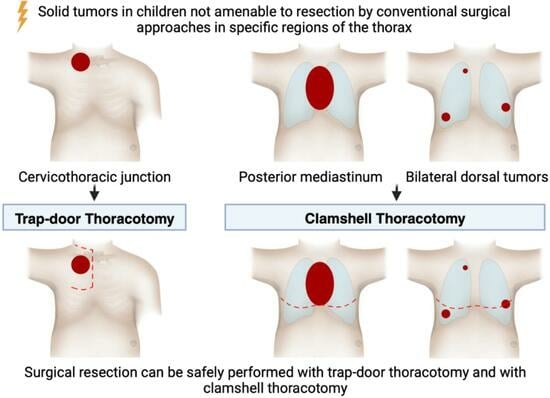
Trap-Door Thoracotomy and Clamshell Thoracotomy as Surgical Approaches for Neuroblastoma and Other Thoracic Tumors in Children
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Trap-Door Thoracotomy
2.3. Clamshell Thoracotomy
2.4. Demographic and Clinical Characteristics
2.5. Surgical and Oncological Data
2.6. Statistical Analysis
3. Results
3.1. Trap-Door Thoracotomy
3.2. Clamshell Thoracotomy
| Variable | All (n = 26) | Trap-Door (n = 14) | Clamshell (n = 12) |
|---|---|---|---|
| Operative time [minutes] * | 197 (104–424) | 207 (122–424) | 179 (104–381) |
| Resection with neurosurgery [n] | 7 (26.9%) | 7 (26.9%) | 0 |
| Intermittent neuromonitoring [n] | 8 (30.8%) | 8 (30.8%) | 0 |
| Resection status | |||
| MCE (neuroblastoma) ** | 11 (42.3%) | 7 (26.9%) | 4 (15.4%) |
| R0 resection (other tumors) | 14 (53.9%) | 7 (26.9%) | 7 (26.9%) |
| MCE (all tumor entities) ** | 25 (96.2%) | 14 (53.8%) | 11 (42.3%) |
| Biopsy | 1 (3.9%) | 0 | 1 (3.9%) |
| Duration of ventilation [days] * | 1 (0–6) | 1 (0–5) | 1 (0–6) |
| Duration of chest tube [days] * | 6 (1–14) | 6 (3–11) | 6 (1–14) |
| Length of ICU stay [days] * | 2 (1–12) | 3 (1–12) | 2 (1–8) |
| Length of hospital stay [days] * | 10 (6–35) | 9 (6–22) | 14 (7–35) |
| Complications [n] *** | 17 (54.2%) | 9 (25%) | 8 (29.2%) |
| 7 (26.9%) | 7 (26.9%) | 0 |
| Diaphragm paresis | 6 (23.1%) | 5 (19.2%) | 1 (3.9%) |
| Pleural effusion | 3 (11.5%) | 2 (7.7%) | 1 (3.9%) |
| Paresis after nerve resection | 3 (11.5%) | 3 (11.5%) | 0 |
| 2 (7.7%) | 2 (7.7%) | 0 |
| 2 (7.7%) | 0 | 2 (7.7%) |
| Pleural effusion | 1 (3.9%) | 0 | 1 (3.9%) |
| Chest wall hematoma | 1 (3.9%) | 1 (3.9%) | 0 |
| Pathology result differs from biopsy [n] | 8 (30.8%) | 6 (23.1%) | 2 (7.7%) |
| Adjuvant chemotherapy [n] | 18 (69.2%) | 8 (30.8%) | 10 (38.5%) |
| Adjuvant radiotherapy [n] | 5 (19.2%) | 3 (11.5%) | 2 (7.7%) |
| Follow-up [months] * | 8 (0–60) | 10 (5–21) | 7 (0–60) |
| Lost to follow-up | 9 (34.6%) | 4 (15.4%) | 4 (15.5%) |
| Tumor recurrence [n] | 7 (38.8%) | 4 (22.2%) | 3 (16.7%) |
| Oncological outcome [n] | |||
| Complete remission | 6 (33.3%) | 4 (22.2%) | 3 (16.7%) |
| Local control | 5 (27.8%) | 4 (22.2%) | 1 (5.6%) |
| Progress | 2 (11.1%) | 1 (5.6%) | 1 (5.6%) |
| Death | 4 (22.2%) | 1 (5.6%) | 3 (16.7%) |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Häcker, F.-M.; Schweinitz, D.V.; Gambazzi, F. The Relevance of Surgical Therapy for Bilateral and/or Multiple Pulmonary Metastases in Children. Eur. J. Pediatr. Surg. 2007, 17, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Zarroug, A.E.; Hamner, C.E.; Pham, T.H.; Houghton, S.G.; Stavlo, P.; Moir, C.R.; Rodeberg, D.A. Bilateral Staged versus Bilateral Simultaneous Thoracotomy in the Pediatric Population. J. Pediatr. Surg. 2006, 41, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Kiely, E. A Technique for Excision of Abdominal and Pelvic Neuroblastomas. Annals 2007, 89, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, J.; Urla, C.; Sparber-Sauer, M.; Schuck, A.; Leuschner, I.; Klingebiel, T.; Blumenstock, G.; Seitz, G.; Koscielniak, E. Treatment and Outcome of Patients with Localized Intrathoracic and Chest Wall Rhabdomyosarcoma: A Report of the Cooperative Weichteilsarkom Studiengruppe (CWS). J. Cancer Res. Clin. Oncol. 2018, 144, 925–934. [Google Scholar] [CrossRef] [PubMed]
- Briccoli, A.; Rocca, M.; Salone, M.; Guzzardella, G.A.; Balladelli, A.; Bacci, G. High Grade Osteosarcoma of the Extremities Metastatic to the Lung: Long-Term Results in 323 Patients Treated Combining Surgery and Chemotherapy, 1985–2005. Surg. Oncol. 2010, 19, 193–199. [Google Scholar] [CrossRef]
- Morgan, K.M.; Siow, V.S.; Strotmeyer, S.; Gow, K.W.; Malek, M.M. Characteristics and Outcomes in Pediatric Non-Central Nervous System Malignant Rhabdoid Tumors: A Report from the National Cancer Database. Ann. Surg. Oncol. 2022, 29, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Tronc, F.; Conter, C.; Marec-Berard, P.; Bossard, N.; Remontet, L.; Orsini, A.; Gamondes, J.-P.; Louis, D. Prognostic Factors and Long-Term Results of Pulmonary Metastasectomy for Pediatric Histologies. Eur. J. Cardio-Thorac. Surg. 2008, 34, 1240–1246. [Google Scholar] [CrossRef]
- Masaoka, A.; Ito, Y.; Yasumitsu, T. Anterior Approach for Tumor of the Superior Sulcus. J. Thorac. Cardiovasc. Surg. 1979, 78, 413–415. [Google Scholar] [CrossRef] [PubMed]
- Lebreton, G.; Baste, J.-M.; Thumerel, M.; Delcambre, F.; Velly, J.-F.; Jougon, J. The Hemiclamshell Approach in Thoracic Surgery: Indications and Associated Morbidity in 50 Patients. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 965–969. [Google Scholar] [CrossRef]
- Dartevelle, P.G.; Chapelier, A.R.; Macchiarini, P.; Lenot, B.; Cerrina, J.; Roy Ladurie, F.L.; Parquin, F.J.F.; Lafont, D.; Deslauriers, J. Anterior Transcervical-Thoracic Approach for Radical Resection of Lung Tumors Invading the Thoracic Inlet. J. Thorac. Cardiovasc. Surg. 1993, 105, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Bains, M.S.; Ginsberg, R.J.; Jones, W.G.; McCormack, P.M.; Rusch, V.W.; Burt, M.E.; Martini, N. The Clamshell Incision: An Improved Approach to Bilateral Pulmonary and Mediastinal Tumor. Ann. Thorac. Surg. 1994, 58, 30–33. [Google Scholar] [CrossRef]
- Abbo, O.; Guatta, R.; Pinnagoda, K.; Joseph, J.-M. Bilateral Anterior Sternothoracotomy (Clamshell Incision): A Suitable Alternative for Bilateral Lung Sarcoma Metastasis in Children. World J. Surg. Onc. 2014, 12, 233. [Google Scholar] [CrossRef]
- Chui, C.H.; Thirugnanam, A. Trapdoor Anterior Thoracotomy for Cervicothoracic and Apical Thoracic Neuroblastoma in Children. Pediatr. Surg. Int. 2020, 36, 891–895. [Google Scholar] [CrossRef] [PubMed]
- De Corti, F.; Avanzini, S.; Cecchetto, G.; Buffa, P.; Guida, E.; Zanon, G.F.; Jasonni, V. The Surgical Approach for Cervicothoracic Masses in Children. J. Pediatr. Surg. 2012, 47, 1662–1668. [Google Scholar] [CrossRef]
- Christison-Lagay, E.R.; Darcy, D.G.; Stanelle, E.J.; DaSilva, S.; Avila, E.; La Quaglia, M.P. “Trap-Door” and “Clamshell” Surgical Approaches for the Management of Pediatric Tumors of the Cervicothoracic Junction and Mediastinum. J. Pediatr. Surg. 2014, 49, 172–177. [Google Scholar] [CrossRef]
- Schmidt, A.; Hempel, J.-M.; Ellerkamp, V.; Warmann, S.W.; Ernemann, U.; Fuchs, J. The Relevance of Preoperative Identification of the Adamkiewicz Artery in Posterior Mediastinal Pediatric Tumors. Ann. Surg. Oncol. 2022, 29, 493–499. [Google Scholar] [CrossRef]
- Brisse, H.J.; McCarville, M.B.; Granata, C.; Krug, K.B.; Wootton-Gorges, S.L.; Kanegawa, K.; Giammarile, F.; Schmidt, M.; Shulkin, B.L.; Matthay, K.K.; et al. Guidelines for Imaging and Staging of Neuroblastic Tumors: Consensus Report from the International Neuroblastoma Risk Group Project. Radiology 2011, 261, 243–257. [Google Scholar] [CrossRef]
- Kiely, E.M. Radical Surgery for Abdominal Neuroblastoma. Semin. Surg. Oncol. 1993, 9, 489–492. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications: A New Proposal With Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann. Surg. 2004, 240, 205. [Google Scholar] [CrossRef]
- La Quaglia, M.P.; Kushner, B.H.; Su, W.; Heller, G.; Kramer, K.; Abramson, S.; Rosen, N.; Wolden, S.; Cheung, N.-K.V. The Impact of Gross Total Resection on Local Control and Survival in High-Risk Neuroblastoma. J. Pediatr. Surg. 2004, 39, 412–417; discussion 412–417. [Google Scholar] [CrossRef] [PubMed]
- Fischer, J.; Pohl, A.; Volland, R.; Hero, B.; Dübbers, M.; Cernaianu, G.; Berthold, F.; von Schweinitz, D.; Simon, T. Complete Surgical Resection Improves Outcome in INRG High-Risk Patients with Localized Neuroblastoma Older than 18 Months. BMC Cancer 2017, 17, 520. [Google Scholar] [CrossRef]
- Holmes, K.; Pötschger, U.; Pearson, A.D.J.; Sarnacki, S.; Cecchetto, G.; Gomez-Chacon, J.; Squire, R.; Freud, E.; Bysiek, A.; Matthyssens, L.E.; et al. Influence of Surgical Excision on the Survival of Patients with Stage 4 High-Risk Neuroblastoma: A Report from the HR-NBL1/SIOPEN Study. J. Clin. Oncol. 2020, 38, 2902–2915. [Google Scholar] [CrossRef]
- Urla, C.; Warmann, S.W.; Schmidt, A.; Mayer, B.; Handgretinger, R.; Neunhoeffer, F.; Schäfer, J.; Fuchs, J. Two-Cavities Approach for Resection of Pediatric Abdominal Neuroblastic Tumors: Experience of a National Reference Pediatric Onco-Surgical Center. J. Cancer Res. Clin. Oncol. 2023, 149, 1485–1493. [Google Scholar] [CrossRef]
- Weber, T.; Mätzl, J.; Rokitansky, A.; Klimscha, W.; Neumann, K.; Deusch, E. Superior Postoperative Pain Relief with Thoracic Epidural Analgesia versus Intravenous Patient-Controlled Analgesia after Minimally Invasive Pectus Excavatum Repair. J. Thorac. Cardiovasc. Surg. 2007, 134, 865–870. [Google Scholar] [CrossRef] [PubMed]
- El Madi, A.; Irtan, S.; Sauvat, F.; Zérah, M.; Schleiermacher, G.; Galmiche-Roland, L.; Minard-Colin, V.; Brisse, H.; Sarnacki, S. Long-Term Results of the Transmanubrial Osteomuscular-Sparing Approach for Pediatric Tumors. Pediatr. Blood Cancer 2017, 64, e26527. [Google Scholar] [CrossRef]
- Schubert, C.; Grimm, A.-S.; Stahl, J.-H.; Küpper, H.; Kegele, J.; Wittlinger, J.; Serna-Higuita, L.; Winter, N.; Groeschel, S.; Grimm, A. Nerve Ultrasound Reference Data in Children from Two to Seven Years. Clin. Neurophysiol. 2020, 131, 859–865. [Google Scholar] [CrossRef] [PubMed]
- Sala, F.; Kržan, M.J.; Deletis, V. Intraoperative Neurophysiological Monitoring in Pediatric Neurosurgery: Why, When, How? Childs Nerv. Syst. 2002, 18, 264–287. [Google Scholar] [CrossRef] [PubMed]
- Li, W.W.L.; Lee, T.W.; Yim, A.P.C. Shoulder Function after Thoracic Surgery. Thorac. Surg. Clin. 2004, 14, 331–343. [Google Scholar] [CrossRef]
- Sauvat, F.; Brisse, H.; Magdeleinat, P.; Lopez, M.; Philippe-Chomette, P.; Orbach, D.; Aerts, I.; Brugieres, L.; Revillon, Y.; Sarnacki, S. The Transmanubrial Approach: A New Operative Approach to Cervicothoracic Neuroblastoma in Children. Surgery 2006, 139, 109–114. [Google Scholar] [CrossRef]
- Ferrari, A.; Brecht, I.B.; Koscielniak, E.; Casanova, M.; Scagnellato, A.; Bisogno, G.; Alaggio, R.; Cecchetto, G.; Catania, S.; Meazza, C.; et al. The Role of Adjuvant Chemotherapy in Children and Adolescents with Surgically Resected, High-Risk Adult-Type Soft Tissue Sarcomas. Pediatr. Blood Cancer 2005, 45, 128–134. [Google Scholar] [CrossRef]


| Variable | All (n = 26) | Trap-Door (n = 14) | Clamshell (n = 12) |
|---|---|---|---|
| Sex [n] | |||
| Female | 17 (65.4%) | 8 (30.8%) | 9 (34.6%) |
| Male | 9 (34.6%) | 6 (23%) | 3 (11.5%) |
| Median age at diagnosis [months] (range) | 51 (4–205) | 50 (4–151) | 42 (11–205) |
| Tumor entity [n] | |||
| Neuroblastoma | 12 (46.2%) | 6 (23.1%) | 6 (23.1%) |
| Malignant rhabdoid tumor | 4 (15.4%) | 4 (15.4%) | 0 |
| Ewing sarcoma | 1 (3.9%) | 1 (3.9%) | 0 |
| Rhabdomyosarcoma | 1 (3.9%) | 0 | 1 (3.9%) |
| Inflammatory myofibroblastic tumor | 1 (3.9%) | 1 (3.9%) | 0 |
| Metastatic disease | 7 (26.9%) | 1 (3.9%) | 6 (23.1%) |
| Osteosarcoma | 3 (11.5%) | 1 (3.9%) | 2 (7.7%) |
| Neuroblastoma | 1 (3.9%) | 0 | 1 (3.9%) |
| Malignant rhabdoid tumor | 1 (3.9%) | 0 | 1 (3.9%) |
| Hepatoblastoma | 1 (3.9%) | 0 | 1 (3.9%) |
| Renal clear cell sarcoma | 1 (3.9%) | 0 | 1 (3.9%) |
| Tumor localization [n] | |||
| Mediastinum | 12 (46.2%) | 4 (15.4%) | 8 (29.2%) |
| Cervicothoracic junction | 6 (23.1%) | 6 (23.1%) | 0 |
| Thoracic inlet | 4 (15.4%) | 4 (15.4%) | 0 |
| Bilateral dorsal thorax | 4 (15.4%) | 0 | 4 (15.4%) |
| Affected structures [n] | |||
| Major vessels encased | 21 (80.8%) | 12 (46.2%) | 9 (34.6%) |
| Nerves and neuroforamina | 16 (61.5%) | 12 (46.2%) | 4 (15.4%) |
| Trachea and bronchi | 7 (26.9%) | 3 (11.5%) | 4 (15.4%) |
| Esophagus | 7 (26.9%) | 2 (7.7%) | 5 (19.2%) |
| Pericardium | 5 (19.2%) | 1 (3.9%) | 4 (15.4%) |
| Preoperative symptoms [n] | 11 (42.3%) | 8 (30.8%) | 3 (11.5%) |
| Horner syndrome | 3 (11.5%) | 3 (11.5%) | 0 |
| Respiratory insufficiency | 3 (11.5%) | 1 (3.9%) | 2 (8.3%) |
| Paresis upper limb | 2 (7.7%) | 2 (7.7%) | 0 |
| Pain upper limb | 2 (7.7%) | 2 (7.7%) | 0 |
| Upper inflow congestion | 2 (7.7%) | 1 (3.9%) | 1 (3.9%) |
| Lymph edema upper limb | 1 (3.9%) | 1 (3.9%) | 0 |
| Neoadjuvant chemotherapy [n] | 24 (92.3%) | 13 (50%) | 11 (42.3%) |
| Preoperative imaging [n] | |||
| Magnetic resonance imaging | 21 (80.8%) | 13 (50%) | 8 (30.8%) |
| Computed tomography | 12 (46.2%) | 3 (11.5%) | 9 (34.6%) |
| Spinal angiography | 7 (26.9%) | 2 (7.7%) | 5 (19.2%) |
| Ultrasound of peripheral nerve | 3 (11.5%) | 3 (11.5%) | 0 |
| Cerebral angiography | 1 (3.9%) | 1 (3.9%) | 0 |
| Median age at surgery [months] (range) | 54 (8–229) | 54 (8–176) | 53 (18–229) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayer, B.F.B.; Schunn, M.C.; Urla, C.; Schäfer, J.F.; Fideler, F.; Neunhoeffer, F.; Schuhmann, M.U.; Warmann, S.W.; Fuchs, J. Trap-Door Thoracotomy and Clamshell Thoracotomy as Surgical Approaches for Neuroblastoma and Other Thoracic Tumors in Children. Cancers 2024, 16, 373. https://doi.org/10.3390/cancers16020373
Mayer BFB, Schunn MC, Urla C, Schäfer JF, Fideler F, Neunhoeffer F, Schuhmann MU, Warmann SW, Fuchs J. Trap-Door Thoracotomy and Clamshell Thoracotomy as Surgical Approaches for Neuroblastoma and Other Thoracic Tumors in Children. Cancers. 2024; 16(2):373. https://doi.org/10.3390/cancers16020373
Chicago/Turabian StyleMayer, Benjamin F. B., Matthias C. Schunn, Cristian Urla, Jürgen F. Schäfer, Frank Fideler, Felix Neunhoeffer, Martin U. Schuhmann, Steven W. Warmann, and Jörg Fuchs. 2024. "Trap-Door Thoracotomy and Clamshell Thoracotomy as Surgical Approaches for Neuroblastoma and Other Thoracic Tumors in Children" Cancers 16, no. 2: 373. https://doi.org/10.3390/cancers16020373
APA StyleMayer, B. F. B., Schunn, M. C., Urla, C., Schäfer, J. F., Fideler, F., Neunhoeffer, F., Schuhmann, M. U., Warmann, S. W., & Fuchs, J. (2024). Trap-Door Thoracotomy and Clamshell Thoracotomy as Surgical Approaches for Neuroblastoma and Other Thoracic Tumors in Children. Cancers, 16(2), 373. https://doi.org/10.3390/cancers16020373