Carcinoma In Situ (CIS): Is There a Difference in Efficacy between Various BCG Strains? A Comprehensive Review of the Literature
Simple Summary
Abstract
1. Introduction
2. Evidence Synthesis
3. Randomized Controlled Trials
4. Phase II Trials and Prospective Studies
5. Retrospective Studies
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bhindi, B.; Kool, R.; Kulkarni, G.S.; Siemens, D.R.; Aprikian, A.G.; Breau, R.H.; Brimo, F.; Fairey, A.; French, C.; Hanna, N.; et al. Canadian Urological Association Guideline on the Management of Non-Muscle-Invasive Bladder Cancer—Full-Text. Can. Urol. Assoc. J. 2021, 15, E424–E460. [Google Scholar] [CrossRef]
- Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Escrig, J.L.D.; Gontero, P.; Liedberg, F.; Masson-Lecomte, A.; Mostafid, A.H.; et al. European Association of Urology Guidelines on Non–muscle-invasive Bladder Cancer (Ta, T1, and Carcinoma in Situ). Eur. Urol. 2022, 81, 75–94. [Google Scholar] [CrossRef]
- Casey, R.G.; Catto, J.W.; Cheng, L.; Cookson, M.S.; Herr, H.; Shariat, S.; Witjes, J.A.; Black, P.C. Diagnosis and management of urothelial carcinoma in situ of the Lower Urinary Tract: A Systematic Review. Eur. Urol. 2015, 67, 876–888. [Google Scholar] [CrossRef]
- Kamat, A.M.; Hahn, N.M.; Efstathiou, J.A.; Lerner, S.P.; Malmström, P.U.; Choi, W.; Guo, C.C.; Lotan, Y.; Kassouf, W. Bladder cancer. Lancet 2016, 388, 2796–2810. [Google Scholar] [CrossRef]
- van Rhijn, B.W.; Hentschel, A.E.; Bründl, J.; Compérat, E.M.; Hernández, V.; Čapoun, O.; Bruins, H.M.; Cohen, D.; Rouprêt, M.; Shariat, S.F.; et al. Prognostic Value of the WHO1973 and WHO2004/2016 Classification Systems for Grade in Primary Ta/T1 Non–muscle-invasive Bladder Cancer: A Multicenter European Association of Urology Non–muscle-invasive Bladder Cancer Guidelines Panel Study. Eur. Urol. Oncol. 2021, 4, 182–191. [Google Scholar] [CrossRef]
- Sylvester, R.J.; Rodríguez, O.; Hernández, V.; Turturica, D.; Bauerová, L.; Bruins, H.M.; Bründl, J.; van der Kwast, T.H.; Brisuda, A.; Rubio-Briones, J.; et al. European Association of Urology (EAU) prognostic factor risk groups for non–muscle-invasive bladder cancer (NMIBC) incorporating the WHO 2004/2016 and WHO 1973 classification systems for grade: An update from the EAU NMIBC guidelines panel. Eur. Urol. 2021, 79, 480–488. [Google Scholar] [CrossRef]
- Subiela, J.D.; Faba, O.R.; Ramos, F.G.; Reyes, H.V.; Pisano, F.; Breda, A.; Palou, J. Carcinoma in situ of the urinary bladder: A systematic review of current knowledge regarding detection, treatment, and outcomes. Eur. Urol. Focus 2020, 6, 674–682. [Google Scholar] [CrossRef]
- Chade, D.C.; Shariat, S.F.; Godoy, G.; Savage, C.J.; Cronin, A.M.; Bochner, B.H.; Donat, S.M.; Herr, H.W.; Dalbagni, G.L. Clinical outcomes of primary bladder carcinoma in situ in a contemporary series. J. Urol. 2010, 184, 74–80. [Google Scholar] [CrossRef]
- Chade, D.C.; Shariat, S.F.; Adamy, A.; Bochner, B.H.; Donat, S.M.; Herr, H.W.; Dalbagni, G. Clinical outcome of primary versus secondary bladder carcinoma in situ. J. Urol. 2010, 184, 464–469. [Google Scholar] [CrossRef]
- Russo, G.I.; Sholklapper, T.N.; Cocci, A.; Broggi, G.; Caltabiano, R.; Smith, A.B.; Lotan, Y.; Morgia, G.; Kamat, A.M.; Witjes, J.A.; et al. Performance of narrow band Imaging (NBI) and photodynamic diagnosis (PDD) fluorescence imaging compared to white light cystoscopy (WLC) in detecting non-muscle invasive bladder cancer: A systematic review and lesion-level diagnostic meta-analysis. Cancers 2021, 13, 4378. [Google Scholar] [CrossRef]
- Xiong, Y.; Li, J.; Ma, S.; Ge, J.; Zhou, L.; Li, D.; Chen, Q. A meta-analysis of narrow band imaging for the diagnosis and therapeutic outcome of non-muscle invasive bladder cancer. PLoS ONE 2017, 12, e0170819. [Google Scholar] [CrossRef]
- Chen, C.; Huang, H.; Zhao, Y.; Liu, H.; Sylvester, R.; Lin, T.; Huang, J. Diagnostic performance of image technique based transurethral resection for non-muscle invasive bladder cancer: Systematic review and diagnostic meta-analysis. BMJ Open 2019, 9, e028173. [Google Scholar] [CrossRef]
- Burger, M.; Grossman, H.B.; Droller, M.; Schmidbauer, J.; Hermann, G.; Drăgoescu, O.; Ray, E.; Fradet, Y.; Karl, A.; Burgués, J.P.; et al. Photodynamic diagnosis of non–muscle-invasive bladder cancer with hexami-nolevulinate cystoscopy: A meta-analysis of detection and recurrence based on Raw Data. Eur. Urol. 2013, 64, 846–854. [Google Scholar] [CrossRef]
- Bladder Cancer Staging: Bladder Cancer Stages. The American Cancer Society. Available online: https://www.cancer.org/cancer/bladder-cancer/detection-diagnosis-staging/staging.html (accessed on 23 January 2023).
- Dyrskjøt, L.; Kruhøffer, M.; Thykjaer, T.; Marcussen, N.; Jensen, J.L.; Møller, K.; Ørntoft, T.F. Gene expression in the urinary bladder: A common carcinoma in situ gene expression signature exists disregarding histopathological classification. Cancer Res. 2004, 64, 4040–4048. [Google Scholar] [CrossRef]
- Heer, R.; Lewis, R.; Vadiveloo, T.; Yu, G.; Mariappan, P.; Cresswell, J.; McGrath, J.; Nabi, G.; Mostafid, H.; Lazarowicz, H.; et al. A Randomized Trial of PHOTOdynamic Surgery in Non–Muscle-Invasive Bladder Cancer. NEJM Evid. 2022, 1, EVIDoa2200092. [Google Scholar] [CrossRef]
- Lamm, D.L.; Morales, A. A BCG success story: From prevention of tuberculosis to optimal bladder cancer treatment. Vaccine 2021, 39, 7308–7318. [Google Scholar] [CrossRef]
- Lobo, N.; Brooks, N.A.; Zlotta, A.R.; Cirillo, J.D.; Boorjian, S.; Black, P.C.; Meeks, J.J.; Bivalacqua, T.J.; Gontero, P.; Steinberg, G.D.; et al. 100 years of bacillus calmette–Guérin immunotherapy: From cattle to COVID-19. Nat. Rev. Urol. 2021, 18, 611–622. [Google Scholar] [CrossRef]
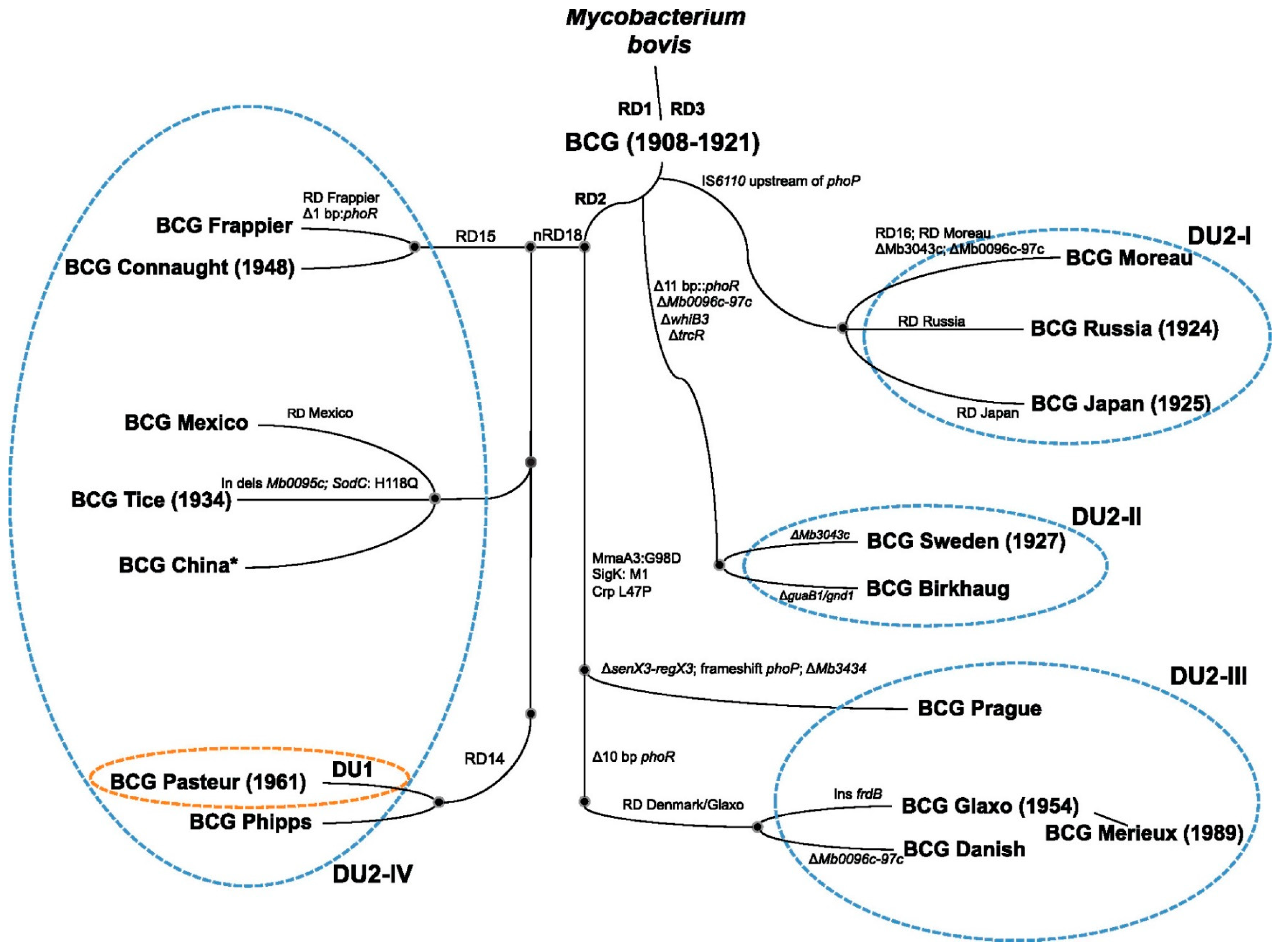
- Bottai, D.; Brosch, R. The BCG Strain Pool: Diversity Matters. Mol. Ther. J. Am. Soc. Gene Ther. 2016, 24, 201–203. [Google Scholar] [CrossRef]
- Gan, C.; Mostafid, H.; Khan, M.S.; Lewis, D.J.M. BCG immunotherapy for bladder cancer—The effects of substrain differences. Nat. Rev. Urol. 2013, 10, 580–588. [Google Scholar] [CrossRef]
- Rentsch, C.A.; Birkhäuser, F.D.; Biot, C.; Gsponer, J.R.; Bisiaux, A.; Wetterauer, C.; Lagranderie, M.; Marchal, G.; Orgeur, M.; Bouchier, C.; et al. Bacillus Calmette-Guérin strain differences have an impact on clinical outcome in Bladder Cancer immunotherapy. Eur. Urol. 2014, 66, 677–688. [Google Scholar] [CrossRef]
- Inamoto, T.; Ubai, T.; Nishida, T.; Fujisue, Y.; Katsuoka, Y.; Azuma, H. Comparable effect with minimal morbidity of low-dose Tokyo 172 strain compared with regular dose Connaught strain as an intravesical bacillus Calmette-Guérin prophylaxis in nonmuscle invasive bladder cancer: Results of a randomized prospective comparison. Urol. Ann. 2013, 5, 7–12. [Google Scholar] [CrossRef]
- Sengiku, A.; Ito, M.; Miyazaki, Y.; Sawazaki, H.; Takahashi, T.; Ogura, K. A prospective comparative study of intravesical Bacillus Calmette-Guérin therapy with the Tokyo or Connaught strain for nonmuscle invasive bladder cancer. J. Urol. 2013, 190, 50–54. [Google Scholar] [CrossRef]
- Mukherjee, A.; Persad, R.; Smith, P.J. Intravesical BCG treatment for superficial bladder cancer: Long-term results using two dif-ferent strains of BCG. Br. J. Urol. 1992, 69, 147–150. [Google Scholar] [CrossRef]
- Fellows, G.J.; Parmar, M.K.; Grigor, K.M.; Hall, R.R.; Heal, M.R.; Wallace, D.M. Marker tumour response to Evans and Pasteur Bacille Calmette-Guérin in multiple recurrent PTA/PT1 bladder tumours: Report from the Medical Research Council subgroup on superficial bladder cancer (Urological Cancer Working Party). Br. J. Urol. 1994, 73, 639–644. [Google Scholar] [CrossRef]
- Unda-Urzaiz, M.; Cozar-Olmos, J.; Miñana-Lopez, B.; Camarero-Jimenez, J.; Brugarolas-Rossello, X.; Zubiaur-Libano, C.; Ribal-Caparros, M.; Suarez-Charneco, A.; Rodriguez-Tesedo, V.; Chantada-Abal, V.; et al. Safety and efficacy of various strains of Bacille Calmette–Guérin in the treatment of bladder tumors in standard clinical practice. Actas Urológicas Españolas 2018, 42, 238–248. [Google Scholar] [CrossRef]
- Tan, G.H.; Kuk, C.; Zlotta, A.R. Are there differences among Bacillus Calmette-Guérin (BCG) strains regarding their clinical efficacy in the treatment of non-muscle invasive bladder cancer? The jury is still out but the answer is likely no. Can. Urol. Assoc. J. 2020, 14, E54–E56. [Google Scholar] [CrossRef]
- Niwa, N.; Kikuchi, E.; Matsumoto, K.; Kosaka, T.; Mizuno, R.; Oya, M. Does switching the bacillus Calmette-Guérin strain affect clinical outcome in patients with recurrent non–muscle-invasive bladder cancer after initial bacillus Calmette-Guérin therapy? Urol. Oncol. Semin. Orig. Investig. 2018, 36, 306.e1–306.e8. [Google Scholar] [CrossRef]
- Zlotta, A.R.; Van Vooren, J.-P.; Denis, O.; Drowart, A.; Daffé, M.; Lefèvre, P.; Schandene, L.; De Cock, M.; De Bruyn, J.; Vandenbussche, P.; et al. What are the immunologically active components of bacille Calmette-Guérin in therapy of superficial bladder cancer? Int. J. Cancer 2000, 87, 844–852. [Google Scholar] [CrossRef]
- Nese, N.; Gupta, R.; Bui, M.H.T.; Amin, M.B. Carcinoma in situ of the urinary bladder: Review of clinicopathologic characteristics with an emphasis on aspects related to molecular diagnostic techniques and prognosis. J. Natl. Compr. Cancer Netw. 2009, 7, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Kaasinen, E.; Wijkström, H.; Rintala, E.; Mestad, O.; Jahnson, S.; Malmström, P.U. Seventeen-year follow-up of the prospective randomized Nordic CIS study: BCG monotherapy versus alternating therapy with mitomycin C and BCG in patients with carcinoma in situ of the urinary bladder. Scand. J. Urol. 2016, 50, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Yokomizo, A.; Kanimoto, Y.; Okamura, T.; Ozono, S.; Koga, H.; Iwamura, M.; Tanaka, H.; Takahashi, S.; Tsushima, T.; Naito, S.; et al. Randomized controlled study of the efficacy, safety and quality of life with low dose bacillus Calmette-Guérin instillation therapy for nonmuscle invasive bladder cancer. J. Urol. 2016, 195, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Koga, H.; Ozono, S.; Tsushima, T.; Tomita, K.; Horiguchi, Y.; Usami, M.; Hirao, Y.; Akaza, H.; Naito, S.; BCG Tokyo Strain Study Group. Maintenance intravesical bacillus Calmette-Guérin instillation for TA, T1 cancer and carcinoma in situ of the bladder: Randomized controlled trial by the BCG Tokyo Strain Study Group. Int. J. Urol. 2010, 17, 759–766. [Google Scholar] [CrossRef] [PubMed]
- de Reijke, T.M.; Kurth, K.H.; Sylvester, R.J.; Hall, R.R.; Brausi, M.; van de Beek, K.E.; Landsoght, K.E.; Carpentier, P. Bacillus Calmette-Guerin versus epirubicin for primary, secondary or concurrent carcinoma in situ of the bladder: Results of a European organization for the research and treatment of cancer—Genito-urinary group phase III trial (30906). J. Urol. 2005, 173, 405–409. [Google Scholar] [CrossRef] [PubMed]
- MartÍNez-PiÑEiro, J.A.; Martínez-Piñeiro, L.; Solsona, E.; RodrÍGuez, R.H.; FernÁNdez GÓMez, J.M.; MartÍN, M.G.; Molina, J.R.; Collado, A.G.; Flores, N.; Isorna, S.; et al. Has a 3-fold decreased dose of bacillus calmette-guerin the same efficacy against recurrences and progression of T1G3 and tis bladder tumors than the standard dose? Results of a prospective ran-domized trial. J. Urol. 2005, 174 Pt 1, 1242–1247. [Google Scholar] [CrossRef]
- Lamm, D.L.; Blumenstein, B.A.; Crissman, J.D.; Montie, J.E.; Gottesman, J.E.; Lowe, B.A.; Sarosdy, M.F.; Bohl, R.D.; Grossman, H.B.; Beck, T.M.; et al. Maintenance bacillus Calmette-Guerin immunotherapy for recurrent TA, T1 and carcinoma in situ transitional cell carcinoma of the bladder: A randomized southwest oncology group study. J. Urol. 2000, 163, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Jakse, G.; Hall, R.; Bono, A.; Höltl, W.; Carpentier, P.; Spaander, J.; van der Meijden, A.; Sylvester, R. Intravesical BCG in patients with carcinoma in situ of the urinary bladder: Long–term results of EORTC GU Group Phase II protocol 30861. Eur. Urol. 2001, 40, 144–150. [Google Scholar] [CrossRef]
- De Kernion, J.B.; Huang, M.Y.; Lindner, A.; Smith, R.B.; Kaufman, J.J. The management of superficial bladder tumors and carcinoma in situ with in-travesical bacillus Calmette-Guerin. J. Urol. 1985, 133, 598–600. [Google Scholar] [CrossRef]
- Rosevear, H.M.; Lightfoot, A.J.; Birusingh, K.K.; Maymí, J.L.; Nepple, K.G.; O’Donnell, M.A.; National BCG/Interferon Investigator Group. Factors affecting response to bacillus Calmette-Guérin plus interferon for urothelial carcinoma in situ. J. Urol. 2011, 186, 817–823. [Google Scholar] [CrossRef]
- Gofrit, O.N.; Pode, D.; Pizov, G.; Zorn, K.C.; Katz, R.; Duvdevani, M.; Shapiro, A. The natural history of bladder carcinoma in situ after initial response to bacillus Calmette-Gúerin immunotherapy. Urol. Oncol. Semin. Orig. Investig. 2009, 27, 258–262. [Google Scholar] [CrossRef]
- Takenaka, A.; Yamada, Y.; Miyake, H.; Hara, I.; Fujisawa, M. Clinical outcomes of bacillus Calmette-Guérin instillation therapy for carcinoma in situ of urinary bladder. Int. J. Urol. 2008, 15, 309–313. [Google Scholar] [CrossRef]
- Mugiya, S.; Ozono, S.; Nagata, M.; Takayama, T.; Ito, T.; Maruyama, S.; Hadano, S.; Nagae, H. Long-term outcome of a low-dose intravesical bacillus Calmette–Guerin therapy for carcinoma in situ of the bladder: Results after six successive instillations of 40 mg BCG. Ultrasound Med. Biol. 2005, 35, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Sood, R.; Sharma, H.; Sharma, B.; Parekh, S.; Pujari, P.; Shewale, S. A prospective comparative study to assess the efficacy and tolerability of 2 different doses of intravesical bacillus Calmette-Guerin (BCG) in patients with non–muscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2020, 38, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Ferro, M.; Chiujdea, S.; Musi, G.; Lucarelli, G.; Del Giudice, F.; Hurle, R.; Damiano, R.; Cantiello, F.; Mari, A.; de Cobelli, O.; et al. Impact of age on outcomes of patients with pure carcinoma in situ of the bladder: Mul-ti-institutional cohort analysis. Clin. Genitourin. Cancer 2022, 20, e166–e172. [Google Scholar] [CrossRef] [PubMed]
- Del Giudice, F.; Busetto, G.M.; Gross, M.S.; Maggi, M.; Sciarra, A.; Salciccia, S.; Ferro, M.; Sperduti, I.; Flammia, S.; Canale, V.; et al. Efficacy of three BCG strains (Connaught, Tice and RIVM) with or without sec-ondary resection (re-TUR) for intermediate/high-risk non-muscle-invasive bladder cancers: Results from a retrospective sin-gle-institution cohort analysis. J. Cancer Res. Clin. Oncol. 2021, 147, 3073–3080. [Google Scholar] [CrossRef] [PubMed]
- Hurle, R.; Lazzeri, M.; Saita, A.; Naselli, A.; Guarneri, A.; Buffi, N.M.; Lughezzani, G.; Fasulo, V.; Mondellini, G.M.; Paciotti, M.; et al. Predictive factors for progression of patients with carcinoma in situ of the bladder at long-term follow-up: Pure versus non-pure CIS. Minerva Urol. Nefrol. 2019, 71, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Sallami, S.; Khouni, H.; Ben Atta, M.; El Makarim, S.A.; Zouari, M.B.; Ben Rhouma, S. Long-term outcome of intravesical bacillus Calmette-Guérin therapy with maintenance for urinary bladder carcinoma in situ: About 47 cases. Tunis. Med. 2016, 94, 844. [Google Scholar] [PubMed]
- Witjes, J.A.; Dalbagni, G.; Karnes, R.J.; Shariat, S.; Joniau, S.; Palou, J.; Serretta, V.; Larré, S.; di Stasi, S.; Colombo, R.; et al. The efficacy of BCG Tice and BCG Connaught in a cohort of 2,099 patients with T1G3 non–muscle-invasive bladder cancer. Urol. Oncol. Semin. Orig. Investig. 2016, 34, 484.e19–484.e25. [Google Scholar] [CrossRef]
- Takashi, M.; Wakai, K.; Hattori, T.; Furuhashi, K.; Ono, Y.; Ohshima, S.; Ohno, Y. Multivariate evaluation of factors affecting recurrence, progression, and survival in patients with superficial bladder cancer treated with intravesical bacillus Calmette-Guerin (Tokyo 172 strain) therapy: Signif-icance of concomitant carcinoma in situ. Int. Urol. Nephrol. 2002, 33, 41–47. [Google Scholar] [CrossRef]
- D’andrea, D.; Soria, F.; Abufaraj, M.; Pones, M.; Gontero, P.; Machado, A.T.; Waksman, R.; Enikeev, D.V.; Glybochko, P.V.; Adonias, S.P.; et al. Comparative effectiveness of intravesical BCG-Tice and BCG-Moreau in patients with non-muscle-invasive bladder cancer. Clin. Genitourin. Cancer 2020, 18, 20–25.e2. [Google Scholar] [CrossRef]
- Del Giudice, F.; Flammia, R.S.; Chung, B.I.; Moschini, M.; Pradere, B.; Mari, A.; Soria, F.; Albisinni, S.; Krajewski, W.; Szydełko, T.; et al. Compared efficacy of adjuvant intravesical BCG-TICE vs. BCG-RIVM for high-risk non-muscle invasive bladder cancer (NMIBC): A propensity score matched analysis. Cancers 2022, 14, 887. [Google Scholar] [CrossRef]
- Nowak, Ł.; Krajewski, W.; Moschini, M.; Chorbińska, J.; Poletajew, S.; Tukiendorf, A.; Muilwijk, T.; Joniau, S.; Tafuri, A.; Antonelli, A.; et al. Assessment of the oncological outcomes of three different bacillus Calmette–Guérin strains in patients with high-grade T1 non-muscle-invasive bladder cancer. Arab. J. Urol. 2021, 19, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Koguchi, D.; Matsumoto, K.; Hirayama, T.; Moroo, S.; Kobayashi, M.; Katsumata, H.; Ikeda, M.; Iwamura, M. Impact of maintenance therapy using a half dose of the bacillus Calmette–Guérin Tokyo strain on recurrence of intermediate and high-risk nonmuscle invasive bladder cancer: A retrospective single-center study. BMC Urol. 2020, 20, 194. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, T.R.L.; Charlton, M.; E Neal, D.; Powell, P.H. Treatment of carcinoma in situ with intravesical bacillus Calmette-Guerin without maintenance. J. Urol. 2002, 167, 2408–2412. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.; Pietzak, E. Immune mechanisms and molecular therapeutic strategies to enhance immunotherapy in non-muscle invasive bladder cancer: Invited review for special issue “Seminar: Treatment Advances and Molecular Biology Insights in Urothelial Carcinoma”. Urol. Oncol. Semin. Orig. Investig. 2023, 41, 398–409. [Google Scholar] [CrossRef]
- Svatek, R.S.; Tangen, C.; Delacroix, S.; Lowrance, W.; Lerner, S.P. Background and Update for S1602 “A Phase III Randomized Trial to Evaluate the Influence of BCG Strain Differences and T Cell Priming with Intradermal BCG Before Intravesical Therapy for BCG-naïve High-grade Non-muscle-invasive Bladder Cancer. Eur. Urol. Focus. 2018, 4, 522–524. [Google Scholar] [CrossRef]
| Study | Strain | Schedule | Median Follow-Up | Number of CIS Patients | CRR | RFS | PFS | OS |
|---|---|---|---|---|---|---|---|---|
| Rentsch et al. (2014) [21] | Connaught vs. Tice | 6 weeks vs. 6 weeks | 47.6 months | CIS (any type): 31 vs. 26 | NA | 74% vs. 48%, p = 0.011 | 94.1% vs. 87.9%, p = 0.344 | 84.9% vs. 93.6%, p = 0.265 |
| Kaasinen et al. (2016) [31] | Connaught | BCG 6 weeks + 10 months vs. MMC 6 weeks + BCG/MMC, 10 months alternating | 119 months | Primary CIS: 91 Secondary CIS: 129 Concomitant CIS: 84 | NA | 26% reduction in risk of recurrence (BCG group). Risk of recurrence was significantly higher in primary CIS vs. concomitant CIS (HR = 0.66, p = 0.043) | No difference (BCG vs. MMC/BCG). Disease progression most likely in concomitant CIS, least likely in primary CIS (HR = 0.57, p = 0.055) | No difference (BCG vs. MMC/BCG) |
| Yokomizo et al. (2016) [32] | Tokyo | 8 weeks SD vs. 1/2D | NA | Pure CIS: 65 Ta + CIS: 46 T1 + CIS: 34 | 85% SD vs. 78% 1/2D (no difference between CIS groups) | No difference | No difference | No difference |
| Koga et al. (2010) [33] | Tokyo | 8 weeks vs. 8 weeks + 4 months Maintenance for 8 weeks | 28.7 months | CIS (any type): 46 | 77% | 74.1% (8 week) vs. 95.8% (M) at 2 years | No difference | 92.6% vs. 97.1% (M) |
| de Reijke et al. (2005) [34] | Connaught | BCG (6 weeks + 3 weeks/3 years) vs. epirubicin (8 weeks + 3 weeks/3 years) | 67 months | Primary CIS: 39 Secondary CIS: 41 Concurrent CIS: 88 | 63% vs. 60% (epi vs. BCG) 59% vs. 63% (epi vs. BCG) 51% vs. 69% (epi vs. BCG) | NA | NA | NA |
| Martínez-Piñeiro et al. (2005) [35] | Connaught | BCG (6 weeks + Q2W × 6) SD vs. 1/3D | 61 months | Primary CIS: 23 Associated CIS: 42 | NA | 61.9% (SD) vs. 49.8% (1/3D) at 5 years (no difference between CIS groups) | 74.3% (SD) vs. 73.5% (1/3D) at 5 years (no difference between CIS groups) | NA |
| Lamm et al. (2000) [36] | Connaught | 6 weeks vs. 6 weeks + (M) (3 weeks/3 years) | Until death | CIS (any type): 278 | 68.1% (6 week) vs. 83.8% (M) | 41% (6 weeks) vs. 60% (M) at 5 years | 70% (6 weeks) vs. 76% (M) at 5 years | 78% vs. 83% (M) |
| Study | Design | Strain | Schedule | Median Follow-Up | Number of CIS Patients | CRR | RFS | PFS | OS |
|---|---|---|---|---|---|---|---|---|---|
| Jakse et al. (2001) [37] | Phase II trial | Connaught | 6 weeks (+6 weeks if no CR) | 91.2 months | CIS (any type): 103 | 75% | NA | NA | NA |
| deKernion et al. (1985) [38] | Phase II trial | TICE | 8 weeks + 12 months | NA | CIS (any type): 19 | 68% | NA | NA | NA |
| Rosevear et al. (2011) [39] | Phase II trial | TICE or Connaught + Interferon-α | 6 weeks + 3 weeks/15 months BCG mixed with 50 MU IFN-α-2b | 24 months | Pure CIS: 146 Papillary + CIS: 85 (CIS + Ta: 45; CIS + T1: 36; CIS + Ta + T1: 4) | No difference in pure CIS vs. papillary + CIS groups * | NA | NA | NA |
| Study | Strain | Schedule | Median Follow-Up | Number of CIS Patients | CRR | RFS | PFS | OS |
|---|---|---|---|---|---|---|---|---|
| Sengiku et al. (2013) [23] | Tokyo vs. Connaught | Single course (6–8 doses) | 855 days | pTis: 14; Papillary + CIS: 17 pTis: 15; Papillary + CIS: 5 | 90.3% 85% | 61.8% at 5 years 56% at 5 years | NA | NA |
| Gofrit et al. (2009) [40] | Connaught | 6 weeks induction, 46% received maintenance | 75 months | Pure CIS: 38 Concomitant CIS: 66 | NA | 63% and 54% at 5 and 10 years (no difference between CIS groups) | 79% and 77% at 5 and 10 years (no difference between CIS groups) | 56.7% (no difference between CIS groups) |
| Takenaka et al. (2008) [41] | Tokyo | 8 weeks | 37.5 months | Primary CIS: 62 Secondary CIS: 63 Concomitant CIS: 60 | 86.5% (no difference between CIS groups) | 66% at 5 years (no difference between CIS groups) | 78.5% at 5 years (no difference between CIS groups) | NA |
| Mugiya et al. (2005) [42] | Tokyo | BCG 1/2D 6 weeks | 54 months | Primary CIS: 13 Secondary CIS: 30 | 85% 83% | 61.9% at 5 years (no difference between CIS groups) | NA | NA |
| Sood et al. (2020) [43] | Moscow, Russian I (80 mg vs. 120 mg) | 6 weeks + 3 weeks/3 years | 36 months | Intermediate- and high-risk NMIBC with or without CIS: 51 (80 mg) vs. 53 (120 mg) | NA | 84.31% (80 mg) vs. 86.79% (120 mg) at 3 years | 84.31% (80 mg) vs. 94.34% (120 mg) at 3 years | NA |
| Study | Strain | Schedule | Median Follow-Up | Number of CIS Patients | CRR | RFS | PFS | OS |
|---|---|---|---|---|---|---|---|---|
| Chade et al. (2010) [8] | Tokyo | 6 weeks + 1 reinduction (if necessary) | 3.3–4.0 years | Primary CIS: 155 | NA | 63.2% * | 55.5% | NA |
| Ferro et al. (2022) [44] | Unspecified | 6 weeks + 3 weeks/3 years | 53 months (RFS); 120 months (PFS) | Primary CIS: 172 | NA | 47.7% | 76.2% | NA |
| Del Giudice et al. (2021) [45] | Connaught vs. TICE vs. RIVM | 6 weeks + 3 weeks/3 years | 72 months 73 months 67 months | pTis: 9; Papillary + CIS: 23 pTis: 8; Papillary + CIS: 15 pTis: 13 Papillary + CIS: 18 | NA | 54.1% at 5 years 61.3% at 5 years 60.2% at 5 years | 74.7% at 5 years 81% at 5 years 78.2% at 5 years | NA |
| Hurle et al. (2019) [46] | Unspecified | 6 weeks + 3 weeks/3 years | 103 months | Pure CIS: 98 Non-pure CIS: 51 | NA | NA | 86% 71% | 81% 78% |
| Sallami et al. (2016) [47] | Pasteur | 6 weeks + 6 monthly | 67.5 months | Primary CIS: 13 Concomitant CIS: 28 Secondary CIS: 6 | 68% (no difference between CIS groups) | 84.6% at 5 years 64.3% at 5 years 50% at 5 years | 87.2% at 5 years (no difference between CIS groups) | 95.7% (no difference between CIS groups) |
| Witjes et al. (2016) [48] | Connaught vs. TICE | 59% received maintenance 18% received maintenance | 62.4 months | Papillary: 731; Papillary + CIS: 226 Papillary: 841; Papillary + CIS: 301 | NA | 54.1% 45.3% | 78.8% 81.5% | 73.1% 74.8% |
| Takashi et al. (2002) [49] | Tokyo | 8 or 10 week | 64.7 months | No concomitant CIS: 112 (65 received 40mg BCG, 47 received 80mg BCG) With concomitant CIS: 34 (26 received 40mg BCG, 8 received 80mg BCG) | NA | 69/112 (61.6%) 18/34 (52.9%) | 90% at 5 years 70% at 5 years | 87% at 5 years 73% at 5 years |
| D’Andrea et al. (2020) [50] | TICE vs. Moreau | 6-week induction 8-week induction + 6 week maintenance | 41 months | Ta or T1: 311 (72 with concomitant CIS); Tis: 10 Ta or T1: 334 (16 with concomitant CIS); Tis: 5 | NA | No difference | Tis subgroup favours TICE (p ≤ 0.01) | NA |
| Del Giudice et al. (2022) [51] | TICE vs. RIVM (1-to-1 propensity score matched analysis) | 6 weeks + 3 weeks/3 years | 53 months | No concomitant CIS: 118; Concomitant CIS: 15 No concomitant CIS: 123; Concomitant CIS: 10 | NA | 56% at 5 years 48% at 5 years | 77% at 5 years 79% at 5 years | NA |
| Nowak et al. (2021) [52] | Moreau vs. TICE vs. RIVM | ≥5-dose induction + ≥2-dose maintenance | 40 months | No concomitant CIS: 110; Concomitant CIS: 28 No concomitant CIS: 222; Concomitant CIS: 46 No concomitant CIS: 134; Concomitant CIS: 45 | NA | 70.5% at 5 years 66.7% at 5 years 55.2% at 5 years | 84% at 5 years 85% at 5 years 77.8% at 5 years | NA |
| Koguchi et al. (2020) [53] | Tokyo | 6 weeks 1/2D vs. 6 weeks 1/2D + 2 weeks/3 years 1/2D | 36.2 months | Ta or T1: 60; Tis: 18 | NA | 65.0% (induction) vs. 89.5% (maintenance) at 3 years (no difference in Ta/T1 and Tis subgroups) | 97.5% (induction) vs. 97.4% (maintenance) | 100% (induction) vs. 84.2% (maintenance) |
| Griffiths et al. (2002) [54] | Connaught | 6-week induction | 41 months | Primary CIS: 23 CIS + Ta: 37 (21 concomitant + 16 secondary) CIS + T1: 75 (46 concomitant + 29 secondary) | 74% 70% 75% | NA | 80% at 5 years 82% at 5 years 51% at 5 years | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llano, A.; Chan, A.; Kuk, C.; Kassouf, W.; Zlotta, A.R. Carcinoma In Situ (CIS): Is There a Difference in Efficacy between Various BCG Strains? A Comprehensive Review of the Literature. Cancers 2024, 16, 245. https://doi.org/10.3390/cancers16020245
Llano A, Chan A, Kuk C, Kassouf W, Zlotta AR. Carcinoma In Situ (CIS): Is There a Difference in Efficacy between Various BCG Strains? A Comprehensive Review of the Literature. Cancers. 2024; 16(2):245. https://doi.org/10.3390/cancers16020245
Chicago/Turabian StyleLlano, Andres, Amy Chan, Cynthia Kuk, Wassim Kassouf, and Alexandre R. Zlotta. 2024. "Carcinoma In Situ (CIS): Is There a Difference in Efficacy between Various BCG Strains? A Comprehensive Review of the Literature" Cancers 16, no. 2: 245. https://doi.org/10.3390/cancers16020245
APA StyleLlano, A., Chan, A., Kuk, C., Kassouf, W., & Zlotta, A. R. (2024). Carcinoma In Situ (CIS): Is There a Difference in Efficacy between Various BCG Strains? A Comprehensive Review of the Literature. Cancers, 16(2), 245. https://doi.org/10.3390/cancers16020245






